Abstract
Background:
Studies have examined patterns of substance use among Men who have Sex with Men (MSM), but few have examined factors predicting transitioning from one substance use pattern to another. We investigated transitioning from one substance use pattern to another over a 12-year period (2004-2016) among the Multicenter AIDS Cohort Study participants.
Method:
Alcohol, marijuana, heroin, cocaine, poppers, uppers (e.g., methamphetamines) and erectile dysfunction(ED) medications use in the last 6 months from 3,568 US MSM was dichotomized (no/yes) to classify participants into substance use classes at each follow up visit. We fit latent transition models to calculate transition probabilities of moving from one substance use class to another over a 3, 4 and 6-year time period. Then fit regression models to identify factors associated with the probability of each participant staying in or moving from the same substance use class.
Results:
Overall, cocaine and ED medication use declined but marijuana and heroin use increased over 2004-2016. We observed most participants (84.6%-100%) stayed in the same class. Increased age was associated with transition from the Minimal-use class to the Alcohol-only class (aOR=1.06,95%CI:1.01-1.13;p<0.01) and non-White MSM reported lower odds of moving from the Alcohol-only class to the Alcohol-Popper class (aOR=0.50,95%CI:0.30-0.82;p<0.01). There were no difference in the transition probabilities by HIV-status.
Conclusion:
Despite decline in substance use in general, participants are highly stable in their choice of substances. However, treating MSM as a homogeneous group can lead to an under-appreciation of the diversity of prevention needs and treatment of substance using MSM.
Keywords: Substance use, Men who have sex with men, Latent transition analysis, MACS, LCA
1. Introduction
Men who have sex with men (MSM) continue to be at higher risk of HIV/ sexually transmitted infections (STIs) compared to the other at-risk populations, especially in North America (U.S. Centers for Disease Control and Prevention, 2018). For example, MSM, in the United States, are 44 times more likely to contract HIV (Purcell et al., 2012), whereas the Canadian MSM are 131 times more likely to contract HIV per year (Yang et al., 2016). MSM also have a high yearly incidence of many STIs compared to non-MSM, especially syphilis (Choudhri et al., 2018). Given the continued and disproportionately high HIV/STI prevalence among MSM, there is a pressing need to identify and understand factors contributing to and affecting higher rates of HIV/STI infections in this population.
Condomless anal sex (CAS) without consistent use of Pre-Exposure Prophylaxis (PrEP) among HIV-negative MSM, and/or in a serodiscordant partnership with detectable viral load remains the key factor for HIV/STI transmission, and psychosocial factors such as poorer mental health (e.g., social anxiety: Hart and Heimberg, 2005; depression: Hart, et al., 2017); childhood bullying and abuse experiences (Hart et al., 2018); experiences of violence and victimization (Mustanski et al., 2007; Stall et al., 2003); and recreational substance (ab)use (Mustanski et al., 2017; Parsons et al., 2012) are significant contributors of increased CAS. While there are multiple factors that account for increased substance use among MSM compared to non-MSM, the association between substance use and CAS among MSM is well documented (e.g., Race et al., 2017; Mustanski et al., 2007). For example, binge drinking in the context of a sexual episode is linked to increased likelihood of CAS (Newcomb, 2013), CAS with serodiscordant partners (Maisto and Simons, 2016; Vosburgh et al., 2012) and CAS with more partners (Hess et al., 2015). Furthermore, use of party drugs (e.g., cocaine, speed, or crystal meth) to enhance sexual experience (e.g., Party and Play: Frederick and Perrone, 2014) and/or attending privately or commercially organized gatherings “for the express purpose of having sex” (Friedman et al., 2008) are prevalent among MSM, and are significantly associated with increased CAS (Grov et al., 2014a; Grov et al., 2014b).
Some MSM may prefer one substance over another (e.g., downer like heroin over upper like crack cocaine) and use it consistently, however, experimenting with or using multiple substances simultaneously, or transitioning from one substance to another substance (or from one group of substances to another group of substances) over time is not uncommon among MSM (Card et al., 2018a; Card et al., 2018b; Lim et al., 2012; McCarty-Caplan et al.,, 2014; Wilkerson et al., 2018). For example, Wilkerson et al. (2018) identified four classes among methamphetamine using U. S. MSM: minimal use class; alcohol-marijuana-nitrite class, alcohol-cocaine-GHB-hallucinogens class, and alcohol-GHB-designer drugs-heroin class, whereas among a sample of Canadian MSM, Card et al (2018a) identified six classes characterizing ‘limited drug use’ (i.e., low use of all drugs, except alcohol), ‘conventional drug use’ (i.e., use of alcohol, marijuana, and tobacco), ‘club drug use’ (i.e., use of alcohol, cocaine, and psychedelics), ‘sex drug use’ (i.e., use of alcohol, crystal meth, GHB, poppers, and erectile dysfunction drugs), ‘street drug use’ (i.e., use of alcohol and street opioids) and ‘assorted drug use’ (i.e., use of most drugs). This heterogeneity in substance use and transitioning into different substances may influence HIV risk as differences in pharmacologic effects can influence sexual behavior (Harzke et al., 2009; Kruse et al., 2009). Further, MSM using only alcohol might have different treatment needs than MSM using a combination of stimulants (e.g., crystal, cocaine) in context of ‘Party N Play’ (Noor et al., 2018), and treatments designed for and targeting generalized substance (ab)use might not work well for types of specific substance use (Society of Clinical Psychology, 2020; Hart et al., 2019). For example, motivational interviewing-based therapies have strong evidence support for mixed substance use disorders but has less support for use with people who have difficulties managing use of stimulants such as cocaine or crystal methamphetamine (Society of Clinical Psychology, 2020). For HIV-positive MSM, substance (ab)use play a more complex role. A recent systematic review highlighted substance use as a coping mechanism for dealing with HIV diagnosis, as well as among the most common barriers to antiretroviral therapy adherence (Quinn and Voisin, 2020). Hence, knowing what substance or class of substances MSM use and whether they are staying at the same class over time or transitioning into different classes might have clinical relevance. Although research examining substance use pattern among MSM is increasing (Lim et al., 2015; McCarty-Caplan et al.,, 2014; Wilkerson et al., 2018), research examining consistency in substance use pattern among MSM is relatively low (Card et al., 2018a; Wilkinson et al., 2017).
Latent class analysis (LCA) is a popular approach to identify relatively homogenous subgroups within a heterogeneous population, favored for its ability to simultaneously consider multiple factors that reveal emergent grouping patterns. As a statistical modeling technique, LCA reveals unobserved heterogeneity in a population and creates meaningful subgroups (latent classes) from observed categorical indicators (McCutcheon, 1987). The LCA starts with the assumption that there is only one group, and subsequently estimates two (e.g., used /not used substance), three, four … and finally n different classes until a model is found that statistically fits the data (Magidson and Vermunt, 2004). Latent transition analysis (LTA) is an extension of the latent class model with the measurement (latent class) and structural (latent transition) components modeled simultaneously (Chung et al., 2007; Nylund, 2007). The relationship between unobserved (latent) variables across time points is described using a transition matrix or transition table. LTA model estimates transitions between categories within the latent classes at successive measurement points (e.g., between visits 1 and 2, between visits 2 and 3, between visits 3 and 4, and so on), using multinomial logistic regressions to produce logits (log-odds) for each cell of the transition table. Multinomial regression values are modeled using longitudinal data, thereby providing probabilities (probabilities being a function of logits) (Muthén and Muthén, 2015). The probability is that of individual i being in latent class k at 1 time point t, given that the individual was in latent class m at the previous time point, t − 1 (Chung et al., 2007; Muthén and Muthén, 2015). Substance use and HIV risk researchers have used LTA to quantify changes over time (e.g., MSM sexual risk: Wilkinson et al., 2017; adult drinking pattern: Staudt et al., 2018; injection drug users’ treatment need: Meacham et al., 2018; adolescent alcohol, tobacco, and marijuana use: Mistry et al. 2015) using longitudinal data; however, we are unaware of any study applying latent class and latent transition analyses to examine intraindividual stability in substance use over a longer time period (over 10 years) among MSM with and without HIV.
Considering the lack of existing research in this area, this analysis was exploratory in nature. Our objectives were, (1) to estimate the prevalence of substance use among a prospective cohort of US MSM with and without HIV over a 12-year time period (2004-2016), and see if there is a change in substance use over time, (2) to identify substance use patterns (i.e., classes) at each visit, (3) to examine probabilities of intra-individual stability in (or transition from) substance use classes over time, and (4) to identify demographic factors contributing to that transition.
2. Methods
2.1. Study design and participants
The Multicenter AIDS Cohort Study (MACS) is a prospective cohort study of the natural and treated history of HIV among MSM in 4 US regions: Baltimore, Maryland/Washington, DC; Chicago, Illinois; Los Angeles, California; and Pittsburgh, Pennsylvania/Columbus, Ohio. Since its inception in 1984, a total of 7,352 HIV-positive and HIV-negative MSM have been enrolled in the study over 4 periods: 4,954 in 1984–1985; 668 in 1987–1991; and 1,350 in 2001–2003 and 380 in 2011-current. Written informed consent was obtained from all study participants, and the MACS protocol was reviewed and approved by the institutional review boards of each participating center (Johns Hopkins University, Northwestern University, University of California Los Angeles, and University of Pittsburgh). The MACS study design has been described previously (Kaslow et al., 1987).
MACS participants return every 6-months for physical examinations, collection of biological specimen and laboratory testing, and completion of a detailed interview and questionnaires. The interview and questionnaires include demographic, psychosocial, behavioral and medical history data. Medical history data are collected by in-person interview and other data collected using Audio Computer Assisted Self-Interviewing. The questionnaires are available online at https://mwccs.org/.
This analysis utilizes a prospective cohort design to examine the substance use pattern at each 6-month visit, estimate probabilities of transitioning from one substance use class to another and identify factors predicting the transition. This analysis included data collected from recreational substance use questions from study visit 40 (data collection in October 2004) through study visit 64 (data collection in April 2016). The analytical sample included 3,568 (1,968 HIV-positive/1,620 HIV-negative) men who participated in the MACS at any visit between October 2004 and April 2016.
2.2. Measures
2.2.1. Substance use
Participants were asked to answer a series of questions related to “recreational or street drugs” that they might have used since their last visit. Substances include alcohol, marijuana, heroin, downers, ethyl chloride, GHB, poppers, speed ball, cocaine, crack, MDA (ecstasy, XTC, X or MDMA), PCP, opiate, stimulants (crystal, methamphetamines, speed, ice), and non-prescription sexual performance enhancing medications. In this analysis we included dichotomized (no/yes) alcohol, marijuana, heroin, poppers, cocaine, stimulants (crystal, methamphetamines, speed, ice), and sexual performance enhancing (ED) medications use. They were selected based on their prevalence of use (at least 5% of the participants reported the use).
2.2.2. HIV serostatus
HIV serostatus was assessed using enzyme-linked immunosorbent assay with confirmatory Western blot tests on all MACS participants at each participant’s initial visit and at every 6-month visit for participants who were initially HIV-seronegative. Standardized flow cytometry was used to quantify CD4+ T-lymphocyte subset levels.
2.2.3. Socio-demographic characteristics
Participants reported sociodemographic characteristics including their date of birth, education level, annual income, and ethnic/racial background (measured at baseline only). We calculated age at each visit using date of birth and was treated as continuous and time-variant. Income was also treated as a continuous measure with $10,000 (USD) increment and treated as time-variant. Educational level (high school degree or less, some college, 4-year degree, some graduate work and graduate degree) was measured at each visit, and treated as time-variant.
2.3. Statistical Analysis
We carried out this analysis in four steps. First, we examined socio-demographic characteristics, means, standard deviations, and normality assumptions of the measures. Descriptive statistics were generated at the index visit using frequencies/percentages and medians/ interquartile ranges (IQRs) where appropriate. The index visit was defined as a participant's first visit during the observation period between October, 2004 and April, 2016. We also calculated proportions of substance use at each visit and compared changes in proportions over time using generalized estimating equations with robust estimators and unstructured correlation matrix addressing non-independence of data across visits, adjusting for demographic characteristics.
Next, we used LCA to identify substance use classes (type of substance used) at each visit based on reported substance use in the last 6 months. Using Mplus 7.4 (Muthén & Muthén, 2015), a series of preliminary latent models with increasing number of classes were estimated to identify a model with the optimal number of classes at each visit. We used the sample adjusted Bayesian Information Criterion (BIC) and the Lo-Mendel-Rubin likelihood ratio test (LMR-LRT: Lo et al., 2001), and bootstrapped likelihood ratio test (BLRT: McLachlan and Peel, 2000) to identify how many classes best fit the data (Magidson and Vermunt, 2004; Nylund et al., 2007).
In the third step, LTA was used to assess intra-individual stability of substance use patterns from one visit to the next. We divided the 12-year time period into 1-, 2-, 3-, 4- and 6-year intervals, however, considering computational time and non-convergent model (1- and 2-year interval models did not converge), and to have adequate time intervals to assess meaningful transition from one substance to another, we fit LTA with 3, 4 and 6-year time intervals. In other words, we fit LTA to estimate probabilities of each participant transitioning from the identified class (identified by LCA at the previous step) at year 2004 to the identified class at year 2007, and from 2007 to 2010, 2010 to 2013 and 2013 to 2016 (3-year interval); from 2004 to 2008, 2008 to 2012, and 2012 to 2016 (4-year interval); and from 2004 to 2010, and 2010 to 2016 (6-year interval). As this analysis was exploratory and to identify true transition between substance use classes at subsequent visits, we did not constrain the number of classes at any of the follow up visits.
Once the LTA model was identified, we transferred class membership assignment (i.e., class 1 = 1; class 2 = 2, and so on) at years 2004, 2007, 2008, 2010, 2012, 2013 and 2016 for each participant into STATA 13.1 (Statacorp LP, 2013). Next, we fit a series of multivariate regression models predicting transition probabilities of each participant between classes from 2004 to 2016 by 3, 4 and 6-year intervals, separately.
All latent variable analyses were done with a full-information maximum likelihood estimator with robust standard errors. These models were estimated under a missing at random assumption using all available data. We used several starting values to avoid the issue of local maxima and to ensure all values converged to identical solutions (Muthén and Muthén, 2015). In this study, we specified 5000 sets of random starting values for the initial stage and 500 optimizations for the final stage of maximum likelihood optimization. All statistical tests were two-tailed.
3. RESULTS
3.1. Participants
A majority of the participants (mean age 42.6 years; Std. deviation = 9.6) were non-Hispanic White (67.8%), had above high-school education (66.2%), and reported an income of less than thirty-thousand US dollars in the last year (63.7%; see Table 1).
Table 1.
Socio-Demographic Characteristics of MACS participants by HIV status at index visit.
| HIV Negative (n=1620) |
HIV Positive (n=1948) |
All Participants (N=3568) |
|
|---|---|---|---|
| Follow-up (six months), median (IQR) | 11 (1 - 14) | 12 (1 - 15) | 11 (1 - 14) |
| Age, median (IQR), years | 44.4 (38.5 - 51.2) | 41.1 (35.7 - 46.3) | 42.5 (36.7 - 48.5) |
| Income in US Dollar, median (IQR) | 10-19.9K (<10K – 40-49.9K) | 20-29.9K (<10K - 40-49.9K) | 20-29.9K (<10K - 40-49.9K) |
| Race/ethnicity, n (%) | |||
| Non-Hispanic white | 1209 (74.6) | 1210 (62.2) | 2419 (67.8) |
| Non-Hispanic black | 331 (20.4) | 574 (29.5) | 905 (25.4) |
| American Indian or Alaskan Native | 28 (1.7) | 77 (3.9) | 105 (2.9) |
| Asian | 11 (0.7) | 9 (0.5) | 20 (0.6) |
| Hispanic | 135 (8.3) | 285 (14.6) | 420 (11.8) |
| Native Hawaiian or Pacific Islander | 2 (0.1) | 2 (0.1) | 4 (0.1) |
| Other | 12 (0.7) | 23 (1.2) | 35 (0.9) |
| Multi-racial | 27 (1.7) | 51 (2.6) | 78 (2.29) |
| Education Level, n (%) | |||
| 12th Grade or Less | 170 (29.7) | 329 (36.3) | 499 (33.8) |
| Some College | 149 (26.5) | 294 (32.5) | 443 (29.9) |
| Four Year Degree | 117 (20.5) | 143 (15.8) | 260 (17.6) |
| Some Graduate Work | 45 (7.9) | 52 (5.7) | 97 (6.6) |
| Post-Graduate Degree | 91 (15.9) | 88 (9.7) | 179 (12.1) |
| Location, n (%) | |||
| Baltimore | 150 (22.49) | 143 (30.6) | 293 (25.8) |
| Chicago | 49 (7.3) | 107 (22.9) | 156 (13.7) |
| Pittsburgh | 111 (16.6) | 77 (16.5) | 188 (16.5) |
| Los Angeles | 360 (53.7) | 141 (30.1) | 501 (44.0) |
Note. The index visit was defined as a participant's first visit during the observation period between October, 2004 and April; 2016; IQR: Inter-quartile range.
3.2. Substance use over time
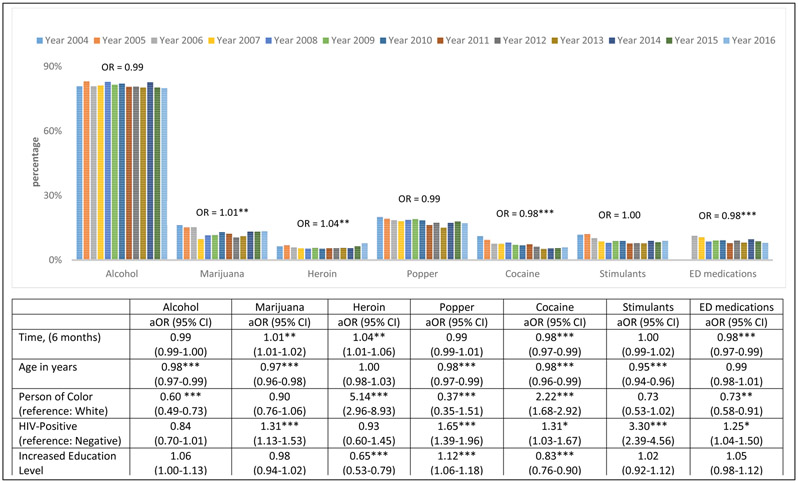
Alcohol was the most reported substance of use followed by poppers, marijuana, ED medications, stimulants (crystal, methamphetamines, speed, ice), cocaine, and heroin (see Figure 1). The test of trend in proportions over time (including all 6-month visits between 2004 and 2016, and adjusting for age, HIV-status, race/ethnicity and educational level) indicated that overall cocaine, and ED medications use decreased, but marijuana and heroin use increased (see Figure 1). Increased age (i.e., growing older) was associated with decreased use of substances over time. Non-Hispanic Whites were more likely to report increased use of alcohol, poppers, and ED medications whereas non-White participants were more likely to report increased use of heroin and cocaine over time. Participants with HIV-positive status had higher odds of using marijuana, poppers, cocaine, stimulants and ED medications.
Figure 1: Prevalence of substance use by year, and odds of change in each substance use over time (2004 to 2016), MACS Study.
Note. OR = Odds Ratio; models are adjusted for age, race/ethnicity, HIV-Status, and education level; Note. Education level was treated as continuous variable; *p <0.05, **p <0.01, ***p <0.001
3.3. Identification of substance use classes
At each visit, we fit LCA models with 2, 3, 4 and 5 classes and compared them on fit indices. Based on relative lower aBIC values and smaller p –values on LMR-LR and BLTR tests we identified that a 3-class solution best fit the year 2004, 2007 and 2008 data, and a 4-class solution best fit the year 2010, 2012, 2013 and 2016 data (data not shown). Considering the relatively lower/higher conditional probability of reporting of alcohol, poppers, marijuana, stimulants, cocaine, heroin and ED medications use, we found a Minimal use class (18% of the sample; no/minimal use of all substances), an Alcohol only class (47% of the sample; higher alcohol use than Minimal use class) and an Alcohol-Marijuana-Popper-Cocaine use class (35% of the sample; higher alcohol, marijuana, popper, cocaine use compared to other two classes) in 2004.
In subsequent years results were similar with Minimal use class increasing slightly to 20% by 2016, Alcohol only class quite steady between 41-43%. Multiple use class expanded beginning in 2012 to include Marijuana-Cocaine use class (8%) and an Alcohol-Marijuana-Popper-ED use class (31%), while in 2013 combinations differed as Alcohol-Popper-ED use class (19%) and an Alcohol-Marijuana-Popper-Cocaine use class (19%) and in 2016 they were Alcohol-Popper use class (22%) and an Alcohol-Marijuana-Cocaine-ED use class (18%) (data not shown).
3.4. Transition between classes over 3, 4 and 6-year interval
We performed three separate latent transition analyses by 3, 4 and 6-year interval and the results are reported in Table 2. Row percentages represent the percentage of participants moved from (or stayed at) the identified class at reference year (T) to the class at follow up year (T + c). We observed higher percentages in the cross diagonal cells from top left to bottom right cells indicating intra-individual stability across classes (i.e., higher percentage of participants staying in the same class). While results were generally similar using the different intervals, the cross diagonal percentages were slightly higher with the shorter 3-year interval (from 84.6% to 100%), than for the lower 6-year interval (72.2% to 95.7%).
Table 2:
Percentage (row) of participants who transitioned to another substance use class during follow-up, MACS Study (2004-2016)
| Time-interval (Ref year, T -→ follow up year, T +c) |
Percentage of participants transitioning and non-transitioning between classes |
||||
|---|---|---|---|---|---|
| 3-year interval | |||||
| Year 2004 ------→ Year 2007 | n | Minimal Use Class (n=373) | Alcohol Only (n=1156) | Alcohol-Marijuana-Popper-Cocaine Class (n=647) | |
| Minimal Use Class | 38 8 |
83 | 16.7 | 0.3 | |
| Alcohol Only | 11 40 |
0 | 100 | 0 | |
| Alcohol-Marijuana-Popper-Cocaine Class | 64 8 |
0.7 | 0.00 | 99.3 | |
| Year 2007 ------→ Year 2010 | Minimal Use Class (n=376) | Alcohol Only (n=997) | Alcohol-Popper Class (n=177) | Alcohol-Marijuana-Popper-Cocaine-ED Class (n=626) | |
| Minimal Use Class | 37 3 |
92.6 | 3.6 | 0 | 3.8 |
| Alcohol Only | 11 56 |
1.6 | 84.6 | 12.9 | 0.8 |
| Alcohol-Marijuana-Popper-Cocaine Class | 64 7 |
1.9 | 1.7 | 7.1 | 89.4 |
| Year 2010 ------→ Year 2013 | Minimal Use Class (n=398) | Alcohol Only (n=981) | Alcohol-Popper-ED Class (n=181) | Alcohol-Marijuana-Popper-Cocaine Class (n=616) | |
| Minimal Use Class | 37 6 |
95.9 | 3 | 1.1 | 0 |
| Alcohol Only | 4.6 | 91.8 | 1.0 | 2.5 | |
| Alcohol-Popper Class | 99 7 |
0 | 0 | 100 | 0 |
| Alcohol-Marijuana-Popper-Cocaine-ED Class | 62 6 |
3.6 | 3.9 | 0 | 92.5 |
| Year 2013 ------→ Year 2016 | Minimal Use Class (N=390) | Alcohol Only Class (n=993) | Alcohol-Popper Class (n=169) | Alcohol-Marijuana-Cocaine-ED Class (n=624) | |
| Minimal Use Class | 39 8 |
95.4 | 0 | 0.4 | 4.2 |
| Alcohol Only | 98 1 |
0 | 100 | 0 | 0 |
| Alcohol-Popper-ED Class | 18 1 |
0 | 13.9 | 86.1 | 0 |
| Alcohol-Marijuana-Popper-Cocaine Class | 61 6 |
0 | 0 | 0 | 100 |
| 6-year interval | |||||
| Year 2004 ------→ Year 2010 | Minimal use Class (n=328) | Alcohol Only Class (n=857) | Alcohol-Popper Class (n=194) | Alcohol-Marijuana-Cocaine-ED Class (n=571) | |
| Minimal Class | 34 4 |
72.2 | 20.6 | 2.8 | 4.4 |
| Alcohol Only Class | 10 28 |
0 | 83.6 | 16.4 | 0 |
| Alcohol-Marijuana-Popper-Cocaine Class | 57 8 |
2.4 | 0.1 | 5.4 | 92.2 |
| Year 2010 ------→ Year 2016 | Minimal use Class (n=361) | Alcohol Only Class (n=847) | Alcohol-Popper Class (n=173) | Alcohol-Marijuana-Cocaine-ED Class (n=569) | |
| Minimal use Class | 32 8 |
92.5 | 0 | 4.6 | 2.9 |
| Alcohol Only Class | 85 7 |
9.2 | 89.5 | 0 | 1.3 |
| Alcohol-Popper Class | 19 4 |
0 | 18.2 | 81.8 | 0 |
| Alcohol-Marijuana-Cocaine-ED Class | 57 1 |
1.8 | 2.5 | 0 | 95.7 |
Furthermore, we observed higher transition (i.e., higher percentage of participants not staying in the same class) from the Minimal use class to other classes (i.e., increased use over time) rather than from other classes to the Minimal use class (i.e., decreased use over time). For example, for 3-year interval (2004-2007), 17% of the participants transitioned from the Minimal use class to the Alcohol only class (16.7%) and to the Alcohol-Marijuana-Popper-Cocaine use class (0.30%), but only 0.7% of the participants transitioned to the Minimal use class from the Alcohol-Marijuana-Popper-Cocaine use class and none from the Alcohol only class. For 4-year interval (2004-2008), 20.6% of the participants transitioned from the Minimal use class, but none (0%) transitioned to the Minimal use class. However, over a larger 6-year interval (2004-2010) we observed slightly more transitions (e.g., 27.8% from, and 2.4% to the Minimal use class).
3.5. Factors predicting transition
Considering similar higher intra-individual stability between classes in 3-year and 4-year interval LTA models (see Table 2), we fit regression models to identify factors for only 3 and 6-year interval transitions. We fit models for overall transition (i.e., any transition between classes: 0= stayed in the same respective class and 1= moved to any other class) as well as class-specific transition (i.e., 0= stayed in the same class and 1 = moved to another class from the original class only). Increased age (i.e., growing older) was positively associated with transition from the Minimal use class to the Alcohol only class during 2004-2007 (OR = 1.06, 95% CI: 1.01-1.13; p < 0.01) as well as during 2004-2010 (OR = 1.07, 95% CI: 1.01-1.1; p < 0.05), but was negatively associated with transition from the Alcohol only use class to the Alcohol-Popper use class during 2007-2010 (OR = 0.98, 95% CI: 0.96-0.99; p < 0.05). Non-White participants had lower odds of moving from one class to another class compared to white participants. Higher educational level was associated with transition from Alcohol only use class to Alcohol-Popper use class during 2007-2010 (OR = 1.27, 95% CI: 1.11-1.46; p < 0.001) as well as between 2004-2010 (OR = 1.22, 95% CI: 1.07-1.38; p < 0.01); and from Alcohol-Marijuana-Popper-Cocaine-ED use class to Alcohol-Popper use class during 2007-2010 (OR = 1.41, 95% CI: 1.04-1.92; p < 0.001). We did not observe any statistically significant differences on intra-class transition by HIV-status (see Table 3).
Table 3:
Predictors of transition to another substance use class, MACS Study (2004-2016)
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
|---|---|---|---|---|---|
| 3 Year Interval: Overall transition | 2004-2007 | 2007-2010 | 2010-2013 | 2013-2016 | |
| Moved/stayed = 17/2159 | Moved/stayed =189/1987 | Moved/stayed =42/2134 | Moved/stayed =20/2156 | ||
| Age in years | 1.06** (1.01-1.11) | 0.99 (0.98-1.01) | 1.02 (0.99-1.06) | 0.96* (0.93-0.99) | |
| Person of Color (Reference: White) | 0.93 (0.33-2.67) | 0.46*** (0.30-0.71) | 0.73 (0.35-1.51) | 0.55 (0.18-1.67) | |
| HIV-Positive (Reference: Negative) | 0.64 (0.22-1.93) | 1.06 (0.77-1.46) | 1.07 (0.57-1.98) | 1.67 (0.60-4.62) | |
| Increased Education Level | 1.18 (0.70-1.97) | 1.36*** (1.21-1.52) | 1.12 (0.88-1.43) | 1.07 (0.74-1.56) | |
| 3 Year Interval: Class Specific transition | Minimal use to Alcohol only class | Alcohol only to Alcohol-Popper class | Alcohol-Marijuana-Popper-Cocaine-ED to Alcohol-Popper class | Alcohol-Popper to Alcohol only class | |
| Moved/stayed = 16/372 | Moved/stayed = 158/995 | Moved/stayed = 19/623 | Moved/stayed = 12/169 | ||
| Age in years | 1.06* (1.01-1.13) | 0.98* (0.96-0.99) | 1.00 (0.95-1.06) | 0.97 (0.91-1.03) | |
| Person of Color (Reference: White) | 0.62 (0.21-1.84) | 0.50** (0.30-0.82) | 0.14 (0.18-1.05) | 0.44** (0.26-0.72) | |
| HIV-Positive (Reference: Negative) | 0.45 (0.14-1.49) | 1.37 (0.95-1.98) | 0.63 (0.25-1.64) | 0.70 (0.18-2.73) | |
| Increased Education Level | 1.35 (0.84-2.19) | 1.27*** (1.11-1.46) | 1.41* (1.04-1.92) | 1.54 (0.78-3.06) | |
| 6 Year Interval: Overall transition | 2004-2010 | 2010-2016 | |||
| Moved/stayed = 217/1733 | Moved/stayed = 71/1879 | ||||
| Age in years | 1.01 (0.99-1.02) | 1.01 (0.99-1.04) | |||
| Person of Color (Reference: White) | 0.57 (0.39-0.84) | 0.67 (0.38-1.18) | |||
| HIV-Positive (Reference: Negative) | 1.04 (0.76-1.40) | 1.03 (0.63-1.68) | |||
| Increased Education Level | 1.32*** (1.18-1.47) | 1.03 (0.88-1.22) | |||
| 6 Year Interval: Class specific transition | Minimal use to Alcohol only class | Alcohol only to Alcohol-Popper use class | Alcohol-Marijuana-Popper-Cocaine-ED to Alcohol-Popper use class | Alcohol only class to Minimal class | Alcohol-Popper class to Alcohol only class |
| Moved/stayed = 16/324 | Moved/stayed = 187/841 | Moved/stayed = 6/568 | Moved/stayed = 36/821 | Moved/stayed = 26/168 | |
| Age in years | 1.07* (1.01-1.14) | 0.99 (0.97-1.01) | 1.02 (0.90-1.16) | 1.01 (0.98-1.04) | 1.03 (0.97-1.10) |
| Person of Color (Reference: White) | 1.02 (0.36-2.91) | 0.54* (0.34-0.87) | - | 0.73 (0.33-1.64) | 1.22 (0.38-3.97) |
| HIV-Positive (Reference: Negative) | 0.52 (0.18-1.56) | 1.40 (0.99-1.97) | 0.41 (0.08-2.25) | 1.19 (0.61-2.35) | 1.26 (0.51-3.12) |
| Increased Education Level | 1.32 (0.89-1.96) | 1.22** (1.07-1.38) | 1.26 (0.86-3.34) | 0.93 (0.74-1.16) | 0.93 (0.63-1.37) |
Note. Education level was treated as continuous variable
4. DISCUSSION
In one of the largest and longest running cohorts of MSM, we observed that substance use was prevalent and using multiple substances simultaneously is not uncommon. Results indicated an overall decline in cocaine, and ED medications use but an increase in marijuana and heroin use over time. Similar trends were also reported by other national surveys of MSM (see Sanchez et. al., 2019; Raymond et al., 2013). Further, results highlighted high intra-individual stability, that is, MSM maintained use of the same substance(s) over longer periods of time.
Similar to previous research, our latent class analyses of substance use patterns at each visit indicated that this sample of MSM was heterogeneous rather than a homogenous group in terms of substance use (see Card et al., 2018b; Lim et al., 2015; Wilkerson et al., 2018). Data consistently divided participants into three classes: a Minimal use class, an Alcohol use class and a Multiple substance use class over follow-up time. However, we observed a three class solution (Minimal use, Alcohol use and Multiple substance use class) during the early cohort (2004-2009) and a four-class solution (Minimal use, Alcohol use, Alcohol-Popper use and Multiple substance use class) in later years (2010-2016). We do not exactly know why, but increased sample size and/or decreased cocaine and ED medications use might have an impact on, and divided the Multiple substance use class into two separate classes. Another explanation could be it was simply an older age-cohort effect (mean age (sd) = 53.2 (9.9) at 2010) as we have observed reduced use in each substances with increased age (see Figure 1).
Latent transition analyses indicated high intra-individual stability across substance use classes over time though there were reductions in specific uses. For example, the sizes of the Minimal use class ranged from 17% to 20%, and from 42% to 49% for the Alcohol use class. Results suggested that this sample of MSM was stable in terms of their choice of substance, and less likely to change their choice of drug across shorter periods of time. Card et al. (2018a) also reported strong longitudinal stability (ICC > 0.97) across classes over 2.5 years. In 3-year intervals we observed 0% - 15% participants transition between classes and in 6-year intervals the percentages transitioning increased to 5% - 28% between classes. Furthermore, we observed comparatively higher transition from the Minimal use class to the other classes (i.e., increased use) rather than from the other classes to the Minimal use class (i.e., decreased use). During the early cohort, (2004-2007) increased age was positively associated with transition from the Minimal use class to Alcohol only class and was negatively associated with transition from the Alcohol-Popper use class to Alcohol only class during later cohort (2007-2010). These results support the notion that at younger age, users are in exploration and in transition to more substance use, and at older age, users are in stable stage.
Higher educational level was associated with transition from the Alcohol only use class to the Alcohol-Popper use class, and from the Alcohol-Marijuana-Popper-Cocaine-ED use class to the Alcohol-Popper use class during 2007-2010. We find the ‘two-edged’ effects of higher education on transition quite interesting. In this sample age, education and income are positively correlated (age-income: r = 0.24; p <0.001; age-education: r = 0.30; p <0.001; education-income: r = 0.53; p <0.001). Higher education level may be a proxy of increased age as well as increased financial resources (i.e., income) that predicting transition to increased substance use. Another possibility is that increased education level may be a proxy of increased awareness and knowledge about harmful effects of substance abuse that predicted transition to decreased substance use. Though we observed the effect of HIV-status on individual substance use over time we did not observe any differences on intra-class transition by HIV-status. Our results are consistent with breadth of research showing higher prevalence of substance use (as well multiple substance use) (for a review see Melendez-Torres and Bourne, 2016) and continued use over time (see Adams et al., 2018) among HIV-positive MSM.
We acknowledge several limitations of our analyses. We relied on self-reported substance use, which presented the possibility of recall bias and/or under/over-reporting. Further, dichotomized substance use variables were used for LCA and LTA, and this categorization undermines richness of data as it ignores heterogeneity in both frequency of use and nature of use. Thus, we did not capture transition in frequency of use, i.e, from frequent use to occasional use. Second, this study used a nonrandom convenience sample and was restricted to HIV-positive and -negative MSM in 4 major metropolitan regions. Therefore, these results may not be generalizable to other MSM in the general population. Due to non-convergence, we were unable to fit models assessing shorter time-intervals. Finally, due to low cell counts, we could not explore race/ethnicity further.
5. CONCLUSION
In summary our results highlight several key points. LCA and LTA show that participating MSM are a heterogeneous group in terms of substance use and simultaneous use of multiple substances is prevalent. Despite overall decline in substance use in general, participants were highly stable in terms of their choice of substances. The small transitions observed between classes over time were not uni-dimensional i.e., not linear progression from single substance use (less severe use) to multiple substance use (more severe use) or vice-versa. Even considering the limitations of the study, results have practical implications. First, substance use treatment should be substance-specific. Treatment targeting alcohol use might not work for crystal methamphetamine or cocaine use. Second, treatment developers should be mindful of the fact that MSM who use multiple substances simultaneously might have different treatment needs than single substance using MSM (e.g., Meacham et al., 2018). Third, reason to and/or the context of substance use as well as the preferred sex role (i.e., top/bottom) should also be considered in treatment development. For example, if amphetamine like stimulant is used to enhance sexual sensation, or popper is used to facilitate anal sex by increasing blood flow and relaxing sphincter muscles (e.g., a bottom in a Party and Play: Frederick and Perrone, 2014; Friedman et al., 2008), or for being a member of a Scene (e.g. micro-culture; Noor et al., 2018) treatment should target the reason, the context as well as preference rather than treating them in silos. Finally, if we consider long-term stable substance use of our participating MSM as a chronic relapsing illness (NIDA, 2016), our results of longitudinal stability, especially for multiple substance use class highlights the gap in the efficacy of the substance use treatments. Either our participating MSM are not accessing the treatment, or the treatment may not be reaching them; or if they do might not be very successful for substances like, alcohol, marijuana, heroin and stimulants. Practitioners should consider longer treatment duration as well as extended post-treatment follow-up assessment point to assess true effect of the treatment. We hope these findings may be helpful as an empirical basis for designing tailored and targeted prevention and treatment interventions for the heterogeneous substance use pattern within this population. We caution against treating MSM as a homogeneous groups that would lead to an under-appreciation of the diversity of prevention needs and treatment that would be appropriate.
Highlights.
Examined change in substance use over a 12-year period among 3,568 U. S. MSM
Using LTA investigated transitioning from one class of substance use to another
Alcohol use was the most prevalent followed by marijuana, popper, cocaine, and ED
Overall decline in cocaine, and ED use but an increase in marijuana and heroin
Participants maintained use of the same substance(s) over longer periods of time
Funding and Acknowledgement:
Data used in this manuscript were collected by the Multicenter AIDS Cohort Study (MACS), now the MACS/WIHS Combined Cohort Study (MWCCS) The contents of this publication are solely the responsibility of the authors and do not represent the official views of the National Institutes of Health (NIH).
The MWCCS (Principal Investigators):Baltimore/DC (Brown & Margolick), U01-HL146201-01; Data Analysis and Coordination Center (D’Souza, Gange & Golub), U01-HL146193-01; Chicago-Northwestern CRS (Wolinsky), U01-HL146240-01; Los Angeles CRS (Detels), U01-HL146333-01; Pittsburgh CRS (Martinson & Rinaldo), U01-HL146208-01.
The MWCCS is funded primarily by the National Heart, Lung, and Blood Institute (NHLBI), with additional co-funding from the Eunice Kennedy Shriver National Institute Of Child Health & Human Development (NICHD), National Human Genome Research Institute (NHGRI), National Institute On Aging (NIA), National Institute Of Dental & Craniofacial Research (NIDCR), National Institute Of Allergy And Infectious Diseases (NIAID), National Institute Of Neurological Disorders And Stroke (NINDS), National Institute Of Mental Health (NIMH), National Institute On Drug Abuse (NIDA), National Institute Of Nursing Research (NINR), National Cancer Institute (NCI), National Institute on Alcohol Abuse and Alcoholism (NIAAA), National Institute on Deafness and Other Communication Disorders (NIDCD), National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The MACS/WIHS Combined Cohort Study website is located at http://www.mwccs.org/.
CNO is supported by the National Institute on Drug Abuse (K01-DA047912).
The authors are indebted to the participants of the Multicenter AIDS Cohort Study (MACS).
Footnotes
Conflict of interest: Authors declare none.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards and conducted under the oversight of the research ethics boards of all participating sites.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adams JW, Bryant KJ, Edelman JE, Fiellin DA, Gaither JR, Gordon AJ, Gordon KS, Kraemer KL, Mimiaga MJ, Operario D, Tate JP, 2018. Association of cannabis, stimulant, and alcohol use with mortality prognosis among HIV-infected men. AIDS Behav. 22, 1341–1351. doi: 10.1007/s10461-017-1905-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Card KG, Armstrong HL, Carter A, Cui Z, Wang L, Zhu J, Lachowsky NJ, Moore DM, Hogg RS, Roth EA, 2018a. Assessing the longitudinal stability of latent classes of substance use among gay, bisexual, and other men who have sex with men. Drug Alcohol Depend. 188, 348–355. doi: 10.1016/j.drugalcdep.2018.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Card KG, Armstrong HL, Carter A, Cui Z, Wang L, Zhu J, Lachowsky NJ, Moore DM, Hogg RS, Roth EA, 2018b. A latent class analysis of substance use and culture among gay, bisexual and other men who have sex with men. Cult Health Sex. 20, 1424–1439. doi: 10.1080/13691058.2018.1439186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U. S. Centers for Disease Control and Prevention. (2018). HIV and gay and bisexual men. Retrieved from https://www.cdc.gov/hiv/pdf/group/msm/cdc-hiv-msm.pdf
- Choudhri Y, Miller J, Sandhu J, Leon A, Aho J, 2018. Sexually transmitted infections: Infectious and congenital syphilis in Canada, 2010–2015. Can Commun Dis Rep 44, 43–48. doi: 10.14745/ccdr.v44i02a02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung H, Walls TA, Park Y, 2007. A latent transition model with logistic regression. Psychometrika 72, 413–435. doi: 10.1007/s11336-005-1382-y [DOI] [Google Scholar]
- Frederick BJ Perrone D, 2014. “Party N Play” on the Internet: Subcultural formation, craigslist, and escaping from stigma. Deviant Behav. 35, 859–884. doi: 10.1080/01639625.2014.897116 [DOI] [Google Scholar]
- Friedman SR, Bolyard M, Khan M, Maslow C, Sandoval M, Mateu-Gelabert P, Krauss B, Aral SO, 2008. Group sex events and HIV/STI risk in an urban network. J. Acquir. Immune Defic. Syndr 49, 440–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Rendina HJ, Breslow AS, Ventuneac A, Adelson S, Parsons JT, 2014a. Characteristics of men who have sex with men (MSM) who attend sex parties: results from a national online sample in the USA. Sex. Transm. Infect 90, 26–32. doi: 10.1136/sextrans-2013-051094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Rendina HJ, Ventuneac A, Parsons JT, 2014b. Partners met via sex parties present significantly greater odds for condomless anal sex among MSM: An event-level analysis of venues where male partners are met. J. Acquir. Immune Defic. Syndr 67(5), 564–568. doi: 10.1097/QAI.0000000000000343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart TA, Noor SW, Vernon JR, Antony MM, Gardner S, O'Cleirigh C 2019. Integrated Cognitive-Behavioral Therapy for Social Anxiety and HIV/STI Prevention for Gay and Bisexual Men: A Pilot Intervention Trial. Behav. Ther E-pub 9 September. doi: 10.1016/j.beth.2019.09.001 [DOI] [PubMed] [Google Scholar]
- Hart TA, Noor SW, Vernon JR, Kidwai A, Roberts K, Myers T, Calzavara L, 2018. Childhood maltreatment, bullying victimization, and psychological distress among gay and bisexual men. J. Sex Res 55, 604–616. doi: 10.1080/00224499.2017.1401972 [DOI] [PubMed] [Google Scholar]
- Hart TA, Noor SW, Adam BD, Vernon JR, Brennan DJ, Gardner S, Husbands W, Myers T, 2017. Number of psychosocial strengths predicts reduced HIV sexual risk behaviors above and beyond syndemic problems among gay and bisexual men. AIDS Behav. 21, 3035–3046. doi: 10.1007/s10461-016-1669-2 [DOI] [PubMed] [Google Scholar]
- Hart TA, Heimberg RG, 2005. Social anxiety as a risk factor for unprotected intercourse among gay and bisexual male youth. AIDS Behav. 9, 505–512. doi: 10.1007/s10461-005-9021-2 [DOI] [PubMed] [Google Scholar]
- Harzke AJ, Williams ML, Bowen AM, 2009. Binge use of crack cocaine and sexual risk behaviors among African-American, HIV-positive users. AIDS Behav. 13, 1106–1118. doi: 10.1007/s10461-008-9450-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hess KL, Chavez PR, Kanny D, DiNenno E, Lansky A, Paz-Bailey G, NHBS Study Group, 2015. Binge drinking and risky sexual behavior among HIV-negative and unknown HIV status men who have sex with men, 20 US cities. Drug Alcohol Depend. 147, 46–52. doi: 10.1016/j.drugalcdep.2014.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaslow RA, Ostrow DG, Detels R, Phair JP, Polk BF, Rinaldo CR Jr, Multicenter AIDS Cohort Study, 1987. The Multicenter AIDS Cohort Study: rationale, organization, and selected characteristics of the participants. Am. J. Epidemiol 126, 310–318. doi: 10.1093/aje/126.2.310 [DOI] [PubMed] [Google Scholar]
- Kruse GR, Barbour R, Heimer R, Shaboltas AV, Toussova OV, Hoffman IF, Kozlov AP, 2009. Drug choice, spatial distribution, HIV risk, and HIV prevalence among injection drug users in St. Petersburg, Russia. Harm Reduct. 6, 22–29. doi: 10.1186/1477-7517-6-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim SH, Ostrow D, Stall R, Chmiel J, Herrick A, Shoptaw S, Kao U, Carrico A, Plankey M, 2012. Changes in stimulant drug use over time in the MACS: evidence for resilience against stimulant drug use among men who have sex with men. AIDS Behav. 16, 151–158. doi: 10.1007/s10461-010-9866-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim SH, Cheung DH, Guadamuz TE, Wei C, Koe S, Altice FL, 2015. Latent class analysis of substance use among men who have sex with men in Malaysia: Findings from the Asian Internet MSM Sex Survey. Drug Alcohol Depend. 151, 31–37. doi: 10.1016/j.drugalcdep.2015.02.040 [DOI] [PubMed] [Google Scholar]
- Lo Y, Mendell NR, Rubin DB, 2001. Testing the number of components in a normal mixture. Biometrika 88, 767–778. doi: 10.1093/biomet/88.3.767 [DOI] [Google Scholar]
- McLachlan G, Peel D, 2000. Finite Mixture Models. Wiley, New York [Google Scholar]
- Magidson J, Vermunt J, (2004). Latent Class Models In Kaplan D (Ed.), The SAGE Handbook of Quantitative Methodology for the Social Sciences (175–198). The United States of America: Sage Publications Inc. [Google Scholar]
- Maisto SA, Simons JS, 2016. Research on the effects of alcohol and sexual arousal on sexual risk in men who have sex with men: implications for HIV prevention interventions. AIDS Behav. 20(1), 158–172. doi: 10.1007/s10461-015-1220-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty-Caplan D, Jantz I, Swartz J, 2014. MSM and drug use: a latent class analysis of drug use and related sexual risk behaviors. AIDS Behav. 18, 1339–1351. doi: 10.1007/s10461-013-0622-x [DOI] [PubMed] [Google Scholar]
- McCutcheon AL (1987). Latent class analysis. Newbury Park, CA: Sage Publications Inc. [Google Scholar]
- Meacham MC, Roesch SC, Strathdee SA, Gaines TL, 2018. Perceived treatment need and latent transitions in heroin and methamphetamine polydrug use among people who inject drugs in Tijuana, Mexico. J. Psychoact. Drugs 50, 62–71. doi: 10.1080/02791072.2017.1370747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melendez-Torres GJ, Bourne A, 2016. Illicit drug use and its association with sexual risk behaviour among MSM: more questions than answers? Curr. Opin. Infect. Dis 29, 58–63. doi: 10.1097/QCO.0000000000000234 [DOI] [PubMed] [Google Scholar]
- Mistry R, Heinze JE, Cordova D, Heish HF, Goldstick JE, Ayer SM, Zimmerman MA, 2015. Transitions in current substance use from adolescence to early-adulthood. J. Youth Adolesc 44, 1871–1883. doi: 10.1007/s10964-015-0309-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Phillips G, Ryan DT, Swann G, Kuhns L, Garofalo R, 2017. Prospective effects of a syndemic on HIV and STI incidence and risk behaviors in a cohort of young men who have sex with men. AIDS Behav. 21, 845–857. doi: 10.1007/s10461-016-1607-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Garofalo R, Herrick A, Donenberg G, 2007. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Ann.Behav. Med 34, 37–45. doi: 10.1007/BF02879919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén BO, Muthén LK, 2015. Mplus (Version 7.4). Los Angeles, CA. [Google Scholar]
- Muthén LK, Muthén BO, 2015. Mplus: Statistical Analysis with Latent Variables User’s Guide. 7th ed. Los Angeles, CA: Muthén and Muthén; 1998–2015. [Google Scholar]
- Muthén BO, Muthén LK, 2000. Integrating person-centered and variable-centered analyses: Growth mixture modeling with latent trajectory classes. Alcohol.: Clin. Exp. Res 24, 882–891. doi: 10.1111/j.1530-0277.2000.tb02070.x [DOI] [PubMed] [Google Scholar]
- NIDA. 2016. Drug abuse and addiction. National Institute on Drug Abuse. Retrieved from https://www.drugabuse.gov/publications/drugs-brains-behavior-science-addiction/drug-abuseaddiction. [Google Scholar]
- Newcomb ME, 2013. Moderating effect of age on the association between alcohol use and sexual risk in MSM: evidence for elevated risk among younger MSM. AIDS Behav. 17, 1746–1754. doi: 10.1007/s10461-013-0470-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noor SW, Adam BD, Brennan DJ, Moskowitz DA, Gardner S, Hart TA (2018). Scenes as micro-cultures: examining heterogeneity of HIV risk behavior among gay, bisexual, and other men who have sex with men in Toronto, Canada. Arch Sex Behav. 47, 309–321. doi: 10.1007/s10508-017-0948-y [DOI] [PubMed] [Google Scholar]
- Nylund KL 2007. Latent transition analysis: Modeling extensions and an application to peer victimization. Los Angeles, CA: University of California Los Angeles. [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO, 2007. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Struct Equ Modeling. 14, 535–569. doi: 10.1080/10705510701575396 [DOI] [Google Scholar]
- Parsons JT, Grov C, Golub SA, 2012. Sexual compulsivity, co-occurring psychosocial health problems, and HIV risk among gay and bisexual men: further evidence of a syndemic. Am. J. Public Health 102, 156–162. 10.2105/AJPH.2011.300284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purcell DW, Johnson CH, Lansky A, Prejean J, Stein R, Denning P, Gau Z, Weinstock H, Su J, Crepaz N, 2012. Suppl 1: Estimating the population size of men who have sex with men in the United States to obtain HIV and syphilis rates. Open AIDS Journal 6, 98–107. doi: 10.2174/1874613601206010098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn KG, Voisin DR, 2020. ART Adherence Among Men Who Have Sex with Men Living with HIV: Key Challenges and Opportunities. Curr HIV/AIDS Rep 17, 290–300. doi: 10.1007/s11904-020-00510-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Race K, Lea T, Murphy D, Pienaar K, 2017. The future of drugs: recreational drug use and sexual health among gay and other men who have sex with men. Sex Health 14, 42–50. doi: 10.1071/SH16080 [DOI] [PubMed] [Google Scholar]
- Raymond HF, Chen YH, Ick T, Scheer S, Bernstein K, Liska S, Louie B, Pandori M, McFarland W, 2013. A new trend in the HIV epidemic among men who have sex with men, San Francisco, 2004–2011. J Acquir. Immune Defic. Syndr 62, pp.584–589. doi: 10.1097/QAI.0b013e318285febf [DOI] [PubMed] [Google Scholar]
- Sanchez TH, Zlotorzynska M, Sineath RC, Kahle E, Tregear S, Sullivan PS, 2018. National trends in sexual behavior, substance use and HIV testing among United States men who have sex with men recruited online, 2013 through 2017. AIDS Behav. 22, 2413–2425. doi: 10.1007/s10461-018-2168-4 [DOI] [PubMed] [Google Scholar]
- Society of Clinical Psychology (2020). Psychological diagnoses and other targets of treatment. Retrieved from: https://div12.org/diagnoses/ on December 14, 2020.
- Staudt A, Freyer-Adam J, Meyer C, John U, Baumann S, 2018. Short-term stability of different drinking patterns over the course of four weeks among adults. A latent transition analysis. Drug Alcohol Depend. 191, 181–186. doi: 10.1016/j.drugalcdep.2018.06.031 [DOI] [PubMed] [Google Scholar]
- Vosburgh HW, Mansergh G, Sullivan PS, Purcell DW, 2012. A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS Behav. 16, 1394–1410. doi: 10.1007/s10461-011-0131-8 [DOI] [PubMed] [Google Scholar]
- Wilkerson JM, Noor SW, Rhoton JM, Li D, Rosser BS, 2018. Differentially classified methamphetamine-using men who have sex with men: A latent class analysis. Drug Alcohol Depend. 192, 129–136. doi: 10.1016/j.drugalcdep.2018.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson AL, El-Hayek C, Fairley CK, Roth N, Tee BK, McBryde E, Hellard M, Stoové M, 2017. Measuring transitions in sexual risk among men who have sex with men: the novel use of latent class and latent transition analysis in HIV sentinel surveillance. Am J Epidemiol. 185, 627–635. doi: 10.1093/aje/kww239 [DOI] [PubMed] [Google Scholar]
- Yang Q, Ogunnaike-Cooke S, Halverson J, Yan P, Zhang F, Tomas K, Archibald CP, 2016, May Estimated national HIV incidence rates among key sub-populations in Canada, 2014. In 25th Annual Canadian Conference on HIV/AIDS Research (CAHR) (12-15). [Google Scholar]