Introduction
The Accreditation Council for Graduate Medical Education (ACGME) has recognized clinician well-being as a major challenge in health care.1 In its assurance function through the Common Program Requirements2 and in its improvement function through the Clinical Learning Environment Review (CLER) Program,3 the ACGME has stressed the importance of resident and faculty safety and well-being. As the COVID-19 pandemic spreads across the country, of significant concern to the ACGME is the threat to the safety and well-being of residents and faculty in GME programs in the context of the entire health care workforce. The leaders of the National Academy of Medicine Action Collaborative on Clinician Well-Being, which includes the ACGME, raised concerns of a parallel pandemic amid the initial surge of COVID-19 cases.4 Of critical importance was the emphasis on psychological safety, which remains a primary concern today.5 These well-being concerns continue to be compounded by the threat to physical safety occurring on the frontlines.6
The spread of the COVID-19 illness varied in the early months as New York and states in the Northeast became the epicenter for the initial outbreak.7 By the summer months, cases were beginning to increase across the South with the highest number of cases in Florida and Texas. To adapt to the new environment, the ACGME issued directives to the GME community throughout the initial phases of the pandemic. This guidance was aimed at providing programs and Sponsoring Institutions the flexibility to respond to the local impact of the pandemic, while requiring certain safety expectations in the clinical care of patients.8 The ACGME also emphasized the need for personal protective equipment (PPE), calling on national leaders to ensure the entire health care workforce has sufficient access to appropriate PPE.9
As the pandemic sweeps across the country, various sites are documenting the health impact of COVID-19 on frontline workers. While its data are incomplete, the Centers for Disease Control and Prevention (CDC) as of December 3, 2020, reported at least 249 033 cases of COVID-19 and 866 health care worker deaths over the last 9 months.10 Kaiser Health News as part of its tracking project estimates 1425 individuals working in health care have died due to COVID-19.11 Among these are 36 confirmed physician deaths.11 There are currently no reports that capture the impact to residents and faculty in graduate medical education (GME).
To assess the health impact of the pandemic on residents and faculty, the ACGME added a supplementary survey to its annual program data update collected from programs and Sponsoring Institutions. This supplementary survey has captured some of the health impacts of the pandemic on residents and faculty during the spring and early summer. All residency and fellowship programs are required to complete the annual update, enabling the opportunity to assess the health impact of COVID-19 across the United States, not just in the hot spot regions during this period.
Methods
An internal ACGME task force of experienced GME leaders drafted survey questions to capture the impact of the SARS-COV-2 virus on residents and faculty in early April 2020 (Box). An outside expert in survey design reviewed the questions for clarity and consistency prior to inclusion as part of the ACGME's Accreditation Data System (ADS) annual update. The ADS annual update is conducted between July 1 and September 30 each year. During this time frame non-procedural and procedural specialties have reporting deadlines of August 31 and September 30, respectively. Programs were assured that the results of this supplementary survey would not be identifiable and would not be used for accreditation purposes. We provide the number of faculty and residents quarantined and hospitalized due to COVID-19 by specialty and region. The number of deceased faculty and residents is reported in aggregate to protect the identity of the programs and Sponsoring Institutions. For regional analyses, we reported the data across 4 regions defined by the US Census Bureau: South, Northeast, Midwest, and West. The programs in Puerto Rico are excluded from regional analysis.
Box Accreditation Data System Questions Regarding Resident and Faculty COVID-19-Related Illness
The responses to the following should reflect what occurred in your program between March 1 and June 30, 2020.
How many residents or fellows were quarantineda due to COVID-19-related illness?
How many faculty members were quarantineda due to COVID-19-related illness?
How many residents or fellows were hospitalized due to COVID-19-related illness?
How many faculty members were hospitalized due to COVID-19-related illness?
If there were any deaths of residents or fellows due to COVID-19-related illness, how many were there?
If there were any deaths of faculty members due to COVID-19-related illness, how many were there?
Required time away from work due to COVID-19 exposure and/or illness.
Results
During the reporting window, 11 925 programs (5329 core residency programs, 6596 subspecialty fellowship programs) provided responses to the annual update supplementary survey. This represents a 99.1% response rate among residency and fellowship programs accredited by the ACGME during the reporting window and in the time frame between March 1 and June 30, 2020. Additional program characteristics are reported in the ACGME's Data Resource Book for the 2019–2020 academic year.12
In response to the question regarding resident quarantine in the first 4 months of the pandemic, across all programs, 4515 (37.5%) reported at least one resident or fellow quarantined due to COVID-19. In total, programs reported 18 357 residents and fellows (12.7% of 144 988 total active residents and fellows) were quarantined due to COVID-19. In core residency programs, 3107 programs (58.3%) reported having at least one resident quarantined due to COVID-19. In subspecialty fellowship programs, 1408 programs (21.4%) reported at least one resident quarantined due to COVID-19. Table 1 provides greater detail on the specialty distribution and number of residents per program quarantined. All core clinical residency disciplines reported whether residents were quarantined. Across all disciplines there were 282 programs that reported quarantining of more than 10 residents. There were 4 disciplines in which at least 10% of core specialty programs reported more than 10 residents requiring quarantine. These were internal medicine (124 programs, 22.1%), pediatrics (29 programs, 13.9%), emergency medicine (31 programs, 11.7%), and anesthesiology (18 programs, 11.3%).
Table 1.
Distribution of Programs by Number of Residents Quarantined Due to COVID-19
| Category | 0 Residents Quarantined, N (%) | 1 to 10 Residents Quarantined, N (%) | 11 or More Residents Quarantined, N (%) | Total Programs, N (%) |
| All Core Programs | 2222 (41.7) | 2825 (53) | 282 (5.3) | 5329 (100) |
| Core Programs by Specialty | ||||
| Allergy and immunology | 64 (79) | 17 (21) | 0 (0) | 81 (100) |
| Anesthesiology | 41 (25.8) | 100 (62.9) | 18 (11.3) | 159 (100) |
| Colon and rectal surgery | 58 (90.6) | 5 (7.8) | 1 (1.6) | 64 (100) |
| Dermatology | 76 (53.1) | 64 (44.8) | 3 (2.1) | 143 (100) |
| Emergency medicine | 55 (20.8) | 178 (67.4) | 31 (11.7) | 264 (100) |
| Family medicine | 226 (32.8) | 443 (64.3) | 20 (2.9) | 689 (100) |
| Internal medicine | 138 (24.6) | 300 (53.4) | 124 (22.1) | 562 (100) |
| Medical genetics and genomics | 44 (93.6) | 3 (6.4) | 0 (0) | 47 (100) |
| Neurological surgery | 54 (46.6) | 61 (52.6) | 1 (0.9) | 116 (100) |
| Neurology | 64 (40) | 94 (58.8) | 2 (1.3) | 160 (100) |
| Child neurology | 55 (72.4) | 21 (27.6) | 0 (0) | 76 (100) |
| Nuclear medicine | 32 (86.5) | 5 (13.5) | 0 (0) | 37 (100) |
| Obstetrics and gynecology | 101 (35.4) | 179 (62.8) | 5 (1.8) | 285 (100) |
| Ophthalmology | 60 (48.8) | 62 (50.4) | 1 (0.8) | 123 (100) |
| Orthopaedic surgery | 79 (40.1) | 111 (56.3) | 7 (3.6) | 197 (100) |
| Osteopathic neuromusculoskeletal medicine | 18 (66.7) | 9 (33.3) | 0 (0) | 27 (100) |
| Otolaryngology-head and neck surgery | 68 (54.8) | 56 (45.2) | 0 (0) | 124 (100) |
| Pathology-anatomic and clinical | 87 (61.3) | 54 (38) | 1 (0.7) | 142 (100) |
| Pediatrics | 42 (20.1) | 138 (66) | 29 (13.9) | 209 (100) |
| Physical medicine and rehabilitation | 33 (35.1) | 59 (62.8) | 2 (2.1) | 94 (100) |
| Plastic surgery | 33 (64.7) | 18 (35.3) | 0 (0) | 51 (100) |
| Plastic surgery-integrated | 46 (56.1) | 36 (43.9) | 0 (0) | 82 (100) |
| Preventive medicine | 56 (78.9) | 15 (21.1) | 0 (0) | 71 (100) |
| Psychiatry | 97 (36.1) | 159 (59.1) | 13 (4.8) | 269 (100) |
| Radiation oncology | 61 (67) | 30 (33) | 0 (0) | 91 (100) |
| Radiology-diagnostic | 88 (45.1) | 105 (53.8) | 2 (1) | 195 (100) |
| Interventional radiology-integrated | 67 (75.3) | 22 (24.7) | 0 (0) | 89 (100) |
| Surgery | 95 (29) | 215 (65.5) | 18 (5.5) | 328 (100) |
| Thoracic surgery | 54 (73) | 20 (27) | 0 (0) | 74 (100) |
| Thoracic surgery-integrated | 14 (46.7) | 16 (53.3) | 0 (0) | 30 (100) |
| Vascular surgery-integrated | 42 (65.6) | 22 (34.4) | 0 (0) | 64 (100) |
| Urology | 77 (53.1) | 65 (44.8) | 3 (2.1) | 145 (100) |
| Transitional year | 71 (43.8) | 90 (55.6) | 1 (0.6) | 162 (100) |
| Internal medicine/pediatrics | 26 (32.9) | 53 (67.1) | 0 (0) | 79 (100) |
| Core Programs by Regiona | ||||
| Midwest | 579 (44.7) | 672 (51.9) | 44 (3.4) | 1295 (100) |
| Northeast | 480 (34.4) | 786 (56.3) | 129 (9.2) | 1395 (100) |
| South | 758 (43.6) | 905 (52) | 77 (4.4) | 1740 (100) |
| West | 384 (45) | 440 (51.5) | 30 (3.5) | 854 (100) |
| All Subspecialty Programs | 5188 (78.7) | 1389 (21.1) | 19 (0.3) | 6596 (100) |
| Subspecialty Programs by Regiona | ||||
| Midwest | 1281 (82.1) | 278 (17.8) | 1 (0.1) | 1560 (100) |
| Northeast | 1333 (72.1) | 503 (27.2) | 12 (0.6) | 1848 (100) |
| South | 1680 (80.5) | 401 (19.2) | 5 (0.2) | 2086 (100) |
| West | 870 (81.2) | 201 (18.8) | 1 (0.1) | 1072 (100) |
| Grand Total | 7410 (62.1) | 4214 (35.3) | 301 (2.5) | 11 925 (100) |
Puerto Rico is excluded (N = 75).
Of 11 925 programs, 7699 (64.6%) reported having no faculty quarantined in the reporting period, with 4226 programs (35.4%) reporting more than one faculty quarantined (Table 2). While 54.2% of core residency programs reported zero faculty quarantines, 72.9% of subspecialty fellowship programs reported zero faculty members quarantined. As can be seen in Table 2, there were 5 specialties in which the majority of programs reported at least one faculty member quarantined: pediatrics, 67.9% of programs; emergency medicine, 67% of programs; anesthesiology, 64.8% of programs; obstetrics and gynecology, 61.8% of programs; and internal medicine, 57.5% of programs.
Table 2.
Distribution of Programs by Number of Faculty Quarantined Due to COVID-19
| Category | 0 Faculty Quarantined, N (%) | 1 to 10 Faculty Quarantined, N (%) | 11 or More Faculty Quarantined, N (%) | Total Programs, N (%) |
| All Core Programs | 2888 (54.2) | 2318 (43.5) | 123 (2.3) | 5329 (100) |
| Core Programs by Specialty | ||||
| Allergy and immunology | 60 (74.1) | 21 (25.9) | 0 (0) | 81 (100) |
| Anesthesiology | 56 (35.2) | 87 (54.7) | 16 (10.1) | 159 (100) |
| Colon and rectal surgery | 43 (67.2) | 20 (31.3) | 1 (1.6) | 64 (100) |
| Dermatology | 91 (63.6) | 51 (35.7) | 1 (0.7) | 143 (100) |
| Emergency medicine | 87 (33) | 164 (62.1) | 13 (4.9) | 264 (100) |
| Family medicine | 366 (53.1) | 320 (46.4) | 3 (0.4) | 689 (100) |
| Internal medicine | 239 (42.5) | 282 (50.2) | 41 (7.3) | 562 (100) |
| Medical genetics and genomics | 42 (89.4) | 5 (10.6) | 0 (0) | 47 (100) |
| Neurological surgery | 73 (62.9) | 43 (37.1) | 0 (0) | 116 (100) |
| Neurology | 91 (56.9) | 68 (42.5) | 1 (0.6) | 160 (100) |
| Child neurology | 53 (69.7) | 23 (30.3) | 0 (0) | 76 (100) |
| Nuclear medicine | 31 (83.8) | 6 (16.2) | 0 (0) | 37 (100) |
| Obstetrics and gynecology | 109 (38.2) | 167 (58.6) | 9 (3.2) | 285 (100) |
| Ophthalmology | 69 (56.1) | 53 (43.1) | 1 (0.8) | 123 (100) |
| Orthopaedic surgery | 110 (55.8) | 85 (43.1) | 2 (1) | 197 (100) |
| Osteopathic neuromusculoskeletal medicine | 18 (66.7) | 9 (33.3) | 0 (0) | 27 (100) |
| Otolaryngology-head and neck surgery | 78 (62.9) | 46 (37.1) | 0 (0) | 124 (100) |
| Pathology-anatomic and clinical | 91 (64.1) | 49 (34.5) | 2 (1.4) | 142 (100) |
| Pediatrics | 67 (32.1) | 123 (58.9) | 19 (9.1) | 209 (100) |
| Physical medicine and rehabilitation | 48 (51.1) | 45 (47.9) | 1 (1.1) | 94 (100) |
| Plastic surgery | 41 (80.4) | 10 (19.6) | 0 (0) | 51 (100) |
| Plastic surgery-integrated | 63 (76.8) | 19 (23.2) | 0 (0) | 82 (100) |
| Preventive medicine | 58 (81.7) | 12 (16.9) | 1 (1.4) | 71 (100) |
| Psychiatry | 137 (50.9) | 128 (47.6) | 4 (1.5) | 269 (100) |
| Radiation oncology | 68 (74.7) | 23 (25.3) | 0 (0) | 91 (100) |
| Radiology-diagnostic | 112 (57.4) | 82 (42.1) | 1 (0.5) | 195 (100) |
| Interventional radiology-integrated | 61 (68.5) | 28 (31.5) | 0 (0) | 89 (100) |
| Surgery | 163 (49.7) | 161 (49.1) | 4 (1.2) | 328 (100) |
| Thoracic surgery | 51 (68.9) | 23 (31.1) | 0 (0) | 74 (100) |
| Thoracic surgery-integrated | 21 (70) | 9 (30) | 0 (0) | 30 (100) |
| Vascular surgery-integrated | 49 (76.6) | 15 (23.4) | 0 (0) | 64 (100) |
| Urology | 95 (65.5) | 49 (33.8) | 1 (0.7) | 145 (100) |
| Transitional year | 97 (59.9) | 64 (39.5) | 1 (0.6) | 162 (100) |
| Internal medicine/pediatrics | 50 (63.3) | 28 (35.4) | 1 (1.3) | 79 (100) |
| Core Programs by Regiona | ||||
| Midwest | 758 (58.5) | 515 (39.8) | 22 (1.7) | 1295 (100) |
| Northeast | 592 (42.4) | 735 (52.7) | 68 (4.9) | 1395 (100) |
| South | 987 (56.7) | 728 (41.8) | 25 (1.4) | 1740 (100) |
| West | 521 (61) | 325 (38.1) | 8 (0.9) | 854 (100) |
| All Subspecialty Programs | 4811 (72.9) | 1752 (26.6) | 33 (0.5) | 6596 (100) |
| Subspecialty Programs by Regiona | ||||
| Midwest | 1194 (76.5) | 364 (23.3) | 2 (0.1) | 1560 (100) |
| Northeast | 1201 (65) | 626 (33.9) | 21 (1.1) | 1848 (100) |
| South | 1541 (73.9) | 537 (25.7) | 8 (0.4) | 2086 (100) |
| West | 850 (79.3) | 220 (20.5) | 2 (0.2) | 1072 (100) |
| Grand Total | 7699 (64.6) | 4070 (34.1) | 156 (1.3) | 11 925 (100) |
Puerto Rico is excluded (N = 75).
Table 3 provides specialty-specific data on reports of resident and faculty hospitalization. One hundred thirty-nine programs (1.2%) reported the hospitalization of one or more than one resident. Three specialties, internal medicine (32 programs, 5.7%), emergency medicine (14 programs, 5.3%), and surgery (10 programs, 3.0%), had more than 3% of programs hospitalize one or more than one resident. Four residents died during the 4-month period from March through June 2020. The ACGME is also aware of a subspecialty fellow death in a program not accredited by the ACGME. Hospitalizations for faculty members were reported more frequently than for residents (Table 3). Of the 405 programs reporting a faculty member hospitalization, 249 were core residency programs (4.7% of all core programs), and 156 were subspecialty fellowship programs (2.4% of all subspecialty programs). The specialties that reported one or more than one faculty hospitalization for COVID-19 were internal medicine (73 residency programs), emergency medicine (22 residency programs), obstetrics and gynecology (22 residency programs), surgery (21 residency programs), and pediatrics (18 residency programs). In response to the question regarding faculty deaths, 46 programs reported the death of a faculty member across 29 institutions. While we can't be sure, it's likely that within an institution, more than one program experienced the loss of the same individual. Faculty from internal medicine residency and fellowship programs accounted for 21 (45.5%) of the programs reporting deaths from COVID-19. Faculty deaths were reported across 26 specialties and subspecialties in the initial phase of the pandemic.
Table 3.
Distribution of Programs by Number of Residents and Faculty Hospitalized Due to COVID-19
| Category | 0 Residents Hospitalized, N (%) | 1 or More Residents Hospitalized, N (%) | 0 Faculty Hospitalized, N (%) | 1 or More Faculty Hospitalized, N (%) |
| All Core Programs | 5217 (97.9) | 112 (2.1) | 5080 (95.3) | 249 (4.7) |
| Core Programs by Specialty | ||||
| Allergy and immunology | 81 (100) | 0 (0) | 81 (100) | 0 (0) |
| Anesthesiology | 156 (98.1) | 3 (1.9) | 151 (95) | 8 (5) |
| Colon and rectal surgery | 64 (100) | 0 (0) | 62 (96.9) | 2 (3.1) |
| Dermatology | 141 (98.6) | 2 (1.4) | 140 (97.9) | 3 (2.1) |
| Emergency medicine | 250 (94.7) | 14 (5.3) | 242 (91.7) | 22 (8.3) |
| Family medicine | 676 (98.1) | 13 (1.9) | 678 (98.4) | 11 (1.6) |
| Internal medicine | 530 (94.3) | 32 (5.7) | 489 (87) | 73 (13) |
| Medical genetics and genomics | 47 (100) | 0 (0) | 47 (100) | 0 (0) |
| Neurological surgery | 116 (100) | 0 (0) | 115 (99.1) | 1 (0.9) |
| Neurology | 156 (97.5) | 4 (2.5) | 156 (97.5) | 4 (2.5) |
| Child neurology | 76 (100) | 0 (0) | 76 (100) | 0 (0) |
| Nuclear medicine | 37 (100) | 0 (0) | 37 (100) | 0 (0) |
| Obstetrics and gynecology | 279 (97.9) | 6 (2.1) | 263 (92.3) | 22 (7.7) |
| Ophthalmology | 119 (96.7) | 4 (3.3) | 117 (95.1) | 6 (4.9) |
| Orthopaedic surgery | 194 (98.5) | 3 (1.5) | 190 (96.4) | 7 (3.6) |
| Osteopathic neuromusculoskeletal medicine | 27 (100) | 0 (0) | 27 (100) | 0 (0) |
| Otolaryngology-head and neck surgery | 123 (99.2) | 1 (0.8) | 121 (97.6) | 3 (2.4) |
| Pathology-anatomic and clinical | 141 (99.3) | 1 (0.7) | 136 (95.8) | 6 (4.2) |
| Pediatrics | 204 (97.6) | 5 (2.4) | 191 (91.4) | 18 (8.6) |
| Physical medicine and rehabilitation | 92 (97.9) | 2 (2.1) | 92 (97.9) | 2 (2.1) |
| Plastic surgery | 51 (100) | 0 (0) | 49 (96.1) | 2 (3.9) |
| Plastic surgery-integrated | 81 (98.8) | 1 (1.2) | 79 (96.3) | 3 (3.7) |
| Preventive medicine | 71 (100) | 0 (0) | 71 (100) | 0 (0) |
| Psychiatry | 265 (98.5) | 4 (1.5) | 257 (95.5) | 12 (4.5) |
| Radiation oncology | 91 (100) | 0 (0) | 91 (100) | 0 (0) |
| Radiology-diagnostic | 193 (99) | 2 (1) | 189 (96.9) | 6 (3.1) |
| Interventional radiology-integrated | 88 (98.9) | 1 (1.1) | 88 (98.9) | 1 (1.1) |
| Surgery | 318 (97) | 10 (3) | 307 (93.6) | 21 (6.4) |
| Thoracic surgery | 74 (100) | 0 (0) | 73 (98.6) | 1 (1.4) |
| Thoracic surgery-integrated | 30 (100) | 0 (0) | 30 (100) | 0 (0) |
| Vascular surgery-integrated | 64 (100) | 0 (0) | 62 (96.9) | 2 (3.1) |
| Urology | 145 (100) | 0 (0) | 140 (96.6) | 5 (3.4) |
| Transitional year | 160 (98.8) | 2 (1.2) | 154 (95.1) | 8 (4.9) |
| Internal medicine/pediatrics | 77 (97.5) | 2 (2.5) | 79 (100) | 0 (0) |
| Core Programs by Regiona | ||||
| Midwest | 1277 (98.6) | 18 (1.4) | 1253 (96.8) | 42 (3.2) |
| Northeast | 1340 (96.1) | 55 (3.9) | 1261 (90.4) | 134 (9.6) |
| South | 1711 (98.3) | 29 (1.7) | 1684 (96.8) | 56 (3.2) |
| West | 845 (98.9) | 9 (1.1) | 837 (98) | 17 (2) |
| All Subspecialty Programs | 6569 (99.6) | 27 (0.4) | 6440 (97.6) | 156 (2.4) |
| Subspecialty Programs by Regiona | ||||
| Midwest | 1555 (99.7) | 5 (0.3) | 1535 (98.4) | 25 (1.6) |
| Northeast | 1833 (99.2) | 15 (0.8) | 1761 (95.3) | 87 (4.7) |
| South | 2082 (99.8) | 4 (0.2) | 2050 (98.3) | 36 (1.7) |
| West | 1069 (99.7) | 3 (0.3) | 1064 (99.3) | 8 (0.7) |
| Grand Total | 11 786 (98.8) | 139 (1.2) | 11 520 (96.6) | 405 (3.4) |
Puerto Rico is excluded (N = 75).
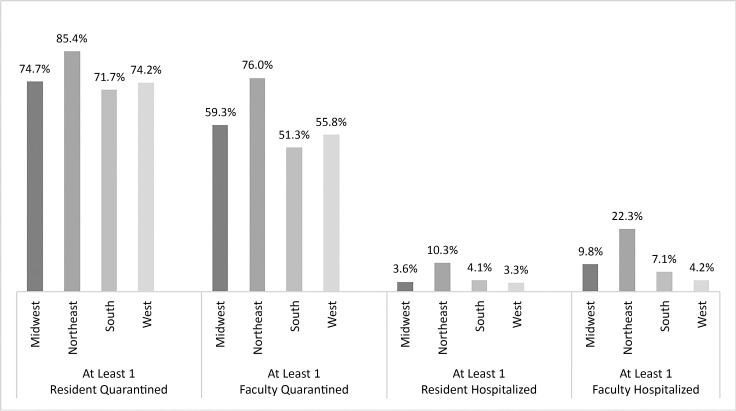
Tables 1, 2, and 3 provide regional statistics for resident and faculty quarantines and hospitalizations for core specialties and subspecialties. Across every question, programs in the Northeast reported higher numbers of faculty and resident quarantine and a higher percentage of programs with resident and faculty hospitalizations than the other 3 regions. Given the variability by specialty, the Figure highlights regional differences in internal medicine and emergency medicine programs alone. In the Northeast, 85.4% of internal medicine and emergency medicine programs had at least one resident quarantined and 76.0% of programs had at least one faculty member quarantined compared to 74% and 55% in the other regions, respectively. The Northeast region also had the highest percentage of internal medicine and emergency medicine programs reporting at least one resident hospitalization and/or at least one faculty hospitalization (10.3% and 22.3% of programs, respectively).
Figure.
Internal Medicine and Emergency Medicine Programs Reporting At Least One Resident/Faculty Quarantined/Hospitalized by Region (N = 826)
Discussion
The impact of the COVID-19 pandemic on resident, fellow, and faculty health is significant. With hospitalizations currently increasing across the country, and community spread worsening in most states, health care workers continue to be at risk of exposure to COVID-19.13 While the exact number is not known, at least hundreds of health care workers have died from COVID-19, with nursing appearing to be the most impacted health profession to date.9 Adequate access to testing and PPE remains a significant concern on the frontlines of health care. The ACGME continues to voice its concern for PPE needs to protect health care professionals, one of our nation's most valuable assets.14
This brief report provides a window into the initial impact of the pandemic on residents and faculty in GME institutions. Given the nature and location of COVID-19 hotspots in the first 4 months of the pandemic, the impact on residents and faculty was most pronounced in these hotspot regions, but not solely confined to them. Similarly, while internal medicine, emergency medicine, anesthesiology, and pediatric residents and faculty were affected, few specialties were spared the impact of COVID-19. Now that the pandemic has significantly affected every state, additional work will be needed to learn about the impact of COVID-19 from July onward, especially during the worst peak of the pandemic being experienced at the time of this report. The ACGME plans to continue follow-up assessment activities on the impact of the pandemic on GME institutions. Additional research will be needed to capture a fuller picture of both the health and educational impacts of the pandemic on GME. The surges in COVID-19 across a broader swath of the United States this past fall clearly continue to impact multiple health care institutions, including teaching hospitals.
Conclusions
Teaching hospitals are on the frontlines of the pandemic, often caring for the sickest COVID-19 patients. The health effects on learners and faculty were and continue to be significant despite what the ACGME is sure are the best efforts by programs and institutions to maintain the safety of residents and faculty. These data from the initial stages will be helpful in following up on the impacts of the significant surge in cases in November 2020 through January 2021, and will set the foundation for an essential need for the entire GME community to reflect and gather lessons during and after the pandemic. The ACGME will continue to advocate stridently for access to and proper training in PPE, as well as continue to interact with the GME community through its pandemic emergency status designations, DIO calls, newsroom, and other communication vehicles. Finally, the ACGME wishes to acknowledge and support the profound professionalism demonstrated by the GME community during one of the worst health care crises in its history.
References
- 1.Dzau VJ, Kirch DG, Nasca TJ. To care is human—collectively confronting the clinician-burnout crisis. N Engl J Med. 2018;378(4):312–314. doi: 10.1056/nejmp1715127. [DOI] [PubMed] [Google Scholar]
- 2.Accreditation Council for Graduate Medical Education. ACGME Common Program Requirements (Residency) 2019. 2020 https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRResidency2019-TCC.pdf Accessed December 8.
- 3.Accreditation Council for Graduate Medical Education. CLER Pathways to Excellence. Expectations for an Optimal Clinical Learning Environment to Achieve Safe and High-Quality Patient Care. Version 2.0. 2020 https://www.acgme.org/Portals/0/PDFs/CLER/1079ACGME-CLER2019PTE-BrochDigital.pdf Accessed December 8.
- 4.Dzau VJ, Kirch DG, Nasca TJ. Preventing a parallel pandemic—a national strategy to protect clinicians' well-being. N Engl J Med. 2020;383(6):513–515. doi: 10.1056/NEJMp2011027. [DOI] [PubMed] [Google Scholar]
- 5.National Academy of Medicine. Resources to Support the Health and WellBeing of Clinicians During the COVID19 Outbreak. 2020 https://nam.edu/initiatives/clinician-resilience-and-well-being/clinician-well-being-resources-during-covid-19/ Accessed December 8.
- 6.Yong E. ‘No One Is Listening to Us' More people than ever are hospitalized with COVID-19. Health-care workers can't go on like this. The Atlantic. 2020 November 13, 2020. https://www.theatlantic.com/health/archive/2020/11/third-surge-breaking-healthcare-workers/617091/ Accessed December 8.
- 7.Thompson CN, Baumgartner J, Pichardo C, Toro B, Li L, Arciuolo R, et al. COVID-19 outbreak—New York City, February 29–June 1, 2020. Centers for Disease Control and Prevention Morbidity and Mortality Weekly. 2020 doi: 10.15585/mmwr.mm6946a2. https://www.cdc.gov/mmwr/volumes/69/wr/mm6946a2.htm Accessed December 8. [DOI] [PMC free article] [PubMed]
- 8.Accreditation Council for Graduate Medical Education. ACGME Guidance Statements. 2020 https://www.acgme.org/COVID-19/ACGME-Guidance-Statements Accessed December 8.
- 9.Accreditation Council for Graduate Medical Education. ACGME Statement on the Shortage of Personal Protective Equipment (PPE) 2020 https://www.acgme.org/Newsroom/Newsroom-Details/ArticleID/10186/ACGME-Statement-on-the-Shortage-of-Personal-Protective-Equipment-PPE Accessed December 8.
- 10.Centers for Disease Control and Prevention. CDC COVID Data Tracker. 2020 https://covid.cdc.gov/covid-data-tracker/ Accessed December 8.
- 11.Lost on the Frontlines. The Guardian. 2020 https://www.theguardian.com/us-news/ng-interactive/2020/aug/11/lost-on-the-frontline-covid-19-coronavirus-us-healthcare-workers-deaths-database Accessed December 8.
- 12.Accreditation Council for Graduate Medical Education. Data Resource Book Academic Year 2019–2020. 2020 https://www.acgme.org/About-Us/Publications-and-Resources/Graduate-Medical-Education-Data-Resource-Book Accessed December 8.
- 13.May M. COVID-19—Associated Hospitalizations Among Health Care Personnel. Centers for Disease Control and Prevention Morbidity and Mortality Weekly. 2020 https://www.cdc.gov/mmwr/volumes/69/wr/mm6943e3.htm Accessed December 8.
- 14.Accreditation Council for Graduate Medical Education. The ACGME Urges Presidential Nominees to Commit to Accelerating PPE Production. 2020 https://www.acgme.org/Newsroom/Newsroom-Details/ArticleID/10689/The-ACGME-Urges-Presidential-Nominees-to-Commit-to-Accelerating-PPE-Production?articleid=10694 Accessed December 8.