Abstract
Background
Wellness initiatives implemented by graduate medical education programs can help mitigate burnout in resident physicians.
Objective
This systematic review seeks to identify factors that impact the effectiveness of resident wellness interventions and to provide a conceptual framework to guide future interventions.
Methods
Using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, 6 electronic databases were searched in November 2019 using variations of the keywords “resident physicians,” “wellness,” and “intervention.” Peer-reviewed full-text English-language articles on controlled studies were considered for inclusion. The quality of the studies was assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) guidelines.
Results
The initial search disclosed 1196 articles, of which 18 studies enrolling 666 resident physicians met inclusion criteria for qualitative review. Interventions using peer support and individual meditation enhanced well-being. Effective wellness interventions also used educational theory to guide program development, surveyed participants to guide intervention design, incorporated programming into existing didactic curricula, and recruited voluntary participants. The quality of most of the included studies was poor (13 of 18, 72%) and could be improved by using standardized wellness assessments supported by validity evidence.
Conclusions
This systematic review suggests that future resident wellness initiatives should focus on grounding interventions in educational theory, forging consensus on wellness instruments with validity evidence, and examining the impact of initiatives on patient outcomes. A logic model can provide a framework for designing and implementing effective wellness interventions.
Introduction
The World Health Organization defines burnout as a “syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed.”1 Up to 54% of physicians in the United States report symptoms of burnout.2–4 Burnout is not uniform across medical specialties, with prevalence and etiology depending on specialty.5,6 Burnout has been associated with depression, anxiety, distress, and occupational stress and is associated with more patient safety incidents, poorer quality of care, reduced patient satisfaction, and increased health care costs.7,8
Burnout is not limited to attending physicians, however. Between 44% and 67% of resident physicians experience burnout.2,6,9–13 Residents are subject to a variety of unique stressors, including learning to master a large amount of didactic material and broad array of clinical skills,14 such as specialty-dependent minor and operating room procedures, while also assuming increasing responsibility for patient care,15 working up to 80 hours a week,16 taking national in-training examinations,17–21 and facing the financial demands of low salaries and student loans.22 There is an inverse relationship between burnout prevalence and the age of physicians in practice, suggesting that residents at the beginning of their medical career are especially susceptible to burnout.23 Resident burnout also increases the financial burden on health care systems by decreasing work hours and increasing turnover costs due to attrition, with younger physicians having the greatest estimated burnout-attributable costs.8
An important way to combat physician burnout is to promote physician well-being,24–26 defined by the Centers for Disease Control and Prevention as including “the presence of positive emotions and moods (eg, contentment, happiness), the absence of negative emotions (eg, depression, anxiety), satisfaction with life, fulfillment, and positive functioning.”27 Indeed, research has indicated that structural reform can alleviate physician burnout and improve resident well-being.28 In response, graduate medical education (GME) programs have implemented wellness interventions to address burnout by improving well-being in resident physicians. These wellness interventions include workplace discussions, altering practice schedules and workflows, community building, cognitive behavioral therapies, and use of mindfulness practices.
The most recent systematic review of burnout prevention for resident physicians was limited by its emphasis on duty hour restrictions set by the Accreditation Council for Graduate Medical Education (ACGME) with little focus on well-being.29 However, in its 2020 Common Program Requirements, the ACGME recognized that residents' work hours do not represent the entirety of their learning and working environment.16 To promote enhancing well-being rather than simply preventing burnout, the ACGME obligates residency programs to take responsibility for optimizing resident well-being, including through wellness initiatives,16 and provides accessible well-being resources.30 An understanding of the effects of interventions beyond those of work hour restrictions is thus necessary. This focus on enhancing well-being also requires the production of reproducible interventions and initiatives. However, the breadth and quality of the evidence base to inform future interventions to address resident well-being are unclear.
Understanding which interventions have been successful in alleviating resident burnout and improving resident well-being is critical to improving the quality of GME. To this end, we systematically reviewed the effectiveness of controlled resident wellness interventions in and outside the United States. We also provide a conceptual framework for informing future research in this area.
Methods
Using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines,31 and with consultation of reference librarians, 2 authors (J.E. and P.P.R.) searched the following databases in November 2019 for studies that fit our inclusion criteria: MEDLINE/PubMed (January 1950 to November 2019), EMBASE (January 1950 to November 2019), CENTRAL (The Cochrane Library, Issue 11, November 2019), PsycInfo (January 1950 to November 2019), Eric (January 1966 to November 2019), and CINAHL (January 1937 to November 2019). Search words included “resident physicians,” “wellness,” “intervention,” and their synonyms (Table 1).
Table 1.
Search Strategy
| Database | Search Query |
| PubMed | (“Internship and Residency/education”[Mesh] OR “resident physicians”[tiab] OR residency[tiab] OR “medical intern”[tiab] OR “medical residents”[tiab] OR “clinical residents”[tiab] OR clerkship[tiab] OR “graduate medical education”[tiab]) AND (wellness[tiab] OR well-being[tiab] OR wellbeing[tiab] OR mindfulness[tiab] OR resilience*[tiab] OR burnout[tiab] OR “stress reduction”[tiab]) AND (strategy[tiab] OR intervention[tiab] OR program[tiab] OR trial[tiab] OR curriculum[tiab]) |
| PsycInfo | AB (“Graduate Medical Education” OR “house officer” OR “medical residency” OR “resident physicians” OR “medical interns” OR “medical residents” OR “clinical residents”) AND AB (wellness OR well-being OR wellbeing OR mindfulness OR resilience* OR burnout OR “stress reduction”) AND AB (strategy OR intervention OR program OR trial OR curriculum) |
| ERIC | |
| CINAHL | |
| Embase | (“Graduate Medical Education” OR “house officer*” OR “medical residency” OR “resident physicians” OR “medical interns” OR “medical residents” OR “clinical residents”) AND (wellness OR well-being OR mindfulness OR resilience* OR burnout OR “stress reduction”) AND (strategy OR intervention* OR program* OR trial* OR curriculum) |
| Cochrane Controlled Register of Trials (CENTRAL) | (Graduate Medical Education OR house officer OR medical residency OR resident physicians OR medical interns OR medical residents OR clinical residents) AND (wellness OR well-being OR wellbeing OR mindfulness OR resilience* OR burnout OR stress reduction) AND (strategy OR intervention OR program OR trial OR study OR curriculum) |
The inclusion criteria were full-text articles published in an English-language peer-reviewed journal. The participants were resident physicians in GME programs. There were no participant restrictions based on practice setting, time period, training specialty, or any other factors. The exclusion criteria were studies without measured wellness objectives or interventions, duplicate studies, and studies with participants other than resident physicians or unavailable in English. To focus our review on programs that enhance well-being rather than simply prevent burnout, we excluded studies specifically focused on work hour limits.16 Uncontrolled studies were also excluded, as their role in evaluating the effects of interventions is unclear.32
The intervention consisted of programs that aimed to improve the well-being of resident physicians, including elective courses, stress management training, mindfulness programs, wellness curricula, facilitated discussion groups, and resiliency training.
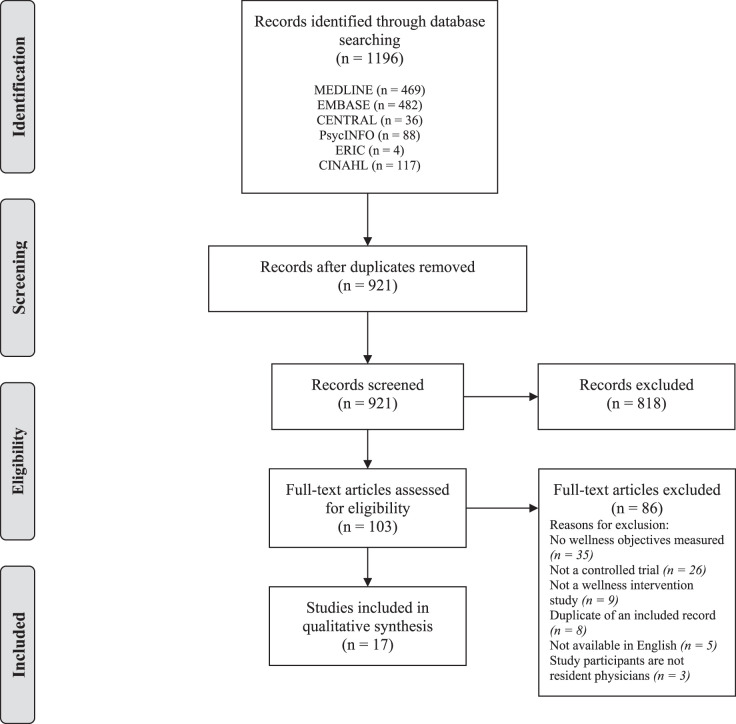
The screening and selection process are displayed in a PRISMA flowchart (Figure 1). We evaluated the certainty of evidence and strength of recommendations of the included studies using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) guidelines.33 We used the GRADEpro Guideline Development Tool software program (McMaster University, Hamilton, Ontario)34 to generate an evidence quality profile of the included studies. The investigators followed Cochrane guidelines to assign study design and subjective metric grades to rate the quality of the included studies. These metrics were: the risk of bias, inconsistency, indirectness, and imprecision. From these inputs, the GRADEpro software generated a final overall GRADE for each included study: “high,” “moderate,” “low,” or “very low.”
Figure 1.
PRISMA Flow Diagram
Results
Study Selection
Our initial search yielded 1196 articles. Further screening resulted in 103 full-text articles, and 17 studies met the inclusion criteria (Figure 1). We identified an additional study that met our inclusion criteria35 in a previous systematic review29; its inclusion resulted in a total of 18 studies. Of the 87 full-text articles excluded, the most common reason (n = 35) was the lack of measured wellness objectives.
Characteristics of Included Studies
The majority of the included articles (11 of 18, 61%) were non-randomized controlled studies (Table 2).36,39,41,44,48,50,51,54,56,57 Seven articles (of 18, 39%) were randomized controlled trials (RCTs).37,38,42,46,47,53,58 The study period of the included articles ranged from 1991 to 2019. Most studies were conducted in the United States (13 of 18, 72%) and Australia (3 of 18, 17%). A total of 666 resident physicians were enrolled in the included studies. Studies were most commonly focused on residents from family medicine (4 of 18, 22%) and any specialty (4 of 18, 22%); specialties are represented in Table 2 with abbreviations derived from the American Board of Medical Specialties.59 The participants' years of training varied; 6 articles studied interventions conducted only with first-year residents,37,46–48,53,57,58 and 2 studied interventions were longitudinal, implemented for a cohort through several years of training.41,56 Participation in most studies was voluntary (14 of 18, 78%).
Table 2.
Characteristics of Included Studies
| Study, Y | Study Design | Specialtya | Sample Size | Educational Theory | Intervention | Intervention Category |
| McCue, 199135 | NRS | Ped, IM | 64 | NR | Workshop | Stress management |
| Ospina-Kammerer, 200336 | NRS | FM | 24 | NR | ROM | Meditation |
| Milstein, 200937 | RCT | Ped | 15 | NR | BATHE psychotherapy | Stress management |
| Bragard, 201038 | RCT | Onc | 96 | NR | Communication and stress management | Stress management |
| Winkel, 201039 | NRS | ObG | 18 | Narrative medicine40 | Reflective writing | Reflection |
| Foster, 201241 | NRS | FM | 18 | NR | RAFT | Discussion |
| Saadat, 201242 | RCT | Anes | 60 | Risk and protective factor model43 | Coping with work and family stress | Stress management |
| Maher, 201344 | NRS | S | 26 | Stress recognition45 | Stress training | Stress management |
| Gunasingam, 201546 | RCT | Any specialty | 31 | NR | Debriefing sessions | Discussion |
| Ripp, 201647 | RCT | IM | 38 | NR | Discussion groups | Discussion |
| Slavin, 201748 | NRS | Ped | 35 | Medical Student Mental Health 3.049 | Resilience training, ethics discussion | Discussion |
| Thimmapuram, 201750 | NRS | Any specialty | 27 | NR | Heartfulness meditation | Meditation |
| Zazulak, 201751 | NRS | ObG, FM | 35 | Visual thinking strategies52 | Art of seeing | Reflection |
| Chanchlani, 201853 | RCT | Any specialty | 53 | NR | Peer mentoring | Mentorship |
| Dotters-Katz, 201854 | NRS | OBG, IM | 20 | Faculty development course55 | Humanism curriculum | Formal curriculum |
| Brennan, 201956 | NRS | FM | 32 | NR | Resiliency skills vs LIFE curriculum | Resilience skills |
| Forbes, 201957 | NRS | Any specialty | 53 | NR | Resiliency skills | Resilience skills |
| Lebares, 201958 | RCT | S | 21 | NR | Mindfulness stress reduction | Stress management |
Abbreviations: NRS, non-randomized controlled study; RCT, randomized controlled trial; FM, family medicine; Onc, oncology; ObG, obstetrics-gynecology; Anes, anesthesiology; S, surgery; IM, internal medicine; Ped, pediatrics; NR, not reported; ROM, Respiratory One Method; BATHE, Background Affect Trouble Handling Empathy; RAFT, Resident Assessment Facilitation Team; LIFE, Learning to Address Impairment and Fatigue to Enhance Patient Safety.
Specialty abbreviations derived from the American Board of Medical Specialties.59
Wellness Interventions
The most common interventions studied were stress management programs (6 of 18, 33%) and facilitated discussion groups (4 of 18, 22%; Table 2). Six studies (6 of 18, 33%) linked wellness interventions to the educational theories on narrative medicine,40 a risk and protective factor model,43 stress recognition,45 mental health,49 visual thinking strategies,52 and humanistic care.55
Wellness Measures
Twenty-seven unique scales and questionnaires were used to measure wellness (Table 3), the most common of which was the Maslach Burnout Inventory (MBI; 11 of 18, 61%). Most of the wellness instruments either reported validity evidence in the literature or were drawn from tools with validity evidence (20 of 27, 74%).
Table 3.
Measures and Outcomes of Included Studies
| Study, Y | Follow-Up Period | Well-Being Measure(s) | Outcomes | GRADE Rating |
| McCue, 199135 | 6 wks | MBIa, LES, ESSI | Improved emotional exhaustion, depersonalization, stress management | Lowc |
| Ospina-Kammerer, 200336 | NR | MBIa | Improved emotional exhaustion | Lowc |
| Milstein, 200937 | 3 mos | MBIa | No significant differences | Moderated |
| Bragard, 201038 | I: 2 mos; C: 8 mos | MBIa; self-efficacy instrument | Increased self-efficacy; decreased stress to communicate | Lowe |
| Winkel, 201039 | 1 y | MBIa; IRIa | Decreased IRI, emotional concern; increased emotional exhaustion | Lowc |
| Foster, 201241 | 2.5 y | AIOSa | No significant differences | Very Lowc,e |
| Saadat, 201242 | 16 wks | Role Quality Scale; CSIa; social support; STAIa; CES-Da; CHIPSa; NSDUHa | Reduced stressors, anxiety; increased social support at work, problem-solving coping | High |
| Maher, 201344 | 24 wks | STAIa | No change in anxiety state | Lowc |
| Gunasingam, 201546 | 10 wks | MBIa | No significant difference in burnout | High |
| Ripp, 201647 | 11 mos | MBIa | No significant differences | High |
| Slavin, 201748 | 10 mos | CES-Da; MBIa; STAIa | Decreased depersonalization, emotional exhaustion, anxiety, mean depression scores, residents with burnout | Lowc |
| Thimmapuram, 201750 | 12 wks | MBIa; EWA | Improved all burnout measures, nearly all EWA attributes | Lowc |
| Zazulak, 201751 | 1 mo | IRIa; Compassion Scalea; FFMQa | No significant differences in IRS, Compassion Scale, overall mindfulness; improved non-judgment of inner experiences, describe/self-expression | Very Lowc,e |
| Chanchlani, 201853 | 12 mos | Semi-structured interview questionsb | Improved stress, morale, support, job satisfaction, psychosocial well-being | High |
| Dotters-Katz, 201854 | 60 days | PMIa; ethical missteps questionnaire | Improved burnout, compassion satisfaction; no differences in interest in and ability to practice, ethical missteps | Lowc |
| Brennan, 201956 | I: 1 y, 2 y, 3 y; C: 1 y | MBIa; ProQOLa; CD-RISCa | Decreased depersonalization, emotional exhaustion | Lowc |
| Forbes, 201957 | 3 mos | ProQOLa; K10a | No change in distress; decreased burnout, secondary traumatic stress; reduced compassion fatigue in controls | Lowc |
| Lebares, 201958 | 8 wks, 1 y | ER89a; CAMS-Ra; Grit-Sa; PSSa; MBIa; PHQ-9a | Increased mindfulness; decreased stress | High |
Abbreviations: NR, not reported; I, intervention; C, control; MBI, Maslach Burnout Inventory; LES, Life Experiences Survey; ESSI, Stress Systems Instrument; IRI, Interpersonal Reactivity Index; AIOS, Arizona Integrative Outcomes Scale; CSI, Coping Strategy Indicator; STAI, State-Trait Anxiety Inventory; CES-D, Center for Epidemiologic Studies Depression Scale; CHIPS, Cohen–Hoberman Inventory of Physical Symptoms; NSDUH, National Survey on Drug Use and Health; EWA, Emotional Wellness Assessment; FFMQ, Five Facet Mindfulness Questionnaire; PMI, Psychological Medicine Inventory; ProQOL, Professional Quality of Life Scale; CD-RISC, Connor-Davidson Resilience Scale; K10, Kessler Psychological Distress Scale; ER89, Ego Resiliency Scale; CAMS-R, Cognitive and Affective Mindfulness Scale–Revised; Grit-S, Short Grit Scale; PSS, Perceived Stress Scale; PHQ-9, 9-item Patient Health Questionnaire.
Supported by validity evidence.
Drawn from tools supported by validity evidence.
Study received lower GRADE rating due to lack of randomization.
Study downgraded due to serious imprecision.
Study downgraded due to serious risk of bias.
Outcomes
The effectiveness of wellness interventions was evaluated using wellness instruments to measure changes in dimensions of burnout, such as emotional exhaustion, depersonalization, stress levels, well-being, and anxiety. Follow-up time for outcomes ranged from 2 weeks44 to 3 years,56 though the follow-up periods of most studies (15 of 18, 83%) were between 1 and 12 months. In 2 studies, follow-up lengths differed between control and intervention participants.38,56
Comparison of Outcomes
Each of the 7 intervention categories in this review had at least 1 study that yielded positive effects on wellness outcomes. The 2 meditation interventions improved emotional exhaustion, burnout, and emotional wellness.36,50 The 2 resilience skills interventions improved levels of depersonalization, emotional exhaustion, and traumatic stress. The mentorship intervention improved stress, morale, and well-being, with certainty of evidence rated “high.”53 The formal curriculum intervention improved burnout scores and compassion satisfaction scores.54
Several interventions had mixed findings. Four of the 6 stress management–based interventions had positive effects on measures of emotional exhaustion,35 self-efficacy,38 stress,35,42 and mindfulness58; 2 resulted in no improvements.37,44 One of the 4 discussion-based interventions decreased depression, burnout, and exhaustion48; the other 3 yielded no significant differences in measured wellness scores.41,46,47 One reflection-based intervention study worsened outcomes, with an increase in emotional exhaustion scores and a decrease in emotional concern scores39; the other yielded no change in empathy, compassion, or overall mindfulness scores, but showed improved mindfulness subdomains of “non-judgment of inner experiences” and “describe/self-expression.”51
Evaluation of Study Quality
Our GRADE evaluations of the included studies found 5 “high,” 1 “moderate,” 10 “low,” and 2 “very low” ratings (Table 3). The major factor resulting in low GRADE ratings was the lack of randomization; just 7 of the studies were RCTs. Three studies were downgraded due to serious risk of bias per GRADE guidelines.38,41,51 Of these, 2 received a “very low” rating41,51 and one received a “low” rating.38 Reasons for high risk of bias for the “very low” GRADE studies included not listing the number of individuals in the control group compared to the intervention group41 and large resident specialty and gender differences between control and intervention groups.51 The high risk of bias of the “low” GRADE was attributed to post-intervention assessments of different lengths for intervention and control groups; furthermore, the authors did not discuss all data that were described as collected in the methods.51 Across all studies, there were no cases of serious inconsistency or indirectness. We did not upgrade any studies based on the magnitude, strength, or plausible confounding of evidence.
Discussion
We conducted a systematic review of 18 controlled studies on the effect of wellness interventions on 666 resident physicians. Improvement in at least 1 studied wellness outcome was reported in 13 studies, only 3 of which received a high GRADE rating.42,53,58
There were several characteristics of successful interventions. First, certain intervention categories—meditation, resilience skills, mentorship, and formal curricular interventions—consistently improved resident wellness. These interventions combined peer support with individual mindfulness or relaxation strategies to promote community building and self-help.36,50,53,54,56,57 Second, incorporating resident feedback in the program design focused the wellness program on the specific needs of the study population. Two studies surveyed residents to identify the humanistic values they found challenging to uphold54 and the specific skills they wanted to learn, respectively.56,60 Third, several studies used educational theory to target improvements in particular wellness objectives.39,42,44,48,51,54 The only successful discussion group intervention was guided by an educational theory-based curricular change program, “Medical Student Mental Health 3.0.”48 Similarly, 1 of the 3 successful studies for which the GRADE evaluation indicated a high quality of evidence was grounded in a risk and protective factor model.42 Drawing on this conceptual theory, which posits that decreasing risk factors and increasing protective factors reduces negative health outcomes, the intervention successfully promoted residents' wellness by alleviating stressors and introducing coping strategies and social support. Grounding medical education in this or other learning theories, such as Kolb's experiential learning cycle or Schon's reflective practice, can produce innovative, robust interventions that are more likely to succeed.61,62 Fourth, integrating wellness programs into the existing didactic residency curriculum made the interventions more available and accessible to residents.51,57,58 In one case, a feasibility study showed that offering interventions during protected class time was possible with strategic planning and coordination with other clinicians to cover shifts.63 Lastly, most of the successful programs had voluntary participation.38,42,50,51,53,54,56–58 This approach acknowledges residents' perceived lack of control over-scheduling and decision-making, which is consistently cited as a precipitating factor for resident burnout.64–66
Limitations of the Evidence Base
One notable limitation of the studies examined in this review was the use of instruments unsupported by validity evidence to assess intervention efficacy. The most common instrument used was the MBI. The MBI is considered the gold standard for measuring burnout, but there is limited validity evidence for its use with physicians-in-training.67 Residents' unique professional life challenges, including performance evaluations and unpredictable schedules, warrant a specific wellness measurement tool.67 Furthermore, the MBI focused exclusively on burnout; hence, it did not offer a complete representation of resident physician well-being, prompting programs to rely on supplementary inventories to more holistically assess well-being.68 Another limitation of the MBI is its cost; researchers must purchase the survey license, manual, and score reports.69 This review highlights the need for a comprehensive wellness instrument supported by validity evidence for resident physicians.
Another limitation was the lack of standardized methodology to assess interventions: the 18 included studies used 27 unique instruments to measure wellness. Indeed, most studies used more than 1 assessment to evaluate multiple domains of wellness in a program. This approach may impact study results: each of the 5 studies that reported no difference in wellness outcomes only utilized 1 instrument to measure well-being.37,41,44,46,47 Equally important, this variability reduces the generalizability of the interventions and makes them more challenging to implement. Furthermore, the lack of consistency in types of reported outcomes across studies hinders comparison between the studies. Future interventions would benefit from a consensus on an appropriate scale for holistically evaluating resident physicians' well-being.
In addition, both the timing of intervention during residency and the post-intervention follow-up periods differed among the included studies. Some interventions targeted only interns,46–48,53,57,58 while others recruited residents of all years.35,37–39,41,42,54,56 Burnout is known to develop cumulatively over time,66 so early and sustained interventions may be particularly effective. Longitudinal interventions can carry several advantages, including allowing researchers to study long-term effects70 and providing adequate time for shaping a culture of wellness that prevents, rather than treats, burnout.71 The post-intervention follow-up periods varied both within38,56 and across studies.35,36,38,39,41,42,44,46–48,50,51,53,54,56–58 The National Academies of Sciences, Engineering, and Medicine recommends that follow-up for clinician wellness interventions occurs at least 6 to 12 months post-intervention2; fewer than half (8 of 18, 44%) of the included studies followed this recommendation.35,39,41,47,48,53,56
Lastly, none of the included studies measured effects of the intervention on patient outcomes. Residents at higher risk of burnout pose greater risks to patient safety.72 Further research is needed to evaluate how resident wellness programming impacts patient safety.
Implications for Residency Training
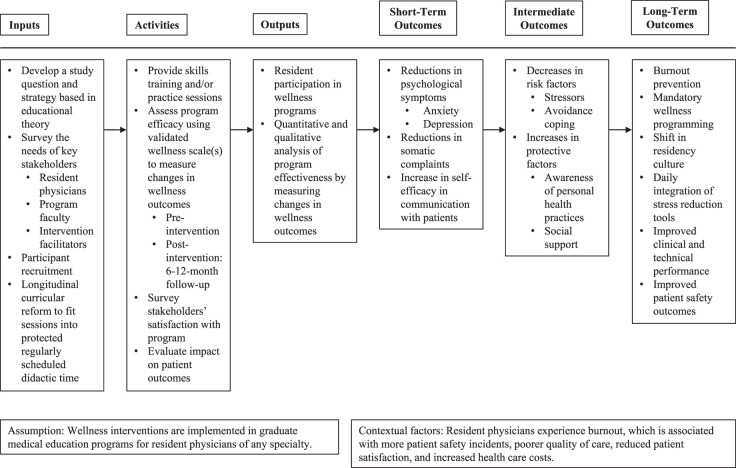
Future wellness initiatives would benefit from a conceptual foundation defining the process and outcomes of the intervention. Logic models can provide such a foundation.73–75 A logic model can serve as a planning tool, which then can be modified to meet the specific needs of a residency program wellness intervention. We formulated a logic model as a framework to guide future wellness interventions for resident physicians (Figure 2). This framework draws on common measures of successful programs studied in this review to outline the inputs, activities, outputs, outcomes, assumptions, and contextual factors to consider in intervention planning and development. The inputs include resources for key stakeholders to leverage, such as educational theories, surveying needs, and protected didactic time. The activities constitute the intervention sessions and evaluations. The ensuing outputs are the engagement of resident physicians in the programming and the analyses of the results of the intervention. The outcomes are divided into short-term, intermediate, and long-term results of the intervention. The assumptions about the setting and population of resident wellness programs, and such contextual factors as the negative outcomes of burnout, are necessary considerations when implementing a wellness program.
Figure 2.
Resident Physician Wellness Intervention Logic Model
Limitations of This Systematic Review
There are several potential limitations of this review. First, we did not include studies based on uncontrolled interventions, studies on duty hours, and studies published in languages other than English. Second, we did not hand-search bibliographies of included studies, and we excluded unpublished studies. Third, the reproducibility of GRADE ratings is limited by the authors' judgments about the quality of evidence and strength of recommendations.76 Fourth, we did not investigate differences across specialties or across countries; however, these comparisons would have been of limited value given the 27 unique instruments used to evaluate resident wellness we uncovered in the literature. Fifth, this review focused on wellness initiatives in residency training programs, so our findings may not be generalizable to fellowship training.
Conclusions
This systematic review highlights several factors that can contribute to the success of a wellness intervention: grounding the intervention in educational theory, soliciting participant feedback, relying on voluntary participation, and integrating the intervention into the existing GME curricula. A logic model can help future resident wellness initiatives implement these findings.
Footnotes
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
The authors would like to thank Andrew Creamer, MAEd, MSLIS, and Kelsey Sawyer, MLIS, Brown University Library, for consulting on the literature search and Alfred A. Paul, MD, for reviewing the manuscript.
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the US Department of Veterans Affairs or the US Government.
References
- 1.World Health Organization. International Statistical Classification of Diseases and Related Health Problems. 2020 https://icd.who.int/ Accessed November 30.
- 2.National Academies of Sciences Engineering and Medicine. Taking Action Against Clinician Burnout A Systems Approach to Professional WellBeing. Washington, DC: The National Academies Press; 2019. [PubMed] [Google Scholar]
- 3.Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. An Official Critical Care Societies Collaborative statement: burnout syndrome in critical care healthcare professionals: a call for action. Crit Care Med. 2016;44(7):1414–1421. doi: 10.1097/CCM.0000000000001885. [DOI] [PubMed] [Google Scholar]
- 4.Shanafelt TD, West CP, Sinsky C, Trockel M, Tutty M, Satele DV, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clin Proc. 2019;94(9):1681–1694. doi: 10.1016/j.mayocp.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 5.Berg S Physician burnout: which medical specialties feel the most stress. American Medical Association. https://www.ama-assn.org/practice-management/physician-health/physician-burnout-which-medical-specialties-feel-most-stress Published January 21, 2020. Accessed November 30, 2020.
- 6.Dyrbye LN, Burke SE, Hardeman RR, Herrin J, Wittlin NM, Yeazel M, et al. Association of clinical specialty with symptoms of burnout and career choice regret among US resident physicians. JAMA. 2018;320(11):1114–1130. doi: 10.1001/jama.2018.12615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Panagioti M, Geraghty K, Johnson J, Zhou A, Panagopoulou E, Chew-Graham C, et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta-analysis. JAMA Intern Med. 2018;178(10):1317–1331. doi: 10.1001/jamainternmed.2018.3713. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 8.Han S, Shanafelt TD, Sinsky CA, Awad KM, Dyrbye LN, Fiscus LC, et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019;170(11):784–790. doi: 10.7326/M18-1422. [DOI] [PubMed] [Google Scholar]
- 9.Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, et al. Burnout among US medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89(3):443–451. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 10.West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306(9):952–960. doi: 10.1001/jama.2011.1247. [DOI] [PubMed] [Google Scholar]
- 11.Attenello FJ, Buchanan IA, Wen T, Donoho DA, McCartney S, Cen SY, et al. Factors associated with burnout among US neurosurgery residents: a nationwide survey. J Neurosurg. 2018;129(5):1349–1363. doi: 10.3171/2017.9.JNS17996. [DOI] [PubMed] [Google Scholar]
- 12.Dyrbye L, Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med Educ. 2016;50(1):132–149. doi: 10.1111/medu.12927. [DOI] [PubMed] [Google Scholar]
- 13.Moradi Y, Baradaran HR, Yazdandoost M, Atrak S, Kashanian M. Prevalence of burnout in residents of obstetrics and gynecology: a systematic review and meta-analysis. Med J Islam Repub Iran. 2015;29(4):235. [PMC free article] [PubMed] [Google Scholar]
- 14.Malek M, Mohammadi S, Attarchi M. Occupational stress and influencing factors, in medical residents of one of the educational hospitals of Tehran University of Medical Sciences. Razi J Med Sci. 2011;18(87):24–35. [Google Scholar]
- 15.Ebrahimi S, Kargar Z. Occupational stress among medical residents in educational hospitals. Ann Occup Environ Med. 2018;30:51. doi: 10.1186/s40557-018-0262-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Accreditation Council for Graduate Medical Education. Common Program Requirements (Residency) 2020 https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRResidency2020.pdf Accessed December 1.
- 17.American College of Physicians. IMITE. 2020 https://www.acponline.org/featured-products/medical-educator-resources/im-ite Accessed December 1.
- 18.American Board of Family Medicine. InTraining Examination. 2020 https://www.theabfm.org/become-certified/acgme-program/in-training-examination Accessed December 1.
- 19.The American Board of Pediatrics. General Pediatrics InTraining Examination. 2020 https://www.abp.org/content/general-pediatrics-training-examination Accessed December 1.
- 20.American Board of Surgery. General Surgery Qualifying Exam. 2020 https://www.absurgery.org/default.jsp?certgsqe Accessed December 1.
- 21.American College of Obstetricians and Gynecologists. CREOG InTraining Examination. 2020 https://www.acog.org/education-and-events/creog/creog-in-training-examination Accessed December 1.
- 22.Association of American Medical Colleges. Statement for the Record Submitted by the Association of American Medical Colleges (AAMC) to the House of Representatives Committee on Small Business: The Doctor is Out. Rising Student Loan Debt and the Decline of the Small Medical Practice. 2020 https://www.aamc.org/system/files/c/1/498034-aamcstatementtothehousesmallbusinesscommitteeregardingmedicaled.pdf Accessed December 1.
- 23.Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377–1385. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 24.Martin M. Physician well-being: physician burnout. FP Essent. 2018;471:11–15. [PubMed] [Google Scholar]
- 25.Spiotta AM, Fargen KM, Patel S, Larrew T, Turner RD. Impact of a residency-integrated wellness program on resident mental health, sleepiness, and quality of life. Neurosurgery. 2019;84(2):341–346. doi: 10.1093/neuros/nyy112. [DOI] [PubMed] [Google Scholar]
- 26.Wei H, Kifner H, Dawes ME, Wei TL, Boyd JM. Self-care strategies to combat burnout among pediatric critical care nurses and physicians. Crit Care Nurse. 2020;40(2):44–53. doi: 10.4037/ccn2020621. [DOI] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention. WellBeing Concepts. 2020 https://www.cdc.gov/hrqol/wellbeing.htm#three Accessed December 1.
- 28.West CP, Dyrbye L, Erwin PJ, Shanafelt T. Interventions to reduce physician burnout: systematic review and meta-analysis. Lancet. 2016;388(10057):2272–2281. doi: 10.1016/S0140-6736(16)31279-X. [DOI] [PubMed] [Google Scholar]
- 29.Busireddy KR, Miller JA, Ellison K, Ren V, Qayyum R, Panda M. Efficacy of interventions to reduce resident physician burnout: a systematic review. J Grad Med Educ. 2017;9(3):294–301. doi: 10.4300/JGME-D-16-00372.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Accreditation Council for Graduate Medical Education. ACGME Aware WellBeing Resources. 2020 https://dl.acgme.org/pages/well-being Accessed December 1.
- 31.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339 doi: 10.1136/bmj.b2535. b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barton S. Which clinical studies provide the best evidence? The best RCT still trumps the best observational study. BMJ. 2000;321(7256):255–256. doi: 10.1136/bmj.321.7256.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schünemann H, Brożek J, Guyatt G, Oxman A. GRADE. Handbook. 2020 https://gdt.gradepro.org/app/handbook/handbook.html Accessed December 1.
- 34.GRADEpro GDT. GRADEpro Guideline Development Tool [computer program] McMaster University: Evidence Prime, Inc;; 2015. [Google Scholar]
- 35.McCue JD, Sachs CL. A stress management workshop improves residents' coping skills. Arch Intern Med. 1991;151(11):2273–2277. [PubMed] [Google Scholar]
- 36.Ospina-Kammerer V, Figley CR. An evaluation of the Respiratory One Method (ROM) in reducing emotional exhaustion among family physician residents. Int J Emerg Ment Health. 2003;5(1):29–32. [PubMed] [Google Scholar]
- 37.Milstein JM, Raingruber BJ, Bennett SH, Kon AA, Winn CA, Paterniti DA. Burnout assessment in house officers: evaluation of an intervention to reduce stress. Med Teach. 2009;31(4):338–341. doi: 10.1080/01421590802208552. [DOI] [PubMed] [Google Scholar]
- 38.Bragard I, Etienne AM, Merckaert I, Libert Y, Razavi D. Efficacy of a communication and stress management training on medical residents' self-efficacy, stress to communicate and burnout: a randomized controlled study. J Health Psychol. 2010;15(7):1075–1081. doi: 10.1177/1359105310361992. [DOI] [PubMed] [Google Scholar]
- 39.Winkel AF, Hermann N, Graham MJ, Ratan RB. No time to think: making room for reflection in obstetrics and gynecology residency. J Grad Med Educ. 2010;2(4):610–615. doi: 10.4300/JGME-D-10-00019.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Charon R. Narrative and medicine. N Engl J Med. 2004;350(9):862–864. doi: 10.1056/NEJMp038249. [DOI] [PubMed] [Google Scholar]
- 41.Foster E, Biery N, Dostal J, Larson D. RAFT. (Resident Assessment Facilitation Team): supporting resident well-being through an integrated advising and assessment process. Fam Med. 2012;44(10):731–734. [PubMed] [Google Scholar]
- 42.Saadat H, Snow DL, Ottenheimer S, Dai F, Kain ZN. Wellness program for anesthesiology residents: a randomized, controlled trial. Acta Anaesthesiol Scand. 2012;56(9):1130–1138. doi: 10.1111/j.1399-6576.2012.02705.x. [DOI] [PubMed] [Google Scholar]
- 43.Coie JD, Watt NF, West SG, Hawkins JD, Asarnow JR, Markman HJ, et al. The science of prevention. A conceptual framework and some directions for a national research program. Am Psychol. 1993;48(10):1013–1022. doi: 10.1037//0003-066x.48.10.1013. [DOI] [PubMed] [Google Scholar]
- 44.Maher Z, Milner R, Cripe J, Gaughan J, Fish J, Goldberg AJ. Stress training for the surgical resident. Am J Surg. 2013;205(2):169–174. doi: 10.1016/j.amjsurg.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 45.Arora S, Sevdalis N, Nestel D, Woloshynowych M, Darzi A, Kneebone R. The impact of stress on surgical performance: a systematic review of the literature. Surgery. 2010;147(3):318–330. doi: 10.1016/j.surg.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 46.Gunasingam N, Burns K, Edwards J, Dinh M, Walton M. Reducing stress and burnout in junior doctors: the impact of debriefing sessions. Postgrad Med J. 2015;91(1074):182–187. doi: 10.1136/postgradmedj-2014-132847. [DOI] [PubMed] [Google Scholar]
- 47.Ripp JA, Fallar R, Korenstein D. A randomized controlled trial to decrease job burnout in first-year internal medicine residents using a facilitated discussion group intervention. J Grad Med Educ. 2016;8(2):256–259. doi: 10.4300/JGME-D-15-00120.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Slavin S, Shoss M, Broom MA. A program to prevent burnout, depression, and anxiety in first-year pediatric residents. Acad Pediatr. 2017;17(4):456–458. doi: 10.1016/j.acap.2016.12.016. [DOI] [PubMed] [Google Scholar]
- 49.Slavin SJ, Schindler DL, Chibnall JT. Medical student mental health 3.0: improving student wellness through curricular changes. Acad Med. 2014;89(4):573–577. doi: 10.1097/ACM.0000000000000166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Thimmapuram J, Pargament R, Sibliss K, Grim R, Risques R, Toorens E. Effect of heartfulness meditation on burnout, emotional wellness, and telomere length in health care professionals. J Community Hosp Intern Med Perspect. 2017;7(1):21–27. doi: 10.1080/20009666.2016.1270806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zazulak J, Sanaee M, Frolic A, Knibb N, Tesluk E, Hughes E, et al. The art of medicine: arts-based training in observation and mindfulness for fostering the empathic response in medical residents. Med Humanit. 2017;43(3):192–198. doi: 10.1136/medhum-2016-011180. [DOI] [PubMed] [Google Scholar]
- 52.Reilly JM, Ring J, Duke L. Visual thinking strategies: a new role for art in medical education. Fam Med. 2005;37(4):250–252. [PubMed] [Google Scholar]
- 53.Chanchlani S, Chang D, Ong JSL, Anwar A, Ong JS. The value of peer mentoring for the psychosocial wellbeing of junior doctors: a randomised controlled study. Med J Aust. 2018;209(9):401–405. doi: 10.5694/mja17.01106. [DOI] [PubMed] [Google Scholar]
- 54.Dotters-Katz SK, Chuang A, Weil A, Howell JO. Developing a pilot curriculum to foster humanism among graduate medical trainees. J Educ Health Promot. 2018;7:2. doi: 10.4103/jehp.jehp_45_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Branch WT, Jr, Frankel R, Gracey CF, Haidet PM, Weissmann PF, Cantey P, et al. A good clinician and a caring person: longitudinal faculty development and the enhancement of the human dimensions of care. Acad Med. 2009;84(1):117–125. doi: 10.1097/ACM.0b013e3181900f8a. [DOI] [PubMed] [Google Scholar]
- 56.Brennan J, McGrady A, Tripi J, Sahai A, Frame M, Stolting A, et al. Effects of a resiliency program on burnout and resiliency in family medicine residents. Int J Psychiatry Med. 2019;54(4–5):327–335. doi: 10.1177/0091217419860702. [DOI] [PubMed] [Google Scholar]
- 57.Forbes M, Byrom L, van der Steenstraten I, Markwell A, Bretherton H, Kay M. Resilience on the run—an evaluation of a wellbeing program for medical interns. Intern Med J. 2020;50(1):92–99. doi: 10.1111/imj.14324. [DOI] [PubMed] [Google Scholar]
- 58.Lebares CC, Guvva EV, Olaru M, et al. Efficacy of mindfulness-based cognitive training in surgery: additional analysis of the mindful surgeon pilot randomized clinical trial. JAMA Netw Open. 2019;2(5):e194108. doi: 10.1001/jamanetworkopen.2019.4108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.American Board of Medical Specialties. Codes and Abbreviations. 2020 https://www.abmsdirectory.com/pdf/Resources_Certification_codes.pdf Accessed December 1.
- 60.Brennan J, McGrady A. Designing and implementing a resiliency program for family medicine residents. Int J Psychiatry Med. 2015;50(1):104–114. doi: 10.1177/0091217415592369. [DOI] [PubMed] [Google Scholar]
- 61.Kamel-ElSayed S, Loftus S. Using and combining learning theories in medical education. Med Sci Educ. 2018;28(1):255–258. [Google Scholar]
- 62.Zackoff MW, Real FJ, Abramson EL, Li S-TT, Klein MD, Gusic ME. Enhancing educational scholarship through conceptual frameworks: a challenge and roadmap for medical educators. Acad Pediatr. 2019;19(2):135–141. doi: 10.1016/j.acap.2018.08.003. [DOI] [PubMed] [Google Scholar]
- 63.Lebares CC, Hershberger AO, Guvva EV, Desai A, Mitchell J, Shen W, et al. Feasibility of formal mindfulness-based stress-resilience training among surgery interns: a randomized clinical trial. JAMA Surg. 2018;153(10):e182734. doi: 10.1001/jamasurg.2018.2734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Alhaffar BA, Abbas G, Alhaffar AA. The prevalence of burnout syndrome among resident physicians in Syria. J Occup Med Toxicol. 2019;14(1):31. doi: 10.1186/s12995-019-0250-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Thomas NK. Resident burnout. JAMA. 2004;292(23):2880–2889. doi: 10.1001/jama.292.23.2880. [DOI] [PubMed] [Google Scholar]
- 66.Ishak WW, Lederer S, Mandili C, Nikravesh R, Seligman L, Vasa M, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;1(2):236–242. doi: 10.4300/JGME-D-09-00054.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Eckleberry-Hunt J, Kirkpatrick H, Barbera T. The problems with burnout research. Acad Med. 2018;93(3):367–370. doi: 10.1097/ACM.0000000000001890. [DOI] [PubMed] [Google Scholar]
- 68.Trockel M, Bohman B, Lesure E, et al. A brief instrument to assess both burnout and professional fulfillment in physicians: reliability and validity, including correlation with self-reported medical errors, in a sample of resident and practicing physicians. Acad Psychiatry. 2018;42(1):11–24. doi: 10.1007/s40596-017-0849-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mind Garden. MBI: Human Services Survey for Medical Personnel. 2020 https://www.mindgarden.com/315-mbi-human-services-survey-medical-personnel Accessed December 1.
- 70.Caruana EJ, Roman M, Hernández-Sánchez J, Solli P. Longitudinal studies. J Thorac Dis. 2015;7(11):e537–e540. doi: 10.3978/j.issn.2072-1439.2015.10.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Eckleberry-Hunt J, Van Dyke A, Lick D, Tucciarone J. Changing the conversation from burnout to wellness: physician well-being in residency training programs. J Grad Med Educ. 2009;1(2):225–230. doi: 10.4300/JGME-D-09-00026.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.De Oliveira GS, Jr, Almeida MD, Ahmad S, Fitzgerald PC, McCarthy RJ. Anesthesiology residency program director burnout. J Clin Anesth. 2011;23(3):176–182. doi: 10.1016/j.jclinane.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 73.Centers for Disease Control and Prevention. Logic Models. 2020 https://www.cdc.gov/eval/logicmodels/index.htm Accessed December 1.
- 74.Baxter SK, Blank L, Woods HB, Payne N, Rimmer M, Goyder E. Using logic model methods in systematic review synthesis: describing complex pathways in referral management interventions. BMC Med Res Methodol. 2014;14(1):62. doi: 10.1186/1471-2288-14-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Peyton DJ, Scicchitano M. Devil is in the details: using logic models to investigate program process. Eval Program Plann. 2017;65:156–162. doi: 10.1016/j.evalprogplan.2017.08.012. [DOI] [PubMed] [Google Scholar]
- 76.Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]