Abstract
Purpose
Bariatric surgery is an effective treatment for obesity with new procedures emerging. However, despite comparable weight loss and improvements in metabolic outcomes, research on nutritional and gastrointestinal symptoms remains limited. Here we compare clinical data on weight, nutritional disorders and gastrointestinal symptoms of patients before and following one anastomosis gastric bypass (OAGB) and Roux-en-Y gastric Bypass (RYGB).
Materials and Methods
In this retrospective study, data on anthropometry, nutritional indices, dietary intake and gastrointestinal symptoms were retrieved in cohorts of patients up to 2 years following OAGB and RYGB.
Results
Seventy-three patients had either a RYGB (28) or an OAGB (45), with 71% seeking these as a revisional procedure. Significant and higher weight loss was observed in the OAGB cohort at 1 year (%TWL 33.0 ± 8.5 vs. 26.6 ± 12.4), albeit comparable at 2 years postoperatively (%TWL 29.0 ± 11.1 vs. 34.1 ± 11.2). Disorders such as vitamin D, active B12, folate, homocystein (Hcy) and hyperparathyroidism were present following both surgeries. Levels of vitamin D, ferritin and total protein significantly worsened over time. Gastrointestinal symptoms of diarrhoea, steatorrhoea and reflux were higher in the OAGB cohort while the RYGB cohort reported more dumping syndrome (DS).
Conclusion
Significant and similar weight loss results are seen following both OAGB and RYGB. Nutritional disorders were common in both cohorts and increased over time. However, the OAGB patients reported more gastrointestinal side effects, which may contribute to poor quality of life and nutritional consequences. Prospective and longer-term studies investigating the nutritional and gastrointestinal health of patients undergoing OAGB is recommended.
Keywords: Nutrition, nutritional disorders; Gastrointestinal symptoms; Obesity surgery; One anastomosis gastric bypass; Roux-en-Y gastric bypass
Introduction
The management of obesity and its related comorbidities remains a global challenge. Despite multimodal treatments in assisting weight loss, the body’s tendency to maintain weight makes most conservative treatments suboptimal [1]. Bariatric surgery is the most effective treatment for the condition of obesity, with resolution of weight-related comorbidities, hence reducing mortality in addition to improving quality of life [2]. However, bariatric procedures result in medical and nutritional consequences, which are unique for each procedure. The procedures continue to evolve and new techniques such as the one anastomosis gastric bypass (OAGB) emerging internationally. However, there are inadequate studies on their long-term nutritional outcomes. Nutritional disorders have been shown to be common among patients who undergo bariatric surgery, and this has been contributed to poor diet quality, chronic dieting and the physiology of chronic obesity [3–8]. Furthermore, the changes in gastrointestinal system and its impact on ingestion, digestion and absorption of nutrients further impact the nutritional health of patients following surgery [4, 8, 9]. Each bariatric procedure results in nutritional deficiencies through slightly different mechanisms. The laparoscopic adjusted gastric banding (LAGB) does this through significantly reducing the diet quantity as well as inducing some food intolerances and hence impacting overall diet quality and nutritional health [10–12]. The gastric bypass procedures and the sleeve gastrectomy (SG) also reduce the diet quantity, however, with less impact on the food tolerance. In these procedures, the rapid transient of the nutrients through the gastrointestinal tract and hence inadequate mixing with the pancreatic enzymes adds to their malabsorptive component. Furthermore, in gastric bypass procedures, bypassing the primary absorption site of certain nutrients can further exacerbate the postoperative nutritional disorders [4, 7, 13].
The identification of the potential side effects will not only allow prevention and optimal treatment of these consequences, but also assist in choice of procedure for the patient in pre surgical moment.
The standard Roux-en-Y gastric bypass (RYGB) procedure has long been the procedure of choice internationally, with significant long-term published data on its risk and benefits [14]. A modified gastric bypass termed one anastomosis gastric bypass (OAGB) has emerged more recently [15], which is thought to be restrictive and malabsorptive thus inducing hormonal changes similar to the RYGB [16]. The current literature indicates that the OAGB produces comparable weight loss and metabolic benefits to that of RYGB, with shorter operative time due to a lesser technical complexity [16, 17]. A recent consensus statement by the international federation of obesity task force, recognised OAGB as an acceptable surgical option, but recommended long-term multidisciplinary follow-up [15].
To date, despite the reported nutritional deficiencies and related complications [3, 18], there are no specific nutritional guidelines for the management of OAGB patients. In the absence of recommendations, nutritional management has been based on the RYGB in most clinical setting [9]. However, the current evidence suggests that compared to the RYGB, OAGB has higher adverse nutritional and digestive symptoms such as diarrhoea, steatorrhoea and bile reflux esophagitis, which in some cases necessitates nutritional support and/or revisional surgery [3, 19]. The malabsorptive nature of this procedure compared to the RYGB is thought to be the contributing factor to malnutrition, and the longer the biliopancreatic limb (BPL) (300 cm cf 150–200 cm), the more severe the consequences [18]. These complications, coupled with the lack of long-term evidence on medical and nutritional outcomes, have slowed universal adoption of OAGB [3, 9, 15, 16, 18].
This study aims to compare clinical data on anthropometry, nutritional indices, dietary intake and gastrointestinal symptoms in cohorts of patients 6, 12 and 24 months following OAGB or RYGB from a private bariatric clinic.
Material and Methods
This retrospective cohort study reports on anthropometric measures, nutritional indices and gastrointestinal symptoms of patients who had undergone OAGB and RYGB in a multidisciplinary private clinic in Sydney, Australia from May 2015 to May 2019. All patients had undergone a multidisciplinary assessment and met the international criteria for bariatric surgery [9, 20]. There were no exclusion criteria, and all 78 patients who presented for either bypass surgery were included in the study.
For the RYGB, a long gastric pouch was fashioned over a size 40 bougie. The stomach was transected at the incisura. A 100-cm BPL and a 100-cm ante-colic alimentary limb were used. The gastrojejunostomy and jejunojejunostomy were created using linear staplers. For the OAGB, a long gastric tube was fashioned over a size 40 bougie. The stomach was transected at the incisura. A 200-cm BPL was typically used. The gastrojejunostomy was performed using a linear stapler.
Electronic medical records were accessed to retrieve data on anthropometry, biochemistry, nutritional markers and reported dietary intake and gastrointestinal symptoms at 6 months, 1 and 2 years postoperatively.
The Clinic Protocol
The clinic protocol included routine consultation by the surgeon and nutritional assessment and counselling by two bariatric trained accredited practicing dietitians at pre and postoperative at 2 and 4 weeks, and then at 2, 6 and 12 months and yearly thereafter.
Nutritional counselling and education was provided by the dietitian according to the ASMBS bariatric guidelines [4, 8, 20] and were personalised for each patient’s individual requirement. Micronutrient supplements recommended were 2 comprehensive bariatric specific high-dose multivitamin aiming to provide 200% of the recommended dietary intake, calcium and vitamin D (aiming for a total of 1500-mg calcium with 800 IU vitamin D). Iron, folate, vitamin B12 and additional vitamin D were recommended based on the ASMBS bariatric guidelines [4, 8, 20] and tailored as needed on an individual basis.
Anthropometry
A Wedderburn scale was used for measuring weight. Height was measured, and body mass index (BMI) {weight (kg)/height2 (cm)}, change in BMI, total weight loss (TWL), percentage of total weight loss (%TWL) (weight loss (kg)/pre op weight × 100) and percentage of excess weight loss (%EWL) were calculated (weight loss (kg)/EW (kg) × 100). We used the highest initial weight for all patients to reflect their full weight loss journey.
Biochemical Assessments
Nutritional indices included biochemical markers such as: serum albumin, total protein, vitamin B12, active B12, serum folate, haemoglobin (Hb), iron, ferritin, homocysteine (Hcy), magnesium, intact parathyroid hormone (iPTH), calcium and vitamin D. These indices were collected using standard hospital procedure. Fasting blood glucose level (FBGL) and C-reactive protein (CRP) were also noted.
Levels of nutrients were assessed based on the standard laboratory values, and patients were considered having disordered levels if, iron < 5 umol/L, ferritin < 15 ug/L, folate < 7 nmol/L, Vitamin D < 50 nmol/L, Hb was < 119 g/L in women and < 130 g/L in men. Furthermore, other biochemical indices were also noted, and patients were considered having disordered levels if, albumin < 37 g/L, Hcy > 14 umol/L, iPTH > 50 pg/ml (or > 6.9 pmol/L) and CRP > 10 mg/L.
Based on previous studies and recommendations, in order to improve sensitivity and specificity for serum vitamin B12, the values of less than 350 pg/ml (250 pmol/L) was considered to be deficient [3, 21].
Dietary Assessment
At each dietetic follow-up, a qualitative dietary assessment using retrospective diet history was conducted and compared to the bariatric dietary recommendations [22]. An unbalanced diet was defined by consuming lower amounts of protein (< 2 servings per day or < 60 g total protein intake), dairy (< 3 servings per day), fruit (< 2 servings per day) and vegetables (< 4 servings per day) and higher in energy dense, low nutrient, low fibre carbohydrates (> 1 serving per day).
Gastrointestinal Symptoms
At each follow-up, as part of routine clinical assessment, both surgeons and the dietitians assessed and recorded any gastrointestinal symptoms reported by patients.
Ethics
The study was approved by the University of Wollongong / Illawarra Shoalhaven Local Health District Human Research Ethics Committee (#2019/108), and for this type of study, formal consent was not required.
Statistical Analysis
Descriptive statistics were expressed as mean ± standard deviation for continuous variables (anthropometry and analytical variables) and percentages for categorical data (deficiency or compliance rates). Inferential analysis was performed using IBM® Statistical Package for the Social Sciences® (SPSS®) version 26. Linear mixed models were used to compare baseline and follow-up data and Bonferroni post-hoc test to pair-wise comparisons. T tests or Mann-Whitney tests were used to compare groups, and comparisons of proportions with nutrient disorders, diet adequacy and presence of gastrointestinal symptoms were performed using Pearson Chi-square when the assumption was met or Fisher’s exact test when the assumption was violated. A p value < 0.05 was considered statistically significant.
Results
Demographics
The baseline characteristics are described in Table 1. A total of 73 patients underwent bypass procedures with a mean preoperative BMI of 45.4 ± 8.1 kg/m2 for the entire cohort. The majority of patients were female, and there was no difference between gender and age between the two cohorts. However, both preoperative weight and BMI were significantly higher in the OAGB cohort (Table 1).
Table 1.
Patients’ preoperative characteristics
| Total | RYGB | OAGB | p value | |
|---|---|---|---|---|
| Number of patients | 73 | 28 | 45 | |
| Gender ratio female/male (%F) | 54/19 (74) | 22/6 (78) | 32/13 (71) | 0.480* |
|
Age (years) (range) |
51.7 ± 10.6 (27-71) |
50.5 ± 9.5 | 52.7 ± 11.3 | 0.447** |
|
Body weight (kg ± SD) (range) |
126.9 ± 22.0 (86.0 – 187.6) |
120.5 ± 24.4 (86.0 -174.0) |
130.85 ± 19.5 (96.0 - 187.6) |
0.049** |
|
BMI (kg/m2 ± SD) (range) |
45.4 ± 8.1 (32.4 – 66.4) |
42.5 ± 7.3 (32.4 – 61.6) |
47.1 ± 8.0 (33.6 – 66.4) |
0.014** |
| Revisional surgery | 73% (52) | 82.1% (23) | 64.4% (29) | 0.104* |
RYGB Roux-en-Y gastric bypass, OAGB one anastomosis gastric bypass, BMI body mass index, SD standard deviation
*Pearson Chi-square; **Independent T test
The majority (71.2% n = 52) of both procedures were performed as revisional surgeries; this was higher in the RYGB cohort (82.1% n = 23 vs. 64.4% n = 29) but with no significant difference (p = 0.104). The main primary procedures in the RYGB cohort were laparoscopic adjusted gastric banding (LAGB) in 37% (n = 9), sleeve gastrectomy (SG) in 33% (n = 8), OAGB in 4% (n = 1) and 6 patients had multiple procedures (25%). In the OAGB cohort, 55% (n = 25) of the revisional cases had a LAGB previously. The indications for revisional surgeries were reflux, diarrhoea and failure of device or ongoing weight management.
Anthropometric Outcomes
The preoperative weight was higher in the OAGB (130.85 ± 19.5) vs. the RYGB (120.5 ± 24.4) cohort (p = 0.049) (Table 1). The mean weight loss (WL) was significant following both procedures compared to pre op. Mean weight and BMI were both significantly different at each time point compared to pre op (Table 2).
Table 2.
Anthropometrical changes of the two cohorts
| Months post op | RYGB (28) | OAGB (45) | p value | |
|---|---|---|---|---|
| Mean WL (kg) | 6/12 | 31.4 ± 16.6 (15) | 36.2 ± 10.9 (32) | 0.321* |
| 12/12 | 31.4 ± 17.7 (16) | 43.1 ± 12.8 (29) | 0.028* | |
| 24/12 |
40.4 ± 19.2 (7) Med 32.4 ± IR 36.6 |
35.2 ± 14.4 (13) Med 32.75 IR 17.35 |
0.546* | |
| Mean %TWL | 6/12 | 25.5 ± 11.3 (15) | 27.9 ± 7.1 (32) | 0.369* |
| 12/12 | 26.6 ± 12.4 (16) | 33.0 ± 8.5 (29) | 0.049* | |
| 24/12 | 34.1 ± 11.2 (7) | 29.0 ± 11.1 (13) | 0.341* | |
| Mean %EWL | 6/12 | 62.8 ± 27.2 (15) | 62.3 ± 16.5 (32) | 0.416* |
| 12/12 | 69.4 ± 28.4 (16) | 71.2 ± 19.7 (29) | 0.828* | |
| 24/12 |
78.7 ± 40.9 (7) Med 88.0 ± IR 56.3 |
69.0 ± 25.8 (13) Med 59.3 ± IR 34.21 |
0.558* 0.336** (38) |
|
| Mean BMI | 6/12 | 31.5 ± 6.5 (15) | 34.0 ± 5.8 (32) | 0.225* |
| 12/12 | 29.2 ± 5.0 (16) | 32.1 ± 5.2 (29) |
0.071* 0.037** (320) |
|
| 24/12 |
27.42 ± 4.3 (7) Med 26.5 ± IR 7 |
69.0 ± 25.8 (13) Med 31.6 ± IR 10 |
0.103* 0.097** (67) |
RYGB Roux-en-y gastric bypass, OAGB one anastomosis gastric bypass, WL weight loss, % TWL % total weight loss, EWL excess weight loss, BMI body mass index, Med median, IR interquartile range
*Independent T test, **Mann-Whitney test
The OAGB cohort achieved a higher weight loss than the RYGB cohort, and the difference in weight loss between the two groups was significant at 12 months following surgery with a %TWL of 26.6 ± 12.4 (43.1 ± 12.8 kg WL) in the OAGB vs. %TWL of 33.0 ± 8.5 (31.4 ± 17.7 kg weight loss) in the RYGB cohort (p = 0.028) (Fig. 1).
Fig. 1.
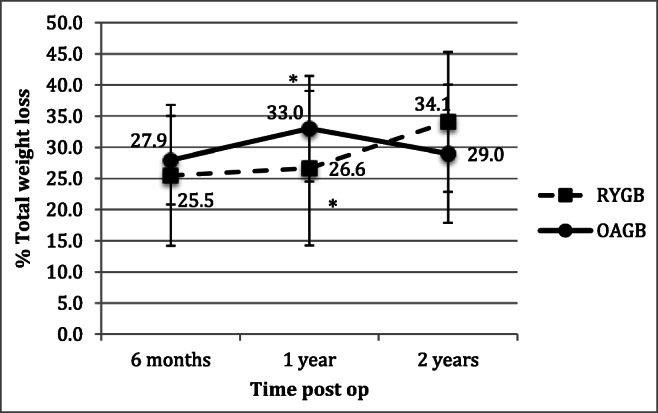
Percentage total weight loss over 2 years following RYGB and OAGB. RYGB, Roux-en-Y gastric bypass; OAGB, one anastomosis gastric bypass. *p = 0.049
Nutritional Outcomes
Preoperative Nutritional Disorders
Preoperative, nutritional disorders were common in both groups. However, a trend for higher disorders in Vitamin D, Hb (females), B12 and protein levels were seen in the RYGB cohort as opposed to more disorders in iPTH, active B12, folate and Hcy in the OAGB cohort (Table 3).
Postoperative Nutritional Disorders
Table 3.
Nutritional disorders in RYGB and OAGB cohorts
| Time | Total | Percentage of disorders | p value§ | ||
|---|---|---|---|---|---|
| RYGB | OAGB | ||||
| iPTH (> 50 pg/ml) | Preoperative | 29.2 (7/24) | 25.0 (2/8) | 31.3 (5/16) | 0.751 |
| 6/12 | 23.3 (7/30) | 27.3 (3/11) | 21.1 (4/19) | 0.698 | |
| 12/12 | 33.3 (9/27) | 25.0 (2/8) | 36.8 (7/19) | 0.551 | |
| 24/12 | 25.0 (5/20) | 0 (0/3) | 29.4 (5/17) | 0.278 | |
| Calcium (< 2.15 mmol/L) | Pre op | 0 (30) | 0 (12) | 0 (18) | - |
| 6/12 | 6.3 (2/32) | 9.1 (1/11) | 4.8 (1/ 21) | 0.631 | |
| 12/12 | 3.0 (1/33) | 0 (13) | 5 (1/20) | 0.413 | |
| 24/12 | 13.8 (4/29) | 0 (7) | 18.2 (4/22) | 0.224 | |
|
Corrected calcium (< 2.15 mmol/L) |
Preoperative | 0 (30) | 0 (12) | 0 (18) | - |
| 6/12 | 3.0 (1/33) | 0 (12) | 4.8 (21) | 0.443 | |
| 12/12 | 0 (33) | 0 (13) | 0 (20) | - | |
| 24/12 | 0 (26) | 0 (6) | 0 (20) | - | |
| Vitamin D (< 50 nmol/L) | Preoperative | 31.9 (15/47) | 40.0 (8/12) | 25.9 (7/27) | 0.306 |
| 6/12 | 21.4 (9/42) | 21.4 (3/14) | 21.4 (6/28) | 1.000 | |
| 12/12 | 30.6 (11/36) | 25.0 (3/12) | 33.3 (8/24) | 0.609 | |
| 24/12 | 25.9 (7/27) | 0 (6) | 33.3 (7/21) | - | |
| Iron (< 5 umol/L) | Preoperative | 11.8 (6/51) | 10 (2/20) | 12.9 (4/31) | 0.753 |
| 6/12 | 11.4 (5/44) | 17.6 (3/17) | 7.4 (2/27) | 0.297 | |
| 12/12 | 15.0 (6/40) | 18.8 (3/16) | 12.5 (3/24) | 0.588 | |
| 24/12 | 9.7 (3/31) | 11.1 (1/9) | 9.1 (2/22) | 0.863 | |
| Ferritin (< 15 ug/L) | Preoperative | 14.8 (8/54) | 15.0 (3/20) | 14.7 (5/34) | 0.977 |
| 6/12 | 11.6 (5/43) | 12.5 (2/16) | 11.1 (3/27) | 0.891 | |
| 12/12 | 22.5 (9/40) | 31.3 (5/16) | 16.7 (4/24) | 0.279 | |
| 24/12 | 30 (9/30) | 33.3 (3/9) | 28.6 (6/21) | 0.794 | |
| Hb (Male) (< 130 g/L) | Preoperative | 0 (15) | 0 (5) | 0 (10) | - |
| 6/12 | 0 (11) | 0 (5) | 0 (10) | - | |
| 12/12 | 16.7 (2/12) | 25.0 (1/4) | 12.5 (1/8) | 0.584 | |
| 24/12 | 12.5 (1/8) | 0 (1) | 14.3 (1/7) | 0.686 | |
| Hb (Female) (< 119 g/L) | Preoperative | 7.5 (3/40) | 13.3 (2/15) | 4.0 (1/25) | 0.278 |
| 6/12 | 15.6 (5/32) | 25.0 (3/12) | 10.0 (2/20) | 0.258 | |
| 12/12 | 10.0 (3/30) | 15.4 (2/13) | 5.9 (1/17) | 0.390 | |
| 24/12 | 4.8 (1/21) | 14.3 (1/7) | 0 (14) | 0.147 | |
| B12 (< 350 pg/ml) | Preoperative | 32.6 (15/46) | 25.7 (4/15) | 35.5 (11/31) | 0.550 |
| 6/12 | 20 (7/35) | 20.0 (2/10) | 20.0 (5/25) | 1.000 | |
| 12/12 | 40 (12/30) | 55.6 (5/9) | 33.3 (7/21) | 0.255 | |
| 24/12 | 42.9 (12/28) | 37.5 (3/8) | 45.0 (9/20) | 0.793 | |
| Active B12(< 35 pmol/L) | Preoperative | 11.8 (4/34) | 7.7 (1/13) | 14.3 (3/21) | 0.562 |
| 6/12 | 0 (33) | 0 (14) | 0 (19) | - | |
| 12/12 | 14.3 (4/28) | 11.1 (1/9) | 15.8 (3/19) | 0.741 | |
| 24/12 | 15.0 (3/20) | 0 (6) | 21.0 (3/14) | 0.147 | |
| Folate (< 7 nmol/L) | Preoperative | 4.4 (2/45) | 0 (19) | 7.7 (2/26) | 0.216 |
| 6/12 | 0 (43) | 0 (16) | 0 (27) | - | |
| 12/12 | 2.6 (1/38) | 0 (12) | 3.8 (1/26) | 0.491 | |
| 24/12 | 0 (24) | 0 (5) | 0 (19) | - | |
| Hcy (14 umol/L) | Preoperative | 8.6 (3/35) | 6.3 (1/16) | 10.5 (2/19) | 0.653 |
| 6/12 | 9.1 (3/33) | 0 (11) | 13.6 (3/22) | 0.199 | |
| 12/12 | 14.8 (4/27) | 12.5 (1/8) | 15.8 (3/19) | 0.826 | |
| 24/12 | 5 (1/20) | 0 (4) | 6.3 (1/16) | 0.608 | |
| Albumin (< 37 g/L) | Preoperative | 0 (56) | 0 (22) | 0 (34) | - |
| 6/12 | 0 (45) | 0 (15) | 0 (13) | - | |
| 12/12 | 4.5 (2/44) | 5.9 (1/17) | 3.7 (1/27) | 0.736 | |
| 24/12 | 2.9 (1/34) | 0 (10) | 4.2 (1/24) | 0.512 | |
| Total protein (< 68g/L) | Preoperative | 12.5 (7/56) | 18.2 (4/22) | 8.8 (3/34) | 0.301 |
| 6/12 | 27.3 (12/44) | 40.0 (6/15) | 20.7 (6/29) | 0.173 | |
| 12/12 | 22.7 (10/44) | 25.0 (4/16) | 21.4 (6/28) | 0.786 | |
| 24/12 | 11.4 (4/35) | 9.1 (1/11) | 12.5 (3/24) | 0.769 | |
| CRP (> 10 mg/L) | Preoperative | 32.0 (15/46) | 15.8 (3/19) | 44.7 (12/27) | 0.041 |
| 6/12 | 19.4 (7/36) | 18.2 (2/11) | 20.0 (5/25) | 0.899 | |
| 12/12 | 6.9 (2/29) | 0 (9) | 10.0 (2/20) | 0.326 | |
| 24/12 | 0 (21) | 0 (4) | 0 (17) | - | |
RYGB Roux-en-Y gastric bypass, OAGB one anastomosis gastric bypass, iPTH parathyroid, Hb haemoglobin, Hcy homocystein, CRP C reactive protein
§Pearson Chi-square; *p < 0.05
Nutritional disorders were common following both procedures, with no significant difference between the two groups. A higher trend in deficiencies of Vitamin D (40% vs. 25.9%), Hb in females (13% vs. 4%) and abnormality in protein levels (18.2% vs. 8.1%) were present in the RYGB group, and in contrast, the OAGB group had more disorders in iPTH (31.3% vs. 25%), active B12 (14.3% vs. 7.7%), folate (7.7% vs. 0) and Hcy (10.5% vs. 6.3%) (Table 3).
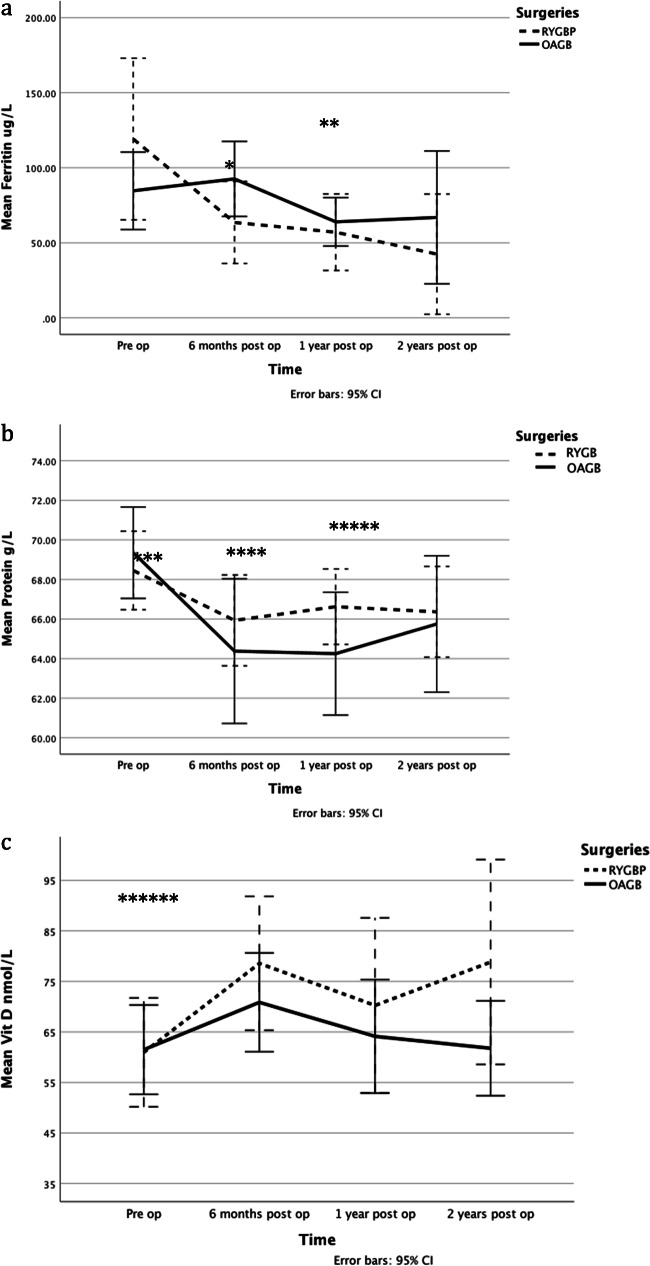
Emergence of Nutritional Disorders Following Surgery
In the group as a whole, over the 2-year periodj, there was a statistical change over time in decreasing mean values of protein (at 6 p = 0.001, 12 p = 0.001 and 24 p = 0.003 months), ferritin (at 12 p = 0.006 and 24 p = 0.008 months), vitamin D (at 6 p = 0.034 and 24 p = 0.066 months). (Fig. 2) Improvements were observed in CRP (at 12 p = 0.006 and 24 p = 0.008 months), insulin (at 24 p = 0.039 months) and FBGL (at 6 p = 0.015, 12 p = 0.000, 24 p = 0.057 and 36 p = 0.057 months). However, no significant change was observed in other nutrition markers.
Fig. 2.
Evolution of nutrient disorders following RYGB and OAGB procedures. a Mean Ferritin levels. b Mean total protein levels. c Mean vitamin D levels. RYGB Roux-en-Y gastric bypass, OAGB one anastomosis gastric bypass. Ferritin: *p: 0.006, **p: 0.008; Protein: ***p: 0.001, ****p: 0.001, *****p: 0.003; Vitamin D: ******p: 0.034, *******p: 0.066
Comparing the two surgical groups, over time, there was no difference or changes in micronutrient status. However, levels of CRP (p = 0.01), ferritin (p = 0.003), vitamin D (p = 0.15) and FBGL (p = 0.001) all changed over time for both groups.
Diet Adequacy
Qualitative diet assessment was available for 58 patients (RYGB n = 20, OAGB n = 38), and overall 62.1% of bariatric patients had an unbalanced diet. This was similar when comparing procedures: 55.0% in the RYGB and 65.8% in the OAGB (p = 0.421 Pearson Chi-square).
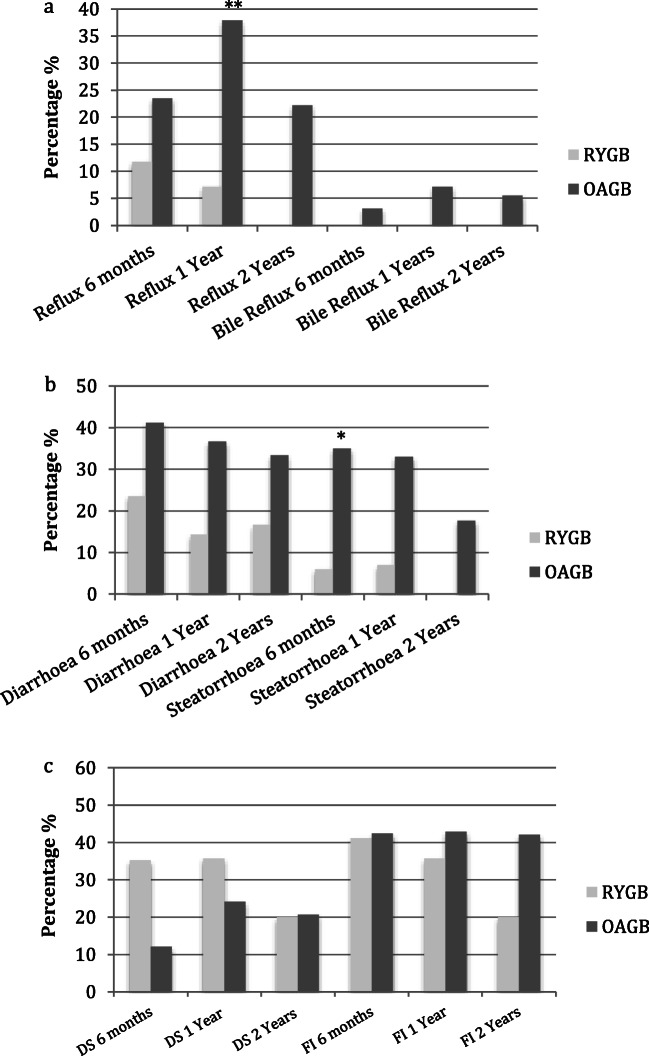
Reported Gastrointestinal (GI) Symptoms
The GI symptoms commonly reported included nausea, vomiting, reflux, diarrhoea, steatorrhoea and food intolerances (Table 4). Constipation was not reported in either group across each time point. The prevalence of nausea, vomiting and diarrhoea tended to be higher in the OAGB cohort than the RYGB group. Nausea and vomiting were predominantly reported in the initial postoperative stages and seemed to resolve over time.
Table 4.
Reported gastrointestinal symptoms following RYGB and OAGB procedures
| Time post op | RYGB % (n) |
OAGB % (n) |
p value§ | |
|---|---|---|---|---|
| Diarrhoea | 6/12 | 23.45 (4) | 41.2 (14) | 0.214 |
| 12/12 | 14.3 (2) | 36.7 (11) | 0.130 | |
| 24/12 | 16.7 (1) | 33.3 (6) | 0.437 | |
| Steatorrhoea | 6/12 | 6.3 (1) | 35.3 (12) | 0.029* |
| 12/12 | 7.1 (1) | 33.3 (10) | 0.062 | |
| 24/12 | (0) | 17.6 (3) | 0.321 | |
| Reflux | 6/12 | 11.8 (2) | 23.5 (8) | 0.318 |
| 12/12 | 7.1 (1) | 37.9 (11) | 0.035* | |
| 24/12 | (0) | 22.2 (4) | 0.246 | |
| Dumping syndrome | 6/12 | 35.3 (6) | 12.1 (4) | 0.052 |
| 12/12 | 35.7 (5) | 24.1 (7) | 0.428 | |
| 24/12 | 20 (1) | 27.8 (5) | 0.612 | |
| Food intolerances | 6/12 | 41.2 (7) | 42.4 (14) | 0.933 |
| 12/12 | 35.7 (5) | 42.9 (12) | 0.657 | |
| 24/12 | 20 (1) | 38.9 (7) | 0.364 |
RYGB Roux-en-Y gastric bypass, OAGB one anastomosis gastric bypass. §Pearson Chi-square. *p < 0.05
Steatorrhoea was reported more in the OAGB than the RYGB cohort and significantly so at 6 months following surgery (p = 0.029*). Reflux was more commonly reported in the OAGB than the RYGB cohort (p = 0.035*). The RYGB cohort tended to have more DS in the initial postoperative year. However, patients in the OAGB also reported experiencing DS.
Regardless of the procedure, over 40% of patients reported some food intolerances at the 6-month postoperative assessment with improvement over time in both groups (Fig. 3).
Fig. 3.
Prevalence and evolution of reported gastrointestinal symptoms following RYGB and OAGB procedures. a Reflux and bile reflux. b Diarrhoea and steatorrhoea. c Dumping syndrome and food intolerances. RYGB Roux-en-Y gastric bypass, OAGB one anastomosis gastric bypass, DS dumping syndrome, FI food intolerances. **p 0.029 *p 0.035
Discussion
Anthropometry
The weight loss achieved following both gastric bypass procedures in this study was significant and consistent with the literature [3, 16, 18, 23, 24]. The weight loss in the OAGB groups was significantly higher at 1 year following surgery at 33.3 %TWL vs. 26.0%TWL, but as also seen in other studies, no difference was found between the two procedures at 2 years [17, 25].
The higher initial weight loss rate in the OAGB cohort is possibly due to its malabsorptive effect as well a higher preop BMI in this group. The literature indicates that the rate of weight loss seems to be dependant on the length of the BPL, in which the longer the BPL, the more malabsorption and hence higher weight loss [18]. Considering that the standard OAGB (BPL of 200 cm) was performed in this cohort, it is reasonable to observe a similar long-term weight loss to that of the RYGB cohort.
Pre op Nutritional Disorders
Preoperative nutritional related disorders were present in both groups with the most common being low levels of vitamins D, B12, elevated iPTH, low ferritin and total protein levels. Our results echo the findings of others, which consistently report on nutritional disorders in the preoperative bariatric surgical patients [3–8].
A large portion of this cohort was seeking both procedures as revisional surgery, and hence the higher level of nutritional disorders seen in this cohort compared to other studies is a consequence of their previous surgery. These surgeries were predominantly LAGB, followed by the sleeve SG, both of which do cause nutritional deficiencies, however, due to different mechanisms [7, 10, 13].
This highlights the nature of the condition of obesity, which may require multiple interventions for its long-term treatment, and hence the need to manage the expected nutritional consequences long term.
Postoperative Nutritional Disorders
The most common nutritional disorders observed in our study following both bypass surgeries were B12, active B12, Hcy, vitamin D, iPTH, iron and ferritin, which is consistent with other findings [3, 4, 8]. We did not find any significant differences in nutritional disorders between the RYGB and the OAGB cohort. To the best of our knowledge, only two other studies have extensively investigated the nutritional consequences of the OAGB [3, 18], and a systematic review by Jia et al. reported the limitation and inconsistencies in the current literature [26].
Robert et al. in a multicentre randomised, non-inferiority trial comparing the RYGB to the OAGB (BPL 200 cm), reported that despite a comparable weight loss and resolution of metabolic disorders, prevalence of adverse events was significantly higher in the OAGB group and 21% of these were nutritional related [18]. Other groups have reported more anaemia (44% vs.17%), hypoalbumanemia (32% vs. 15%) and hypocalcaemia (19% vs. 8%) when comparing OAGB to RYGB [27].
Protein–energy malnutrition has been reported following the OAGB, with some patients having their procedure revised due to its severity [24, 28]. The malabsorptive nature of this procedure has been the contributing factor, compared to the RYGB, and the longer the BPL (300 cm cf 150–200 cm), the more severe the malnutrition [18]. In this cohort, albumin disorders were minimal, and furthermore, no difference was found between the two procedures. In the OAGB cohort, low albumin was seen in only 3.7% at 1 year and 4.2% at 2 years following surgery. Our findings are similar to those of Kessler et al. (3.4%) [3] and a review by Parmar et al. (0–3.8%) [24]. A higher level of abnormalities was seen in total protein levels (21.4% at 1- and 12.5% at 2-year postoperative stage), which is consistent with others; 25.6% at 12–20 months following surgery [3]. No patient required readmission to hospital for enteral or parenteral nutritional support; however, one patient required additional nutrition support in the form of oral high protein supplementation to meet their macronutrient requirements.
Albumin levels below normal values should not be used as the only indicators for malnutrition. Albumin and CRP does fluctuate in states of inflammation, hence cannot solely be used to diagnose malnutrition [29]. We recommend that future studies use a validated malnutrition assessment tool in diagnosing malnutrition.
In this study, folate deficiency was rare both before and after surgery. In contrast, a folate deficiency of 30.9% pre and 11.8% at 12–20 post surgery in 86 OAGB patients have been reported by others [3]. Patients in our cohort as well as others, reported good adherence to the supplementations and hence this difference may be due to the population difference in dietary intake of folate and/or the difference in multivitamin supplement formulation.
Low iron was present in 12% of our OAGB cohort compared to a much higher level of 33.9% by others [3]. Prevalence of iron deficiency anaemia is reported to be 5–10%, with varying treatment modalities, based on the severity and the response to the treatment [23, 24]. In our study, we did not find a difference in Hb levels between the two cohorts. This is contrary to the findings of others of a higher Hb deficiency in the OAGB cohorts (n = 10.0 vs. n = 20.6 p 0.036) [18]. In the OAGB cohort, anaemia was observed in 5.9% (1/17 female) at 1-year post surgery, which is again lower than reported by others at 42.9% [3]. These differences may be related to smaller sample size in our study compared to others and adherence to supplementation in the OAGB group.
Low ferritin levels were observed in 16.7% at 1 and 28.6% at 2 years following OAGB, which is much higher than other studies; 7.8% at 12–20 months post surgery [3]. We did not find a difference between the two procedures in contrast to others [18].
Previous literature has reported vitamin B12 deficiency in 20% of the RYGB patients [8]. The potential causes of this may be bypassing the gastric fundus, the primary site for intrinsic factor production, which aids in B12 complex absorption [5], malabsorption related to common medications (metformin and proton pump inhibitors) as well as dietary restrictions induced by the surgery, which may result in food intolerances and suboptimal protein intake in longer term [30]. Hence supplementation and ongoing monitoring is required.
Low vitamin B12 levels (< 350 pg/ml or < 250 pmol/L) was observed in 33.3% at 12 months and 45.0% at 24 months following the OAGB, which was much higher than reported by others at 28.4% [3]. Similarly, to others, no difference was seen between the procedures [18].
Serum B12 may not be adequate to identify metabolic deficiencies of vitamin B12 [5] and hence active B12 level and Hcy were also measured. We observed lower disorder levels of 15.8% at 12 months and 21.0% at 24 months post OAGB compared to the literature and no difference in between the groups. This might be population related, with higher individual B12 stores, or related to a more comprehensive multivitamin formula and/or better adherence to the recommended supplementations.
Metabolic bone health is one area that is still under investigation and data on best management continues to emerge. Prior to and post bariatric procedures, Vitamin D and iPTH deficiencies are common and need close attention long term [5]. There are limited studies reporting on these nutrients post OAGB [3, 18], while a reduction in bone mass has reported [31]. In our study, disorders in vitamin D and iPTH were observed following both procedures. Vitamin D deficiency in this OAGB cohort was 25.9%, which is lower than reported by others (54.7% at 12–20 months post surgery) [3]. The RYGB group had a higher level of vitamin D deficiency (40% vs. 25.9%), while the OAGB impacted on iPTH more (31.3% vs. 25%). This could be due to the larger cohort of patients seeking RYGB as revisional surgery following a sleeve gastrectomy and hence carrying through the nutritional impact of their primary procedure.
To the best of our knowledge, no other studies have investigated the change over time of the levels of nutrients in the postoperative phase following OAGB. However, some studies have aspects of these issues e.g. Kessler et. al. [3] and Syn et. al. [32]. In this study, both groups, over the 2-year period showed a significant reduction in mean values of protein, ferritin and vitamin D, however an improvement in mean values of CRP, insulin and FBGL. However, no significant change was observed in other nutrition markers. Furthermore, we did not observe a difference when comparing the two surgical groups.
Diet Adequacy
The qualitative dietary assessment revealed an unbalanced diet in 62% of all patients in this cohort with no difference between the RYGB vs. the OAGB group. Changes in dietary intake and lifestyle long term are essential for optimal surgical outcome, and ongoing counselling and support need to be provided through a multidisciplinary approach [33]. The limited studies reporting on dietary intake beyond the 1-year post show a lower intake of protein, higher intake of fats and carbohydrates [30]. Further and more robust dietary assessment studies, to investigate the nutritional intake of this cohort, are necessitated.
Reported Gastrointestinal (GI) Symptoms
We identified the common gastrointestinal symptoms to be nausea, vomiting, reflux, diarrhoea, steatorrhoea and food intolerances, with some symptoms more prevalent in the OAGB cohort due to its anatomical configuration and malabsorptive effect.
Consistent with findings of others [3, 18, 23], steatorrhoea and diarrhoea were more common in the OAGB than the RYGB cohort. Robert et al. compared the RYGB and the OAGB bypass, and at 2-year post op, diarrhoea and related nutritional complications were exclusively found in the OAGB group with 4 (10%) patients requiring revisional surgery. The longer BPL in the OAGB compared to the RYGB has been thought to be the main contributor, resulting in reduced absorptive mucosal surface, reduced activity of pancreatic and enteric enzymes, lactase deficiency, small intestinal bacterial over-growth and irritable bowel symptoms due to undigested carbohydrates [3, 34].
Reflux was also more common in the OAGB cohort and significantly so at 1-year post op, and bile reflux was reported in 2 patients in the OAGB and none in the RYGB cohort. Reflux and in particular bile reflux are some of main concerns of this procedure and further studies have been recommended [16, 23].
Following bariatric surgery, DS occurs as a result of the alterations to the gastric motor function as well as its physiology [22, 35]. The reduction in the gastric capacity and the rapid introduction of energy-dense nutrients to the small bowel exert local osmotic effect and delayed hypoglycemia. Consumption of simple sugars, high-fat foods and in general energy dense foods can result in DS. This is exacerbated when these items are consumed rapidly and in large volumes. The symptoms of DS are varied in each case but do include abdominal pain, nausea, epigastric fullness, dizziness, flushing, dyspnea, tachycardia, apathy, weakness and syncope [35]. This study reports DS to be more common in the RYGB cohort; however, the OAGB patients too experience this [18]. There is limited literature investigating DS following OAGB but there is the assumption that early DS is less common; however, there is no consensus when comparing the two procedures for the frequency of late DS [36]. In both procedures, the gastrojejunostomy can result in the rapid transfer of hyperosmolar food from the gastric pouch into the jejunum; however, this may more rapid in case of the RYGB due to the smaller pouch and hence may explain the higher rate of early DS in this cohort.
The anatomical and physiological alterations of the gastrointestinal system following gastric bypass surgery lead to expected changes in food tolerance. The symptoms are more significant in the early stages and improve with time [37]. In this study, regardless of the procedure, over 40% of patients reported some food intolerances in the early stages with improvements over time, and there was no difference between the groups. Consistent with our findings, studies using a validated questionnaire have found an improvement in diet tolerance over time, with some reporting good or excellent satisfaction with quality of alimentation by over 79% of patients [3, 12, 38]. However, poor tolerance to red meat does persist and contribute to nutritional deficiencies [38].
Poor diet tolerance, significant gastrointestinal symptoms and malnutrition, have been the main reasons for revising an OAGB. In the YOMEGA study by Robert et al., 4 patients (10%) had their OAGB converted to a RYGB due to gastrointestinal or nutritional complications [18]. In this study, only one patient had their OAGB converted to a RYGB. However, poor adherence to dietary recommendations and high consumption of energy dense foods on the background of poor psychological health also contributed to this.
The limitations of our study were primarily due to the retrospective nature of the study, with reliance on reported data as well as missing data. Secondly, the patients were not randomly allocated to each surgical group, and a large number had the bypass procedure as a revisional surgery. Thirdly, a small sample size, partly due to loss-to-follow-up as reported in the literature for this cohort, and partly due to COVID 19 and its restrictions, imposed on clinics and patients movements. Finally, as the majority of both bypass cohorts have had revisional surgery, there is a likelihood that some the nutritional and/or gastrointestinal consequences may be attributed to their primary procedure. Notwithstanding, the RYGB cohort reported less overall symptoms despite more patients undertaking it as a revisional procedure than that of the OAGB.
However, with limited studies published on nutrition status following the OAGB, we feel that this study presents a realistic observation of non-research funded, private bariatric clinics and hence encourages others to reflect on clinical practice.
Conclusion
Significant but similar weight loss is seen following both OAGB and RYGB. However, the OAGB patients experience more gastrointestinal side effects, which may contribute to poor quality of life and nutritional consequences. The nutritional deficiencies were common in this cohort and increased over time. To further investigate the nutritional and gastrointestinal health of the OAGB, the authors call for future prospective studies, with more comprehensive biochemical data, longer term follow-up and a superior follow up rate of this new procedure.
Acknowledgements
The authors would like to gratefully acknowledge the assistance of A/Prof. Garrett Smith and Dr. Steve Leibman for permission to recruit subjects and the staff at Shore Surgical for their administrative support.
Declarations
Ethics Approval
Ethics approval was granted and for this type of study formal informed consent is not required.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Key Points
•OAGB has a similar weight loss outcome to the RYGB
•Nutritional disorders are common prior to and following both procedures
•The OAGB patients report more gastrointestinal symptoms
•Long-term studies investigating the nutritional and gastrointestinal outcomes following OAGB are recommended
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nazy Zarshenas, Email: nazy.nutrition@gmail.com.
Linda Clare Tapsell, Email: ltapsell@uow.edu.au.
Marijka Batterham, Email: marijka@uow.edu.au.
Elizabeth Phillipa Neale, Email: elizan@uow.edu.au.
Michael Leonard Talbot, Email: MichaelT@uppergisurgery.com.au.
References
- 1.Sumithran P, Proietto J. The defence of body weight: a physiological basis for weight regain after weight loss. Clin Sci. 2013;124:231–241. doi: 10.1042/CS20120223. [DOI] [PubMed] [Google Scholar]
- 2.Sjostrom L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–2693. doi: 10.1056/NEJMoa035622. [DOI] [PubMed] [Google Scholar]
- 3.Kessler Y, Adelson D, Mardy-Tilbor L, Ben-Porat T, Szold A, Goitein D, et al. Nutritional status following one anastomosis gastric bypass. Clin Nutr (Edinburgh, Scotland) 2020;39(2):599–605. doi: 10.1016/j.clnu.2019.03.008. [DOI] [PubMed] [Google Scholar]
- 4.Aills L, Blankenship J, Buffington C, Furtado M. Bariatric nutrition: suggestions for the surgical weight loss patient. Surg Obes Relat Dis. 2008;4(5):S73–S108. doi: 10.1016/j.soard.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 5.O’Kane M, Parretti HM, Pinkney J, Welbourn R, Hughes CA, Mok J, et al. British Obesity and Metabolic Surgery Society Guidelines on perioperative and postoperative biochemical monitoring and micronutrient replacement for patients undergoing bariatric surgery—2020 update. Obes Rev. 2020;21:1–23. doi: 10.1111/obr.13087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Toh SY, Zarshenas N, Jorgensen JO. Prevalence of nutrient deficiencies in bariatric patients. Nutrition (Burbank, Los Angeles County, Calif) 2009;25(11-12):1150–1156. doi: 10.1016/j.nut.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 7.Zarshenas N, Nacher M, Loi KW, Jorgensen JO. Investigating nutritional deficiencies in a group of patients 3 years post laparoscopic sleeve gastrectomy. Obes Surg. 2016;26(12):2936–2943. doi: 10.1007/s11695-016-2211-3. [DOI] [PubMed] [Google Scholar]
- 8.Parrott J, Frank L, Rabena R, Craggs-Dino L, Isom KA. American Society for Metabolic and Bariatric Surgery Integrated Health Nutritional Guidelines for the Surgical Weight Loss Patient. Surg Obes Relat Dis. 2016;13:727–741. doi: 10.1016/j.soard.2016.12.018. [DOI] [PubMed] [Google Scholar]
- 9.Mechanick JI, Apovian C, Brethauer S, Garvey WT, Joffe AM, Kim J, et al. Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures - 2019 update: cosponsored by American Association of Clinical Endocrinologists/American college of Endocrinology, The Obesity Society, American Society for Metabolic & Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists - Executive Summary. Endocr Pract. 2019;25(12):1346–1359. doi: 10.4158/gl-2019-0406. [DOI] [PubMed] [Google Scholar]
- 10.McGrice MA, Porter JA. The micronutrient intake profile of a multicentre cohort of Australian LAGB patients. Obes Surg. 2014;24(3):400–404. doi: 10.1007/s11695-013-1101-1. [DOI] [PubMed] [Google Scholar]
- 11.McGrice MA, Porter JA. What are gastric banding patients eating one year post-surgery? Obes Surg. 2012;22(12):1855–1858. doi: 10.1007/s11695-012-0741-x. [DOI] [PubMed] [Google Scholar]
- 12.Freeman RA, Overs SE, Zarshenas N, Walton KL, Jorgensen JO. Food tolerance and diet quality following adjustable gastric banding, sleeve gastrectomy and Roux-en-Y gastric bypass. Obes Res Clin Pract. 2014;8(2):e115–e200. doi: 10.1016/j.orcp.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 13.Van Rutte PJW, Aarts EO, Smulders JF, Nienhuijs SW. Nutrient deficiencies before and after sleeve gastrectomy. Obes Surg. 2014;24(10):1639–1646. doi: 10.1007/s11695-014-1225-y. [DOI] [PubMed] [Google Scholar]
- 14.DeMaria EJ, Pate V, Warthen M, Winegar DA. Baseline data from American Society for Metabolic and Bariatric Surgery-designated Bariatric Surgery Centers of Excellence using the bariatric outcomes longitudinal database. Surg Obes Relat Dis. 2010;6:347–355. doi: 10.1016/j.soard.2009.11.015. [DOI] [PubMed] [Google Scholar]
- 15.De Luca M, Tie T, Ooi G, Higa K, Himpens J, Carbajo MA, et al. Mini gastric bypass-one anastomosis gastric bypass (MGB-OAGB)-IFSO position statement. Obes Surg. 2018;28:1188–1206. doi: 10.1007/s11695-018-3182-3. [DOI] [PubMed] [Google Scholar]
- 16.Parikh M, Eisenberg D, Johnson J, El-Chaar M. American Society for Metabolic and Bariatric Surgery review of the literature on one-anastomosis gastric bypass. Surg Obes Relat Dis. 2018;14:1088–1092. doi: 10.1016/j.soard.2018.04.017. [DOI] [PubMed] [Google Scholar]
- 17.Lee WJ, Yu PJ, Wang W, Chen TC, Wei PL, Huang MT. Laparoscopic Roux-en-Y versus mini-gastric bypass for the treatment of morbid obesity: a prospective randomized controlled clinical trial. Ann Surg. 2005;242(1):20–28. doi: 10.1097/01.sla.0000167762.46568.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robert M, Espalieu P, Pelascini E, Caiazzo R, Sterkers A, Khamphommala L, et al. Efficacy and safety of one anastomosis gastric bypass versus Roux-en-Y gastric bypass for obesity (YOMEGA): a multicentre, randomised, open-label, non-inferiority trial. Lancet (London, England) 2019;393(10178):1299–1309. doi: 10.1016/s0140-6736(19)30475-1. [DOI] [PubMed] [Google Scholar]
- 19.Poghosyan T, Caille C, Moszkowicz D, Hanachi M, Carette C, Bouillot J-L. Roux-en-Y gastric bypass for the treatment of severe complications after omega-loop gastric bypass. Surg Obes Relat Dis. 2017;13(6):988–994. doi: 10.1016/j.soard.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 20.Mechanick JI, Youdim A, Jones DB, Garvey WT, Hurley DL, McMahon MM, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient--2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Endocr Pract. 2013;19(2):337–372. doi: 10.4158/ep12437.Gl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stabler S. Clinical practice. Vitamin B12 deficiency. N Engl J Med. 2013;368:149–160. doi: 10.1056/NEJMcp1113996. [DOI] [PubMed] [Google Scholar]
- 22.Moizé V, Pi-Sunyer X, Mochari H, Vidal J. Nutritional pyramid for post-gastric bypass patients. Obes Surg. 2010;20:1133–1141. doi: 10.1007/s11695-010-0160-9. [DOI] [PubMed] [Google Scholar]
- 23.Aleman R, Lo Menzo E, Szomstein S, Rosenthal R. Efficiency and risks of one-anastomosis gastric bypass. 2020; p. 7. [DOI] [PMC free article] [PubMed]
- 24.Parmar CD, Mahawar KK. One anastomosis (Mini) gastric bypass is now an established bariatric procedure: a systematic review of 12,807 patients. Obes Surg. 2018;28(9):2956–2967. doi: 10.1007/s11695-018-3382-x. [DOI] [PubMed] [Google Scholar]
- 25.Lee WJ, Ser KH, Lee YC, Tsou JJ, Chen SH, Chen JC. Laparoscopic Roux-en-Y vs. mini-gastric Bbypass for the treatment of morbid obesity: a 10-year experience. Obes Surg. 2012;22:1827–1834. doi: 10.1007/s11695-012-0726-9. [DOI] [PubMed] [Google Scholar]
- 26.Jia D, Tan H, Fang F, Faramand A. One anastomosis gastric bypass versus Roux-en-Y gastric bypass for obesity: a Ssystematic review and meta-analysis of randomized clinical trials. Obes Surg. 2020;30(4):1211–1218. doi: 10.1007/s11695-019-04288-3.2-52.0-85075290841. [DOI] [PubMed] [Google Scholar]
- 27.Bhandari M, Nautiya H, Kosta S, Mathur W, Fobi M. Comparison of one-anastomosis gastric bypass and Roux-en-Y gastric bypass for treatment of obesity: a 5-year study. Surg Obes Relat Dis. 2019;15(12):2038–2044. doi: 10.1016/j.soard.2019.05.025. [DOI] [PubMed] [Google Scholar]
- 28.Hussain A, Van den Bossche M, Kerriganc DD, Alhamdanid A, Parmard C, Javedc S, et al. Retrospective cohort study of 925 OAGB procedures. The UK MGB/OAGB T collaborative group. Int J Surg. 2019;69:13–18. doi: 10.1016/j.ijsu.2019.07.003. [DOI] [PubMed] [Google Scholar]
- 29.Baron M, Hudson M, Steele R. (CSRG) tCSRG. Is serum albumin a marker of malnutrition in Chronic Disease? The Scleroderma Paradigm. J Am Coll Nutr. 2010;29(2):144–151. doi: 10.1080/07315724.2010.10719828. [DOI] [PubMed] [Google Scholar]
- 30.Zarshenas N, Tapsell LC, Neale EP, Batterham M, Talbot ML. The relationship between bariatric surgery and diet quality: a systematic review. Obes Surg. 2020;30:1768–1792. doi: 10.1007/s11695-020-04392-9. [DOI] [PubMed] [Google Scholar]
- 31.Luger M, Kruschitz R, Winzer E, Schindler K, Grabovac I, Kainberger F, Krebs M, Hoppichler F, Langer F, Prager G, Marculescu R, Ludvik B. Changes in bone mineral density following weight loss induced by one-anastomosis gastric bypass in patients with Vitamin D Supplementation. Obes Surg. 2018;28(11):3454–3465. doi: 10.1007/s11695-018-3353-2. [DOI] [PubMed] [Google Scholar]
- 32.Syn N, Lee P, Kovalik J, Tham K, Ong H, Chan W, et al. Associations of bariatric interventions with micronutrient and endocrine disturbances. JAMA Netw Open. 2020;1:3(6). doi: 10.1001/jamanetworkopen.2020.5123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sherf Dagan S, Keidar A, Raziel A, Sakran N, Goitein D, Shibolet O, Zelber-Sagi S. Do bariatric patients follow dietary and lifestyle recommendations during the first postoperative year? Obes Surg. 2017;27(9):2258–2271. doi: 10.1007/s11695-017-2633-6. [DOI] [PubMed] [Google Scholar]
- 34.Hussain A, EL-Hasani S. Short- and mid-term outcomes of 527 one anastomosis gastric bypass/mini-gastric bypass (OAGB/MGB) operations: retrospective study. Obes Surg. 2019;29:262–267. doi: 10.1007/s11695-018-3516-1. [DOI] [PubMed] [Google Scholar]
- 35.Handzlik-Orlik G, Holecki M, Orlik B, Wyleżoł M, Duława J. Nutrition management of the post–bariatric surgery patient. Nutr Clin Pract. 2015;30(3):383–392. doi: 10.1177/0884533614564995. [DOI] [PubMed] [Google Scholar]
- 36.Ramos AC, Chevallier J-M, Mahawar K, Brown W, Kow L, White KP, et al. IFSO (International Federation for Surgery of Obesity and Metabolic Disorders) Consensus Conference Statement on One-Anastomosis Gastric Bypass (OAGB-MGB): results of a modified Delphi study. 2020. p. 1625-34. [DOI] [PubMed]
- 37.Suter M, Calmes JM, Paroz A, Giusti V. A new questionnaire for quick assessment of food tolerance after bariatric surgery. Obes Surg. 2007;17:2–8. doi: 10.1007/s11695-007-9016-3. [DOI] [PubMed] [Google Scholar]
- 38.Cano-Valderrama O, Sanchez-Pernaute A, Rubio-Herrera MA, Dominguez-Serrano I, Torres-Garcia AJ. Long-term food tolerance after bariatric surgery: comparison of three different surgical techniques. Obes Surg. 2017;27(11):2868–2872. doi: 10.1007/s11695-017-2703-9. [DOI] [PubMed] [Google Scholar]