Abstract
Objective
Individuals with chronic pain are uniquely challenged by the COVID-19 pandemic, as increased stress may exacerbate chronic pain, and there are new barriers to receiving chronic pain treatment. In light of this, using a large online sample in the United States, we examined 1) the early impact of COVID-19 on pain severity, pain interference, and chronic pain management; and 2) variables associated with perceived changes in pain severity and pain interference.
Design
A cross-sectional study.
Methods
Online survey data for 1,453 adults with chronic pain were collected via Amazon’s Mechanical Turk platform.
Results
Although a large proportion of participants reported no perceived changes in their pain severity and pain interference since the outbreak, approximately 25–30% of individuals reported exacerbation in these domains. Individuals identifying as Black and of non-Hispanic origin, who experienced greater disruptions in their mood and sleep quality, were more likely to report worsened pain interference. The majority of participants reported engaging in self-management strategies as usual. However, most appointments for chronic pain treatment were either postponed or canceled, with no future session scheduled. Furthermore, a notable proportion of participants had concerns about or difficulty accessing prescription opioids due to COVID-19.
Conclusions
We may expect to see a long-term exacerbation of chronic pain and related interference in functioning and chronic pain management among individuals most impacted by the pandemic. These individuals may benefit from remotely delivered intervention to effectively mitigate COVID-19–related exacerbations in chronic pain and interruptions in face-to-face treatment.
Keywords: COVID-19, Coronavirus, Chronic Pain, Pain Management, Disparities, Opioids
Introduction
Novel coronavirus (COVID-19) has spread to almost every corner of the world, infecting millions of people, leaving billions under home confinement, and contributing to a significant increase in psychosocial distress [1]. As many as 100 million individuals in the United States suffer from chronic pain, and this population may be negatively affected by the pandemic. As it is well documented that pain increases in response to stressors [2, 3], pandemic-related stress may exacerbate pain and decrease functioning among individuals with chronic pain [4]. Furthermore, individuals with chronic pain may have substantially reduced access to their treatments, as facilities close or transition to new models of delivery [5]. To better identify current and future needs of such individuals during this pandemic, it is imperative to understand the impact of COVID-19 on pain intensity, pain interference, and chronic pain management.
The impact of COVID-19 on pain severity and pain interference is likely to vary across individuals. Recent reports suggest that COVID-19 disproportionately affects racial and ethnic minorities and individuals with low socioeconomic status [6–8]. These demographic subgroups are also likely to experience greater pain and disability [9–14]. Individuals with chronic pain from these subgroups may be more susceptible to having COVID-19 negatively impact their pain experiences. Other biopsychosocial factors that may also exacerbate pain severity and pain interference include worsened mood, sleep quality, and social support, which have been frequently reported by the general population during the pandemic [15, 16] and are some of the key factors that can modulate a person’s pain-related experience [17–19]. To our knowledge, however, no studies to date have examined the impact of sociodemographic characteristics, mood, sleep quality, and social support on worsened pain severity and pain interference in the context of COVID-19.
Chronic pain management, including the self-management of pain and medical and pharmacological treatments, is likely to be disrupted during the pandemic [5]. Significant lifestyle changes, such as increased caregiving needs and financial strain, may pose barriers to self-management strategies, such as exercise or meditation practices. Chronic pain treatment facilities are also being closed or transitioned to new models of delivery to prioritize resources to meet the current acute need of preventing and treating COVID-19 [5]. These changes are reducing access to face-to-face chronic pain treatments. Other factors, such as loss of or changes in insurance, may pose additional barriers to seeking chronic pain treatment. Nevertheless, the impact of COVID-19 on chronic pain management is unknown.
The present study aimed to elucidate the early impact of the COVID-19 pandemic on chronic pain and its management by examining cross-sectional survey responses from a large online sample. First, we examined the impact of the outbreak on perceived changes in pain severity and pain interference. Second, we explored whether select demographic factors and changes in mood, sleep quality, and social support are associated with greater COVID-19 impact on pain severity and pain interference. Lastly, we investigated the COVID-19 impact on various domains of chronic pain management, including engagement in self-management practice, appointments for chronic pain treatments, and access to prescribed opioids.
Methods
The present study is part of a larger study characterizing individual differences in emotional regulation and their association with pain and mood-related outcomes among individuals with chronic pain. To date, no study using this parent data has been published. The primary aims of the present study focus on the impact of COVID-19 on chronic pain and its management and, therefore, do not overlap with those of the parent study.
Participants
Participants were recruited between April 22, 2020, and May 15, 2020, from Amazon Mechanical Turk (MTurk), a crowdsourcing website. A third party, Cloud Research, was used to recruit MTurk “workers” to respond to a Human Intelligence Task (HIT) advertisement for our survey titled “demographic background, thoughts, feelings, and physical and mental health symptoms.” MTurk provides access to large and demographically diverse samples, and studies suggest that MTurk responses have overall good validity and reliability [20, 21]. MTurk has also been used to collect data from large samples of individuals with chronic pain in previous studies [22, 23]. We aimed to achieve a sample representative of the online chronic pain population in the United States in terms of gender, race, and ethnicity, based on findings from Johannes and his colleagues [24]. Demographic rates were monitored during data collection, and Black/African American race, Hispanic ethnicity, and women were oversampled to achieve rates similar to those found by Johannes and colleagues [24].
An initial screening question was embedded into ongoing MTurk surveys: “Have you had pain most days (more than half) over the past 3 months?” MTurk workers who responded affirmatively to this question were invited to complete an additional screener to determine eligibility. Specifically, this screener assessed whether the individual resided in the United States, assessed whether the individual was willing to be recontacted for a future study, and gathered additional information about pain. With regard to pain assessment, participants completed select items from the Brief Pain Inventory (BPI [25]) to determine the presence of pain (item #1 from BPI) and pain severity (items #3–6 in BPI). Because of potential delays between initial screening and completion of the survey battery, participants were asked once again to indicate whether they had had pain for most days over the previous 3 months.
Inclusion criteria included: 1) age 18 years or more, 2) additional chronic pain criteria (i.e., experience of pain in the past week and average past week pain severity of 3/10 as per the BPI [25], 3) residence in the United States, 4) proficiency in English, and 5) willingness to participate in follow-up data collection approximately 12 weeks in the future. In addition, to maximize the overall quality and reliability of survey responses, only workers with a minimum approval rating of 95% from other MTurk “requesters” (those who post studies like us) were invited to participate in the full survey.
A total of 30,096 MTurk workers responded to the initial screening question. Of these, 10,308 (34.3%) responded affirmatively, indicating the presence of chronic pain; these MTurk workers were invited to complete the additional eligibility screener. Of these, 2,153 (20.9%) who completed the screener were deemed eligible. Of the 2,153 eligible to participate in the full study, 1,809 (84.0%) initiated the survey. To ensure the validity of participants’ responses, we excluded data from participants who 1) took substantially more than (>60 minutes) or less than (<16 minutes) the average survey duration (i.e., 35 minutes) to complete the survey, and 2) those who provided inaccurate responses to three embedded attention check items (e.g., “Please select Never True”). A total of 325 participants (18%) were excluded on the basis of these criteria. We also found 31 cases that had duplicate IDs; these cases were excluded from the dataset. As a result, the final sample size of the present study was 1,453.
Procedures
MTurk workers who were eligible for participation on the basis of the initial screening survey received an online link to a study that included self-report questionnaire batteries. Respondents were compensated $5 for their participation. All study procedures were approved by the Johns Hopkins University School of Medicine Institutional Review Board.
Measures
Change in employment status. With a binary (yes/no) question (i.e., have you experienced changes in employment status related to the coronavirus outbreak [for example: job loss, laid off, furloughed, reduction in work hours, etc.]?), participants were asked whether they had experienced any changes in employment status related to the coronavirus outbreak.
Perceived changes in pain severity, pain interference, mood, sleep quality, and social support after the COVID-19 outbreak. We assessed perceived changes in pain severity, pain interference, mood, sleep quality, and social support by adapting items from the previously validated Patient Global Impression of Change (PGIC) measure, which is frequently used as an indicator of meaningful change in pain-related experiences [26, 27]. Respondents described perceived changes in pain severity, pain’s interference with their day-to-day activities, mood, sleep quality, and social support since the start of the COVID-19 outbreak, using the following seven-point Likert scale: 1) “very much improved,” 2) “much improved,” 3) “minimally improved,” 4) “no change,” 5) “minimally worse,” 6) “much worse,” and 7) “very much worse.” Cronbach’s alpha was not calculated because these were single-item scales.
Impact of COVID-19 on engaging in self-management of chronic pain. Respondents indicated how the coronavirus outbreak had impacted their chronic pain management at home (e.g., yoga, meditation, tai chi, exercise) on the following categorical scale: 1 = “no longer practicing home,” 2 = “practicing at home less than usual,” 3 = “practicing at home more than usual,” 4 = “no impact—practicing at home the same as usual,” and 5 = “others.”
Impact of COVID-19 on chronic pain treatment appointments. Respondents indicated how the COVID-19 outbreak had impacted their chronic pain treatment appointments, including 1) mental health treatment (e.g., counseling, therapy) for chronic pain, 2) physical therapy, 3) complementary medical treatments (e.g., massage, acupuncture, chiropractic care), and 4) other medical treatments (e.g., injections, spinal cord stimulation). The categorical scale that was used to evaluate impact for these pain treatments included: 1 = “appointments canceled with no future sessions scheduled,” 2 = “appointments postponed,” 3 = “appointments changed to telehealth (sessions delivered via video or phone),” 4 = “no impact,” and 5 = “other impact.” For these items, participants were permitted to select more than one response, as their ongoing chronic pain treatment may have been rapidly impacted in multiple ways during the COVID-19 pandemic.
Impact of COVID-19 on access to prescription opioids. Respondents also indicated how the COVID-19 outbreak had impacted their access to prescription opioids. The categorical scale that was used to evaluate the impact of these treatments included: 1 = “I have limited access to prescription opioid medication,” 2 = “I have access now but am concerned about access in the future,” 3 = “no impact on my opioid medication prescribed for pain,” and 4 = “other impact.”
Power Analysis
We calculated the sensitivity to detect an effect based upon the sample size. According to the G*Power calculation, a sample of 1,453 with an alpha level at 0.05 (two-tailed) can produce a statistical power of 0.80 to detect very small effects (Cohen’s d = 0.01) using multiple regression analysis.
Data Analytic Strategy
To summarize the characteristics of the current sample, descriptive statistics were computed for sociodemographics, duration of chronic pain, the number of people who tested positive for COVID-19, and the number of people whose employment status changed because of COVID-19. Perceived changes in pain severity, pain interference, mood, sleep quality, and social support due to COVID-19 were first presented descriptively in a frequency table. We then used standard multiple regression to determine whether select sociodemographic factors (i.e., age, gender, race, ethnicity, education level, income level, and change in employment status due to the outbreak) and self-reported impact of COVID-19 on mood, sleep quality, and social support were associated with perceived changes in pain severity and pain interference. We entered these variables into the model simultaneously. Hierarchical multiple regression was not used, as we did not have any a priori hypothesis that certain variables should be considered as covariates or are theoretically the most important predictors of the outcomes. Stepwise multiple regression (e.g., forward, backward, and stepwise selection) was also not used, as this approach can cause biases in model parameters, model overfitting, and inflation of Type I errors by multiple testing [28]. Before multiple regression was conducted, the categorical race variable was categorized to 1) Asian, 2) Black/African American, 3) White, 4) Mixed-Race, and 5) Other Race. As numerous studies suggest significant pain disparities among individuals who are Black/African American [11, 12], we designated Black/African American as the reference group for racial group comparisons. In terms of gender, we focused on the gender binary (male vs. female) in the regression analysis, as a very small proportion (0.5%) of individuals reported that they fall under the nonbinary/genderqueer category. Lastly, the impact of COVID-19 on chronic pain management was visually summarized by using bar charts.
Results
Sample Characteristics
Table 1 provides a detailed summary of the demographic characteristics of the study sample. The breakdown of race, ethnicity, and gender in the present sample was similar to that of the representative chronic pain population reported by Johannes and colleagues [24]. The participants’ mean age was 41.7 years (standard deviation = 13.1), and the majority of participants were female, were White, had at least some college education, and were currently working either part or full time. Most participants had an income greater than $24,999 and were married. A total of 62 participants reported that they had been tested for COVID-19. Among them, 9 (14.5%) reported having a positive result, 52 (83.9%) reported having a negative result, and 1 (1.6%) reported not yet knowing the result of their test. Nearly half (42.7%) of the sample endorsed a change in employment status due to COVID-19.
Table 1.
Demographic characteristics of the sample
| Demographic Variables | Mean ± SD) or n (%) |
|---|---|
| Age, years | 41.7±13.1 |
| Chronic pain duration, years | 10.9±9.1 |
| Gender | |
| Female | 968 (65.2) |
| Male | 498 (34.3) |
| Other (nonbinary/genderqueer) | 7 (0.5) |
| Race | |
| White | 1,189 (81.9) |
| Black/African American | 99 (6.8) |
| Asian/Asian American | 50 (3.4) |
| American Indian/Alaska Native | 13 (0.9) |
| Native Hawaiian/Pacific Islander | 0 (0) |
| Mixed Race | 67 (4.6) |
| Other Race | 28 (1.9) |
| Prefer not to answer | 5 (0.3) |
| Don’t know | 1 (0.1) |
| Ethnicity | |
| Hispanic | 144 (9.9) |
| Non-Hispanic | 1,297 (89.4) |
| Prefer not to answer | 7 (0.5) |
| Don’t know | 3 (0.2) |
| Education | |
| Less than high school graduate | 9 (0.6) |
| GED or high school graduate | 168 (11.6) |
| Some college, no degree | 402 (27.7) |
| Associate’s degree (2-year degree) | 224 (15.4) |
| Bachelor’s degree/college degree | 399 (27.5) |
| Above college education | 250 (17.2) |
| Prefer not to answer | 1 (0.1) |
| Employment status | |
| Working full time | 694 (47.8) |
| Working part time | 209 (14.4) |
| Unemployed or laid off | 176 (12.1) |
| Looking for work | 49 (3.4) |
| Keeping house or raising children full time | 110 (7.6) |
| Retired | 103 (7.1) |
| Other | 112 (7.7) |
| Income | |
| Less than $5,000 | 45 (3.1) |
| $5,000–$11,999 | 67 (4.6) |
| $12,000–$15,999 | 54 (3.7) |
| $16,000–$24,999 | 148 (10.2) |
| $25,000–$34,999 | 211 (14.5) |
| $35,000–$49,999 | 224 (15.4) |
| $50,000–$74,999 | 310 (21.3) |
| $75,000–$99,999 | 177 (12.2) |
| $100,000 and greater | 201 (13.8) |
| Prefer not to answer | 8 (0.5) |
| Don’t know | 7 (0.5) |
| Marital status | |
| Married | 663 (45.7) |
| Divorced | 198 (13.6) |
| Separated | 29 (2.0) |
| Widowed | 32 (2.2) |
| Single | 517 (35.6) |
| Prefer not to answer | 13 (0.9) |
| Changes in employment status due to COVID-19 | |
| Yes | 620 (42.7) |
The Impact of COVID-19 Outbreak on Perceived Changes in Pain Severity and Pain Interference
Table 2 represents the perceived impact of the COVID-19 outbreak on changes in pain severity and pain interference. Overall, a large proportion of individuals (60.3% for pain severity and 62.4% for pain interference) reported that they had not perceived any changes in their pain severity and pain interference since the COVID-19 outbreak. Of those who reported changes in pain severity and interference, 29.7% and 25.6% of individuals reported an exacerbation in pain severity and interference, respectively.
Table 2.
Response frequency of perceived changes in pain severity, pain interference, mood, sleep quality, and social support
| Response Choice | Changes in Pain Severity, % | Changes in Pain Interference, % | Changes in Mood, % | Changes in Sleep Quality, % | Changes in Social Support, % |
|---|---|---|---|---|---|
| Very much improved | 0.6 | 1.3 | 1.0 | 1.0 | 1.7 |
| Much improved | 2.1 | 2.6 | 2.6 | 3.1 | 4.3 |
| Minimally improved | 7.4 | 8.2 | 6.1 | 5.2 | 10.0 |
| No change | 60.3 | 62.4 | 28.8 | 38.2 | 49.8 |
| Minimally worse | 20.5 | 19.1 | 37.7 | 28.1 | 18.9 |
| Much worse | 8.2 | 5.2 | 18.0 | 17.0 | 9.5 |
| Very much worse | 1.0 | 1.3 | 5.7 | 7.3 | 5.8 |
The Impact of COVID-19 on Perceived Changes in Mood, Sleep Quality, and Social Support
Table 2 also presents the impact of COVID-19 on perceived changes in mood, sleep quality, and social support. Only 28.8% of individuals reported that they had not perceived any changes in their mood. The majority (61.4%) of individuals reported worsened mood since the outbreak. Although 38.2% of individuals reported “no change” in their sleep quality, a large proportion (52.4%) of individuals reported that COVID-19 had negatively impacted their sleep quality. In terms of changes in social support, approximately half (49.8%) of individuals reported no change in social support since the outbreak. However, 34.2% of individuals reported worsened social support.
Variables Associated with Perceived Changes in Pain Severity and Pain Interference
Table 3 summarizes the findings of multiple regression analyses. Among numerous demographic variables, race (between Black and Asian; B = –0.36, P = 0.015, 95% confidence interval [CI]: –0.66 to –0.07) and ethnicity (B = –0.16, P = 0.028, 95% CI: –0.31 to –0.02) were significantly associated with perceived change in pain interference. Specifically, on average, individuals who are Asian reported a 0.36-point (on a 1–7 rating scale) lower negative impact score of pain interference since the outbreak than that of individuals who are Black. Also, individuals of Hispanic origin reported a 0.16-point lower negative impact score of pain interference since the outbreak than that of individuals of non-Hispanic origin. No other demographic factor was significantly associated with pain severity or pain interference.
Table 3.
Multiple regression analyses on perceived changes in pain severity and interference as outcomes
| Changes in Pain Severity |
Changes in Pain Interference |
|||||||
|---|---|---|---|---|---|---|---|---|
| Predictors | Estimates | CI | Std. Beta | P | Estimates | CI | Std. Beta | P |
| Intercept | 2.62 | 2.27 to 2.96 | 0.15 | <0.001 | 2.39 | 2.05 to 2.74 | 0.11 | <0.001 |
| Age | –0.00 | –0.01 to 0.00 | –0.03 | 0.193 | 0.00 | –0.00 to 0.00 | 0.00 | 0.898 |
| Sex (Male) | –0.09 | –0.18 to 0.00 | –0.10 | 0.060 | 0.04 | –0.05 to 0.13 | 0.05 | 0.376 |
| Race (Asian vs. Black) | –0.12 | –0.41 to 0.17 | –0.14 | 0.409 | –0.36 | –0.66 to –0.07 | –0.42 | 0.015 |
| Race (Mixed vs. Black) | –0.17 | –0.43 to 0.09 | –0.20 | 0.194 | –0.11 | –0.38 to 0.15 | –0.13 | 0.394 |
| Race (Other vs. Black) | 0.03 | –0.28 to 0.35 | 0.04 | 0.837 | 0.16 | –0.16 to 0.48 | 0.18 | 0.330 |
| Race (White vs. Black) | –0.09 | –0.26 to 0.08 | –0.11 | 0.282 | –0.10 | –0.28 to 0.07 | –0.12 | 0.253 |
| Ethnicity (Hispanic) | –0.13 | –0.28 to 0.02 | –0.05 | 0.087 | –0.23 | –0.38 to –0.07 | –0.08 | 0.004 |
| Education | 0.00 | –0.02 to 0.03 | 0.01 | 0.756 | –0.02 | –0.04 to 0.01 | –0.04 | 0.163 |
| Income | 0.00 | –0.02 to 0.02 | 0.00 | 0.894 | 0.01 | –0.01 to 0.03 | 0.03 | 0.316 |
| Changes in employment status | –0.02 | –0.10 to 0.07 | –0.02 | 0.658 | –0.03 | –0.12 to 0.06 | –0.03 | 0.494 |
| Changes in mood | 0.24 | 0.19 to 0.28 | 0.31 | <0.001 | 0.25 | 0.20 to 0.29 | 0.32 | <0.001 |
| Changes in sleep quality | 0.14 | 0.09 to 0.18 | 0.19 | <0.001 | 0.13 | 0.09 to 0.18 | 0.18 | <0.001 |
| Changes in social support | 0.02 | –0.02 to 0.06 | 0.03 | 0.280 | 0.02 | –0.02 to 0.06 | 0.03 | 0.246 |
| R2/R2 adjusted | 0.219 / 0.211 | 0.214 / 0.206 | ||||||
Std. = Standardized. The boldfaced values represent statistically significant regression estimates.
Among non-demographic variables, self-reported changes in mood were significantly associated with changes in pain severity (B = 0.24, P < 0.001, 95% CI: 0.19 to 0.28) and pain interference (B = 0.25, P < 0.001, 95% CI: 0.20 to 0.29), respectively. In other words, every 1-unit (on a 1–7 rating scale) increase of worsened mood since the COVID-19 outbreak was related to a 0.24-point greater negative impact score of pain severity and a 0.25-point greater negative impact score of pain interference. We also found that worsened sleep quality since the COVID-19 outbreak was related to exacerbated pain severity and pain interference. Specifically, every 1-unit increase (on a 1–7 rating scale) of worsened sleep quality since the COVID-19 outbreak was related to a 0.14-point greater negative impact score of pain severity (B = 0.14, P < 0.001, 95% CI: 0.09 to 0.18) and a 0.13-point greater negative impact score of pain interference (B = 0.13, P < 0.001, 95% CI: 0.09 to 0.18).
R-squared results show that 21.9% and 21.4% of perceived changes in the outcome variances for pain severity and pain interference, respectively, were explained by all the variables that were included in the regression models.
The Impact of COVID-19 on Chronic Pain Management
The Impact on Engagement in Self-Management of Chronic Pain
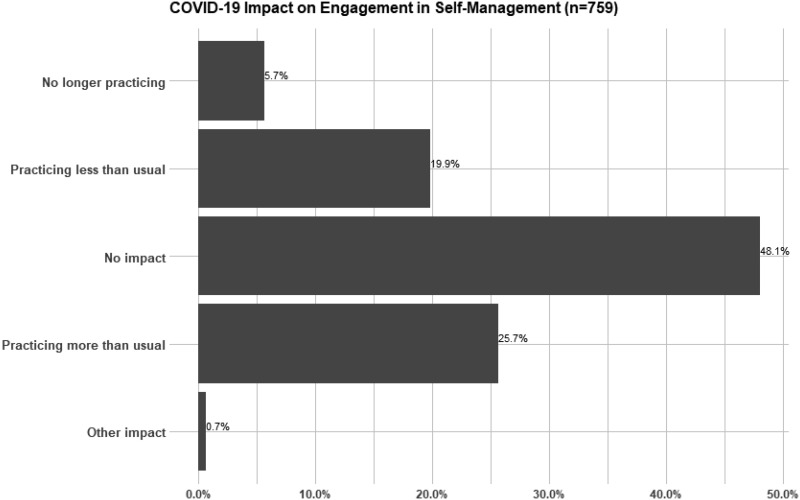
A total of 759 individuals (52.2% of the total sample) reported the use of self-management approaches (e.g., yoga, meditation, tai chi, exercise) to manage chronic pain. Among these individuals, 48.1% reported that there was no impact on their self-management practice. Among those who reported some impact, as shown in Figure 1, 19.9% reported that they were practicing self-management “less” than usual because of COVID-19, and 5.7% reported that they no longer practiced self-management as a result of COVID-19. More than one fourth (25.7%) of participants reported that they practiced self-management “more” than usual.
Figure 1.
A bar chart presenting the impact of COVID-19 on engagement in self-management of chronic pain. Examples of self-management activities include yoga, meditation, tai chi, exercise.
The Impact on Chronic Pain Treatment Appointments
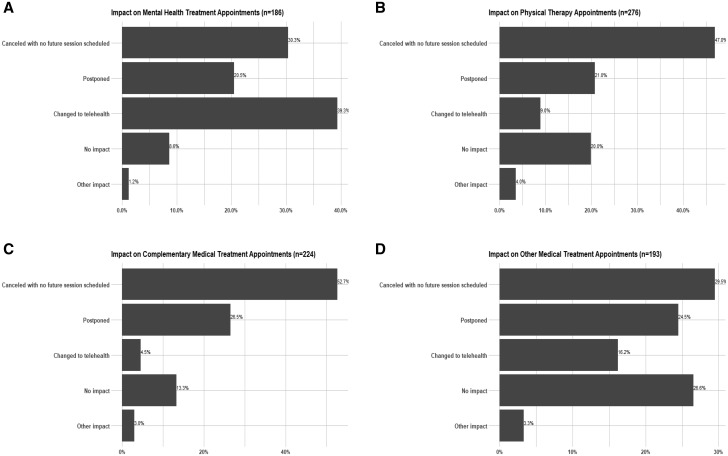
Mental health treatment. A total of 186 individuals (12.7% of the total sample) reported receiving mental health treatment for chronic pain. Among these individuals, as shown in Figure 2A, a small number of participants (8.6%) reported that there had been no impact on their mental health treatment for chronic pain. Among those who reported an impact, 30.3% reported that appointments had been canceled with no future sessions scheduled, and 20.5% reported that appointments had been postponed. Close to 40% of participants reported that their appointments had been changed to telehealth.
Figure 2.
Bar charts presenting the impact of COVID-19 on chronic pain treatment appointments.
Physical therapy. A total of 276 individuals (19% of the total sample) reported receiving physical therapy for chronic pain. Among these individuals, as shown in Figure 2B, 20% reported that there had been no impact on their physical therapy for chronic pain. Among those who reported an impact, 47% reported that appointments had been canceled with no future sessions scheduled, and 21% reported that appointments had been postponed. Less than 10% of participants reported that their appointments had been changed to telehealth.
Complementary medical treatment. A total of 224 individuals (15.4% of the total sample) reported receiving complementary treatment for chronic pain (e.g., massage, acupuncture, chiropractic care). Among these individuals, as shown in Figure 2C, 13.3% of individuals reported that there had been no impact on their complementary medical treatment for chronic pain. Among those who reported an impact, 52.7% of appointments had been canceled with no future sessions scheduled, and 26.5% of appointments had been postponed. Only 4.5% of participants reported that their appointments had been changed to telehealth.
Other medical treatment. A total of 193 individuals (13.3% of the total sample) reported receiving other medical treatment (e.g., injections, spinal cord stimulation) for chronic pain. Among these individuals, as shown in Figure 2D, 26.6% of individuals reported that there had been no impact on their other medical treatment for chronic pain. Among those who reported an impact, 29.5% reported that appointments had been canceled with no future sessions scheduled, and 24.5% reported that appointments had been postponed. Approximately 16% of participants reported that their appointments had been changed to telehealth.
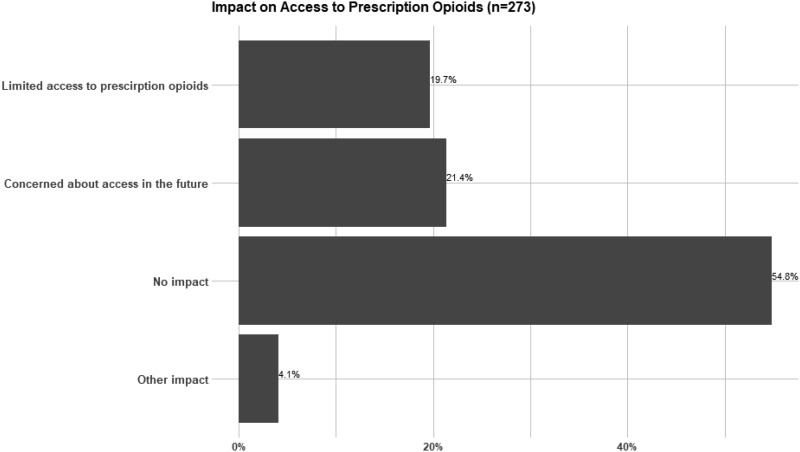
The Impact on Access to Prescription Opioids
A total of 273 individuals (18.8% of the total sample) reported receiving opioid therapy for chronic pain. Among these individuals, as shown in Figure 3, 54.8% of participants reported that there had been no impact on their opioid medication prescription. Among those who reported an impact, 19.7% reported that they currently had limited access to opioid medication because of COVID-19, and 21.4% of those who currently had access to opioid medication were concerned about access in the future.
Figure 3.
A bar chart presenting the impact of COVID-19 on access to prescription opioids.
Discussion
Using a large online sample (n = 1,453) of individuals with chronic pain in the United States, we investigated the impact of the COVID-19 pandemic on pain severity, pain interference, and chronic pain management. Close to a third (25–30%) reported worsening in pain severity and pain interference. Individuals who are Black and of non-Hispanic origin, who had greater self-reported disruptions in mood and sleep quality, reported greater negative COVID-19 impact on pain severity and pain interference. Although engagement in chronic pain self-management was largely sustained, most participants reported that their medical appointments for chronic pain had been disrupted. More than 40% of individuals also reported concerns about or difficulty accessing prescription opioids because of the pandemic.
Contrary to our expectation, most individuals reported no perceived changes in their pain severity and pain-related interference since the outbreak. One possible explanation for this unexpected finding may be that the present study was conducted during the early phase of the pandemic when stay-at-home orders went into effect in most U.S. states; hence, our data capture the acute impact of COVID-19 on these pain-related experiences. We may see a more pronounced impact of the outbreak on pain severity and pain interference with time, with the persistence of COVID-19–related stress and impact on daily life. Another possibility is that COVID-19 stay-at-home orders had some benefits for individuals with chronic pain. In our clinical experience, some patients with chronic pain have reported benefiting from the additional flexibility that work-from-home or changes to employment has afforded, which can, for example, allow more opportunity for activity pacing, reduction in work-related stressors, and increased integration of self-management practice into daily life. Future longitudinal studies will be important to understand more fully the impact of COVID-19 on pain severity and pain interference. It would be particularly helpful to collect and analyze follow-up assessment data from ongoing population-level studies that have data on pain-related experiences and physical activity levels before the outbreak.
In terms of individual differences in changes in pain severity and pain interference during the early phase of the pandemic, we did not find significant gender or socioeconomic differences. However, such demographic disparities in pain severity and pain interference have been well established in the literature, and we may expect to see a differential impact of COVID-19 on pain severity and pain interference over time. It should also be noted that perceived changes in pain interference significantly differed by race and ethnicity. Specifically, we found that participants who identified as Asian experienced lower negative impact on their pain interference since the outbreak than those who identified as Black. Although the present study cannot ascertain which particular underlying sociocultural factors resulted in this racial difference in pain interference, this finding is quite consistent with recent findings from the Centers for Disease Control and Prevention. They found that during the COVID-19 pandemic, people who identified as Black reported increased substance use and suicide ideation in the prior month more commonly than did those who identified as Asian [29]. We also found that compared to individuals of non-Hispanic origin, those of Hispanic origin reported lower negative impact on their pain interference since the outbreak. This finding is consistent with a recent systematic review suggesting that Hispanic Americans report fewer pain conditions and pain comorbidities (e.g., depression and anxiety) and less pain interference than non-Hispanic Americans [30]. There may be specific psychosocial factors associated with Hispanic ethnicity that serve as protective factors against exacerbation of pain interference during the pandemic, which warrants future investigation. Certainly, there are likely other factors at play in findings of racial and ethnic differences in the impact of the COVID-19 pandemic on chronic pain, such as the presence of other intersecting identities. This was beyond the scope of the present study; however, an in-depth investigation of the effect of cultural differences on COVID-19’s impact on chronic pain is essential to subvert patterns of inequitable care in the aftermath of COVID-19 and also to highlight unique culture strengths.
As hypothesized, those who experienced greater disturbances in mood and sleep quality since the start of the pandemic reported worsened pain severity and pain interference. These findings are consistent with extant literature suggesting that disturbances in mood and sleep quality serve as important risk factors for the maintenance and exacerbation of chronic pain [17, 18]. However, note that the present study is cross-sectional, and thus, it is possible that worsened mood, sleep quality, and social support may have been impacted by exacerbation of pain experiences. Nonetheless, to effectively assist those experiencing acute exacerbations of pain and functioning during the pandemic, a rapid introduction of remotely supported psychosocial interventions that can target mood, sleep, and pain may be important [5]. Evidence-based online psychosocial interventions, such as cognitive behavioral therapy and acceptance- and mindfulness-based interventions, appear to be promising in that regard. These online interventions are not only easily accessible and scalable, but also have demonstrated effect sizes comparable to those found in interventions delivered in person [31, 32].
Overall, individuals with chronic pain reported experiencing myriad changes in their ongoing chronic pain management. With regard to the impact of COVID-19 on chronic pain self-management practice (e.g., yoga, meditation, tai chi, exercise), more than 70% of our sample reported that they had either experienced no impact or had been practicing self-management at home more than usual since the outbreak. This finding suggests that engaging in self-management to address chronic pain can be sustained or enhanced despite the vast impact of COVID-19 on daily life. However, it is also important to note that around one in four participants reported they had ceased practicing or were practicing self-management less frequently since the start of the pandemic. These individuals may be at risk for poor pain-related outcomes as the pandemic persists, and future research could identify factors that negatively influence engagement in chronic pain self-management during the pandemic to better assist this subset of individuals.
Consistent with our expectation, the majority of chronic pain treatment appointments were either postponed or canceled because of COVID-19, without future sessions scheduled, and the conversion to telehealth varied across chronic pain treatments. Among those receiving psychological treatment for chronic pain, close to 40% indicated that their appointments had been converted to telehealth. On the other hand, among those receiving physical therapy, complementary medical treatments, or other medical treatments for chronic pain, only 4.5% to 16% reported that their appointments had been switched to telehealth. These early findings suggest the feasibility of rapid and wide-scale conversion of psychological treatment for chronic pain from in-person to telehealth delivery; however, the effectiveness of these interventions, as compared to face-to-face delivery, is unclear. These early findings also suggest that patients may have significantly reduced access to treatments that require person-to-person contact (e.g., massage, acupuncture, injections) during the pandemic; however, we suspect that access to such treatments may increase over time as we continue to adopt new models of service delivery.
Among individuals prescribed opioid medications, approximately 40% of individuals who were currently prescribed opioids reported either experiencing limited access to these medications or being concerned about future access because of COVID-19. Indeed, a recent study demonstrated, using the Texas Prescription Monitoring Program data, that there has been a significant decrease in the numbers of patients and prescribers filling and writing opioid and benzodiazepine prescriptions [33]. It will be important that providers closely monitor and develop safety plans for their patients who have been prescribed pain medication for a long time, as reduced access to this medication may result in symptoms of withdrawal and exacerbation of pain.
A strength of the present study is that the data from a large sample were collected in a narrow window of time (approximately 3 weeks), offering a unique snapshot of the early phase of the COVID-19 pandemic in the United States. The present study also had several limitations, however. First, the present findings are based on a cross-sectional design, and thus, causal inference cannot be drawn from our findings. However, it should be noted that we specifically adapted our study questionnaires to capture individuals’ perception of changes in pain-related experiences since the COVID-19 outbreak and their experience of COVID-19’s impact on various domains of their chronic pain management. Second, our measures on perceived changes in pain interference, mood, sleep quality, and social support were based on the PGIC measure but have not been previously validated. Future studies should examine the psychometric properties of these measures. Third, the perceived change measures were based on a single item. For instance, our item on changes in social support captures only the overall impact of COVID-19 and thus does not provide detailed information on what specific elements (e.g., availability, frequency, quality) of social support were affected. Future longitudinal studies should more comprehensively assess these domains. Fourth, participants’ geographic location (e.g., state of residence) was not collected. Those residing in certain areas in the United States may have exhibited greater negative impact on pain-related experiences and chronic pain treatments. Fifth, our MTurk sample is likely to have excluded many older adults, especially those who are age 70 or older. Older adults may be more impacted by the pandemic because of comorbidity burden, greater likelihood of being socially isolated, and limited use of technology. Sixth, because the present study was conducted within a narrow time frame, the interpretation and implications of our findings may be limited to this specific time phase of the pandemic. Seventh, the item that measures negative change in employment status was worded quite ambiguously (i.e., “have you experienced changes in employment status related to the coronavirus outbreak [for example: job loss, laid off, furloughed, reduction in work hours, etc.]?”), and thus it might also be the case that some participants experienced a positive change in employment. Lastly, the way that impact of COVID-19 on chronic pain treatment appointments was measured in the present study did not allow for us to conduct inferential statistics. As described earlier, because the present study was conducted in the beginning of the pandemic, where participants’ ongoing chronic pain treatment access may have been impacted in multiple ways, participants were permitted to select more than one response so as to more accurately capture their experience of changes in access to pain care.
To our knowledge, this is one of the first studies to examine the early impact of COVID-19 on individuals with chronic pain in the United States. Approximately 25% to 30% of individuals reported some exacerbation in pain severity and pain interference. Individuals identifying as Black and of non-Hispanic origin, who experienced greater disruptions in their mood and sleep quality, were more likely to report worsened pain-related experiences. Although there was no effect of gender or socioeconomic status on perceived changes in pain severity and pain interference, we may expect greater disparity to arise as the pandemic progresses, reflecting trends well established in the broader chronic pain literature. In terms of the impact of COVID-19 on chronic pain management, the majority of participants’ engagement in a self-management approach was sustained since the outbreak. However, most chronic pain treatment appointments were either canceled or postponed, and many individuals reported concern about access to opioids for their pain management. Implementing telehealth and/or evidence-based online interventions will be critical for those who are experiencing acute exacerbation of pain amid the pandemic. Longitudinal studies are also required to provide a more nuanced understanding of both the short- and long-term impact of the pandemic on pain-related experiences, pain coping, and physical functioning among individuals with chronic pain.
Funding sources: Funding for this research was provided by National Institute on Drug Abuse (F32DA049393 awarded to CJM) and National Institute on Minority Health and Health Disparities (R01MD009063 awarded to CMC).
Conflicts of interest: The authors have no conflicts of interest to disclose.
References
- 1.Coronavirus Resource Center. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE). Baltimore, MD: Johns Hopkins University (JHU; ); 2020. Available at: https://coronavirus.jhu.edu/map.html. (accessed May 5, 2020). [Google Scholar]
- 2. Jennings EM, Okine BN, Roche M, Finn DP. Stress-induced hyperalgesia. Prog Neurobiol 2014;121:1–18. [DOI] [PubMed] [Google Scholar]
- 3. Olango WM, Finn DP. Neurobiology of stress-induced hyperalgesia Curr Topics Behav Nuerosci 2014;20:251–80. [DOI] [PubMed] [Google Scholar]
- 4. Chapman CR, Tuckett RP, Song CW. Pain and stress in a systems perspective: Reciprocal neural, endocrine, and immune interactions. J Pain 2008;9(2):122–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Eccleston C, Blyth FM, Dear BF, et al. Managing patients with chronic pain during the COVID-19 outbreak: Considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain 2020;161(5):889–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CDC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep 2020;69(12):343–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Raifman M, Raifman J. Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. Am J Prev Med 2020;59(1):137–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shevlin M, McBride O, Murphy J, et al. Anxiety, depression, traumatic stress, and COVID-19 related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open 2020;6(6):e125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL. Sex, gender, and pain: A review of recent clinical and experimental findings. J Pain 2009;10(5):447–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Riley JL, Wade JB, Myers CD, et al. Racial/ethnic differences in the experience of chronic pain. Pain 2002;100(3):291–8. [DOI] [PubMed] [Google Scholar]
- 11. Janevic MR, McLaughlin SJ, Heapy AA, Thacker C, Piette JD. Racial and socioeconomic disparities in disabling chronic pain: Findings from the health and retirement study. J Pain 2017;18(12):1459–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Campbell CM, Edwards RR. Ethnic differences in pain and pain management. Pain Manag 2012;2(3):219–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. LeResche L. Defining gender disparities in pain management. Clin Orthop Relat Res 2011;469(7):1871–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Poleshuck EL, Green CR. Socioeconomic disadvantage and pain. Pain 2008;136(3):235–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res 2020;288:112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zhang J, Lu H, Zeng H, et al. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav Immun 2020;87:49–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kroenke K, Wu J, Bair MJ, et al. Impact of depression on 12-month outcomes in primary-care patients with chronic musculoskeletal pain. J Musculoskelet Pain 2012;20(1):8–17. [Google Scholar]
- 18. Finan PH, Goodin BR, Smith MT. The association of sleep and pain: An update and a path forward. J Pain 2013;14(12):1539–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. López-Martínez AE, Esteve-Zarazaga R, Ramírez-Maestre C. Perceived social support and coping responses are independent variables explaining pain adjustment among chronic pain patients. J Pain 2008;9(4):373–9. [DOI] [PubMed] [Google Scholar]
- 20. Casler K, Bickel L, Hackett E. Separate but equal? A comparison of participants and data gathered via Amazon’s MTurk, social media, and face-to-face behavioral testing. Comput Human Behav 2013;29(6):2156–60. [Google Scholar]
- 21. Buhrmester M, Kwang T, Gosling SD. Amazon’s Mechanical Turk: A new source of inexpensive, yet high-quality data? In: Kazdin AE, ed. Methodological Issues and Strategies in Clinical Research. Washington, DC: American Psychological Association; 2016:133–9. [DOI] [PubMed] [Google Scholar]
- 22. Attridge N, Crombez G, Van Ryckeghem D, Keogh E, Eccleston C. The experience of cognitive intrusion of pain: Scale development and validation. Pain 2015;156(10):1978–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Attridge N, Noonan D, Eccleston C, Keogh E. The disruptive effects of pain on n-back task performance in a large general population sample. Pain 2015;156(10):1885–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: Results of an Internet-based survey. J Pain 2010;11(11):1230–9. [DOI] [PubMed] [Google Scholar]
- 25. Cleeland CS, Ryan KM. Pain assessment: Global use of the Brief Pain Inventory. Ann Acad Med Singapore 1994;23(2):129–38. [PubMed] [Google Scholar]
- 26. Scott W, McCracken LM. Patients’ impression of change following treatment for chronic pain: Global, specific, a single dimension, or many? J Pain 2015;16(6):518–26. [DOI] [PubMed] [Google Scholar]
- 27. Geisser ME, Clauw DJ, Strand V, et al. Contributions of change in clinical status parameters to Patient Global Impression of Change (PGIC) scores among persons with fibromyalgia treated with milnacipran. Pain 2010;149(2):373–8. [DOI] [PubMed] [Google Scholar]
- 28. Harrell FE. Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis. New York: Springer; 2015. [Google Scholar]
- 29. Czeisler MÉ, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. Morb Mortal Wkly Rep 2020;69(32):1049–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hollingshead NA, Ashburn-Nardo L, Stewart JC, Hirsh AT. The pain experience of Hispanic Americans: A critical literature review and conceptual model. J Pain 2016;17(5):513–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zachariae R, Lyby MS, Ritterband LM, O’Toole MS. Efficacy of Internet-delivered cognitive-behavioral therapy for insomnia—a systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev 2016;30:1–10. [DOI] [PubMed] [Google Scholar]
- 32. Spijkerman MPJ, Pots WTM, Bohlmeijer ET. Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis of randomised controlled trials. Clin Psychol Rev 2016;45:102–14. [DOI] [PubMed] [Google Scholar]
- 33. Downs CG, Varisco TJ, Bapat SS, Shen C, Thornton JD. Impact of COVID-19 related policy changes on filling of opioid and benzodiazepine medications. Res Soc Adm Pharm 2020;17(1):2005–8. [DOI] [PMC free article] [PubMed] [Google Scholar]