Abstract
Since the outbreak of the COVID-19 pandemic, most countries have recommended their citizens to adopt social distance, hand hygiene, and face mask wearing. However, wearing face masks has not been well adopted by many citizens. While the reasons are complex, there is a general perception that the evidence to support face mask wearing is lacking, especially for the general public in a community setting. Face mask wearing can block or filter airborne virus-carrying particles through the working of colloid and interface science. This paper assesses current knowledge behind the design and functioning of face masks by reviewing the selection of materials, mask specifications, relevant laboratory tests, and respiratory virus transmission trials, with an overview of future development of reusable masks for the general public. This review highlights the effectiveness of face mask wearing in the prevention of COVID-19 infection.
Keywords: Porous materials, Face masks, Filtering, Aerosols, Airborne colloids, Viral particles, Fibers, Fabric
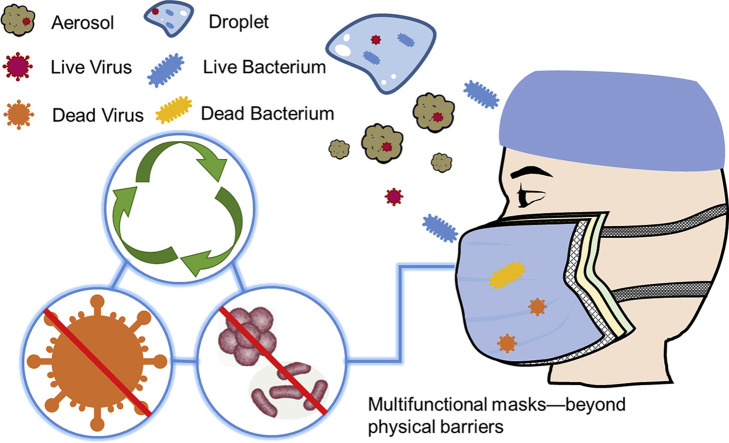
Graphical abstract
Introduction
Since the beginning of this century, we have witnessed five major epidemic/pandemic outbreaks of respiratory viral infections (RVIs), with the previous four being the severe acute respiratory syndrome (SARS) in 2002–2003, the H1N1 influenza (bird flu) in 2009–2010, the Middle East respiratory syndrome (MERS) in 2012 and Ebola in 2014–2016. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes acute respiratory disease, coronavirus diseases 2019 (COVID-19), which can be life-threatening in a proportion of those infected [1∗].Since its outbreak in January 2020, treatment has remained largely supportive and no effective vaccine against the virus was available until the last quarter of 2020. Widespread infections are still being reported across the globe at the time of finalizing this review, with the total COVID-19 deaths reaching 2,000,000 and the total infections 80 million (WHO Coronavirus Disease (COVID-19) Dashboard). The COVID-19 pandemic is imposing huge strains on global health systems and economies.
SARS-CoV-2 viruses are spherical particles with diameters around 100 nm. Because of their small sizes, they are easily dispersed in aerosols or droplets out of our breaths. Scientific evidence is now emerging to indicate that SARS-CoV-2 can remain active and infectious in aerosols or droplets suspended in the air [2∗∗]. Droplets are widely thought to be the main means of person-to-person transmission following close contact in homes, hospitals, care homes, public transport, schools, restaurants, and other public and social places. The SARS-CoV-2 can remain viable on surfaces for hours and spread by touching contaminated surfaces and transferring it to mucus membranes of the eyes, nose, and mouth (https://www.ecdc.europa.eu/en/covid-19/latest-evidence/transmission).
The World Health Organization (WHO) has issued extensive guidance and recommendations about how to control virus spreading and reduce person-to-person infections. Countries and regions across the globe have also issued regulations to manage the outbreaks, with most European and Northern American countries introducing lockdowns in March and April this year aiming at managing the pandemic by restricting movement and mass social interactions, in addition to recommendations on social distancing, hand hygiene, and face covering [3, 4, 5, 6]. In the UK context, the stricter lockdown had been imposed by the end of 2020 due to the resurging of the infections. A recent review of the latest science affirmed that cloth face coverings were a critical tool in the fight against COVID-19, particularly when used universally within communities [7∗]. Meanwhile, there is increasing evidence that cloth face coverings help prevent people who have COVID-19 from spreading the virus to others [8∗]. In order to have a direct insight of mask wearing requirements in facing COVID-19 spreading, a brief summary of universal masking policy in different countries has been listed in Table 1 .
Table 1.
Policy or recommendation of mask wearing in different countries to prevent COVID-19 transmission.
| The Country or International Organization | Policy about Public Mask Wearing | Recommended or Mandatory (R/M) | Notes and Comments |
|---|---|---|---|
| 1. The WHO | The WHO advises that governments should encourage the general public to wear masks where there is widespread transmission and physical distancing is difficult, such as on public transport, in shops, or in other confined or crowded environments. (June 6, 2020) | R | The WHO had previously argued there was not enough evidence to say that healthy people should wear masks. |
| 2. The USA | CDC recommends that people wear masks in public settings and when around people who do not live in your household, especially when other social distancing measures are difficult to maintain. (August 7, 2020) | R | Masks should not be worn by children under the age of 2 or anyone who has trouble breathing, is unconscious, incapacitated, or otherwise unable to remove the mask without assistance. |
| 3. China | Masks were relatively common even before the coronavirus pandemic, which is credited to populations used to wearing coverings because of either pollution or previous experience with the SARS and H1N1 outbreaks. | R | Now in the area of low infection risk, people are encouraged not to wear a mask. |
| 4. The UK |
In England and Scotland, face coverings are compulsory in a number of indoor spaces: banks, building societies, and post offices; places of worship; museums, galleries and entertainment venues; libraries, and public reading rooms. Face coverings are compulsory for anyone traveling by public transport in England, Scotland, Wales, and Northern Ireland (unless they have an exemption or a reasonable excuse). Many of the UK’s secondary school pupils will have to wear face coverings when they return for the autumn term. (August 28, 2020) |
M | Face coverings do not have to be worn where it would be '‘impractical’ to do so, for instance, restaurants, pubs and gyms. |
| 5. France |
France has issued a partial list of ‘indoor, enclosed’ places in which masks are to become obligatory from July 20, alongside further recommendations of how to wear a mask safely and effectively. (July 19, 2020) Wearing a face mask in public has become mandatory across Paris and several surrounding areas. (August 28, 2020) |
M | On August 28, the country recorded 7379 new infections - its highest number since early May. |
| 6. Germany |
Individual states have been given the power to implement their own rules regarding masks. Most states now require residents to wear face masks or coverings while in shops, grocery stores, and shopping malls, as well as on local public transportation. Berlin is the only state where masks are not required in shops and supermarkets, but rather ‘strongly recommended’. (April 22, 2020) |
R/M | Thousands of people, packed close together and not wearing face masks, protested in Berlin on August 1, against official measures intended to curb the spread of the coronavirus. |
| 7. India | Many states in India have made wearing masks compulsory while going out in order to curb the spread of the infection in India. (April 8, 2020) | M | – |
| 8. Italy | Italy’s government said that from 6 pm to 6 am, the wearing of masks would be mandatory in public areas where groups could form. (August 16, 2020) | M | It is compulsory to wear masks inside shops. |
| 9. Canada | Wearing a homemade nonmedical mask/facial covering in the community is recommended for periods of time when it is not possible to consistently maintain a 2-m physical distance from others, particularly in crowded public settings, such as: stores, shopping areas, and public transportation. | R | The best thing you can do to prevent spreading COVID-19 is to wash your hands frequently with warm water and soap for at least 20 s. If none is available, use a hand sanitizer containing at least 60% alcohol. |
| 10. Australia |
Everyone in the state of Victoria must wear a face covering whenever they leave home unless an exemption applies. This is because of the higher rates of community transmission of coronavirus in the state. (August 2, 2020) People in New South Wales should consider wearing a face mask in situations where physical distancing is not possible. |
R | Masks are an extra precaution to protect against COVID-19 in areas with community transmission. Check your local state and territory advice about mask recommendations and requirements. |
| 11. Vietnam | Vietnam made face masks compulsory for people to wear in public on March 16. | M | – |
| 12. Spain | Spain made it compulsory on May 20 for everyone older than six to wear masks in indoor public spaces and outdoor ones when it is impossible to keep more than two meters apart. (May 20, 2020) | M | – |
| 13. South Africa | South Africa is moving to make it mandatory to wear nonmedical cloth masks when people are outside their homes. | M | Wearing cloth masks is being introduced in conjunction with maintaining a physical distance of at least 1.5 m and strictly following hygiene measures such as hand washing. |
On the March 20, of this year, the BBC re-broadcast its 2009 TV drama Spanish Flu: The Forgotten Fallen. It depicted how Dr. James Niven, a Mancunian doctor, worked out how to deal with the 1918 flu pandemic in Manchester through different interventions, with face covering as one of the key measures recommended to prevent flu transmission. By adopting these measures, working-class people living in dense populations could manage to go out and make a living. Although in the intervening century, the world has experienced numerous RVIs, including four major outbreaks in the past two decades, the current COVID-19 pandemic has exposed serious deficiencies in preparedness for epidemic RVI. Common features arising from these viral pandemic outbreaks are fast infection rates, high mortality, and lack of effective treatment. Under these situations, the only way to mitigate would be to adopt a ‘bundle’ of nonpharmaceutical interventions. Evidence from the past 9 months has indicated a high degree of variation in adopting the recommended measures across countries, especially in face mask wearing.
The views on the effectiveness of face mask wearing in preventing COVID-19 transmissions are still divided. It is, however, comforting to indicate at this point that the UK government online surveys over the past few months have revealed very positive attitudes of people from the majority of countries (http://www.coviddatahub.com; data were updated during May–October 2020). Over 80% of people surveyed from Italy, Spain, and the USA have revealed their willingness to wear a face mask in public places, well in line with the trend from those surveyed in China, India, Japan, Singapore, and South Korea. However, this is in sharp contrast to the outcome surveyed from Denmark, Finland, Norway, and Sweden, with some 90% of people expressing no consideration of mask wearing at all. Australia and the UK are somewhat in the middle, reflecting that the task ahead is still huge to convince the general public of the benefits of mask wearing. Our ongoing work in urban shanties in Kenya (unpublished) shows similar levels of willingness to wear masks among some of the most deprived populations, provided the economic and technical barriers could be overcome.
This paper aims to review the design, manufacturing, functional performance, and effectiveness of various types of face masks. It will start by outlining the working principle of face masks in reducing the risk of airborne infections from a basic viewpoint of colloid and interface science. It will then review the main scientific studies conducted over the past 10 years or so to assess the effectiveness of face masks for both medical professionals and the general public. It will also review current requirements and standards for designing and manufacturing face masks, followed by further technical considerations on their functional performance. A brief outlook is given on the future development of reusable face masks, especially for use in resource-constrained settings. The review is themed by the ongoing challenges presented by the viral particles of SARS-CoV-2 underlined by the interdisciplinary knowledge from colloid and interface, fiber and textile technology, microbiology, and clinical medicine of the authors. Face mask wearing presents a range of technical challenges, many of which originate from existing concepts of droplets and their interactions with fabric bundles or porous media.
Caution must, however, be drawn in reading the scientific data summarized from both laboratory-based studies and clinical trials. Some key literature studies, standards, and guidelines cited in this review tend to base their evidence or arguments on bacterial and fungal work. Viral particles are much smaller than bacteria or fungi. This, together with their different physical and biological properties, may make some of the conclusions less reliable. In particular, many types of face masks aimed at the general public are fast coming into the market, but the amount of research that shows their fit-for-purpose is currently lacking. In addition, face mask wearing may bear social, cultural, and geographical influences, with some unfortunate politicization since the COVID-19 outbreak. Furthermore, wearers may not wear them properly, have repeated handling and compromise hygiene, etc., resulting in a false sense of security that could actually make the transmissions worse. As will be seen in the following, the impacts from these factors may make the outcome from well-controlled laboratory research ‘too obvious and biased’, but they may become well reflected in clinical trials because results from the latter do not tend to offer ‘unanimous’ verdicts. Finally, some of the new masks to be introduced showcase technological excellence and capability as ‘future wonders’, but their sophistication may mount up difficulties in scale up with potentially high costs.
Principle of protection from face masks: against aerosols and large droplets
Theoretically, respiratory viruses can be transmitted through fine aerosols (droplets and droplet nuclei with aerodynamic diameters ≤ 5 μm), respiratory droplets (including larger droplets that fall rapidly near the source, as well as coarse aerosols with aerodynamic diameters > 5 μm), or direct contact with secretions [9,10∗]. A face mask provides a barrier to prevent the respiratory tract from being exposed to droplets and airborne aerosols. The physical interception, therefore, reduces the risk of RVIs. Studies have revealed that SARS-CoV-2-containing particles can be ejected several meters from a coughing or sneezing patient. These particles vary significantly in size, which, in turn, affects the distance from the source that the particles travel through the air. Large particles will precipitate on surfaces of laptops, desks, chairs, and any other items nearby, but the smaller ones will be suspended in air for a much longer time, and travel further, depending on airflow dynamics [11]. Aerosols refer to the small end of airborne water droplets exhaled from or sneezed out of a patient, with typical sizes below 2–3 μm. They remain airborne for prolonged periods because of their small size and low settling velocity. According to the study about the role of particle size in transmission by Knight [12], settling times for spherical particles of verified sizes, in a 3-m fall (the height of a room) for specific diameters, were 10 s for 100 μm, 4 min for 20 μm, 17 min for 10 μm and 62 min for 5 μm; and particles with diameters 1–3 μm essentially did not settle [4].
The study of SARS-CoV-2 in aerosols and its stability on various surfaces has attracted researchers’ attention since the beginning of the COVID-19 outbreak and was even compared with SARS-CoV-1. Doremalen et al. [2] from the National Institute of Allergy and Infectious Diseases (the USA) estimated the stability of both SARS-CoV-2 and SARS-CoV-1 in aerosols and on various surfaces (for example, plastic, stainless steel, copper, and cardboard) and evaluated their reduction rates using a Bayesian regression model. Both SARS-CoV-1 and SARS-CoV-2 remained viable in aerosols for 3 h (the experimental duration) and showed a reduction in infectious titer from 103.5 to 102.7 TCID50 (50% tissue-culture infectious dose) and from 104.3 to 103.5 TCID50 per liter of air, respectively.
Cowling et al. [5] applied a mathematical model to the data obtained from randomized controlled trials of influenza A virus transmissions in households of Hong Kong (China) and Bangkok (Thailand). According to their analyses based on the two key factors from the aerosol transmission, the timing of secondary infections, and clinically different presentation of secondary infections caused by aerosol transmission, they concluded that aerosol transmission accounted for approximately half of all transmission events. As a clinical feature, infections via aerosol transmission may have a higher risk of febrile illness from volunteer studies. These findings provided new insights into the understanding, and therefore, prevention of influenza transmission in confined spaces such as classrooms and offices. They also indicated that just relying on cutting down transmission via contacts or large droplets might not be sufficient.
In order to demonstrate the role of aerosols in influenza transmission, Noti et al. [13] carried out the first laboratory study in 2012 to assess the efficacy of medical masks and N95 respirators in blocking inhalation of influenza in aerosols. They first demonstrated that infectious influenza could be recovered in all aerosol fractions, with about 5% in particles with aerodynamic diameters >4 μm, 75% in 1–4 μm, and 20% in <1 μm. They then found that while tightly sealed masks could block entries of 95% of both infectious viruses and total viruses, the tightly sealed respirators could block >99.6% for both types of viruses. However, poorly fitted respirators and loosely fitted masks performed equally badly, with the blocked entries being less than 70% of the infectious and total viruses.
Although the protective effects of both surgical masks and respirators have been studied extensively, the performance of cloth masks still remains unclear. Cloth masks are commonly made of synthetic or natural textiles or other similar materials available domestically, such as cotton cloth of different thread count per inch, natural silk, flannel (a hybrid of cotton and polyester), synthetic silk (100% polyester), spandex (a hybrid of nylon, polyester and spandex), chiffon (a hybrid of polyester and spandex), and polyester and cotton blends. Because manufacturing techniques of woven fabric are different from melt-blown fabric, nonwoven fabric materials can have more pores per unit area and higher filtration efficiency than textiles. Against surgical masks and respirators, the fit of homemade masks is often looser. This, together with the more diverse range of cloth porosities and fabric properties, could lead to poor functional properties and compromise to wearers’ protection. In a cluster randomized trial comparing the efficacy of cloth masks with medical masks in hospital healthcare workers (HCWs), MacIntyre et al. [14] concluded that cloth masks caused significantly higher rates of influenza-like illness than medical masks. These authors also showed that the filtration efficacy and facial fit of cloth masks were inferior to those of medical masks and respirators. They thus concluded that cloth masks should not be used by the HCWs as they should be equipped with appropriate medical face masks and respirators [15]. Cloth masks are a more suitable option for the general public in a community setting because of their easy availability, reusability, good comfortability, and breathability.
On the other hand, the filtration efficacy of cloth face masks varies and depends on a variety of factors: the type of material used (structure and composition of the fabric), number of layers, moisture degree in a mask, and the size and shape of the particles exposed [16,17]. Studies by Konda and Davies [17,18] demonstrated that a wide range of textiles could ensure the efficient removal of most airborne particles. They also showed that masks made of quality cloth were capable of intercepting the majority of large respiratory droplets. Furthermore, when a specific combination of different fabrics was used to form multilayered masks, their filtration efficiencies would improve further. Filtration efficiencies of the hybrid fabrics were larger than 80% for particles <300 nm and 90% for particles >300 nm. Macro particles (diameters > 0.6 μm, e.g., polluted aerosols and most bacteria) are usually larger than pore sizes of the mask filters and can be intercepted outside face masks. The microparticles (∼0.3–0.6 μm, e.g., some bacteria and large viruses) have a chance to move through the pores, but these particles will possibly get caught by the fibers and thus become hard to reach the wearers. For nanoparticles with diameters <0.3 μm, such as viruses, they can easily flow through the pores as air inhalation and do not become adhered to fiber walls. Masks made from nanofibers with higher porosity and smaller pore size could improve capturing efficiencies, and electrospun nanofibers may perform even more efficiently in this process due to the electrostatic effect [19]. Leonas and Jones [20] have assessed six types of face masks with different pore sizes. They pointed out that face masks with smaller pore sizes mostly have higher bacterial filtration efficiencies. Wang et al. [21] used nanofibrous membranes consisting of polyethersulfone and BaTiO3 to increase the filtration efficiency and comfortability of face masks. They showed that the pore size decreased from 2.6 μm to 1.5 μm, and the porosity increased from 52% to 91% as the concentration of BaTiO3 increased from 0 wt% to 2 wt%. Consequently, the filtration efficiency had a significant rise from 91% to 96%. Increase in the thickness of the nanofibrous membrane could also decrease the pore size and increase the porosity, but such improvement to the filtration efficiency of face masks was usually marginal.
Face mask wearing has played an important role in protecting both HCWs and the general public by reducing the incidences of infection through airborne transmission. The face mask worn by a patient can reduce not only the release of virus-carrying droplets into the open air but also the inhalation of the virus-carrying droplets from the open air. Mask wearing can prevent the release of viruses into the open air by an infected but asymptomatic healthcare provider. At the same time, the mask can also prevent breathing in viruses suspended in the air. Mask wearing in a clinical setting can help reduce the incidences of infection through airborne transmission between patients and healthcare workers. The implication of this scenario to the general public is that mask wearing could help cut down infection spreading from asymptomatic carriers to healthy people.
Mask wearing is thus a crucial measure to prevent the virus from spreading via airborne aerosols. It is useful at this point to mention that in addition to sizes, the settling time of aerosols can be affected by ambient airflow. In terms of the dynamic process, ‘aerosol’ is not an absolute but rather a relative term. In environments with strong cross-flow or natural ventilation, a larger respiratory droplet (>100 μm) can remain airborne for a longer time. This environmental factor makes it possible for the suspended pathogens to cause infections at considerable distances away from the source. In the recent work by Tellier et al. [10], they pointed out that the cross-flow environment often changes vastly and instantly in healthcare settings, such as with frequent door opening and closing, and people walking back and forth. On the contrary, a significant downdraft could decrease the suspension time, even for smaller droplets [10]. Notably, incomplete understanding of viral, environmental, and host factors means that the potential for aerosol transmission may be underestimated.
Analyses comparing infection rates in Hong Kong, Japan and South Korea, and the USA and the UK where general consensus as to whether face coverings should be mandatory in community (nonmedical) settings, have provided ample evidence on the efficacy of face coverings to slow transmission [22,23]. It is possible that some of us are asymptomatic carriers, just like some of the healthcare workers. Without wearing a face mask, the asymptomatic sufferer can easily pass the viruses onto others in close contact through respiratory and oral droplets and possibly aerosols.
Mask wearing as a necessity to beat COVID-19 transmission
Because of complex situations in real living settings, it can be difficult to make a convincing case that face mask wearing is effective. As other factors such as social distancing and hand washing also contribute to the reduction of infections, it is not straightforward to quantify the contribution of each measure separately. This situation, together with many cultural and socio-behavioral factors, has made it hard to justify the implementation of face mask wearing to the general public [24].
However, COVID-19 infections share features similar to a common flu or H1N1 pandemic. Extensive scientific studies have been conducted to support face mask wearing. A recent study by Wang et al. [25∗∗] monitored the temporal evolution of infection rates among HCWs following the implementation of face mask wearing in the Mass General Brigham (MGB) to both HCWs and patients during March–April of this year when COVID-19 started to spread in Boston area. MGB is the largest healthcare system in Massachusetts, with 12 hospitals and more than 75,000 HCWs. The multipronged infection reduction strategy involved systematic testing of symptomatic HCWs and universal masking of all HCWs and patients. The study reported a clear control of the SARS-CoV-2 infection rate among HCWs associated with hospital masking, suggesting a decrease in transmission among HCWs and between patients and HCWs. However, other interventions inside and outside the MGB system, such as restrictions on elective procedures, social distancing, and increased masking in the general public outside, could also have contributed to the reduction of the HCW infections. On the other hand, the authors did notice the continued increase of infection numbers from the general public in Massachusetts throughout the study period. This example indicates that it is impractical to deploy a randomized, double-blinded, and controlled trial of face masking to HCWs or to a community of the general public during a pandemic. Nonetheless, their results strongly support face covering as part of a multimeasure infection control strategy in healthcare settings [25].
A number of randomized clinical trials and technical assessments of face masks conducted in community and healthcare settings over the past decades, using varied interventions, including a mixed approach of mask wearing and hand washing (Table 2 ), have demonstrated the efficacy of face covering in reducing the transmission of respiratory viruses [26, 27, 28, 29]. At the point of writing this review, more clinical trials and related research studies have shown that the use of face masks as personal protective equipment (PPE) is valuable to prevent the spread of respiratory infections [30∗, 31, 32, 33]. Milton et al. [34] studied how surgical masks could intercept respiratory aerosols when worn by patients suffering from seasonal influenza. They found a significant reduction of cultivable influenza viruses from surgical mask wearing, with the overall number of RNA copies being decreased by 3.4 folds. They also found that mask wearing is more effective at blocking large particles (>5 μm) than small ones (<5 μm) in the exhaled aerosols.
Table 2.
Representative trials and experiments of masks to prevent respiratory virus transmission.
| Study, year of publication | Area, Country | Virus Type and Prevention Setting | Type of Study and Population | Main Findings |
|---|---|---|---|---|
| 1. Wang et al. [25] (2020) | Massachusetts, the USA | SARS-CoV-2; surgical masks | Cluster and systematic testing; healthcare workers | These results support universal masking as part of a multipronged infection reduction strategy in healthcare settings. |
| 2. Leung et al. [30] (2020) | Hong Kong, China | Seasonal human coronaviruses, influenza viruses, and rhinoviruses; surgical face masks | Cluster randomized trial; symptomatic individuals | Aerosol transmission is a potential mode of transmission for viruses; surgical face masks could prevent transmission of human coronaviruses and influenza viruses from symptomatic individuals. |
| 3. Milton et al. [34] (2013) | the USA | Seasonal influenza; surgical masks | Individual trail; volunteers | Surgical masks worn by patients reduce aerosol’s shedding of the virus. |
| 4. Aiello et al. [33] (2010) | Michigan, the USA | Influenza A/H1N1; face mask use, face masks with hand hygiene | Randomized intervention trial; young adults | Face masks and hand hygiene may reduce respiratory illnesses in shared living settings and mitigate the impact of the influenza A/H1N1 pandemic. |
| 5. MacIntyre et al. [35] (2011) | Australia | Respiratory virus; fit-tested and nonfit-tested N95 respirators to medical masks | Cluster randomized clinical trial; healthcare workers | The rates of clinical respiratory illness, influenza-like illness, laboratory-confirmed respiratory virus infection, and influenza infection were consistently lower for the N95 group than medical masks. |
| 6. Loeb et al. [36] (2009) | Ontario, Canada | Influenza A/H1N1; surgical masks, N95 respirators | Randomized trial; healthcare workers | This study indicated that the use of a surgical mask compared with an N95 respirator resulted in noninferior rates of laboratory-confirmed influenza. |
| 7. MacIntyre et al. [26] (2015) | Australia | Seasonal influenza, pandemic influenza, MERS-CoV; facemasks and respirators | Randomized controlled trials, literature review work | Facemasks and respirators are important but understudied forms of personal protective equipment against respiratory infections. |
| 8. Liang et al. [37] (2020) | China | Influenza viruses, SARS, and SARS-CoV-2; masks | Literature review work and meta-analysis | An additional evidence of the enhanced protective value of masks, which stresses that the use of masks serves as an adjunctive method against the COVID-19 outbreak. |
| 9. Ma et al. [32] (2020) | Qingdao, China | SARS-CoV-2; mask-wearing and handwashing | Experiments, literature review, and control experiences | Mask wearing plus instant hand hygiene slows down the exponential spread of SARS-CoV-2. |
| 10. Zhou et al. [38] (2018) | the USA | Human influenza A and rhinoviruses; respiratory face mask | Technical assessment and experiment | The results demonstrated >99.7% efficiency of each test mask configuration for the exclusion of influenza A virus, rhinovirus 14, and S. aureus. |
| 11. Noti et al. [13] (2012) | Morgantown, the USA | Infectious influenza virus; respirators and masks | Laboratory studies in the simulation chamber | This study supported a role for aerosol transmission; tightly sealed masks and respirators are of good performance in blocking inhalation of influenza in aerosols; a poorly fitted respirator performs no better than a loosely fitting mask. |
Several other clinical trials and experimental studies have also demonstrated that masks can effectively protect the general public from being infected by various airborne infections by interrupting viral/bacterial transmission routes [17,29,39]. Apart from material properties, both facial fit and particle filtration efficacy by surgical masks play a major role in protecting HCWs [15,16]. These previous observations are consistent with the recent clinical results from Leung et al. [30∗], who found that surgical face masks could significantly reduce the quantity of influenza and coronavirus RNA detected in respiratory aerosols. Given varied interpretations concerning the protective effects of face masks, Liang et al. [37∗] made a meta-analysis of 21 recent studies. The pooled analysis showed that face masks are effective in preventing the transmission of RVIs. Such protective effect of mask wearing is evident for both healthcare workers and the general public, and the evidence was also highly consistent across Asian and Western populations. Furthermore, the use of surgical and N95 masks can significantly decrease the risks of healthcare workers when they are exposed to high-risk environments [40,41].
Mask application and development status: civil sanitary, surgical, and N95 masks
Historically, surgical face masks were offered to sick individuals to prevent the respiratory disease from spreading. It was also recommended to prevent them from infections or contaminations. It was later recommended to medical professionals to prevent them from catching infections from their patients. With the current COVID-19 pandemic expanding, various mask devices are being manufactured and used in both healthcare and community settings worldwide, ranging from cloth masks (cotton or gauze), medical masks (medical, surgical or procedural) to respirators (N95, N99, N100, P2, P3, FFP2, and FFP3). Medical masks and cloth masks are designed to prevent the spread of virus infection from wearers to others, but are also commonly used to protect the wearers from splashes, pathogenic bacteria or sprays of blood or other forms of body fluids [26]. The main difference between face masks and respirators is that face masks cannot provide a good seal around the face, while respirators are well-fitted devices designed to protect the wearers from respiratory infections. Respirator seals around the face are well designed and manufactured, and they can be regulated according to their filtration capacities [42].
Apart from medical masks and respirators, various models targeted at the general public are now also available or in the process of being developed (Table 3 ). It is worth mentioning that more and more novel technologies are employed in face mask design to achieve novel functions, e.g., incorporation of silver nanoparticles or silver ions to enhance antimicrobial protection. Coating of graphene or polygrene (a new graphene polymer range) into the outer layer of the mask makes it to be both antibacterial and antiviral, and even with photothermal properties. Meanwhile, the application of novel technologies and new materials in mask production helps eliminate worries from customers about their mask wearing, such as inhalation of nanoparticles and other safety issues. More and more commercial brands (e.g., Mizuno, Yonex and Uniqlo) are designing and marketing reusable and washable masks and heat absorptive ones for summer use, providing more choices for the general public with different expectations.
Table 3.
Features of typical face masks in use or under development.
| Face Mask Type | Mask Name | Supplier/Manufacturer Information | Main Features |
|---|---|---|---|
| 1. Nanofilter Masks | Teflon nanofilter masks | Guangzhou Donghong Fluoro Plastic Co. Ltd, China |
|
| Bionic spider web nanofilter masks | Nanjing Tech University, China |
|
|
| Nanofiber masks | Huafang Nano Technology Co. Ltd, China |
|
|
| Nano protective filter masks | Junyeyoupin Co. Ltd, China |
|
|
| 2. Masks Modified with Inorganic Nanoparticles/Layers | Nano Ag antimicrobial masks | ANSONBIOTECH, China |
|
| Face masks with antimicrobial protection using silver ion technology | Meryl Palo Alto, the USA |
|
|
| Copper oxide containing respiratory face masks | Cupron Scientific, Modi’in, Israel |
|
|
| 3. Masks Modified with Graphene Materials | Self-cleaning and photothermal graphene masks | Hong Kong Polytechnic University and Hong Kong Research Institute of Textiles and Apparel, China |
|
| 2AM Graphene-enhanced face masks | Planar TECH, the UK & IDEATI Co., Ltd. Thailand |
|
|
| Graphene enhanced protective face mask | Versarien PLC, Gloucestershire, the UK |
|
|
| Graphene-based masks | Changzhou Tanxing Technology Co. LTD & Southeast University, China |
|
|
| Laser-induced graphene masks with rapid bacterial killing | City University of Hong Kong & Hong Kong Polytechnic University & Nankai University, China |
|
|
| 4. Cloth/Fabric Masks | Reusable cloth face masks | Max Threads, the USA |
|
| Cloth cut protective face masks | DG Mask, LLC, the USA |
|
|
| Apparel fabric masks (sports fabric, swimwear) | Mizuno/Yonex/Uniqlo/Knit Waizu Co. Ltd, Japan |
|
|
| Ergonomic and children protective barrier cloth face masks | Bossong Hosiery Mills, the USA |
|
|
| Washable and K95 nonmedical face masks | Fabtrends, Montreal, Canada |
|
Mask design standards or requirements
Surgical masks and PPE respiratory masks have strict design standards in most countries. In the European Union, all mask manufacturers must follow Rule PPE Regulation (EU) 2016/425, BS EN 149:2001 when manufacturing filtering half-face masks to protect against particles, BS EN 136:1998 when making full-face masks - class 1/2/3, BS EN 140:1999 when making half/quarter masks, BS EN 143:2000 for making particle filters and BS EN 14387:2006 for making gas filters & combined filters. A recent CEN document CEN 14683:2019+AC, approved in 2018, specifies construction, design, performance requirements, and test methods for medical face masks to control the transmission of infective agents from staff to patients in medical settings. Similarly, Document AS/NZS 1716:2012 specifies the breath of PPE requirements in Australia and New Zealand.
Cloth face coverings, including home-made masks, are recommended by the Centers for Disease Control and Prevention as they help stop the wearers from spreading infection or becoming infected. Many individuals turn to reusable face masks, most often the ‘do-it-yourself’ ones made from different fabric materials. Many countries have begun to develop their regulations, standards, and guidelines to ensure the appropriate applications of various face masks under the current intensified COVID-19 spreading. As masks are potentially in close contact with the skin for a long period of time, adequate material and biocompatibility checks are strongly recommended. Relevant performance testing for fabric face masks includes barrier function testing, breathing resistance testing, color fastness testing, ear loop attachment strength, and restricted substances assessment. Of all the specifications, barrier performance is most crucial for reusable fabric masks. Most countries or regions have adopted particulate filtration efficiency (PFE) as the key barrier capacity. Barrier efficiency regulations/standards/guidelines in certain markets are summarized in Table 4 .
Table 4.
Regulations and requirements for civil sanitary mask design and manufacture in different countries.
| Country | Type of Specification | Regulation/Standard/Guidelines | Test Method | Barrier Performance and Requirements |
|---|---|---|---|---|
| USA | Recommendation by industry | General Purpose Woven Face Coverings – Guidance and Considerations | ASTM F2299 or technical equivalent, with modified micron size | 3 μm particles ≥70% filtration efficiency as minimal |
| China | Association standard | T/CNTAC 55-2020 & T/CNITA 09104-2020 | GB/T 38413-2019 | PFE; PM 2.5 daily reusable protective mask as received: ≥95%, aftercare: ≥90% General daily reusable protective mask as received: ≥90%, aftercare: ≥85% |
| UK | Recommendation | British Standards Institution (BSI) guide to masks and face coverings for use in the UK during the COVID-19 pandemic | EN 13274–7:2019 | PFE; Requirement to be determined by the Cabinet Office/Department for Business, Energy and Industrial Strategy (BEIS) |
| France | Regulation/Guidelines | AFNOR Spec S76-001 v1.1 | DGA method Annex 2 or equivalent | PFE; 3 μm particles: >90% for UNS Class I >70% for UNS Class II |
| Germany | Recommendation | BfArM Recommendations | – | Attention on marking and labeling issue |
| EU Countries | Reference document from the CEN Members | CEN Workshop Agreement CWA 17553 |
EN 13274–7:2019 | PFE; Particles size: 3 μm Level 90%: min 90% Level 70%: min 70% |
| South Africa | Recommendation | Recommended Guidelines | EN 13274–7:2019 | PFE; Particle size: 5 μm ≥75% |
The requirements for civil sanitary mask design are different across the globe. China recently revised its standard under ‘Chinese Civil Sanitary Mask Design’ jointly issued by China National Textile and Apparel Council (CNTAC) and China Nonwovens and Industrial Textiles Association (CNITA). It is updated from the previous standards for the daily protective masks (GBT 32610-2016). In this document, bacterial filtration efficiency (BFE), PFE, airflow resistance, and flame retardant properties are the four main requirements imposed in face mask design and manufacture (Table 5 ). This document also provides an essential guideline for trading and purchase of civil sanitary masks. Beijing Civil Administration has recently issued its first ‘Reusable Civil Sanitary Mask Design’ guidance to specify that reusable civil masks meet the following requirements: more than 3 washable times; accumulated and effective wearing time over 24 h, the nose clip not falling off during wearing, no obvious deformation during use, same particle filtration efficiency as KN90 masks (GB2626-2019), antibacterial efficiency over 90% if labeled as antimicrobial, shell-life of 5 years.
Table 5.
Quality requirements for civil sanitary mask design and manufacture in group standard T/CNTAC 55-2020 & T/CNITA 09104-2020 (China). Note that no data are available concerning virus management. It is common to treat viral infection control requirements the same as those adopted for bacteria and fungi by assuming that they all cause infections through the droplet or particle route.
| Test Program | Requirements |
|
|---|---|---|
| Masks for adults | Masks for children | |
| Length of nose clip/cm | ≥8.0 | ≥5.5 |
| Connection strength between mask band and mask body/N | ≥5 | |
| Bacterial filtration efficiency/% | ≥95 | |
| Inorganic particle filtration efficiency/% | ≥90 | |
| Airflow resistance/Pa | ≤49 | ≤30 |
| Fastness to dry rubbing/degree | ≥3 | ≥4 |
| Residue of ethylene oxide/(μg/g) | ≤10 | |
| Formaldehyde content/(mg/kg) | ≤20 | |
| pH | 4.8∼8.5 | 4.0∼7.5 |
| Decomposable carcinogenic aromatic amine dye/(mg/kg) | Forbidden to use | |
| Microbial detection | Requirements | |
| Total number of bacterial colony/(CFU/g) | ≤200 | |
| Escherichia coli | Not detected | |
| Staphylococcus aureus | Not detected | |
| Pseudomonas aeruginosa | Not detected | |
| Streptococcus hemolyticus | Not detected | |
| Total number of fungal colony/(CFU/g) | ≤100 | |
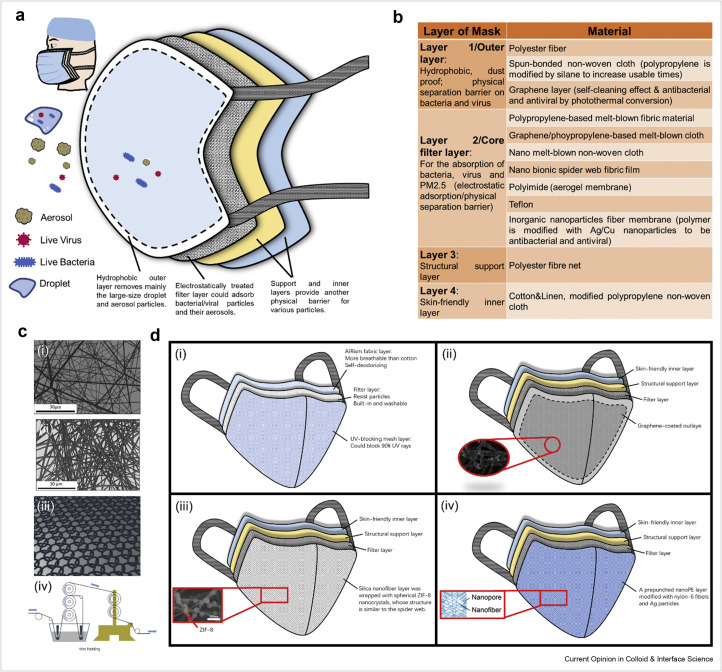
Surgical masks are most widely used [43], but they are usually intended to ensure the safety of healthcare workers by preventing their infections from patients by filtering off bacteria/viruses from airborne droplets and aerosols. Different types of surgical masks have distinctly different designs. Surgical masks often have 3–4 layers, including two nonwoven fabric layers and a melt-blown polymer fabric between them. Also, different layers in a surgical mask function differently. The nonwoven fabric incorporates electrostatic charges and can remove bacteria/viruses and aerosols containing microorganisms by physical filtration and electrostatic absorption when air is permeated through (Figure 1 a). Majchrzycka and coworkers [44] investigated the survival of microorganisms on five different commercial filtering nonwoven masks. They found that structural parameters of the tested nonwovens (mass per unit area and thickness) and contact angle changes did not greatly affect microorganism survival, but the survival fraction was more dependent on microorganism species. Medical masks are for single use, but a common shortcoming is the quick loss of their static charges during wearing. The exact charge loss is, however, affected by environmental temperature and humidity. The fabric is often produced from polypropylene (PP), but it can also be made of other materials like polystyrene, polycarbonate, or polyester. The pleats on masks are designed to allow the wearers to expand the masks to their faces from nose to chin. Head ties or elastic straps are commonly used to secure the mask. As many medical and healthcare professionals wear masks on a daily basis, preference on the straps is emerging, with some of them preferring to use the head ties for better comfort.
Figure 1.
Structure and composition of materials in different layers of a standard medical face mask and illustrations of key features from four commercial face masks. (a) Schematic assignment of the function of the respective layers in a medical face mask: a combination of a physical barrier and electrostatic absorption against droplets, viruses, bacteria, and aerosols, containing viruses/bacteria. (b) Typical materials used in respective layers. (c) 3D Morphologies of (i) spunbonded nonwoven fabrics and (ii) melt-blown nonwoven fabrics; (iii) 3D structure of a knitted fabric and (iv) schematic of a wet padding process. (d) Comparison of four representative commercial face masks. (i) UNIQLO AIRism face mask consisting of three functional layers, sunscreen layer, particle filtration layer, and skin-friendly layer; (ii) Graphene-coated mask surface is of excellent self-cleaning and photothermal properties; (iii) Bioinspired spider web-like mask filling ZIF-8 around the nanofibers; (iv) Thermal-management nanofiber-based face mask coating with Ag thin layer. Inset pictures in Figure 1d are reprinted from Ref. [53, 61, 67] with permissions from American Chemical Society and Elsevier.
N95 masks are shaped into a convex cap and are the most popular particle-filtering respirators. Meanwhile, a malleable aluminum strip is placed above the nose area to provide a tighter seal. This kind of respirator can filter at least 95% of airborne particles but is not resistant to oil droplets [45]. As in the case of some surgical masks, the N95 mask is also comprised of four layers, but it is structured in a more complex manner than that adopted in a surgical mask. The outer layer is similarly produced by a hydrophobic polypropylene surface. The second layer consists of cellulose and polyester, which can be modified by positively charged copper and zinc ions to attract bacteria and viruses (with negatively charged membranes) by electrostatic interaction. Then, a melt-blown polymer is the third layer and the fourth layer (inner layer) is made of spun-bound polypropylene. In terms of more complex aerosol filtration containing pathogenic influenza and rhinoviruses, as well as the fine particulates (PM 2.5), N95 respiratory masks show improved performance over other types of masks [38]. In a cluster randomized clinical trial, MacIntyre et al. [35] reported comprehensive outcomes covering clinical respiratory illness, influenza-like illness, laboratory-confirmed respiratory virus infection, and influenza, with the N95 group showing consistently better results than the group using medical masks. Additionally, a previously randomized trial conducted among healthcare workers also indicated that the use of a surgical mask compared with an N95 respirator resulted in similar rates of transmission of laboratory-confirmed influenza [36]. These studies, together with the extensive work by MacIntyre et al. [35,41,46] show that, when manufactured properly and used by following adequate guidance, face masks and respirators are highly effective at preventing virus infections, even though the manufacturing standards and approval requirements are based on particle blockage, bacterial and fungal tests.
Fibers, nonwoven fabrics, and textile technologies
Both natural and synthetic fibers have been used to manufacture nonwoven mats. PP is the ideal fibrous material to produce face mask textiles due to its low-cost, excellent antimicrobial behavior, mechanical strength, and chemical resistance. Traditional 3-layered planar-structured surgical face masks consist of two layers of porous nonwoven fabrics and a nonwoven filtration medium, to form a stacking structure of spunbond-melt-blown-spunbond layers. The outer leak-proof layer and the inner direct skin contact layer generally adopt spunbonded PP nonwoven fabrics with ∼20 μm fiber diameters. As the spunbonded layers support the structure of a surgical mask, the melt flow index of PP is set between 2.5 and 6.0 g/min at 230 °C, according to the standard ASTM D 1238. Occasionally, staple fiber-based nonwoven fabrics are also used as the inner layer to improve skin touch. In contrast, the middle layer often uses melt-blown nonwoven fabric with 2 μm fiber diameters. During the melt-blown fabrication process, high flowability PP is required with a melt flow index around 100–200 g/min at 230 °C, following the same ASTM standard. Furthermore, electrostatic treatment would be carried on the middle layer. Hence, compared with the physical barrier of diffusion entrapment and inertial collision, the electrostatic adsorption of the middle layer could significantly enhance the capture of aerosols or airborne particles. The outer layer can block droplets and large particles due to the water-resistant property and inertia effect, while the inner layer provides the major absorption of moisture from respiration and filtration capacity based on the electrostatic effect, the intricate network, and the extensive pore structure of the nonwoven fabric.
There are also other types of nonwoven fabrics such as electrospun, air-laid, wet-laid, and spunlaced nonwovens. To facilitate hygienic requirements and reduce production costs, spunbonded and melt-blown methods are preferred. The spunbonded process was developed in the 1940s and then adopted in the field of nonwoven fabrics. During the production, the polymers are melted and directly spun into filaments through small nozzle die heads, and then the filaments are stretched to 10–30 μm in diameter. The as-prepared fibers are laid down on the porous support and transport belt. Afterward, the as-prepared webs are consolidated by a so-called ‘calendaring process’ [47]. Figure 1c shows the main morphological features of spunbonded nonwoven fabrics and melt-blown nonwoven fabrics.
The melt-blown process is also an efficient approach to producing micro-sized or nano-sized fibers, typically by melting and extruding the granular thermoplastic propylene into a die and then attenuating it in the high-temperature and high-velocity air streams. The fibers are then deposited onto a collector to form a nonwoven web [47]. These fibers can mostly have diameters in 2–7 μm, but could even reach diameters around 500 nm. All fabric materials so produced must undertake subsequent processes covering pretreatment, printing, dyeing, and finishing. Recently, functional finishing technologies are widely introduced to equip them with antibacterial, superhydrophobic, antistatic, and charge properties through chemical coatings, deposition, and exposure to infrared, electret, and plasma.
In addition to the effective blockage of particles, medical masks can benefit from other functions. One key aspect is to develop bactericidal or bacteriostatic materials and investigate the durability of filtration materials toward the disinfection process. Graphene, as a remarkable 2D material, has shown enhanced protection property of face masks. Graphene enhanced protective face masks have been produced from graphene-modified polymers to protect against airborne pathogens and reduce viral infection spreading. (http://www.versarien.com/files/3815/9619/6343/Versarien_KN95_Facemask_Datasheet.pdf). Also, silver-metalized fibers have been developed to launch the sanitary masks, which can be reused after more than 50 washing cycles. (https://www.mitsufuji.co.jp/en/information/hamonagmask_20200317/). Melt-blown nanofibers have also been investigated for reusability as face mask filters upon spraying with and dipping in 75% ethanol in the coronavirus pandemic [48∗]. The results have indicated consistent efficiency of the nanofabric filters after multiple reuses. A further study by applying nanoporous membranes as replaceable layers to enhance the reusability and filtration efficiency of N95 masks has revealed clear improvement [49∗].
Besides nonwoven fabrics, woven and knitted structures can also be used as medical textiles with different sewing techniques. As knitted fabric materials can provide porous and extensible features with the interloping structures, as shown in Figure 1c, they can be applied as the inner layer in face masks to improve comfortable sensation. Padding is a process using biological enzymes to soften textiles and squeeze the fabric sheet through two rollers before steaming and drying to optimize the treatment effect (Figure 1c). The as-treated fabric will become weakened and softened, with a much-improved hand feeling.
Although various fabrics and textiles are already available and more are being manufactured, it still remains largely unclear how their physical and geometrical properties affect the blockage of particles and droplets and how such data can be correlated to the performance of face masks against viruses that are far smaller than bacteria and fungi. More data is expected to support the current view that they are all transmitted via particles or droplets and that current approaches are adequate in maximizing efficiencies of face masks.
Transforming to abundant civic masks for general public – making the competition for medical PPEs a story of the past
Because of the global shortages of PPEs, the supplies of medical masks and N95 respirators became severely depleted over the first half of 2020 in many countries, with existing supplies having to be prioritized for those in more urgent need. As a result, many healthcare workers had to use medical masks and respirators for prolonged periods or use substandard ones. In some extreme periods, medical workers had to use self-made or locally sourced substitutes to protect themselves. Mandates for mask use in public and a global shortage of commercial supplies have led to widespread use of homemade masks and mask alternatives. It is important to acknowledge at this point that the evidence for mask use is still widely debated (https://www.cebm.net/covid-19/masking-lack-of-evidence-with-politics/). Many of us accept that wearing such masks reduces the likelihood for an infected person to spread the disease or for a healthy person to become infected, but the opposite statement is also often heard, often from some well-respected individuals. In the early stage of COVID-19 outbreak, there was a huge shortage of them, restricting their access. Many approaches were pursued to try to ease the situation. For example, an Easybreath Decathlon mask, characterized by its high sealing power, was introduced in some European hospitals [50] to work as substitutes for FFP2 masks and face shields against COVID-19. Such masks would equally work well in African countries, where standard PPE protections for medical professionals are not always guaranteed. The sterilization techniques developed by Kumar and colleagues [51] could help decontaminate N95 respirators via autoclave treatment, ethylene oxide gas, low-temperature hydrogen peroxide gas plasma treatment, vaporous hydrogen peroxide exposure, and peracetic acid dry fogging without damaging their shape, delicate structure, and material properties so that they can replicate their performance as when they are brand new. For the decontamination of N95 respirators over long-term usage and the removal of accumulated viruses and bacteria on the respirator surfaces, a new mask capable of photothermal decontamination was also designed [52∗] by applying a plasmonic and superhydrophobic coating on the surface of N95 respirators, offering significantly better protection. In a similar design strategy, the same team has developed a reusable and recyclable graphene mask that can self-sterilize under sunlight illumination [53]. Based on similar strategies, researchers from City University of Hong Kong, The Hong Kong University of Science and Technology and Nankai University found that laser-induced graphene (LIG) modified antibacterial masks could improve the bacterial inhibition rate to ∼80%, combined with the graphene layer’s photothermal effect, resulting in 99.998% bacterial killing efficiency within 10 min [54∗].
Compared with surgical masks and particle filtration masks with specific design requirements and devoted uses, daily protection masks for the general public tend to be incorporated with various features to meet demands from different groups. Commercial masks take user experience into consideration. While considering protective safety, they take into more serious account the comfort and aesthetics in product design. In a recent study of masks’ droplet filtering efficacy, Fischer et al. [54,55∗∗] designed an easy-to-use measurement setup to allow for rapid evaluation of mask performance during speaking, sneezing, or coughing. Among 14 masks, including a 3-layer surgical mask, an N95 mask, homemade masks, and mask alternatives, they found that the N95 mask was most effective in reducing droplet emissions (nearly 100%) and that the 3-layer surgical mask and the one made with a combination of cotton and PP were the next best alternatives (over 90%). Additionally, even without the hydrophobic PP, pleated style masks made with 2-layer cotton provided a good physical barrier and gave rise to a noticeable reduction of transmitted droplets (about 80%) with a significant delay between speaking and detecting particles. The masks effectively acted as temporal low pass filters, smoothed the ejection droplet rate over time, and reduced the overall risk of transmission effectively. This study provided an important insight into the usefulness of nonmedical face masks in personal protection against droplet emission [55].
Amirav et al. [56] have compared the small air hood and face mask in the aerosol delivery of inhaled medications to infants with a mean age of 2.8 years old hospitalized with viral bronchiolitis. Basis on their randomized, double blinded, controlled trials, they found both methods to be equally effective with similar clinical scores. Interestingly, however, 80% of parents favored the hoods, and 18% of parents preferred the masks, with about 2% showing no preference. This example demonstrates that public opinion, though not scientifically based, can twist and drive diversified demands from different communities in choosing PPEs of different types. Parents, in this case, did cast their views on comfort and aestheticism. The current trend of mask wearing is strongly featuring these two aspects, especially from younger groups. Many civil mask manufacturers avoid nose clips in their products because young consumers like to show their face shape when wearing masks. Such preferences are also posing challenges to the selection of mask materials. When applying a design to fit the face, the mask must adopt an elegant 3D structure supported by facial features and will look more fashionable than traditional single-use masks.
Since the start of the COVID-19 pandemic, many sportswear and apparel brands like Yonex, Mizuno and Uniqlo have begun their personalized mask design and manufacture supported by various functionalized sports fabric materials. The mask products produced by these companies have desirable advantages such as being washable, easy to breathe, quick drying and even environment friendly. In the following section, we focus on a few examples to highlight the technical advances in the field.
UNIQLO AIRism Mask for Summer. High temperatures in the summer can lead to a high risk of heat stroke for face mask wearers. UNIQLO Japan recently launched a new product named AIRism mask made from the AIRism fabric containing breathable cupro fibers and micro nylon (Figure 1d). This material quickly absorbs and releases perspiration, which results in a low level of the moisture trapped under the mask. UNIQLO used ultra-fine fibers in AIRism to minimize the friction between the cloth and human skin so that the wearer could have a comfortable feeling at all times.
The AIRism mask consists of three layers. The outer layer is UV-blocking with a mesh structure that could filter up to 90% UV rays, an important feature to attract many young Japanese and Asians. The middle layer is the main filter zone to resist bacteria and viruses. The inner layer is the AIRism fabric layer in contact with the face skin. This product could be machine washed up to 20 times without losing its effectiveness. The AIRism mask from UNIQLO not only protects wearers from viruses and bacteria but also provides them with UV protection, cool and comfortable feeling.
Reusable Graphene Mask with Self-sterilization. A reusable and self-cleaning graphene mask has been developed by a team from Hong Kong Polytechnic University. As explained previously, a graphene layer is coated onto the nonwoven mask by the dual-mode laser-induced forward transfer method. Compared with traditional medical face masks, the graphene mask has a superhydrophobic surface, which makes the incoming aqueous droplets bounce off, as schematically shown in Figure 1d. The temperature on the graphene mask surface could increase to over 80 °C under sunlight illumination, and the mask becomes reusable after photothermal sterilization. The graphene mask is thus recyclable and can be reused in solar-driven decontamination. The researchers have recently applied the technology to N95 respirators. The graphene coating combined with silver nanoparticles can provide not only photothermal decontamination but also enhanced disinfection [52]. However, masks of these types will drive costs up and limit their use for the general public.
Bionic Spiderweb-mimicking Nanofiber Mask. The bionic spiderweb-like nanofiber masks recently entered into mass production early this year in China. Many of these products were donated to Italy to ease off the local mask shortage earlier this year. The mask is featured by having a middle layer of zeolitic imidazolate framework (ZIF-67) trapped in the polystyrene hierarchical porous nanofiber membrane (ZIF-67/PS HPNFM), offering good efficiency to filter particulate matters (PM) and airborne harmful chemicals [52,57]. The ZIFs act as a good gas adsorbent because of their micropores (high porosity, high surface area) and stability in the acidic environment [58,59]. The nanofibers could be modified with ZIFs by electrospinning technology to enhance their ability to remove PM and harmful gas compounds [60]. Inspired by the spiderweb morphological features, the researchers developed a beads-on-strings composite membrane by filling ZIF-8 around the nanofibers (Figure 1d) [61]. The multifunctional nanofibers with the spiderweb-like structure work as an ideal material for the PM and pollutant air filtration. In comparison with traditional melt-blown fibers, this new type of filter fibers has a better air permeability and can be reused. The masks made of the membrane material could filter off pollutants without static electret. As a result, these masks could be washed by water and ethanol without losing filter efficiency.
Thermal-management Nanofiber-based Face Mask. In order to achieve a high efficiency to remove PM, many commercial face masks usually involve fiber layers [62] that can cause high resistance to airflow. As a result, these masks would create discomfort for breathing and impose danger for elderly people and those with lung diseases. Extensive work has been undertaken to improve their suitability as mask materials under representative conditions [63]. People wearing face masks in a high-temperature environment tend to sweat more easily and feel more uncomfortable. A moist and warm face mask could also provide a fertile environment for bacteria to grow and threaten the wearer’s health. A team from Stanford University developed polymer nanofibers, including polyacrylonitrile, polyimide, and nylon-6, with high PM removal efficiency and air permeability [64, 65, 66]. Recently, they demonstrated a thermal-management face mask with a combination of fiber/nanoporous polyethylene (nanoPE) and Ag (Figure 1d) [67]. NanoPE formed the supporting substrate according to its transparency to the mid-infrared (IR) radiation from humans. In a high-temperature environment, the combination of fiber and nanoPE performed high PM removal efficiency, air permeability, and cooling property. In a low-temperature environment, the addition of a thin layer of Ag contributed to the reflection of radiation from the human body, leading to high effectivity of heat preservation.
Enhanced Antimicrobial Face Masks Modified with Nanoparticles. Many face masks can block bacteria by their highly hydrophobic fabric outer layer. However, the addition of nanomaterials has been shown to contribute to the antimicrobial ability of the face masks [68,69]. A study demonstrated that copper nanoparticles have inhibitory activity against bacterial and fungal growth, including Escherichia coli and Candida albicans [70]. Similar antimicrobial effects have been reported from nanoparticles such as Ag, Ti/Ni, and MgF2 when incorporated in membranes or face masks [69,71,72]. Under the current COVID-19 epidemic, however, it would be highly necessary to see data conducted on viral blockage and viral transmission control.
These exemplar cases of mask products have applied different approaches to upgrade from single-use masks to reusable ones by modifying textile materials and employing specific design strategies. The manufacturers must have considered the costs and customers they were aiming for. It is difficult for people living in poverty-stricken areas to adopt them shortly. These reusable masks have quite sophisticated technologies involved in producing the perfect materials. This, together with the procedures and costs in manufacturing, makes them out of the options range for many populations living in third-world countries.
An important aim for the scientific and business sectors is to provide feasible mask designs to produce reusable face masks with low technical sophistication and good affordability. These efforts will help those living in poverty to get out of the shortage of face masks. However, some design concepts as outlined above are still useful to inspire us. Firstly, coating a superhydrophobic layer on the outer layer works well to prevent the attachment of bacterial and viral drops, but the challenges lie in the development of easier and cheaper routes to make the superhydrophobic surface coating washable, reusable, and robust. Secondly, fiber materials with stable charges could be developed to substitute melt-blown fibers as the middle layer to improve filter efficiency against loss of static charges with temperature and humidity. The new material could be manufactured as a replaceable filler into a mask holder with a middle ‘pocket’ to avoid production sophistication.
As a summary remark, it is useful to point out that although the current demand has driven many commercial masks from various manufacturers and suppliers, there is a lack of agreed standards or requirements concerning their manufacturing and testing that would provide evidence-based guidelines on their safe use for the general public, and hence, fit for purpose. More crucially, there is an urgent need to conduct research to examine how effective these face masks work in preventing viral transmission instead of bacteria and fungi. For reusable masks, it is highly relevant to examine how effective management of moisture and condensation may influence mask performance and time of reuses.
Future perspectives in mask development
Some 9 months into the outbreak of COVID-19, there is no sign of slowing down of its invasion into people’s lives across the world. More and more countries are now recommending their citizens to wear face masks to protect themselves and others. WHO and many other infection control authorities have warned that COVID-19 is likely to stay with us over the foreseeable future and that we must learn how to live into the ‘new normal’ lives, making mask wearing a long-term addition to our daily rituals. As already indicated, disposable medical masks were originally intended for patients, medical and healthcare workers. Over the past 9 months, their daily consumptions have mounted enormously across the globe. Because they are made of PP and for single use only, concerns have already been raised about the sustainability and environmental impact of this current practice.
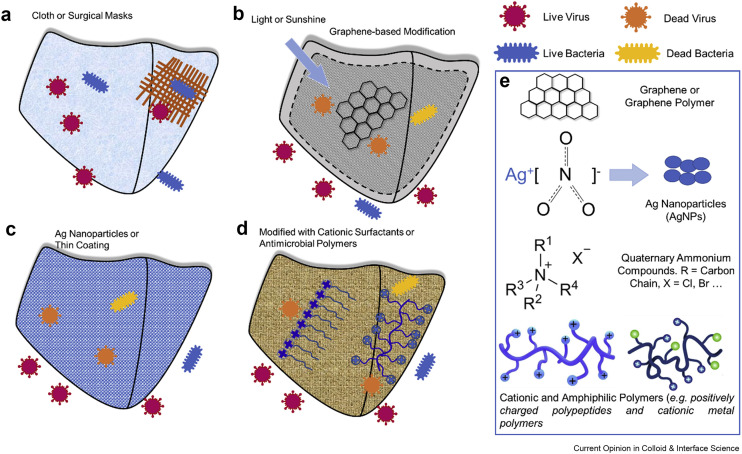
While the demands of medical masks and respirators will continue, it is becoming more difficult to justify the use of single-use PPE items by the general public. Developing reusable masks is the way forward to ease off the burden of the shortage of medical masks. This is clearly the future as the standards for general public protection are not as vigorous as those for the medical and healthcare professionals. Unlike single-use medical masks that intercept most of the particles and droplets mainly by electrostatic interaction, reusable masks work mainly by filtering barriers such as hydrophobicity and porosity. These features, together with ongoing demands for good comfort, low cost, and attraction, will drive a new wave of design and material exploration. As indicated earlier, many researchers and manufacturers have started to develop reusable and low-cost mask designs. These efforts are improving the market situation and providing better protections to fight COVID-19 infections. The market development has already driven the scientific and technological endeavors to explore fiber materials and cloth fabrications that can support the ongoing demands for new properties and functions: reusable, degradable, environment-friendly, cheap, easy, and comfortable wearing [76∗∗]. Meanwhile, the resilient microbial viability on common face masks poses a big threat to population of long-time mask wearing because the majority of bacteria remain proliferative even after 8 h. In the short and medium terms, surface modifications of degradable fibers by coating materials that have already shown bactericidal (bacterial killing and bacteriostatic) and biocompatible properties (Figure 2 ) will be explored to support the expanding demands. Among them, PPE materials with intrinsic and environmental conditions and enhanced antibacterial and antiviral activities improve the protection effect of masks and are assuming their roles gradually [53,54]. Apart from masks in role of health protection, direct sampling and analysis of trace constituents in exhaled breath aerosols can be achieved on a used face mask, a simple and noninvasive approach (face mask microextraction) can rapidly provide useful insights into human physiological and pathological status [46,77∗]. Finally, international standardization and guidance for reusable masks aimed at the general public will emerge from infection control organizations and regulatory bodies that will guide manufacturing and testing. This evolving process will drive new research and fulfill the current gaps in antiviral tests and assessment, drawing closer relevance to the properties and functioning of face masks.
Figure 2.
Antimicrobial/bacterial filtration mechanisms of different mask types and their corresponding antimicrobial agents. (a) Virus/bacterial filtration via a physical barrier and electrostatic absorption in cloth and surgical masks. Antimicrobial/antiviral action via masks modified with (b) silver-nanoparticle coating, (c) graphene layer with photothermal effects, and (d) cationic surfactants/polymers, and amphiphilic polymers [73, 74, 75]. (e) The chemical structure of some commonly used antimicrobial agents: graphene, quaternary ammonium compounds, silver nanoparticles, cationic and amphiphilic polymers (from top to bottom). The last picture in Figure 2e are reprinted from Ref. [73] with permission from Elsevier.
Author contributions
M.L. and H.L. undertook literature search and manuscript drafting. M.L., H.L., J.L. and X.L. wrote the manuscript. All authors discussed, reviewed, edited, and approved the manuscript. M.N., X.L., K.B. and J.L. were responsible for funding.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We thank the University of Manchester for a COVID-19 GCRF research fund entitled Assessing the Effectiveness of Bespoke Locally Sourced Face Masks in Reducing COVID-19 Transmission within Informal Settlements in Kenya (P122809 Task Code KC96), overseas research studentships from the University of Manchester to M.L., H.L. and X.H., studentship from China Scholarship Council to M.L., research grants from Lonza to H.L and from Syngenta to X.H. This work also benefited from grant support from a Marie Curie Fellowship ITN grant (grant number 608184) under SNAL (small nano-objects for alteration of lipid bilayers) and a BBSRC LINK grant with AstraZeneca (BB/S018492/1).
This review comes from a themed issue on Hot Topic: COVID-19
Edited by Reinhard Miller and Libero Liggieri
References
- Cheng V.C., Wong S.C., Chuang V.W., So S.Y., Chen J.H., Sridhar S., et al. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J Infect. 2020;81:107–114. doi: 10.1016/j.jinf.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study indicated that community-wide mask wearing, even a cloth mask wearing, might contribute to the control of COVID-19.
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study evaluated the stability of SARS-CoV-2 in aerosols and on various surfaces and compared its decay rates with SARS-CoV-1.
- 3.Nicolaides C., Avraam D., Cueto-Felgueroso L., González M.C., Juanes R. Hand-hygiene mitigation strategies against global disease spreading through the air transportation network. Risk Anal. 2020;40:723–740. doi: 10.1111/risa.13438. [DOI] [PubMed] [Google Scholar]
- 4.Tellier R. Review of aerosol transmission of influenza a virus. Emerg Infect Dis. 2006;12:1657–1662. doi: 10.3201/eid1211.060426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cowling B.J., Ip D.K., Fang V.J., Suntarattiwong P., Olsen S.J., Levy J., et al. Aerosol transmission is an important mode of influenza a virus spread. Nat Commun. 2013;4:1935. doi: 10.1038/ncomms2922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang G., Zhang Y., Zhao J., Zhang J., Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395:945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks J.T., Butler J.C., Redfield R.R. Universal masking to prevent SARS-CoV-2 transmission—the time is now. J Am Med Assoc. 2020;324:635–637. doi: 10.1001/jama.2020.13107. [DOI] [PMC free article] [PubMed] [Google Scholar]; This editorial emphasized the urgency for the general public to clearly understand when and how to wear cloth face coverings properly.
- Gostin L.O., Cohen I.G., Koplan J.P. Universal masking in the United States: the role of mandates, health education, and the cdc. J Am Med Assoc. 2020;324:837–838. doi: 10.1001/jama.2020.15271. [DOI] [PubMed] [Google Scholar]; A comprehensive viewpoint from statewide mandates and CDC’s recommendations on face coverings in response to COVID-19.
- Shiu E.Y.C., Leung N.H.L., Cowling B.J. Controversy around airborne versus droplet transmission of respiratory viruses: implication for infection prevention. Curr Opin Infect Dis. 2019;32:372–379. doi: 10.1097/QCO.0000000000000563. [DOI] [PubMed] [Google Scholar]; This review pointed out that quantitative measurements of virus transmission over the aerosol route must be evaluated in infectivity of respiratory viruses.
- 10.Tellier R., Li Y., Cowling B.J., Tang J.W. Recognition of aerosol transmission of infectious agents: a commentary. BMC Infect Dis. 2019;19:101. doi: 10.1186/s12879-019-3707-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nicas M., Nazaroff W.W., Hubbard A. Toward understanding the risk of secondary airborne infection: emission of respirable pathogens. J Occup Environ Hyg. 2005;2:143–154. doi: 10.1080/15459620590918466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Knight V. Viruses as agents of airborne contagion. Ann N Y Acad Sci. 1980;353:147–156. doi: 10.1111/j.1749-6632.1980.tb18917.x. [DOI] [PubMed] [Google Scholar]
- 13.Noti J.D., Lindsley W.G., Blachere F.M., Cao G., Kashon M.L., Thewlis R.E., et al. Detection of infectious influenza virus in cough aerosols generated in a simulated patient examination room. Clin Infect Dis. 2012;54:1569–1577. doi: 10.1093/cid/cis237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.MacIntyre C.R., Seale H., Dung T.C., Hien N.T., Nga P.T., Chughtai A.A., et al. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015;5 doi: 10.1136/bmjopen-2014-006577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chughtai A.A., Seale H., Macintyre C.R. Effectiveness of cloth masks for protection against severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26:1–5. doi: 10.3201/eid2610.200948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sharma S.K., Mishra M., Mudgal S.K. Efficacy of cloth face mask in prevention of novel coronavirus infection transmission: a systematic review and meta-analysis. J Educ Health Promot. 2020;9:192. doi: 10.4103/jehp.jehp_533_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davies A., Thompson K.A., Giri K., Kafatos G., Walker J., Bennett A. Testing the efficacy of homemade masks: would they protect in an influenza pandemic? Disaster Med Public Health Prep. 2013;7:413–418. doi: 10.1017/dmp.2013.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Konda A., Prakash A., Moss G.A., Schmoldt M., Grant G.D., Guha S. Aerosol filtration efficiency of common fabrics used in respiratory cloth masks. ACS Nano. 2020;14:6339–6347. doi: 10.1021/acsnano.0c03252. [DOI] [PubMed] [Google Scholar]
- 19.Tebyetekerwa M., Xu Z., Yang S., Ramakrishna S. Electrospun nanofibers-based face masks. Adv Fiber Mater. 2020;2:161–166. doi: 10.1007/s42765-020-00049-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leonas K.K., Jones C.R., Hall D. The relationship of fabric properties and bacterial filtration efficiency for selected surgical face masks. J Tex. Appar Technol Manag. 2003;3:1–8. [Google Scholar]
- 21.Wang N., Cai M., Yang X., Yang Y. Electret nanofibrous membrane with enhanced filtration performance and wearing comfortability for face mask. J Colloid Interface Sci. 2018;530:695–703. doi: 10.1016/j.jcis.2018.07.021. [DOI] [PubMed] [Google Scholar]
- 22.Han Q., Lin Q., Ni Z., You L. Uncertainties about the transmission routes of 2019 novel coronavirus. Influenza and Other Respiratory Viruses. 2020;14:470–471. doi: 10.1111/irv.12735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martin G.P., Hanna E., McCartney M., Dingwall R. Science, society, and policy in the face of uncertainty: reflections on the debate around face coverings for the public during COVID-19. Crit Publ Health. 2020:1–8. [Google Scholar]
- 24.Face masks and coverings for the general public: behavioural knowledge, effectiveness of cloth coverings and public messaging. The Royal Society; 2020. [Google Scholar]
- Wang X., Ferro E.G., Zhou G., Hashimoto D., Bhatt D.L. Association between universal masking in a health care system and SARS-CoV-2 positivity among health care workers. J Am Med Assoc. 2020;324:703–704. doi: 10.1001/jama.2020.12897. [DOI] [PMC free article] [PubMed] [Google Scholar]; This three-phase study revealed that universal masking was associated with a significantly lower rate of SARS-CoV-2 infection among healthcare workers.
- 26.MacIntyre C.R., Chughtai A.A. Facemasks for the prevention of infection in healthcare and community settings. BMJ Br Med J. 2015;350:h694. doi: 10.1136/bmj.h694. [DOI] [PubMed] [Google Scholar]
- 27.Chung S.J., Ling M.L., Seto W.H., Ang B.S., Tambyah P.A. Debate on MERS-CoV respiratory precautions: surgical mask or N95 respirators? Singapore Med J. 2014;55:294–297. doi: 10.11622/smedj.2014076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang P., Seale H., Raina MacIntyre C., Zhang H., Zhang Z., Zhang Y., et al. Mask-wearing and respiratory infection in healthcare workers in Beijing, China. Braz J Infect Dis. 2011;15:102–108. doi: 10.1016/S1413-8670(11)70153-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jefferson T., Canini L., Andréoletti L., Ferrari P., D'Angelo R., Blanchon T., et al. Surgical mask to prevent influenza transmission in households: a cluster randomized trial. PloS One. 2010;5 doi: 10.1371/journal.pone.0013998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung N.H.L., Chu D.K.W., Shiu E.Y.C., Chan K.H., McDevitt J.J., Hau B.J.P., et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. 2020;26:676–680. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]; This brief communication reported that surgical face masks significantly reduced coronavirus RNA in aerosols and influenza virus RNA in respiratory droplets.
- 31.Zhai Z. Facial mask: a necessity to beat COVID-19. Build Environ. 2020;175:106827. doi: 10.1016/j.buildenv.2020.106827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ma Q.X., Shan H., Zhang H.L., Li G.M., Yang R.M., Chen J.M. Potential utilities of mask-wearing and instant hand hygiene for fighting SARS-CoV-2. J Med Virol. 2020;92:1567–1571. doi: 10.1002/jmv.25805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aiello A.E., Murray G.F., Perez V., Coulborn R.M., Davis B.M., Uddin M., et al. Mask use, hand hygiene, and seasonal influenza-like illness among young adults: a randomized intervention trial. J Infect Dis. 2010;201:491–498. doi: 10.1086/650396. [DOI] [PubMed] [Google Scholar]
- 34.Milton D.K., Fabian M.P., Cowling B.J., Grantham M.L., McDevitt J.J. Influenza virus aerosols in human exhaled breath: particle size, culturability, and effect of surgical masks. PloS One. 2013;9 doi: 10.1371/journal.ppat.1003205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.MacIntyre C.R., Wang Q., Cauchemez S., Seale H., Dwyer D.E., Yang P., et al. A cluster randomized clinical trial comparing fit-tested and non-fit-tested N95 respirators to medical masks to prevent respiratory virus infection in health care workers. Influ Other Respiratory Viruses. 2011;5:170–179. doi: 10.1111/j.1750-2659.2011.00198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Loeb M., Dafoe N., Mahony J., John M., Sarabia A., Glavin V., et al. Surgical mask vs N95 respirator for preventing influenza among health care workers. J Am Med Assoc. 2009;302:1865–1871. doi: 10.1001/jama.2009.1466. [DOI] [PubMed] [Google Scholar]
- Liang M., Gao L., Cheng C., Zhou Q., Uy J.P., Heiner K., et al. Efficacy of face mask in preventing respiratory virus transmission: a systematic review and meta-analysis. Trav Med Infect Dis. 2020;36:101751. doi: 10.1016/j.tmaid.2020.101751. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study confirmed the enhanced protective effect of masks in the COVID-19 outbreak.
- 38.Zhou S.S., Lukula S., Chiossone C., Nims R.W., Suchmann D.B., Ijaz M.K. Assessment of a respiratory race mask for capturing air pollutants and pathogens including human influenza and rhinoviruses. J Thorac Dis. 2018;10:2059–2069. doi: 10.21037/jtd.2018.03.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lai A.C.K., Poon C.K.M., Cheung A.C.T. Effectiveness of facemasks to reduce exposure hazards for airborne infections among general populations. J R Soc Interface. 2012;9:938–948. doi: 10.1098/rsif.2011.0537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Offeddu V., Yung C.F., Low M.S.F., Tam C.C. Effectiveness of masks and respirators against respiratory infections in healthcare workers: a systematic review and meta-analysis. Clin Infect Dis. 2017;65:1934–1942. doi: 10.1093/cid/cix681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.MacIntyre C.R., Chughtai A.A., Rahman B., Peng Y., Zhang Y., Seale H., et al. The efficacy of medical masks and respirators against respiratory infection in healthcare workers. Influenza and Other Respiratory Viruses. 2017;11:511–517. doi: 10.1111/irv.12474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Siegel J.D., Rhinehart E., Jackson M., Chiarello L. Health Care Infection Control Practices Advisory, C., 2007 guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am J Infect Contr. 2007;35(10 Suppl 2):S65–S164. doi: 10.1016/j.ajic.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Smith J.D., MacDougall C.C., Johnstone J., Copes R.A., Schwartz B., Garber G.E. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis. Can Med Assoc J. 2016;188:567–574. doi: 10.1503/cmaj.150835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Majchrzycka K., Okrasa M., Szulc J., Jachowicz A., Gutarowska B. Survival of microorganisms on nonwovens used for the construction of filtering facepiece respirators. Int J Environ Res Publ Health. 2019;16:1154. doi: 10.3390/ijerph16071154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Niosh-approved N95 particulate filtering facepiece respirators. Centers for Disease Control and Prevention; 2016. [Google Scholar]
- 46.MacIntyre C.R., Chughtai A.A. A rapid systematic review of the efficacy of face masks and respirators against coronaviruses and other respiratory transmissible viruses for the community, healthcare workers and sick patients. Int J Nurs Stud. 2020;108:103629. doi: 10.1016/j.ijnurstu.2020.103629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kellie G. Woodhead Publishing; 2016. Advances in technical nonwovens. [Google Scholar]
- Ullah S., Ullah A., Lee J., Jeong Y., Hashmi M., Zhu C., et al. Reusability comparison of melt-blown vs nanofiber face mask filters for use in the coronavirus pandemic. ACS Appl Nano Mater. 2020;3:7231–7241. doi: 10.1021/acsanm.0c01562. [DOI] [PubMed] [Google Scholar]; This work compared the conventional melt-blown filter with nanofiber filter and evaluated their reusability.
- El-Atab N., Qaiser N., Badghaish H., Shaikh S.F., Hussain M.M. Flexible nanoporous template for the design and development of reusable anti-COVID-19 hydrophobic face masks. ACS Nano. 2020;14:7659–7665. doi: 10.1021/acsnano.0c03976. [DOI] [PMC free article] [PubMed] [Google Scholar]; This work designed a flexible nanoporous mask with a replaceable membrane, showing good breathability and enhanced filtration efficiency.
- 50.Addi R.Ait, Benksim A., Cherkaoui M. Easybreath decathlon mask an efficient personal protective equipment (PPE) against covid-19 in Africa. J Clin Exp Invest. 2020;11 [Google Scholar]
- 51.Kumar A., Kasloff S.B., Leung A., Cutts T., Strong J.E., Hills K., et al. 2020. N95 mask decontamination using standard hospital sterilization technologies. [Google Scholar]
- Zhong H., Zhu Z., You P., Lin J., Cheung C.F., Lu V.L., et al. Plasmonic and superhydrophobic self-decontaminating N95 respirators. ACS Nano. 2020;14:8846–8854. doi: 10.1021/acsnano.0c03504. [DOI] [PubMed] [Google Scholar]; The superhydrophobic coating was introduced onto N95 respirators to prohibit droplets from accumulating on the respirator surface.
- 53.Zhong H., Zhu Z., Lin J., Cheung C.F., Lu V.L., Yan F., et al. Reusable and recyclable graphene masks with outstanding superhydrophobic and photothermal performances. ACS Nano. 2020;14:6213–6221. doi: 10.1021/acsnano.0c02250. [DOI] [PubMed] [Google Scholar]
- Huang L., Xu S., Wang Z., Xue K., Su J., Song Y., et al. Self-reporting and photothermally enhanced rapid bacterial killing on a laser-induced graphene mask. ACS Nano. 2020;14:12045–12053. doi: 10.1021/acsnano.0c05330. [DOI] [PubMed] [Google Scholar]; This work designed a graphene-based mask with the photothermal effect, achieving a 99.998% bacterial killing efficiency within 10 min.
- Fischer E.P., Fischer M.C., Grass D., Henrion I., Warren W.S., Westman E. Low-cost measurement of facemask efficacy for filtering expelled droplets during speech. Sci Adv. 2020;6 doi: 10.1126/sciadv.abd3083. [DOI] [PMC free article] [PubMed] [Google Scholar]; A rapid evaluation of mask performance under different conditions could be achieved through an inexpensive measurement setup.
- 56.Amirav I., Oron A., Tal G., Cesar K., Ballin A., Houri S., et al. Aerosol delivery in respiratory syncytial virus bronchiolitis: Hood or face mask? J Pediatr. 2005;147:627–631. doi: 10.1016/j.jpeds.2005.05.035. [DOI] [PubMed] [Google Scholar]
- 57.Hu M., Yin L., Low N., Ji D., Liu Y., Yao J., et al. Zeolitic-imidazolate-framework filled hierarchical porous nanofiber membrane for air cleaning. J Membr Sci. 2020;594:117467. [Google Scholar]
- 58.Zhong G., Liu D., Zhang J. The application of ZIF-67 and its derivatives: adsorption, separation, electrochemistry and catalysts. J Mater Chem. 2018;6:1887–1899. [Google Scholar]
- 59.Pang S.H., Han C., Sholl D.S., Jones C.W., Lively R.P. Facet-specific stability of ZIF-8 in the presence of acid gases dissolved in aqueous solutions. Chem Mater. 2016;28:6960–6967. [Google Scholar]
- 60.Zhang Y., Yuan S., Feng X., Li H., Zhou J., Wang B. Preparation of nanofibrous metal–organic framework filters for efficient air pollution control. J Am Chem Soc. 2016;138:5785–5788. doi: 10.1021/jacs.6b02553. [DOI] [PubMed] [Google Scholar]
- 61.Zhu Q., Tang X., Feng S., Zhong Z., Yao J., Yao Z. ZIF-8@SiO2 composite nanofiber membrane with bioinspired spider web-like structure for efficient air pollution control. J Membr Sci. 2019;581:252–261. [Google Scholar]
- 62.Liu C., Hsu P.-C., Lee H.-W., Ye M., Zheng G., Liu N., et al. Transparent air filter for high-efficiency PM2.5 capture. Nat Commun. 2015;6:6205. doi: 10.1038/ncomms7205. [DOI] [PubMed] [Google Scholar]
- 63.Lipp A., Edwards P. Disposable surgical face masks for preventing surgical wound infection in clean surgery. Cochrane Database Syst Rev. 2016 doi: 10.1002/14651858.CD002929.pub3. [DOI] [PubMed] [Google Scholar]
- 64.Xu J., Liu C., Hsu P.C., Liu K., Zhang R., Liu Y., et al. Roll-to-roll transfer of electrospun nanofiber film for high-efficiency transparent air filter. Nano Lett. 2016;16:1270–1275. doi: 10.1021/acs.nanolett.5b04596. [DOI] [PubMed] [Google Scholar]
- 65.Zhang R., Liu C., Hsu P.C., Zhang C., Liu N., Zhang J., et al. Nanofiber air filters with high-temperature stability for efficient PM2.5 removal from the pollution sources. Nano Lett. 2016;16:3642–3649. doi: 10.1021/acs.nanolett.6b00771. [DOI] [PubMed] [Google Scholar]
- 66.Khalid B., Bai X., Wei H., Huang Y., Wu H., Cui Y. Direct blow-spinning of nanofibers on a window screen for highly efficient PM2.5 removal. Nano Lett. 2017;17:1140–1148. doi: 10.1021/acs.nanolett.6b04771. [DOI] [PubMed] [Google Scholar]
- 67.Yang A., Cai L., Zhang R., Wang J., Hsu P.C., Wang H., et al. Thermal management in nanofiber-based face mask. Nano Lett. 2017;17:3506–3510. doi: 10.1021/acs.nanolett.7b00579. [DOI] [PubMed] [Google Scholar]
- 68.Javid A., Kumar M., Yoon S., Lee J.H., Han J.G. Size-controlled growth and antibacterial mechanism for Cu: C nanocomposite thin films. Phys Chem Chem Phys. 2017;19:237–244. doi: 10.1039/c6cp06955j. [DOI] [PubMed] [Google Scholar]
- 69.Hiragond C.B., Kshirsagar A.S., Dhapte V.V., Khanna T., Joshi P., More P.V. Enhanced anti-microbial response of commercial face mask using colloidal silver nanoparticles. Vacuum. 2018;156:475–482. [Google Scholar]
- 70.Ramyadevi J., Jeyasubramanian K., Marikani A., Rajakumar G., Rahuman A.A. Synthesis and antimicrobial activity of copper nanoparticles. Mater Lett. 2012;71:114–116. [Google Scholar]
- 71.Schabes-Retchkiman P.S., Canizal G., Herrera-Becerra R., Zorrilla C., Liu H.B., Ascencio J.A. Biosynthesis and characterization of Ti/Ni bimetallic nanoparticles. Opt Mater. 2006;29(1):95–99. [Google Scholar]
- 72.Lellouche J., Friedman A., Lahmi R., Gedanken A., Banin E. Antibiofilm surface functionalization of catheters by magnesium fluoride nanoparticles. Int J Nanomed. 2012;7:1175–1188. doi: 10.2147/IJN.S26770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ganewatta M.S., Tang C. Controlling macromolecular structures towards effective antimicrobial polymers. Polymer. 2015;63:A1–A29. [Google Scholar]
- 74.Gong H., Liao M., Hu X., Fa K., Phanphak S., Ciumac D., et al. Aggregated amphiphilic antimicrobial peptides embedded in bacterial membranes. ACS Appl Mater Interfaces. 2020;12:44420–44432. doi: 10.1021/acsami.0c09931. [DOI] [PubMed] [Google Scholar]
- 75.Gong H., Sani M.A., Hu X., Fa K., Hart J.W., Liao M., et al. How do self-assembling antimicrobial lipopeptides kill bacteria? ACS Appl Mater Interfaces. 2020 doi: 10.1021/acsami.0c17222. [DOI] [PubMed] [Google Scholar]
- Karim N., Afroj S., Lloyd K., Oaten L.C., Andreeva D.V., Carr C., et al. Sustainable personal protective clothing for healthcare applications: a review. ACS Nano. 2020;14:12313–12340. doi: 10.1021/acsnano.0c05537. [DOI] [PMC free article] [PubMed] [Google Scholar]; This review provided a systematic overview of protective medical fabric development and the perspective of next generation personal protective equipment.
- Yuan Z.C., Li W., Wu L., Huang D., Wu M., Hu B. Solid-phase microextraction fiber in face mask for in vivo sampling and direct mass spectrometry analysis of exhaled breath aerosol. Anal Chem. 2020;92:11543–11547. doi: 10.1021/acs.analchem.0c02118. [DOI] [PubMed] [Google Scholar]; This work provided a screening method to detect some respiratory diseases from face mask wearing.