Abstract
Purpose:
HIV pre-exposure prophylaxis (PrEP) is underutilized by adolescent and young adult women (AYAW), especially in the Southern US. Family planning (FP) clinics are potentially ideal PrEP delivery sites for AYAW, but little is known about their PrEP services. We describe models of PrEP care in Title X FP clinics in the South and explore clinic resources that are needed to facilitate PrEP provision.
Methods:
Providers and administrators from 38 clinics participated in qualitative interviews. We assessed five steps of PrEP care: 1) HIV risk assessment, 2) PrEP education, 3) Laboratory testing, 4) PrEP prescription, and 5) PrEP monitoring.
Results:
Among 38 clinics, 23 conducted at least one step and were classified into three models. Model 1 (n=8) and Model 2 (n=4) clinics provided up to Steps 1 and 2, respectively, but referred to an external PrEP provider. Model 3 clinics (n=11) conducted all steps. Few barriers were identified for Step 1; utilizing an HIV risk assessment tool was a key facilitator. PrEP educational materials facilitated Step 2; clinics not providing education believed they could easily do so with training and educational resources. Funding- and staff-related resource barriers were noted for Steps 3–5, including costs of lab tests and lack of time for longitudinal visits.
Conclusions:
PrEP-providing publicly-funded FP clinics in the Southern US use referral services for many steps of PrEP care, which introduce patient burden. Increasing onsite PrEP services will require addressing concerns related to training, educational materials, cost, and staffing.
Keywords: HIV/AIDS, PrEP, Family Planning, Adolescents, Implementation
Youth ages 13 to 24 comprise approximately 20% of the nearly 40,000 people diagnosed with HIV annually in the United States (US) [1]. 1 in 8 new HIV diagnoses among this age group occur in adolescent and young adult women (AYAW) [1], and rates of new diagnoses among AYAW are highest in Southern states compared to all other regions of the US [1]. HIV Pre-exposure prophylaxis (PrEP) is a safe and effective HIV prevention intervention that the US Food and Drug Administration approved in 2012 [2]. Open label studies and demonstration projects have found that PrEP delivery is feasible in “real world” settings, including for AYAW [3–5].
Consequently, dissemination and implementation efforts are now focused on bringing PrEP to scale in the US [6]. Despite these efforts, PrEP awareness and use among AYAW in the US remain low [7–10], while high levels of awareness and increased use among men have been recently documented [11]. In the last quarter of 2017, women were less than 5% of PrEP users, and women and adolescents had significantly lower levels of PrEP use relative to epidemic need [12].
Low access to PrEP providing clinics [13] is a major potential barrier to PrEP use among AYAW in the South, particularly since the degree to which PrEP is provided in settings where most AYAW receive health care (i.e., women’s health and family planning clinics) is largely unknown. Models of PrEP care currently exist in sexually transmitted infection (STI) treatment clinics, community-based organizations, pharmacy-based programs, and community health centers [14]. However, family planning (FP) clinics in high HIV incidence settings (such as much of the Southern US) are potentially ideal for expanding PrEP care for AYAW, since they are already utilized by sexually active AYAW for sexual health services, including HIV testing and prevention counseling. Further, most AYAW use and trust women’s health clinics for sexual health services, especially AYAW ages 18–29 [15, 16]. Title X-funded FP clinics are an ideal setting for integrating PrEP into FP services given that they are important safety net sources of care for AYAW, particularly in regions without Medicaid expansion, which closely overlap with regions that would most benefit from expansion of HIV prevention services [17]. Title X FP clinics serve nearly 4 million clients, including 1.5 million in the South [18]. 87% of the clients are women, 17% are under 20 years of age, and 46% are 20 to 29 years of age [18]. While clinical guidelines for women’s health providers have recently incorporated recommendations for PrEP [19], to date, there has not been widespread integration of PrEP services into Title X FP clinics, especially in the South [20, 21].
PrEP care based on clinical guidelines is a multi-stepped process [22]. The steps in PrEP care include: 1) assessing a patient’s HIV risk, 2) providing PrEP education and counseling to determine interest in PrEP, 3) assessing a patient’s medical eligibility for PrEP through laboratory testing, 4) prescribing PrEP, and 5) follow-up and monitoring. Due to organization-level differences in structure, services provided, partnerships, capacity, and resources, clinics may implement different models of PrEP care which may include provision of a varying number of these steps onsite versus through referral [23]. Thus, FP clinics may vary considerably in their overall PrEP care models. The purpose of this study is to understand current models of PrEP care utilized in safety net FP clinics in the South and to explore clinic resources that facilitate PrEP provision, which will ultimately inform strategies to scale-up PrEP in these important women’s health care settings.
METHODS
Study Design
The overall study utilized an explanatory, sequential mixed-methods research design [24] to explore models of PrEP care and barriers/facilitators to PrEP provision in FP clinics across the South. Quantitative surveys were administered online in Spring 2018 [25], followed by qualitative interviews to gain an in-depth understanding of the quantitative data captured. This study focuses on the results of the qualitative interviews. Results of the quantitative surveys are described elsewhere [20]. Qualitative interviews were conducted between March and July 2018. This study was based at Emory University and the Emory IRB approved the study protocol.
Study Participants and Recruitment
We invited FP providers and clinic administrators from Title X-funded clinics in the 18 states that comprise the Southern U.S. (DHHS regions III [Mid-Atlantic], IV [Southeast], and VI [Southwest]) to participate. FP providers were considered individuals who have the potential ability to prescribe, counsel, or screen for PrEP. Clinic administrators were individuals who served in an administrative oversight capacity over the Title X activities in their clinic.
As a part of the survey for this study [25], participants were asked to indicate willingness to participate in a follow-up qualitative phone interview. Individuals were uniquely selected based on various factors (i.e., purposive sampling), including whether their clinic prescribes PrEP, state, DHHS region, clinic classification (i.e. health department, community clinic, etc.), and urbanicity. Interviews took approximately 45 minutes to one hour and participants received a $50 gift card upon completion.
Of the 519 individuals that completed the survey, 45 participants (34 providers and 11 administrators) from 38 unique clinics completed a qualitative interview. There were 7 clinics that had 2 interviewees participate. For the purposes of this clinic-level study, interview data from participants in the same clinic were combined to gain a more robust picture of clinic operations and PrEP procedures.
Measures
Semi-structured interviews sought to assess potential barriers and facilitators to integrating PrEP into clinic services using implementation-focused constructs from the Consolidated Framework for Implementation Research (CFIR) [26]. The guide consisted of 8 primary domains: HIV Priority, PrEP Priority, Capacity & Implementation, Resources, Adoption & Decision Making around New Practices, Champions, Trainings, and External Factors. Interviews were conducted by trained research staff; interviews were recorded and transcribed verbatim.
Classifying Models of PrEP Care
Five steps of PrEP care were assessed through the interviews (Figure 1): Step 1) HIV risk assessment, Step 2) PrEP education, Step 3) laboratory assessment for PrEP eligibility, Step 4) PrEP prescription, and Step 5) PrEP monitoring. During Step 1, patients are screened for HIV risk factors and tested for HIV. During Step 2, patients are educated about PrEP as well as assessed on their interest and ability to adhere to PrEP. During Step 3, patients are assessed for any signs and symptoms of HIV infection and receive laboratory testing for kidney function, Hepatitis B and C, pregnancy, and other STIs. Step 4 involves prescribing PrEP to patients who are eligible (based on HIV risk factors, medical eligibility, and interest in PrEP). This step also may involve enrolling the patient in insurance or medication assistance programs to ensure they can pay for PrEP. Step 5 involves follow-up visits every 3 months for HIV testing, adherence counseling, risk reduction support, side effect assessment, pregnancy testing, STI testing, and kidney function testing. After reading the qualitative interviews from the 38 clinics, we classified each clinic based on which steps of PrEP care were implemented to identify PrEP models.
Figure 1.
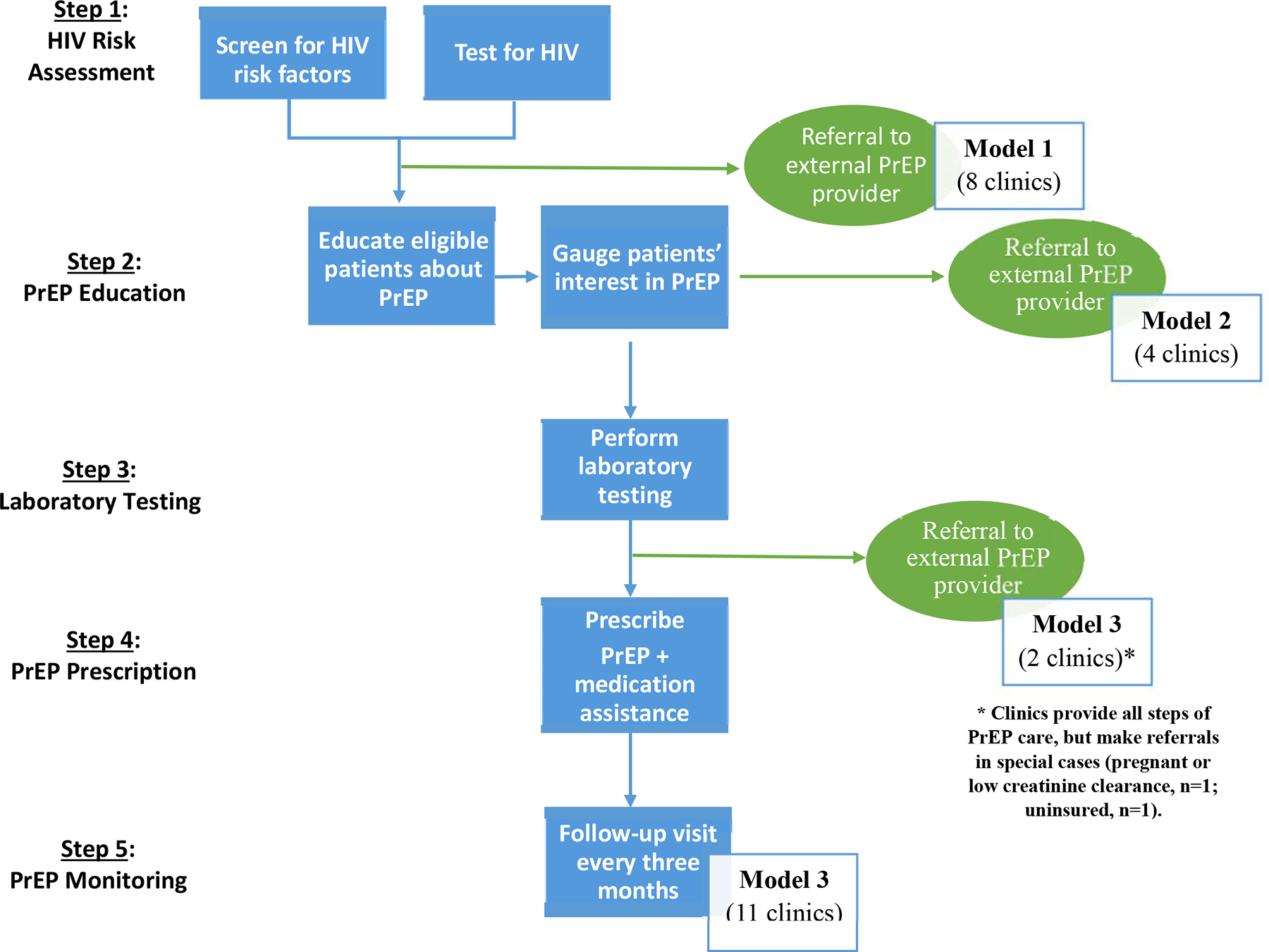
PrEP care models in Title X family planning clinics in the Southern US (analysis of n=23 clinics)
Data Analysis
We ran descriptive statistics on the characteristics of the 38 clinics (stratified by model of PrEP care) including location (large metropolitan, medium metropolitan, and small/non-metropolitan), clinic type (health department, specialized FP, FQHC, community, hospital, and other), region (III, IV, and VI), services (FP only or both FP and primary care), staff to enroll patients in insurance (yes or no), onsite pharmacy (yes or no), and onsite lab (yes or no). We also performed descriptive statistics on characteristics of the clinic’s county, including percent of the population under 200% of the poverty level, percent of the population by race, percent of the population who are uninsured, and HIV prevalence [27].
Using NVivo 12, we employed standard qualitative data analyses methods including reading of transcripts, creation of a codebook, coding and consensus meetings [28]. In the qualitative interviews, clinic resources emerged as the most salient factor for PrEP implementation and therefore is the focus of this analysis. The codebook was created based on clinic resources (e.g. money, training, education, physical space, and time) the participants needed to conduct each step of PrEP care. We entered the resources into an Excel matrix by model and site and then assessed the direction (i.e. barrier or facilitator) and strength (i.e. likelihood of impacting PrEP delivery) of the resource across clinics and model type. In order to ensure that codes were being applied to the data accurately and consistently, two independent analysts separately coded, and then compared codes and resolved all discrepancies through discussion. Resource-related barriers and facilitators that were salient across clinics were summarized for each step of the PrEP cascade, by model type. Exemplar quotes that are presented in the results were selected because of their ability to represent the experiences of our sample of clinics.
RESULTS
PrEP Models
Out of the 38 clinics that participated in the qualitative interviews, 23 clinics conducted at least one step PrEP care (the 15 clinics that provided no PrEP-related services [39%] were excluded from further analyses). Among the 23 clinics that provided PrEP-related services, we identified three different models of PrEP care (see Figure 1). Model 1 clinics (n=8) only conducted Step 1 of PrEP care and then referred potential candidates to an external PrEP provider. Model 2 clinics (n=4) conducted steps 1 and 2 of PrEP care: If they believed the patient was a good candidate for PrEP based on HIV risk assessments and PrEP education, Model 2 clinics would then refer patients to an external PrEP provider. Model 3 clinics (n=11) conducted all steps of PrEP care. Two of the Model 3 clinics indicated that they may refer patients to an external PrEP provider in special circumstances, including if the patient is pregnant, ineligible based on creatinine clearance, or uninsured.
See Table 1 for a description of clinic characteristics. Notably, Model 1 clinics had the highest representation of clinics from non-metropolitan areas, the highest percent county-level poverty, and the highest county-level HIV prevalence. Model 2 clinics had the highest representation of clinics from large metropolitan areas, highest county-level percent non-White individuals, and were more commonly from Region IV (Southeast). Model 3 clinics had a higher representation of clinics from medium metropolitan locations, more commonly had a pharmacy onsite, and were more commonly from Region III-Mid-Atlantic.
Table 1.
Clinical characteristics, by model of PrEP care
| Total (N=23) n (%) |
Model 1a (N=8) n (%) |
Model 2b (N=4) n (%) |
Model 3c (N=11) n (%) |
|
|---|---|---|---|---|
| Clinic Location | ||||
| Large Metro | 11 (47.8) | 3 (37.5) | 3 (75.0) | 5 (45.5) |
| Medium Metro | 7 (30.0) | 2 (25.0) | 1 (25.0) | 4 (36.4) |
| Small/Non-metro | 5 (21.7) | 3 (37.5) | 0 (0.0) | 2 (18.2) |
| Clinic Type | ||||
| Health Department | 12 (52.2) | 5 (62.5) | 3 (75.0) | 4 (36.4) |
| Family Planning | 4 (17.4) | 1 (12.5) | 0 (0.0) | 3 (27.3) |
| FQHC | 3 (13.0) | 0 (0.0) | 0 (0.0) | 3 (27.3) |
| Community | 2 (8.7) | 1 (12.5) | 1 (25.0) | 0 (0.0) |
| Hospital | 1 (4.3) | 1 (12.5) | 0 (0.0) | 0 (0.0) |
| Other | 1 (4.3) | 0 (0.0) | 0 (0.0) | 1 (9.0) |
| Regiond | ||||
| III | 10 (43.4) | 3 (37.5) | 1 (25.0) | 6 (50.0) |
| IV | 8 (34.7) | 3 (37.5) | 3 (75.0) | 2 (16.7) |
| VI | 5 (21.7) | 2 (25.0) | 0 (0.0) | 3 (25.0) |
| Services Provided | ||||
| Family Planning | 16 (69.6) | 5 (62.5) | 3 (75.0) | 8 (72.7) |
| Family Planning + Primary Care | 7 (30.4) | 3 (37.5) | 1 (25.0) | 3 (27.3) |
| Payment Assistancee | ||||
| Yes | 16 (69.6) | 7 (87.5) | 4 (100) | 5 (45.5) |
| No | 7 (30.4) | 1 (12.5) | 0 (0.0) | 6 (54.5) |
| Onsite Pharmacy | ||||
| Yes | 14 (60.9) | 5 (62.8) | 1 (25.0) | 8 (72.7) |
| No | 9 (39.1) | 3 (37.5) | 3 (75.0) | 3 (27.2) |
| Onsite Lab | ||||
| Yes | 10 (43.5) | 3 (37.5) | 2 (50.0) | 5 (45.5) |
| No | 10 (43.5) | 5 (62.5) | 1 (25.0) | 4 (36.4) |
| Unknown | 3 (13.0) | 0 (0.0) | 1 (25.0) | 2 (18.2) |
| Percent Poverty, mean (min, max)f | 16.8 (5.9, 22.7) | 18.2 (14,4, 22.7) | 14.7 (8.8, 18.0) | 16.6 (5.9, 21.1) |
| Percent Uninsured, mean (min, max)f | 11.3 (4.3,21.1) | 11.1 (6.7, 14.0) | 12.0 (6.9, 16.9) | 11.2 (4,6, 21.1) |
| HIV Prevalence Rate, mean (min, max)f | 724.6 (57, 2590) | 811.6 (67, 2307) | 635.0 (106, 1167) | 695.6 (57, 2590) |
| Percent of Population by Race, mean (min, max)f | ||||
| White | 64.5 (29.6, 97.9) | 63.7 (29.6, 96.4) | 56.9 (33.3, 86.3) | 67.7 (38.5, 97.9) |
| Black | 23.9 (0.6, 63.7) | 24.4 (1.1, 63.7) | 33.0 (5.0, 54.3) | 20.2 (0.6, 50.7) |
| Asian | 2.7 (0.2, 5.6) | 2.3 (0.5, 5.6) | 3.4 (1.4, 5.1) | 2.8 (0.2, 6.2) |
| American Indian/ Alaska Native | 0.6 (0.2, 4.8) | 1 (0.2, 4.8) | 0.4 (0.2, 0.5) | 0.5 (0.2, 1.2) |
| Other | 5.8 (0.2, 21.9) | 6.0 (0.2, 17.2) | 4.2 (2.2, 6.2) | 6.3 (0.4, 21.9) |
| More than 1 race | 2.4 (0.7, 4.4) | 2.5 (1.5, 4.4) | 2.1 (1.1, 2.6) | 2.5 (0.7, 3.2) |
Clinics refer to an external PrEP provider after step 1
Clinics refer to an external PrEP provider during step 2
Clinics conduct the all steps of PrEP delivery
Department of Health and Human Services regions III (Washington D.C., Delaware, Maryland, Pennsylvania, Virginia, West Virginia), IV (Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, Tennessee), and VI (Arkansas, Louisiana, New Mexico, Oklahoma, Texas)
Onsite staff to help enroll patients in Medicaid/insurance programs/payment assistance programs
Based on AIDSVu 2015 data from clinic’s county
Barriers and Facilitators to PrEP Care
The following sections highlight the most prominent resource-related considerations for implementing each step of PrEP care (see Tables 2 and 3). Table 2 depicts the prevalence of each resource across clinics in the sample. Table 3 lists the resources required for each step of PrEP care, as well as an exemplar quote that extends the results presented below.
Table 2.
Summary of available and needed resources for each step in PrEP care, by model of PrEP care*
| Resource Available | Resource Needed | |||||
|---|---|---|---|---|---|---|
| Model 1 (N=8) n (%) |
Model 2 (N=4) n (%) |
Model 3 (N=11) n (%) |
Model 1 (N=8) n (%) |
Model 2 (N=4) n (%) |
Model 3 (N=11) n (%) |
|
| Step 1: HIV Risk Assessment | ||||||
| HIV Risk Assessment Tool | 2 (25.0) | 3 (75.0) | 5 (45.5) | 1 (12.5) | 1 (25.0) | 1 (9.0) |
| Assessment Support Staff | 1 (12.5) | 2 (50.0) | 3 (27.2) | 3 (37.5) | - | - |
| Risk Assessment Tool Integrated into EMR | 1 (12.5) | - | 2 (18.2) | 1 (12.5) | 1 (25.0) | - |
| Step 2: PrEP Education | ||||||
| Patient Educational Materials | 1 (12.5) | 3 (75.0) | 2 (18.2) | 3 (37.5) | - | - |
| Educational Support Staff | 4 (50.0) | - | 2 (18.2) | 1 (12.5) | - | 2 (18.2) |
| Staff Training and Education | - | 1 (25.0) | 3 (27.2) | 2 (25.0) | - | - |
| Step 3: Lab Assessment for PrEP Eligibility | ||||||
| Laboratory (Onsite or Offsite) | 5 (62.5) | - | 4 (36.4) | - | - | - |
| Staff Training and Education | 3 (37.5) | - | 6 (54.5) | 4 (50.0) | 1 (25.0) | - |
| Funding for Lab Tests | - | - | - | 5 (62.5) | - | 2 (18.2) |
| Step 4: PrEP Prescription | ||||||
| Funding for Prescription | - | - | 3 (27.2) | 3 (37.5) | - | - |
| Insurance Navigators | - | 1 (25.0) | 5 (45.5) | 5 (62.5) | - | 2 (18.2) |
| Step 5: PrEP Monitoring | ||||||
| Staffing | 1 (12.5) | - | 1 (9.0) | 1 (12.5) | - | 2 (18.2) |
| Appointment Reminder/Follow-up System | - | - | 3 (27.2) | 1 (12.5) | - | - |
Model 1 clinics refer to an external PrEP provider after Step 1; Model 2 clinics refer to an external PrEP provider after Step 2; Model 3 clinics conduct all steps of PrEP delivery.
Table 3.
Resource-Related Barriers and Facilitators to PrEP Implementation, by Step of PrEP Care.
| Resource | Exemplar Quote |
|---|---|
| Step 1: Assessing HIV Risk | |
| Formal, standardized HIV risk assessment tool | “So on their risk assessment they usually have to fill out – how many partners they’ve had, if they’ve had any STDs in the past six months, what types of sex that they’re having, are they currently having sex with someone who’s HIV positive? – so that risk assessment normally is a good guide on letting me know if they will be a good candidate for PrEP from the jump before I even start discussing anything with them.” (Clinic 15, Model 3) |
| Available staff to conduct HIV risk assessment prior to appointment | “The nurses do the assessment. We don’t have any sheets that we pass out before they get there. So during the intake is when all [HIV risk] is assessed and put into the computer and then the nurses talk to them. And then when I go in the room after reviewing the chart, I look at the answers, and then I go in and reinforce or teach or educate depending on what’s going on.” (Clinic 9, Model 2) |
| Incorporation of HIV risk assessment in electronic medical records | “We have electronic medical records, so if they could… get to the point where they did [HIV risk assessment] actually in an electronic history, then it could just populate it in the chart.” (Clinic 4, Model 1) |
| Step 2: PrEP Education | |
| Patient educational materials | “We have some really good tools in terms of patient education sheets on PrEP that we can provide to patients that go over what the potential risks are, what the side effects are, what the benefits are. So our clinicians aren’t having to just come up with that out of thin air or remember it, memorize from our protocol. So we’ve got, basically, an education sheet that’s right in front of them that they can be giving to the patient as they go through it.” (Clinic 18, Model 3) |
| Availability of health educators/support staff | “The medical assistants are well informed. And our medical assistants do a lot of the education for our patients and counseling for our patients. ” (Clinic 14, Model 3) |
| Staff PrEP training and education | “I mean, I know a lot about HIV. I’ve been here a while, but some of the other staff wouldn’t, and I think that all the nurses in this clinic should be at least trained if we did implement this, to know what it’s about.” (Clinic 8, Model 1) |
| Step 3: Lab Assessment for PrEP Eligibility | |
| Access to laboratory | “In terms of testing for kidney function, hepatitis, those are send out tests. So we can draw blood right there in the clinic. We don’t have to send [patients] out to get their blood drawn. We’ll draw it, and we’ll send it off [to external lab].” (Clinic 22, Model 3) |
| Staff training and education on lab tests | “We talked to the lab and then we did a training amongst ourselves after we got that information. The rest of the tests - they’re easy. We all have had to take classes for the HIV so we all know how to do that test and the other ones you just draw the blood in the proper tube and it goes to the state. The BMP [Basic Metabolic Profile] was the only thing different that we hadn’t been doing. And since that goes to a private lab the state doesn’t do it, we just had to learn to process.” (Clinic 22, Model 3) |
| Funding for lab tests | “And then, if we’re gonna do lab tests, we would have to know who’s gonna pay for that. Like, in our Title X funding, I’m not sure the Title X grant is gonna pay for that. We do have the [CLINIC] system to back us up, but then they have to have a separate financial assessment to be eligible for what they’re gonna pay for their labs. We have a lab here that they could just walk next door and get their blood drawn, but who’s gonna pay for that?” (Clinic 4, Model 1) |
| Step 4: Prescribe PrEP | |
| Funding for PrEP prescription | “The thing that’s made it easy for us is just the state paying for it [PrEP prescriptions] for one thing and it being free to the patients and having the PrEP coordinator too has definitely helped too. We don’t have to deal with any insurance rejections or denials or anything of that sort and we don’t have to deal with copays because everything is basically free. I don’t think it will always be that way. I think that eventually, they’re [the state] gonna run out of money or they’re gonna decide that they should bill patients that have insurance or something like that. But right now and ever since we’ve started doing PrEP, it’s been this way that everything is free, including all the lab tests too. So we haven’t really had any barriers, any significant barriers to implementing it.” (Clinic 16, Model 3) |
| Insurance navigators | “We have an eligibility department that, once they call in, we screen them first before they come in to see, you know, what they’re coming for and what, if they have insurance. And once we do the over the phone screening, then they—when we find out they don’t have insurance, then we’ll set them up an appointment with eligibility and then they will sit with them prior to the doctor and, you know, I guess bring in certain paperwork like proof of income, proof of residency, photo ID and whatever else they may need.” (Clinic 15, Model 3) |
| Step 5: PrEP Monitoring | |
| Clerical scheduling staff | “Mainly just appointment reminders, clerical staff to help with that, sending out appointment reminders and calling patients to remind them of appointments and that sort of thing.” (Clinic 16, Model 3) |
| Automated scheduling/appointment reminder systems | “We have an appointment reminder system, like an automatic call. They made their appointment and then they missed it and so that will prompt the system to say, “Hey, you’ve missed your appointment. Please call and reschedule.” (Clinic 20, Model 3) |
Step 1: Assessing HIV risk
Model 1, 2, and 3 clinics all collected information about patients’ sexual behaviors and conducted HIV tests. Many clinics utilized an HIV risk assessment tool, which asked patients about their sexual partners, condom use, STD history, and injection drug use. These tools enabled providers to systematically identify which patients may be candidates for PrEP. In most cases, these tools were generated by the clinics to assess sexual health (since validated tools do not exist) and were embedded into general intake assessments that patients completed prior to their visit. Providers believed that assessments should be completed prior to seeing the clinician, so that clinicians had more time to discuss the results during the patient’s appointment. Some clinics collected information on risk behaviors using a paper and pencil questionnaire, which was completed by patients in the waiting area. In other clinics, nurses or medical assistants administered the tool during a one-on-one conversation with the patient and entered their answers into an electronic form. Having the assessment integrated into the electronic medical records (EMR) also facilitated providers’ access to assessment results and reduced the need for data entry. Overall, clinics identified very few barriers to implementing this first step of PrEP care; however, having a risk assessment tool, having staff available to assess patients prior to seeing a clinician, and integrating the assessment into EMR were all facilitators.
Step 2: PrEP Education
Model 2 and 3 clinics successfully integrated PrEP education into their routine procedures. For these clinics, PrEP educational materials and handouts helped facilitate the process, by serving as a resource for patients and helping to guide the provider through the educational session. In some clinics, PrEP education was provided by medical assistants or health educators, which limited the burden on clinicians. Even though they do not currently conduct step 2, Model 1 clinics believed they had the capacity to adopt PrEP education, if they had access to educational materials for patients. Model 1 clinics also wanted staff to be trained on HIV and PrEP before providing any patient education.
Step 3: Laboratory Assessment for PrEP Eligibility
Model 3 clinics conducted this step of PrEP care. They either conducted the tests at an onsite or external laboratory. Before implementing this step, clinics conducted staff trainings on the procedures for drawing the tests and sending them to the lab, which facilitated a smooth transition. Model 3 clinics noted that they were already familiar with many of the tests required for PrEP, so staff training was not a large burden. Also, because many of the Model 3 clinics received funding for PrEP (through grants or state-level PrEP assistance programs), they encountered few cost-related barriers to conducting the laboratory tests. However, Model 1 and 2 clinics were concerned they would not be able to offer lab testing without additional funding, and they believed that referring to an external PrEP provider for lab testing and continued care was the best option for them currently.
Step 4: Prescribe PrEP
In our sample, Model 3 clinics conducted step 4, while Model 1 and 2 clinics did not. For Model 3 clinics, a critical facilitator for step 4 was acquiring grant funding for PrEP medications or being located in a state that offers PrEP assistance programs (i.e., states are billed for PrEP costs, so medications, visits, and labs are free to patients). Clinics without this funding, utilized staff, such as insurance navigators, to help enroll patients in Medicaid (which covers the cost of PrEP) or pharmaceutical medication assistance programs (which covers medication expenses for eligible patients). However, Model 1 and 2 clinics believed that their lack of funding and insurance navigators (coupled with the high cost of PrEP care) would limit patient access to PrEP at their clinic.
Step 5: PrEP Monitoring
Only Model 3 clinics conducted PrEP monitoring. The primary challenge Model 3 clinics reported was retaining patients in care, including patient adherence to PrEP medication and attendance at quarterly follow-up appointments. For Model 3 clinics, having clerical staff available to schedule appointments facilitated patient visits every 3 months. Additionally having automated scheduling systems and automatic patient reminders enhanced the feasibility of PrEP monitoring and decreased the burden on staff. Model 1 and 2 clinics felt that it would be possible for them to conduct follow-ups, but they were concerned that patients would not be compliant with appointments. They were also concerned that more staff would be needed to schedule and follow-up with patients.
DISCUSSION
Efforts to improve PrEP access for AYAW seeking sexual health care in Title X FP clinics in the Southern US are needed. We identified 3 current models of PrEP care in these clinics: a) HIV risk assessment followed by referral to an external PrEP provider (Model 1), HIV risk assessment and PrEP education followed by referral to an external PrEP provider (Model 2), and completion of all PrEP care steps onsite (Model 3). Most clinics fell into one of the two models that utilized referral for PrEP care, despite intentional sampling of individuals from PrEP-providing clinics. Since referral models introduce additional patient burden for accessing PrEP, increasing onsite PrEP services in Title X clinics will require addressing identified barriers to PrEP care. Alternatively, PrEP access could be enhanced for AYAW seeking care at Title X clinics by strengthening linkages to nearby PrEP-providing clinics and developing referral strategies that are acceptable for AYAW.
Notably, few barriers were identified for the first step (HIV risk assessment), but having a formal risk assessment tool, having the tool integrated into the EMR, and having support staff to administer the tool before the clinician appointment were key facilitators. Assessment of HIV risk has been noted to be a key challenge in PrEP care, particularly for AYAW. For US women, risk assessment tools that predict HIV acquisition risk do not exist, and CDC clinical practice guidelines may not adequately identify women who are at risk and motivated to use PrEP [29, 30]. Despite inadequacies with HIV risk assessment tools, they can serve as reminders to take a detailed sexual history [31, 32] and can guide clinicians in conversations about PrEP [7, 31, 32].
In addition, clinics not providing PrEP education believed they could easily do step 2 with training and patient educational materials. These findings add to those from an earlier nationwide survey indicating that FP clinicians reported lack of training as a key barrier to PrEP implementation [21]. In a recent study among FP providers in Atlanta, we observed significant increases in providers’ PrEP skills and knowledge after a single, 1 hour training [7]. Also, having health educators and educational materials to share with patients were key facilitators for providing PrEP education in the current study. Women-focused PrEP information tools have been developed, such as those shared online by HIVE at the University of California San Francisco (https://hiveonline.org/prevention4women) [33]. Thus, agencies that support the training and service delivery needs of Title X clinics should consider strengthening awareness and accessibility of PrEP educational materials.
However, substantial funding- and staff-related resource barriers were notable in the later steps of PrEP care (steps 3–5). Given that the South has a higher proportion of individuals living without health insurance than other US regions [34], and many states have not expanded Medicaid, resource barriers are likely exacerbated in this region. While the cost of PrEP medication and medical visits are frequently cited patient barriers to PrEP use [35, 36], clinics that service high proportions of uninsured AYAW, such as Title X clinics in the South, also have unique resource-related challenges to provide PrEP. Specifically, for clinics not conducting laboratory tests or prescribing PrEP, the cost of the laboratory tests, costs of PrEP prescriptions, and lack of dedicated insurance/cost navigation staff were frequently cited barriers. However, for clinics doing all steps, once they received training as well as funding to cover the costs of laboratory testing and PrEP prescriptions, they faced very few barriers to conducting the remaining steps of PrEP care. These findings indicate that scaling-up onsite PrEP in Southern states, which have high proportions of uninsured patients and high HIV prevalence, will require strengthening funding to offset costs of PrEP services.
In addition, emerging models of providing PrEP may also alleviate some of the identified barriers in the later steps of PrEP care. These include pharmacy-based PrEP [37], telemedicine for PrEP care [38], at-home PrEP services [39], and mobile PrEP delivery [40]. Nonetheless, to date, few of these emerging models of PrEP implementation have been investigated in the Southern US, and none have been adapted for or studied in AYAW. Therefore, optimizing access to PrEP for AYAW in the US in the short-term must include expansion of PrEP services within publicly-funded women’s health clinics in high HIV burden areas in the South
Our study has several limitations, including the use of a convenience sample, use of self-reported information, and lack of generalizability to other women’s health settings not located in the South. Nonetheless, a key strength of this study was the diversity in geographic location and clinic characteristics among our sample. The results of this study also provide critical insight into clinic-level resources that facilitate PrEP provision, which will inform strategies to scale-up PrEP services in Title X FP clinics. In our ongoing work, we are utilizing this qualitative research to inform implementation and evaluation of PrEP adoption in Title X clinics in the South. This study focuses on one important determinant of PrEP implementation (i.e., clinic resources), but future work will explore additional determinants, such as provider attitudes, leadership engagement, and implementation climate [20].
In conclusion, our study noted 3 different models of PrEP care among publicly-funded FP clinics in the Southern US, mostly requiring referral services for some of the steps of PrEP care. Resource concerns related to training, educational materials, cost, and staffing must be addressed to expand onsite PrEP availability in these otherwise ideal sites for AYAW to receive PrEP services. All Title X clinics should be provided with the support and resources (most of which are freely available) to provide universal PrEP education to their patients, particularly in the South, where the epidemic burden is high and PrEP awareness among AYAW remains low. In the absence of PrEP service offerings in the South, linkages between current women’s health and PrEP programs must be strengthened in the region, and alternative PrEP care models that occur outside of the clinic setting must also be adapted for and studied in AYAW.
Implications and Contribution:
This study describes the different models of PrEP care currently utilized by Title X-funded family planning clinics and identifies key barriers and facilitators to PrEP provision at each point in the care cascade. Results can inform PrEP implementation planning and strategies to overcome barriers in this setting.
Acknowledgments of funding and conflicts of interest:
This research was supported by the National Institutes of Health grant U24HD089880. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. J. Sales and A. Sheth received grant funding from Gilead Sciences, Inc, to Emory University for unrelated work. This work was also presented at the Society for Adolescent Health and Medicine (2020).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- [1].Centers for Disease Control and Prevention. HIV Surveillance Report, 2017. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html (accessed November 2019).
- [2].Fonner VA, Dalglish SL, Kennedy CE, et al. Effectiveness and safety of oral HIV preexposure prophylaxis for all populations. AIDS 2016; 30(12):1973–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Grant RM, Anderson PL, McMahan V, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Infect Dis 2014; 14(9): 820–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Liu AY, Cohen SE, Vittinghoff E, et al. Pre-exposure prophylaxis for HIV infection integrated with municipal- and community-based sexual health services. JAMA Int Med 2016; 176(1):75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Celum CL, Delany-Morethwe S, Baeten JM, et al. HIV pre-exposure prophylaxis for adolescent girls and young women in Africa: from efficacy trials to delivery. J Int AIDS Soc 2019; 22(S4):e25298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Fauci AS, Redfield RR, Sigounas G, et al. Ending the AIDS epidemic: a plan for the United States. JAMA 2019; 321(9): 844–845 [DOI] [PubMed] [Google Scholar]
- [7].Sales JM, Cwiak C, Haddad LB, Phillips A, Powell L, Tamler I, Sheth AN. Impact of PrEP training for family planning providers on HIV prevention counseling and patient interest in PrEP in Atlanta, Georgia. Journal of Acquired Immune Deficiency Syndrome 2019; 81(4):414–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Sales JM, Phillips AL, Tamler I, Munoz T, Sheth AN. Patient recommendations for PrEP information dissemination at family planning clinics in Atlanta, Georgia. Contraception 2019. January 31. doi: 10.1016/j.contraception.2018.12.008. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Patel AS, Goparaju L, Sales JM, et al. Brief report: PrEP eligibility among at-risk women in the Southern US: associated factors, awareness, and acceptability. Journal of Aquired immune Deficiency Syndrome 2019; 80(5):527–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Calabrese SK, Dovidio JF, Tekeste M, et al. HIV pre-exposure prophylaxis as a multidimensional barrier to uptake among women who attend planned parenthood. et al, Journal of Aquired immune Deficiency Syndrome 2018; 79(1): 46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Finlayson T, Cha S, Xia M. Change in HIV preexposure prophylaxis awareness and use among men who have sex with men – 20 urban areas, 2014 and 2017. MMWR 2019; 68(27): 597–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Siegler AJ, Mouhanna F, Giler RM, Weiss K, Pembleton E, Guest J, Jones J, Castel A, Yeung H, Kramer M, McCallister S, Sullivan PS. The prevalence of pre-exposure prophylaxis use and the pre-exposure prophylaxis-to-need ratio in the fourth quarter of 2017, United States. Ann Epidemiol 2018;28(12):841–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Seigler AJ, Bratcher A, Weiss KM, et al. Location location location: an exploration of disparities in access to publicly listed pre-exposure prophylaxis clinics in the United States. Ann Epidemiol 2018; 28(12): 858–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Mayer KH, Chan PA, Patel R, et al. Evolving models and ongoing challenges for HIV preexposure prophylaxis implementation in the United States. J Acquir Immune Defic Syndr 2018; 77(2): 119–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Auerbach JD, Kinsky S, Brown G, Charles V. Knowledge, attitudes, and likelihood of pre-exposure prophylaxis (PrEP) use among US women at risk of acquiring HIV. AIDS Patient Care STDs 2015;29(2):102–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Stormo AR, Saraiya M, Hing E, Henderson JT, Sawaya GF. Women’s clinical preventive services in the United States: Who is doing what? JAMA Intern Med 2014;174(9):1512–1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Jones RK, Sonfield A. Health insurance coverage among women of reproductive age before and after implementation of the affordable care act. Contraception 2016; 93(5): 386–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Fowler CI, Gable J, Wang J, Lasater B, & Wilson E (2019, August). Family Planning Annual Report: 2018 national summary. Research Triangle Park, NC: RTI International; Available at: https://opa.hhs.gov/sites/default/files/2020-07/title-x-fpar-2018-national-summary.pdf [Google Scholar]
- [19].Preexposure prophylaxis for the prevention of human immunodeficiency virus. Committee Opinion No. 595. American College of Obstetricians and Gynecologists. Obstet Gynecol 2014;123:1133–6. Reaffirmed, 2019. [DOI] [PubMed] [Google Scholar]
- [20].Sales JM, Escoffery C, Hussen SA, Tamler I, Powell L, Filipowicz T, Sanchez M, Mccumber M, Kwiatkowski E, Renshaw L, Psioda M, Haddad LB, Sheth AN. Factors influencing potential adoption of PrEP services in Title X-funded family planning clinics in the Southern United States. 10th IAS Conference on HIV Science (IAS 2019), Mexico City, Mexico, July 21–24, 2019. [Google Scholar]
- [21].Seidman D, Carlson K, Weber S, Witt J, Kelly PJ. United States family planning providers’ knowledge of and attitudes towards preexposure prophylaxis for HIV prevention: a national survey. Contraception 2016; 93(5):463–469. [DOI] [PubMed] [Google Scholar]
- [22].Centers for Disease Control and Prevention: US Public Health Service: Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 Update: a clinical practice guideline. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf. Published March 2018.
- [23].Malcolm N, Marx K, Hart J, Rollison J, Erickson C, Hall C, Johnson D & Moskosky S (2019). Decision-Making Guide for the Provision of PrEP Services in Title X-Funded Family Planning Service Sites. Rockville, MD: U.S. Department of Health and Human Services, Office of Population Affairs [Google Scholar]
- [24].Tashakkori A, Teddlie C. Sage handbook of mixed methods in social & behavioral research. Thousand Oaks, CA: Sage; 2010. [Google Scholar]
- [25].Sales JM, Escoffery C, Hussen SA, Haddad LB, Phillips A, Filipowicz T, Sanchez M, McCumber M, Rupp B, Kwiatkowski E, Psioda MA, Sheth AN. Integrating PrEP into Family Planning Services at Title X Clinics in the Southeastern US – Phase 1 (ATN 155). JMIR Research Protocols 2019;8(6):e12774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation science 2009;4(1):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].AIDSVu (aidsvu.org). Emory University, Rollins School of Public Health. [Google Scholar]
- [28].Miles MB, Huberman AM, Saldana J. Qualitative data analysis. Thousand Oaks, CA: Sage; 2014. [Google Scholar]
- [29].Sheth AN, Rolle CP, Gandhi M. PrEP in Women. Journal of Virus Eradication 2016;2(3):149–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Calabrese SK, Willie TC, Galvao RW, et al. Current US guidelines for prescribing HIV pre-exposure prophylaxis (PrEP) disqualify many women who are at risk and motivated to use PrEP. J Acquir Immune Defic Syndr 2019; 81 (4): 395–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Calabrese SK, Krakower DS, Willie TC, et al. US guideline criteria for human immunodeficiency virus preexposure prophylaxis: clinical considerations and caveats. Clin Infect Dis 2019; 69(5): 884–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Mullens TL, Lally M, Zimet G, Kahm JA. Clinician attitudes toward CDC interim pre-exposure prophylaxis (PrEP) guidance and operationalizing PrEP for adolescents. AIDS Patient Care STDs 2015; 29 (4): 193–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Collier KL, Colarossi LG, Sanders K. A PrEP information and self-screening tool for women. AIDS Educ Prev 2018; 30(1): 13–25. [DOI] [PubMed] [Google Scholar]
- [34].US Census Bureau. Health insurance coverage in the United States: 2017 [online data report]. 2018. Available at: https://www.census.gov/library/publications/2018/demo/p60-264.html. Last accessed: March 19, 2019.
- [35].Goparaju L, Praschan NC, Warren-Jeanpiere L, Experton LS, Young MA, Kassaye S. Stigma, partners, providers and costs: potential barriers to PrEP uptake among US women. J AIDS Clin Res 2017;8(9), pii: 730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Dobleki-Lewis S, Liu A, Feaster DJ, et al. Healthcare access and PrEP continuation in San Francisco and Miami. J Acquir Immune Defic Syndr 2017; 74(5): 531–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Tung EL, Thomas A, Eichner A, Shalit P. Implementation of a community pharmacy-based pre-exposure prophylaxis service: a novel model for pre-exposure prophylaxis care. Sex Health 2018;15(6):556–61. [DOI] [PubMed] [Google Scholar]
- [38].Hoth AB, Shafer C, Dillon DB, et al. Iowa TelePrEP: a public-health-partnered telehealth model for human immunodeficiency virus preexposure prophylaxis delivery in a rural state. Sex Trans Dis 2019; 46(8): 507–512. [DOI] [PubMed] [Google Scholar]
- [39].Siegler AJ, Mayer KH, Liu AY, Patel RR, Ahlschlager LM, Kraft CS, et al. Developing and assessing the feasibility of a home-based PrEP monitoring and support program. Clin Infect Dis 2019;68(3):501–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Doblecki-Lewis S, et al. PrEP on the Go! Implementation of Mobile PrEP, STI, and HIV Prevention Services in South Florida. IDWeek 2019, Abstract #1965. [Google Scholar]


