Abstract
Background:
Motoric Cognitive Risk (MCR) syndrome is characterized by cognitive complaints and slow gait speed in the absence of dementia. There is consistent evidence that it predicts dementia and premature mortality. Less is known about its antecedents, particularly the role of psychological function. Purpose in life is an aspect of well-being that reflects a goal-oriented and driven life that has been implicated in cognitive aging.
Objective:
To examine the cross-sectional association between purpose in life and MCR and to test the hypothesis that purpose is associated with lower risk of new cases of MCR over an up to 12-year follow-up.
Design:
Cross-sectional and longitudinal multi-cohort design.
Subjects:
Participants were from the Health and Retirement Study (HRS; N=6,785) and the National Health and Aging Trends Study (NHATS; N=5,665).
Methods:
Participants reported on their purpose in life and cognitive complaints and completed a walking speed assessment. Cognitive complaints and walking speed were assessed again up to 12 years later in HRS and up to 7 years later in NHATS.
Results:
Higher purpose in life was associated with a 33% lower risk of MCR concurrently (meta-analytic OR=.75; 95% CI=.62, .90, p=.002) and an about 26% lower risk of incident MCR longitudinally (meta-analytic HR=.77; 95% CI=.70, .84, p<.001). These associations were significant in each sample, were independent of sociodemographic covariates, and persisted after controlling for personality and health-related factors (depressive symptoms, physical activity, disease burden).
Conclusions:
Purpose in life is associated with lower risk of incident MCR, an association that replicated in two independent samples. Purpose is a malleable aspect of psychological function that is a promising target of intervention for healthier cognitive aging.
Keywords: Purpose in life, Pre-dementia, Risk syndrome, Cognitive impairment, Well-being
Introduction
Prior to the onset of cognitive impairment, individuals often complain of declines in their memory or other cognitive functions1 and many have motor limitations, such as slow walking speed2. The combination of these two factors has been identified as a pre-dementia risk syndrome3–5. Specifically, Motoric Cognitive Risk (MCR) syndrome is the combination of subjective cognitive complaints and slow gait speed in the absence of concurrent cognitive impairment3. MCR has been associated with increased risk of dementia4 and premature mortality5. Although sociodemographic factors (e.g., age, education), chronic disease (e.g., hypertension, diabetes), and brain volume (e.g., low total gray matter) have been implicated in the development of MCR, there is still little understanding of the risk factor for its development6. Psychological factors, including a history of depression7 and personality8, 9, have been implicated recently in assessments of MCR. There may be other aspects of psychological function that also contribute to the development of new cases of MCR over time. Purpose in life is one such psychological factor that may be associated with lower risk of MCR.
Purpose in life is a component of psychological well-being that reflects feeling that one’s life is directed and goal oriented10. Purpose has been linked to better health across the adult lifespan. Individuals who feel that their lives are purposeful, for example, tend to report better subjective health in young adulthood11, have healthier cardiovascular and inflammatory profiles in middle adulthood12, perform better on walking speed and other tests of physical function in older adulthood13, and ultimately have lower risk of premature mortality14. Purpose in life has also been associated with healthier cognitive aging. Higher purpose, for example, has been associated with lower risk of Alzheimer’s disease15 and dementia16 and greater resilience to Alzheimer’s disease neuropathology17. And, prior to the onset of cognitive impairment, purpose has been associated with fewer subjective memory complaints18, better executive function19, higher verbal fluency20, and less age-related cognitive decline21. Given that purpose promotes healthier cognition and faster walking speed, it may be associated with less risk of developing MCR, which may help to maintain cognitive function and ultimately reduce risk of cognitive impairment.
The present research examines the relation between purpose in life and MCR cross-sectionally and the development of incident MCR longitudinally. We test the preregistered hypothesis that higher purpose in life is associated with lower risk of having the MCR syndrome measured concurrently and with lower risk of developing the syndrome over the follow-up. We test this hypothesis in two large samples of older adults. We also examine whether the association between purpose and MCR is moderated by age, gender, race, education, or baseline cognition to evaluate whether the association is limited to a specific population or whether it generalizes across sociodemographic and cognitive characteristics. Finally, in unregistered sensitivity analyses, we test the robustness of the longitudinal relations with three sensitivity analyses. First, because personality traits have been associated with incident MCR9, we test whether the association is independent of personality traits and whether purpose interacts with personality to predict incident MCR. Second, we test whether the association is independent of depressive symptoms, disease burden, and physical activity, as these factors could be mechanisms of the association between purpose and MCR risk. Third, to address the possibility of reverse causality, we selected participants with the longest follow-up interval – 12 years in the HRS – to test whether the association holds when the outcome is separated from the baseline assessment by over a decade.
Method
Participants and Procedure
Participants were from two large-scale studies of health and aging: the Health and Retirement Study (HRS) and the National Health and Aging Trends Study (NHATS). This analysis was preregistered at https://osf.io/2b8mt/?view_only=f34e1462ebf442d093dc665e6b5e3907.
HRS is a longitudinal study of Americans 50 and older and their spouses22. The site https://hrs.isr.umich.edu/about provides information about the HRS and how to access the data. The present research excluded participants younger than 65 years because they did not complete the timed walk necessary to compute MCR (see below). Purpose in life and walking speed were first measured in the 2006 wave for a random half of the HRS sample, the other half of the sample completed these measures in 2008. These two waves were combined as baseline. Cognitive complaints were measured at every assessment. Follow-up assessments occurred in 2010/2012, 2014/2016, and 2018 (half sample only). After excluding participants with dementia (see below for how dementia was identified) at each assessment (participants who developed MCR before dementia were retained in the sample), a total of 6,785 and 4,616 participants in HRS had the relevant data to be included in the cross-sectional and longitudinal analyses, respectively. Across the follow-up, 1488 participants developed dementia before MCR and/or died. The remaining 681 participants who did not have follow-up data had less education (d=.22, p<.001), were more likely to be African American (χ2=42.05, p<.001), had lower purpose in life (d=.12, p=.001), and scored lower in cognitive function (d=.40, p<.001) than participants with follow-up data. There was no difference by age or gender.
NHATS is a longitudinal study of Medicare beneficiaries23. More information about NHATS and how to access the data can be found at https://www.nhatsdata.org/. All participants were aged 65 or older at the baseline assessment. All measures were available in the baseline assessment (2011) and at annual assessments through 2018. After excluding participants with dementia (see below for how dementia was identified) at each assessment (participants who developed MCR before dementia were retained in the sample), a total of 5,665 and 2,877 participants in NHATS had the relevant data to be included in the cross-sectional and longitudinal analyses, respectively. Across the follow-up, 2039 participants developed dementia before MCR and/or died. The remaining 772 participants who did not have follow-up data had less education (d=.30, p<.001), were more likely to be African American (χ2=27.74, p<.001), had lower purpose in life (d=.09, p=.018), and scored lower in cognitive function (d=.30, p<.001) than participants with follow-up data. There was no difference by age or gender.
Measures
MCR.
Motoric cognitive risk syndrome was computed in the standard way for HRS and NHATS5. In HRS, cognitive complaints were scored as responding either fair or poor to the item “How would you rate your memory at the present time? Would you say it is excellent, very good, good, fair, or poor?” or responding worse to the item “Compared to (the last 2 years/2 years ago), would you say your memory is better now, about the same, or worse now than it was then?” In NHATS, cognitive complaints were scored as responding fair or poor to the item “How would you rate your memory at the present time? Would you say it is excellent, very good, good, fair, or poor?”, or responding worse to the item “Compared to 1 year ago, would you say your memory is better now, about the same, or worse now than it was then?”, or responding every day, most days, or some days to the item “In the last month, how often did memory problems interfere with your daily activities? Would you say every day, most days, some days, rarely, or never?”. In both HRS and NHATS, slow gait speed was defined as walking speed <=1 SD below age-specific (65–74 years/75+ years) and sex-specific (male/female) means within each cohort on a timed walk. At each assessment in both samples, MCR was defined as the presence of both cognitive complaints and slow gait speed in the absence of dementia.
Purpose in life.
In the HRS, purpose in life was assessed with the 7-item Purpose in Life scale from the Ryff Measures of Psychological Well-being scale10. Items (e.g., “I have a sense of direction and purpose in my life.”) were rated from 1 (strongly disagree) to 6 (strongly agree). Items were scored in the direction of greater purpose and the mean taken across items (alpha reliability=.74). In the NHATS, purpose in life was measured with the single item, “My life has meaning and purpose” rated from 1 (agree a lot) to 3 (agree not at all). The item was reverse scored in the direction of greater purpose. In both samples, purpose in life was entered into the analysis as a continuous variable.
Cognitive function.
In the HRS, cognitive function was measured with the modified Telephone Interview for Cognitive Status (TICSm24). The TICSm is the sum of performance on three cognitive tasks: memory, serial 7s, and backward counting. In NHATS, cognitive function was measured as the sum of three tasks that measured memory (immediate and delayed word recall), orientation (date, month, year, day of the week, President and Vice President), and executive function (clock drawing)23. Dementia in HRS was defined as a score <7 on the TICSm, and dementia in NHATS was defined as doctor diagnosis of dementia/Alzheimer’s disease, a score of ≥2 on the AD8 Dementia Screening interview, or a score of ≤1.5 SD below the mean in at least two of three tasks.
Sociodemographic covariates.
Sociodemographic covariates were age in years, gender (male versus female), race (African American versus white/other), and years of education.
Covariates for sensitivity analyses.
Personality traits were assessed with the Midlife Development Inventory (MIDI25) in both samples. HRS used a 26-item version and NHATS used a 10-item version to measure neuroticism, extraversion, openness, agreeableness, and conscientiousness. Depressive symptoms were measured with an 8-item version of the Centers for Epidemiological Studies Depression scale in the HRS and with the Patient Health Questionnaire-2 in the NHATS. Disease burden in both cohorts was measured as the sum of seven chronic diseases (hypertension, diabetes, cancer [excluding skin], lung disease, heart condition, stroke, arthritis). Physical activity was measured as frequency of moderate physical activity on a 4-point item in the HRS and as having engaged in physical activity in the last month (yes/no) in the NHATS.
Analytic Strategy
Logistic regression was used to examine the cross-sectional association between purpose in life and MCR controlling for the sociodemographic covariates (Model 1) and with cognitive function as an additional covariate (Model 2). Cox regression was used to examine the risk of incident MCR over the follow-up. Specifically, time was coded as time-to-incidence from baseline to the first instance of MCR over the follow-up. Participants who did not develop MCR were censored at their last available assessment. Purpose was used to predict risk of incident MCR over the follow-up, controlling for sociodemographic covariates (Model 1) and with baseline cognitive function as an additional covariate (Model 2). Participants with MCR at baseline were not included in the survival analysis. The proportional hazards assumptions were met in both HRS and NHATS (i.e., the time × purpose interaction was nonsignificant [p>.05] in either sample). All continuous variables were standardized to a mean of 0 and standard deviation of 1 (i.e., z-score) before analysis. Moderation analyses tested whether the association varied by age, gender, race, education, or baseline cognition in both the cross-sectional and longitudinal analyses.
We then did four sensitivity analyses. First, we included the five personality traits as additional covariates to test whether the association was independent of personality. We also tested for an interaction between purpose and each trait to test for interactive effects on MCR risk. Second, we included depressive symptoms, disease burden, and physical activity as additional covariates to determine whether these factors explained the association between purpose and risk of incident MCR. Third, we used inverse probability weighting to examine whether the pattern of attrition had an effect on the results in both studies. Fourth, in the HRS, we tested the association between purpose and risk of MCR with the longest follow-up interval possible – 12 years – to evaluate whether the association between purpose and MCR risk could be due solely to reverse causality.
Results
Descriptive statistics for study variables in HRS and NHATS are shown in Table 1. At baseline, the prevalence of MCR was ~6% in both HRS and NHATS. About 10% of participants in the HRS developed incident MCR over the up to 12-year follow-up, and nearly 7% of NHATS participants developed incident MCR over the up to 7-year follow-up.
Table 1.
Descriptive Statistics for Study Variables in the Health and Retirement Study (HRS) and the National Health and Aging Trends Study (NHATS) at Baseline and Baseline Characteristics by MCR Status as Follow-up
| Variable | HRS | NHATS | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | No Incident MCR | Incident MCR | Baseline | No Incident MCR | Incident MCR | |||
| N | 6,785 | 4,170 | 446 | 5,665 | 2,679 | 198 | ||
| Age (years) | 74.01 (6.66) | 72.78 (5.78) | 73.37 (6.60) | 76.56 (7.44) | 75.63 (7.16) | 77.89 (8.06) | ||
| Gender (female) | 57.5% (3899) | 58.8% (2451) | 55.0% (285) | 57% (3230) | 59.4% (1590) | 58.6% (116) | ||
| Race (African American) | 9.3% (632) | 7.1% (298) | 14.6% (65) | 19.4% (1101) | 15.3% 409) | 25.3% (50) | ||
| Educationa | 12.64 (2.90) | 13.04 (2.67) | 12.00 (3.11) | 5.24 (2.20) | 5.64 (2.20) | 4.66 (1.97) | ||
| Cognitive functionb | 15.11 (3.73) | 15.97 (3.45) | 14.96 (3.47) | 18.08 (4.34) | 19.44 (4.36) | 16.72 (4.46) | ||
| Baseline MCR (yes) | 6.0% (405) | 0% | 0% | 6.3% (355) | 0% | 0% | ||
| Incident MCR (yes) | 10.8% (518) | 0% | 100% (446) | 13.8% (584) | 0% | 100% (198) | ||
| Purpose in lifec | 4.60 (.91) | 4.72 (.86) | 4.41 (.90) | 2.83 (.42) | 2.89 (.32) | 2.81 (.39) | ||
Note. N=6,785 in HRS and N=5,665 in NHATS for the baseline sample and N=4,616 in HRS and N=2,877 in NHATS for the longitudinal sample. Values are means (standard deviations) or percentages (ns). MCR=Motoric Cognitive Risk syndrome.
Education was measured in years in HRS and on a scale from 1 (no school completed) to 9 (Masters, professional, or doctorate degree).
Measured with the modified Telephone Interview for Cognitive Status in HRS and with three tasks that measured memory, orientation, and executive function in NHATS.
Measured on a 6-point scale from 1 (strongly disagree) to 6 (strongly agree) in HRS and on a 3-point scale from 1 (agree not at all) to 3 (agree a lot) in NHATS.
Cross-sectional analysis.
The cross-sectional associations for both samples are shown in Table 2. In the HRS, participants with a higher purpose in life had a 47% lower risk of concurrent MCR. Likewise, in NHATS, higher purpose was associated with a 22% lower risk of concurrent MCR. The combined meta-analytic effect was OR=.75 (95% CI=.62, .90), p=.002. The association persisted after controlling for concurrent cognitive function in both samples (meta-analytic OR=.77; 95% CI=.64, .94), p=.008). In HRS, although significant for both genders, the association was slightly stronger among females than males (ORpurpose × gender=.80, 95% CI=.65-.98, p=.030). This interaction did not replicate in NHATS, and there was no moderation by age, race, education, or baseline cognition in either sample (all ps>.05), which indicated that purpose had the same association with lower risk of MCR across sociodemographic groups and cognition.
Table 2.
The Cross-sectional Association between Purpose in Life and Motoric Cognitive Risk Syndrome in HRS and NHATS
| Predictor | HRS | NHATS | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |||||||||
| OR (CI) | p | OR (CI) | P | OR (CI) | p | OR (CI) | p | |||||
| Age (years) | 1.14 (1.03–1.26) | .010 | 1.04 (.94–1.15) | .465 | 1.12 (1.01–1.25) | .040 | .88 (.78–.99) | .040 | ||||
| Gender (female) | .92 (.74–1.13) | .408 | .97 (.78–1.19) | .751 | 1.10 (.88–1.37) | .419 | 1.21 (.96–1.53) | .106 | ||||
| Race (African American) | 2.72 (2.07–3.57) | .000 | 2.10 (1.58–2.78) | .000 | 2.50 (1.98–3.16) | .000 | 1.95 (1.52–2.49) | .000 | ||||
| Education (years) | .69 (.63–.75) | .000 | .78 (.71–.86) | .000 | .60 (.53–.69) | .000 | .78 (.68–.89) | .000 | ||||
| Cognitive function | -- | -- | .66 (.58–.74) | .000 | -- | -- | .47 (.41–.54) | .000 | ||||
| Purpose in life | .68 (.61–.75) | .000 | .70 (.63–.78) | .000 | .82 (.74–.89) | .000 | .85 (.78–.93) | .000 | ||||
Note. N=6,785 in HRS and N=5,665 in NHATS. OR=odds ratio. CI=95% confidence interval. Model 2 includes cognitive function as an additional covariate.
Longitudinal analysis.
The results of the Cox regression are shown in Table 3. Consistent with the cross-sectional analysis, purpose in life was associated with lower risk of developing MCR over time in both samples (Figure 1). In HRS, participants with higher purpose were at a 35% reduced risk of developing MCR over the up to 12-year follow-up. In NHATS, purpose was associated with a nearly 25% reduced risk of developing MCR over the up to 7-year follow-up. The combined meta-analytic effect was HR=.77 (95% CI=.70, .84), p<.001. In both samples, the association persisted controlling for baseline cognitive function (meta-analytic HR=.78; 95% CI=.71, .84, p<.001). There was a marginally significant interaction between purpose and depressive symptoms in the HRS, which indicated that the association between purpose and risk of MCR was slightly stronger among individuals lower in depressive symptoms than higher in depressive symptoms (HR=1.09; 95% CI=1.01, 1.17, p=.030); the interaction did not replicate in NHATS (HR=.99; 95% CI=.90, 1.09, p=.852). This association was not moderated by age, gender, race, education or baseline cognition in either sample (all ps>.05).
Table 3.
Cox Regression Predicting Risk of Incident Motoric Cognitive Risk Syndrome from Baseline Purpose in Life in HRS and NHATS
| Predictor | HRS | NHATS | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |||||||||
| HR (CI) | p | HR (CI) | P | HR (CI) | p | HR (CI) | p | |||||
| Age (years) | 1.29 (1.17–1.41) | .000 | 1.26 (1.14–1.38) | .000 | 1.44 (1.25–1.65) | .000 | 1.25 (1.07–1.46) | .000 | ||||
| Gender (female) | .79 (.66–.96) | .015 | .81 (.67–.98) | .028 | .72 (.54–.96) | .026 | .80 (.59–1.07) | .798 | ||||
| Race (African American) | 2.38 (1.82–3.12) | .000 | 2.11 (1.59–2.79) | .000 | 2.02 (1.45–2.81) | .000 | 1.54 (1.08–2.20) | .016 | ||||
| Education (years) | .75 (.69–.81) | .000 | .78 (.72–.85) | .000 | .62 (.53–.72) | .000 | .75 (.64–.89) | .001 | ||||
| Cognitive function | -- | -- | .85 (.77–.95) | .004 | -- | -- | .60 (.50–.71) | .000 | ||||
| Purpose in life | .74 (.67–.81) | .000 | .75 (.69–.82) | .000 | .81 (.72–.91) | .000 | .82 (.73–.93) | .002 | ||||
Note. N=4,616 in HRS and N=2,877 in NHATS. HR=Hazard ratio. CI=95% confidence interval. Model 2 includes cognitive function as an additional covariate.
Figure 1.
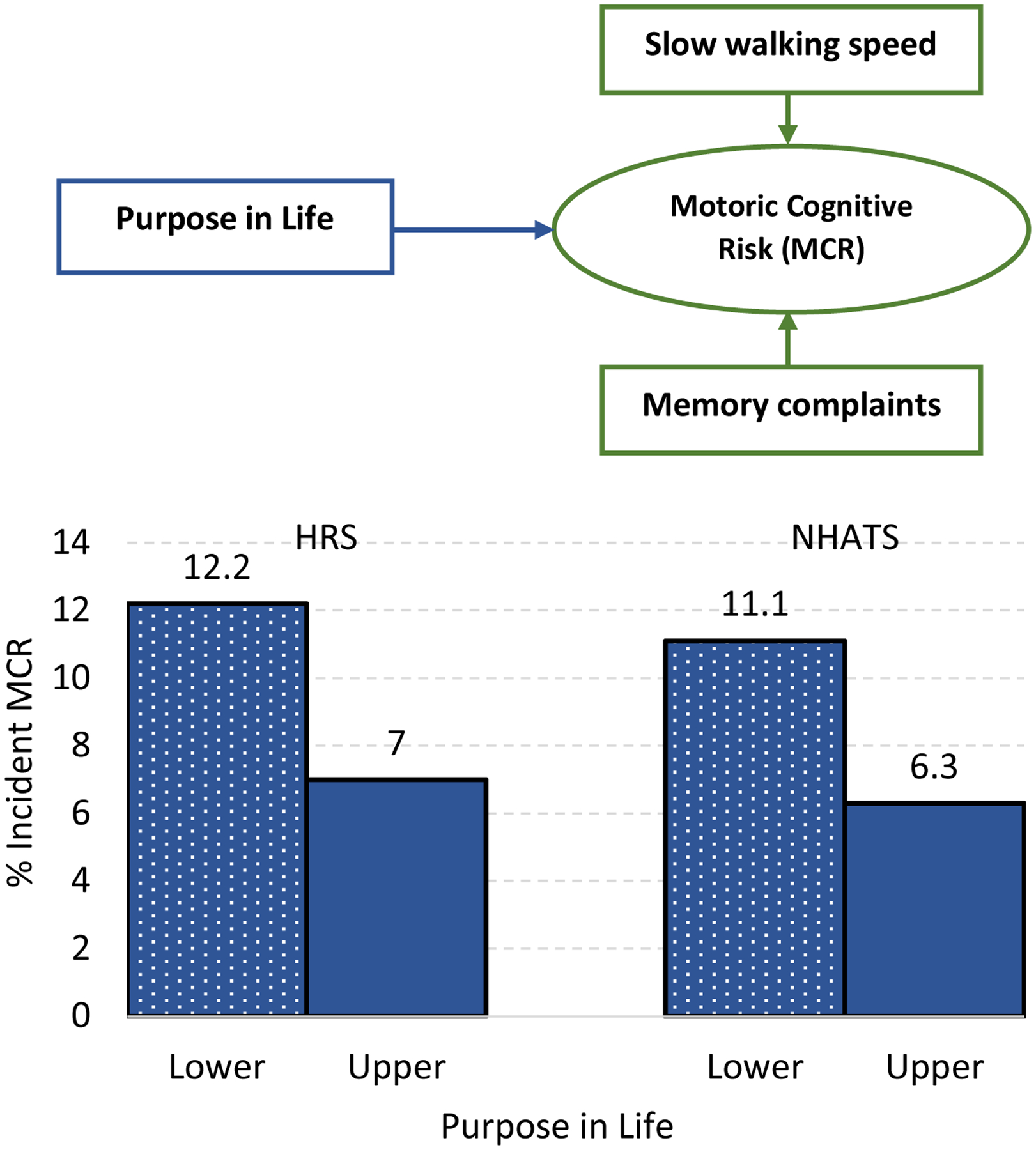
Diagram of purpose in life on motoric cognitive risk (MCR) syndrome (upper panel). Percent new cases of MCR by purpose in life over the up to 12-year follow-up in the Health and Retirement Study (HRS; left) and the up to 7-year follow-up in National Health and Aging Trends Study (NHATS; right) (lower panel). Note that Purpose in life is divided into upper and lower values for the figure; purpose was entered into the analysis as a continuous variable.
Sensitivity analyses.
We did four sensitivity analyses to test the robustness of the association. First, controlling for the five personality traits, purpose in life remained a significant predictor of MCR in both cohorts (HR=.81, 95% CI=.73, .91, p<.01 and HR=.80, 95% CI=.68, .95, p<.05 for HRS and NHATS, respectively). There were no interactions between purpose and any of the traits on risk of incident MCR in either sample (all ps>.05). Second, the association between purpose and MCR was also independent of depressive symptoms, disease burden, and physical activity in both cohorts (HR=.82, 95% CI=.74, .90, p<.01 and HR=.85, 95% CI=.75, .96, p<.01, respectively, for HRS and NHATS). Third, the coefficients were similar and the pattern of association identical when inverse probably weighting was used to account for the patterns of attrition in both studies. Finally, purpose in life remained a significant predictor of MCR risk in HRS when the sample was limited to participants with the 12-year follow-up (HR=.69, 95% CI=.55, .88, p<.01; N=953, n=75 incident MCR).
Discussion
This study provides replicable evidence that purpose in life is associated with lower risk of MCR. When measured concurrently, individuals higher in purpose were less likely to have the syndrome. When measured longitudinally, every standard deviation higher purpose was associated with an ~25% reduced risk of developing incident MCR. The cross-sectional and longitudinal findings replicated across the HRS and NHATS. The relation was also apparent across sociodemographic groups, which indicates that the association is evident even among individuals with lower education, advanced age, and other groups that are at higher risk for cognitive impairment. The sensitivity analyses supported the robustness of the association.
Previous research has linked purpose in life and the two components of MCR. In particular, there is a growing literature on purpose and physical activity and physical function. Individuals who feel that their life is purposeful are more physically active, as measured by accelerometer26, and such activity may be one factor that helps maintain their physical function in older adulthood13. Purpose may delay the onset of slow gait through greater engagement in physical activity. Less research has examined the association between purpose and subjective cognition. There is evidence, however, from a related construct. Specifically, meaning in life, a construct similar but not identical to purpose, is associated with fewer cognitive complaints in older adulthood18. Purpose may be associated with fewer cognitive complaints because it supports healthier cognitive function across adulthood, and individuals higher on purpose may have fewer complaints because they maintain good cognition. The present research shows that purpose is also associated with lower risk of the combination of these two risk factors. It is of note that MCR is a stronger predictor of dementia than its individual components3. A better understanding of the predictors of the development of MCR is needed to better predict its course and how to delay it. Most work to identify such predictors has focused on sociodemographic factors, chronic disease, and brain correlates6. There is recent evidence that psychological factors are implicated in MCR. Individuals with a history of depression7 and individuals higher in neuroticism and lower in conscientiousness, extraversion, or openness8 are at greater risk of MCR cross-sectionally, and individuals lower in openness are at greater risk longitudinally9. The present research indicates that a psychological factor implicated in well-being, purpose in life, is associated with lower risk of its development over time, independent of both depressive symptoms and personality.
There are likely a number of mechanisms that link purpose to lower risk of MCR. First, individuals higher in purpose tend to engage in healthier behavior, such as avoiding tobacco use27 and engaging in more physically activity26. The benefits of such behavior may accumulate across the lifespan and culminate in maintaining better function in older adulthood. Second, individuals higher in purpose tend to be more socially connected. In particular, purpose is associated with larger social networks and greater social integration28. Such social connection is critical for cognitive health29. Finally, purpose is also associated with volunteering and other ways of staying active that are associated with both physical and cognitive function30. A lifetime of greater engagement may help the brain and body against decline.
The sensitivity analyses support the robustness of the association, suggest mechanisms, and help reduce possible confounding. In particular, purpose remained a significant predictor of incident MCR controlling for depressive symptoms, disease burden, and physical activity. Such factors have been associated with both purpose13, 14 and MCR risk6. Although the association persisted, its magnitude was also reduced somewhat. These three factors could either be mechanisms (as would be hypothesized in a theoretical model) or confounders of the association. Experimental data are needed to tease apart these possibilities. It is of note, however, that regardless of the role they play, depressive symptoms, disease burden, and physical activity did not account for all of the association.
Purpose in life may be a useful target of intervention for healthier cognitive aging. In particular, there is replicable evidence that purpose can be increased through intervention31. These interventions, however, were not designed to promote healthier cognitive aging. The next step is to test whether one outcome of an intervention to increase purpose is maintenance of cognition, perhaps through lower risk of MCR. Given that purpose is associated with better cognition19, 20 and lower risk of impairment15, 16, increases in purpose may help better maintain cognitive function with age. There is also evidence that purpose can be changed through brief experimental manipulations32. Such work will be critical for testing the mechanisms through which purpose helps maintain cognition to improve interventions for healthier cognitive aging.
Another possibility is that that purpose in life is associated with MCR because low purpose could be an emerging symptom linked to neurodegeneration during the preclinical phase, prior to the onset of cognitive impairment and dementia. Other psychological and behavioral factors are associated with underlying neurodegeneration in participants with normal cognitive function33, as well as participants with mild cognitive impairments.34 Further, increases in symptoms, such as symptoms of depression, are linked with the presence of neuropathology.33 Similarly, it may be that lower purpose is driving the association with MCR because lower purpose reflects emerging neuropsychiatric symptoms linked to the underlying disease. If purpose is an early marker of the disease process, however, it is remarkable that such neuropathology-induced changes would occur before the emergence of the cognitive and physical declines that define MCR. Further, work on related constructs has demonstrated that psychological changes are not detectable in the preclinical phase of the disease35. Our sensitivity analysis also indicated that purpose remained a significant risk factor for incident MCR when we accounted for depressive symptoms and when the sample was limited to participants with over 10 years of follow-up.
The present research has several strengths, including two large samples, longitudinal assessments, and replicable associations. There are also limitations that could be addressed in future research. For example, although a strength, the two samples were only of older adults. More research is needed to test whether purpose measured earlier in life – either in young or middle adulthood – is also associated with lower risk of MCR. Future work also needs to manipulate purpose to experimentally determine its effect on the components of MCR. There were also nonrandom patterns of attrition in both the HRS and the NHATS that reduced the representativeness of the samples. Results, however, were similar when inverse probability weighting was used to account for these patterns of attrition. Finally, future work would also benefit from a measure of neuropsychiatric symptoms, including apathy, to address the relation between purpose in life and neuropsychiatric symptoms and their relation to MCR.
Despite these limitations, the present research provides replicable evidence for the role of purpose in life in the development of MCR. Purpose is emerging as an important factor that is associated with better cognition across the developmental pathway from healthy cognitive function to impairment. It may be thus one modifiable factor that is a useful target of intervention for healthier cognitive aging.
Acknowledgements
Role of the sponsor: The sponsor had no role in the design, methods, subject recruitment, data collections, analysis and preparation of this paper.
Funding: Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number R01AG053297. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of interest: The authors have no conflicts of interest.
References
- 1.Mendonça MD, Alves L, Bugalho P. From subjective cognitive complaints to dementia: who is at risk?: a systematic review. Am J Alzheimers Dis Other Demen. 2016;31: 105–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kueper JK, Speechley M, Lingum NR, Montero-Odasso M. Motor function and incident dementia: a systematic review and meta-analysis. Age Ageing. 2017;46: 729–738. [DOI] [PubMed] [Google Scholar]
- 3.Verghese J, Wang C, Lipton RB, Holtzer R. Motoric cognitive risk syndrome and the risk of dementia. J Gerontol A Biol Sci Med Sci. 2013;68: 412–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Verghese J, Annweiler C, Ayers E, et al. Motoric cognitive risk syndrome: multicountry prevalence and dementia risk. Neurology. 2014;83: 718–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ayers E, Verghese J. Motoric cognitive risk syndrome and risk of mortality in older adults. Alzheimers Dement. 2016;12: 556–564. [DOI] [PubMed] [Google Scholar]
- 6.Semba RD, Tian Q, Carlson MC, Xue QL, Ferrucci L. Motoric cognitive risk syndrome: Integration of two early harbingers of dementia in older adults. Ageing Res Rev. 2020;58: 101022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beauchet O, Sekhon H, Launay CP, et al. Motoric cognitive risk syndrome and mortality: results from the EPIDOS cohort. Eur J Neurol. 2019;26: 794–e756. [DOI] [PubMed] [Google Scholar]
- 8.Stephan Y, Sutin AR, Canada B, Terracciano A. Personality and motoric cognitive risk syndrome. J Am Geriatr Soc. 2020;68: 803–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ayers E, Gulley E, Verghese J. The effect of personality traits on risk of incident pre-dementia syndromes. J Am Geriatr Soc. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol. 1989;57: 1069–1081. [Google Scholar]
- 11.Stoddard SA, Pierce J, Hurd NM, Bauermeister JA, Zimmerman MA. Purpose and mastery as predictors of perceived health and substance use problems. J Community Psychol. 2019;47: 1514–1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zilioli S, Slatcher RB, Ong AD, Gruenewald TL. Purpose in life predicts allostatic load ten years later. J Psychosom Res. 2015;79: 451–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim ES, Kawachi I, Chen Y, Kubzansky LD. Association between purpose in life and objective measures of physical function in older adults. JAMA Psychiatry. 2017;74: 1039–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cohen R, Bavishi C, Rozanski A. Purpose in life and its relationship to all-cause mortality and cardiovascular events: a meta-analysis. Psychosom Med. 2016;78: 122–133. [DOI] [PubMed] [Google Scholar]
- 15.Boyle PA, Buchman AS, Barnes LL, Bennett DA. Effect of a purpose in life on risk of incident Alzheimer disease and mild cognitive impairment in community-dwelling older persons. Arch Gen Psychiatry. 2010;67: 304–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sutin AR, Stephan Y, Terracciano A. Psychological well-being and risk of dementia. Int J Geriatr Psychiatry. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boyle PA, Buchman AS, Wilson RS, Yu L, Schneider JA, Bennett DA. Effect of purpose in life on the relation between Alzheimer disease pathologic changes on cognitive function in advanced age. Arch Gen Psychiatry. 2012;69: 499–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Steinberg SI, Negash S, Sammel MD, et al. Subjective memory complaints, cognitive performance, and psychological factors in healthy older adults. Am J Alzheimers Dis Other Demen. 2013;28: 776–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lewis NA, Turiano NA, Payne BR, Hill PL. Purpose in life and cognitive functioning in adulthood. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn. 2017;24: 662–671. [DOI] [PubMed] [Google Scholar]
- 20.Sutin AR, Luchetti M, Stephan Y, Strickhouser JE, Terracciano A. The association between purpose/meaning in life and verbal fluency in 24 countries. Arch Gerontol Geriatr 2020. [Google Scholar]
- 21.Kim G, Shin SH, Scicolone MA, Parmelee P. Purpose in life protects against cognitive decline among older adults. Am J Geriatr Psychiatry. 2019;27: 593–601. [DOI] [PubMed] [Google Scholar]
- 22.Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, Weir DR. Cohort profile: the Health and Retirement Study (HRS). Int J Epidemiol. 2014;43: 576–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Freedman VA, Kasper JD. Cohort profile: The National Health and Aging Trends Study (NHATS). Int J Epidemiol. 2019;48: 1044–1045g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Crimmins EM, Kim JK, Langa KM, Weir DR. Assessment of cognition using surveys and neuropsychological assessment: the Health and Retirement Study and the Aging, Demographics, and Memory Study. J Gerontol B Psychol Sci Soc Sci. 2011;66 Suppl 1: i162–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lachman ME, Weaver SL. Midlife Development Inventory (MIDI) personality scales: Scale construction and scoring. Unpublished Technical Report; Brandeis University, 1997. [Google Scholar]
- 26.Hooker SA, Masters KS. Purpose in life is associated with physical activity measured by accelerometer. J Health Psychol. 2016;21: 962–971. [DOI] [PubMed] [Google Scholar]
- 27.Morimoto Y, Yamasaki S, Ando S, et al. Purpose in life and tobacco use among community-dwelling mothers of early adolescents. BMJ Open. 2018;8: e020586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scheier MF, Wrosch C, Baum A, et al. The Life Engagement Test: assessing purpose in life. J Behav Med. 2006;29: 291–298. [DOI] [PubMed] [Google Scholar]
- 29.Sutin AR, Stephan Y, Luchetti M, Terracciano A. Loneliness and risk of dementia. J Gerontol B Psychol Sci Soc Sci. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Infurna FJ, Okun MA, Grimm KJ. Volunteering is associated with lower risk of cognitive impairment. J Am Geriatr Soc. 2016;64: 2263–2269. [DOI] [PubMed] [Google Scholar]
- 31.Park CL, Pustejovsky JE, Trevino K, et al. Effects of psychosocial interventions on meaning and purpose in adults with cancer: A systematic review and meta-analysis. Cancer. 2019;125: 2383–2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scott MJ, Cohen AB. Surviving and thriving: fundamental social motives provide purpose in life. Pers Soc Psychol Bull. 2019: 146167219883604. [DOI] [PubMed] [Google Scholar]
- 33.Lussier FZ, Pascoal TA, Chamoun M, et al. Mild behavioral impairment is associated with β-amyloid but not tau or neurodegeneration in cognitively intact elderly individuals. Alzheimers Dement. 2020;16: 192–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krell-Roesch J, Vassilaki M, Mielke MM, et al. Cortical β-amyloid burden, neuropsychiatric symptoms, and cognitive status: the Mayo Clinic Study of Aging. Transl Psychiatry. 2019;9: 123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Terracciano A, An Y, Sutin AR, Thambisetty M, Resnick SM. Personality change in the preclinical phase of Alzheimer disease. JAMA Psychiatry. 2017;74: 1259–1265. [DOI] [PMC free article] [PubMed] [Google Scholar]


