Abstract
COVID-19 rapidly emerged as a crippling public health crisis in the last few months, which has presented a series health risk. Understanding of the immune response and biomarker analysis is needed to progress toward understanding disease pathology and developing improved treatment options. The goal of this study is to identify pathogenic factors that are linked to disease severity and patient characteristics. Patients with COVID-19 who were hospitalized from March 17 to June 5, 2020 were analyzed for clinical features of disease and soluble plasma cytokines in association with disease severity and sex. Data from COVID-19 patients with acute illness were examined along with an age- and gender-matched control cohort. We identified a group of 16 soluble factors that were found to be increased in COVID-19 patients compared to controls, whereas 2 factors were decreased. In addition to inflammatory cytokines, we found significant increases in factors known to mediate vasculitis and vascular remodeling (PDGF-AA, PDGF-AB-BB, soluble CD40L (sCD40L), FGF, and IP10). Four factors such as platelet-derived growth factors, fibroblast growth factor-2, and IFN-γ-inducible protein 10 were strongly associated with severe disease and ICU admission. Th2-related factors (IL-4 and IL-13) were increased with IL-4 and sCD40L present at increased levels in males compared with females. Our analysis revealed networking clusters of cytokines and growth factors, including previously unknown roles of vascular and stromal remodeling, activation of the innate immunity, as well activation of type 2 immune responses in the immunopathogenesis of COVID-19. These data highlight biomarker associations with disease severity and sex in COVID-19 patients.
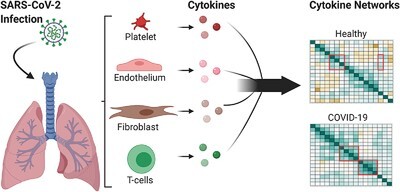
Graphical Abstract
Inflammatory cytokines and vasculitis factors are increased in COVID-19 infection with links to disease severity and sex variables.
Introduction
Coronavirus disease 2019 (COVID-19) is a rapidly emergent pandemic disease caused by a single-stranded RNA virus termed as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). COVID-19 rapidly emerged as a crippling public health crisis in the few months following the first reports of a mysterious pneumonia-like disease in Wuhan, China. The spectrum of illness associated with COVID-19 ranges from mild respiratory symptoms to severe disease requiring hospitalization in up to one-third of patients. Susceptible individuals frequently develop widespread inflammatory injury to the lungs, where acute-respiratory distress syndrome (ARDS) becomes a life-threatening complication as the alveolar-capillary barrier is compromised and fluid leaks into the lungs. It is currently not known why some individuals are more severely affected than others; however, hypertension, diabetes, and advanced age are reported as consistent risk factors for disease severity. Immune compromised patients infected with SARS-2-CoV do not present with increased severity compared with healthy individuals, suggesting that the host innate immune response appears to be a primary driver of COVID-19 pathobiology.1
Acute viral infections result in the activation of Toll-like receptors and induction of robust type I and III IFN responses, leading to transcription of hundreds of IFN-stimulated genes and production of proinflammatory cytokines and chemokines (e.g., IL-6, TNF-a, MCP-1, and Mip-1α) and robust differentiation of Th1 cells, which eliminate infected target cells.2 Proinflammatory Th1 responses are constrained by Th2 cytokines, and typically result in resolution of infection and immunity. SARS-CoV-1 and Middle East Respiratory Syndrome (MERS)-CoV have evolved mechanisms to suppress type I IFN responses3 and result in a Th17-type cytokine storm. COVID-19 patients can present with deteriorating symptoms following initial improvement, consistent with a delayed and exacerbated immune response.4,5 Dysregulation of Th1 and Th2 responses can lead to cytokine release syndrome (CRS) where high levels of diverse cytokines drive a positive feedback loop of pathogenic inflammation. Severe influenza, SARS-CoV-1, and MERS-CoV are all associated with ARDS and CRS. Studies of critically ill COVID-19 cases in China have demonstrated that SARS-CoV-2 infection also triggers CRS with uncontrolled proinflammatory responses,6 and differences in immune factors in moderate and severe cases of COVID-19 have begun to emerge.7 However, the aged population in Western Europe and the United States suggest that reduced Th1 immunity could lead to poor outcomes during infection.8 Thus, associations between cytokine responses and poor clinical outcomes in different populations warrants further investigation.
MERS-CoV, SARS-CoV-1, and SARS-CoV-2 infections all result in CRS in susceptible individuals despite significant immunologic differences and tropism, underscoring a critical need to understand the acute-phase cytokine response in COVID-19.9 To date, determinants of susceptibility leading to severe disease manifestations and the presence of shared- or population-specific CRS in COVID-19 are not known. We therefore recruited 22 COVID-19 patients, including 8 critically ill patients with ARDS and 15 moderately severe patients requiring hospitalization and analyzed patient clinical data in concert with circulating plasma cytokine networks to delineate the host immune response in SARS-CoV-2 infection.
Methods
Study design
All patients with SARS-CoV-2 infection (n = 22) requiring hospitalization due to acute illness were recruited from the University of Utah Health Sciences Center in Salt Lake City. We prospectively collected and analyzed data on patients with SARS-CoV-2 infection confirmed by RT-PCR, in accordance with current standards. We collected acid citrate dextrose (ACD)-anticoagulated whole blood from hospitalized patients with COVID-19 from March 17 to June 5, 2020. All COVID-19 patients were recruited under study protocols approved by the Institutional Review Board of the University of Utah (IRB#: 00102638, 00093575). Patients were approached for enrollment in this study and clinical trials within 24 h of admission. Blood samples were collected within 48 ± 24 h of hospital admission. Patients were co-enrolled in clinical trials of hydroxychloroquine or remdesivir. Healthy, age-, and gender-matched donors were enrolled and recruited under a separate IRB protocol (IRB#: 0051506). In accordance with the Declaration of Helsinki, each study participant or their legal authorized representative provided written informed consent for study enrollment. Our enrollment criteria included individuals of age greater than 18, respiratory symptoms including cough and shortness of breath, fever, hospital admission, positive SARS-CoV-2 testing, and informed consent. We summarize demographic, clinical characteristics, and illness severity data including sequential organ failure assessment (SOFA) scores in Table 1. All COVID-19 patients were hospitalized and were further stratified into moderate (non-ICU) and severe (critically ill ICU) COVID-19 patients.
TABLE 1.
Clinical and epidemiologic profiles of study cohort
| Characteristic | Healthy donors (n = 14) | Moderate COVID-19 infection (n = 14) | Severe COVID-19 infection (n = 8) | P-value |
|---|---|---|---|---|
| Age (mean ± sd) | 45.2 ± 16.1 | 48.9 ± 14.9 | 63.4 ± 18.2 | 0.047 |
| Male n (%) | 7 (50.0%) | 8 (57.1%) | 5 (62.5%) | 0.841 |
| Hispanic/Latino/Black n (%) | 0 (0.0%) | 4 (30.8%) | 3 (37.5%) | 0.050 |
| BMI (mean ± sd) | NA | 35.7 ± 10.3 | 31.6 ± 10.0 | 0.369 |
| Diabetes n (%) | 0 (0.0%) | 6 (42.9%) | 5 (62.5%) | 0.004 |
| Hypertension n (%) | 0 (0.0%) | 7 (50.0)% | 4 (50.0%) | 0.007 |
| Chronic lung disease n (%) | 0 (0.0%) | 3 (21.4%) | 2 (25.0%) | 0.153 |
| SOFA score (mean ± sd) | NA | 1.9 ± 1.1 | 5.8 ± 1.3 | <0.0001 |
| ARDS n (%) | NA | 2 (14.3%) | 8 (100.0%) | 0.0001 |
| Mechanical ventilation n (%) | NA | 0 (0.0%) | 5 (62.5%) | 0.0008 |
| Survival to date n (%) | 14 (100.0%) | 14 (100.0%) | 5 (62.5%) | 0.0033 |
| Aspirin (%) | NA | 12.5% | 11.8% | 0.95 |
| Hydroxychloroquine (%) | NA | 16.7% | 29.4% | 0.34 |
| Remdesivir (%) | NA | 20.8% | 23.5% | 0.84 |
| Convalescent plasma (%) | 0% | 5.9% | 0.24 | |
| WBC (mean ± sd) | NA | 5.8 ± 2.1 | 8.5 ± 2.5 | 0.014 |
|
Platelet count (mean ± sd) P-value indicates χ2 test for independence. BMI, body mass index; SOFA, sequential organ failure assessment; ARDS, acute-respiratory distress syndrome. |
NA | 269.6 ± 116.5 | 264.8 ± 49.0 | 0.913 |
Multiplex array
Plasma samples were analyzed using a Human Cytokine/Chemokine Panel I Multiplex Array (MilliporeSigma catalog# HCYTMAG60PMX41, Burlington, MA) according to manufacturer’s instructions on a Luminex 200 instrument. Plasma samples from 14 healthy adults were used as controls for cross-comparison.
Statistical methods
Means and standard deviations were used to describe clinical and epidemiologic profiles of study cohort for COVID-19 patients and controls along with the first level of cytokine analysis. For categorical characteristics, we used frequencies (n) and relative frequencies (%) for descriptive statistics. To identify any differences in the continuous characteristics of patients between controls and COVID-19 patients, we used the two samples independent t-test. The one-way ANOVA was used to assess mean differences between controls, moderate COVID-19 infection, and severe COVID-19 infection. To compare the percentages, for categorical variables, between controls and COVID-19 patients, or controls, moderate COVID-19 infection, and severe COVID-19 infection, we employed the χ2 test for independence. To compare median cytokine/chemokine levels between groups, we used the Mann-Whitney-Wilcoxon test while adjusting for multiple testing by using the SIDAK correction.10 To assess the effect size for the difference between medians, we used the ratio A/1–A from the A measure of stochastic superiority, which gives the odds that an individual in one group will score higher than an individual in the other group.11 Logistic regression models were utilized to assess the classification power of cytokines/chemokines by calculating the area under the receiver operating characteristic curve or ROC curve (AUC). AUC values from 0.90 to 1.00 indicate excellent accuracy; 0.80–0.90: good accuracy; 0.70–0.80: fair accuracy; 0.60–0.70: poor accuracy; and 0.50: no discriminating ability. To assess the intercorrelations between cytokines/chemokines, we used the Spearman correlation coefficients. Heat maps were used to visualize these intercorrelations. All statistical analyses were done by SAS version 9.4 (SAS Institute, Inc., Cary, NC, USA) and Prism using two-sided tests. All P-values less than 0.05 were deemed significant, whereas those between 0.04 and 0.05 were considered marginally significant, and those between 0.05 and 0.10 were assumed to be on the boundary of significance. Nonsignificant cytokines/chemokines that maintained large effect sizes were still considered clinically significant or relevant.
Results
Epidemiologic and clinical characteristics
Our cohort study comprises 22 COVID-19 patients admitted to the University of Utah Health Sciences Center with respiratory distress and positive SARS-CoV-2 testing along with 14 healthy controls. The COVID-19 patients studied consist of 13 males and 9 females with a mean age of 54.2 (±17.3) and ranged from 18 to 82 yr of age (Table 1) were compared with age- and gender-matched controls. Moderate COVID-19 cases ranged in age from 18 to 71 yr, with a mean age of 48.9 (±14.9). Hypertension (50.0% of moderate, 50.0% of critical cases) and diabetes mellitus (42.9% of moderate, 62.5% of critical cases) were the most common comorbid conditions, with no significant difference in body mass index (BMI) between groups (P = 0.369). Most of the critically ill patients with ARDS (n = 8) were 48 yr or older, apart from a 24 yr old of Hispanic ethnicity. Of these, 5 required endotracheal intubation and 28 day mortality was 37.5% for critically ill patients and 13.6% in total. To note, the severe infection group has a mean age of 63 suggesting in our cohort more severe disease with age. Patients were administered aspirin, or co-enrolled in clinical trials for hydroxychloroquine, or remdesivir within 24 h of hospitalization as shown in Table 1. In one case of severe disease, a patient was administered convalescent plasma. The mean SOFA score in moderate COVID-19 patients was 1.9 (±1.1) for moderate cases compared with 5.8 (±1.3) in critically ill patients (P < 0.0001). The mean initial Pao2/Fio2 ratio was 326.8 (±109.6) for moderate compared with 94.3 (±19.3) for critically ill patients (P < 0.0001). Three of the severe patients perished from our study, whereas the rest recovered.
COVID-19 patients produce systemic inflammatory cytokines
Because COVID-19 patients are known to have an excessive inflammatory response leading to tissue damage, we sought to examine circulating cytokines in plasma samples of COVID-19-infected patients compared to noninfected, healthy controls and perform a complex analysis of these cytokines for a more in depth understanding of the cytokine storm. Patient plasma from 22 COVID-19-infected patients was compared to 14 healthy controls. Samples from 13 infected males and 9 infected females were compared to 7 males and 7 female age-matched controls (Table 1). Eight critical inflammatory cytokines were significantly increased in the COVID-19 patient plasma compared to controls. As shown in Figure 1A–H, IL-6, IL-8, G-CSF, GROα, MCP-3, IL-1α, MCP-1, and TNF-α were all increased in COVID-19 patient samples. We further evaluated cytokines by SIDAK adjustment for multiple testing to examine effect size between medians to give odds that patients in the infected group will have greater cytokine levels than individuals in the control group (Table 2).
FIGURE 1.

COVID-19 infected patients have increased plasma proinflammatory cytokines/chemokines as shown by multiplex array, where 8 analytes are significantly increased compared to control plasma (A–H). *P < 0.05 by two samples t-test
TABLE 2.
SIDAK adjusted P-values from Mann-Whitney-Wilcoxon test for observed cytokine means (pg/ml)
| Cytokines | Controls (n = 14) | COVID-19 cases (n = 22) | SIDAK adjusted P-value | Odds A/1–A | |
| 1 | IL-10 | 6.6 | 33.02 | 0.000 | 101.67 |
| 2 | IL-6 | 3.17 | 37.52 | 0.000 | 50.33 |
| 3 | PDGF-AB-BB | 649.57 | 2128.06 | 0.000 | 24.67 |
| 4 | IP10 | 266.59 | 1090.44 | 0.000 | 21 |
| 5 | IL-1RA | 19.7 | 147.6 | 0.002 | 9.27 |
| 6 | sCD40L | 93.44 | 262.76 | 0.003 | 8.33 |
| 7 | TNFα | 5.85 | 15.21 | 0.007 | 6.9 |
| 8 | IL-8 | 6.76 | 15.55 | 0.011 | 6.16 |
| 9 | MCP-1 | 251.09 | 509.79 | 0.012 | 6 |
| 10 | IL-4 | 20.19 | 49.47 | 0.053 | 4.36 |
| 11 | MDC | 588.7 | 358.31 | 0.055 | 4.31 |
| 12 | MCP-3 | 20.91 | 68.9 | 0.057 | 4.27 |
| 13 | FGF-2 | 83.51 | 120.66 | 0.105 | 3.74 |
| 14 | Flt-3L | 29.73 | 21.62 | 0.225 | 3.16 |
| 15 | IL-1α | 0.53 | 8.85 | 0.198 | 3.13 |
| 16 | PDGF-AA | 59.08 | 228.51 | 0.237 | 3.11 |
| 17 | GCSF | 52.5 | 73.67 | 0.301 | 2.92 |
| 18 | IL-7 | 1.38 | 5.31 | 0.601 | 2.4 |
| 19 | GROα | 217 | 1012.19 | 0.645 | 2.35 |
| 20 | IL-15 | 2.94 | 5.22 | 0.645 | 2.35 |
| 21 | IFNγ | 3.64 | 7.65 | 0.712 | 2.23 |
| 22 | Fractaline | 125.66 | 151.76 | 0.820 | 2.07 |
| 23 | IL-13 | 4.5 | 10.34 | 0.914 | 1.89 |
| 24 | MIP-1β | 12.92 | 10.34 | 0.940 | 1.81 |
| 25 | GM-CSF | 3.19 | 4.74 | 0.940 | 1.78 |
| 26 | IL-1β | 0.08 | 0.22 | 0.940 | 1.74 |
| 27 | TNFB | 3.86 | 19.28 | 0.961 | 1.68 |
| 28 | IL-12p70 | 0.52 | 1.67 | 0.961 | 1.67 |
| 29 | IL-12p40 | 10.43 | 13.75 | 0.968 | 1.6 |
| 30 | IL-2 | 0.41 | 1 | 0.961 | 1.59 |
| 31 | RANTES | 924.91 | 898.61 | 0.969 | 1.57 |
| 32 | IL-3 | 0.82 | 1.39 | 0.987 | 1.45 |
| 33 | IL-5 | 1.49 | 0.93 | 0.999 | 1.27 |
| 34 | IL-17A | 5.22 | 4.18 | 0.999 | 1.27 |
| 35 | TGF-α | 1.09 | 0.85 | 0.999 | 1.26 |
| 36 | VEGF | 47.79 | 34.26 | 0.999 | 1.26 |
| 37 | MIP-1α | 9.92 | 9.25 | 0.999 | 1.22 |
| 38 | Eotaxin | 156.91 | 146.36 | 0.999 | 1.15 |
| 39 | EGF | 30.48 | 20.97 | 0.999 | 1.14 |
| 40 | IFNα2 | 15.75 | 16.28 | 0.999 | 1.05 |
| 41 | IL-9 | 0.87 | 0.87 | 0.999 | 1.05 |
The significant changes in inflammatory cytokines detected in COVID-19 patients were generally indicative of an innate immune response. These cytokines (IL-6, IL-8, G-CSF, GROα, MCP-3, IL-1α, MCP-1, and TNF-α) may be commonly produced by professional and nonprofessional innate immune cells, particularly circulating neutrophils, monocytes, dendritic cells, and fibrocytes. Several of these cytokines also may act as chemokines, attracting other innate immune cells to sites of infection to exacerbate inflammation. After SIDAK adjustment, it should be noted that G-CSF, GROα, and IL-1α become nonsignificant, but still maintain a large or a marginally large effect size (i.e., A/1–A > 2.5) as illustrated in our previous work.12 Figure 1D appears to indicate two different populations of expression levels for GROα; however, there was no association with disease activity or demographic factors that we could delineate.
COVID-19 patients produce systemic anti-inflammatory cytokines
During a cytokine storm, anti-inflammatory cytokines may be produced in an effort by the immune system to keep inflammation in check. Thus, IL-10 and IL-1RA were also found to be significantly increased in COVID-19 patients compared to control (Fig. 2A and B). With SIDAK analysis, IL-10 shows the highest odds ratio with a 99% classification power between COVID-19 patients and controls as shown by ROC curve as a standard technique for summarizing classifier performance between true positives and false positives (Fig. 2C). Thus, a ROC curve is a plot showing the ability to predict an event correctly. IL-1RA also remains significant after SIDAK adjustment. These results suggest an increase in anti-inflammatory cytokines as may typically be seen during a cytokine storm, but are not able to keep the overall inflammation in check.
FIGURE 2.

COVID-19 infected patients have increased plasma anti-inflammatory cytokines as shown by multiplex array where (A) IL-10 and (B) IL-1RA are increased significantly compared to control patients and (C) 99% classification power between COVID-19 patients and controls IL-10 receiver operating characteristic (ROC) curve shows that IL-10 classifies COVID-19 infection 99% of the time. *P < 0.05 by two samples t-test
Signatures of vascular remodeling and vasculitis are highly increased
Although the typical inflammatory cytokines are expected during cytokine storm from infection, we unexpectedly identified several growth factors with potent roles in vessel remodeling and angiogenesis were significantly increased in the plasma of infected patients compared to controls. These molecules included Platelet-derived growth factor (PDGF)-AA, AB-BB, PDGF-AA, Fibroblast growth factor-2 (FGF-2), and soluble CD40L (sCD40L; Fig. 3A–D). PDGF-AB-BB, PDGF-AA, and sCD40L were found to have a strong Spearman correlation (Table 3). However, we observed no significant difference in these molecules between moderate and severe COVID-19 patients, suggesting circulating levels may be independent of ARDS status. Although CD40L is well known to play a key role as a costimulatory molecule expressed by activated T cells engaging CD40 expressed on B cells and APCs,13 in this context it exists in a membrane-bound form involved in immunoglobulin isotype switching. The major source of sCD40L present in plasma is derived from platelets, suggesting that platelets may become activated in the pulmonary microvasculature in COVID-19. sCD40L may locally activate microvascular endothelial cells, pericytes, and smooth muscle cells, and promote expression of FGF-2.14 Both PDGF-AB-BB and FGF-2 possess broad mitogenic and cell survival activities, and similar to sCD40L, may be released from circulating activated platelets.15 Our analysis also revealed significant increases in IP10 (Fig. 3E), which may be secreted by several cell types including monocytes, dendritic cells, fibroblasts, and endothelial cells and is strongly associated with vasculitis.16 CXCR3 ligands such as Interferon gamma-induced protein 10 (IP10) can promote lymphocyte adhesion to endothelial cells, and our data indicate IP10 levels closely resemble those reported in patients with multisystem vascular inflammatory condition known as Kawasaki disease.17
FIGURE 3.

COVID-19 infected patients have increased plasma factors of vasculitis/vascular remodeling as shown by multiplex array, where 5 analytes are significantly increased compared to control plasma (A–E). *P < 0.05 by two samples t-test
TABLE 3.
Spearman correlation of sCD40L, PDGF-AA, -AB/BB, and IL-4 showing the association of these factors in patient samples
| Spearman correlation coefficients Prob > |r| under H0: ρ = 0 | ||||
|---|---|---|---|---|
| PDGF-AA | PDGF-AB-BB | sCD40L | IL-4 | |
| PDGF-AA | 0.81559 (<0.0001) | 0.58893 (0.0039) | 0.63985 (0.0013) | |
| PDGF-AB-BB | 0.64396 (0.0129) | 0.72522 (0.0001) | 0.61253 (0.0024) | |
| sCD40L | 0.46813 (0.0914) | 0.21319 (0.4643) | 0.56787 (0.0058) | |
| IL-4 | 0.44322 (0.1124) | 0.33297 (0.2447) | 0.37045 (0.1923) | |
COVID-19 patient cytokine classification by disease status
Differences were noted in patients with moderate vs. severe infection (non-ICU vs. ICU) in SOFA score, ARDS WBC counts, and survival (Table 1). Furthermore, while most cytokines we detected appeared to be increased in COVID-19 patients compared to healthy controls, we observed decreased levels of two soluble factors in our patient population. Macrophage-derived chemokine (MDC22), a chemokine mainly produced by macrophages and dendritic cells, was significantly decreased in COVID-19 patients compared to controls (Fig. 4A). Although MDC22 is associated with lung inflammation and hemorrhage,18 our data indicate that MDC22 is decreased in COVID-19 infected patients. We also observed a decrease in the hematopoietic growth factor FMS-like tyrosine kinase 3 ligand (FLT-3L, Fig. 4B), which can increase monocyte-derived myeloid dendritic cells (and plasmacytoid dendritic cells) and is implicated to provide protective immunity in bacterial lung infections.19
FIGURE 4.

COVID-19 infected patients have decreased plasma factors (A) macrophage-derived chemokine (MDC) and (B) FLT-3L, and (C) multiple factors associated with severe disease compared to moderate disease (ICU vs. non-ICU). (D) MDC decrease and TNF-α predicting acute-respiratory distress syndrome (ARDS) status 86% of the time correctly. *P < 0.05 by two samples t-test
We next compared cytokine expression in COVID-19 patients presenting with moderate vs. severe infection (non-ICU vs. ICU) and found that MDC22, FLT-3L, and IL-12 were decreased in severe patients with ARDS compared to moderate (Fig. 4C). We also found that levels of TNF-α were increased in patients with severe disease. Furthermore, decreased levels of MDC22 and TNF-α can classify ARDS status 86% of the time in our patient cohort when analyzed by AUC (Fig. 4D). The differences in the four soluble factors between moderate and severe cases suggest potential biomarkers for severity of disease.
Type 2 immune response signals are increased in COVID-19 patients
While there is limited evidence recently published on the type 2 immune response in COVID-19 patients,20 our data presented earlier suggest that SARS-Cov2 triggers hyperinflammatory conditions resulting in the influx of innate immune cells likely followed by the activation of the T-cell responses. Thus, we analyzed Th1/Th2/Th17 cytokine profile in the COVID-19 patients. We observed that in contrast to MERS-CoV infections that are known to mount Th1/Th17 responses,20 COVID-19 patients show dramatic increase in the Th2 response cytokine IL-4 (Fig. 5A) and while not reaching significance after SIDAK adjustment, a trend in increase of IL-13 was also observed (Fig. 5B). These data suggest that SARS-Cov2 infection mounts a Th2 response in patients requiring hospitalization.
FIGURE 5.

COVID-19 infected patients have increased Th2 factors (A) IL-4 and (B) IL-13 and differences between female and male levels of (C) IL-4 and (D) sCD40L that (E) classify biologic sex status 73.5% of the time correctly. *P < 0.05 by two samples t-test
Sex differences
Of particular interest among COVID-19 patients, a trend toward increased IL-4 and sCD40L was observed in men (Fig. 5C and D). Further analysis of these factors showed that the association between IL-4 and sCD40L showed a correct prediction for male infection vs. female 73.5% of the time when analyzed by AUC (Fig. 5E). Although further analysis is needed, we observed several trends showing differences between female and male cytokine responses (Table 4). The overall trends suggest that potential differences in a productive Th2 response between males and females may be associated with poor outcomes in males suffering from COVID-19.
TABLE 4.
Plasma concentrations of cytokines by sex shown as pg/ml and analyzed by Wilcoxon’s test
| Medians | Significance | |||
|---|---|---|---|---|
| Variable | F (n = 9) | M (n = 13) | p1 | ES2 |
| IL-4 | 46.38 | 63.73 | 0.087 | 2.60 |
| sCD40L | 180.86 | 305.56 | 0.109 | 2.44 |
| PDGF-AB-BB | 1890.15 | 2280.06 | 0.204 | 2.00 |
| IL-10 | 27.6 | 40.37 | 0.256 | 1.85 |
| TNFα | 10.98 | 16.25 | 0.270 | 1.82 |
| MDC | 433.12 | 324.89 | 0.442 | 1.52 |
| IL-6 | 41.31 | 37.12 | 0.593 | 1.34 |
| IL-1RA | 140.09 | 155.1 | 0.640 | 1.29 |
| MCP-3 | 59.87 | 83.72 | 0.640 | 1.29 |
| IP10 | 1111.42 | 1069.47 | 0.841 | 1.13 |
| IL-8 | 15.55 | 15.55 | 0.920 | 1.07 |
| MCP-1 | 447.94 | 515.54 | 1.000 | 1.02 |
Wilcoxon’s test.
Probability-based effect size expressed as odds.
Discrete cytokine clusters are present in COVID-19
In order to assess the relationships between the cytokines observed in COVID-19, we performed correlation analysis on those cytokines demonstrated to be statistically significant between healthy controls and COVID-19 patients. To distinguish the degree of correlation between cytokines, we set up a cut-off for Spearman correlation coefficient corresponding to significant P-value (P < 0.05). Our data indicate that concentration levels of sCD40L, PDGF-AA, PDGF-AB/BB, and IL-4 have doubled among COVID-19 patients relative to healthy controls (Fig. 3). Specifically, their concentration levels went up from 120.60, 726.75, 110.29, and 31.29 among controls to 230.00, 2340.00, 274.64, and 62.09 among COVID-19 patients for PDGF-AA, PDGF-AB-BB, sCD40L, and IL-4, respectively. Intercorrelation between these molecules is substantially significant among COVID-19 patients and clustered together in dark green as shown in Figure 6B. Among our control population, the Spearman correlation between these molecules is not statistically significant except between PDGFs, as expected. In contrast, among COVID-19 patients the intercorrelations between these markers are highly significant (Table 2). This observation suggests that these molecules act jointly in COVID-19 pathobiology. After SIDAK adjustment, only PDGF-AB-BB and sCD40L remained significant. However, these four factors were found to be highly associated in infected patients when analyzed by Spearman correlation (Fig. 6B), suggesting they work jointly in COVID-19. Interestingly, Spearman correlation analysis also suggests of a relationship between MDC22 and FLT-3L (P < 0.01), the only two cytokines found to be decreased in our patient cohort (Fig. 4C), implicating dendritic cell (DC) dysregulation in COVID-19. Our study shows that of the inflammatory cytokines, IL-6 was highly significant, consistent with its known roles in CRS and acute lung injury (Fig. 1A). Upon further analysis of IL-6 in relation to other COVID-19 plasma cytokines, we found that IL-6 is increased independent of disease severity. IL-6 levels are able to classify COVID-19 infected patients 99% of the time when analyzed by AUC (Fig. 6C) and is likely to play a triggering role in the cytokine storm during early innate immune response to SARS-Cov2, similar to previous observations of MERS-CoV and SARS-CoV infections.21
FIGURE 6.

Discrete clusters of cytokines differ in plasma between (A) control and (B) COVID-19 as shown by Spearman correlation with (C) IL-6 levels able to classify patients with COVID-19 infection 99% of the time
Discussion
Patients with COVID-19 exhibit a broad spectrum of clinical manifestations of disease and our understanding of the clinical, epidemiologic, and pathologic characteristics is still evolving. Although most infected individuals present with mild disease pathology, approximately 30% of hospitalized patients with COVID-19 develop progressive, sustained lung injury. Many patients with severe COVID-19 suffer from a cytokine storm. Although the mechanistic link between the cytokine storm and lung injury during SARS-Cov2 infection remains to be elucidated, it is currently believed that high levels of cytokines promote relentless destruction of the pulmonary capillary beds. Pulmonary complications are believed to result from vascular barrier disruption, leading to tissue edema, fluid accumulation in the lung, and robust inflammatory cell infiltrate ultimately manifesting as ARDS. However, limited published reports revealed discrepancies in the cytokine storm profile initially reported in Asian countries, when compared to the Western world population over the last few months. This warranted more investigation. Thus, in a current report, we examined relationships between clinical parameters of disease in patients and expression levels of plasma cytokines. This study cohort of 22 COVID-19 patients examined the relationships between clinical parameters of disease in patients and expression levels of plasma cytokines in detail. In our cohort, advanced age is a significant risk factor for development of severe complications of COVID-19, as with prior reports (Table 1). Our data independently confirm elevated plasma levels of 10 cytokines previously reported in COVID-19 cases in the United States and worldwide.22 A novel observation was that plasma levels of several growth cytokines, sCD40L, and growth factors were altered in response to SARS-CoV-2 infection and significantly associated with ARDS status. We also observed formation of intercorrelative networking clusters with these molecules, suggesting that activation of the innate immunity, vascular and stromal remodeling, as well activation of type 2 immune responses are involved in the immunopathogenesis of COVID-19 and ARDS complication.
As previously reported,23,24 we observed that advanced age is a significant risk factor for development of severe complications of COVID-19. However, in contrast to prior study,25,26 diabetic status, BMI, hypertension, or prior history of chronic lung disease did not distinguish development of severe complications compared with moderately affected patients in our cohort. This is may be due to the small size of studied cohort of the COVID-19 patients. However, our data indicate that 18 cytokines comprising proinflammatory, anti-inflammatory, and mitogenic responses are significantly increased, and two cytokines are significantly decreased in our COVID-19 cohort. These findings are consistent with the observation of cytokine response syndrome in COVID-19 patients consistent with previous studies.6,27 As previously seen in the COVID-19 patients worldwide,22,27,28 we observed that CRS in our cohort shows elevated levels of G-CSF, IL1RA, IL-10, IP10, MCP-3, FGF-2, IL-4, IL-7, IL-8, and TNF-α. However, in our study cohort several cytokines reported in the Asian population were not significantly increased in our study population. Although the cause of these differences in cytokine storm profile remains to be elucidated, it is possible that some COVID-19 patients in the Asian population experienced a past exposure to SARS-CoV infection over the last two decades.29,30 Although only 8098 infected individuals were identified in the 2002–2003 SARS outbreak, seroepidemiologic studies suggest that a larger number of individuals may have been exposed to a SARS-like virus that frequently caused an asymptomatic infection.31–33 This type of exposure is reminiscent of COVID-19, and could perhaps allow some “priming” of the immune system to mount aggressive innate and adaptive type 1 immune responses. This hypothesis is supported by the fact that only minor differences have been found between the genome sequences of SARS-CoV-2 and SARS-CoV viruses.30 Our data are also in contrast from prior studies of COVID-19 in patients in Asia, where leukopenia was commonly observed in severely affected individuals. Rather than a decrease in leukocytes, severely affected patients in our study group demonstrate modestly elevated leukocyte counts, consistent with reports of severe patients in other regions of the United States.34,35 While lymphopenia has been noted in severe COVID-19, we did not routinely collect differential white blood cell counts in our study. Further, the ethnic differences in patient populations studied, past vaccinations (e.g., smallpox, polio),36,37 or social determinants of health may also be contributing factors to the observed differences in cytokine profiles.
A novel observation from our study was that plasma levels PDGF-AA, PDGF-AB, GROα, FLT-3L, sCD40L, and MDC22 are altered in response to SARS-CoV-2 infection and, additionally, MDC22, FLT-3L, TNF-α, and IL-12(p40) significantly associated ARDS status. We also observed an increase in FGF-2 and IP10. All molecules mentioned earlier are known to play a critical role in extracellular matrix and vascular remodeling.11,38–40 Although there are reports of thrombocytopenia in COVID-19 patients, our cohort exhibited relatively normal platelet counts,41 and all were administered standard thromboprophylaxis treatment. It is currently not known whether SARS-CoV-2 directly leads to platelet activation or consumption, but the widespread expression of ACE2 receptors within endothelial cells, evidence of viral infection, and endothelitis in COVID-19 suggest the endothelium plays a central role. Our observation of high levels of IP10, a biomarker and mediator of Kawasaki disease pathobiology, is particularly of interest given that although children appear to be minimally susceptible to COVID-19, a recent outbreak of severe Kawasaki-like disease in children is particularly concerning.42,43 Although IP10 levels are also increased in response to hepatitis C virus and rhinovirus infections, the levels of IP10 in these conditions are much lower (<500 pg/ml) than those detected in acute states of Kawasaki disease and in the present study of COVID-19. Taken together our data suggest that immunopathogenesis of SARS-Cov2 infection is likely to involve the activation of platelets, stromal cell and smooth muscle cells that via release of the above-mentioned cytokines and growth factors form a distinct networking cluster involved in the vascular and overall extracellular matrix remodeling. In fact, vasculitis, fibrotic plugs, and overall cardiovascular complications have been reported in COVID-19 patients.44
Furthermore, our cytokine network analysis revealed strong intercorrelation between molecules involved ECM and vascular remodeling (CD40L, PDGF-AA, PDGF-AB/BB) and Th2 cytokine IL-4. This is a previously unreported finding; however, a recent report by Roncati and colleagues45 suggests that in COVID-19, a life-threatening escalation from Th2 immune response to type 3 hypersensitivity with the subsequent deposition of antigen-antibody complexes, particularly inside the walls of blood vessels, may generate a systemic vasculitis. In this context, another important player of inflammation of vascular remodeling contributing to cytokine storm and its complication is likely to be IL-6. Although standing alone in our networking analysis, IL-6 is ranked among the key cytokine released by macrophages, smooth muscle cells, and fibroblast during cardiovascular inflammation,46,47 is among the highest during COVID-19 cytokine storm release syndrome role48 and suggested as well to be an important player in mounting type 2 immune responses.49 Additionally, we observed that the levels of several cytokines, and particularly IL-4, while not reaching significance, were higher in male vs. female patients with COVID-19. Although the mechanism by which gender difference impacts the severity of CRS and this disease outcome is not yet described, multiple reports have shown that SARS-CoV-2 affects women less than men.50,51 Interestingly, a recent study52 shows that severe disease in male COVID-19 patients was associated with low testosterone level and estradiol level in these patients was positively correlated with IL-6. Taken together, these data suggest that sex hormones could be among the determinants of CRS and disease severity.
In conclusion, here we present several novel observations on cytokine responses during COVID-19 infection. First, beyond a typical innate immune cytokine storm, we found an unreported cluster of soluble factors related to vascular remodeling and vasculitis. We also show a decrease in three factors (MDC and FLT-3L) and an increase in TNF-α in patients with severe disease compared to moderate disease as potential biomarkers. Finally, our data show a trend toward sex differences in several important factors such as sCD40L and IL-4, which could be clues to why there were observed differences in males and females in some reports. Although we have begun to unravel the complexity of the inflammatory response here, more studies are needed to clarify the inflammation-induced pathogenesis seen during infection leading to poor outcome for some patients.
Acknowledgment
This study was supported by startup funds from the University of Utah.
Abbreviations
- ACD
Acid Citrate-Dextrose
- ARDS
Acute Respiratory Distress Syndrome
- APC
Antigen Presenting Cell
- COVID-19
Corona Virus Disease 2019
- CRS
Cytokine Release Syndrome
- ECM
Extracellular Matrix
- FGF
Fibroblast Growth Factor
- FLT-3L
FMS-like Tyrosine Kinase 3 Ligand
- ICU
Intensive Care Unit
- IP10
Interferon Gamma-Induced Protein 10
- MDC22
Macrophage-derived Chemokine
- MERS
Middle East Respiratory Syndrome
- PDGF
Platelet-derived Growth Factor
- ROC
Receiver Operating Characteristic Curve
- SARS-CoV
Severe Acute Respiratory Syndrome Coronavirus
- sCD40L
Soluble CD40 Ligand
- SOFA
Sequential Organ Failure Assessment
Contributor Information
Aaron C Petrey, Molecular Medicine Program, University of Utah, Salt Lake City, Utah, USA; Division of Microbiology and Immunology, Department of Pathology, University of Utah, Salt Lake City, Utah, USA.
Fares Qeadan, Department of Family and Preventative Medicine, University of Utah, Salt Lake City, Utah, USA.
Elizabeth A Middleton, Molecular Medicine Program, University of Utah, Salt Lake City, Utah, USA; Division of Gastroenterology, Department of Internal Medicine, University of Utah, Salt Lake City, Utah, USA.
Irina V Pinchuk, Division of Gastroenterology, Department of Medicine, Pennsylvania State Health, Hershey, Pennsylvania, USA.
Robert A Campbell, Molecular Medicine Program, University of Utah, Salt Lake City, Utah, USA; Division of Gastroenterology, Department of Internal Medicine, University of Utah, Salt Lake City, Utah, USA.
Ellen J Beswick, Division of Microbiology and Immunology, Department of Pathology, University of Utah, Salt Lake City, Utah, USA; Division of Gastroenterology, Department of Internal Medicine, University of Utah, Salt Lake City, Utah, USA.
Disclosures
The authors declare no conflicts of interest.
References
- D’Antiga L. Coronaviruses and immunosuppressed patients: the facts during the third epidemic. Liver Transpl. 2020;26(6):832-834. [DOI] [PubMed] [Google Scholar]
- Kahan SM, Wherry EJ, Zajac AJ. T cell exhaustion during persistent viral infections. Virology. 2015;479-480:180-193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu L, Manopo I, Leung BP, et al. Immunological characterization of the spike protein of the severe acute respiratory syndrome coronavirus. J Clin Microbiol. 2004;42(4):1570-1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan WJ, Ni ZY, Hu Y, et al. China medical treatment expert group for C. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708-1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425-434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y, Shen C, Li J, et al. Plasma IP-10 and MCP-3 levels are highly associated with disease severity and predict the progression of COVID-19. J Allergy Clin Immunol. 2020. 10.1016/j.jaci.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Jiang M, Chen X, Montaner LJ. Cytokine storm and leukocyte changes in mild versus severe SARS-CoV-2 infection: review of 3939 COVID-19 patients in China and emerging pathogenesis and therapy concepts. J Leukoc Biol. 2020;108(1):17-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okada H, Kuhn C, Feillet H, Bach JF. The ‘hygiene hypothesis’ for autoimmune and allergic diseases: an update. Clin Exp Immunol. 2010;160(1):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li K, Hao Z, Zhao X, Du J, Zhou Y. SARS-CoV-2 infection-induced immune responses: friends or foes? Scand J Immunol;2020:e12895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saeed AI, Qeadan F, Sood A, et al. A novel cytokine profile associated with cancer metastasis to mediastinal and hilar lymph nodes identified using fine needle aspiration biopsy - A pilot study. Cytokine. 2017;89:98-104. [DOI] [PubMed] [Google Scholar]
- Balasubramaniam V, Le Cras TD, Ivy DD, Grover TR, Kinsella JP, Abman SH. Role of platelet-derived growth factor in vascular remodeling during pulmonary hypertension in the ovine fetus. Am J Physiol Lung Cell Mol Physiol. 2003;284(5):L826-L833. [DOI] [PubMed] [Google Scholar]
- Qeadan F, Bansal P, Hanson JA, Beswick EJ. The MK2 pathway is linked to G-CSF, cytokine production and metastasis in gastric cancer: a novel intercorrelation analysis approach. J Transl Med. 2020;18(1):137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bretscher PA. A two-step, two-signal model for the primary activation of precursor helper T cells. Proc Natl Acad Sci U S A. 1999;96(1):185-190. 10.1073/pnas.96.1.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinders ME, Sho M, Robertson SW, Geehan CS, Briscoe DM. Proangiogenic function of CD40 ligand-CD40 interactions. J Immunol. 2003;171(3):1534-1541. [DOI] [PubMed] [Google Scholar]
- Pintucci G, Froum S, Pinnell J, Mignatti P, Rafii S, Green D. Trophic effects of platelets on cultured endothelial cells are mediated by platelet-associated fibroblast growth factor-2 (FGF-2) and vascular endothelial growth factor (VEGF). Thromb Haemost. 2002;88(5):834-842. [PubMed] [Google Scholar]
- Strunk D, Schmidt-Pogoda A, Beuker C, et al. Biomarkers in vasculitides of the nervous system. Front Neurol. 2019;10:591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko TM, Kuo HC, Chang JS, et al. CXCL10/IP-10 is a biomarker and mediator for Kawasaki disease. Circ Res. 2015;116(5):876-883. [DOI] [PubMed] [Google Scholar]
- Richter JR, Sutton JM, Belizaire RM, et al. Macrophage-derived chemokine (CCL22) is a novel mediator of lung inflammation following hemorrhage and resuscitation. Shock. 2014;42(6):525-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winter C, Taut K, Langer F, et al. FMS-like tyrosine kinase 3 ligand aggravates the lung inflammatory response to Streptococcus pneumoniae infection in mice: role of dendritic cells. J Immunol. 2007;179(5):3099-3108. [DOI] [PubMed] [Google Scholar]
- Prompetchara E, Ketloy C, Palaga T. Immune responses in COVID-19 and potential vaccines: lessons learned from SARS and MERS epidemic. Asian Pac J Allergy Immunol. 2020;38(1):1-9. [DOI] [PubMed] [Google Scholar]
- Rokni M, Ghasemi V, Tavakoli Z. Immune responses and pathogenesis of SARS-CoV-2 during an outbreak in Iran: comparison with SARS and MERS. Rev Med Virol. 2020;30(3):e2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarzi-Puttini P, Giorgi V, Sirotti S, et al. COVID-19, cytokines and immunosuppression: what can we learn from severe acute respiratory syndrome? Clin Exp Rheumatol. 2020;38(2):337-342. [PubMed] [Google Scholar]
- Chen R, Liang W, Jiang M, et al. Medical treatment expert group for C. Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China. Chest. 2020. 10.1016/j.chest.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Z, Peng F, Xu B, et al. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect. 2020. 10.1016/j.jinf.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y, Yang D, Cheng B, et al. Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication. Diabetes Care. 2020. 10.2337/dc20-0660. [DOI] [PubMed] [Google Scholar]
- Petrakis D, Margina D, Tsarouhas K, et al. Obesity a risk factor for increased COVID19 prevalence, severity and lethality (Review). Mol Med Rep. 2020;22(1):9-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamilloux Y, Henry T, Belot A, et al. Should we stimulate or suppress immune responses in COVID-19? Cytokine and anti-cytokine interventions. Autoimmun Rev. 2020;19(7):102567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peeri NC, Shrestha N, Rahman MS, et al. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned? Int J Epidemiol. 2020. 10.1093/ije/dyaa033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrosillo N, Viceconte G, Ergonul O, Ippolito G, Petersen E. COVID-19, SARS and MERS: are they closely related? Clin Microbiol Infect. 2020;26(6):729-734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo PC, Lau SK, Tsoi HW, et al. Relative rates of non-pneumonic SARS coronavirus infection and SARS coronavirus pneumonia. Lancet. 2004;363(9412):841-845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ip M, Chan PK, Lee N, et al. Seroprevalence of antibody to severe acute respiratory syndrome (SARS)-associated coronavirus among health care workers in SARS and non-SARS medical wards. Clin Infect Dis. 2004;38(12):e116-e118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan Y, Zheng BJ, He YQ, et al. Isolation and characterization of viruses related to the SARS coronavirus from animals in southern China. Science. 2003;302(5643):276-278. [DOI] [PubMed] [Google Scholar]
- Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020. 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arentz M, Yim E, Klaff L, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020. 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haralambieva IH, Ovsyannikova IG, Kennedy RB, Larrabee BR, Shane Pankratz V, Poland GA. Race and sex-based differences in cytokine immune responses to smallpox vaccine in healthy individuals. Hum Immunol. 2013;74(10):1263-1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chumakov K, Benn CS, Aaby P, Kottilil S, Gallo R. Can existing live vaccines prevent COVID-19? Science. 2020;368(6496):1187-1188. [DOI] [PubMed] [Google Scholar]
- Hristov M, Gumbel D, Lutgens E, Zernecke A, Weber C. Soluble CD40 ligand impairs the function of peripheral blood angiogenic outgrowth cells and increases neointimal formation after arterial injury. Circulation. 2010;121(2):315-324. [DOI] [PubMed] [Google Scholar]
- Schultz GS, Wysocki A. Interactions between extracellular matrix and growth factors in wound healing. Wound Repair Regen. 2009;17(2):153-162. [DOI] [PubMed] [Google Scholar]
- Svystonyuk DA, Ngu JM, Mewhort HE, et al. Fibroblast growth factor-2 regulates human cardiac myofibroblast-mediated extracellular matrix remodeling. J Transl Med. 2015;13:147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu P, Zhou Q, Xu J. Mechanism of thrombocytopenia in COVID-19 patients. Ann Hematol. 2020;99(6):1205-1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viner RM, Whittaker E. Kawasaki-like disease: emerging complication during the COVID-19 pandemic. Lancet. 2020;395(10239):1741-1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdoni L, Mazza A, Gervasoni A, et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020;395(10239):1771-1778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu H, Rhee JW, Cheng P, et al. Correction to: cardiovascular complications in patients with COVID-19: consequences of viral toxicities and host immune response. Curr Cardiol Rep. 2020;22(5):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roncati L, Ligabue G, Fabbiani L, et al. Type 3 hypersensitivity in COVID-19 vasculitis. Clin Immunol. 2020;217:108487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ijaz T, Sun H, Pinchuk IV, Milewicz DM, Tilton RG, Brasier AR. Deletion of NF-kappaB/RelA in angiotensin II-sensitive mesenchymal cells blocks aortic vascular inflammation and abdominal aortic aneurysm formation. Arterioscler Thromb Vasc Biol. 2017;37(10):1881-1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song Y, Shen H, Schenten D, Shan P, Lee PJ, Goldstein DR. Aging enhances the basal production of IL-6 and CCL2 in vascular smooth muscle cells. Arterioscler Thromb Vasc Biol. 2012;32(1):103-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C, Wu Z, Li JW, Zhao H, Wang GQ. Cytokine release syndrome in severe COVID-19: interleukin-6 receptor antagonist tocilizumab may be the key to reduce mortality. Int J Antimicrob Agents. 2020;55(5):105954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roncati L, Nasillo V, Lusenti B, Riva G. Signals of Th2 immune response from COVID-19 patients requiring intensive care. Ann Hematol. 2020;99(6):1419-1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conti P, Younes A. Coronavirus COV-19/SARS-CoV-2 affects women less than men: clinical response to viral infection. J Biol Regul Homeost Agents. 2020;34(2). 10.23812/Editorial-Conti-3. [DOI] [PubMed] [Google Scholar]
- He R, Lu Z, Zhang L, et al. The clinical course and its correlated immune status in COVID-19 pneumonia. J Clin Virol. 2020;127:104361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- https://www.medrxiv.org/content/10.1101/2020.05.07.20073817v1. BMJ Yale. 2020. 10.1101/2020.05.07.20073817 [DOI]


