Abstract
Introduction:
In Massachusetts, recent outbreaks of HIV have been fueled by injection and sexual exposures among people who inject drugs (PWID). Understanding pre-exposure prophylaxis (PrEP) need, knowledge, and use among PWID will help inform and evaluate interventions.
Methods:
In 2019, investigators analyzed 2018 National HIV Behavioral Surveillance data from PWID in Boston, Massachusetts, who met eligibility criteria. Proportions of PWID with U.S Preventive Services Task Force–based PrEP indication were estimated by types of HIV acquisition risk in the past year: injection exposure only, sexual exposure only, and overlapping injection and sexual exposures. Investigators then evaluated PrEP awareness, conversations with healthcare providers about PrEP, and self-reported PrEP use among those with and without PrEP indications.
Results:
The prevalence of PrEP indication was 92% overall (389/423), with 290 (69%) indicated for injection exposures only, 3 (<1%) indicated for sexual exposures only, and 96 (23%) indicated for both injection and sexual exposures. Among those indicated for PrEP (n=389), 152 (39%) reported being aware of PrEP, 41 (11%) had discussed PrEP with a healthcare provider, and 8 (2%) had used PrEP in the past year. There were no statistically significant differences between PrEP-indicated and non-indicated PWID with respect to PrEP awareness, discussion with a healthcare provider, and PrEP use.
Conclusions:
Indication for PrEP was high but awareness was low, conversations about PrEP with healthcare providers were uncommon, and PrEP use was extremely low. These findings highlight important areas for clinical and community-based interventions to improve PrEP uptake among and delivery to PWID.
INTRODUCTION
Notable HIV outbreaks and clusters attributed to injection drug use have recently affected cities and towns across the U.S., including in Indiana, West Virginia, Pennsylvania, Washington, and Massachusetts.1-5 The prevalence of injection drug use is increasing: As reflected in national data, substance use treatment admissions involving injection drug use increased 85% in 1 decade.6 In addition to rising prevalence of injection drug use, HIV risk among people who inject drugs (PWID) is increasing along with the surge of illicitly manufactured fentanyl in local opioid (including heroin) and stimulant drug markets.7,8 The consumption of fentanyl, which has a shorter half-life than other commonly injected opioids,9,10 has been associated with increased injection frequency and thus increased exposures to HIV via contaminated injection equipment.11 The confluence of factors—increasing injection drug use in the population and rising levels of fentanyl and fentanyl-contaminated drugs that PWID are injecting—has already set back decades of public health progress in reducing injection-related HIV transmission.
Risk of HIV acquisition is experienced by PWID through injection and sexual exposures. In 2018, nationally 59% of PWID reported past-year receptive sharing of used syringes or other injection equipment, or using used syringes to divide drugs.12 High proportions of PWID surveyed nationally have also reported condomless vaginal sex (67%) and the median number of opposite sexual partners was 2 (IQR=1–4).12 Many PWID experience both injection and sexual exposures that put them at risk for HIV during the same period (e.g., past year).13 For example, qualitative research in this socially marginalized population has documented the frequent co-occurrence of injection and sexual exposures that increase risk for HIV acquisition, including common experiences of having non-monogamous injection and sexual partners and engaging in transactional sex to obtain drugs.14 Despite evidence that harm-reduction services such as syringe service programs and medications for opioid use disorder help reduce HIV transmission,15,16 geographic coverage of these services remains limited,17,18 and such medications are persistently underprescribed.19,20 Taken together, these studies suggests that PWID could benefit from antiretroviral pre-exposure prophylaxis (PrEP) as an additional efficacious HIV prevention tool.21
The U.S. Public Health Service recommended that PrEP be offered to at-risk PWID,22 and in 2019, U.S. Preventive Services Task Force (USPSTF) guidelines gave PrEP an “A” grade, indicating that offering PrEP to PWID would be of a substantial net benefit with high certainty.23 Yet, PrEP uptake among PWID has been limited compared with that in other populations (e.g., men who have sex with men),24,25 representing an important disparity in PrEP implementation. There also remains a limited quantification of PrEP need among PWID, with existing studies involving small samples recruited through local harm-reduction venues.26,27 Though informative, these studies do not provide a thorough understanding of the distribution of multiple avenues of HIV acquisition (and thus multiple indicators of PrEP need) in larger, more representative samples of PWID. To help inform research and programmatic efforts to improve PrEP delivery to PWID, the prevalence of PrEP indication was examined by type of risk (i.e., indication by injection exposures only, sexual exposures only, or both injection and sexual exposures) among PWID in the Greater Boston Area, where repeated clusters of HIV transmission among PWID have been identified.28,29
METHODS
Study Sample
In 2019, data were analyzed from the 2018 PWID National HIV Behavioral Surveillance System (NHBS) survey in the Greater Boston Area.30 NHBS is a repeated, cross-sectional survey with 3 populations at risk for HIV acquisition (men who have sex with men, PWID, high-risk heterosexuals) in 22 cities across the U.S. Participants in the PWID cycle were recruited using respondent driven sampling31,32 and were eligible if they were aged ≥18 years, reported injecting drugs in the past 12 months, lived in a 5-county sampling area in and around Boston, were able to complete the interview in English or Spanish, and had not previously participated in NHBS. Of 612 recruited PWID, 469 met NHBS eligibility criteria and were enrolled. For this analysis, all HIV-negative, cis-gender participants with complete data were included, resulting in a final analytic sample of 423 PWID.
Measures
Trained interviewers administered the NHBS questionnaire to recruited PWID. All participants were compensated $25 for completing the survey, and were offered HIV testing for which they were compensated an additional $25.30
Measures included participant characteristics, health service and substance use behaviors, and PrEP knowledge and experiences. Participant characteristics included age, sex (male or female), sexual identity (lesbian or gay, bisexual, or heterosexual), race and ethnicity (non-Hispanic White, non-Hispanic Black/African American, Hispanic/Latinx, or other), marital status (currently married/cohabitating, divorced/separated/widowed, or single), educational attainment (less than high school, high school/GED, or more than high school), employment, income ($0–$9,999, $10,000–$14,999, $15,000–$24,999, or ≥$25,000), current homelessness, and past-year detention, jail, or prison for ≥24 hours and having ≥1 self-reported disability ([1] deaf or serious difficulty hearing; [2] blind or serious difficulty seeing; [3] a physical, mental, or emotional condition causing serious difficulty concentrating, remembering, or making decisions; [4] serious difficulty walking or climbing stairs; [5] difficulty dressing or bathing; and [6] a physical, mental, or emotional condition causing difficulty doing errands alone).
Healthcare utilization included current insurance status, ever being tested for hepatitis C virus or HIV, past-year receipt of safe injection supplies, syringe service program– or pharmacy-based access to sterile syringes, visiting a healthcare provider (past year), having a routine source of care (defined by having a place that you usually go when you are sick or need advice about your health and then describing that place as a clinic, healthcare center, doctor’s office, or HMO), and past-year participation in a drug treatment program).
Substance use behaviors included past-month binge drinking, past-year non-injection use of any drugs not prescribed to the participant, past-year injection frequency, past-year injection of heroin (by itself) or any stimulants (by themselves, including methamphetamine, crack cocaine, and powder cocaine), past-year speedball injection (heroin and cocaine together), and past-year overdose from heroin or “painkillers.”
The PrEP variables included past-year PrEP knowledge defined by the question: PRE-exposure prophylaxis, or PrEP, is an antiretroviral medicine, such as Truvada, taken for months or years by a person who is HIV-negative to reduce the risk of getting HIV. Before today, have you ever heard of PrEP? Among those answering affirmatively that they had heard of PrEP before, past-year discussion with a healthcare provider about taking PrEP was assessed. PrEP use was assessed as: In the past 12 months, have you taken PrEP to reduce the risk of getting HIV? Based on these questions, a PrEP care continuum was created that includes PrEP indication (defined below), PrEP awareness, PrEP discussions with healthcare providers, and PrEP use.33
Based on USPSTF guidelines for considering individuals for PrEP (Appendix Figure 1),23 a categorical variable was created separating PrEP indication according to type of HIV acquisition risk: (1) not indicated for PrEP, (2) indicated for PrEP based on past-year injection exposure only (receptive sharing of drug injection equipment), (3) indicated for PrEP based on past-year sexual exposure only (inconsistent condom use during anal or vaginal sex with someone whose HIV status is positive, indeterminate, or unknown, or with someone who has ever injected drugs; having a sexually transmitted infection in the past year), and (4) indicated for PrEP based on both past-year injection and past-year sexual exposures (i.e., multiple types of HIV acquisition risk exposures).
Statistical Analysis
One-way ANOVA F-tests were used to compare differences in continuous variables across PrEP indication categories and Fisher’s exact tests for binary and categorical variables where cell counts were small. All tests were 2-sided and considered significant at the p<0.05 level. Stata, version 15.1 was used for all analyses.
RESULTS
Among 423 PWID, mean age was 41 (SD=11) years, 274 (65%) identified as male, 303 (72%) identified as heterosexual, 260 (61%) were non-Hispanic White, 262 (62%) were single, 202 (48%) had a high school education or GED, 375 (89%) were unemployed, 248 (59%) reported an income of $0–$9,999, 302 (71%) were currently homeless, and 163 (39%) reported being held in detention, jail, or prison for >24 hours in the past year (Table 1). Healthcare utilization was relatively high among this sample and almost all participants were insured (96%). Most 338 (80%) reported receiving safe injection supplies in the past year, most reported accessing sterile syringes through syringe service programs (81%), and 380 (90%) visited a healthcare provider in the past year.
Table 1.
Sample Characteristics and Differences Across PrEP Indication Categories Among 423 People Who Inject Drugs in the Greater Boston Area, Massachusetts, NHBS 2018
| Characteristics | Overall (n=423) n (%) |
Not indicated (N=34) n (%) |
Injection only (N=290) n (%) |
Sexual only (n=3) n (%) |
Multiple risk (n=96) n (%) |
p-value |
|---|---|---|---|---|---|---|
| Participant characteristics | ||||||
| Age, years, mean (SD) | 41 (11) | 41 (10) | 41 (11) | 43 (7) | 42 (11) | 0.777 |
| Sex | <0.001 | |||||
| Male | 274 (65) | 22 (65) | 162 (56) | 3 (100) | 87 (91) | |
| Female | 149 (35) | 12 (35) | 128 (44) | 0 (0) | 9 (9) | |
| Sexual identity | 0.505 | |||||
| LGB | 120 (28) | 6 (18) | 85 (13) | 1 (33) | 28 (29) | |
| Heterosexual | 303 (72) | 28 (82) | 205 (71) | 2 (67) | 68(71) | |
| Race and Ethnicity | 0.412 | |||||
| Non-Hispanic, White | 260 (61) | 17 (50) | 182 (63) | 3 (100) | 58 (60) | |
| Non-Hispanic, Black/African American | 46 (11) | 7 (21) | 27 (9) | 0 (0) | 12 (13) | |
| Hispanic/Latino | 80 (19) | 5 (15) | 59 (20) | 0 (0) | 16 (17) | |
| Other | 37 (9) | 5 (15) | 22 (8) | 0 (0) | 10 (10) | |
| Marital status | 0.091 | |||||
| Currently married/Co-habitating | 42 (10) | 1 (3) | 33 (11) | 0 (0) | 8 (8) | |
| Divorced/Separated/Widowed | 119 (28) | 7 (21) | 79 (27) | 3 (100) | 30 (31) | |
| Single | 262 (62) | 26 (76) | 178 (61) | 0 (0) | 58 (60) | |
| Education attainment | 0.138 | |||||
| Less than high school | 110 (26) | 9 (26) | 69 (24) | 2 (67) | 30 (31) | |
| High school/GED | 202 (48) | 16 (47) | 137 (47) | 0 (0) | 49 (51) | |
| More than high school | 111 (26) | 9 (26) | 84 (29) | 1 (33) | 17 (18) | |
| Employment | 0.354 | |||||
| Employed | 48 (11) | 4 (12) | 35 (12) | 1 (33) | 8 (8) | |
| Unemployed | 375 (89) | 30 (88) | 255 (88) | 2 (67) | 88 (92) | |
| Homelessness | 0.549 | |||||
| Currently homeless | 302 (71) | 22 (65) | 205 (71) | 2 (67) | 73 (76) | |
| Not currently homeless | 121 (29) | 12 (35) | 85 (29) | 1 (33) | 23 (24) | |
| Held in detention, jail, or prison for >24 hoursa | 0.033 | |||||
| Yes | 163 (39) | 9 (26) | 107 (37) | 0 (0) | 47 (49) | |
| No | 260 (61) | 25 (74) | 183 (63) | 3 (100) | 49 (51) | |
| Insurance status | 0.724 | |||||
| Insured | 404 (96) | 32 (94) | 276 (95) | 3 (100) | 93 (97) | |
| Uninsured | 19 (4) | 2 (6) | 14 (5) | 0 (0) | 3 (3) | |
| Income | 0.897 | |||||
| $0–$9,999 | 248 (59) | 20 (59) | 168 (58) | 3 (100) | 57 (59) | |
| $10,000–$14,999 | 84 (20) | 4 (12) | 59 (20) | 0 (0) | 21 (22) | |
| $15,000–$24,999 | 34 (8) | 4 (12) | 24 (8) | 0 (0) | 6 (6) | |
| ≥$25,000 | 57 (13) | 6 (18) | 39 (13) | 0 (0) | 12 (13) | |
| One or more disability | 0.013 | |||||
| Yes | 341 (81) | 24 (71) | 231 (80) | 1 (33) | 85 (89) | |
| No | 82 (19) | 10 (29) | 59 (20) | 2 (67) | 11 (11) | |
| Health services | ||||||
| Received safe injection suppliesa | 0.242 | |||||
| Yes | 338 (80) | 23 (68) | 232 (80) | 3 (100) | 80 (83) | |
| No | 85 (20) | 11 (32) | 58 (20) | 0 (0) | 16 (17) | |
| Goes to syringe exchange for needlesa | 0.905 | |||||
| Yes | 344 (81) | 28 (82) | 233 (80) | 3 (100) | 80 (83) | |
| No | 79 (19) | 6 (18) | 57 (20) | 0 (0) | 16 (17) | |
| Goes to syringe exchange or pharmacy for needlesa | 0.878 | |||||
| Yes | 388 (92) | 32 (94) | 264 (91) | 3 (100) | 89 (93) | |
| No | 35 (8) | 2 (6) | 26 (9) | 0 (0) | 7 (7) | |
| Visting a healthcare providera | 0.926 | |||||
| Yes | 380 (90) | 30 (88) | 261 (90) | 3 (100) | 86 (90) | |
| No | 43 (10) | 4 (12) | 29 (10) | 0 (0) | 10 (10) | |
| Drug treatmenta | 0.948 | |||||
| Yes | 260 (61) | 21 (62) | 180 (62) | 2 (66) | 57 (59) | |
| No | 163 (39) | 13 (38) | 110 (38) | 1 (33) | 39 (41) | |
| Have a usual source of care | 0.517 | |||||
| Yes | 266 (63) | 25 (74) | 182 (63) | 2 (67) | 57 (59) | |
| No | 157 (37) | 9 (26) | 108 (37) | 1 (33) | 39 (41) | |
| HCV testing/diagnosis | 0.040 | |||||
| Never tested | 30 (7) | 0 (0) | 21 (7) | 0 (0) | 9 (9) | |
| Tested, not diagnosed | 97 (23) | 11 (32) | 63 (22) | 3 (100) | 20 (21) | |
| Tested, diagnosed | 296 (70) | 23 (68) | 206 (71) | 0 (0) | 67 (70) | |
| HIV testing/diagnosis | 0.487 | |||||
| Never tested | 30 (7) | 2 (6) | 18 (6) | 0 (0) | 10 (10) | |
| Tested, not diagnosed | 393 (93) | 32 (94) | 272 (94) | 3 (100) | 86 (90) | |
| Substance use and behaviors | ||||||
| Binge drinkb | 0.106 | |||||
| Yes | 151 (34) | 8 (24) | 99 (34) | 2 (67) | 42 (44) | |
| No | 170 (40) | 17 (50) | 124 (43) | 1 (33) | 28 (29) | |
| Don’t know/Refused | 102 (24) | 9 (26) | 67 (23) | 0 (0) | 26 (27) | |
| Non-injection drug usea | 0.236 | |||||
| Yes | 378 (89) | 29 (85) | 263 (91) | 2 (67) | 84 (88) | |
| No | 45 (11) | 5 (15) | 27 (9) | 1 (33) | 12 (13) | |
| Injection frequencya | 0.681 | |||||
| More than once a day | 289 (68) | 26 (76) | 189 (65) | 2 (67) | 72 (75) | |
| Once a day | 49 (12) | 3 (9) | 36 (12) | 1 (33) | 9 (9) | |
| More than once a week | 45 (11) | 2 (6) | 34 (12) | 0 (0) | 9 (9) | |
| Once a week or less | 40 (9) | 3 (9) | 31 (11) | 0 (0) | 6 (6) | |
| Injection of heroina | 0.329 | |||||
| Yes | 396 (94) | 32 (94) | 272 (94) | 2 (67) | 90 (94) | |
| No | 27 (6) | 2 (6) | 18 (6) | 1 (33) | 6 (6) | |
| Stimulant usea | 0.013 | |||||
| Yes | 373 (88) | 28 (82) | 254 (88) | 1 (33) | 90 (94) | |
| No | 50 (12) | 6 (18) | 36 (12) | 2 (67) | 6 (6) | |
| Inject speedballa | 0.108 | |||||
| Yes | 235 (56) | 18 (53) | 153 (53) | 1 (33) | 63 (66) | |
| No | 188 (44) | 16 (47) | 137 (47) | 2 (67) | 33 (34) | |
| Inject methamphetaminea | 0.061 | |||||
| Yes | 159 (38) | 11 (32) | 100 (34) | 1 (33) | 47 (49) | |
| No | 264 (62) | 23 (68) | 190 (66) | 2 (67) | 49 (51) | |
| Overdoseda | 0.009 | |||||
| Yes | 201 (48) | 8 (24) | 139 (48) | 1 (33) | 53 (55) | |
| No | 222 (52) | 26 (76) | 151 (52) | 2 (67) | 43 (35) | |
Note: Boldface indicates statistical significance (p<0.05).
In the past 12 months.
In the past 30 days.
PrEP, preexposure prophylaxis; NHBS, National HIV Behavioral Surveillance; LGB, lesbian, gay, or bisexual; HCV, hepatitis C virus
The majority of participants (89%) reported non-injection drug use involving substances not prescribed to them, and past-year injection frequency was high, with 289 (68%) participants injecting more than once a day. Nearly all participants (94%) reported injecting heroin in the past year, and more than half (56%) reported speedball injection (heroin and cocaine together) in this period. Any stimulant use (injection and non-injection) was high in this sample (88%) and methamphetamine injection was reported by 159 (38%) participants. A total of 151 (34%) reported binge drinking alcohol in the past month. Almost half of participants reported overdosing on heroin or painkillers in the past year (48%).
Based on USPSTF guidelines, 92% (389/423) of participants in the sample were indicated for PrEP (Table 1, Figure 1). A total of 386 (91%, 386/423) were indicated based on injection exposures, with 324 (77%) reporting using a needle after someone else had used it (past 12 months) as the most frequently reported injection exposure (Table 2). Ninety-nine PWID (23%) reported any sexual exposure leading to PrEP indication, of whom 85% (85/99) identified as heterosexual and 70% (70/99) reported inconsistent use of condoms with a partner whose HIV status is unknown and is at high risk for HIV acquisition (Table 2). PrEP indication based on sexual exposures only was reported by 3 (<1%) PWID. Overall, among the 389 PrEP-indicated PWID, 99% (386/389) were indicated for injection exposures and 25% (99/389) for sexual exposures.
Figure 1.
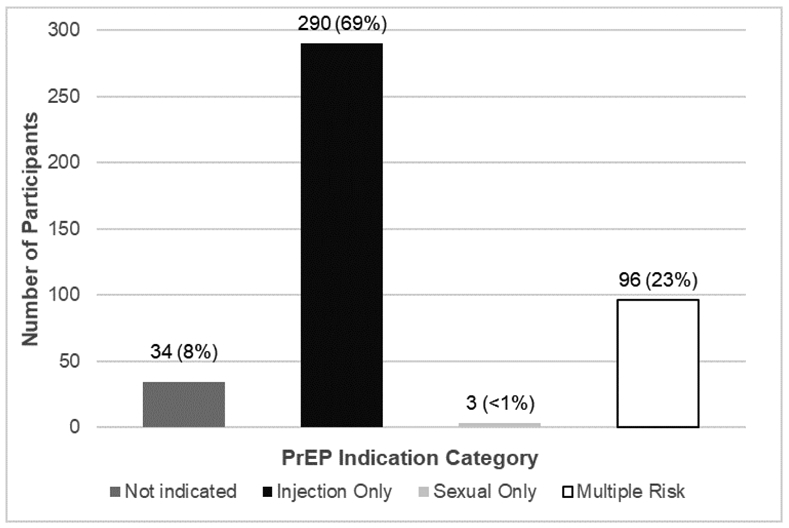
PrEP indication among 423 PWID by route of HIV acquisition in Greater Boston Area, Massachusetts, NHBS.
PrEP, preexposure prophylaxis; PWID, people who inject drugs; NHBS, National HIV Behavioral Surveillance.
Table 2.
Distribution of Injection and Sexual Exposures for PrEP Indication Among 423 People Who Inject Drugs in the Greater Boston Area, Massachusetts, NHBS 2018
| Route of HIV acquisition risk | n (%) |
|---|---|
| Injection exposures | 386 (91) |
| Used a needle after someone else injected with ita | 324 (77) |
| Used the same cooker, cotton, or rinse water that someone else had already useda | 304 (72) |
| Used drugs that had been divided with a syringe that someone else had already useda | 207 (49) |
| Sexual exposures | 99 (23) |
| Men who have sex with men (with one or more of risk exposure below) | 15 (4) |
| A serodiscordant sex partner (i.e., in a sexual relationship with a partner living with HIV)a | 0 (0) |
| Inconsistent use of condoms during receptive or insertive anal sexa | 12 (3) |
| A sexually transmitted infection (STI) with syphilis, gonorrhea, or chlamydiaa | 5 (1) |
| Heterosexually active women and men (with one or more risk exposure below) | 85 (20) |
| A serodiscordant sex partner (i.e., in a sexual relationship with a partner living with HIV)a | 1 (<1) |
| Inconsistent use of condoms during sex with a partner whose HIV status is unknowna and who is at high risk (e.g., a person who injects drugsb or a man who has sex with men and women)a | 70 (17) |
| An STI with syphilis, gonorrhea, or chlamydiaa | 15 (4) |
| Individuals who engage in transactional sex and have 1 of the following characteristics | 50 (12) |
| A serodiscordant sex partner (i.e., in a sexual relationship with a partner living with HIV)a | 0 (0) |
| Inconsistent use of condoms during sex with a partner whose HIV status is unknowna and who is at high risk (e.g., a person who injects drugsb or a man who has sex with men and womena) OR Inconsistent use of condoms during receptive or insertive anal sex (if MSM)a | 44 (10) |
| An STI with syphilis or gonorrheaa | 8 (2) |
In the past 12 months.
Ever reported (based on participant knowledge of partner's behavior).
PrEP, preexposure prophylaxis; NHBS, National HIV Behavioral Surveillance; MSM, men who have sex with men.
A total of 290 HIV-negative PWID were indicated for PrEP based on injection exposure only (69%, 290/423) (Figure 1) compared with nearly a quarter of participants in both sexual and injection exposure category (i.e., multiple risk exposures PrEP indication; 23%, 96/423) (Figure 2). A significantly higher proportion of participants with multiple risk exposures were male (91%, 87/96) compared with 56% (162/290) of participants with injection-only exposure and 65% (22/34) of participants not indicated for PrEP (p<0.001). Those with multiple risk exposures had a higher proportion of participants recently incarcerated (49%, 47/96) compared with 37% (107/290) of participants with injection-only exposure and 26% (9/34) of non-indicated participants (p=0.033). Having ≥1 disability was reported by a higher proportion of participants in the multiple risk exposures category (89%, 85/96) compared with 80% (231/290) of participants indicated from injection exposure only and 71% (24/34) of those not indicated for PrEP (p=0.013).
Figure 2.
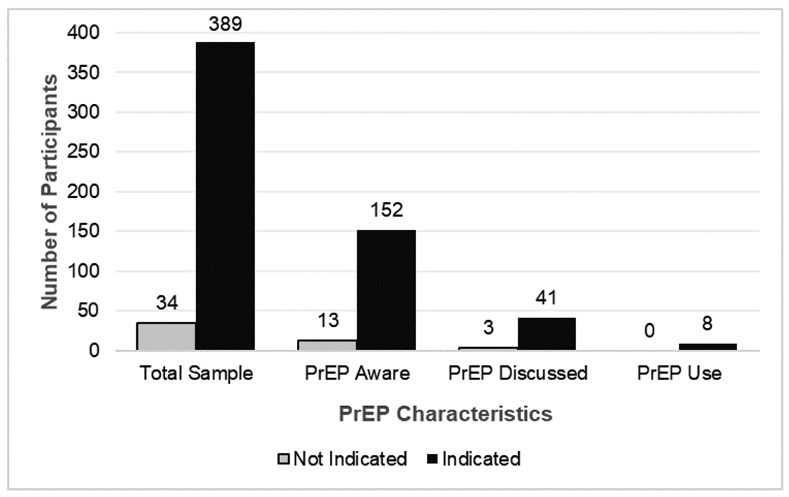
PrEP care continuum among 423 PWID by indication status in Greater Boston Area, Massachusetts, NHBS 2018.
PrEP, preexposure prophylaxis; PWID, people who inject drugs; NHBS, National HIV Behavioral Surveillance.
Injection frequency did not statistically differ across categories of PrEP indication (p<0.681). Stimulant use (injection or non-injection) was reported by a higher proportion of participants in the multiple risk exposures category (94%, 90/96) compared with 88% (254/290) of participants indicated based on only injection exposure and 82% (28/34) of participants not indicated for PrEP (p=0.013). A higher proportion of participants in the multiple risk exposures category reported overdosing on heroin or painkillers in the past 12 months (55%, 53/96) compared with 48% (139/290) of those indicated based on injection exposure only and 24% (8/34) of participants not indicated for PrEP (p=0.009).
Among those indicated for PrEP (n=389), 152 (39%) reported being aware of PrEP, 41 (11%) had discussed PrEP with a healthcare provider, and 8 (2%) had used PrEP in the past year (Figure 2). There were no statistically significant differences between PrEP-indicated and non-indicated participants along each step of the PrEP care continuum. Among the 389 PrEP-indicated participants, loss from this continuum occurred as follows. From PrEP indication to PrEP knowledge, 61% of participants were lost owing to a lack of awareness. From PrEP awareness to PrEP discussions with healthcare providers, 73% were lost because of no PrEP discussions with healthcare providers. From PrEP discussions with healthcare providers to actual PrEP use, 80% were lost owing to never having started PrEP.
DISCUSSION
Based on USPSTF guidelines, 92% of PWID in the Boston NHBS had an indication for PrEP, but only 2% were using it. Increasing prevalence of injection drug use and related HIV outbreaks signal a critical opportunity for expanded access to PrEP and other essential HIV prevention services for PWID, and understanding PrEP need in this population can help inform programmatic and implementation efforts.
The vast majority of PWID in this sample were indicated for PrEP because they reported injection exposures that increase the risk of HIV transmission, reflecting an urgent need for prevention efforts as opioid and polysubstance use continue to drive HIV outbreaks.17 Despite the very high proportions of PWID in Boston who reported having health insurance, routine sources of medical care, past-year visits with healthcare providers, and access to harm-reduction services, most participants still reported engaging in past-year receptive syringe sharing, highlighting the need to expand access to PrEP and other HIV prevention services.34 Moreover, fentanyl is increasingly present in illicit drug supplies in Massachusetts and is associated with increased injection frequency,11,35 underscoring the need for increased supply of syringes available to this population.34
Although most PWID had PrEP indication due to injection exposure, nearly a quarter were also indicated because of sexual exposure that increases risk of HIV acquisition. This “multiple risk” subsample (i.e., PWID reporting both injection and sexual exposures indicating them for PrEP) had higher levels of stimulant use, including methamphetamine injection, than the rest of the sample. Stimulant use, particularly involving methamphetamine, has been associated with increased engagement in sexual exposures that increase HIV transmission among PWID36,37 as well as high levels of injection equipment sharing.38 This is concerning as recent data reveal that stimulant-related deaths in Massachusetts increased >300% from 2000–2018,39 and nationally, there was a >5-fold increase in the drug overdose death rate involving psychostimulants (including methamphetamine).40 These trends have important implications for PrEP need among PWID in the Northeast and other regions of the country as well.
In addition to identifying the high prevalence of PrEP indication in this sample of PWID, aspects of the PrEP Care Continuum were examined.33 Beginning with PrEP awareness, 39% of participants reported being aware of PrEP before the interview, which did not significantly differ between those with and without PrEP indication. This is a higher level than what has been found in other studies with PWID in metropolitan areas, in which awareness ranged from 12% to 31%.26,41,42 A recent study with PWID in 2 urban centers in the U.S. Northeast (including PWID in the Greater Boston Area) found that, although 36% of participants expressed awareness of PrEP, interviews revealed limited factual understanding of it and confusion with post-exposure prophylaxis.24 Professional key informants attributed this low knowledge to PrEP programming failures, including marketing focused on other populations (e.g., men who have sex with men) and healthcare providers’ reluctance to prioritize discussing PrEP with PWID. Combined with low PrEP knowledge, limited HIV risk perceptions among PWID in this region could also limit PrEP uptake.3,24,25 Communicating about injection and sexual exposures that increase HIV risk could help motivate individuals to take up PrEP. At the same time, efforts to improve accurate knowledge of how PrEP works, the significance of adherence, and where to obtain it could also help increase PrEP uptake,24 because although PrEP awareness may be improving over time,30,43 accurate knowledge is essential to optimizing its use over time.
Moving along the PrEP Care Continuum, dramatic declines in the proportions of PWID reporting discussions about PrEP with healthcare providers (11% of those indicated for PrEP) and actually using PrEP were observed (only 2% of those indicated for PrEP). There were no significant differences along the PrEP care continuum between PWID with and without indications for PrEP, suggesting that PrEP uptake outcomes are no better for those that may actually benefit the most. As previous research has identified low willingness of providers to prescribe PrEP to PWID,44 studies should explore reasons for this and identify intervention targets at the provider and clinical systems levels. Additional interventions will be needed to address the extremely low PrEP use among PWID, including those that target individual-level factors (e.g., low PrEP motivation), interpersonal challenges (e.g., stigma), and clinical and structural-level barriers (e.g., complex PrEP protocol, decentralized care, and transportation difficulties).24,25,45
Limitations
This study is not without limitations. First, respondent-driven sampling helps obtain representative samples of PWID at risk of HIV46 but NHBS does not provide weights for single-site analyses; therefore, results may not be generalizable to the greater Boston PWID population. Additionally, findings may not generalize to less-insured populations or more rural and underserved communities that have also been adversely affected by injection drug use.47 Third, detecting statistically significant differences between non-indicated and indicated PWID may have been limited by small numbers. Fourth, although the use of illicitly manufactured fentanyl is rising in Massachusetts35 and could be an important factor to consider in research on PrEP with PWID, NHBS did not assess fentanyl use. Fifth, levels of PrEP indication were assessed rather than clinical eligibility, which would require additional patient evaluation. Finally, PrEP indication categories describe varying degrees of HIV risk that were not captured in these analyses (e.g., numbers and types of sexual and injection partners).
CONCLUSIONS
In this sample of PWID in Boston in 2018, PrEP indication according to USPSTF guidelines was extremely high but discussions with providers were uncommon, and actual PrEP use was very low. Taken together, these findings reveal a high unmet need for PrEP among PWID in this area and underscore the need for PrEP uptake interventions tailored for PWID. With increasing HIV outbreaks fueled by opioid use and injection involving fentanyl,17,35 polysubstance use including stimulants, prevalent sexual exposures that increase the risk for HIV transmission, and suboptimal healthcare utilization among PWID with access to care, efforts to improve PrEP provision to this socially marginalized population should be a public health priority.
Supplementary Material
ACKNOWLEDGMENTS
The content of this study is the sole responsibility of the authors and does not necessarily represent the views of the funders. Publication of the study results was not contingent on the sponsor’s approval of the manuscript.
ARB and JJE are supported by NIH grant K01DA043412. ARB and KBB are supported by the Providence/Boston Center for AIDS Research (NIH grant P30AI042853) and NIH grant R01DA051849. ARB is supported by the BU Peter Paul Career Development Professorship. RMK was supported by the Centers for Disease Control and Prevention Cooperative Agreement No. NU62PS005074-02-03.
JJE, ARB, and RMK designed the study. JJE conducted the literature review and wrote the first draft of the manuscript. JJE and RMK undertook data management and JJE conducted statistical analyses with input from ARB, KBB, and RMK. JJE and RMK had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors reviewed, contributed revisions, and approved of the final manuscript.
No financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Adams J HIV outbreak in Indiana. N Engl J Med. 2015;373(14): 1379–1381. 10.1056/nejmc1510396#SA1. [DOI] [PubMed] [Google Scholar]
- 2.Zibbell JE, Iqbal K, Patel RC, et al. Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years — Kentucky, Tennessee, Virginia, and West Virginia, 2006–2012. MMWR Morb Mortal Wkly Rep. 2015;64(17):453–458. [PMC free article] [PubMed] [Google Scholar]
- 3.Cranston K, Alpren C, John B, et al. Notes from the field: HIV diagnoses among persons who inject drugs — Northeastern Massachusetts, 2015–2018. MMWR Morb Mortal Wkly Rep. 2019;68(10):253–254. 10.15585/mmwr.mm6810a6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Golden MR, Lechtenberg R, Glick SN, et al. Outbreak of human immunodeficiency virus infection among heterosexual persons who are living homeless and inject drugs — Seattle, Washington, 2018. MMWR Morb Mortal Wkly Rep. 2019;68(15):344–349. 10.15585/mmwr.mm6815a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pennsylvania Department of Health Bureau of Epidemiology. 2018 Annual HIV Surveillance Summary Report. https://www.health.pa.gov/topics/Documents/Programs/HIV/2018%20Annual%20HIV%20Surveillance%20Report.pdf. Published 2019. Accessed October 8, 2020. [Google Scholar]
- 6.Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Treatment Episode Data Set (TEDS): 2017 Admissions to and Discharges from Publicly-Funded Substance Use Treatment. https://www.samhsa.gov/data/report/treatment-episode-data-set-teds-2017-admissions-and-discharges-publicly-funded-substance-use. Published 2019. Accessed October 8, 2020. [Google Scholar]
- 7.Spencer MR, Warner M, Bastian BA, Trinidad JP, Hedegaard H Drug overdose deaths involving Fentanyl, 2011–2016. Natl Vital Stat Rep. 2019;68(3): 1–19. [PubMed] [Google Scholar]
- 8.Pardo B Illicit supply of Fentanyl and other synthetic opioids: transitioning markets and evolving challenges. RAND Corporation. Published 2019. 10.7249/ct515. [DOI] [Google Scholar]
- 9.Armenian P, Vo KT, Barr-Walker J, Lynch KL. Fentanyl, fentanyl analogs and novel synthetic opioids: a comprehensive review. Neuropharmacology. 2018;134(part A):121–132. 10.1016/j.neuropharm.2017.10.016. [DOI] [PubMed] [Google Scholar]
- 10.Ciccarone D, Ondocsin J, Mars SG. Heroin uncertainties: exploring users’ perceptions of fentanyl-adulterated and -substituted ‘heroin.’ Int J Drug Policy. 2017;46:146–155. 10.1016/j.drugpo.2017.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lambdin BH, Bluthenthal RN, Zibbell JE, Wenger L, Simpson K, Kral AH. Associations between perceived illicit fentanyl use and infectious disease risks among people who inject drugs. Int J Drug Policy. 2019;74:299–304. 10.1016/j.drugpo.2019.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. HIV Infection, Risk, Prevention, and Testing Behaviors among Persons Who Inject Drugs - National HIV Behavioral Surveillance: Injection Drug Use, 23 U.S. Cities, 2015. https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-special-report-number-18.pdf. Revised May 2018. Accessed October 8, 2020. [Google Scholar]
- 13.CDC. HIV Infection, Risk, Prevention, and Testing Behaviors among Persons Who Inject Drugs – National HIV Behavioral Surveillance: Injection Drug Use, 20 U.S. Cities, 2012. https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-HSSR_NHBS_PWID_2012.pdf. Published August 2015. Accessed October 8, 2020 [Google Scholar]
- 14.Edeza A, Bazzi A, Salhaney P, et al. HIV pre-exposure prophylaxis for people who inject drugs: the context of co-occurring injection- and sexual-related HIV risk in the U.S. Northeast. Subst Use Misuse. 2020;55(4):525–533. 10.1080/10826084.2019.1673419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abdul-Quader AS, Feelemyer J, Modi S, et al. Effectiveness of structural-level needle/syringe programs to reduce HCV and HIV infection among people who inject drugs: a systematic review. AIDS Behav. 2013;17(9):2878–2892. 10.1007/s10461-013-0593-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.MacArthur GJ, Minozzi S, Martin N, et al. Opiate substitution treatment and HIV transmission in people who inject drugs: systematic review and meta-analysis. BMJ. 2012;345:e5945 10.1136/bmj.e5945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alpren C, Dawson EL, John B, et al. Opioid use fueling HIV transmission in an urban setting: an outbreak of HIV infection among people who inject drugs-Massachusetts, 2015–2018. Am J Public Health. 2020; 110(1):37–44. 10.2105/ajph.2019.305366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haffajee RL, Lin LA, Bohnert ASB, Goldstick JE. Characteristics of US counties with high opioid overdose mortality and low capacity to deliver medications for opioid use disorder. JAMA Netw Open. 2019;2(6):e196373 10.1001/jamanetworkopen.2019.6373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Canary L, Hariri S, Campbell C, et al. Geographic disparities in access to syringe services programs among young persons with hepatitis C virus infection in the United States. Clin Infect Dis. 2017;65(3):514–517. 10.1093/cid/cix333. [DOI] [PubMed] [Google Scholar]
- 20.SEP Locations, https://www.nasen.org/map/. Accessed January 8, 2020.
- 21.Choopanya K, Martin M, Suntharasamai P, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–2090. 10.1016/s0140-6736(13)61127-7. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. US Public Health Service: Preexposure Prophylaxis for the Prevention of HIV Infection in the United States - 2017 Update: A Clinical Practice Guideline, https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf. Published 2018. Accessed October 8, 2020. [Google Scholar]
- 23.Owens DK, Davidson KW, Krist AH, et al. Preexposure prophylaxis for the prevention of HIV infection: US Preventive Services Task Force Recommendation Statement. JAMA. 2019;321 (22):2203–2213. 10.1001/jama.2019.6390. [DOI] [PubMed] [Google Scholar]
- 24.Bazzi AR, Biancarelli DL, Childs E, et al. Limited knowledge and mixed interest in pre-exposure prophylaxis for HIV prevention among people who inject drugs. AIDS Patient Care STDS. 2018;32(12):529–537. 10.1089/apc.2018.0126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Biello KB, Bazzi AR, Mimiaga MJ, et al. Perspectives on HIV pre-exposure prophylaxis (PrEP) utilization and related intervention needs among people who inject drugs. Harm Reduct J. 2018; 15:55 10.1186/s12954-018-0263-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sherman SG, Schneider KE, Park JN, et al. PrEP awareness, eligibility, and interest among people who inject drugs in Baltimore, Maryland. Drug Alcohol Depend. 2019;195:148–155. 10.1016/j.drugalcdep.2018.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roth A, Aumaier B, Felsher M, et al. An exploration of factors impacting pre-exposure prophylaxis eligibility and access among syringe exchange users. Sex Transm Dis. 2017;45(4):217–221. 10.1097/olq.0000000000000728. [DOI] [PubMed] [Google Scholar]
- 28.Brown CM, Jaeger JL. Increase in Newly Diagnosed HIV Infections among Persons Who Inject Drugs in Boston. Massachusetts Department of Public Health, Boston Public Health Commission. https://c4innovates.com/wp-content/uploads/praxis/Joint-HIV-Outbreak-PWID-Advisory.012519.FINAL.pdf. Published January 25, 2019. Accessed October 8, 2020. [Google Scholar]
- 29.Madoff L, Brown CM, Lo JJ. Increase in Newly Diagnosed HIV Infections among Persons Who Inject Drugs in Boston. Massachusetts Department of Public Health, Boston Public Health Commission. https://static1.squarespace.com/static/585977ce6b8f5be690f0d819/t/5e18ba6097d1414eb77b98b0/1578678880958/Joint_DPH_BPHC_clinical_advisory-HIV-FINAL+.pdf. Published January 8, 2020. Accessed October 8, 2020 [Google Scholar]
- 30.Centers for Disease Control and Prevention. National HIV Behavioral Surveillance System Round 5: Model Surveillance Protocol. https://www.cdc.gov/hiv/pdf/statistics/systems/nhbs/NHBS_Model_Protocol_Round5.pdf. Published 2018. Accessed October 21, 2020. [Google Scholar]
- 31.Lansky A, Abdul-Quader AS, Cribbin M, et al. Developing an HIV behavioral surveillance system for injecting drug users: the National HIV Behavioral Surveillance System. Public Health Rep. 2007;122(suppl 1):48–55. 10.1177/00333549071220s108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gallagher KM, Sullivan PS, Lansky A, Onorato IM. Behavioral surveillance among people at risk for HIV infection in the U.S.: the National HIV Behavioral Surveillance System. Public Health Rep. 2007;122(suppl 1):32–38. 10.1177/00333549071220s106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nunn AS, Brinkley-Rubinstein L, Oldenburg CE, et al. Defining the HIV pre-exposure prophylaxis care continuum. AIDS. 2017;31(5):731–734. 10.1097/qad.0000000000001385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Des Jarlais DC, Feelemyer J, LaKosky P, Szymanowski K, Arasteh K. Expansion of syringe service programs in the United States, 2015–2018. Am J Public Health. 2020; 110(4):517–519. 10.2105/ajph.2019.305515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Massachusetts Department of Public Health. Data Brief: Opioid-Related Overdose Death among Massachusetts Residents, https://www.mass.gov/doc/dph-opioid-related-overdose-deaths-among-ma-residents-may-2019/download. Published May 2019. Accessed October 8, 2020. [Google Scholar]
- 36.Hittner JB. Meta-analysis of the association between methamphetamine use and high-risk sexual behavior among heterosexuals. Psychol Addict Behav. 2016;30(2): 147–157. 10.1037/adb0000162. [DOI] [PubMed] [Google Scholar]
- 37.Zule WA, Costenbader EC, Meyer WJ, Wechsberg WM. Methamphetamine use and risky sexual behaviors during heterosexual encounters. Sex Transm Dis. 2007;34(9):689–694. 10.1097/01.olq.0000260949.35304.22. [DOI] [PubMed] [Google Scholar]
- 38.Glick SN, Burt R, Kummer K, Tinsley J, Banta-Green CJ, Golden MR. Increasing methamphetamine injection among non-MSM who inject drugs in King County, Washington. Drug Alcohol Depend. 2018;182:86–92. 10.1016/j.drugalcdep.2017.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rate of Stimulant-Related Overdose Deaths in Combination with Any Opioid by Gender, MA Residents: 2000-2018. https://www.mass.gov/doc/data-brief-trends-in-stimulant-related-overdose-deaths-february-2020/download. Published 2000. Accessed October 21, 2020. [Google Scholar]
- 40.Hedegaard H, Miniño AM, Warner M. Drug overdose deaths in the United States, 1999–2018. NCHS Data Brief. 2020;356:1–8. https://www.cdc.gov/nchs/data/databriefs/db356-h.pdf. Accessed October 8, 2020. [PubMed] [Google Scholar]
- 41.Walters SM, Reilly KH, Neaigus A, Braunstein S. Awareness of pre-exposure prophylaxis (PrEP) among women who inject drugs in NYC: the importance of networks and syringe exchange programs for HIV prevention. Harm Reduct J. 2017;14:40 10.1186/s12954-017-0166-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Roth A, Tran N, Piecara B, Welles S, Shinefeld J, Brady K. Factors associated with awareness of pre-exposure prophylaxis for HIV among persons who inject drugs in Philadelphia: National HIV Behavioral Surveillance, 2015. AIDS Behav. 2019;23:1833–1840. 10.1007/s10461-018-2293-0. [DOI] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention. National HIV Behavioral Surveillance System Round 4: Model Surveillance Protocol. https://www.cdc.gov/hiv/pdf/statistics/systems/nhbs/nhbs_round4modelsurveillanceprotocol.pdf. Published 2015. Accessed October 21, 2020. [Google Scholar]
- 44.Edelman EJ, Moore BA, Calabrese SK, et al. Primary care physicians’ willingness to prescribe HIV pre-exposure prophylaxis for people who inject drugs. AIDS Behav. 2017;21(4): 1025–1033. 10.1007/s10461-016-1612-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Biancarelli DL, Biello KB, Childs E, et al. Strategies used by people who inject drugs to avoid stigma in healthcare settings. Drug Alcohol Depend. 2019;198:80–86. 10.1016/j.drugalcdep.2019.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Solomon SS, McFall AM, Lucas GM, et al. Respondent-driven sampling for identification of HIV- and HCV-infected people who inject drugs and men who have sex with men in India: a cross-sectional, community-based analysis. PLoS Med. 2017; 14(11):e1002460 10.1371/journal.pmed.1002460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Massachusetts Department of Public Health. An Assessment of Opioid-Related Overdoses in Massachusetts 2011–2015. https://www.mass.gov/doc/data-brief-chapter-55-opioid-overdose-study-august-2017/download. Published August 2017. Accessed October 8, 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


