Abstract
Local dynamic running stability is the ability of a dynamic system to compensate for small perturbations during running. While the immediate effects of footwear on running biomechanics are frequently investigated, no research has studied the long-term effects of barefoot vs. shod running on local dynamic running stability. In this randomized single-blinded controlled trial, young adults novice to barefoot running were randomly allocated to a barefoot or a cushioned footwear running group. Over an 8-week-period, both groups performed a weekly 15-min treadmill running intervention in the allocated condition at 70% of their VO2 max velocity. During each session, an inertial measurement unit on the tibia recorded kinematic data (angular velocity) which was used to determine the short-time largest Lyapunov exponents as a measure of local dynamic running stability. One hundred running gait cycles at the beginning, middle, and end of each running session were analysed using one mixed linear multilevel random intercept model. Of the 41 included participants (48.8% females), 37 completed the study (drop-out = 9.7%). Participants in the barefoot running group exhibited lower running stability than in the shod running group (p = 0.037) with no changes during the intervention period (p = 0.997). Within a single session, running stability decreased over the course of the 15-min run (p = 0.012) without differences between both groups (p = 0.060). Changing from shod to barefoot running reduces running stability not only in the acute phase but also in the longer term. While running stability is a relatively new concept, it enables further insight into the biomechanical influence of footwear.
Subject terms: Musculoskeletal system, Biophysics, Outcomes research, Clinical trial design
Introduction
Barefoot vs. shod running has achieved an increased public and scientific attention over the last years with advocates on both sides of the cushioning spectrum1–4. Studies focussing on barefoot running primarily investigate biomechanical, physiological or injury-related outcomes and a final conclusion on its benefits or detriments still needs to be determined5.
While the dependence of various biomechanical variables on footwear and their implications on injuries has been frequently investigated over the last decades6–10, nonlinear running gait features have rarely been addressed11–13. On the basis of nonlinear time series analysis, the local dynamic stability or running stability can be calculated11,12,14. In the current literature, this was done based on the vertical trunk coordinates11,14 as well as on the angular velocity data of the thorax, pelvis or foot12. Small internal or external perturbations are present during each movement and affect the neuromuscular and locomotion system15. To quantify, how well the locomotion system responds to these small perturbations during walking and running, the largest Lyapunov exponent can be used15,16 as a measure of local dynamic running stability (also known as local dynamic stability; LDS). Local dynamic running stability is defined as the ability of a dynamic system to compensate for small perturbations during running. While for walking a low capacity of compensating for small perturbations (reduction of LDS) can directly be translated into clinical relevance (increased risk of falls)15,17, for running the direct causal link is still missing. However, a lower running stability with the associated lower capacity of compensation for small perturbations may increase the risk for overuse injuries such as bone stress injuries resulting from repetitive monotonous loads that exceed bone loading capacity18,19.
Running stability can be affected by running surface, footwear (stability based on the vertical trunk displacement)11,14, running experience (stability based on the angular velocity of the foot) and fatigue (stability based on the angular velocity of the pelvis and trunk)12. It has also been shown that the running stability increases during an exertional 5000 m run (measured at the beginning, the middle and the end of the run, stability based on the angular velocity of the pelvis) and is higher in elite runners compared to recreational runners (stability based on the angular velocity of the foot)12. Furthermore, Ekizos, et al.11 found a decreased running stability (based on the vertical trunk displacement) when habitually shod runners change to barefoot running. This decreased running stability was accompanied by the same changes of running gait parameters seen in other studies, such as a more anterior foot strike pattern, increased cadence, decreased step length and reduced contact time11,20,21. In another study, decreased running stability was induced after changing from a rearfoot strike pattern to a more anterior strike pattern in the short term22. However, the differences were alleviated after a 14-week transition to the more anterior footstrike pattern and, thus, discussed to be a reaction of the locomotor system to a new running strategy22. While the specific physiological mechanisms that influence running stability are unclear, it can be assumed that running barefoot challenges the sensorimotor system in habitual shod runners11,23,24.
While many studies investigated acute effects of barefoot vs. shod running, some recent studies investigated effects of barefoot vs. shod running on biomechanics over time7,25,26. However, the effect of repeated test conditions period of running barefoot vs. shod running on running stability has not been investigated.
Therefore, this study aimed to determine the effects of repeated test conditions to barefoot running on nonlinear biomechanics, measured as running stability. The running stability is expressed by the largest Lyapunov exponent based on the angular velocity of the tibia. We hypothesized that a new unfamiliar situation of barefoot running (compared to shod running) would show a decreased running stability in the beginning and that this difference would alleviate over seven sessions in an 8-week period.
Methods
Study design
This study was part of a randomized single-blinded controlled study with an intervention lasting 8 weeks. Results from this study regarding the overall outcomes have already been reported elsewhere27,28 and this study analysed weekly measurements during the individual intervention sessions. The reporting of this study adhered to the CONSORT (Consolidated Standards of Reporting Trials) statement29 and it was registered in the German Clinical Trial Register (DRKS00011073, date of registration: 11/01/2017). This study was approved by the institutional review board of the University of Hamburg (protocol number ID37) and all research was performed in accordance with relevant guidelines/regulations. Informed written consent was obtained from all participants.
Participants and setting
Physically active and habitually shod participants between 18 and 35 years of age were recruited from the university surrounding (Table 1). Participants were novice to barefoot running and no specific running experience was required. Further exclusion criteria were a habituation to any barefoot or minimally shod sports (e.g. barefoot running, beach volleyball, taekwondo, karate, ballet, gymnastics) and any injury or neuromuscular disease in the six months prior to study. The recruitment and conduct took place between April 2016—April 2017 in the university biomechanics laboratories.
Table 1.
Mean ± standard deviation of participant demographics.
| Barefoot intervention group (n = 21) | Footwear intervention group (n = 20) | |
|---|---|---|
| Age [years] | 25.2 ± 3.4 | 25.2 ± 2.9 |
| Height [cm] | 175.3 ± 7.6 | 177.7 ± 8.3 |
| Weight [kg] | 71.3 ± 12.2 | 71.4 ± 10.8 |
| BMI [kg/m2] | 23.0 ± 2.5 | 22.5 ± 1.9 |
| Sex (percentage females) | 52.4% | 50.0% |
Interventions and randomisation
Block randomization was performed by the same research team member with stratification for sex. Participants were assigned to a barefoot or a shod intervention group. There was a third passive group that did not perform any running intervention28. Since such a passive group is not relevant for the analysis of the hypothesis, the data of this group was not analysed in this study.
The researcher (DH) involved in the data processing and statistical analysis was blinded to study arm allocation. Participants and researchers administering the treatment were not able to be blinded.
Intervention
After conducting a VO2max test on a treadmill (Quark CPET COSMED, Rome, Italy)30 in week one, participants received seven intervention sessions in the allocated footwear condition. The seven sessions were one week (± 1 day) apart from each other and consisted of 15 min of running on an instrumented treadmill at 70% of their individual VO2max velocity to prevent exhaustive effects (TRAC 4000, Ergo-Fit GmbH & Co. KG, Pirmasens, Germany). Participants were allowed to miss a maximum of one session to be included in the final analysis.
For the shod intervention, a new cushioned running shoe (Asics Cumulus 17, 10 mm heel drop, neutral arch support, weight: 336 g for US size male 9) was individually used for every participant and stayed in the laboratory during the conduct of the study. The barefoot intervention was conducted barefoot. Participants were allowed to continue their physical activity/sports in their usual footwear but were requested to not initiate any barefoot sport.
Instrumentation
To register running gait kinematics, an inertial measurement unit (IMU, Shimmer3, Shimmer, Dublin, Ireland; gyroscope range of measurement: ± 2000°/s; sampling rate: 256 Hz) was fixed to the tibia (medial and distal to the tibial tuberosity) with an elastic strap. The measurement was started while the participants were standing on the treadmill.
Data processing
The unfiltered IMU data (three-dimensional angular velocity) was exported using the software Consensys (version 1.6, Shimmer, Dublin, Ireland). The following data processing was conducted with self-made MATLAB (version 2014a; The MathWorks, Inc., Natick, USA) scripts. Since the measurement was started and stopped while the participant stood on the treadmill, the start and end of the running sessions were visually detected.
Primary outcome
As a prerequisite for calculating LDS foot–ground contacts were identified as local minima of the angular velocity of the sagittal plane as described previously for human gait31. Thereafter, the first and last 50 running gait cycles were excluded from the following data analysis.
The primary outcome of this study was the running stability measured as the LDS. LDS has frequently been used to assess non-linear walking biomechanics and less frequently been applied to running biomechanics11,12,22,32. We calculated the LDS based on the angular velocity data of the tibia from the first, middle and last 100 running gait cycles of each session. The method to determine LDS has been described extensively33,34. In brief, the three-dimensional angular velocity data of each 100 consecutive running gait cycles were time-normalized to 10,000 samples35. To reconstruct a state space, we applied the time-delayed embedding method. The time delay (τ) was chosen based on the first minimum mutual information analysis36 which was determined for each plane separately (x-axis [mean ± standard deviation]: τ = 7.6 ± 1.7; y-axis: τ = 12.2 ± 2.4; z-axis: τ = 11.8 ± 2.2). The mean (τ = 11) was used as a fixed time delay in each state space reconstruction for all participants. The embedding dimension (dE) was determined using the global false nearest neighbour analysis37. False neighbors were identified by comparing the actual state space with a state space including an additional time delayed copy of the 3D kinematic data (Rtol = 15.0 and Atol = 2.0). Therefore, dE could only be a multiple of 3 (e.g. dE = 3, dE = 6, dE = 9 etc.). Since the attractor formed using delayed reconstruction is equivalent to the attractor in the unknown space of the original system only if the embedding dimension is sufficiently large, we used the maximum dE across all participants as the fixed embedding dimension (maximum dE = 9, mean dE = 6.2, standard deviation of the dE = 0.3)38. Taken together, the following state space ‘S(t)’ was reconstructed:
with ‘a’ representing the angular velocity data (the subscript indicates the corresponding sensor axis) and τ the time delay (in our case 11).
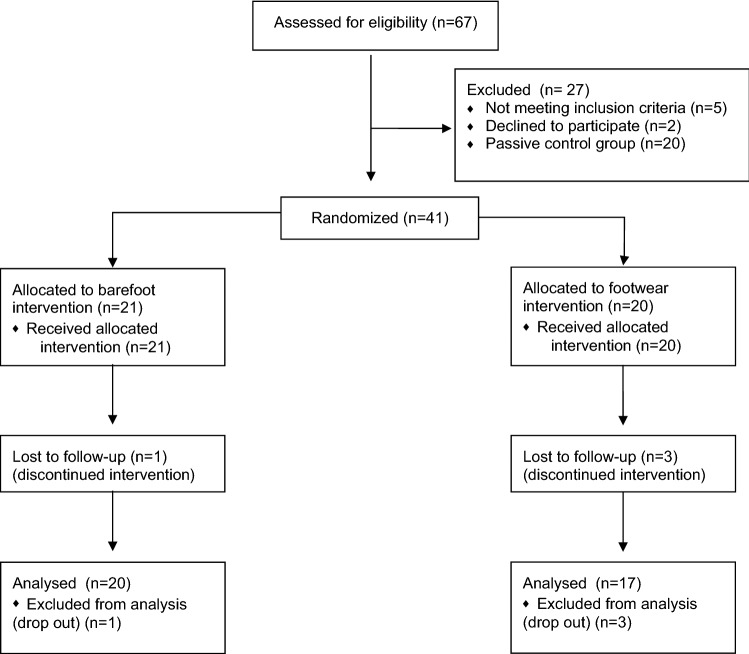
The short-time largest Lyapunov exponent was calculated upon the state space using the algorithm of Rosenstein, et al.39. Thereto, for each point in the state space, we searched for the nearest neighbour (Euclidean distance) and tracked the distance of the initially nearest neighbour as it evolves in time. The short-time largest Lyapunov exponent is then defined as the slope of the linear fit of the mean of the logarithm of these divergence curves. Based on a visual inspection (Fig. 1) of the mean of the logarithm of this divergence curves, we fitted the line to a time frame representing the first 5% (5 time-normalised samples) of the running gait cycle.
Figure 1.
Divergence curve (mean across participants of the middle of the 15-min sessions)
Statistical methods
We used a linear multi-level random intercept model (level 1: measurement within each participant; level 2: participants) to analyse the fixed effects group (barefoot vs. shod running), intersession time (the 7 sessions), and intrasession time (the beginning, middle and end of each session) on LDS (the largest Lyapunov exponent). Furthermore, all possible interaction effects were included into the model. The model was analysed using the restricted maximum likelihood (REML) estimator in IBM SPSS Statistics for Windows (Version 22.0. Armonk, NY: IBM Corp). Differences between groups were compared with independent t-tests (age and BMI) and Fisher’s excact χ2 test. The significance level was set to α = 5%.
Results
Participants
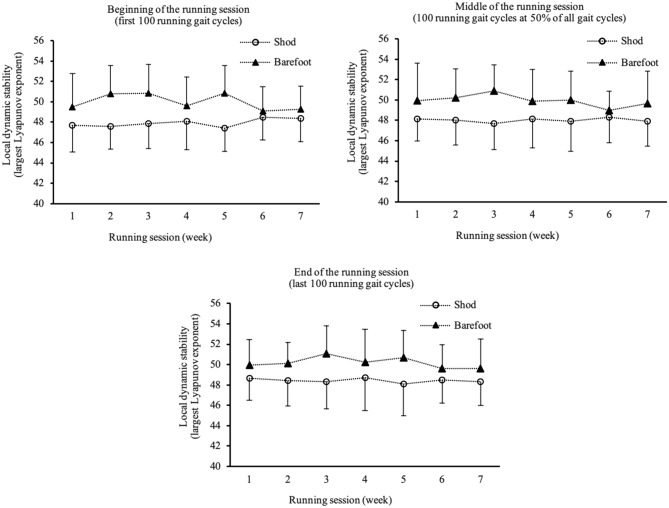
Overall, 41 participants were included in this randomised controlled trial (48.8% females, mean ± SD age 25.2 ± 3.1 years, BMI 22.8 ± 2.2 kg/m2) with no statistically significant differences between groups for age (p = 0.992), BMI (p = 0.424) or sex (p = 1.000) (Table 1). Three participants discontinued the intervention in the shod and one participant in the barefoot group (drop-out-rate: 9.7%). Reasons for the drop-outs were not related to the intervention (three illnesses and one anterior cruciate ligament rupture). The overall adherence with the training session was 97.3% (98.5% in the shod group and 96.3% in the barefoot group). The participant flow through the study can be found in Fig. 2. There were no adverse events during the conduct of the study.
Figure 2.
Flowchart of participants.
Decreased running stability during barefoot running compared to shod running
We found a significant group effect, participants in the barefoot running condition exhibited lower running stability compared to participants running shod (t(group) = 2.1, p = 0.037, b = 1.924). This group effect was existent in the first session, over the course of the intervention and this difference remained unchanged (t(group*intersession time) = −0.5, p = 0.633, b = −0.045). No effect of the intersession time was shown (t(intersession time) < 0.1, p = 0.997, b < 0.001) (Table 2). Taken together, there was a significant group effect (barefoot vs. shod running) that remained unchanged within the session as well as across the sessions.
Table 2.
Effects of group (shod n = 17; barefoot n = 20), intersession time (the 7 sessions), intrasession time (the beginning, middle, and end of each session), and all possible interaction effects on dynamic running stability (the largest Lyapunov exponent).
| Fixed effects | b | t (df) | p | 95% CI |
|---|---|---|---|---|
| Intercept | 47.998 | 76.597 (52.746) | < 0.001 | [46.741 to 49.255] |
| Intrasession time | 0.579 | 2.521 (510.645) | 0.012 | [0.128 to 1.030] |
| Group (reference: shod = 0) | 1.924 | 2.137 (52.840) | 0.037 | [0.118 to 3.729] |
| Intersession time | 0.000 | 0.004 (512.140) | 0.997 | [−0.126 to 0.127] |
| Intrasession time * Group | −0.612 | −1.881 (510.639) | 0.060 | [−1.252 to 0.027] |
| Intrasession time * Intersession time | −0.082 | −1.680 (510.641) | 0.094 | [−0.178 to 0.014] |
| Group * Intersession time | −0.045 | −0.478 (513.141) | 0.633 | [−0.228 to 0.139] |
| Intersession time * Group * Intrasession time | 0.113 | 1.596 (510.637) | 0.111 | [−0.026 to 0.253] |
| Random effects | Estimates | Wald Z | p | 95% CI |
|---|---|---|---|---|
| Residual | 1.922 | 15.979 | < 0.001 | [1.700 to 2.173] |
| Intercept | 5.385 | 3.924 | < 0.001 | [3.268 to 8.873] |
The effects were analysed with a linear 2 level random intercept model.
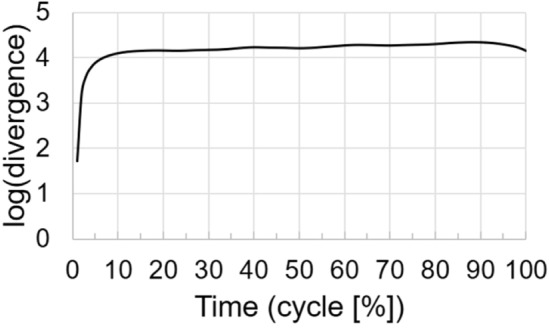
Running stability within a running session
Within the 15-min running sessions (from the beginning to the middle to the end of each session), running stability decreased (t(intrasession time) = 2.5, p = 0.012, b = 0.579) in both groups (Table 2 and Fig. 3). There was a non-significant tendency that the decrease in running stability within a session was not as pronounced in the barefoot running group compared to shod running group (t(intrasession time*group) = −1.9, p = 0.060, b = −0.612).
Figure 3.
Local dynamic (running) stability (largest Lyapunov exponent) depicted for all seven running sessions for the beginning (3a), middle (3b) and end (3c) of the 15-min sessions.
Discussion
This randomized-controlled trial presents the results of a barefoot vs. shod running intervention over seven sessions on running stability. Running stability was lower in the barefoot running group compared to the shod running group, which was already existent in the first session. Furthermore, running stability did not change over the course of the intervention period, but was reduced over a single session of 15 min of running.
Running barefoot versus shod affects running stability
The differences between the barefoot and shod group were existent from the first session and throughout the intervention period. A simple explanation could be a present random group effect as an alternative explanation to the interventional effect. This would be in line with a cross-over study by Frank et al.40, showing that cushioning properties of footwear seem to not acutely alter the local dynamic running stability. In contrast, with a similar cross-over design, it has been shown that running barefoot acutely affects the running stability11. When habitually shod runners switched to barefoot running, Ekizos, et al.11 described a lower running stability measured by local dynamic stability, which is in accordance with our results. While the cohort of habitually shod participants was similar, our study adds that the running stability was constantly lower over an 8-week/7-session running period in the barefoot group. While the underlying mechanisms of running stability are still mostly speculative, we expect an influence of the sensorimotor system on running stability41,42. Given the strength of a randomized controlled trial design and the finding of acute changes of footwear11, we conclude that barefoot running leads to reduced running stability compared to shod running in habitually shod runners.
Barefoot locomotion is thought to increase the sensory input (tactile and proprioceptive) and the non-habituated condition of barefoot running has been suggested to induce a less stable movement pattern11,23,24,34,43. Alternatively, footwear properties such as cushioning, flexibility and stability might also increase or decrease the running stability as it has been shown to influence several aspects of running biomechanics acutely and over time6,21,44,45. The acute changes in running stability and other biomechanics indicate that unfamiliar conditions such as a change of footwear are challenging for habitual running patterns. We expected that a repeated application to the new (barefoot) running condition would not only induce changes in foot strike patterns or ground reactions forces as seen in other studies28,46–48 but also in running stability. Another explanation could be that no full habituation was achieved over the 8 weeks with relatively few barefoot running (7 sessions of 15 min). It shall be emphasised that no running experience was required to qualify for this study and that all participants in this study were novice to barefoot running. There is no consensus what a habituated footwear status defines and there are currently no evidence-based recommendations on how to transition to (simulated) barefoot running4,7 as have been published for gait retraining protocols for injury prevention and rehabilitation49. Future investigations should focus on cohorts that are habituated for a longer period or habitually barefoot populations50.
Running stability reduces during session
The running stability measured at the tibia decreased over the course of the 15 min of running in this study. In contrast, a recent study by Hoenig, et al.12 showed that running an exhaustive 5000 m run increased the running stability measured at the pelvis and thorax, but not at the foot. However, different time-delay as well as a different embedding dimension was used in our study. While the time was comparable for the competitive group (16–19 min), the difference between studies was that the velocity run in our study was non-exhaustive at 70% of the individual runners VO2 max velocity on a treadmill. It has been shown that acute fatigue influences dynamic stability of different motor tasks, while the underlying physiological mechanisms are not well understood51–53. Asgari, et al.52 interpreted that fatigue influenced the motor control and their ability to maintain repetitive dynamic tasks. It is has been shown that a cognitive component might also influence the ability to withstand small perturbations and increase local dynamic stability at least in walking54. Therefore, one could speculate that the monotonous task of running at a low speed on an indoor treadmill might decrease the awareness and attention of the participants on our study and decrease the cognitive resources used for the locomotors system to be kept stable.
Strengths, limitations (Sources of bias) and generalizability
This was the first study to investigate repeated test condition effects of barefoot running on running stability measured by the largest Lyapunov exponent. While it can be determined from 3D motion capturing or IMU data, there is no consensus on the localisation of marker or IMU placement12,16. While Ekizos, et al.16 showed that marker clusters on the spine have high reliability to measure running stability with motion capture other studies have found different results depending on IMU location12. Further research is needed to investigate the impact of marker/IMU placement on running stability.
The population investigated consisted of active healthy adults that did not necessarily have a strong running background. Since it has been shown that the experience level of runners (recreational vs. competitive) has an effect on running stability12, caution needs no be taken when extrapolating the finding to other population, such as elite runners. As seen for biomechanics but also injuries, age and sex of the runners may also be of relevance for running stability55,56.
Recommendations for further research
While some influencing factors on running stability (footwear, fatigue, running surface, running background) have been described in the literature, currently there is a need to better understand components contributing to this concept. Considering the trend of an intrasession decrease in the barefoot group future research should consider an individual perspective of adaptations, e.g. the relevance of responders and non-responders47. While the definition of running stability (ability of a dynamic system to compensate for small perturbations) is very precise, it is still to be determined whether a runner should strive for high or low running stability. Thus, practical (for running performance) and clinical implications (for running injuries) associated with an increased or decreased running stability should be in the focus of future research. Possible intervention strategies are still at an early stage of development. However, considering the wide availability of IMUs that can be worn on the body or in textiles as ‘wearables’57–59, the concept of running stability might be a promising field for future research.
Conclusion
With good knowledge of the effects of footwear on running biomechanics, this study adds to the effects of footwear on the concept of running stability. In adults novice to barefoot running, running stability was lower in the barefoot running group when compared to the shod running group over the whole intervention period. This may be explained by long-term difficulties to adapt to the new running conditions and to develop a stable running pattern. Further studies are needed to explore if longer habituation periods to barefoot running are needed for improvements of running stability.
Ethics approval and consent to participate
This study was approved by the institutional review board of the University of Hamburg (protocol number ID37) and was prospectively registered in the German Clinical Trial Register (DRKS00011073). Written informed consent was obtained prior to participation.
Acknowledgements
The authors thank Stephanie Meining, Ann-Kathrin Otto and Dr. Katharina Lindlein for their help with data acquisition.
Author contributions
K.H. and A.Z. participated in the conception and design of the study, and the drafting of the manuscript. D.H. lead the data processing, statistical analysis and prepared the figures. All authors have contributed to, read and approved the final manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL.. Open Access funding enabled and organized by Projekt DEAL. This project was funded by the Ministry for Science and Research in Hamburg (grant number LFF-FV13). The research fellowship of KH was funded by the German Research Foundation (Grant Number HO 6214/2–1).
Data availability
All data generated or analysed during this study are included in this published article and its tables and figures, or is available upon request.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nigg B, Enders H. Barefoot running—some critical considerations. Footwear Sci. 2013;5:1–7. doi: 10.1080/19424280.2013.766649. [DOI] [Google Scholar]
- 2.Lieberman DE, et al. Foot strike patterns and collision forces in habitually barefoot versus shod runners. Nature. 2010;463:531–535. doi: 10.1038/nature08723. [DOI] [PubMed] [Google Scholar]
- 3.Hannigan JJ, Pollard CD. A 6-week transition to maximal running shoes does not change running biomechanics. Am. J. Sports Med. 2019;47:968–973. doi: 10.1177/0363546519826086. [DOI] [PubMed] [Google Scholar]
- 4.Warne JP, Gruber AH. Transitioning to minimal footwear: a systematic review of methods and future clinical recommendations. Sports Med. Open. 2017;3:33. doi: 10.1186/s40798-017-0096-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tam N, Astephen Wilson JL, Noakes TD, Tucker R. Barefoot running: an evaluation of current hypothesis, future research and clinical applications. Br. J. Sports Med. 2014;48:349–355. doi: 10.1136/bjsports-2013-092404. [DOI] [PubMed] [Google Scholar]
- 6.Hall JP, Barton C, Jones PR, Morrissey D. The biomechanical differences between barefoot and shod distance running: a systematic review and preliminary meta-analysis. Sports Med. 2013;43:1335–1353. doi: 10.1007/s40279-013-0084-3. [DOI] [PubMed] [Google Scholar]
- 7.Hollander K, Heidt C, Van der Zwaard BC, Braumann KM, Zech A. Long-term effects of habitual barefoot running and walking: a systematic review. Med. Sci. Sports Exerc. 2017;49:752–762. doi: 10.1249/MSS.0000000000001141. [DOI] [PubMed] [Google Scholar]
- 8.Hollander K, Johnson CD, Outerleys J, Davis IS. Multifactorial determinants of running injury locations in 550 injured recreational runners. Med. Sci. Sports Exerc. 2021;53:102–107. doi: 10.1249/MSS.0000000000002455. [DOI] [PubMed] [Google Scholar]
- 9.Ceyssens L, Vanelderen R, Barton C, Malliaras P, Dingenen B. Biomechanical risk factors associated with running-related injuries: a systematic review. Sports Med. 2019;49:1095–1115. doi: 10.1007/s40279-019-01110-z. [DOI] [PubMed] [Google Scholar]
- 10.Subotnick SI. A biomechanical approach to running injuries. Ann. N. Y. Acad. Sci. 1977;301:888–899. doi: 10.1111/j.1749-6632.1977.tb38256.x. [DOI] [PubMed] [Google Scholar]
- 11.Ekizos A, Santuz A, Arampatzis A. Transition from shod to barefoot alters dynamic stability during running. Gait Posture. 2017;56:31–36. doi: 10.1016/j.gaitpost.2017.04.035. [DOI] [PubMed] [Google Scholar]
- 12.Hoenig T, Hamacher D, Braumann KM, Zech A, Hollander K. Analysis of running stability during 5000 m running() Eur. J. Sport Sci. 2019;19:413–421. doi: 10.1080/17461391.2018.1519040. [DOI] [PubMed] [Google Scholar]
- 13.Schutte KH, Seerden S, Venter R, Vanwanseele B. Influence of outdoor running fatigue and medial tibial stress syndrome on accelerometer-based loading and stability. Gait Posture. 2018;59:222–228. doi: 10.1016/j.gaitpost.2017.10.021. [DOI] [PubMed] [Google Scholar]
- 14.Santuz A, Ekizos A, Eckardt N, Kibele A, Arampatzis A. Challenging human locomotion: stability and modular organisation in unsteady conditions. Sci. Rep. 2018;8:2740. doi: 10.1038/s41598-018-21018-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bruijn SM, Meijer OG, Beek PJ, van Dieen JH. Assessing the stability of human locomotion: a review of current measures. J. R. Soc. Interface. 2013;10:20120999. doi: 10.1098/rsif.2012.0999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ekizos A, Santuz A, Schroll A, Arampatzis A. The maximum lyapunov exponent during walking and running: reliability assessment of different marker-sets. Front Physiol. 2018;9:1101. doi: 10.3389/fphys.2018.01101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dingwell JB, Marin LC. Kinematic variability and local dynamic stability of upper body motions when walking at different speeds. J. Biomech. 2006;39:444–452. doi: 10.1016/j.jbiomech.2004.12.014. [DOI] [PubMed] [Google Scholar]
- 18.Matcuk GR, Jr, et al. Stress fractures: pathophysiology, clinical presentation, imaging features, and treatment options. Emerg. Radiol. 2016;23:365–375. doi: 10.1007/s10140-016-1390-5. [DOI] [PubMed] [Google Scholar]
- 19.Hoenig, T., Tenforde, A., Strahl, A., Rolvien, T. & Hollander, K. Does MRI grading correlate with return to sports following bone stress injuries? A systematic review and meta-analysis. Am J Sports Med. 10.1177/0363546521993807 (2021). [DOI] [PubMed]
- 20.Bonacci J, et al. Running in a minimalist and lightweight shoe is not the same as running barefoot: a biomechanical study. Br. J. Sports Med. 2013;47:387–392. doi: 10.1136/bjsports-2012-091837. [DOI] [PubMed] [Google Scholar]
- 21.Hollander K, Argubi-Wollesen A, Reer R, Zech A. Comparison of minimalist footwear strategies for simulating barefoot running: a randomized crossover study. PLoS ONE. 2015;10:e0125880. doi: 10.1371/journal.pone.0125880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ekizos A, Santuz A, Arampatzis A. Short- and long-term effects of altered point of ground reaction force application on human running energetics. J. Exp. Biol. 2018 doi: 10.1242/jeb.176719. [DOI] [PubMed] [Google Scholar]
- 23.Kelly LA, Lichtwark G, Cresswell AG. Active regulation of longitudinal arch compression and recoil during walking and running. J. R. Soc. Interface. 2015;12:20141076. doi: 10.1098/rsif.2014.1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Holowka NB, et al. Foot callus thickness does not trade off protection for tactile sensitivity during walking. Nature. 2019;571:261–264. doi: 10.1038/s41586-019-1345-6. [DOI] [PubMed] [Google Scholar]
- 25.Sanchez-Ramirez C, Alegre LM. Plantar support adaptations in healthy subjects after eight weeks of barefoot running training. PeerJ. 2020;8:e8862. doi: 10.7717/peerj.8862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mizushima J, et al. Long-term effects of school barefoot running program on sprinting biomechanics in children: a case-control study. Gait Posture. 2021;83:9–14. doi: 10.1016/j.gaitpost.2020.09.026. [DOI] [PubMed] [Google Scholar]
- 27.Zech A, et al. Effects of barefoot and footwear conditions on learning of a dynamic balance task: a randomized controlled study. Eur. J. Appl. Physiol. 2018;118:2699–2706. doi: 10.1007/s00421-018-3997-6. [DOI] [PubMed] [Google Scholar]
- 28.Hollander K, et al. Adaptation of running biomechanics to repeated barefoot running: a randomized controlled study. Am. J. Sports Med. 2019;47:1975–1983. doi: 10.1177/0363546519849920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schulz, K. F., Altman, D. G., Moher, D. & Group, C CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8:18. doi: 10.1186/1741-7015-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lindlein K, Zech A, Zoch A, Braumann KM, Hollander K. Improving running economy by transitioning to minimalist footwear: a randomised controlled trial. J. Sci. Med. Sport Sports Med. Aust. 2018;21:1298–1303. doi: 10.1016/j.jsams.2018.05.012. [DOI] [PubMed] [Google Scholar]
- 31.Hamacher D, Hamacher D, Taylor WR, Singh NB, Schega L. Towards clinical application: repetitive sensor position re-calibration for improved reliability of gait parameters. Gait Posture. 2014;39:1146–1148. doi: 10.1016/j.gaitpost.2014.01.020. [DOI] [PubMed] [Google Scholar]
- 32.Hamacher D, et al. Gait stability and its influencing factors in older adults. Front Physiol. 2018;9:1955. doi: 10.3389/fphys.2018.01955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hamacher D, Hamacher D, Singh NB, Taylor WR, Schega L. Towards the assessment of local dynamic stability of level-grounded walking in an older population. Med. Eng. Phys. 2015;37:1152–1155. doi: 10.1016/j.medengphy.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 34.Dingwell JB, Cusumano JP. Nonlinear time series analysis of normal and pathological human walking. Chaos. 2000;10:848–863. doi: 10.1063/1.1324008. [DOI] [PubMed] [Google Scholar]
- 35.Raffalt PC, Kent JA, Wurdeman SR, Stergiou N. Selection procedures for the largest Lyapunov exponent in gait biomechanics. Ann. Biomed. Eng. 2019;47:913–923. doi: 10.1007/s10439-019-02216-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fraser AM, Swinney HL. Independent coordinates for strange attractors from mutual information. Phys. Rev. A Gen. Phys. 1986;33:1134–1140. doi: 10.1103/physreva.33.1134. [DOI] [PubMed] [Google Scholar]
- 37.Kennel MB, Brown R, Abarbanel HD. Determining embedding dimension for phase-space reconstruction using a geometrical construction. Phys. Rev. A Atom. Mol. Opt. Phys. 1992;45:3403–3411. doi: 10.1103/physreva.45.3403. [DOI] [PubMed] [Google Scholar]
- 38.Kantz H, Schreiber T. Nonlinear Time Series Analysis. 2. Cambridge: Cambridge University Press; 2010. [Google Scholar]
- 39.Rosenstein MT, Collins JJ, De Luca CJ. A practical method for calculating largest Lyapunov exponents from small data sets. Physica D. 1993;65:117–134. doi: 10.1016/0167-2789(93)90009-p. [DOI] [Google Scholar]
- 40.Frank NS, Prentice SD, Callaghan JP. Local dynamic stability of the lower extremity in novice and trained runners while running intraditional and minimal footwear. Gait Posture. 2019;68:50–54. doi: 10.1016/j.gaitpost.2018.10.034. [DOI] [PubMed] [Google Scholar]
- 41.Federolf PA, Roos L, Nigg B. The effect of footwear on postural control in bipedal quiet stance. Footwear Sci. 2012;4:115–122. doi: 10.1080/19424280.2012.666270. [DOI] [Google Scholar]
- 42.Shultz SJ, Schmitz RJ, Tritsch AJ, Montgomery MM. Methodological considerations of task and shoe wear on joint energetics during landing. J. Electromyogr. Kinesiol. 2012;22:124–130. doi: 10.1016/j.jelekin.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 43.Hoogkamer W, et al. Toward new sensitive measures to evaluate gait stability in focal cerebellar lesion patients. Gait Posture. 2015;41:592–596. doi: 10.1016/j.gaitpost.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 44.Hoogkamer W, Kipp S, Kram R. The biomechanics of competitive male runners in three marathon racing shoes: a randomized crossover study. Sports Med. 2019;49:133–143. doi: 10.1007/s40279-018-1024-z. [DOI] [PubMed] [Google Scholar]
- 45.Warne JP, et al. Kinetic changes during a six-week minimal footwear and gait-retraining intervention in runners. J. Sports Sci. 2017;35:1538–1546. doi: 10.1080/02640414.2016.1224916. [DOI] [PubMed] [Google Scholar]
- 46.Khowailed IA, Petrofsky J, Lohman E, Daher N. Six weeks habituation of simulated barefoot running induces neuromuscular adaptations and changes in foot strike patterns in female runners. Med. Sci. Monit. 2015;21:2021–2030. doi: 10.12659/MSM.893518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tam N, Astephen Wilson JL, Coetzee DR, van Pletsen L, Tucker R. Loading rate increases during barefoot running in habitually shod runners: Individual responses to an unfamiliar condition. Gait Posture. 2016;46:47–52. doi: 10.1016/j.gaitpost.2016.02.013. [DOI] [PubMed] [Google Scholar]
- 48.Hoenig T, Rolvien T, Hollander K. Footstrike patterns in runners: concepts, classifications, techniques, and implicationsfor running-related injuries. Deutsche Zeitschrift für Sportmedizin. 2020;71:55–61. doi: 10.5960/dzsm.2020.424. [DOI] [Google Scholar]
- 49.Davis IS, Tenforde AS, Neal BS, Roper JL, Willy RW. Gait retraining as an intervention for patellofemoral pain. Curr. Rev. Musculoskelet Med. 2020;13:103–114. doi: 10.1007/s12178-020-09605-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hollander K, et al. Foot strike patterns differ between children and adolescents growing up barefoot vs. shod. Int. J. Sports Med. 2018;39:97–103. doi: 10.1055/s-0043-120344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Granata KP, Gottipati P. Fatigue influences the dynamic stability of the torso. Ergonomics. 2008;51:1258–1271. doi: 10.1080/00140130802030722. [DOI] [PubMed] [Google Scholar]
- 52.Asgari N, Sanjari MA, Esteki A. Local dynamic stability of the spine and its coordinated lower joints during repetitive Lifting: Effects of fatigue and chronic low back pain. Hum. Mov. Sci. 2017;54:339–346. doi: 10.1016/j.humov.2017.06.007. [DOI] [PubMed] [Google Scholar]
- 53.Hamacher D, et al. Effects of physical exhaustion on local dynamic stability and automaticity of walking. Gait Posture. 2018;66:135–138. doi: 10.1016/j.gaitpost.2018.08.031. [DOI] [PubMed] [Google Scholar]
- 54.Hamacher D, Schley F, Hollander K, Zech A. Effects of manipulated auditory information on local dynamic gait stability. Hum. Mov. Sci. 2018;58:219–223. doi: 10.1016/j.humov.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 55.Krabak BJ, et al. Youth running consensus statement: minimising risk of injury and illness in youth runners. Br. J. Sports Med. 2020 doi: 10.1136/bjsports-2020-102518. [DOI] [PubMed] [Google Scholar]
- 56.Hollander, K. et al. Sex-specific differences in running injuries: a systematic review with meta-analysis and meta-regression. Sports Med. 10.1007/s40279-020-01412-7 (2021). [DOI] [PMC free article] [PubMed]
- 57.Machulik M, Hamacher D, Lindlein K, Zech A, Hollander K. Validation of an inertial measurement unit based magnetictiming gate system during running and sprinting. Deutsche Zeitschrift für Sportmedizin. 2020;71:69–75. doi: 10.5960/dzsm.2020.426. [DOI] [Google Scholar]
- 58.Hollander K. Biomechanik des Laufens—Implikationen für laufbedingte Verletzungen und zukünftige Forschungsfelder. Deutsche Zeitschrift für Sportmedizin. 2020;71:53–54. doi: 10.5960/dzsm.2019.411. [DOI] [Google Scholar]
- 59.Johnson CD, et al. Comparison of tibial shock during treadmill and real-world running. Med. Sci. Sports Exerc. 2020;52:1557–1562. doi: 10.1249/MSS.0000000000002288. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article and its tables and figures, or is available upon request.