Abstract
COVID-19 is spreading rapidly in Brazil, a country of continental dimensions, but the incidence of the disease is showing to be very heterogeneous, affecting cities and regions differently. Thus, there is a gap regarding what factors would contribute to accentuate the differences in the incidence of COVID-19 among Brazilian cities. This work aimed to evaluate the effect of altitude on the incidence of COVID-19 in Brazilian cities. We analyzed the relative incidence (RI), the relative death rate (RDR) of COVID-19, and air relative humidity (RH) in all 154 cities in Brazil with a population above 200 thousand inhabitants, located between 5 and 1135 m in altitude. Pearson's correlation analysis was performed to compare a relationship between altitude with RI and RDR, and between RH with RI and RDR. Altitudes were classified into three classes [low (altitude ≤ 97 m a. s. l), middle (97 < altitude ≤ 795 m a. s. l), high (795 < altitude ≤ 1135 m a. s. l)] for the RI, RDR, and RH variables. To compare the three classes of altitude, analysis of variance (ANOVA) and Tukey test were used to compare averages (p < 0.05). Our epidemiological analysis found that the RI, RDR, and RH were lower in cities located in high altitudes (795 < altitude ≤ 1135 m a. s. l) when compared to the middle (97 < altitude ≤ 795 m a. s. l) and low (altitude ≤ 97 m a. s. l) cities altitudes. Furthermore, our study shows that there is a negative correlation between the incidence of COVID-19 with altitude and a positive correlation with RH in the cities analyzed. Brazilian cities with high altitude and low RH have lower RI and RDR from COVID-19. Thus, high altitude cities may be favorable to shelter people at risk. This study may be useful for understanding the behavior of SARS-CoV2, and start point for future studies to establish causality of environmental conditions with SARS-CoV2 contributing to the implementation of measures to prevent and control the spread of COVID-19.
Subject terms: Environmental sciences, Environmental social sciences, Diseases, Health care, Medical research
Introduction
In December 2019, a new coronavirus was identified—initially called 2019-nCoV and later renamed SARS-CoV-2—in Hubei province, People's Republic of China1. The pathogen causes coronavirus-19 disease (COVID-19), which spread rapidly, reaching the pandemic level on March 11, 20202. The incidence of cases and deaths caused by COVID-19 in the world increased at different rates from the first cases. In Brazil, a country of continental dimensions, the spread of the disease is very heterogeneous, affecting cities and regions differently.
Efforts to minimize its spread are announced every minute in the media. Also, thousands of searches worldwide are focused on the various nuances of COVID-19. However, studies that relate to the incidence of the disease to environmental factors are incipient, especially in countries like Brazil, which stands out for its great socioeconomic and environmental diversity2. As the behaviour of COVID-19 concerning climatic attributes is still poorly understood, investigating the influence of altitude and environmental characteristics of cities on the incidence and deaths caused by COVID-19 can generate results that contribute to the development of public policies that minimize the spread of the disease.
In Brazil, COVID-19 began to be disseminated from large cities located in the coastal zone, that have high air relative humidity (RH), and quickly reached the interior, but the contamination speed of the population is not homogeneous2. Some cities have higher incidence and deaths from COVID-19 than other cities with similar numbers of inhabitants. About that, some questions were raised about the differences between the records of infection and deaths between cities. What factors would be able to contribute to accentuate these differences in the incidence of COVID-19 among Brazilian cities? Thus, the hypothesis arose that cities located at higher altitudes are less favourable for the spread of COVID-19.
Since, cities outside the coastal zone with a high incidence of COVID-19, such as Manaus—Amazonas, are located at low altitudes (< 100 m a. s. l). Brazil has 154 cities with a population above 200 thousand inhabitants located at altitudes ranging from 5 to 1135 m a. s. l. The incidence of COVID-19 in these cities is not similar. Could altitude be a determining factor that would influence the incidence of this virus?
During the survey of epidemiological data from Brazil, in May 2020, a study was published showing the relationship between altitude and the spread of COVID-19 based on epidemiological data from China, Bolivia, and Ecuador3. The authors showed that inhabitants are less susceptible to develop serious adverse effects caused by COVID-19 in cities with altitudes above 3000 m a.s.l.3. These authors related this low incidence to compensatory adjustments in physiological systems and environmental factors, such as higher ultraviolet radiation and thinner atmosphere. A recent review examined geographic components (altitude) and physiological factors associated with high altitude in regards to the incidence and severity of COVID-19 infections. There were found clues that physiological and genetic aspects of high altitude populations may influence the pattern of SARS-CoV-2 expansion and COVID-19 infection severity4. Thus, altitude can be a determining factor in the transmission rate of COVID-19. However, due to the importance and urgency of understanding the disease and its behaviour in different locations, it is necessary to highlight the relationships of COVID-19 in other countries, especially in those with greater altitudinal and environmental diversity, such as Brazil.
This work aims to evaluate the incidence of COVID-19 in 154 Brazilian cities with a population above 200 thousand inhabitants, located between 5 and 1135 m in altitude. The results may be useful to apply public policies for the prevention and control of the spread of COVID-19 in Brazil and the world.
Material and methods
Cities data
Data from all 154 Brazilian cities with a population above 200 thousand inhabitants (Fig. 1) were collected on May, June, and July, 2020. These cities are located between 5 and 1135 m in altitude, have 98,080,747 inhabitants (46.7% of the Brazilian population—Brazilian Institute of Geography and Statistics—IBGE)5. Figure 1 shows the sampled locations, and the different altitudes in Brazil divided into three classes based on the available data DIVA-GIS (http://www.diva-gis.org/Data).
Figure 1.
Distribution of 154 Brazilian cities with a population above 200 thousand inhabitants selected to analyse the relative incidence and relative deaths per 100.000 inhabitants of Coronavirus Disease-19 (COVID-19) cases according to three classes of altitudes. Low (red), middle (orange) and high (blue). The information is available in free spatial data DIVA-GIS (http://www.diva-gis.org/Data). The map was made using Quantum geographic information system (QGIS) version 3.14.156.
Data collect
The altitude data for each city was carefully obtained from the average of five measurements obtained in their respective north, south, east, west, and central positions, from Google Earth at https://earth.google.com/web/@0,0,-24018.82718741a,36750128.22569847d,35y,0h,0t,0r/data=KAE (Google Earth, 2020).
The population for each city was obtained using data from IBGE, referring to July 1, 2019, at https://agenciadenoticias.ibge.gov.br/agencia-detalhe-de-midia.html?view=mediaibge&catid=2103&id=30985.
Data on confirmed cases and deaths, resulting from COVID-19, were obtained, on May 17, 2020, on June 01 and 16, 2020 and on July 01, 2020 at https://covid.mapbiomas.org/7.
The data regarding RH were obtained from the National Institute of Meteorology address http://www.inmet.gov.br/portal/index.php?r=estacoes/estacoesAutomaticas8, for the 63, 58, 57 and 59 cities with a population over 200 thousand inhabitants and that have data from automatic weather stations and correspond respectively to the average of the period from March 01 to May 17, May 18 to June 01, 2020, June 02 to June 16, 2020 and June 17 to July 01, 2020.
Statistical analysis
The COVID-19 incidence and death data were calculated per 100,000 inhabitants and are called relative incidence (RI) and relative death rate (RDR). This objective procedure removes the effect of the number of inhabitants in the analyses.
Pearson's correlation analysis was performed to compare a relationship between altitude with RI and RDR, and between RH with RI and RDR.
Define as a predetermined variable as altitudes were divided into three classes [low (altitude ≤ 97 m a. s. l) with 65 cities, middle (97 < altitude ≤ 795 m a. s. l) with 66 cities, high (795 < altitude ≤ 1135 m a. s. l with 23 cities)] for the RI, RDR variables and the same classes for the RH variable. However, for the RH were considered 63 cities (March 01 to May 17, 2020), 58 cities (May 18 to June 01, 2020), 57 cities (June 02 to June 16, 2020), and 56 cities (June 17 to July 01, 2020) according to data provided by the National Institute of Meteorology. We verified that high altitude cities had lower COVID-19 RI and RDR than cities of low altitude. We defined three classes to test our hypotheses, assuming that there would be a staggered decrease in RI and RDR with increasing altitude. To compare three classes of altitude (until May 17 and until June 1, 2020 for the variables RI and RDR and between March 1 and May 17 and between May 18 and June 1 for the RH variable), analysis of variance (ANOVA) and Tukey test were used to compare media (p < 0.05). The COVID-19 mortality and death data were transformed into a log (X + 1) to stabilize the variance, and the non-transformed data were submitted to ANOVA. Both show significance. Thus, we prefer to display a statistical output of unprocessed data as analyses and figures were performed in Excel and Sigma plot 12.5 software9.
Consent for publication
The researchers of this study confirm that they have given due consideration to protect the intellectual property associated with this work and that there are no impediments to publication, including the timing of publication, with respect to intellectual property. In so doing we confirm that we have followed the regulations of our institutions concerning intellectual property.
Results
The 154 municipalities studied correspond to 2.76% of the Brazilian municipalities (5570 municipalities) but are home to 46.7% of the Brazilian population (98,080,747 inhabitants) (Table 1). A total of 13 municipalities are in the central west region with 53.4% of the region's population; 12 are in the northern region with 39.59% of its population; 74 are in the south-eastern region and with 58.7% of the region's population; 28 are in the northeast region with 32.99% of the region's population, and 27 are located in the south region with 38% of the region's population.
Table 1.
Cities and regions of Brazil, altitude, population, relative incidence (RI), relative death rate (RDR), air relative humidity (RH). Data from the first case, and acceleration of the incidence of COVID-19.
| City | Region | Altitude (m) | Population (no.) | RI1 (100,000 hb-1) | RDR1 (100,000 hb-1) | RH3 (%) | 1º cases (data) | IA (data) | RH4 (%) | RI2 (100,000 hb-1) | RDR2 (100,00 0 hb-1) | RH5 (%) | RI6 (100,000 hb-1) | RDR6 (100,00 hb-1) | RH7 (%) | RI8 (100.000 hb-1) | RDR8 (100.000 hb-1) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cuiabá | CW | 195 | 612,547 | 44.73 | 0.33 | 63.6 | 20/Mar | 31/Mar | 62.5 | 129.79 | 1.80 | 62 | 316.87 | 10.94 | – | 647.13 | 30.37 |
| Várzea Grande | CW | 195 | 284,971 | 26.67 | 1.40 | – | 23/Mar | 08/May | – | 90.18 | 4.21 | – | 209.50 | 17.55 | – | 463.91 | 44.57 |
| Rondonópolis | CW | 260 | 232,491 | 39.14 | 1.29 | 72.1 | 30/Mar | 13/Apr | 69.2 | 88.61 | 3.01 | 66.7 | 245.17 | 8.17 | 61.7 | 522.60 | 20.65 |
| Palmas | CW | 266 | 299,127 | 83.24 | 1.00 | 75.2 | 18/Mar | 28/Apr | 69.0 | 204.26 | 2.67 | 58.4 | 349.35 | 4.01 | 51.2 | 629.83 | 6.35 |
| Dourados | CW | 445 | 222,949 | 18.84 | 0.45 | 52 | 28/Mar | 15/May | – | 125.14 | 0.90 | 59.4 | 579.50 | 2.24 | 55.6 | 1,197.58 | 10.76 |
| Campo Grande | CW | 590 | 895,982 | 19.42 | 0.56 | 60.4 | 14/Mar | 15/Apr | 60.6 | 32.70 | 0.78 | 73.5 | 87.50 | 0.89 | 61.9 | 278.02 | 1.12 |
| Rio Verde | CW | 740 | 235,647 | 10.61 | 0.85 | 56.4 | 12/Mar | 29/Apr | 62.0 | 46.26 | 0.85 | – | 782.10 | 2.12 | – | 1,785.30 | 14.85 |
| Goiânia | CW | 787 | 1,516,113 | 60.75 | 1.98 | 72.5 | 12/Mar | 26/Mar | 68.2 | 114.11 | 3.50 | 62.3 | 253.87 | 6.27 | 60.9 | 458.80 | 11.02 |
| Aparecida de Goiânia | CW | 803 | 578,179 | 26.81 | 1.21 | – | 18/Mar | 27/Apr | – | 78.18 | 1.90 | – | 195.10 | 3.98 | – | 464.39 | 9.17 |
| Luziânia | CW | 980 | 208,299 | 20.64 | 1.44 | 74.9 | 25/Mar | 14/May | 70.3 | 39.37 | 1.92 | 63 | 160.35 | 2.88 | 62.1 | 345.18 | 3.36 |
| Anápolis | CW | 1043 | 386,923 | 13.44 | 0.52 | – | 16/Mar | 12/Apr | – | 40.83 | 0.52 | – | 108.29 | 1.29 | – | 223.04 | 1.29 |
| Brasília | CW | 1,075 | 3,015,268 | 112.49 | 1.79 | 78.4 | 07/Mar | 24/Mar | 72.2 | 292.08 | 5.21 | 67.7 | 705.84 | 9.55 | 65.2 | 1452.61 | 17.88 |
| Águas Lindas de Goiás | CW | 1,135 | 212,440 | 13.18 | 0.47 | – | 28/Mar | 29/Apr | – | 98.85 | 2.35 | – | 193.00 | 6.59 | – | 345.04 | 11.77 |
| Region mean | 654.9 | 669,303 | |||||||||||||||
| Aracaju | NE | 9 | 657,013 | 309.28 | 3.04 | – | 14/Mar | 28/Apr | – | 618.10 | 10.81 | – | 1499.06 | 24.35 | – | 2204.83 | 41.40 |
| Jaboatão dos Guararapes | NE | 10 | 702,298 | 266.84 | 24.21 | – | 17/Mar | 07/Apr | – | 454.22 | 45.28 | – | 570.27 | 59.52 | – | 687.88 | 80.73 |
| Fortaleza | NE | 13 | 2,669,342 | 575.83 | 43.98 | 80.2 | 16/Mar | 18/Mar | 79.9 | 902.99 | 78.07 | 79.4 | 1160.81 | 112.61 | 73.2 | 1322.91 | 123.18 |
| Recife | NE | 17 | 1,645,727 | 593.78 | 36.21 | 79.5 | 12/Mar | 28/Mar | 84.8 | 959.09 | 65.69 | 84.3 | 1113.98 | 93.45 | 79.5 | 1259.56 | 110.89 |
| Cabo de Santo Agostinho | NE | 23 | 207,048 | 171.46 | 26.08 | – | 03/Apr | 26/Apr | – | 312.97 | 45.88 | – | 393.15 | 59.41 | – | 445.31 | 77.76 |
| João Pessoa | NE | 23 | 809,015 | 209.76 | 9.27 | 78.5 | 18/Mar | 02/Apr | 82.6 | 489.36 | 16.07 | 81.5 | 1046.21 | 28.80 | 76.4 | 1569.07 | 39.31 |
| Paulista | NE | 23 | 331,774 | 354.76 | 22.00 | – | 03/Apr | 09/Apr | – | 568.16 | 44.91 | – | 702.59 | 53.05 | – | 793.91 | 60.88 |
| Natal | NE | 25 | 884,122 | 134.03 | 3.96 | 82.4 | 12/Mar | 28/Mar | 87.3 | 291.36 | 9.61 | 84.2 | 609.31 | 21.38 | 82.7 | 1312.38 | 49.99 |
| Olinda | NE | 27 | 392,482 | 419.38 | 26.75 | – | 22/Mar | 09/Apr | – | 667.04 | 43.31 | – | 799.78 | 51.72 | – | 963.36 | 57.33 |
| Caucaia | NE | 31 | 361,400 | 245.71 | 10.51 | – | 28/Mar | 13/Apr | – | 499.17 | 24.90 | – | 848.92 | 65.58 | – | 996.40 | 77.20 |
| Mossoró | NE | 32 | 297,378 | 168.81 | 7.73 | 73.7 | 21/Mar | 03/Apr | – | 331.56 | 16.14 | – | 555.52 | 28.92 | – | 959.39 | 42.37 |
| São Luís | NE | 32 | 1,101,884 | 529.09 | 35.76 | 89.4 | 20/Mar | 30/Mar | 86.9 | 839.93 | 47.74 | 85.8 | 1097.67 | 59.35 | 84.9 | 1192.87 | 75.69 |
| Salvador | NE | 36 | 2,872,347 | 185.56 | 6.58 | 83.6 | 13/Mar | 21/Mar | 84.9 | 397.97 | 16.50 | 84.7 | 736.75 | 26.98 | 81.4 | 1166.47 | 40.49 |
| Maracanaú | NE | 41 | 227,886 | 230.82 | 27.21 | – | 29/Mar | 05/Apr | – | 716.15 | 50.90 | – | 1231.76 | 82.50 | – | 1587.64 | 93.47 |
| Camaçari | NE | 44 | 299,132 | 31.76 | 1.34 | – | 20/Mar | 23/Apr | – | 69.53 | 1.34 | – | 195.23 | 4.35 | – | 463.34 | 7.69 |
| Parnamirim | NE | 44 | 261,469 | 84.14 | 2.29 | – | 20/Mar | 16/Apr | – | 211.11 | 3.82 | – | 526.26 | 13.00 | – | 1116.00 | 29.83 |
| Itabuna | NE | 61 | 213,223 | 298.75 | 5.16 | – | 19/Mar | 07/Apr | – | 419.28 | 15.48 | – | 714.28 | 19.70 | – | 1210.00 | 26.26 |
| Maceió | NE | 65 | 1,018,948 | 156.34 | 13.25 | 79.1 | 08/Mar | 13/Apr | – | 598.36 | 28.26 | – | 1108.40 | 47.40 | – | 1511.76 | 58.88 |
| Sobral | NE | 72 | 208,935 | 261.8 | 9.09 | – | 18/Mar | 22/Apr | – | 1063.49 | 34.94 | – | 2042.74 | 84.24 | – | 3142.13 | 109.12 |
| Teresina | NE | 115 | 864,845 | 145.69 | 4.51 | 78.9 | 19/Mar | 30/Mar | 67.0 | 266.41 | 10.41 | 62 | 563.92 | 25.67 | – | 959.02 | 44.75 |
| Feira de Santana | NE | 235 | 614,872 | 33.67 | 0.33 | 80.8 | 06/Mar | 30/Mar | 87.5 | 79.04 | 0.98 | 88.1 | 177.27 | 4.55 | 85.9 | 519.78 | 7.81 |
| Arapiraca | NE | 263 | 231,747 | 56.1 | 2.59 | – | 18/Apr | 27/Apr | – | 180.37 | 5.18 | – | 647.26 | 10.79 | – | 1296.24 | 15.53 |
| Juazeiro | NE | 370 | 216,707 | 12 | 0.92 | – | 23/Mar | 14/May | – | 18.92 | 2.31 | – | 83.52 | 3.69 | – | 286.56 | 8.77 |
| Petrolina | NE | 380 | 349,145 | 24.63 | 1.15 | 63.2 | 23/Mar | 06/May | 64.2 | 44.68 | 2.29 | 65.2 | 69.60 | 3.44 | 63.7 | 195.05 | 7.16 |
| Juazeiro do Norte | NE | 408 | 274,207 | 17.87 | 2.55 | – | 20/Mar | 26/Apr | – | 102.84 | 4.01 | – | 312.17 | 17.14 | – | 625.44 | 32.09 |
| Campina Grande | NE | 512 | 409,731 | 70.78 | 1.22 | 80.9 | 27/Mar | 18/Apr | 87.7 | 370.73 | 4.88 | 86.2 | 1101.21 | 14.89 | 85.1 | 1587.63 | 25.14 |
| Caruaru | NE | 565 | 361,118 | 38.49 | 3.32 | 85.5 | 23/Mar | 18/Apr | 91.4 | 104.95 | 9.14 | 91.9 | 230.40 | 16.06 | – | 481.01 | 32.68 |
| Vitória da Conquista | NE | 970 | 341,597 | 19.61 | 1.17 | – | 01/Apr | 12/Apr | – | 36.89 | 1.46 | – | 113.29 | 1.46 | – | 209.90 | 4.39 |
| Region mean | 158.79 | 672,335 | |||||||||||||||
| Macapá | N | 11 | 503,327 | 531.26 | 14.3 | 84.6 | 20/Mar | 03/Apr | 82.3 | 1009.09 | 27.02 | 82 | 1508.56 | 40.33 | 82.2 | 2581.82 | 50.86 |
| Belém | N | 20 | 1,492,745 | 391.43 | 43.68 | 69.4 | 18/Mar | 06/Apr | 82.5 | 796.18 | 89.43 | 81.2 | 1103.81 | 119.11 | 78.5 | 1314.42 | 128.62 |
| Ananindeua | N | 21 | 530,598 | 231.63 | 20.73 | – | 25/Mar | 15/Apr | – | 519.98 | 45.42 | – | 690.73 | 57.67 | – | 824.54 | 62.57 |
| Castanhal | N | 39 | 200,793 | 158.37 | 22.41 | 87.1 | 26/Mar | 19/Apr | 83.8 | 357.58 | 47.31 | 81.6 | 642.45 | 72.21 | 80.8 | 794.35 | 82.67 |
| Santarém | N | 44 | 304,589 | 84.7 | 5.91 | – | 01/Apr | 30/Apr | – | 332.58 | 30.86 | – | 540.07 | 48.92 | – | 1093.28 | 56.47 |
| Manaus | N | 60 | 2,182,763 | 476.78 | 43.48 | 79.7 | 13/Mar | 22/Mar | 79.9 | 838.07 | 62.44 | 78.1 | 1081.75 | 75.36 | 73.8 | 1244.71 | 82.01 |
| Boa Vista | N | 80 | 399,213 | 314.12 | 8.27 | – | 23/Mar | 13/Apr | – | 655.04 | 24.05 | 78.6 | 1304.32 | 41.08 | 79.3 | 2751.91 | 56.86 |
| Porto Velho | N | 86 | 529,544 | 284.96 | 9.63 | – | 21/Mar | 14/Apr | – | 660.00 | 20.58 | – | 1536.42 | 46.27 | – | 2480.06 | 68.93 |
| Marabá | N | 97 | 279,349 | 71.95 | 8.95 | 82.9 | 23/Mar | 27/Apr | 82.4 | 140.33 | 33.65 | 76.8 | 824.77 | 39.74 | 69.1 | 1426.89 | 49.76 |
| Imperatriz | N | 146 | 258,682 | 329.36 | 13.92 | 78.1 | 01/Apr | 17/Apr | 73.2 | 786.29 | 38.66 | 66.2 | 1252.89 | 62.63 | 61.0 | 1570.27 | 78.47 |
| Rio Branco | N | 157 | 407,319 | 324.81 | 13.01 | 85.2 | 17/Mar | 17/Apr | – | 1007.56 | 28.48 | – | 1339.74 | 48.12 | – | 1719.05 | 64.57 |
| Parauapebas | N | 180 | 208,273 | 90.27 | 11.04 | – | 28/Mar | 24/Apr | – | 751.90 | 29.77 | – | 2998.95 | 47.05 | – | 4758.18 | 57.62 |
| Region mean | 78.42 | 608,100 | |||||||||||||||
| Guarujá | SE | 9 | 320,459 | 115.46 | 4.68 | – | 31/Mar | 14/Apr | – | 312.05 | 16.23 | – | 731.45 | 28.08 | – | 1152.72 | 40.57 |
| Campos dos Goytacazes | SE | 10 | 507,548 | 36.84 | 1.97 | 77.6 | 24/Mar | 27/Apr | 76.4 | 146.00 | 6.11 | 79.2 | 239.39 | 11.62 | 75.3 | 353.86 | 17.93 |
| Angra dos Reis | SE | 14 | 203,785 | 179.11 | 7.36 | 83.8 | 30/Mar | 28/Apr | – | 437.23 | 16.68 | – | 732.14 | 28.46 | – | 1077.12 | 40.73 |
| Macaé | SE | 14 | 256,672 | 43.64 | 6.23 | 71.9 | 31/Mar | 16/Apr | 79.5 | 326.10 | 10.91 | 84.2 | 617.13 | 21.04 | 74.2 | 923.75 | 30.00 |
| Santos | SE | 14 | 433,311 | 322.4 | 19.85 | – | 30/Mar | 01/Apr | – | 802.66 | 34.16 | – | 1454.15 | 51.93 | – | 2140.73 | 85.39 |
| Magé | SE | 15 | 245,071 | 142 | 13.87 | – | 02/Apr | 23/Apr | – | 267.27 | 36.32 | – | 493.33 | 45.70 | – | 661.03 | 53.86 |
| Cabo Frio | SE | 17 | 219,863 | 60.95 | 2.73 | – | 07/Apr | 23/Apr | – | 171.47 | 8.19 | – | 256.07 | 11.83 | – | 396.61 | 19.56 |
| Vitória | SE | 17 | 362,097 | 344.94 | 15.47 | 70.0 | 19/Mar | 05/Apr | 69.4 | 677.44 | 26.51 | 65.6 | 1406.25 | 49.99 | 66.1 | 2023.21 | 69.59 |
| São Gonçalo | SE | 18 | 1,084,839 | 58.26 | 5.99 | – | 23/Mar | 07/Apr | – | 149.24 | 14.66 | – | 271.56 | 25.72 | – | 470.39 | 39.64 |
| Vila Velha | SE | 18 | 493,838 | 277.82 | 9.72 | 81.6 | 19/Mar | 08/Apr | 81 | 490.65 | 20.05 | 82.6 | 1012.07 | 38.88 | 81.5 | 1550.51 | 56.90 |
| Niterói | SE | 20 | 513,584 | 231.32 | 12.66 | 76.5 | 12/Mar | 26/Mar | 73.7 | 596.79 | 20.25 | 79.4 | 909.49 | 28.43 | 68.3 | 1241.67 | 44.78 |
| Duque de Caxias | SE | 22 | 919,596 | 99.94 | 15.77 | 74.1 | 24/Mar | 07/Apr | 56.5 | 163.33 | 27.19 | – | 241.19 | 37.08 | – | 338.19 | 46.76 |
| Rio de Janeiro | SE | 23 | 6,718,903 | 192.31 | 27.4 | 78.3 | 06/Mar | 18/Mar | 69.4 | 433.95 | 53.25 | 80.2 | 630.83 | 75.76 | 68.1 | 847.40 | 97.49 |
| São Vicente | SE | 23 | 365,798 | 112.36 | 4.1 | – | 31/Mar | 15/Apr | – | 268.73 | 21.87 | – | 454.08 | 30.34 | – | 836.53 | 45.11 |
| Praia Grande | SE | 24 | 325,073 | 89.83 | 13.23 | – | 01/Apr | 15/Apr | – | 215.95 | 17.23 | – | 582.02 | 20.92 | – | 777.98 | 26.46 |
| Itaboraí | SE | 25 | 240,592 | 152.54 | 13.3 | – | 27/Mar | 04/Apr | – | 470.09 | 32.42 | – | 728.62 | 44.47 | – | 1023.31 | 51.96 |
| Nova Iguaçu | SE | 27 | 821,128 | 93.29 | 11.57 | – | 28/Mar | 04/Apr | – | 142.49 | 22.16 | – | 314.08 | 33.98 | – | 397.75 | 41.65 |
| Belford Roxo | SE | 32 | 510,906 | 73.01 | 9.98 | – | 26/Mar | 11/Apr | – | 139.16 | 19.77 | – | 214.13 | 29.16 | – | 279.50 | 34.64 |
| São João de Meriti | SE | 32 | 472,406 | 99.07 | 10.16 | – | 30/Mar | 09/Apr | – | 183.74 | 18.20 | – | 279.63 | 32.39 | – | 350.33 | 45.51 |
| Cachoeiro de Itapemirim | SE | 62 | 208,972 | 38.28 | 1.44 | – | 20/Mar | 29/Apr | – | 126.33 | 5.74 | – | 449.34 | 13.88 | – | 798.67 | 29.19 |
| Cariacica | SE | 62 | 381,285 | 237.09 | 9.44 | – | 20/Mar | 13/Apr | – | 480.22 | 24.13 | – | 935.78 | 46.42 | – | 1344.93 | 63.21 |
| Serra | SE | 65 | 517,510 | 257.58 | 15.07 | – | 23/Mar | 01/Apr | – | 484.63 | 30.34 | – | 984.72 | 46.57 | – | 1481.71 | 59.71 |
| Governador Valadares | SE | 165 | 279,885 | 25.72 | 1.79 | 80.0 | 26/Mar | 25/Apr | 80.2 | 67.17 | 2.50 | 80.6 | 148.28 | 3.57 | 80.1 | 406.24 | 12.86 |
| Ipatinga | SE | 245 | 263,410 | 13.67 | 0 | – | 12/Mar | 15/Apr | – | 93.39 | 0.38 | – | 268.78 | 6.45 | – | 750.54 | 15.94 |
| Volta Redonda | SE | 400 | 273,012 | 163.73 | 6.59 | – | 24/Mar | 02/Apr | – | 254.93 | 13.19 | – | 413.17 | 18.68 | – | 619.75 | 20.88 |
| Presidente Prudente | SE | 430 | 228,743 | 39.35 | 2.19 | 58.0 | 08/Apr | 24/Apr | 55.2 | 60.33 | 2.62 | 69.9 | 105.36 | 5.25 | 59.5 | 291.59 | 8.31 |
| São José do Rio Preto | SE | 518 | 460,671 | 77.93 | 2.6 | – | 18/Mar | 07/Apr | – | 151.95 | 4.99 | – | 282.41 | 8.47 | – | 563.74 | 17.37 |
| Bauru | SE | 559 | 376,818 | 58.12 | 3.45 | 69.3 | 31/Mar | 15/Apr | 65.2 | 78.02 | 3.98 | 77.6 | 129.77 | 4.51 | 69.8 | 363.31 | 6.90 |
| Piracicaba | SE | 570 | 404,142 | 55.92 | 4.21 | 64.6 | 30/Mar | 27/Apr | 50.4 | 141.53 | 7.18 | 63.2 | 277.63 | 10.89 | 50.3 | 508.73 | 21.77 |
| Ribeirão Preto | SE | 570 | 703,293 | 63.98 | 1.85 | – | 26/Mar | 04/Apr | – | 134.08 | 3.41 | – | 281.25 | 9.10 | – | 562.64 | 22.18 |
| Limeira | SE | 580 | 306,114 | 23.85 | 0.33 | – | 01/Apr | 28/Apr | – | 50.96 | 1.31 | – | 118.26 | 6.86 | – | 266.24 | 11.76 |
| Americana | SE | 582 | 239,597 | 27.55 | 1.67 | – | 31/Mar | 18/Apr | – | 50.50 | 2.50 | – | 101.84 | 4.59 | – | 225.80 | 10.02 |
| Jacareí | SE | 590 | 233,662 | 37.23 | 1.71 | – | 08/Apr | 17/Apr | – | 92.44 | 3.85 | – | 166.48 | 8.99 | – | 292.30 | 12.41 |
| Rio Claro | SE | 590 | 206,424 | 12.6 | 4.36 | – | 25/Mar | 17/Apr | – | 23.25 | 5.33 | – | 111.91 | 9.20 | – | 300.35 | 14.53 |
| Sumaré | SE | 590 | 282,441 | 41.07 | 1.06 | – | 07/Apr | 06/May | – | 68.69 | 2.48 | – | 145.52 | 4.60 | – | 383.80 | 11.33 |
| Taubaté | SE | 595 | 314,924 | 18.73 | 1.27 | 74.1 | 19/Mar | 27/Apr | 70.4 | 43.82 | 1.59 | 77.9 | 60.65 | 1.59 | 73.9 | 153.05 | 2.54 |
| Sorocaba | SE | 600 | 679,378 | 107.45 | 4.27 | 72.5 | 27/Mar | 25/Apr | 63.5 | 135.42 | 6.48 | 76.3 | 230.80 | 10.89 | 69.5 | 632.93 | 17.96 |
| São José dos Campos | SE | 610 | 721,944 | 62.33 | 2.77 | – | 18/Mar | 04/Apr | – | 124.80 | 4.85 | – | 212.34 | 7.76 | – | 407.65 | 12.74 |
| Indaiatuba | SE | 615 | 251,627 | 22.65 | 3.97 | – | 01/Apr | 17/Apr | – | 58.02 | 7.95 | – | 79.88 | 10.33 | – | 233.68 | 17.49 |
| Hortolândia | SE | 620 | 230,851 | 45.92 | 5.63 | – | 20/Mar | 18/Apr | – | 66.71 | 5.20 | – | 134.29 | 8.66 | – | 334.41 | 11.26 |
| Marília | SE | 640 | 238,882 | 13.81 | 0.42 | 65.9 | 03/Apr | 15/May | 57.5 | 25.95 | 0.42 | 73.7 | 66.14 | 1.67 | 65.0 | 149.86 | 5.02 |
| Montes Claros | SE | 660 | 409,341 | 9.77 | 0.49 | 72.4 | 06/Apr | 08/May | 68.2 | 16.86 | 0.49 | 62.5 | 34.69 | 0.73 | 60.1 | 64.98 | 0.98 |
| Campinas | SE | 682 | 1,204,073 | 81.97 | 3.07 | – | 18/Mar | 07/Apr | – | 151.32 | 6.48 | – | 322.57 | 12.37 | – | 666.07 | 26.24 |
| Araraquara | SE | 694 | 236,072 | 59.73 | 1.69 | – | 02/Apr | 15/Apr | – | 99.12 | 1.69 | – | 240.60 | 2.54 | – | 402.84 | 4.66 |
| Divinópolis | SE | 745 | 238,230 | 53.31 | 0.42 | 80.6 | 08/Mar | 01/Apr | 78.7 | 79.34 | 0.84 | 76.7 | 106.20 | 1.26 | 75.9 | 138.52 | 4.62 |
| Guarulhos | SE | 750 | 1,379,182 | 110.79 | 11.96 | – | 17/Mar | 01/Apr | – | 200.77 | 20.59 | – | 307.72 | 34.01 | – | 496.16 | 49.45 |
| Jundiaí | SE | 754 | 418,962 | 95.47 | 6.92 | – | 25/Mar | 16/Apr | – | 245.13 | 13.61 | – | 482.86 | 26.26 | – | 865.71 | 42.49 |
| Itaquaquecetuba | SE | 760 | 370,821 | 92.77 | 9.17 | – | 31/Mar | 15/Apr | – | 160.45 | 19.42 | – | 241.90 | 27.24 | – | 381.05 | 35.87 |
| Carapicuíba | SE | 770 | 400,927 | 147.16 | 9.73 | – | 14/Mar | 09/Apr | – | 257.90 | 18.96 | – | 413.29 | 27.69 | – | 623.06 | 36.17 |
| Mogi das Cruzes | SE | 770 | 445,842 | 137.49 | 9.64 | – | 20/Mar | 10/Apr | – | 223.85 | 19.07 | – | 316.03 | 27.14 | – | 466.76 | 35.89 |
| Sete Lagoas | SE | 770 | 239,639 | 4.59 | 0.42 | 76.5 | 17/Mar | 19/Apr | 72.9 | 12.10 | 0.42 | 68 | 18.78 | 0.42 | 65.3 | 95.14 | 1.67 |
| Juiz de Fora | SE | 777 | 568,873 | 72.42 | 2.81 | 73.5 | 14/Mar | 31/Mar | 76.7 | 108.46 | 5.27 | 79.5 | 154.87 | 6.68 | 77.3 | 296.20 | 9.32 |
| Diadema | SE | 778 | 423,884 | 150.28 | 12.03 | – | 27/Mar | 07/Apr | – | 279.09 | 19.82 | – | 478.20 | 30.20 | – | 768.13 | 41.28 |
| Suzano | SE | 780 | 297,637 | 125.32 | 12.77 | – | 19/Mar | 11/Apr | – | 222.08 | 16.80 | – | 354.12 | 28.89 | – | 493.22 | 34.94 |
| Itapevi | SE | 781 | 237,700 | 137.99 | 14.72 | – | 30/Mar | 15/Apr | – | 225.07 | 26.92 | – | 335.72 | 42.49 | – | 490.95 | 55.95 |
| Osasco | SE | 785 | 698,418 | 247.85 | 29.07 | – | 18/Mar | 31/Mar | – | 389.17 | 44.53 | – | 592.77 | 57.27 | – | 832.17 | 69.30 |
| São Paulo | SE | 785 | 12,252,023 | 293.27 | 23.14 | 81.3 | 25/fev | 11/Mar | 73.4 | 498.91 | 35.13 | 83.5 | 762.71 | 46.13 | 74.3 | 1037.53 | 58.46 |
| Barueri | SE | 786 | 274,182 | 265.52 | 29.91 | 76.8 | 18/Mar | 16/Apr | 68.5 | 433.29 | 46.32 | 78.7 | 599.97 | 62.00 | 70.9 | 767.37 | 73.67 |
| Santo André | SE | 790 | 718,773 | 180.31 | 9.46 | – | 16/Mar | 30/Mar | – | 322.49 | 18.50 | – | 552.47 | 27.41 | – | 889.02 | 35.62 |
| Taboão da Serra | SE | 790 | 289,664 | 136.02 | 10.36 | – | 25/Mar | 01/Apr | – | 283.78 | 22.44 | – | 475.38 | 34.87 | – | 733.95 | 44.53 |
| Uberaba | SE | 790 | 333,783 | 29.96 | 1.50 | 75.7 | 20/Mar | 06/Apr | 74.5 | 59.92 | 1.80 | 70.2 | 115.04 | 4.19 | 72.1 | 221.70 | 7.79 |
| São Bernardo do Campo | SE | 795 | 838,936 | 172.36 | 14.3 | – | 16/Mar | 30/Mar | – | 313.73 | 25.27 | – | 554.51 | 34.09 | – | 923.43 | 44.46 |
| Santa Luzia | SE | 800 | 219,134 | 9.13 | 0.46 | – | 29/Mar | 13/May | – | 21.90 | 0.46 | – | 65.26 | 0.91 | – | 145.12 | 2.74 |
| Mauá | SE | 805 | 472,912 | 122.01 | 8.04 | – | 16/Mar | 07/Apr | – | 217.17 | 12.48 | – | 350.17 | 23.89 | – | 481.48 | 30.87 |
| Embu das Artes | SE | 810 | 273,726 | 117.64 | 9.86 | – | 25/Mar | 02/Apr | – | 202.39 | 16.81 | – | 313.09 | 25.21 | – | 450.09 | 32.15 |
| Cotia | SE | 820 | 249,210 | 139.64 | 13.64 | – | 18/Mar | 31/Mar | – | 239.96 | 20.06 | – | 355.52 | 26.48 | – | 564.99 | 35.71 |
| Betim | SE | 830 | 439,340 | 8.65 | 0.68 | – | 23/Mar | 06/May | – | 28.45 | 1.37 | – | 90.59 | 3.87 | – | 190.29 | 7.28 |
| Ribeirão das Neves | SE | 870 | 334,858 | 6.87 | 0.3 | – | 02/Apr | 27/Apr | – | 24.19 | 0.60 | – | 58.23 | 0.90 | – | 168.43 | 2.99 |
| São Carlos | SE | 870 | 251,983 | 22.62 | 1.19 | 68.0 | 06/Apr | 09/May | 64.9 | 48.81 | 1.98 | 72.7 | 100.80 | 2.78 | 68.9 | 194.46 | 5.16 |
| Petrópolis | SE | 889 | 306,191 | 69.56 | 8.82 | – | 21/Mar | 14/Apr | – | 136.84 | 13.72 | – | 223.72 | 20.90 | – | 265.19 | 30.05 |
| Uberlândia | SE | 892 | 691,305 | 56.27 | 1.59 | 64.2 | 17/Mar | 02/Apr | 63.3 | 130.04 | 2.60 | 56.1 | 314.77 | 5.93 | 58.3 | 930.85 | 11.72 |
| Belo Horizonte | SE | 904 | 2,512,070 | 46.18 | 1.23 | 72.9 | 16/Mar | 23/Mar | 75.2 | 74.92 | 1.95 | 71 | 138.85 | 3.03 | 74.3 | 235.46 | 5.73 |
| Contagem | SE | 953 | 663,855 | 16.87 | 0.45 | – | 23/Mar | 17/Apr | – | 39.32 | 1.51 | – | 101.23 | 3.16 | – | 134.82 | 6.48 |
| Franca | SE | 962 | 353,187 | 10.19 | 0.57 | 66.4 | 02/Apr | 28/Apr | 62.1 | 23.22 | 0.57 | – | 28.88 | 1.70 | 60.2 | 68.24 | 2.55 |
| Region Mean | 500.4 | 700,862 | |||||||||||||||
| Rio Grande | S | 5 | 211,005 | 4.74 | 0.47 | – | 23/Mar | 02/May | – | 9.00 | 0.47 | – | 32.70 | 0.95 | – | 94.31 | 1.90 |
| Itajaí | S | 6 | 219,536 | 80.17 | 1.37 | 80.0 | 21/Mar | 27/Mar | 75.6 | 209.99 | 4.56 | 86.3 | 460.06 | 9.11 | 83.9 | 828.11 | 15.94 |
| Pelotas | S | 12 | 342,405 | 10.22 | 0 | – | 25/Mar | 14/Apr | – | 25.12 | 0.00 | – | 47.90 | 0.00 | – | 81.19 | 0.88 |
| Canoas | S | 13 | 346,616 | 13.85 | 0.87 | – | 21/Mar | 17/Apr | – | 29.72 | 1.73 | – | 69.24 | 2.02 | – | 170.51 | 5.77 |
| Florianópolis | S | 22 | 500,973 | 94.42 | 1.2 | 70.6 | 12/Mar | 23/Mar | 71.1 | 137.13 | 1.40 | 77.7 | 191.63 | 1.80 | 73.5 | 287.04 | 2.79 |
| Gravataí | S | 32 | 281,519 | 10.66 | 0.36 | – | 25/Mar | 02/Apr | – | 22.38 | 1.42 | – | 52.93 | 1.78 | – | 142.09 | 3.91 |
| Joinville | S | 32 | 590,466 | 52.16 | 1.86 | – | 13/Mar | 30/Mar | – | 71.64 | 3.90 | – | 104.66 | 4.06 | – | 304.17 | 6.60 |
| Novo Hamburgo | S | 37 | 246,748 | 29.99 | 0.81 | – | 29/Mar | 03/Apr | – | 60.39 | 1.62 | – | 112.26 | 3.24 | – | 310.03 | 10.13 |
| São Leopoldo | S | 42 | 236,835 | 48.13 | 0.42 | – | 21/Mar | 09/Apr | – | 97.54 | 0.84 | – | 156.23 | 2.53 | – | 369.46 | 7.18 |
| São José | S | 44 | 246,586 | 36.09 | 0.41 | – | 19/Mar | 09/Apr | – | 50.29 | 0.81 | – | 101.38 | 0.81 | – | 185.74 | 3.65 |
| Blumenau | S | 47 | 357,199 | 117.02 | 0.84 | – | 22/Mar | 06/Apr | – | 184.49 | 1.12 | – | 226.76 | 1.68 | – | 454.37 | 2.52 |
| Criciúma | S | 52 | 215,186 | 130.58 | 2.79 | – | 20/Mar | 09/Apr | – | 178.45 | 4.18 | – | 226.78 | 4.18 | – | 294.16 | 5.11 |
| Alvorada | S | 57 | 210,305 | 10.94 | 3.8 | – | 19/Mar | 17/Apr | – | 31.86 | 1.43 | – | 73.23 | 1.90 | – | 184.02 | 4.28 |
| Porto Alegre | S | 58 | 1,483,771 | 40.57 | 1.42 | 71.7 | 11/Mar | 20/Mar | 76.3 | 50.14 | 2.49 | 83.0 | 105.68 | 3.84 | 76.8 | 181.97 | 6.20 |
| Viamão | S | 92 | 255,224 | 12.93 | 0.39 | – | 23/Mar | 13/Apr | – | 18.42 | 1.57 | – | 29.78 | 3.53 | – | 68.57 | 5.49 |
| Santa Maria | S | 116 | 282,123 | 15.6 | 0.71 | 68.9 | 22/Mar | 08/Apr | 78.9 | 65.57 | 1.06 | 86.2 | 151.71 | 2.84 | 90.7 | 205.23 | 6.03 |
| Foz do Iguaçu | S | 202 | 258,532 | 29.01 | 0.77 | 63.3 | 18/Mar | 29/Mar | 66.3 | 48.74 | 0.77 | 71.0 | 70.78 | 1.55 | 58.9 | 153.56 | 3.09 |
| Maringá | S | 518 | 423,666 | 21.72 | 1.42 | 56.3 | 18/Mar | 21/Apr | 57.7 | 38.71 | 1.42 | 74.1 | 106.69 | 2.60 | 65.4 | 274.27 | 4.25 |
| Londrina | S | 554 | 569,733 | 23.52 | 2.81 | – | 17/Mar | 01/Apr | – | 74.25 | 4.21 | – | 162.36 | 8.25 | – | 245.03 | 13.34 |
| Passo Fundo | S | 661 | 203,275 | 152.5 | 10.82 | 66.2 | 26/Mar | 21/Apr | 75.9 | 364.53 | 15.25 | 82.7 | 613.95 | 18.20 | 74.7 | 918.46 | 21.65 |
| Chapecó | S | 671 | 220,367 | 229.62 | 0 | – | 20/Mar | 26/Apr | – | 419.75 | 1.82 | – | 507.34 | 2.72 | 71.1 | 1129.48 | 4.99 |
| Cascavel | S | 743 | 328,454 | 42.02 | 1.52 | – | 23/Mar | 03/Apr | – | 140.05 | 2.13 | – | 337.34 | 5.48 | – | 861.00 | 14.01 |
| Caxias do Sul | S | 758 | 510,906 | 14.68 | 0.39 | – | 12/Mar | 30/Mar | – | 32.69 | 0.78 | – | 84.56 | 1.57 | – | 219.02 | 3.91 |
| São José dos Pinhais | S | 910 | 323,340 | 14.85 | 0.93 | – | 29/Mar | 12/May | – | 32.16 | 1.24 | – | 70.20 | 3.71 | – | 126.18 | 8.35 |
| Ponta Grossa | S | 930 | 351,736 | 9.1 | 0 | – | 21/Mar | 23/Apr | – | 20.47 | 0.00 | – | 42.36 | 0.28 | – | 99.22 | 0.28 |
| Curitiba | S | 940 | 1,933,105 | 33.06 | 1.71 | 71.6 | 12/Mar | 19/Mar | 59.8 | 50.90 | 2.43 | 69.1 | 98.18 | 4.29 | 66.0 | 212.87 | 7.50 |
| Colombo | S | 998 | 243,726 | 11.9 | 0 | – | 22/Mar | 04/May | – | 20.51 | 0.00 | – | 58.26 | 1.64 | – | 135.81 | 5.74 |
| Region mean | 316.7 | 421,975 | |||||||||||||||
| Total | 98,080,747 |
IA incidence acceleration, RH air relative humidity, RI relative incidence, RDR relative death rate, CW central-west, NE northeast, N north, SE southeast, S south. 1: until May 17, 2020. 2: until June, 01, 2020. 3: between March 01 and May, 17, 2020. 4: between May 18 and June, 01, 2020.5: 4: between June 02 and June, 16, 2020. 6: until June, 16, 2020; 7: between June 17 and July, 01, 2020; 8: until July, 01, 2020.
On May 17, 2020, these municipalities concentrated 71% of the cases (171,287) and 78% (12,610) of deaths due to COVID-19 in Brazil. On June, 01, 2020, these municipalities concentrated 63% of the cases (330,271) and 76% (22,567) of deaths due to COVID-19 in Brazil. On June, 16, 2020, these municipalities concentrated 59% of the cases (544,408) and 72% (32,829) of deaths due to COVID-19 in Brazil. On July, 01, 2020, these municipalities concentrated 56% of the cases (815,016) and 66% (42,949) of deaths due to COVID-19 in Brazil. The decrease in RDR in cities with a population over 200 thousand inhabitants, between May, 17 and July, 01, indicates that the COVID-19 virus is spreading to smaller cities.
The altitude varies between 5 and 1135 m a.s.l, and the cities located at higher altitudes are in the central-west region, followed by the southeast and south regions. The northern region has the lowest altitude gradient, and all cities are below 180 m a.s.l. (Table 1).
On May 17, 2020, the RI varied between 4.74 (Rio Grande) and 593.78 (Recife) (Table 1) and was higher in the north, followed by the northeast, southeast, central-west and, south (Table 2). On June 01, 2020, the RI varied between 12.10 (Sete Lagoas) and 1063.49 (Sobral) (Table 1) and was higher in the north, followed by the northeast, southeast, central-west and, south (Table 2). On June 16, 2020, the RI changed between 18.78 (Sete Lagoas) and 2998.95 (Parauapebas) (Table 1) and was higher in the north, followed by the northeast, southeast, central-west, and south (Table 2). On July 01, 2020, the RI changed between 64.98 (Montes Claros) and 4758.18 (Parauapebas) (Table 1) and was higher in the north, followed by the northeast, central-west, southeast, and south (Table 2).
Table 2.
Mean relative incidence (RI), average relative death rate (RDR), average air relative humidity (RH) by geographic region and in Brazil.
| Region | RI | RDR | RH (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| May /17 | June/01 | June/16 | July/01 | May /17 | June/01 | June/16 | July/01 | May /17 | June/01 | June/16 | July/01 | |
| NO | 357.07 | 739.67 | 1163.09 | 1619.31 | 28.33 | 52.64 | 71.29 | 81.58 | 81.0 | 80.7 | 77.8 | 75.0 |
| NE | 284.35 | 529.16 | 837.25 | 1163.52 | 17.34 | 32.06 | 48.87 | 62.36 | 79.7 | 82.2 | 81.2 | 78.0 |
| SE | 156.84 | 297.06 | 483.79 | 719.44 | 13.5 | 22.45 | 35.59 | 44.87 | 73.3 | 69.1 | 74.3 | 69.1 |
| SU | 42.45 | 75.90 | 136.16 | 273.63 | 1.40 | 2.18 | 3.57 | 6.49 | 68.6 | 70.2 | 78.8 | 73.4 |
| CO | 60.46 | 160.78 | 407.94 | 884.84 | 1.34 | 3.23 | 6.86 | 14.31 | 67.3 | 66.8 | 64.1 | 59.0 |
| Brazil mean | 174.6 | 336.73 | 555.06 | 905.91 | 12.90 | 23.01 | 33.47 | 45.06 | 74.0 | 73.8 | 75.2 | 70.9 |
CW central-west, NE northeast, N north, SE southeast, S south.
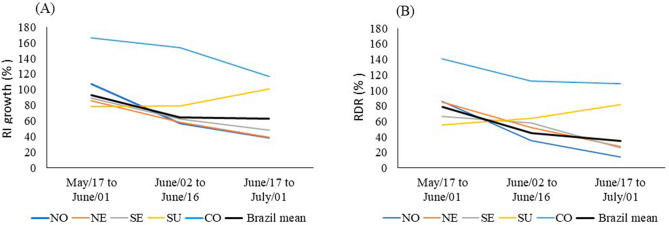
In Brazil, between May 17 and June 01, between June 02 and June 16, and between June 17 and July, 01, 2020, the RI increased 92.3% 64.8%, 63.20%, respectively. The largest increase in RI was observed in the central-west region and the smallest in the northeast region (Table 2), and the rate of RI growth decelerated in all regions, except in the southern region (Fig. 2).
Figure 2.
(A) Acceleration rate of relative incidence (RI), and (B) Acceleration rate of relative death rate (RDR) between May 17 and June 1, 2020; between June 2 and June 16, 2020; and between June 17 and July 01, 2020 in north (N), northeast (NE), southeast (SE), south (S), and central weast (CW) region.
On May 17, 2020, the RDR varied between 0 (Chapecó, Colombo, Ipatinga, Pelotas and, Ponta Grossa) and 43.98 (Fortaleza) (Table 1) and was higher in the north, followed by the northeast, southeast, south and central-west (Table 2). On June 01, 2020, the RDR varied between 0 (Colombo, Pelotas and, Ponta Grossa) and 78.07 (Fortaleza) (Table 1) and was higher in the north, followed by the northeast, southeast, central-west and south (Table 2). On June 16, 2020, the RDR changed between 0 (Pelotas) and 119.11 (Belém) (Table 1). On July 01, 2020, the RDR changed between 0.28 (Ponta Grossa) and 128.62 (Belém) (Table 1) and was higher in the north, followed by the northeast, southeast, central-west and south (Table 2).
Between May 17 and June 01, between June 02 and June 16, and between June 17 and July 01, the RDR increased respectively 78.4%, 45.5% and 34.6% in Brazil. The largest increase in RDR was observed in the central-west region and the smallest in the north region (Table 2), and the rate of RDR growth decelerated in all regions, except in the southern region (Fig. 2).
Between March 01 and May 17, 2020, the average RH data of 63 cities were analysed, which varied between 52 and 89.4% (Table 1) with an RH average of 74% (Table 2). Between May 18 and June 01, 2020, the average RH data of 58 cities were analysed, which varied between 50.4 and 91.4% (Table 1) with an RH average of 73.8% (Table 2). Between June 02 and June 16, 2020, the average RH of 57 cities varied between 56.1 and 91.9% (Table 1) with an RH of 75.2% (Table 2). Between June 17 and July 01, 2020, the average RH of 58 cities varied between 50.3 and 92.5% (Table 1) with an RH of 70.9% (Table 2). The cities in the central-west region had the lowest average RH values. Cities in the northern and northeast region had the highest RH values (Table 1).
The first confirmed case in Brazil occurred on February 26 of 2020 in the city of São Paulo, and until April 8 of 2020, all cities in Brazil with a population of up to 200 thousand inhabitants confirmed at least one case of COVID-19 (Table 1). There were no significant differences between cities concerning the period of accelerated dissemination. Would, then, the altitude and the RH have contributed to accelerate the spread of the virus in Brazil?
The correlation between altitude and RI calculated from data collected in 154 cities until May 17, 2020, was negative and significant, according to Pearson's correlation (r = − 0.38, n = 154, p < 0.01). The correlation between altitude and RI calculated from data collected in 154 cities until June 01, 2020, was higher (r = − 0.44, n = 154, p < 0.01). The correlation between altitude and RI calculated from data collected in 154 cities until June 16, 2020, was also negative and significant (r = − 0.41, n = 154, p < 0.01). The correlation between altitude and RI calculated from data collected in 154 cities until July 01, 2020, was also negative and significant (r = − 0.36, n = 154, p < 0.01).The same occurred between altitude and RDR until May 17, 2020 (r = − 0.29, n = 154, p < 0.01), until June 01, 2020 (r = − 0.37, n = 154, p < 0.01), until June 16, 2020 (r = − 0.41, n = 154, p < 0.01) and until July 01, 2020 (r = − 0.43, n = 154, p < 0.01).
The correlation between RH and RI calculated from data collected in the period from March 01 to May 17, 2020, in 63 cities (r = 0.48, n = 63, p < 0.01), in the period from May 18 to June 01, 2020, in 58 cities (r = 0.47, n = 58, p < 0.01), in the period from June 02 to June 16, 2020, in 56 cities (r = 0.28, n = 57, p = 0.04), and in the period from June 17 to July 01, 2020, in 54 cities, (r = 0.28, n = 54, p < 0.04) was positive and significant.
The correlation between RH and RDR calculated from data collected in the period from March 01 to May 17, 2020, in 63 cities (r = 0.38, n = 63, p < 0.01), in the period from May 18 to June 01, 2020, in 58 cities (r = 0.37, n = 58, p < 0.01), in the period from June 02 to June 16, 2020, in 56 cities (r = 0.31, n = 56, p = 0.01), and in the period from June 17 to July 01, 2020, in 54 cities (r = 0.30, n = 54, p = 0.02), was positive and significant.
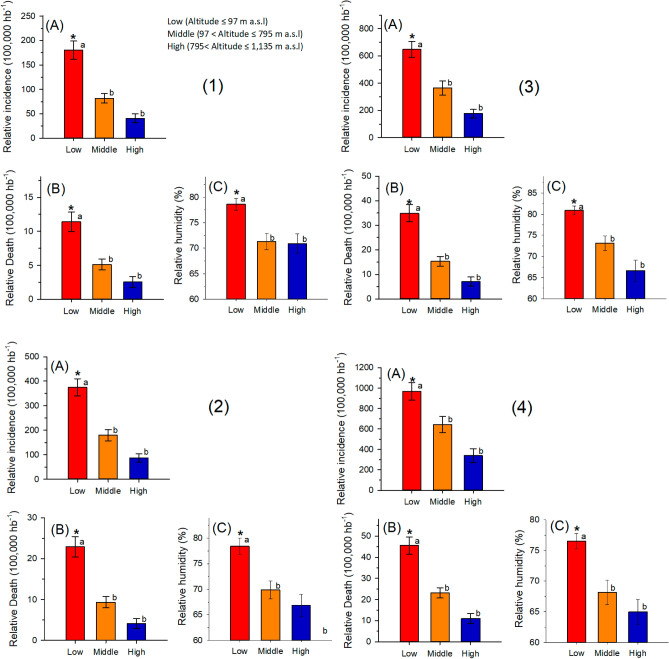
The cities were grouped into three classes of altitude: low (altitude ≤ 97 m a. s. l), middle (97 < altitude ≤ 795 m a. s. l), high (795 < altitude ≤ 1135 m a. s. l) (Fig. 2). For RI, RDR and RH, the analysis of variance (hierarchical classification) for data collected until May 17, 2020 (RI: F2,151 = 18.80; p < 0.001; RDR: F2,151 = 12.46; p < 0.001; RH: F2,60 = 7.35; p < 0.001), for data collected until June 01, 2020 (RI: F2,151 = 19.40; p < 0.001; RDR: F2,151 = 18.64; p < 0.001; RH: F2,55 = 7.98; p < 0.001), for data collected until June 16, 2020 (RI: F2,151 = 13.40; p < 0.001; RDR: F = 20.35; p < 0.001; RH: F2,53 = 10.52; p < 0.001), and for data collected until July 01, 2020 (RI: F2,151 = 9.38; p < 0.001; RDR: F2,151 = 21,31; p < 0.001; RH: F2,51 = 7.16; p = 0.001) was highly significant. The averages of RI, RDR, and RH were compared using the Tukey test, which showed that the incidence is lower at high altitudes in the four analysed periods (Fig. 3).
Figure 3.
Mean and standard deviation of (A) relative incidence (RI); (B) relative death rate (RDR) and (C) air relative humidity (RH) at low, medium and high altitudes in cities in Brazil with a population above 200 thousand inhabitants (1) until May 17, 2020; (2) until June, 01, 2020; (3) until June, 16, 2020; (4) until July, 01, 2020. *Significant difference by analysis of variance and average values followed by the same letters (superscript a or superscript b) do not differ by the Tukey test (p < 0.05).
The r-values of Pearson's correlation between altitude and RI and RDR and the F values of ANOVA for all dependent variables were significant in the four analysed period. Thus, the altitude and the RH may have contributed to accelerate the spread and mortality of the virus in Brazil.
Discussion
Our epidemiological analysis of the COVID-19 pandemic in Brazil indicates a direct association between the incidence of COVID-19 with altitude and RH in Brazilian cities with a population above 200 thousand inhabitants. The low RI and RDR in cities with higher altitudes may be related to environmental factors, which influence the spread of the virus and the physiology of human beings.
Climatic factors can be determinant for transmission by some viruses10,11. Thus, a study performed in Russia assessed possible climatic predictors in the rise of COVID-19 intensity. The results showed that temperature seasonality influenced COVID-19 spread in humid continental Russia, whereas temperature (diurnal range and seasonality) was influential in sub-artic Russia10. In addition, another study aimed to examine the linkage between climatic variables and COVID-19 in National Capital Territory (NCT) of Delhi, India. The results of that study suggested that climatic conditions in NCT of Delhi were favourable for COVID-19 and the disease may spread further with the increasing temperature, relative humidity, evaporation and wind speed11. However, it is necessary to consider comprehensive biophysical assessments of altitude, humidity, UV radiation in the maintenance and transmission of SARS-CoV-212,13. Recently studies have been published about temperature and UV index, and that heating, and UV radiation can eliminate the viral infectivity12,13. These findings could help to understand the relationship of COVID-19 cases in different Brazilian cities due to altitude.
In contrast to what other studies report regarding the greater spread of the influenza virus in environments with lower RH14, our data show that COVID-19 RI is higher in cities where RH is highest. These results are in line with those obtained by C Arias-Reyes, N Zubieta-DeUrioste, L Poma-Machicao, F Aliaga-Raudan, F Carvajal-Rodriguez, M Dutschmann, E Schneider-Gasser, G Zubieta-Calleja and J Soliz3, which lists air dryness as one of the factors that control the spread of the virus at high altitudes. In working with climatic data from 5 large Brazilian cities (Manaus, Fortaleza, Brasília, Rio de Janeiro, and São Paulo)15, showed that moderate relative air humidity (averages between 77.7 and 81.6%) favor the spread of this disease. In the present study, 5 cities with the highest RI, in the four periods analyzed, had an average RH between 79.3 and 84.8%, values similar to those found by A Auler, F Cássaro, V da Silva and L Pires16.
Another point that should be considered is that the higher altitude, by itself, favors a higher incidence of ultraviolet (UV) radiation, especially in the UVA and UVB spectra, which can produce a bactericidal effect due to changes in the molecular chains of DNA and RNA. Thus, as a hypothesis, UV radiation would shorten the virus half-life, thereby reducing the virus's ability to survive in Brazilian cities located at higher altitudes and, consequently, the survival of the COVID-19 virus. M Blumthaler, W Ambach, and R Ellinger17 observed an increase of 9 ± 2% in UV radiation for every 1000 m of altitude, under clear sky conditions. In addition, the increase in UV radiation can reach 11.3% (5 to 1135 m altitude) between the Brazilian cities studied in this work. Besides, considering that vitamin D production is dependent on exposure to UV radiation and that vitamin D levels positively modulate the immune system18, the hypothesis of higher immune defense against SARS-CoV- 2 is plausible in cities with higher altitude. Future studies should investigate this hypothesis.
The low air density and greater distance between molecules in Brazilian cities located at higher altitudes could also reduce the inoculation of airborne viruses compared to sea level. C Arias-Reyes, N Zubieta-DeUrioste, L Poma-Machicao, F Aliaga-Raudan, F Carvajal-Rodriguez, M Dutschmann, E Schneider-Gasser, G Zubieta-Calleja, and J Soliz3 suggested that inhabitants of cities with altitudes above 3000 m a.s.l are less susceptible to developing effects caused by COVID-19 due to ultraviolet radiation and thinner air.
Physiological factors can influence the pathogenicity of SARS-CoV-2 at high altitudes. The barometric reading varies with changing weather conditions and becomes lower as the altitude increases. Thus, the volumes of inspired air, which require humidification, are much higher than at sea level, and the air density is lower at high altitudes19. As a result, compensatory adjustments to facilitate the release of oxygen to cells occur in individuals living at higher altitudes, such as the increase in the levels of 2,3-diphosphoglycerate (2,3-DPG), a chemical compound found inside the red blood cell, whose function is to reduce hemoglobin's affinity for oxygen in order to facilitate its release into tissues20. Given the above, a probable hypothesis for less severity in individuals infected with COVID-19 living in cities with higher altitude could be due to adaptations in these compensatory adjustments to increase the bioavailability of peripheral oxygen. This adaptation is proven in individuals who live at altitudes above 3000 m a.s.l.
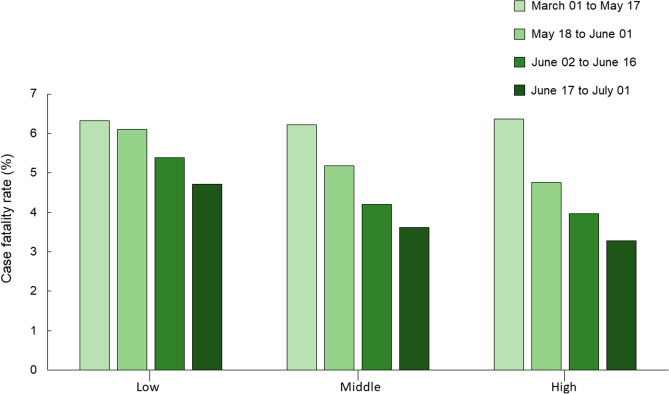
Other studies have also investigated the relationship between altitude, infection, and case fatality by COVID-19. In Peru, infection by COVID-19 reduced with increasing altitude. However, case-fatality rate was not dependent of altitude20. In addition, case studies in the USA and Mexico showed that mortality due to COVID-19 was greater in cities with altitude higher than 2000 m versus located lower than 1500 m21. A publication from Italy showed no association of COVID-19 with altitude22. In our study, RI and RDR became lower as the altitude increase (Fig. 4). In addition, although the case fatality rate (deaths/cases) decreased over the period analysed for all altitude classes, the reduction was greater at high altitudes (Fig. 5). In this way, such adaptations, even to a lesser extent, could contribute to minimizing the severity of infection in cities located at higher altitudes.
Figure 4.
Relative incidence average (RI) and relative death rate average (RDR) in all the cities in Brazil with a population above 200 thousand inhabitants, grouped in three classes of altitude (low, middle and high), for the 4 periods analysed.
Figure 5.
Case fatality rate in all the cities in Brazil with a population above 200 thousand inhabitants, grouped in three classes of altitude (low, middle and high), for the 4 periods analysed.
The casual movement of dissolved oxygen molecules establishes the PO2 of plasma and tissue fluids. The pressure of oxygen in the solution helps to regulate breathing, particularly at higher altitudes, when the ambient PO2 decreases considerably; it also determines the uptake of oxygen by haemoglobin in the lungs and the subsequent release into the tissues. However, haemoglobin saturation with oxygen changes very little until the oxygen pressure has decreased to about 60 mmHg. Even when alveolar PO2 drops to 75 mmHg, as it does at high altitudes, haemoglobin saturation decreases by only approximately 6%. At 60 mmHg alveolar PO2, haemoglobin is still 90% saturated with oxygen. Below that pressure, the volume of oxygen combined with haemoglobin decreases more quickly.
As exposed, the S shape of the oxyhaemoglobin dissociation curve indicates that there is only a small change in the percentage saturation of haemoglobin with oxygen up to an altitude of approximately 3,048 m. At 1,981 m, for example, the alveolar PO2 falls from its value at sea level from 100 to 78 mmHg3. However, haemoglobin remains 90% saturated with oxygen.
In addition, regarding the possible physiological factors, the receptor-binding domain (RBD) in the SARS-CoV-2 protein was recently identified and that the RBD protein-bound firmly to the receptors of the human angiotensin-converting enzyme 2 (ACE2)23. Human ACE2 is part of the renin-angiotensin system (RAS), an essential hormonal system for controlling blood pressure and fluid and electrolyte balance. In the classical view, RAS peptides are generated from a single precursor protein called angiotensinogen (ATG). After being cleaved by the protease renin, this protein forms the inactive decapeptide angiotensin I, which is hydrolysed by the angiotensin-converting enzyme (ACE) and forms the octapeptide angiotensin II (Ang II), the principal peptide in the system. ACE2 cleaves a single residue of angiotensin I (Ang I) that generates the Ang- (1–9) peptide and degrades Ang II to the Ang- (1–7) vasodilator. Current data obtained during the pandemic suggest that the use of ACE inhibitors and angiotensin type I receptor blockers increase the expression of ACE2. Consequently, increased expression of ACE2 would facilitate infection by COVID-1924,25. Studies show that RAS elements are modulated at high altitudes26–28. In this way, it is possible that the expression of ACE2 can be down-regulated due to the high altitude and favour a lower incidence of COVID-19 infection. Other studies speculate in this direction and suggest different paths for an ACE2 down-regulation3,29, but future studies need to clarify this hypothesis.
Given the above, considering that the Brazilian cities studied at a higher altitude are around 1100 m5, probably the hypothesis of compensatory adjustments related to ACE2 in pulmonary epithelial cells, i.e., a protective factor for virus penetration and evolution of severe pulmonary edema, should be studied with caution in residents of Brazilian cities with higher altitudes. Furthermore, this population is also not exposed to conditions of chronic hypoxia. The results presented in this work can be useful for the implementation of public policies for prevention, control of the dissemination of COVID-19 in Brazil and the world. In addition, it can contribute to future studies, including other zoonotic viruses that cause respiratory diseases, as well as allowing the recommendation of changing the environment for people at risk in COVID-19.
Our findings identified that virulence by SARS-CoV-2 is lower in Brazilian cities with a population above 200 thousand inhabitants, located at relative high altitudes, and where the RH is lowest (Fig. 3). These findings are in line with the physiological compensatory adjustments of the inhabitants of cities located at higher altitudes, as well as with the common characteristics. Thus, our study starts point for future studies to establish causality of environmental conditions with SARS-CoV2, contributing to the implementation of measures to prevent and control the spread of COVID-19. It is, however, important to note that the information presented here clearly lacks any physiological evidences, which may merit further investigation. In addition, we cannot assume uniform density population in every city studied, as well quality of care, probability of infection, among other ecological variables, that may affect the outcome. In other words, future studies should consider those variables. As prospective, longitudinal studies are needed to confirm whether these associations remain over time.
Acknowledgements
We thank the Universidade Federal dos Vales do Jequitinhonha e Mucuri for institutional support. The CNPq, CAPES-Finance Code 001, and FAPEMIG for support and scholarships.
Author contributions
J.S.C.F.: Formal analysis, data curation, methodology. R.S.d.S.: Formal analysis, data curation, methodology, writing—review & editing—original draft, A.C.S.: Formal analysis, data curation, methodology, writing—review & editing. D.C.V.: Writing—review & editing. V.A.M.: Writing—review & editing. A.C.R.L.: Conceptualization, data curation, writing—review & editing—original draft.
Funding
There are currently no funding sources in the list.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Huang, X. et al. Epidemiology and clinical characteristics of COVID-19. Arch. Iran. Med.23, 268–271, 10.34172/aim.2020.09 (2020). [DOI] [PubMed]
- 2.World Health Organization. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
- 3.Arias-Reyes C, et al. Does the pathogenesis of SAR-CoV-2 virus decrease at high-altitude? Respir. Physiol. Neurobiol. 2020;277:103443. doi: 10.1016/j.resp.2020.103443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Joyce KE, et al. Geographic components of SARS-CoV-2 expansion: A hypothesis. J. Appl. Physiol. 2020;129:257–262. doi: 10.1152/japplphysiol.00362.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Instituto Brasileiro de Geografia e Estatística. https://agenciadenoticias.ibge.gov.br/agencia-detalhe-de-midia.html?view=mediaibge&catid=2103&id=3098.
- 6.Quantum GIS Development Team. Quantum GIS Geographic Information System. (Open Source Geospatial Foundation Project, 2014).
- 7.Portal GEOCOVID-19 Brasil. https://covid.mapbiomas.org/.
- 8.Instituto Nacional de Meteorologia. http://www.inmet.gov.br/portal/index.php?r=estacoes/estacoesAutomaticas.
- 9.SigmaPlot: SigmaPlot Version 12.5. (Systat Software, Inc., San Jose, 2012).
- 10.Pramanik M, et al. Climatic factors influence the spread of COVID-19 in Russia. Int. J. Environ. Res. Public Health. 2020 doi: 10.1080/09603123.2020.1793921. [DOI] [PubMed] [Google Scholar]
- 11.Singh O, et al. Association between climatic variables and COVID-19 pandemic in National Capital Territory of Delhi, India. Environ. Dev. Sustain. 2020 doi: 10.1007/s10668-020-01003-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gunthe SS, et al. On the global trends and spread of the COVID-19 outbreak: Preliminary assessment of the potential relation between location-specific temperature and UV index. J. Public Health (Berl.) 2020 doi: 10.1007/s10389-020-01279-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duan S, et al. Stability of SARS coronavirus in human specimens and environment and its sensitivity to heating and UV irradiation. Biomed. Environ. Sci. 2003;16:246–255. [PubMed] [Google Scholar]
- 14.Casanova LM, et al. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl. Environ. Microbiol. 2010;76:2712–2717. doi: 10.1128/AEM.02291-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Auler A, et al. Evidence that high temperatures and intermediate relative humidity might favor the spread of COVID-19 in tropical climate: A case study for the most affected Brazilian cities. Sci. Total Environ. 2020;729:139090. doi: 10.1016/j.scitotenv.2020.139090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hart PH, et al. Exposure to UV wavelengths in sunlight suppresses immunity. To what extent is UV-induced vitamin D3 the mediator responsible? Clin. Biochem. Rev. 2013;34:3–13. [PMC free article] [PubMed] [Google Scholar]
- 17.Blumthaler M, et al. Increase in solar UV radiation with altitude. J. Photochem. Photobiol. B Biol. 1997;39:130–134. doi: 10.1016/S1011-1344(96)00018-8. [DOI] [Google Scholar]
- 18.Hodkinson P. Acute exposure to altitude. J. R. Army Med. Corps. 2011;157:85–91. doi: 10.1136/jramc/157-01-15. [DOI] [PubMed] [Google Scholar]
- 19.Mulquiney, P.J. et al. Model of 2,3-bisphosphoglycerate metabolism in the human erythrocyte based on detailed enzyme kinetic equations: Computer simulation and metabolic control analysis. Biochem. J.342, 597–604, 10.1042/0264-6-21:3420597 (1999) [PMC free article] [PubMed]
- 20.Segovia-Juarez, J. et al. High altitude reduces infection rate of COVID-19 but not case-fatality rate. Respir. Physiol. Neurobiol.281, 103494, 10.1016/j.resp.2020.103494 (2020). [DOI] [PMC free article] [PubMed]
- 21.Woolcott, O.O. et al. Mortality attributed to COVID-19 in high-altitude populations. High Alt. Med. Biol.4, 409–416, 10.1089/ham.2020.0098 (2020). [DOI] [PubMed]
- 22.Perone G. The determinants of COVID-19 case fatality rate (CFR) in the Italian regions and provinces: An analysis of environmental, demographic, and healthcare factors. Sci. Total Environ. 2020;755:142523. doi: 10.1016/j.scitotenv.2020.142523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tai W, et al. Characterization of the receptor-binding domain (RBD) of 2019 novel coronavirus: Implication for development of RBD protein as a viral attachment inhibitor and vaccine. Cell. Mol. Immunol. 2020;17:613–620. doi: 10.1038/s41423-020-0400-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fang L, et al. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir. Med. 2020;8:e21. doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patel AB, et al. COVID-19 and angiotensin-converting enzyme inhibitors and angiotensin receptor blockers: What is the evidence? JAMA. 2020;18:1769–1770. doi: 10.1001/jama.2020.4812. [DOI] [PubMed] [Google Scholar]
- 26.Hogan RP, 3rd, et al. Effect of altitude on renin-aldosterone system and metabolism of water and electrolytes. J. Appl. Physiol. 1973;35:385–390. doi: 10.1152/jappl.1973.35.3.385. [DOI] [PubMed] [Google Scholar]
- 27.Colice GL. Effect of hypoxemia on the renin-angiotensin-aldosterone system in humans. J. Appl. Physiol. 1985;58:724–730. doi: 10.1152/jappl.1985.58.3.724. [DOI] [PubMed] [Google Scholar]
- 28.Epstein M, et al. Effects of simulated high altitude on renin-aldosterone and Na homeostasis in normal man. J. Appl. Physiol. 1972;33:204–210. doi: 10.1152/jappl.1972.33.2.204. [DOI] [PubMed] [Google Scholar]
- 29.Choquenaira-Quispe C. Factors involved in low susceptibility to COVID-19: An adaptation of high altitude inhabitants. Med. Hypotheses. 2020;143:110068. doi: 10.1016/j.mehy.2020.110068. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.