Abstract
Objective:
Racial/ethnic disparities in obesity may be due, in part, to minority groups consuming more energy-rich diets in response to greater stress exposure. The present study systematically reviewed the literature describing the effects of stress on food consumption among various racial/ethnic groups in the United States.
Methods:
PubMed and PsycINFO databases were searched for studies reporting associations between stress and food consumption by different racial/ethnic groups, conducted between January 1, 1999 to November 25, 2019. The search included terms related to food consumption, stress, and race/ethnicity. After screening 3,660 records, 30 studies were included for review.
Results:
The selected studies assessed diverse stressors and eating constructs; African-American and Hispanic/Latinx were the most commonly studied minority groups. Studies generally supported that diverse forms of stress exposure are associated with reduced healthy eating patterns and increased obesogenic eating patterns across racial/ethnic groups. However, studies that directly compared stress – eating associations among multiple racial/ethnic groups showed mixed results.
Conclusion:
Members of diverse racial/ethnic groups are susceptible to stress-induced unhealthy eating patterns, though evidence is insufficient to conclude whether the degree of susceptibility differs among groups. Additional studies utilizing observational measures of food intake and culturally-sensitive measures of stress are needed to identify the most influential stressors on dietary behaviors, to assess whether some stressors are more salient for given racial/ethnic groups, and to examine the extent to which stress-induced eating contributes to racial/ethnic disparities in obesity and obesity-related diseases.
Keywords: obesity, health disparities, dietary patterns, stress, eating
Obesity places tremendous burdens on Americans. By imparting risk for myriad medical conditions, including cancer, high blood pressure, heart disease, stroke, chronic inflammatory lung diseases, and diabetes [1–4], obesity constitutes a leading cause of disability and preventable death in the United States (US) [5], with annual costs reaching hundreds of billions of dollars in medical treatment and lost productivity [6]. However, the burden of obesity is not equally distributed: African Americans (AA), Hispanic/Latinx (HL), and Native Americans (NA) experience higher obesity prevalence than do Non-Hispanic Whites (NHW) [7, 8]. Disparate obesity prevalence sets the stage for inequitable health trajectories, with HL, AA, and NA exhibiting higher prevalence of obesity-related diseases [9–12] and reductions in life expectancy [13]. As access to care for obesity and obesity-related health conditions is also inequitably dispersed among US racial/ethnic groups [14], explicating mechanisms that contribute to racial/ethnic disparities in obesity is crucial, in order to identify strategies to prevent obesity and resultant long-term health disparities among AA, HL, and NA.
Racial/ethnic obesity disparities are likely determined by the interaction of myriad genetic, epigenetic, biological, environmental, behavioral, and social factors [15–17], which have been reviewed elsewhere [e.g., 16]. However, the role of stress exposure in the development of obesity disparities has been relatively overlooked. Racial/ethnic obesity disparities may be due, in part, to racial/ethnic differences in stress exposure [18], which may influence dietary patterns. Systemic social inequalities expose minority groups to greater stress [19, 20]; stress exposure, in turn, contributes to obesity by promoting the consumption of energy-rich foods [19, 21]. Although the association between stress exposure and food consumption has received extensive empirical attention [e.g., 21–24], less is known regarding the links between stress and eating patterns among US minority groups or whether groups most at risk for obesity are also most susceptible to stress-induced eating. To our knowledge, these topics have not been previously reviewed systematically. The present study fills this gap by synthesizing evidence regarding the effects of stress on eating patterns among US-based minority groups. This systematic review examines 1) whether racial/ethnic minorities exhibit stress-induced eating patterns, and 2) whether racial/ethnic groups differ in their eating behavior in response to stress.
The human psychological stress response is multi-faceted, and includes both the awareness of a stressor (an event, circumstance, or stimuli that poses a threat to equilibrium [25]) and the subjective appraisal of and emotional response to that stressor [21, 26]. Stressors that are appraised to be acutely threatening to survival or well-being (including social stressors, which endanger the interpersonal connections that are critical to human life), that are difficult to control, or that exceed one’s coping resources activate the hypothalamic-pituitary-adrenal (HPA) axis of the stress response system, which partially governs appetite and eating behavior [21, 22, 27]. Palatable food consumption following a stressor activates dopaminergic and opioid-related neural circuits, which modulate this HPA response [21]. Additionally, highly emotionally arousing or uncontrollable stressors may evoke emotion-focused or avoidant coping strategies, such as the consumption of highly palatable, energy rich food, which ameliorate stress-induced negative mood states [28] when stressors cannot be resolved directly. These stress – eating processes allow for restoration of equilibrium following moderate, manageable, or one-time stressors. However, intense, uncontrollable, or chronic stress recalibrates the HPA axis, alters brain structure and function, and reinforces behavioral patterns in ways that promote the consumption of highly-palatable, energy-rich foods, reduce inhibitory control, and increase the regulatory effect of pleasurable activities, such as eating [22, 29–31]. Therefore, exposure to such stress triggers a cascade, in which the consumption of highly palatable foods may serve as an increasingly effective and difficult-to-resist method of short-term emotional and physiological self-regulation.
Racial/ethnic minority groups are exposed to more uncontrollable, distressing, and socially threatening stressors, such as discrimination, microaggressions, and the enduring impact of institutional inequalities on social position, economic status, and safety, than are other groups [20]. Additionally, racial/ethnic minorities have more frequent exposure to stressors that are common to all groups [20]. These repeated, intense, threatening, and difficult-to-cope-with stress exposures may make minority groups particularly vulnerable to stress-induced eating. Although such differential susceptibility to stress-induced eating provides a plausible mechanism underpinning racial/ethnic obesity disparities (e.g., Environmental Affordances Model; [32]), limited literature examines how the effect of stress on food consumption might vary by racial/ethnic group. In contrast, most literature linking stress to eating has either been conducted in primarily NHW samples [e.g., 33] or has failed to explore possible racial/ethnic differences within heterogeneous samples (such as, adjusting for effects of race/ethnicity on eating without examining whether effects of stress on eating differ by racial/ethnic group [e.g., 34]). Several studies seminal in establishing links between stress and eating did not report the racial/ethnic composition of participants whatsoever [e.g., 35–37]. Moreover, while most research on stress, eating, and obesity in minority groups have focused on AA and/or HL, other racial/ethnic groups in the US, such as Asian Americans (AS), NA, and Pacific Islanders (PI) have been under-represented in the literature, despite also showing divergent risks for obesity compared to NHW [7, 8, 38].
Therefore, the effect of stress on food consumption remains largely unexplored outside of majority-NHW samples. This review summarizes existing research to examine how stress influences eating behavior among minority racial/ethnic groups in the US and whether evidence supports the effects of stress on eating vary by race/ethnicity. Particular attention is paid to how different components of stress (e.g., the occurrence of discrete stressors vs. subjective perceptions of stress) and different forms of stress (e.g., discrimination-related stress vs. other forms of general life stressors) are associated with eating behavior across racial/ethnic groups. Additionally, sample characteristics (e.g., age, sex/gender) and study methodologies are reviewed as possible moderators of stress – eating associations.
Methods
This systematic review aimed to identify studies that 1) examine the impact of stress on eating behavior in distinct racial/ethnic groups, or 2) compare the effect of stress on eating behavior among racial/ethnic groups. Guidelines set forth by the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) were followed [39].
Inclusion and Exclusion Criteria
The following criteria were employed for inclusion in the current review. First, studies must include measurement of at least one index of food consumption, include measurement of at least one index of stress, and report effects of stress on food consumption or associations between stress and food consumption. Studies that only reported the effects of food consumption on stress or the joint effects of stress and eating on a third variable did not meet this inclusion criterion. Stress was defined as the objective occurrence of discrete stressors (whether or how frequently potentially threatening events occurred), the subjective/emotional experience of discrete stressors (e.g., how stressful or upsetting the participant viewed certain potentially threatening experiences to be), or subjective appraisals of the overall stressfulness of one’s life or circumstances (how stressful or upsetting the participant viewed life in general to be or certain domains of life to be). Second, studies must either a) include only one racial/ethnic minority group, b) examine effects separately in each sampled racial/ethnic group, or c) test whether effects differ by racial/ethnic group (e.g., using moderation analyses). Third, study participants had to reside in the United States.
Exclusion criteria included studies of solely clinical populations (i.e., those diagnosed with major medical or mental health disorders) and studies using exclusively qualitative methods (e.g., focus groups). Studies that reported on proxies for eating behavior (e.g., food purchasing) were excluded. Studies that reported the effects of stress on a single index that included both eating and other behaviors (e.g., exercise) or attitudes (e.g., perceptions of body shape) were excluded. Lastly, studies that examined the influence of one person’s stress exposure on another person’s food consumption (e.g., the influence of parental stress on child feeding practices) were excluded.
Search and Review
An electronic database search of PubMed and PsycINFO included results published in English from January 1, 1999 to November 25, 2019. Search terms included eating/consumption terms (i.e., diet, dietary, eating, food intake, food consumption, calor*, nutrient*, energy intake, Kcal), race and ethnicity terms (i.e., ethnic*, race, racial, black*, African-American*, African American*, Hispanic, Latin*, Mexican, Asian*, minority groups, indigenous, Native American*, cultural groups, demographic*, multi-racial, multi racial, multiracial, Pacific Islander*, bi-racial, biracial), and stress-related terms (i.e., stress*, emot*). PubMed identified 2,054 records and PsycINFO identified 1,696 records. Of these, 90 duplicate records were removed. References were managed using Mendeley software. The final set of studies screened for in/out eligibility included 3,660 records.
Studies discussed herein were selected using several steps. First, a screening team applied exclusion and inclusion criteria to titles and abstracts of studies identified from the database searches. The lead author reviewed a portion of sorted studies, which yielded acceptable interrater agreement (>80%); sorting was discussed and disagreements were resolved in weekly team meetings to control for screener drift. Of the original records, 347 were screened in for full text review based on abstract content. Next, the full texts of these 347 studies were screened for eligibility; of these, 30 met criteria for inclusion in the review. Lastly, the references of included studies and relevant review papers were examined to identify records not retrieved by electronic searches, but this did not yield any additional papers for inclusion. The screening process is described in detail in a PRISMA flow diagram (see Figure 1).
Figure 1.
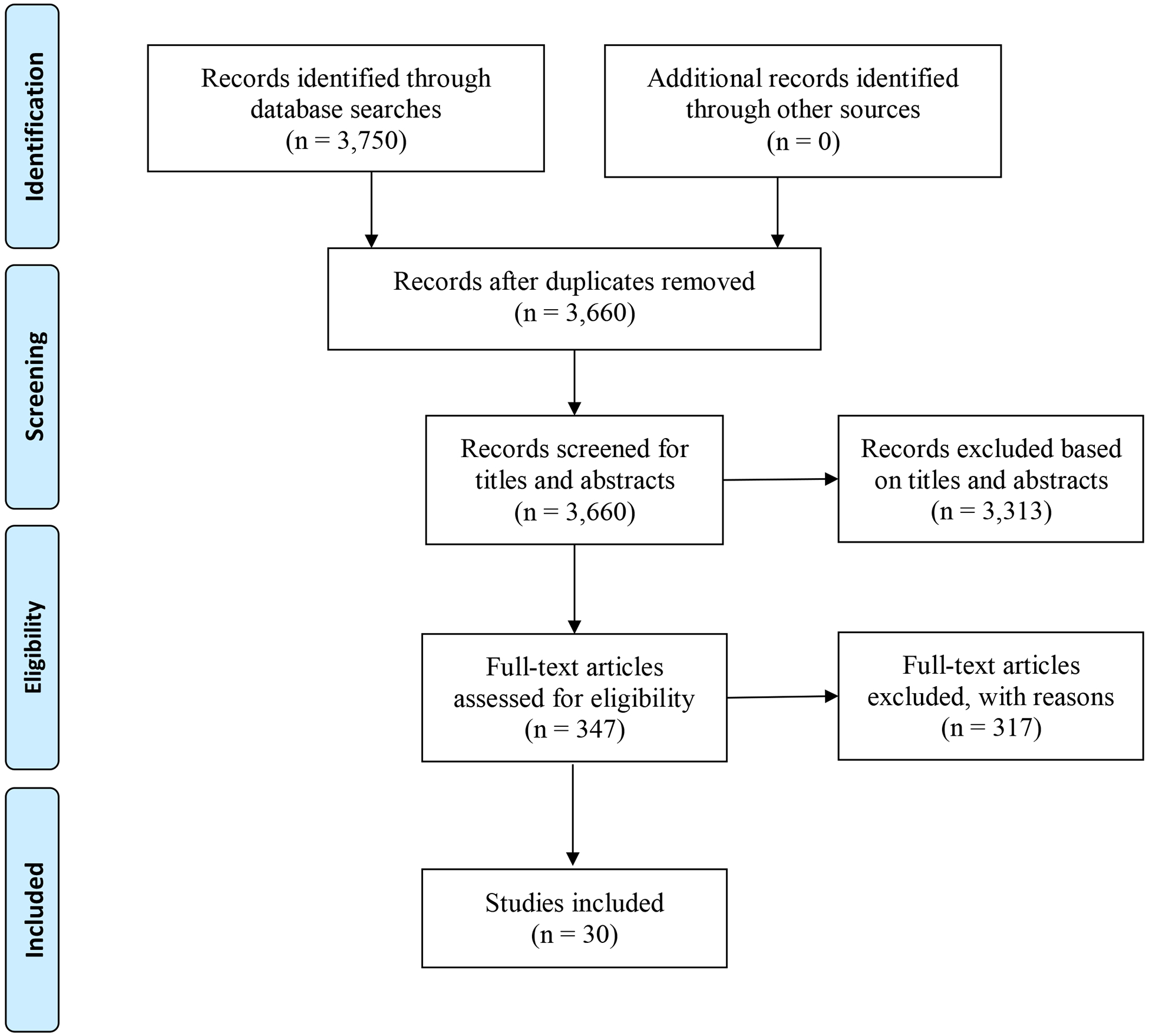
PRISMA four-phase flow diagram of study screening and selection process
Results
Aim 1: Effects of stress on eating, separately by racial/ethnic group
The review yielded 25 studies examining the association of stress and eating within one racial/ethnic group; of these, 16 studies examined AA, 8 examined HL, and 1 examined AS. No studies assessed stress and eating among NA, PI, or any other racial/ethnic groups.
African Americans.
Sixteen studies generally supported that stressful events are associated with less healthful eating and/or more obesogenic eating patterns for AA (see Table 1). No studies showed appetite-suppressive effects of stress among AA. Stress constructs measured included perceived stress (the extent to which participants rate life generally or specific life domains as subjectively stressful), occurrence of stressors (whether or how frequently stressors occurred), combined measures (assessing both whether an event or series of events occurred, and if so, how stressful or upsetting the participant considered each event to be), and discrimination-related stress (including measures of the occurrence and/or perception of unfair treatment related to any personal characteristic).
Table 1.
Studies describing associations between stress and eating in African-American samples, organized by domain of stress assessed.
| Authors (Year) | Participants (% female) | Stress Measure | Eating Measure | Findings: Effect of Stress on Eating |
|---|---|---|---|---|
| Perceived stress | ||||
| Austin et al., 2009 [48]a | 25 Children and adolescents (60%) | Perceived stress (PSS) | Healthy eating (self-report) | Mixed. Increase in stress → decrease in healthy eating across time, for girls only; stress ≠ healthy eating cross-sectionally |
| Carson et al., 2015 [47]b | 355 Adults (100%) | Perceived stress (PSS) | Meeting recommended dietary intake (24-hr recalls) | NS. Stress ≠ meeting eating recommendations |
| Diggins et al., 2015 [40]b | 99 Young adults (100%) | Perceived stress (PSS) | EE (self-report) | POSITIVE. Stress → EE |
| Horton et al., 2018 [46]b | 251 Young adult college students (78%) | Perceived stress (PSS) | Dietary fat intake (self-report) | MIXED. Stress ≠ fat intake; if highly religious, stress → fat intake |
| Johnson et al., 2012 [41]b | 350 Adults, mostly obese (100%) | Perceived stress1 | EE (self-report) | POSITIVE. Stress → EE |
| Longmire-Avital & McQueen, 2019 [42]b | 149 Young adult college students (100%) | Perceived stress (PSS) | EE (self-report) | POSITIVE. Stress → EE |
| Pickett & McCoy, 2018 [43]b | 191 Premenopausal adults (100%) | Perceived stress (PSS) | Eating behavior (multiple domains, self-report) | POSITIVE. Stress → less low-fat foods and more: snacking on sweets, haphazard planning, meal skipping, EE |
| Sims et al., 2008 [44]b | 159 Adults (52%) | Perceived stress (PSS) | Eating behavior (multiple domains, self-report) | MIXED. Stress → EE; greater association for highly obese participants; ≠ low-fat foods, snacking on sweets |
| Sims et al., 2017 [45]b | 5,301 Adults (63%) | Perceived stress (GPSS) | Percent calories from fat (self-report) | POSITIVE. Stress → fat intake |
| Occurrence of stressful events | ||||
| Klassen et al., 2009 [49]b | 156 Adults in public housing, at baseline of a dietary intervention (100%) | Stressful life events in past year2 | Healthy eating (24-hr recall) | POSITIVE. Stressful events → less heathy eating |
| Sims et al., 2017 [45]b | 5,301 Adults (63%) | Minor events in past week (WSI-event); major events in past year (MLE) | Percent calories from fat (self-report) | MIXED. Minor events → fat intake; major events ≠ fat intake |
| Zenk et al., 2014 [50]c | 100 Adults (100%) | Daily hassles (DHC); EMA assessment of stressful event occurrence3 and social stressor occurrence4 | Snack food consumption (EMA) | MIXED. Individual (high stress relative to own mean value): Daily hassles → concurrent food consumption; stressful events, social events ≠ food consumption Group (high stress relative to others): Daily hassles, stressful events → lagged and concurrent food consumption; social events ≠ food consumption |
| Combined: Occurrence and perceived stressfulness of events | ||||
| Austin et al., 2009 [48]a | 25 Children and adolescents (60%) | Combined occurrence and perceived stressfulness of daily hassles | Healthy eating (self-report) | NS. Hassles ≠ healthy eating |
| Harrington et al., 2010 [51]b | 179 Adult trauma survivors (100%) | Combined occurrence and perceived stressfulness of traumatic events (LSC-R; SES) | Binge eating; eating for psychological reasons (self-reports) | MIXED. Trauma ≠ either eating measure; trauma → binge eating through other psychosocial mediators (e.g. emotion regulation) |
| Sims et al., 2017 [45]b | 5,301 Adults (63%) | Combined occurrence and perceived stressfulness of minor life events in past week (WSI-impact) | Percent calories from fat (self-report) | NS. Stress ≠ fat intake |
| Discrimination-related stress | ||||
| Coleman et al., 2019 [52]b | 118 Adolescent-father dyads (0%) | Frequency of discrimination experiences (EDS) | EE (self-report) | POSITIVE. Discrimination → EE |
| Diggins et al., 2015 [40]b | 99 Young adults (100%) | Contextualized stress related to race and gender (JHP) | EE (self-report) | NS. Contextualized stress ≠ EE |
| Hayman et al., 2015 [55]d | 124 Young adult college students (100%) | Experimentally manipulated social exclusion (CB) by NHW or AA confederate | Snack food consumption (observed) | MIXED. Excluded (rather than included) by NHW confederate → chip consumption; excluded (rather than included) by AA confederate ≠ chip consumption; NS for chocolate consumption |
| Hoggard et al., 2019 [53]b | 150 Young adult college students (59%) | Frequency of race-related hassles (DLE) | EE (by type; self-report) | MIXED. Discrimination → angry and depressed EE; discrimination ≠ anxious EE |
| Johnson et al., 2012 [41]b | 350 Adults, mostly obese (100%) | Occurrence of race-related discrimination (PDQ) | EE (self-report) | POSITIVE. Discrimination → EE |
| Longmire-Avital & McQueen, 2019 [42]b | 149 Young adult college students (100%) | Combined occurrence and perceived stressfulness of racism-related events (IRRS) | EE (self-report) | POSITIVE. Discrimination → EE; (holds when adjusting for perceived stress) |
| Sims et al., 2016 [54]b | 4,452 Adults (63%) | Frequency of everyday discrimination; occurrence of lifetime discrimination; perceived stressfulness of lifetime discrimination (JHSDIS) | Percent calories from fat (self-report) | MIXED. Lifetime discrimination → fat intake; everyday discrimination → fat intake for women only; stressfulness of discrimination ≠ fat intake |
Note: EE = emotional eating; EMA = Ecological Momentary Assessment; POSITIVE = association between stress and eating; NS= no association between stress and eating; MIXED = mixed support for associations between stress and eating; ≠ = not significantly associated with; → = associated with; NHW = Non-Hispanic White.
Longitudinal self-report (2 measures, 1 month apart) methodology.
Cross-sectional self-report methodology.
Seven-day ecological momentary assessment methodology (EMA), with EMA measured five times per day and stress-eating associations tested at both concurrent measurement points and lagged measurement points (time N stress predicting time N+1 eating).
Experimental, observational methodology, with participants randomly assigned to in-group inclusion (included by AA confederate), in-group exclusion (excluded by AA confederate), out-group inclusion (included by NHW confederate) and out-group exclusion (excluded by NHW confederate) conditions, and food consumption directly observed.
Stress Measures: PSS = Perceived Stress Scale; GPSS = Global Perceived Stress Scale; WSI-event = Weekly Stress Inventory (number of stressful events endorsed in past week); MLE = Major Life Events, index of past year; DHC = Daily Hassles Checklist; LSC-R = Life Stressors Checklist–Revised; SES = sexual experiences survey; WSI-impact = Weekly Stress Inventory (subjective stressfulness of events endorsed in past week); EDS = Everyday Discrimination Scale; JHP = The Jackson Hogue Phillips Contextualized Stress Measure; CB = Cyberball; DLE = Daily Life Experiences Scale, a subscale of the Racism and Life Experience scale; PDQ = Perceived Discrimination Questionnaire; IRRS = Index of Race Related Stress; JHSDIS = Jackson Heart Study Discrimination Instrument.
Unnamed, single-item measure of global perception of stressfulness of life on 1–10 scale.
Unnamed, list of whether 11 stressors (e.g., loss of job, arrest, death of loved one) occurred in last year.
Unnamed, single item ecological momentary assessment measure, “Have you experienced a stressful event since your last entry?”
Unnamed, single item ecological momentary assessment measure, “Have you experienced a stressful or problematic social interaction since your last entry?”
Nine studies examined the effects of perceived stress on eating. Findings supported that more global perceptions of life stress were associated with more emotional eating [40–43] (though in one study this association held only for obese participants [44]), as well as with greater fat intake [45] and less consumption of low-fat foods [43] (though in one study these associations were only detectable among highly religious participants [46] or not detected whatsoever [44]). Effects of perceived stress on other eating behaviors were mixed, with greater stress perceptions associated with more snacking on sweets, haphazard meal planning, and meal skipping in one study [43] but not associated with snacking on sweets in another study [44]. Perceived stress was not associated with whether participants met daily dietary recommendations [47]. One repeated-measures study found that perceived stress was not associated with healthy eating cross-sectionally, but increases in stress perceptions were associated with decreases in healthy eating across time for girls only [48].
Three studies measured whether discrete stressors occurred in samples of adults. Greater numbers of self-reported stressful events in the past year were associated with less healthy eating [49] but not with fat intake [45]. Self-reports of minor stressors experienced over the previous week were associated with fat intake [45]. One study utilizing ecological momentary assessment (EMA) methodologies found that on days when participants experienced more hassles they consumed more snacks; additionally, reporting more daily hassles or the occurrence of stressful events during an EMA sampling period was associated with more snacking both concurrently and in the next sampling period [50]. However, in the same study, EMA assessments of whether a social stressor occurred were not associated with snacking. Three studies assessed both whether a range of stressful events occurred and, if so, how stressful participants perceived each event to be. Using this methodology, daily hassles, past-week stressors, and lifetime traumatic stressors were not directly associated with any eating measure [45, 48, 51].
Finally, seven studies examined the effects of discrimination-related stress on food consumption. Of five studies assessing emotional eating, four found discrimination to be associated with greater emotional eating [41, 42, 52, 53] while one did not [40]. The lifetime occurrence of discrimination was associated with consuming more calories from fat, whereas the perceived stressfulness of those discrimination experiences was not [54]. The frequency of everyday experiences of discrimination was associated with fat consumption for women only [54]. One study utilized an experimental design to assess the effects of social exclusion by a member of a privileged racial/ethnic group, finding that college students consumed more chips when excluded by a NHW peer than when included by a NHW peer; however, eating did not differ when participants were excluded by an AA peer versus included by an AA peer [55].
Nine of the 16 reviewed studies were conducted in a homogenously female population, and one was conducted in a homogenously male population. Though effects of stress on unhealthy eating patterns were typically observed across samples of males and females, one study found this effect for girls but not for boys [48]. Fourteen reviewed studies measured adults, five of which focused on young adults (predominantly college students); one study measured both adolescents and adults, and one study measured children and adolescents. No consistent age-based differences were observed in the effect of stress on eating behavior. One study used a longitudinal repeated-measures design, one study used EMA, and one study used an experimental manipulation; the remaining 13 studies employed cross-sectional, self-report methodology. Most studies utilized self-reports of eating behaviors, though two studies collected more detailed 24-hour dietary recalls, one study used EMA assessments of stress and eating, and one study observed food consumption in the laboratory. No consistent methodological differences were observed in the effect of stress on eating behavior.
In sum, among AA, stressors were generally associated with a range of unhealthy eating behaviors. Perceived stress, the occurrence of stressful events, and discrimination-related stress were typically correlated with unhealthy eating patterns, though these effects varied somewhat based on the specific eating behavior or stress measure utilized. Perceived stress and discrimination-related stress both showed consistent associations with emotional eating, but more variable association with other food consumption measures. Stress measures that combined ratings of whether stressors occurred and how stressful they were perceived to be were generally not associated with eating behaviors for AA.
Hispanic/Latinx Americans.
Eight studies largely supported that stress is associated with more obesogenic eating behavior among HL (see Table 2). No studies showed appetite-suppressive effects of stress. Stress measures included perceived stress (assessed both globally and with respect to academic and pregnancy-related domains), the occurrence of stressful events (including experimentally-induced stress), combined measures assessing the occurrence and perception of stress, and discrimination-related stress (including acculturative stress).
Table 2.
Studies describing associations between stress and eating in Hispanic/Latinx samples, organized by domain of stress assessed.
| Authors (Year) | Participant Characteristics (% female) | Stress Measure | Eating Measure | Findings: Effect of Stress on Eating |
|---|---|---|---|---|
| Perceived stress | ||||
| Fabian et al., 2013 [61]a | 275 Puerto Rican college students (68%) | Perceived academic stress1 | Dietary patterns, snack consumption (self-reports) | MIXED. Academic stress → chocolate intake; ≠ all other dietary patterns, snack foods |
| Isasi et al., 2015 [56]a | 5,077 Adults (62%) | Perceived stress (PSS) | Energy intake; calories from saturated fat; healthy eating (24-hr recalls) | POSITIVE. Stress → calories, saturated fat, less healthy eating |
| Laugero et al., 2011 [57]a | 1,336 Puerto Rican middle aged and older adults (70%) | Perceived stress (PSS) | Dietary intake (self-report) | POSITIVE. Stress → less protein, fruit, vegetables, fiber, omega-3s, and more carb/salty snacks, sweets, high glycemic index foods |
| Lopez-Cepero et al., 2019 [59]a | 580 Adults (51%) | Perceived stress (PSS) | EE (self-report) | POSITIVE. Stress → EE |
| Singh et al., 2017 [60]a | 108 Pregnant adolescents (100%) | Perceived stress (PSS); level of concern over pregnancy-related stressors (PDQ) | Dietary intake of macronutrients and micronutrients (24-hr recall) | MIXED. Stress more → vitamin E; ≠ macronutrient intake, intake of other micronutrients. Pregnancy-related stress → less vitamins B6, C; ≠ macronutrient intake, intake of other micronutrients |
| Villegas et al., 2019 [58]a | 137 Adult Mexican-American immigrant mothers (100%) | Perceived stress (PSS) | Healthy eating (self-report) | POSITIVE. Stress → less healthy eating |
| Occurrence of stressful events | ||||
| Cardel et al., 2016 [62]b | 9 Young adults (67%) | Experimentally manipulated social status2 | Ad-libitum eating (observed) | MIXED. Low social status manipulation → food intake (marginal) |
| Isasi et al., 2015 [56]a | 5,077 Adults (62%) | Number of chronic stressors3 | Energy intake; calories from saturated fat; healthy eating (24-hr recalls) | MIXED. Chronic stressors → calories; ≠ saturated fats, healthy eating |
| Combined: Occurrence and perceived stressfulness of events | ||||
| Simmons & Limbers, 2019 [63]a | 168 Young adolescent middle schoolers (74%) | Occurrence and perceptions of general stressors; combined general and acculturative stress (SAFE-C) | EE (total, anxiety/anger/frustration, depressed, and unsettled, self-report) | MIXED. General stress, combined stress → EE (total, anxiety/anger/frustration, depressed); ≠ EE (unsettled) |
| Discrimination-related stress | ||||
| Simmons & Limbers, 2019 [63]a | 168 Young adolescent middle schoolers (74%) | Occurrence and perceptions of acculturative stress (overall; process and discrimination subdomains; SAFE-C) | EE (total, anxiety/anger/frustration, depressed, and unsettled, self-report) | MIXED. Overall acculturative stress, process → EE (total, anxiety/anger/frustration, depressed); ≠ EE (unsettled); discrimination stress ≠ EE (all domains) |
Note: EE = emotional eating; POSITIVE = association between stress and eating; NS= no association between stress and eating; MIXED = mixed support for associations between stress and eating; ≠ = not significantly associated with; → = associated with; marginal = p-value .05–.10.
Cross-sectional self-report methodology.
Experimental, observational methodology, using randomized, cross-over design to expose participants to both “high social status” and “low social status” conditions, and ad libitum food consumption from buffet meal direction observed.
Stress Measures: PSS = Perceived Stress Scale; SAFE-C = Social, Attitudinal, Familial, and Environmental Acculturative Stress Scale for Children (includes two sub-scales: Process Stress, e.g. “People think I am shy, when really I just have trouble speaking English,” and Discrimination Stress, e.g. “I feel bad when others make jokes about people who are in the same group as me,”); PDQ = Pregnancy Distress Questionnaire.
Unnamed, 27-item measure of perceived academic stress.
Unnamed, participants play a game of monopoly after being assigned to a high social status game piece (Rolls Royce) or low social status game piece (shoe); monopoly opponent was assigned opposite social status.
Unnamed, eight items assessing whether chronic stressors in multiple life domains have been present for at least 6 months.
Six studies assessed perceptions of stress. Global perceived stress was associated with more calories and saturated fats consumed [56], less healthy eating [56–58], more emotional eating [59], and more consumption of vitamin E but not of other micro- or macro-nutrients [60]. Notably, vitamin E is frequently found in the vegetable oils used in processed foods [60]. Perceptions of academic stress specifically were associated with more consumption of chocolate in college students but not with other dietary behaviors [61]. Perceptions of pregnancy-related stress were associated with less consumption of vitamins B6 and C but not of other micro- or macro-nutrients [60].
Two studies assessed the occurrence of stressful events. Experiencing a greater number of chronic stressors was associated with more calorie consumption but not more consumption of saturated fats or less healthy eating [56]. Experiencing an experimentally manipulated stressor was marginally associated with eating, such that that those in the high-stress condition (i.e., assigned to low social status during a game) trended towards eating more [62]. One study used a combined measure of the stressfulness and occurrence of life events, finding stress to be positively associated with most types of emotional eating assessed [63]. One study assessed multiple forms of acculturative stress, finding that total acculturative stress and process stress (but not discrimination stress) were associated with most types of emotional eating patterns assessed [63].
Two of the eight studies were conducted in homogenously female samples; none of the remaining studies reported gender differences. Six of the eight studies included adults of varying ages (one study of young adults, one study of college students, one study of middle aged and older adults only, three studies of adults of varying ages), while two included children and/or adolescents; no consistent age-related differences in the effect of stress on eating were observed. One study observed food consumption following an experimental stress manipulation. The remaining seven studies used cross-sectional, self-report methodologies; of these, two utilized 24-hour dietary recalls, while the remainder administered self-report eating questionnaires. No consistent methodological differences were observed.
In sum, perceptions of stress were typically associated with less healthy eating patterns among HL. Individual studies of chronic stress, general stress, experimentally-manipulated stress exposure, and acculturative stress showed at least partial evidence for associations with unhealthy eating; however, each of these stress types was assessed in only single studies.
Asian Americans.
Our search also identified one stress – eating study conducted in an AS sample. Tseng and Fang [64] utilized 48-hour dietary recalls and self-reports of both the life events (assessed via the Life Experiences Survey) and acculturation-related stress (assessed via the Migration–Acculturation Stressor Scale) with 426 adult Chinese-American females who had immigrated to the US in the last 20 years. Results of this cross-sectional study indicated that both life stress (measured as the combined occurrence and stressfulness of life events) and frequency of migration/acculturation-related stressors were associated with consuming fewer grams of food, but more fatty, energy-dense foods and a fewer carbs and grains. However, stress measures were not related to total calorie intake or percent energy from protein intake.
Aim 2: Comparing racial/ethnic groups in degree of stress-induced eating
As shown in Table 3, five studies included two or more racial/ethnic groups and either conducted a direct statistical comparison of degree of stress-induced eating by group or reported on the same stress – eating associations separately in multiple groups. No studies showed appetite- suppressive effects of stress for any group. Stress constructs included perceived stress (both global and related to perceptions of parental criticism specifically), combined measures of the occurrence and stressfulness of stressors (including both typical life stress and traumatic stress), and discrimination-related stress (including acculturative stress). Of these, two studies showed no group differences, one study showed minimal group differences, and two studies supported that groups differ in at least one important way.
Table 3.
Studies describing associations between stress and eating among multiple racial/ethnic groups, organized by domain of stress assessed.
| Author & Year | Participant Characteristics (% female) | Participant Race/Ethnicity | Stress Measure | Eating Measure | At-risk groups | Protected groups | Findings: Differential Effect of Stress on Eating |
|---|---|---|---|---|---|---|---|
| Perceived Stress | |||||||
| Chang et al., 2016 [65]a | 332 Adult pregnant women enrolled in WIC (100%) | 58% NHW, 42% AA | Perceived stress (PSS) | Fast food, fruit, vegetable, and fat intake (self-report) | None | AA, NHW | No difference. Stress ≠ fast food, fruit, vegetable, or fat intake in either group |
| Goel et al., 2019 [66]a | 1,713 Young adult college students (100%) | 43% NHW, 20% AA, 18% AS, 12% Multi, 7% HL | Perceived parental criticism (FROST-MPS) | Loss of control eating (self-report) | NHW, AA | HL, AS, Multi | Differences. Parental criticism → loss of control eating for NHW and AA, but not for HL, AS, or Multiracial |
| Combined: Occurrence and perceived stressfulness of events | |||||||
| Harrington et al., 2006 [67]a | 178 Young adult college students (100%) | 52% AA, 48% NHW | Combined occurrence of daily hassles in past month (SRLE) and overall perceptions of stress (PSS); Combined occurrence and stressfulness of traumatic events (LSC-R) | Binge eating (self-report) | NHW, AA | AA |
Differences. Stress → binge eating both groups separately; magnitude of stress → eating effect is greater for NHW; in full sample, ethnicity moderates the effect of stress such that stress → eating holds for NHW only Trauma → binge eating for NHW (not for AA) when tested separately; in full sample, no main effect of trauma or trauma by ethnicity interaction |
| Discrimination-related stress | |||||||
| Harrington et al., 2006 [67]a | 178 Young adult college students (100%) | 52% AA, 48% NHW | Perceived stressfulness of racist and sexist events (SRE; SSE) | Binge eating (self-report) | AA | NHW | Differences. Discrimination → binge eating for AA (not for NHW) when tested separately; in full sample, no main effect of stress or stress by ethnicity interaction |
| Kelly et al., 2017 [68]a | 798 Young adults (0%) | 34% HL, 33% AA, 33% AS | Discrimination stress (EDS, AARSI, DSS)1; discrimination related to 2016 election2 | Loss of control eating (self-report) | AA, HL, AS | AS with high ethnic identity | Minimal differences. Discrimination stress → loss of control eating for AA, HL, and AS low in ethnic identity; election-related discrimination → loss of control eating for all groups |
| Kroon Van Diest et al., 2014 [69]a | 247 Young adult college students (100%) | 37% HL, 34% AA, 29% AS | Perceived acculturative stress (SAFE-SF) | Combined: binge eating and EE (self-report) | AA, HL, AS | None | No difference. Acculturative stress → combined binge and EE for all groups |
Note: AA = African-American; AS = Asian; HL = Hispanic/Latinx; NHW = Non-Hispanic White; Multi = Multi-racial/Multi-ethnic; EE = Emotional Eating; → = is associated with; ≠ = not significantly associated with; NS = non-significant.
At-risk groups indicate the racial/ethnic group(s) that exhibited associations between stress and unhealthy eating within a particular study. Protected groups indicate the racial/ethnic group(s) that did not exhibit associations between stress and unhealthy eating within a particular study.
Cross-sectional self-report methodology.
Stress Measures: PSS = Perceived Stress Scale; SRLE = Survey of Recent Life Experiences; LSC-R = Life Stressors Checklist-Revised; SRE = Schedule of Racist Events; SSE = Schedule of Sexist Events; EDS = Everyday Discrimination Scale; AARSI = Asian American Racism-Related Stress Inventory; DSS = Discrimination Stress Scale; SAFE-SF = Societal, Attitudinal, Familial, and Environmental Acculturative Stress Scale, short form; FROST-MPS = Frost Multidimensional Perfectionism Scale.
Measure of discrimination stress varied by racial ethnic group. AA completed EDS, a measure of frequency of unfair treatment; AS completed AARSI, a combined measure of the occurrence and perceived stressfulness of race-related discrimination; HL completed DSS, a combined measure of the occurrence and perceived stressfulness of race-related stressors.
Unnamed, single item measure of race-related stress since the 2016 election, “My experiences with race-related stress and discrimination (e.g., being threatened or harassed, being disrespected) have become worse since Mr. Trump was selected as our next president.”
One study found that global perceptions of stress were not associated with consumption of fast food, fruits, vegetables, or fats for either AA or NHW [65]. However, in another study, racial/ethnic groups differed when perceptions of parental criticism were assessed, such that more parental criticism was associated with greater loss of control in eating for NHW and AA, but not for HL, AS, or multi-racial respondents [66]. In a third study, stress (measured as a combined factor of the occurrence of daily hassles and global perceptions of life stressfulness) was associated with binge eating for both NHW and AA when correlations were measured in each group separately, though effects were stronger for NHW [67]. Similarly, in regression models, ethnicity moderated the effect of stress, such that stress was associated with binge eating only for NHW but not for AA [67]. Parallel analyses found that trauma-related stress (combined occurrence and perception of traumatic events) was associated with binge eating for both NHW and AA when correlations were measured in each group separately; however, in regression models, there was no main effect of trauma, and ethnicity was not supported as a moderator [67].
Finally, three studies examined the effects of discrimination-related or acculturative stress across groups. One study compared AA to NHW, finding that perceptions of discrimination stress related to racism and sexism were associated with binge eating for AA but not for NHW (though in regression models, there was no main effect of discrimination and ethnicity was not supported as a moderator). Two additional studies compared stress-based eating among AA, HL, and AS, finding no or minimal differences in the effect of discrimination- or acculturation-related stress on loss of control eating or a combined index of binge and emotional eating; discrimination was associated with unhealthy eating patterns for all groups [68, 69].
Of the five studies that compared racial/ethnic groups, four included only females and one included only males. All studies measured adult samples, with four of the five studies sampling young adults exclusively (typically college students). All studies used cross-sectional, self-report methodologies. The homogenous nature of the study samples and methods precludes the detection of differences based on gender, age, or methods.
In sum, this limited evidence provides preliminary support that discrimination-related stress is associated with unhealthy eating behaviors for AA, HL, and AS, but not for NHW. Evidence is mixed as to whether NHW differ from other groups as to the effect of other forms of stressors on eating behavior, though when differences emerge, NHW appear to be at greater risk for stress-induced unhealthy eating.
Discussion
The 30 selected studies in this review showed considerable variation in the effects of stress on eating behavior. However, the majority of reviewed studies supported that stress is associated with at least some form of increased obesogenic eating and/or decreased healthy eating patterns in both AA and HL samples. Of those studies examining only one racial/ethnic group, only one study examined stress – eating associations among AS, and no studies assessed NA, PI, or any other racial/ethnic groups. Studies that compared stress – eating associations among racial/ethnic groups had mixed results, with evidence indicating that AA, HL and AS are all sensitive to the effects of discrimination-related stress, but NHW are not. However, contrary to hypotheses, NHW may be more sensitive to the effects of other stressors on obesogenic eating than are other racial/ethnic groups, though the small number of studies directly comparing racial/ethnic groups (N = 5) require that these conclusions remain tentative.
Among AA, global perceptions of stress were generally associated with maladaptive eating behaviors. Perceived stress was most commonly measured with the Perceived Stress Scale (PSS) [70], which assesses subjective and emotional stress appraisals, such as being upset about things that have happened, feeling “stressed,” and perceiving the self as unable to cope with the problems one is facing. This measure may be particularly adept at capturing participants’ perceptions that life circumstances are threatening, highly emotionally arousing, and outside of their capacity to control or manage. Similarly, discrimination-related stressors, which are typically both socially threatening and uncontrollable, were generally associated with unhealthy eating behaviors. Such stressors are particularly likely to evoke the types of HPA activation and recalibration that promote the consumption of energy-rich foods. Additionally, uncontrollable stressors, which exclude the use of direct problem-solving efforts, may particularly trigger passive or emotion-focused coping, such as the consumption of highly palatable foods. Surprisingly, among AA, measures of the occurrence of stressful events were more commonly associated with eating behavior than were measures that accounted for both the occurrence and perceived stressfulness of events. This finding is in contrast to models that highlight the importance of appraisal in shaping both stress response and its downstream impact on eating behavior [e.g., 21]. Stress – eating associations observed in AA held across a wide range of eating measures, including emotional eating, healthy eating, fat consumption, and snack consumption. However, effects were most consistently observed when emotional eating was assessed as the eating behavior measure, suggesting that stress may particularly promote eating as a form of emotion-focused coping.
In studies of HL, associations between subjective stress and eating behavior were commonly detected, particularly when stress was measured globally using the PSS. In line with findings in AA samples, overall perceptions of life stressfulness, emotional difficulty of life, and difficulty coping may be particularly well-suited to induce obesogenic eating via both physiological and behavioral mechanisms. However, perceptions of the stressfulness of discrete stressors (academic stress, pregnancy-related stress) showed less consistent associations with eating measures. Only one study examined the effects of acculturative stress (a discrimination-related stressor) on emotional eating among HL, finding a positive association overall, but not on the discrimination sub-scale. Although more evidence is needed to determine whether race-related stress is as consistent a predictor of eating behavior among HL as it is among AA, two studies that compared AA and HL found no differences in the effect of racial/ethnic discrimination or acculturative stress on risky eating patterns (emotional eating, binge eating, and uncontrolled eating). Therefore, discrimination may be a salient, yet understudied, contributor to HL eating patterns. Stress was shown to influence a wide variety of dietary behaviors among HL including emotional eating, healthy eating, observed ad libitum eating, and dietary intake of calories and macronutrients.
Other US-based racial/ethnic minority groups were under-represented in the literature. As NA and certain PI ethnic groups are at increased risk for obesity [8, 38], the influence of stress on dietary patterns in these groups is markedly under-studied. Among AS, one study of Chinese-American immigrant women suggests that stress alters the type, but not number, of calories consumed. Specifically, in response to stress, AS eat fewer grams in total, but those grams are used for more calorically-dense, fatty foods [64]. This finding suggests that AS women may maintain energy balance even while engaging in some forms of unhealthy eating. Although further research is needed to determine whether this pattern of eating in response to stress is replicated in larger, more diverse samples of AS, if supported, such stress – eating associations may help protect certain subgroups of AS from developing stress-linked obesity. Although no studies examined discrimination-related stress in AS samples alone, two studies that included multiple groups supported that racial/ethnic discrimination and acculturative stress have similar effects on eating behavior across AA, HL and AS [68, 69]; therefore, research is needed to examine the effects of race-related stress among AS specifically.
The five studies that included two or more racial/ethnic groups yielded inconsistent results as to whether groups typically differ in stress – eating associations. Notably, in three studies examining the effects of discrimination-related stresses on eating, all minority groups assessed (AA, HL, AS) showed at least some stress – eating associations; the only study that also included NHW did not support that discrimination was associated with eating for this group. Additional research is needed to determine whether members of minority groups show greater vulnerability for risky eating patterns in response to discrimination and to assess whether this vulnerability, in conjunction with greater rates of exposure to discrimination-related stress, contributes to racial/ethnic obesity disparities. In contrast, of the three studies that utilized other stress measures to compare members of different racial/ethnic groups, two studies supported that NHW are at greater risk for stress – eating associations, while one study did not detect stress – eating associations in any group. NHW may be more susceptible to parental criticism than are HL, AS, or multi-racial Americans, and more susceptible to both general stressors and trauma-related stress than are AA. This finding is unexpected, given that NHW show lower rates of obesity than do AA or HL. These findings may be because stress influences eating behavior more markedly for NHW, but influences other aspects of energy balance, such as activity level, for HL or AA [71, 72]. Additionally, even if NHW show a greater magnitude of stress effects on eating, if minority groups have greater stress exposure, they may still engage in obesogenic eating more frequently, thereby contributing to obesity-related health disparities. Alternatively, minority groups, who have greater stress exposure, may have habituated to the effects of stress on eating behavior, possibly through downregulation of the HPA axis or other mechanisms. Finally, minority groups may benefit from protective social-cultural or genetic factors that disrupt links between stress and dietary patterns.
However, group differences may also reflect measurement limitations. For instance, whereas studies that measured stress – eating associations within homogeneous groups often used measures that were validated in the racial/ethnic samples being assessed [e.g., 73, 74], studies that recruited heterogeneous samples may have used stress measurements that are more adept at capturing the type of stressors NHW experience or the types of eating behaviors NHW engage in. In support of this idea, the only instance in which NHW were less susceptible to stress-induced eating was when racial discrimination was measured as the relevant stressor (using a questionnaire developed for AA populations but modified to measure racism-related distress across races [67]). Additionally, all studies that conducted group comparisons used only self-reported eating variables. AA, HL, and NA may be more likely to under-estimate their food consumption compared to NHW and AS [75]; therefore, self-report instruments may be poorly suited for accurately measuring group differences. Self-report methodology confounds should also be considered with respect to stress measurement, as minority participants may hesitate to report stressful experiences to researchers, who are predominantly NHW [76]. Finally, group comparisons were only conducted in populations of young adults, who were generally college students. These convenience samples may have limited generalizability to broader populations of racial/ethnic groups in the United States. Additionally, the reviewed studies included a wide variety of measures of eating behaviors, which limits the ability to draw conclusions about how stressors shape specific unhealthy eating patterns. Future studies should consistently employ observational measures of in-lab eating or 24-hour diet recalls to more precisely assess group differences in stress – eating associations. Moreover, as most of the studies included were cross-sectional, the directionality of effects for stress and eating cannot be determined. Future studies should employ both longitudinal methods and experimental designs to examine how stress shapes eating behavior over time.
Most stress assessments utilized global or composite measures (e.g., rating overall stressfulness of life, rating the stressfulness of multiple life domains [e.g., work, family, health] in a single measure, measuring whether a wide variety of stressors occurred in a given time period). However, seven studies assessed stress related to a single domain or construct, other than discrimination or acculturation-related stress. These included: traumatic events (N = 2), experimentally-manipulated social exclusion by an in-group or out-group member (N = 1), experimentally-manipulated social status (N = 1), academic stress (N = 1), pregnancy-related stress (N = 1), and parental criticism (N = 1). These stressors may represent additional, important stress constructs (e.g., intra-familial stressors, social stressors, health-related stressors) which may also exert unique effects on eating behaviors among various racial/ethnic groups. However, the small number of each type of stressor precludes such cross-study integration to assess these broader constructs until more research is conducted.
The inconsistent findings reported across studies highlights the importance of identifying moderating variables. Several studies included analyses of moderators, identifying female gender, low ethnic identity, high religiosity, and obesity as multiplicative risk factors. However, protective psychosocial factors, such as supportive relationships and effective coping strategies, may diminish the effect of stress on eating patterns [77, 78]. Whether these moderators are effective within specific racial/ethnic groups remains unknown.
In addition to race/ethnicity, sex/gender, age, and country-of-origin/culture may have moderating influences on the effects of stress on eating behaviors. Women and girls were over-represented, with over half of studies (N = 16) measuring only female participants, but just two studies assessing only male participants. Although some evidence suggests that women may be particularly susceptible to the effects of stress on eating behavior generally [e.g., 35], reviewed studies provided insufficient evidence to examine whether these sex/gender differences exist within particular racial/ethnic groups. Although a range of ages and developmental stages were represented, studies primarily included adults, often college students. This precludes assessing racial/ethnic differences in the developmental course of stress – eating associations and limits the generalizability of results. Given that racial/ethnic disparities in obesity emerge by childhood and adolescence, identifying the onset of stress-induced eating may have important clinical implications, as identifying and disrupting early risky trajectories in childhood may prevent the development of obesity and related adverse health outcomes in adulthood. Additionally, understanding stress – eating associations in middle and later life may also prove valuable, as the health consequences of obesogenic eating behavior emerge during these developmental periods. In order to fully examine the developmental trajectory of stress – eating associations, longitudinal studies are needed to assess how early stress exposure shapes later eating behavior among various racial/ethnic groups. Notably, only one of 30 reviewed studies utilized a longitudinal method, with two assessments separated by only one month [48]. Moreover, significant heterogeneity in culture and country-of-origin exists within US racial/ethnic groups, which may further moderate the influence of stress on eating patterns. For example, although we synthesized findings across studies that included HL populations, the nature of stress – eating associations may vary between subgroups, e.g., Puerto Rican [57, 61] and Mexican-American participants [58]; however, the limited number of studies examining homogeneous HL subpopulations precluded reviewing groups separately. Additional studies are needed to identify the potential moderating roles of culture and country-of-origin within racial/ethnic groups. Lastly, reviewed studies did not consistently delineate definitions of race/ethnicity employed; participants may respond differently when asked to describe their US Census racial/ethnic category, the racial/ethnic group with which they most identify, or the racial/ethnic group they are most commonly perceived as belonging to by others. Future studies should specify the measure of race/ethnicity utilized and consider employing multidimensional measures of racial/ethnic classification, in order to further specify the moderating role of race/ethnicity.
In sum, the 30 reviewed studies support that stress-induced eating is a plausible link in the chain from stress exposure to obesity across diverse racial/ethnic groups in the US. Additional research using observational measures of eating and cross-culturally valid measures of stress are needed to determine whether racial/ethnic groups differ in their susceptibility to stress-induced eating and to determine the magnitude of these effects. To this end, more studies are needed that examine the effects of stress on eating patterns in racial/ethnic groups separately or that examine the moderating role or race/ethnicity in stress – eating associations within diverse samples. Limited evidence supports that members of minority groups may be more susceptible to discrimination-related stresses, while NHW may be more susceptible to other forms of stress. While the current study examined the direct relationship between stress and eating behaviors within individuals, research linking systemic, social stressors to obesity-related health in broader populations is also needed in order to understand how multiple social-ecological systems simultaneously contribute to racial/ethnic obesity disparities [e.g., 79]. Future studies should additionally identify both relatively static moderating characteristics (e.g., sex/gender) in order to identify populations at the greatest risk for eating patterns in response to stress, as well as dynamic moderating characteristics (e.g., coping, social support) in order to leverage naturally-occurring protective factors. Determining these risk and resilience factors is a necessary foundation for the development and implementation of interventions to protect against racial/ethnic disparities in both obesity and its associated public health burdens, by breaking links between stress and obesogenic eating patterns. The present review provides initial evidence that stress shapes eating patterns in AA and HL populations, and points to the need for targeted future research to examine whether eating behavior provides a mechanism by which the unequal burden of stress among US minority groups shapes a cascade of inequalities, including obesity, associated diseases, and premature death.
Acknowledgements:
The authors wish to thank their colleagues from the Biobehavioral Research on Adolescent Development (BRoAD) Lab at the University of California, Irvine, for their contributions.
Funding: This work was supported, in part, by grants from the National Institutes of Health (F32MD014050, R01DA040966, R01MD010757, and R01MH108155).
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflicts of interest/Competing interests: On behalf of all authors, the corresponding author states that there are no conflicts of interest that may influence this work. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Availability of data and material: Not applicable.
Code availability: Not applicable.
References
- 1.Bhaskaran K, Douglas I, Forbes H, dos-Santos-Silva I, Leon DA, Smeeth L. Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5.24 million UK adults. Lancet. 2014; 384:755–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Institute of Health, National Heart, Lung, and Blood Institute. Managing overweight and obesity in adults: Systematic evidence review from the obesity expert panel. 2013. https://www.nhlbi.nih.gov/sites/default/files/media/docs/obesity-evidence-review.pdf. Accessed Jan 24 2020.
- 3.National Heart, Lung, Blood Institute, National Institute of Diabetes, Digestive, & Kidney Diseases. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report (No. 98). 1998.
- 4.Franssen FME, O’Donnell DE, Goossens GH, Blaak EE, Schols AMWJ. Obesity and the lung: 5· Obesity and COPD. Thorax. 2008; 63(12): 1110–7. [DOI] [PubMed] [Google Scholar]
- 5.U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. 2020. leading health indicators: Nutrition, physical activity, and obesity. http://www.healthypeople.gov/2020/leading-health-indicators/2020-lhi-topics/Nutrition-Physical-Activity-and-Obesity. Accessed Jan 24 2020.
- 6.Hammond RA, Levine R. The economic impact of obesity in the United States. Diabetes Metab Syndr Obes. 2010; 3:285–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015–2016. NCHS data brief, no 288. Hyattsville, MD: National Center for Health Statistics. 2017. [Google Scholar]
- 8.Broussard BA, Johnson A, Himes JH et al. Prevalence of obesity in American Indians and Alaska Natives. Am J Clin Nutr. 1991; 53(6):1535S–1542S. [DOI] [PubMed] [Google Scholar]
- 9.National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on Community-Based Solutions to Promote Health Equity in the United States; Baciu A, Negussie Y, Geller A, et al. , editors. Communities in Action: Pathways to Health Equity. Washington (DC): National Academies Press (US); 2017. January 11. 2, The State of Health Disparities in the United States. Available from: https://www.ncbi.nlm.nih.gov/books/NBK425844/ [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Health disparities experienced by black or African Americans--United States. MMWR: morbidity and mortality weekly report. 2005; 54(1): 1–3. [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Health disparities experienced by Hispanics--United States. MMWR: Morbidity and mortality weekly report. 2004; 53(40): 935–937. [PubMed] [Google Scholar]
- 12.O’Keefe EB, Meltzer JP, Bethea TN. Health disparities and cancer: racial disparities in cancer mortality in the United States, 2000–2010. Front Public Health. 2015; 3: 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clarke CA, Miller T, Chang ET, Yin D, Cockburn M, Gomez SL. Racial and social class gradients in life expectancy in contemporary California. Soc Sci Med. 2010;70(9):1373–1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American College of Physicians. Racial and Ethnic Disparities in Health Care: A Position Paper of the American College of Physicians. Ann Intern Med. 2004;141: 226–232. [DOI] [PubMed] [Google Scholar]
- 15.Abraham PA, Kazman JB, Zeno SA, Deuster PA. Obesity and African Americans: physiologic and behavioral pathways. ISRN obesity. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Krueger PM, Reither EN. Mind the gap: race/ethnic and socioeconomic disparities in obesity. Curr Diab Rep. 2015; 15(11): 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stryjecki C, Alyass A, Meyre D. Ethnic and population differences in the genetic predisposition to human obesity. Obes Rev. 2018; 19(1): 62–80. [DOI] [PubMed] [Google Scholar]
- 18.Sternthal MJ, Slopen N, Williams DR. Racial disparities in health: how much does stress really matter? Bois Rev Soc Sci Res Race. 2011;8:95–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boardman JD, Alexander KB. Stress trajectories, health behaviors, and the mental health of black and white young adults. Soc Sci Med. 2011; 72:1659–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hatch SL, Dohrenwend BP. Distribution of traumatic and other stressful life events by race/ethnicity, gender, SES and age: a review of the research. Am J Community Psychol. 2007; 40 (3–4):313–32. [DOI] [PubMed] [Google Scholar]
- 21.Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav. 2007; 91:449–58. [DOI] [PubMed] [Google Scholar]
- 22.Sominsky L, Spencer SJ. Eating behavior and stress: a pathway to obesity. Front Psychol. 2014; 5:434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.O’Connor DB, Conner M. Effects of stress on eating behavior. In Contrada RJ, Baum A (eds) Handbook of Stress Science: Psychology, Biology and Health. New York: Springer Publishing Company. 2011: 275–286. [Google Scholar]
- 24.Hill DC, Moss RH, Sykes-Muskett B, Conner M, O’Connor DB. Stress and eating behaviors in children and adolescents: systematic review and meta-analysis. Appetite. 2018; 123: 14–22. [DOI] [PubMed] [Google Scholar]
- 25.Chrousos GP, Loriaux DL, Gold PW Introduction: the concept of stress and its historical development. In: Chrousos GP, Loriaux DL, Gold PW (eds) Mechanisms of Physical and Emotional Stress. Advances in Experimental Medicine and Biology, vol 245. Boston: Springer. 1988. 3–7. [Google Scholar]
- 26.Fink G Stress: Definition and history. In: Fink G (ed) Stress Science: Neuroendocrinology. Sand Diego: Elsevier Academci Press. 2010:3–9. [Google Scholar]
- 27.Bosch JA, de Geus EJ, Carroll D, et al. A general enhancement of autonomic and cortisol responses during social evaluative threat. Psychosom Med. 2009; 71(8):877–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Macht M, Mueller J. Immediate effects of chocolate on experimentally induced mood states. Appetite, 2007; 49(3): 667–674 [DOI] [PubMed] [Google Scholar]
- 29.Dallman MF, Pecoraro N, Akana SF et al. Chronic stress and obesity: a new view of “comfort food”. Proc Natl Acad Sci USA. 2003; 100(20):11696–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Danese A, Tan M. Childhood maltreatment and obesity: systematic review and meta-analysis. Mol Psychiatry. 2014; 19(5):544–54. [DOI] [PubMed] [Google Scholar]
- 31.Yau YH, Potenza MN. Stress and eating behaviors. Minerva Endocrinol. 2013; 38(3):255–67. [PMC free article] [PubMed] [Google Scholar]
- 32.Mezuk B, Abdou CM, Hudson D, Kershaw KN, Rafferty JA, Lee H, et al. “White Box” epidemiology and the social neuroscience of health behaviors: The environmental affordances model. Soc Ment Health. 2013; 3, 79–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kandiah J, Yake M, Jones J, Meyer M. Stress influences appetite and comfort food preferences in college women. Nutr Res. 2006; 26(3):118–123. [Google Scholar]
- 34.Cartwright M, Wardle J, Steggles N, Simon AE, Croker H, Jarvis MJ. Stress and dietary practices in adolescents. Health Psychol. 2003; 22(4):362–9. [DOI] [PubMed] [Google Scholar]
- 35.Zellner DA, Loaiza S, Gonzalez Z, et al. Food selection changes under stress. Physiol Behav 2006; 87:789–93. [DOI] [PubMed] [Google Scholar]
- 36.Stone AA, Brownell KD. The stress-eating paradox: multiple daily measurements in adult males and females. Psychol Health. 1994; 9(6):425–436. [Google Scholar]
- 37.Oliver G,Wardle J, Gibson EL. Stress and food choice: a laboratory study. Psychosom Med. 2000;62(6):853–65. [DOI] [PubMed] [Google Scholar]
- 38.Davis J, Busch J, Hammatt Z, Novotny R, Harrigan R, Grandinetti A, Easa D. The relationship between ethnicity and obesity in Asian and Pacific Islander populations: a literature review. Ethnicity & disease. 2004; 14(1): 111–118. [PubMed] [Google Scholar]
- 39.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009; 151(4):264–269. [DOI] [PubMed] [Google Scholar]
- 40.Diggins A, Woods-Giscombe C, Waters S. The association of perceived stress, contextualized stress, and emotional eating with body mass index in college-aged Black women. Eat Behav. 2015; 19:188–192. [DOI] [PubMed] [Google Scholar]
- 41.Johnson P, Risica PM, Gans KM, Kirtania U, Kumanyika SK. Association of perceived racial discrimination with eating behaviors and obesity among participants of the SisterTalk study. J Natl Black Nurses Assoc. 2012; 23(1):34–40. [PMC free article] [PubMed] [Google Scholar]
- 42.Longmire-Avital B, McQueen C. Exploring a relationship between race-related stress and emotional eating for collegiate Black American women. Women Health. 2019; 59(3):240–251. [DOI] [PubMed] [Google Scholar]
- 43.Pickett S, McCoy TP. Effect of psychosocial factors on eating behaviors and BMI among African American women. Clin Nurs Res. 2018; 27(8):917–935. [DOI] [PubMed] [Google Scholar]
- 44.Sims R, Gordon S, Garcia W, et al. Perceived stress and eating behaviors in a community-based sample of African Americans. Eat Behav. 2008; 9(2):137–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sims M, Lipford KJ, Patel N, Ford CD, Min YI., Wyatt SB. Psychosocial factors and behaviors in African Americans: the Jackson heart study. Am J Prev Med. 2017; 52(1):S48–S55. [DOI] [PubMed] [Google Scholar]
- 46.Horton SE, Timmerman GM, Brown A. Factors influencing dietary fat intake among black emerging adults. J Am Coll Health. 2018; 66(3):155–164. [DOI] [PubMed] [Google Scholar]
- 47.Carson TL, Desmond R, Hardy S. et al. A study of the relationship between food group recommendations and perceived stress: findings from black women in the Deep South. J Obes. 2015; 203164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Austin AW, Smith AF, Patterson SM. Stress and dietary quality in black adolescents in a metropolitan area. Stress Health. 2009; 25(2):171–178. [Google Scholar]
- 49.Klassen AC, Smith KC, Black MM, Caulfield LE. Mixed method approaches to understanding cancer-related dietary risk reduction among public housing residents. J Urban Health. 2009; 86(4):624–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zenk SN, Horoi I, McDonald A, Corte C, Riley B, Odoms-Young AM. Ecological momentary assessment of environmental and personal factors and snack food intake in African American women. Appetite. 2014; 83:333–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Harrington EF, Crowther JH, Shipherd JC. Trauma, binge eating, and the “strong Black woman”. J Consult Clin Psychol. 2010; 78(4):469–79. [DOI] [PubMed] [Google Scholar]
- 52.Coleman A, O’Neil J, Ferris AM. The mediation effect between everyday discrimination, gender role conflict, emotional eating, and obesity in African American fathers and sons. Psychol Men Masc. 2019; 20(2):182. [Google Scholar]
- 53.Hoggard LS, Volpe V, Thomas A, Wallace E, Ellis K. The role of emotional eating in the links between racial discrimination and physical and mental health. J Behav Med. 2019; 42(6):1091–1103. [DOI] [PubMed] [Google Scholar]
- 54.Sims M, Diez-Roux AV, Gebreab SY, et al. Perceived discrimination is associated with health behaviours among African-Americans in the Jackson Heart Study. J Epidemiol Community Health. 2016; 70(2):187–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hayman LW Jr, McIntyre RB, Abbey A. The bad taste of social ostracism: the effects of exclusion on the eating behaviors of African-American women. Psychol Health. 2015; 30(5):518–33 [DOI] [PubMed] [Google Scholar]
- 56.Isasi CR, Parrinello CM, Jung MM, et al. Psychosocial stress is associated with obesity and diet quality in Hispanic/Latino adults. Ann Epidemiol. 2015; 25(2):84–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Laugero KD, Falcon LM, Tucker KL. Relationship between perceived stress and dietary and activity patterns in older adults participating in the Boston Puerto Rican Health Study. Appetite. 2011; 56(1):194–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Villegas E, Wiley A, Hannon B, Teran-Garcia M, Hammons A. The effects of Hispanic immigrant mother’s resiliency on children’s dietary adjustment. J Immigr Minor Health. 2019; 21(4):778–86. [DOI] [PubMed] [Google Scholar]
- 59.Lopez-Cepero A, Frisard C, Bey G, Lemon SC, Rosal MC. Association between food insecurity and emotional eating in Latinos and the mediating role of perceived stress. Public Health Nutr. 2019; 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Singh A, Trumpff C, Genkinger J, et al. Micronutrient dietary intake in Latina pregnant adolescents and its association with level of depression, stress, and social support. Nutrients. 2017; 9(11):1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fabian C, Pagan I, Rios JL, et al. Dietary patterns and their association with sociodemographic characteristics and perceived academic stress of college students in Puerto Rico. P R Health Sci J. 2013; 32(1):36–43. [PubMed] [Google Scholar]
- 62.Cardel MI, Johnson SL, Beck J, et al. The effects of experimentally manipulated social status on acute eating behavior: a randomized, crossover pilot study. Physiol Beha. 2016; 162:93–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Simmons S, Limbers CA. Acculturative stress and emotional eating in Latino adolescents. Eat Weight Disord. 2019; 24(5):905–914. [DOI] [PubMed] [Google Scholar]
- 64.Tseng M, Fang CY. Stress is associated with unfavorable patterns of dietary intake among female Chinese immigrants. Ann Behav Med. 2011. ;41(3):324–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chang MW, Brown R, Nitzke S. Fast food intake in relation to employment status, stress, depression, and dietary behaviors in low-income overweight and obese pregnant women. Matern Child Health J. 2016; 20(7):1506–17. [DOI] [PubMed] [Google Scholar]
- 66.Goel NJ, Burnette CB, Mazzeo SE. Racial and ethnic differences in the association between parent-oriented perfectionism and disordered eating in college women. Int J Eat Disord. 2019. [DOI] [PubMed] [Google Scholar]
- 67.Harrington EF, Crowther JH, Payne Henrickson HC, Mickelson KD. The relationships among trauma, stress, ethnicity, and binge eating. Cultur Divers Ethnic Minor Psychol. 2006; 12(2):212–29. [DOI] [PubMed] [Google Scholar]
- 68.Kelly NR, Smith TM, Hall GC, et al. Perceptions of general and postpresidential election discrimination are associated with loss of control eating among racially/ethnically diverse young men. Int J Eat Disord. 2018; 51(1):28–38. [DOI] [PubMed] [Google Scholar]
- 69.Kroon Van Diest AM, Tartakovsky M, Stachon C, Pettit JW, Perez M. The relationship between acculturative stress and eating disorder symptoms: is it unique from general life stress? J Behav Med. 2014; 37(3):445–57. [DOI] [PubMed] [Google Scholar]
- 70.Cohen S, Kamarck T, Mermelstein R. Perceived stress scale. Measuring stress: A guide for health and social scientists. 1994; 10: 1–2. [Google Scholar]
- 71.Crespo CJ, Smit E, Andersen RE, Carter-Pokras O, & Ainsworth BE (2000). Race/ethnicity, social class and their relation to physical inactivity during leisure time: results from the Third National Health and Nutrition Examination Survey, 1988–1994. Am J Prev Med. 2000; 18(1): 46–53. [DOI] [PubMed] [Google Scholar]
- 72.Stults-Kolehmainen MA, Sinha R. The Effects of Stress on Physical Activity and Exercise. Sports Med. 2014; 44: 81–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Schlundt DG, Hargreaves MK, Buchowski MS. The eating behavior patterns questionnaire predicts dietary fat intake in African American women. J Am Diet Assoc. 2003; 103(3):338–45 [DOI] [PubMed] [Google Scholar]
- 74.Fernandez S, Olendzki B, Rosal MC. A dietary behaviors measure for use with low-income, Spanish-speaking Caribbean Latinos with type 2 diabetes: the Latino Dietary Behaviors Questionnaire. J Am Diet Assoc. 2011; 111(4):589–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hebert JR, Patterson RE, Gorfine M, Ebbeling CB, Jeor STS, Chlebowski RT. Differences between estimated caloric requirements and self-reported caloric intake in the women’s health initiative. Ann Epidemiol. 2003; 13(9):629–637. [DOI] [PubMed] [Google Scholar]
- 76.Lin L, Stamm K, Christidis P. How diverse is the psychology workforce? News from APA’s Center for Workforce Studies. Monitor on Psychology. 2018; 49(2): 19. [Google Scholar]
- 77.Pollard TM, Steptoe A, Canaan L, Davies GJ, Wardle J. Effects of academic examination stress on eating behavior and blood lipid levels. Int J Behav Med. 1995; 2(4):299–320. [DOI] [PubMed] [Google Scholar]
- 78.Young D, Limbers CA. Avoidant coping moderates the relationship between stress and depressive emotional eating in adolescents. Eat Weight Disord. 2017; 22(4):683–691. [DOI] [PubMed] [Google Scholar]
- 79.Archibald PC, Parker L & Thorpe R Criminal Justice Contact, Stressors, and Obesity-Related Health Problems Among Black Adults in the USA. J. Racial and Ethn Health Disparities 2018; 5, 387–97. 10.1007/s40615-017-0382-9 [DOI] [PMC free article] [PubMed] [Google Scholar]


