Abstract
Purpose
The South Australian Aboriginal Birth Cohort (SAABC) is a prospective, longitudinal birth cohort established to: (1) estimate Aboriginal child dental disease compared with population estimates; (2) determine the efficacy of an early childhood caries intervention in early versus late infancy; (3) examine if efficacy was sustained over time and; (4) document factors influencing social, behavioural, cognitive, anthropometric, dietary and educational attainment over time.
Participants
The original SAABC comprised 449 women pregnant with an Aboriginal child recruited February 2011 to May 2012. At child age 2 years, 324 (74%) participants were retained, at age 3 years, 324 (74%) participants were retained and at age 5 years, 299 (69%) participants were retained. Fieldwork for follow-up at age 7 years is underway, with funding available for follow-up at age 9 years.
Findings to date
At baseline, 53% of mothers were aged 14–24 years and 72% had high school or less educational attainment. At age 3 years, dental disease experience was higher among children exposed to the intervention later rather than earlier in infancy. The effect was sustained at age 5 years, but rates were still higher than general child population estimates. Experiences of racism were high among mothers, with impacts on both tooth brushing and toothache. Compared with population estimates, levels of self-efficacy and self-rated oral health of mothers at baseline were low.
Future plans
Our data have contributed to a better understanding of the environmental, behavioural, dietary, biological and psychosocial factors contributing to Aboriginal child oral and general health, and social and emotional well-being. This is beneficial in charting the trajectory of cohort participants’ health and well-being overtime, particularly in identifying antecedents of chronic diseases which are highly prevalent among Aboriginal Australians. Funding for continued follow-up of the cohort will be sought.
Trial registration number
ACTRN12611000111976; Post-results.
Keywords: community child health, public health, epidemiology
Strengths and limitations of this study.
One of the largest, most contemporary Aboriginal Birth Cohorts in Australia (indeed, of an Indigenous population in the world), that recruited during pregnancy and that will have follow-ups at five key time-points (child age 2 years, 3 years, 5 years, 7 years (data currently being collected) and 9 years (funding available)).
Established Aboriginal Reference Group who provide governance and oversight of all study processes, strong rapport with South Australian Aboriginal community and excellent participant retention.
There are very few insights into Aboriginal child development stemming from prospective longitudinal birth cohorts; our richly characterised and representative information is able to answer questions that Aboriginal communities want answered with respect to Aboriginal child health and development.
Small sample size (n=449) due to the small sampling pool who were eligible during recruitment.
Follow-up at age 7 years has been impacted due to social distancing restrictions necessitated by the COVID-19 pandemic. This may impact our age 9 years follow-up also.
Introduction
Untreated dental caries (tooth decay) in children may cause substantial pain and have severe consequences on eating, sleeping, playing, learning and general quality of life.1 It is associated with other chronic childhood conditions such as malnutrition, and is the strongest predictor of poor oral health in adulthood.2 Childhood caries is entirely preventable, yet Indigenous Australian children experience high prevalence of the disease, with Indigenous children in some areas having up to five times the prevalence of their non-Indigenous counterparts.3 In the 2012–2014 National Child Oral Health Survey, the mean number of decayed, missing or filled tooth surfaces in the primary dentition of Indigenous children aged 5–10 years was 6.3 compared with 2.9 among non-Indigenous children.4
Provision of dental care to young Indigenous children can pose many challenges because of child stage of emotional and physical development, and consequent capacity for cooperation in the dental chair. The issues are multiplied for Indigenous children in rural and remote locations, where access to dental care is severely limited. Hospital-based treatment under general anaesthetic is an increasingly utilised mode of dental treatment for such children, with Indigenous Australian children having twice the rate of hospital admissions for dental care than non-Indigenous children.5 However, dental treatment under general anaesthetic does not prevent the occurrence of new dental decay, with children frequently readmitted for hospital-based dental general anaesthetic after their initial treatment.6 Oral rehabilitation under general anaesthetic also does little to alleviate dental fear or to change non-cooperative behaviour and may, in fact, heighten these characteristics. Moreover, comprehensive dental care under general anaesthetic is not without risk, including the potential for long-term adverse neuro-developmental effects.7–9 Dental general anaesthetics are extremely expensive for the tax-payer and community more broadly, and require considerable time and financial investments from carers (to transport child to hospital, stay overnight, ensure fasting prior to operation, etc). The estimated mean cost of dental general anaesthetics for Indigenous children is substantially higher than the cost of care for non-Indigenous children.7 Preventive approaches that can be undertaken in the homes or Aboriginal Community Controlled Health Organisations of Indigenous children to reduce the number of children undergoing dental general anaesthetics is thus urgently required.
Regrettably, Australian Aboriginal children score worse on almost every indicator of general health and well-being relative to their non-Aboriginal counterparts. There is a higher prevalence of nutrition-related stunting, non-optimal blood pressure and growth outcomes10 and poorer social and emotional well-being.11 Around one-fifth of Aboriginal children are overweight or obese,12 and around 30% may not be exercising at recommended levels.11 Little is known about the dietary patterns of Aboriginal children but there is some evidence of low rates of fruit, vegetables, water and milk consumption.13 The literature suggests that many of the conditions experienced in Aboriginal childhood are antecedents to chronic disease in later life. Recent studies have shown that growth in childhood, especially rapid weight gain around 4–5 years, is associated with increased risk of being overweight,14 elevated blood pressure, clustered metabolic risk,15 coronary events16 and stroke.17 Data suggest that individuals who are small in the first 2 years of life and subsequently gain weight rapidly present the highest levels of risk. Evidence from a recent national report on the Australian Early Development Census, which contained information on almost 290 000 5-year old Australian children, indicated that almost half the Aboriginal children were developmentally vulnerable on one or more of the five domains (physical, social, emotional, cognitive/language and communication). This was more than twice the proportion of non-Aboriginal children.18
Methods
Study design
The South Australian Aboriginal Birth Cohort (SAABC) study was established in 2011 to provide direct estimates of Aboriginal child dental disease in South Australia compared with general population estimates, to determine if an intervention aiming to reduce prevalence of early childhood caries was more effective in early versus late infancy, to examine if these differences were sustained over time, and to document social, behavioural, cognitive, anthropometric, dietary and educational attainment over time. Funding was originally received in 2011 to establish the cohort and to follow-up at child ages 2 and 3 years.19 Further funding was received to follow-up the children at age 5 years, with current funding received to follow-up the children at age 7 years (currently suspended due to COVID-19 restrictions) and 9 years.
At baseline, 449 women pregnant with an Aboriginal child were recruited and randomly allocated to either an immediate intervention (n=223) or delayed intervention group (n=225, figure 1). The immediate intervention group received the following:
Figure 1.
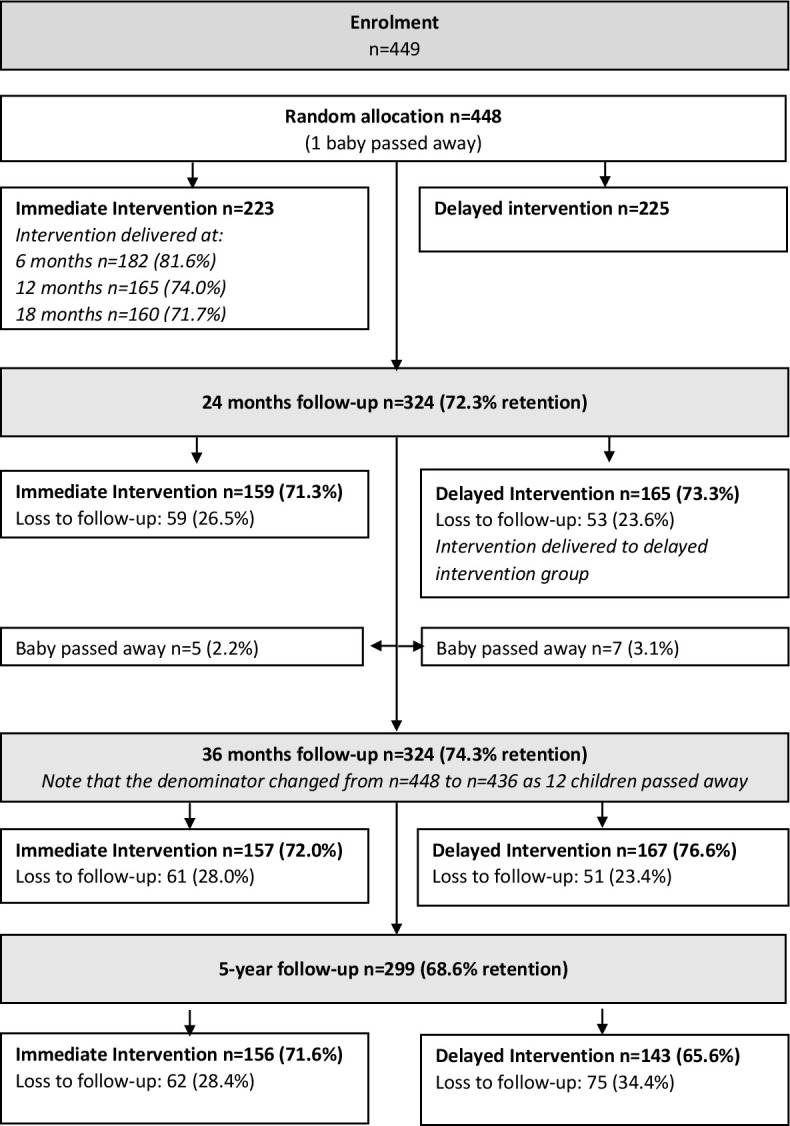
Flow diagram of participants through key stages of the study intervention comprised: (1) dental care to mother; (2) anticipatory guidance (mother); (3) motivational interviewing (mother) and; (4) fluoride varnish application (child). Intervention delivered during pregnancy to child aged 18 months for immediate intervention group, at child aged 24–36 months for delayed intervention group.
Dental care to pregnant mothers: mothers who were allocated randomly to the immediate intervention arm and who were eligible for publically funded dental care (through ownership of a means-tested government healthcare card) received dental care through the South Australian Dental Service (SADS). Study staff organised transport and appointments, through assistance from SADS’s Aboriginal Liaison Programme. Six private dentists provided care to participants who were not eligible for publically funded care. Dental care included X-rays, check-ups, scale and prophylaxis, fillings and extractions (including wisdom teeth). Not provided were cosmetic dentistry, endodontics and orthodontics.
Fluoride varnish applied at child ages 6, 12 and 18 months: the protocol for fluoride varnish was based on that used by Slade and colleagues.20 Study staff were trained in its use and applied it. Children were supine, with their teeth cleaned and dried with gauze. Fluoride varnish was applied from the back teeth first, before moving forward to the front teeth. Children (through their carers) were advised to not eat food or drink for half an hour.
Anticipatory guidance: oral health educational packages that were tailored to contain dental-specific information relevant for pregnant mothers (focus on dental treatment, pregnancy gingivitis) and when children were aged 6 months (focus on first solids, caring for baby teeth on initial eruption), 12 months (focus on tooth brushing and fluoride, avoiding sugar-containing beverages and foods) and 18 months (focus on child’s first dental check-up, molar teeth eruption).
Motivational interviewing (MI): in combination with anticipatory guidance, MI was implemented with pregnant mothers and at child ages 6, 12 and 18 months. Study staff completed an initial 2-day MI training course, followed by an intensive 1-day follow-up. One-day follow-up training was continued monthly for 6 months. This was followed by 1-day coaching every 2 months, with occasional telephone coaching, for a further year. Each MI session was conducted on a one-to-one basis in venues where participants felt comfortable (eg, community halls, local Aboriginal health services, participants’ homes). MI sessions ranged from 30 to 90 min. Pictorial prompts and plain English summaries were used.21 A member of the Motivational Interviewing Network of Trainers conducted the fidelity testing of the MI sessions, which was found to be acceptable.22
When children were aged 24 months, delayed intervention group mothers received dental care. Fluoride varnish application, anticipatory guidance and MI for delayed intervention participants were delivered when children were aged 24, 30 and 36 months, respectively.
Statistical analysis
Intention-to-treat principles have been used for all data analyses to estimate the effect of the intervention on dental caries experience. General linear regression models were used to compare the efficacy of the intervention on mean number of decayed, missing and filled teeth between immediate and delayed intervention groups at child age 5 years. To account for any contributing factors, we adjusted for baseline maternal sociodemographic, health status and dental behaviour characteristics. The ‘Proc genmod’ function was used in SAS, with link=identity and distribution=normal, so Generalised Linear Models (GLM) could be fitted and the least squares estimates obtained. Because, at age 5 years, nearly one-third of mother–child pairs were lost to follow-up, a Fully Conditional Specification method was used to impute missing data, based on the assumption that data were missing at random (MAR). Immediate and delayed intervention groups were imputed separately. Fifty imputed datasets were created using 50 iterations, with the results from the imputed datasets combined using Rubin’s rules via the ‘Proc mianalyse’ function. Sensitivity analyses were conducted using the ‘MNAR adjust statement’, with different scenarios for dental outcomes, which included different percentages of MAR assumptions and maximum and minimum value imputations. SAS statistical software (SAS V.9.4, SAS Institute Inc, Cary, North Carolina, USA) was used for all analysis and imputation.
Cohort description
Who is in the cohort?
This prospective birth cohort study was developed in partnership with local Aboriginal communities and endorsed by the study’s Aboriginal Reference Group. Ethical approvals were received from the University of Adelaide Human Research Ethics Committee (H-057-2010), the Aboriginal Health Council of South Australia (04-09-362), the South Australian Department for Health, including the human research ethics committees of participating South Australian hospitals (Flinders Medical Centre: 435-10; Lyell McEwin Hospital: 2010-160; and the Women’s and Children’s Hospital: REC2322/11/13). Participants provided signed informed consent. Participants were 449 women pregnant with an Aboriginal child who were residing in South Australia during the recruitment period of February 2011 to May 2012. Recruitment was through the antenatal clinics of South Australian Aboriginal Community Controlled Health Organisations and hospitals. The sample represented two-thirds of those who were eligible during the recruitment period, and was representative by age, socioeconomic position and tobacco smoking status.23 One child passed away in utero and a further 12 passed away before their second birthday. At child age 2 years, 324 (74% retention) participants were followed up (figure 1). At age 3 years, 324 (74% retention) participants were followed up. At age 5 years, 299 (69% retention) participants were followed up.
How often have they been followed up?
Participants were recruited during pregnancy (baseline) and have been followed up at child mean ages 2, 3, 5 and 7 years (currently suspended due to COVID-19). Baseline and lost to follow-up sample characteristics are shown for pregnancy and child ages 2, 3 and 5 years in table 1. At baseline, over half (53%) of mothers were aged 14–24 years and 72% had achieved high school or less as their highest educational attainment. Around 86% received their income from Centrelink (government agency who provide welfare based on means testing) and 82% owned a healthcare card (means-tested, allows access to some health services, eg, dental public health services that otherwise incur out-of-pocket expenses). Around 61% resided in non-metropolitan locations and almost two-thirds (64%) usually visit a dentist because of a problem. Three-quarters (75%) of mothers reported brushing their teeth the previous day and while 55% rated their oral health as fair or poor, only 10% rated their general health as fair or poor. A higher proportion of participants who were not followed-up at child ages 2, 3 and 5 years had (at baseline) lower educational attainment, received their income from Centrelink, owned a healthcare card, resided in metropolitan locations, usually visited a dentist because of a problem, did not brush their teeth the previous day, rated their oral health as fair or poor and rated their general health as fair or poor.
Table 1.
Baseline and follow-up/lost to follow-up characteristics at child age 2 years, 3 years and 5 years
| Baseline (pregnancy) (n=448) |
Child age 2 years follow-up (n=324) |
Child age 2 years lost to follow-up (n=112) |
Child age 3 years follow-up (n=324) |
Child age 3 years lost to follow-up (n=112) |
Child age 5 years follow-up (n=299) |
Child age 5 years lost to follow-up (n=137) |
|
| Maternal age | |||||||
| 14–24 | 238 (53.1) | 172 (53.1) | 66 (53.2) | 173 (53.2) | 59 (52.7) | 156 (52.2) | 76 (55.5) |
| 25+ | 210 (46.9) | 152 (46.9) | 58 (46.8) | 152 (46.8) | 53 (47.3) | 143 (47.8) | 61 (44.5) |
| Education | |||||||
| High school or less | 322 (72.4) | 226 (70.0) | 88 (79.3) | 232 (72.1) | 82 (73.2) | 203 (68.4) | 111 (81.0) |
| Trade or University | 123 (27.6) | 97 (30.0) | 23 (20.7) | 90 (28.0) | 30 (26.8) | 94 (31.7) | 26 (19.0) |
| Income | |||||||
| Job | 62 (14.0) | 56 (17.34) | 4 (3.7) | 55 (17.1) | 5 (4.5) | 47 (15.9) | 13 (9.6) |
| Centrelink | 381 (86.0) | 267 (82.7) | 105 (96.3) | 267 (82.9) | 106 (95.5) | 249 (84.1) | 123 (90.4) |
| HCC status | |||||||
| Yes | 358 (82.2) | 254 (79.9) | 95 (89.6) | 252 (79.3) | 97 (91.5) | 236 (80.8) | 113 (85.6) |
| No | 77 (17.8) | 64 (20.1) | 11 (10.4) | 66 (20.8) | 9 (8.5) | 56 (19.2) | 19 (14.4) |
| Residential location | |||||||
| Metropolitan | 171 (38.7) | 116 (36.3) | 55 (45.1) | 116 (36.1) | 51 (46.0) | 132 (44.8) | 35 (25.7) |
| Non- metropolitan | 271 (61.3) | 204 (63.8) | 67 (54.9) | 205 (63.9) | 60 (54.1) | 163 (55.2) | 101 (74.3) |
| Usual reason visit dentist | |||||||
| Problem | 275 (64.0) | 195 (61.9) | 72 (69.2) | 194 (62.4) | 74 (67.9) | 184 (63.7) | 83 (63.8) |
| Check-up | 155 (36.1) | 120 (38.1) | 32 (30.8) | 117 (37.6) | 35 (32.1) | 105 (36.3) | 47 (36.2) |
| Brush yesterday | |||||||
| Yes | 321 (75.0) | 239 (76.0) | 74 (69.8) | 240 (77.4) | 74 (67.9) | 217 (75.9) | 96 (72.7) |
| No | 107 (25.0) | 73 (23.4) | 32 (30.2) | 70 (22.6) | 35 (32.1) | 69 (24.1) | 36 (27.3) |
| Self-rated oral health | |||||||
| Excellent, very good or good | 203 (45.3) | 153 (47.2) | 43 (38.4) | 151 (46.5) | 46 (41.1) | 130 (43.5) | 66 (48.2) |
| Fair or poor | 245 (54.7) | 171 (52.8) | 69 (61.6) | 174 (53.5) | 66 (58.9) | 169 (56.5) | 71 (51.8) |
| Self-rated general health | |||||||
| Excellent, very good or good | 402 (89.9) | 294 (91.0) | 97 (86.6) | 298 (92.0) | 94 (83.9) | 272 (91.0) | 119 (87.5) |
| Fair or poor | 45 (10.1) | 29 (9.0) | 15 (13.4) | 26 (8.0) | 18 (16.1) | 27 (9.0) | 17 (12.5) |
What has been measured?
Broad categories of variables collected at baseline and each follow-up phase are provided in table 2, with more detail of these variables provided in table 3. Most items have been based on those used in other national surveys of child health in Australia, for example, the Longitudinal Study of Indigenous Children and the National Child Oral Health Survey. Data linkage to government repositories has been approved and is currently underway, with participant consent. Details of the government linkage datasets are provided in table 4. Self-report questionnaires were completed with the assistance of trained research officers if required. Dental examinations were standardised and conducted by three calibrated dental professionals. Procedures appropriate for young children were used when children were aged 2 years and 3 years, for example, in the 'knee-to-knee' position on their carer’s lap. Before examinations, teeth were dried with cotton pads. Standard infection control procedures were followed and a fibre-optic light used as a light source. Diagnosis was based on visual criteria only. Any child diagnosed with carious lesions was referred for dental care through the SADS (provided free of charge). Weight was measured in duplicate to the nearest 0.1 kg using Seca model 803 scales and averaged. If measures differed by >0.2 kg, a third measure was taken and the average of the two closest values used in analyses. Height was measured in duplicate to the nearest 1 mm using a Seca model 213 portable stadiometer, using a standard anthropometric procedure. If measures differed by >5 mm a third measurement was taken and the average of the closest two used in analyses. Blood pressure was measured using a portable oscillometric device (Omron HEM-7211) and a cuff selected to suit the child’s midupper arm circumference using a standard protocol.
Table 2.
Broad categories of variables collected at baseline and each follow-up phase
| Phase | Measurements |
| Baseline | Mother self-reported questionnaire
|
| Child mean age 2 years | Carer self-reported questionnaire
Child height, weight, blood pressure, upper arm circumference Child dental examination |
| Child mean age 3 years | Carer self-reported questionnaire
Child height, weight, blood pressure, upper arm circumference Child dental examination |
| Child mean age 5 years | Carer self-reported questionnaire
Child height, weight, blood pressure, upper arm circumference Child dental examination |
| Child mean age 7 years | Carer self-reported questionnaire
Child height, weight, blood pressure, upper arm circumference Child dental examination |
Table 3.
Details of variables collected at baseline and each follow-up phase
| Baseline (pregnancy, n=449) | 2 years (n=324) | 3 years (n=324) | 5 years (n=299) | 7 years (ongoing) |
|
| Oral health-related variables | |||||
| Dental examinations (child dental caries, gingivitis, trauma) | ✓ | ✓ | ✓ | ✓ | |
| Dental treatment needs (mother and child) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Oral health-related behaviours (oral hygiene habits) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Oral health self-efficacy (mother) | ✓ | ✓ | ✓ | ✓ | |
| Oral health literacy (mother) | ✓ | ✓ | ✓ | ||
| Knowledge of children’s oral health (mother) | ✓ | ✓ | ✓ | ✓ | |
| Oral health fatalism (mother and child) | ✓ | ✓ | ✓ | ✓ | |
| Dental perceptions | ✓ | ||||
| Oral health-related quality of life (mother and child) | ✓ | ✓ | ✓ | ✓ | ✓ |
| General health | |||||
| Anthropometric measurements (height weight, arm circumference, blood pressure) (child) | ✓ | ✓ | ✓ | ✓ | |
| General health conditions and hospitalisations (child) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Health-related behaviours (smoking, alcohol intake) (mother) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Physical activity (child) | ✓ | ✓ | |||
| Self-rated general and oral health (mother and child) | ✓ | ✓ | ✓ | ✓ | ✓ |
| 24-hour dietary recalls (child) | ✓ | ||||
| Breastfeeding habits (child) | ✓ | ||||
| Other dietary-related habits (mother and child) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Socioeconomic and psychosocial factors | |||||
| Income, education, socioeconomic hardship, employment (mother) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Experience of racism (mother) | ✓ | ✓ | ✓ | ||
| Cultural identity (mother) | ✓ | ✓ | |||
| Self-stem (child) | ✓ | ||||
| Social support and sense of self-control (mother) | ✓ | ||||
| Family functioning and home environment | |||||
| Parental functioning and home environment (mother and child) | ✓ | ✓ | ✓ | ||
| Time-use diaries (child) | ✓ | ||||
| Child development | |||||
| Cognitive outcomes (child) | ✓ | ✓ | |||
| Social and emotional well-being (child) | ✓ | ✓ | |||
Table 4.
Datasets to be included in data linkage
| Database domain | Types of information |
| Hospital admissions | Length of stay, ICD codes describing each hospitalisation event |
| Presentations at hospital emergency departments | Presenting problem, diagnosis |
| Well-child health checks | Child growth and development collected by nurses at routine health checks and ad hoc visits to local health clinics |
| Perinatal information | Medical information about pregnancy and child’s birth |
| Public dental care | Dental treatments received by child in public dental clinics |
| School enrolment | Information provided by carers at the time the child was enrolled at school including carer education, languages spoken at home and school absences |
| Literacy and numeracy | Results on reading, writing and numeracy collected from a national assessment programme when child is in year 3 (approximate age 8) at school |
| Housing | Information about families living in homes provided by the government |
ICD, International Classification of Diseases.
Patient and public involvement
The study’s Aboriginal Reference Group has been involved in the design, governance and general oversight of all phases of the research to date.
Study participants have been encouraged to communicate to the research team through Facebook and other social media platforms. Newsletters and community presentations are frequently shared with participants and relevant key stakeholder groups. Members of the study’s Aboriginal Reference Group have presented the study findings at international conferences.
Findings to date
The prevalence of mothers who were pregnant with their first child at baseline was 38.5%. Rates of dental disease among Aboriginal children in South Australia were less among those exposed to the intervention earlier rather than later in childhood.24 25 The effect appeared to be sustained at age 5 years, although the rates of dental disease were still far higher than estimates reported in Australia’s National Child Oral Health Survey 2012–2014.26 Rates of psychosocial stress among mothers pregnant with Aboriginal children were high compared with general Australian population estimates.27 Experiences of racism were high among mothers, with impacts on tooth brushing behaviours28 and experience of toothache.29 Compared with population estimates, levels of self-efficacy and self-rated oral health of study participants at baseline were low,30 with differences in the frame of reference regarding participants’ self-rated oral health and self-rated general health described.31 Smithers and colleagues reported that the proportion of total energy from discretionary foods (including sugars in discretionary foods) was far higher for study children at age 3 years than for non-Aboriginal Australian children.32 Haag and others described how breast feeding >24 months was associated with higher dental caries prevalence at child age 3 years compared with children who were never breast fed.33 This is contrary to the many findings that support prolonged breast feeding among Indigenous Australians for better child health outcomes. Santiago and colleagues demonstrated how social support was characterised among study participants,34 and the impact of personal control on self-reported health outcomes.35 The effectiveness of implementing a MI approach to preventing poor oral health among Indigenous children and their families was discussed,22 with comparisons made with other studies involving MI and the oral health of vulnerable children.36
Strengths and limitations
The main strength of the study is the Aboriginal community engagement, involvement and partnership, orchestrated through the study’s Aboriginal Reference Group, through the Aboriginal Community Controlled Health Organisation stakeholder groups and by the Senior Aboriginal research officer (JH). This has, without doubt, contributed to the excellent follow-up rates, which need to be taken into context. For example, this cohort study has been undertaken over vast distances (eg, travelling 700 km to the west of South Australia, 400 km east, 800 km north), involving highly disadvantaged participants who have not always enjoyed positive research interactions. The fact that participants represented two-thirds of those eligible to be recruited during the recruitment period demonstrates the widespread community support and generalisability of the results. The main limitation is the small sample size, which was essentially limited by the small population size of Aboriginal people in South Australia (around 2% of the total population). That we were able to recruit two-thirds of those who were eligible at baseline (and have had strong retention of participants since) suggests that had the target population size been larger at baseline, the sample size of our study would consequently also be larger. Participants reported that the dietary recalls (collected at child age 2 years) were burdensome and this may have increased non-response or socially desirable responses. At the time of writing, follow-up at age 7 years was suspended due to social distancing restrictions necessitated by the COVID-19 pandemic. This may impact our age 9 years follow-up also.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge the support of the South Australian Aboriginal Birth Cohort study participants, study staff and partners: South Australian Dental Service, Colgate Palmolive, Women’s and Children’s Hospital, Lyell McEwen Hospital, Flinders’ Medical Centre, Aboriginal Family Support Services, Aboriginal Primary Health Unit, Metro Aboriginal Family Birthing Programme, Kura Yerlo Centre, Aboriginal Legal Rights Movement, Wodlitinattoai Programme, Ninko Kutangga Patpangga, Kanggawodli Step Down Service, Kaurna Plains, Fleurieu Families, Gilles Plains Community Health, MADEC Community Support Services, Naporendi Aboriginal Forum, Nunga MiMinar, Aboriginal Strategy Unit of Families South Australia, Inbarendi College, Para West Adult Campus, Pangula Mannanurna Aboriginal Health Corporation and the Muno Parra Medical Centre, Second Story, Inner Southern Health Service, The Corner House, Louise Place, PARKS, Talking Realities Programme, Child Youth Women’s Health Services, Southern Junction Community Services, TAFE campuses, GP Plus centres, employment programmes, childcare centres, women’s centres, domestic violence shelters and primary and high schools.
Footnotes
Collaborators: Proposals for possible collaborations in further analyses of the data should be addressed to Lisa Jamieson (lisa.jamieson@adelaide.edu.au) and will be reviewed by the SAABC research team and Aboriginal Reference Group.
Contributors: LMJ, JH, XJ, KK, CL, DGH, PRS, DMM, RMR and LGS helped in study conceptualisation. Methodology was done by XJ, DGH, LGS and LMJ. Resources were obtained by LMJ. Data curation was performed by LMJ, JH, XJ, KK, CL, DGH, PRS, DMM, RMR and LGS. Writing and original draft preparation was done by LMJ. Writing and review and editing along with visualisation were performed by JH, XJ, KK, CL, DGH, PRS, DMM, RMR and LGS. All authors have read and agreed to the published version of the manuscript.
Funding: This study was funded by the National Health and Medical Research Council of Australia (NHMRC, Project Grants 627350 and 1153662) and a Channel 7 Children’s Research Foundation grant (10547012). LMJ is supported by a NHMRC Senior Research Fellowship.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. Study data are not freely available because of ethical and data protection constraints. The deidentified data are stored at the University of Adelaide and cannot be sent outside the institution. Proposals for possible collaborations in further analyses of the data should be addressed to Lisa Jamieson (lisa.jamieson@adelaide.edu.au)
References
- 1.Peres MA, Macpherson LMD, Weyant RJ, et al. Oral diseases: a global public health challenge. Lancet 2019;394:249–60. 10.1016/S0140-6736(19)31146-8 [DOI] [PubMed] [Google Scholar]
- 2.Isaksson H, Alm A, Koch G, et al. Caries prevalence in Swedish 20-year-olds in relation to their previous caries experience. Caries Res 2013;47:234–42. 10.1159/000346131 [DOI] [PubMed] [Google Scholar]
- 3.Jamieson LM, Armfield JM, Roberts-Thomson KF. Oral health inequalities among indigenous and nonindigenous children in the Northern Territory of Australia. Community Dent Oral Epidemiol 2006;34:267–76. 10.1111/j.1600-0528.2006.00277.x [DOI] [PubMed] [Google Scholar]
- 4.LG D, Spencer AJ. Oral health of Australian children: the National child oral health study 2012–14. Adelaide: University of Adelaide Press, 2016. [Google Scholar]
- 5.Australian Institute of Health and Welfare Oral health and dental care in Australia: key facts and figures trends 2014. Canberra: AIHW, 2014. [Google Scholar]
- 6.Tahmassebi JF, Achol LT, Fayle SA. Analysis of dental care of children receiving comprehensive care under general anaesthesia at a teaching hospital in England. Eur Arch Paediatr Dent 2014;15:353–60. 10.1007/s40368-014-0123-2 [DOI] [PubMed] [Google Scholar]
- 7.Alsharif AT, Kruger E, Tennant M. A population-based cost description study of oral treatment of hospitalized Western Australian children aged younger than 15 years. J Public Health Dent 2015;75:202–9. 10.1111/jphd.12088 [DOI] [PubMed] [Google Scholar]
- 8.Lee HH, Milgrom P, Starks H, et al. Trends in death associated with pediatric dental sedation and general anesthesia. Paediatr Anaesth 2013;23:741–6. 10.1111/pan.12210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ing C, DiMaggio C, Whitehouse A, et al. Long-term differences in language and cognitive function after childhood exposure to anesthesia. Pediatrics 2012;130:e476–85. 10.1542/peds.2011-3822 [DOI] [PubMed] [Google Scholar]
- 10.Haysom L, Williams R, Hodson EM, et al. Natural history of chronic kidney disease in Australian Indigenous and non-Indigenous children: a 4-year population-based follow-up study. Med J Aust 2009;190:303–6. 10.5694/j.1326-5377.2009.tb02417.x [DOI] [PubMed] [Google Scholar]
- 11.Blair EM, Zubrick SR, Cox AH, et al. The Western Australian Aboriginal child health survey: findings to date on adolescents. Med J Aust 2005;183:433–5. 10.5694/j.1326-5377.2005.tb07112.x [DOI] [PubMed] [Google Scholar]
- 12.Heath DL, Panaretto KS. Nutrition status of primary school children in Townsville. Aust J Rural Health 2005;13:282–9. 10.1111/j.1440-1584.2005.00718.x [DOI] [PubMed] [Google Scholar]
- 13.Zubrick SR, Lawrence DM, Silburn SR. The Western Australian Aboriginal child health survey: the health of Aboriginal children and young people. Perth: Telethon Institute for Child Health Research, 2004. [Google Scholar]
- 14.Victora CG, Adair L, Fall C, et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet 2008;371:340–57. 10.1016/S0140-6736(07)61692-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ekelund U, Ong KK, Linné Y, et al. Association of weight gain in infancy and early childhood with metabolic risk in young adults. J Clin Endocrinol Metab 2007;92:98–103. 10.1210/jc.2006-1071 [DOI] [PubMed] [Google Scholar]
- 16.Barker DJP, Osmond C, Forsén TJ, et al. Trajectories of growth among children who have coronary events as adults. N Engl J Med 2005;353:1802–9. 10.1056/NEJMoa044160 [DOI] [PubMed] [Google Scholar]
- 17.Osmond C, Kajantie E, Forsén TJ, et al. Infant growth and stroke in adult life: the Helsinki birth cohort study. Stroke 2007;38:264–70. 10.1161/01.STR.0000254471.72186.03 [DOI] [PubMed] [Google Scholar]
- 18.Australian Government Department of Education Australian early development census national report 2018. Canberra: Australian Government Department of Education, 2019. [Google Scholar]
- 19.Merrick J, Chong A, Parker E, et al. Reducing disease burden and health inequalities arising from chronic disease among Indigenous children: an early childhood caries intervention. BMC Public Health 2012;12:323. 10.1186/1471-2458-12-323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Slade GD, Bailie RS, Roberts-Thomson K, et al. Effect of health promotion and fluoride varnish on dental caries among Australian Aboriginal children: results from a community-randomized controlled trial. Community Dent Oral Epidemiol 2011;39:29–43. 10.1111/j.1600-0528.2010.00561.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Venner KL, Feldstein SW, Tafoya N. Native American motivational interviewing: weaving native American and western practices. Albuquerque: University of New Mexico, Center on Alcoholism, Substance Abuse and Addictions, Department of Psychology, 2006. [Google Scholar]
- 22.Jamieson L, Bradshaw J, Lawrence H, et al. Fidelity of motivational interviewing in an early childhood caries intervention involving Indigenous Australian mothers. J Health Care Poor Underserved 2016;27:125–38. 10.1353/hpu.2016.0036 [DOI] [PubMed] [Google Scholar]
- 23.Government of South Australia Pregnancy outcome in South Australia 2011. Adelaide: Government of South Australia, 2013. [Google Scholar]
- 24.Jamieson L, Smithers L, Hedges J, et al. Dental disease outcomes following a 2-year oral health promotion program for Australian Aboriginal children and their families: a 2-Arm parallel, single-blind, randomised controlled trial. EClinicalMedicine 2018;1:43–50. 10.1016/j.eclinm.2018.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jamieson LM, Smithers LG, Hedges J, et al. Follow-Up of an intervention to reduce dental caries in Indigenous Australian children: a secondary analysis of a randomized clinical trial. JAMA Netw Open 2019;2:e190648. 10.1001/jamanetworkopen.2019.0648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jamieson L, Smithers L, Hedges J, et al. Follow-Up of intervention to prevent dental caries among Indigenous children in Australia: a secondary analysis of a randomized clinical trial. JAMA Netw Open 2019;2:e1915611. 10.1001/jamanetworkopen.2019.15611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Santiago PHR, Roberts R, Smithers LG, et al. Stress beyond coping? A Rasch analysis of the perceived stress scale (PSS-14) in an Aboriginal population. PLoS One 2019;14:e0216333. 10.1371/journal.pone.0216333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ben J, Jamieson LM, Priest N, et al. Experience of racism and tooth brushing among pregnant Aboriginal Australians: exploring psychosocial mediators. Community Dent Health 2014;31:145. [PubMed] [Google Scholar]
- 29.Ben J, Paradies Y, Priest N, et al. Self-reported racism and experience of toothache among pregnant Aboriginal Australians: the role of perceived stress, sense of control, and social support. J Public Health Dent 2014;74:301–9. 10.1111/jphd.12059 [DOI] [PubMed] [Google Scholar]
- 30.Jamieson LM, Parker EJ, Roberts-Thomson KF, et al. Self-efficacy and self-rated oral health among pregnant aboriginal Australian women. BMC Oral Health 2014;14:29. 10.1186/1472-6831-14-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chand R, Parker E, Jamieson L. Differences in, and frames of reference of, Indigenous Australians' self-rated general and oral health. J Health Care Poor Underserved 2017;28:1087–103. 10.1353/hpu.2017.0099 [DOI] [PubMed] [Google Scholar]
- 32.Smithers LG, Lynch J, Hedges J, et al. Diet and anthropometry at 2 years of age following an oral health promotion programme for Australian Aboriginal children and their carers: a randomised controlled trial. Br J Nutr 2017;118:1061–9. 10.1017/S000711451700318X [DOI] [PubMed] [Google Scholar]
- 33.Haag DG, Jamieson LM, Hedges J, et al. Is there an association between breastfeeding and dental caries among three-year-old Australian Aboriginal children? Nutrients 2019;11:2811. 10.3390/nu11112811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Santiago PHR, Roberts R, Smithers LG. Networks of support: psychometric properties of the social support scale (SSS) in two Aboriginal samples. Australian and New Zealand Journal of Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Santiago PHR, Nielsen T, Roberts R, et al. Sense of personal control: can it be assessed culturally unbiased across Aboriginal and non-Aboriginal Australians? PLoS One 2020;15:e0239384. 10.1371/journal.pone.0239384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jamieson LM, Garcia RI, Sohn W, et al. Challenges and solutions for improved oral health: examples from motivational interviewing trials. JDR Clin Trans Res 2020;5:107–8. 10.1177/2380084419894575 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


