Abstract
Introduction
Predialysis education for patients with advanced chronic kidney disease (CKD) typically focuses narrowly on haemodialysis and peritoneal dialysis as future treatment options. However, patients who are older or seriously ill may not want to pursue dialysis and/or may not benefit from this treatment. Conservative kidney management, a reasonable alternative treatment, and advance care planning (ACP) are often left out of patient education and shared decision-making. In this study, we will pilot an educational intervention (Conservative Kidney Management Options and Advance Care Planning Education—COPE) to improve knowledge of conservative kidney management and ACP among patients with advanced CKD who are older and/or have poor functional status.
Methods and analysis
This is a single-centre pilot randomised controlled trial at an academic centre in Philadelphia, PA. Eligible patients will have: age ≥70 years and/or poor functional status (as defined by Karnofsky Performance Index Score <70), advanced CKD (estimated glomerular filtration rate<20 mL/min/1.73 m2), prefer to speak English during clinical encounters and self-report as black or white race. Enrolled patients will be randomised 1:1, with stratification by race, to receive enhanced usual care or usual care and in-person education about conservative kidney management and ACP (COPE). The primary outcome is change in knowledge of CKM and ACP. We will also explore intervention feasibility and acceptability, change in communication of preferences and differences in the intervention’s effects on knowledge and communication of preferences by race. We will assess outcomes at baseline, immediately post-education and at 2 and 12 weeks.
Ethics and dissemination
This protocol has been approved by the Institutional Review Board at the University of Pennsylvania. We will obtain written informed consent from all participants. The results from this work will be presented at academic conferences and disseminated through peer-reviewed journals.
Trial registration number
This trial is registered at ClinicalTrials.gov under NCT03229811.
Keywords: chronic renal failure, end stage renal failure, adult palliative care, geriatric medicine
Strengths and limitations of this study.
This is a pilot randomised controlled trial evaluating an intervention designed to primarily educate older and seriously ill patients with advanced chronic kidney disease (CKD) about conservative kidney management and advance care planning.
Patients will receive an educational intervention that is integrated into their advanced CKD care.
This study will investigate racial disparities between black and white patients in knowledge about conservative kidney management and advance care planning.
As this study is being conducted at a single-centre and is being limited to black and white patients, we are unable to generalise study results to different regions or patients of different races or ethnicities.
Introduction
The benefits of dialysis remain uncertain for older and seriously ill patients with advanced chronic kidney disease (CKD). In the USA, over 720 000 individuals have kidney failure with > 80% of these patients ultimately receiving haemodialysis.1 For older and frail patients with advanced CKD, it is unclear whether dialysis improves health or survival, with some evidence to suggest that it can negatively impact quality of life and functional status.2–9 Additionally, patients of all ages with CKD have a higher prevalence of frailty and poor functional status, which is an independent risk factor for mortality and increased hospitalisations.3 5 7 10 11
Conservative kidney management is an approach to care for patients with kidney failure who do not want to pursue dialysis or who are unlikely to benefit from this treatment, especially those who are older with functional limitations.6–9 This is nondialytic therapy that focuses on slowing the progression of kidney disease with medications and fosters a multidisciplinary approach to address care needs and emotional and physical symptoms associated with kidney failure; however, many care models of conservative kidney management have been developed outside of the USA, and implementation strategies have not been investigated in this country.8 12–14
Patients with advanced CKD who are managed with conservative kidney management are more likely to receive palliative care consultation, use hospice and discuss goals of care.14 15 Advance care planning (ACP) is a process in which clinicians elicit and document patients’ values and desired goals of care as their health deteriorates and/or if they were to become incapacitated.16–22 Among seriously ill patients, early discussions about advanced care preferences improves patients’ understanding of their health status and facilitates more informed ACP and decision-making.23–26 Specifically, studies have demonstrated that as for other seriously ill patient populations, patients with advanced CKD would prefer to have ACP and goals of care discussions earlier in the disease course.19 27 However, these conversations are often challenging and available evidence suggests that nephrologists tend not to engage in ACP with their patients.19 27–30 Additionally, some studies have shown racial disparities in ACP knowledge, and that racial and ethnic minority patients are less likely to engage in goals of care discussions and ACP when compared with white patients.16 18 31 32 Education and improving informed decision-making may mitigate racial disparities in care for older patients with CKD.18 33 Thus, we are testing whether a novel educational intervention incorporated into routine advanced CKD care, called Conservative Kidney Management Options and Advance Care Planning Education (COPE), can improve knowledge and communication among patients who are older and/or with poor functional status.
Methodology and analysis
Conceptual framework
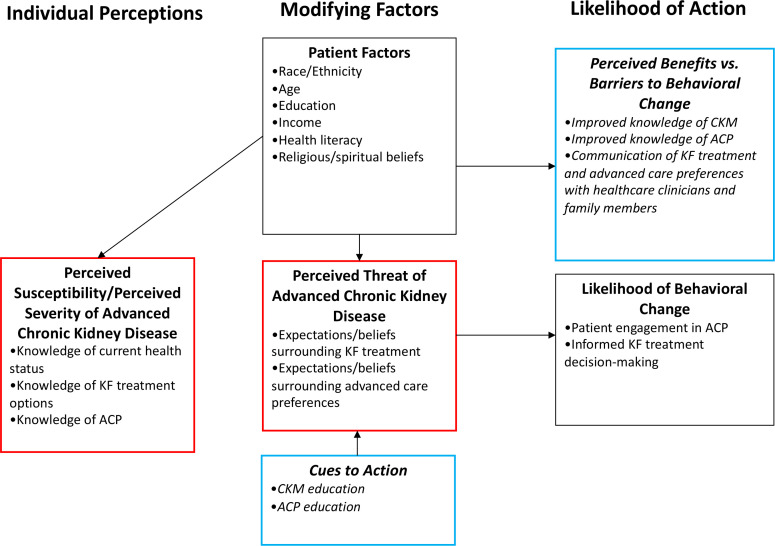
The COPE intervention was developed to address patient knowledge, expectations and beliefs about kidney failure treatments and ACP (figure 1). The conceptual framework for this intervention is adapted from the Health Belief Model (figure 1).34 This model hypothesises that health-related action depends on the simultaneous occurrence of three factors: (1) the existence of sufficient motivation to make health issues salient or relevant, (2) the belief that one is susceptible to a serious health problem or sequelae of that illness or condition (e.g., perceived threat) and (3) the belief that following a particular health recommendation would be beneficial in reducing the perceived threat.34 Under this model, patient factors such as age, race, ethnicity and education are posited to be associated with perceived severity (including knowledge of kidney failure treatment and ACP) and the threat of kidney disease (expectations and beliefs surrounding kidney failure treatments and advanced care preferences).
Figure 1.
Health belief model (adapted for COPE). ACP, advance are planning; CKM, conservative kidney management; COPE, Conservative Kidney Management Options and Advance Care Planning Education; KF, kidney failure.
Intervention development
To support the development of the intervention, we conducted a qualitative study among key stakeholders as well as a comprehensive literature review.
Qualitative study
We conducted in-depth interviews with clinicians (nephrologists and primary care physicians), older patients and their caregivers at an academic medical centre in Boston, Massachusetts.35 Specifically, we assessed interviewees’ prior experiences with discussions about kidney replacement therapies and ACP. We found that nephrologists and primary care physicians were mostly aligned with respect to their roles in discussing dialysis and ACP. However, despite clarity about responsibilities and communication among nephrologists and primary care physicians, patients and their caregivers were uncertain about the impact of dialysis on their lives as well as the importance of ACP. In developing interventional educational materials for the trial, we included key concepts about conservative kidney management and ACP that were most unclear to patients and caregivers based on what we learnt in semistructured interviews.
Educational materials
We also performed a literature review of published studies describing patient education and detailing programmes that implemented conservative kidney management and ACP for patients with advanced CKD. We subsequently developed a brief eight-page brochure and educational script based on existing materials and modified them after receiving input from patients with advanced CKD and their caregivers. The brochure was specifically created at a sixth-grade reading level to maximise understanding for patients.36
Intervention training
The principal investigator trained a nurse practitioner who has experience with serious illness communication and palliative care to deliver the intervention among all enrolled patients. Specifically, the nurse practitioner is trained to discuss all treatment options (including conservative kidney management) and ACP. We conducted this training during several hour-long sessions followed by observed interactions with volunteer patients to determine competency in delivery of information.
Study design and setting
We will test the COPE intervention to provide education to patients with advanced CKD who are older and/or with poor functional status (defined as a Karnofsky Performance Index Score <7011 in a single-centre pilot randomised controlled trial (RCT). The objective of this intervention is to increase participants’ knowledge of treatment options including conservative kidney management and ACP and improve communication of patients’ treatment and care preferences with their clinicians and family members. We hypothesise that educating patients about treatment options, eliciting their treatment preferences and communicating these with clinicians and families will promote patient engagement in ACP, improve informed treatment decision-making, and reduce racial disparities in knowledge and communication of care preferences. We will recruit patients from outpatient renal clinics associated with the University of Pennsylvania Perelman School of Medicine in Philadelphia, PA. The Institutional Review Board at the University of Pennsylvania has approved this study.
Participants
Those eligible to participate in this trial will be (1) age ≥70 years and/or have poor functional status (defined as a Karnofsky Performance Index Score <70,11 (2) have advanced CKD defined as having at least two estimated glomerular filtration measurements <20 mL/min/1.73 m2 separated by at least 3 months,37 (3) prefer to speak English during clinical encounters and (4) self-report as black or white race. Exclusion criteria include being listed for kidney transplant, being legally blind or screening positive for severe cognitive dysfunction defined as having eight or more errors on the Short Portable Mental Status Questionnaire for assessment of organic brain deficit.38 For potentially eligible patients <70 years of age, we will ask treating clinicians to complete a Karnofsky Performance Index Score.
Recruitment
Research staff will access electronic medical records of scheduled clinic patients and nephrologists’ list of patients with poor functional status to identify potential study participants. Prior to approaching patients to invite them to participate in the study, a study coordinator will also confirm study suitability with each patient’s nephrologist. Given the diverse patient demographics in the outpatient renal clinics, we anticipate equal representation of black and white patients.
Study procedures
Prior to the initiation of the pilot RCT, we will assess the feasibility and acceptability of COPE among a small sample of patients (n=10). Immediately after receiving education, patients will be asked to rate satisfaction on a Likert scale and usefulness based on the modified Yorkshire Dialysis Decision Aid (YoDDA) usefulness scale.39 We will assess the reasons for refusal and attrition data before finalising recruitment and study procedures.
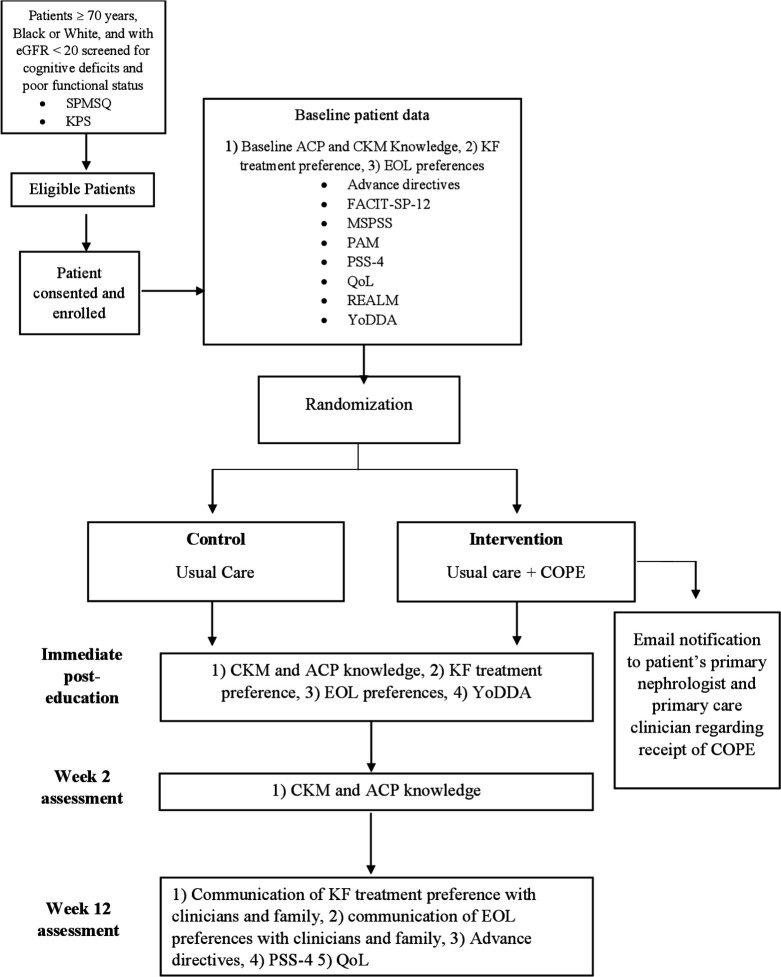
We will randomise patients (n=100) in a 1:1 fashion with stratification by race to receive one of two arms: (1) enhanced usual care or (2) usual care and COPE. We will collect baseline data for patients at the time of enrollment and prior to randomisation (table 1). Further data collection will take place via phone sessions at prespecified time intervals (figure 2).
Table 1.
Demographic, clinical and knowledge outcomes
| Patient demographics | Age, sex, race, ethnicity, marital status, employment status, annual household income, health insurance coverage |
| Knowledge | Conservative kidney management and advance care planning |
| Additional information | Completion of advanced directives, Charlson Comorbidity Index scores, kidney failure treatment preferences, end-of-life preferences |
Figure 2.
Study flow chart. ACP, advance care planning; CKM, conservative kidney management; COPE, Conservative Kidney Management Options and Advance Care Planning Education; EOL, end-of-life;FACIT-SP-12, Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being; KF, kidney failure; KPS, Karnofsky Performance Index Score; MSPSS, Multidimensional Scale of Perceived Social Support; PAM, Patient Activation Measure; PSS-4, Perceived Stress Scale; QOL, McGill Quality of Life Questionnaire-Part A; REALM, Rapid Estimate of Adult Literacy in Medicine; SPMSQ, Short Portable Mental Status Questionnaire; YoDDA, Modified Yorkshire Dialysis Decision Aid.
Enhanced usual care
Nephrology care within the University of Pennsylvania system includes monthly predialysis educational classes where patients with advanced CKD can learn more about CKD and treatment options for kidney failure. The treatment options covered in the classes include haemodialysis, peritoneal dialysis and kidney transplantation. Using a PowerPoint presentation, these sessions are provided in-person by nephrology nurse practitioners and typically last around 60 min. Patients’ nephrologists may also provide ad hoc education during routine clinical visits. To ensure all enrolled patients receive similar education about conservative kidney management and ACP, everyone will receive the National Kidney Foundation’s educational pamphlet titled ‘If you choose to not do dialysis’.40 This is a 16-page document that describes the process of not starting dialysis as well as ACP.
Intervention
The study coordinator will schedule an appointment for all enrolled patients to meet with the nurse practitioner to receive the COPE educational intervention within 2–4 weeks of enrollment. The intervention will be a one-time visit with the primary goal of educating patients about treatment options and ACP. Intervention content includes a discussion about disease understanding, dialysis treatments, conservative kidney management, patient goals and values, and ACP (including review of state-specific advance directives). Importantly, patients will learn that conservative kidney management is not abandonment of care. COPE will last approximately 45–60 min. Patients may invite family members and other loved ones to attend the educational sessions although only patient participants will complete survey items. After completion of COPE, the study principal investigator will communicate with the patient’s primary care physician and primary nephrologist via joint standardised e-mails to notify them of their patient’s enrollment in the study. All sessions will be audiotaped and two recordings will be randomly selected at 2-month intervals to assess the fidelity of the intervention. A study coordinator will complete the fidelity checklist and retraining of the nurse practitioner will occur if 80% of criteria are not met.
Outcomes
The primary outcome for this intervention is change in knowledge of conservative kidney management and ACP. Additional outcomes include assessing the feasibility and acceptability of COPE, and patient communication of kidney failure and advanced care treatment preferences with clinicians and family members. We will also evaluate racial disparities in conservative kidney management, ACP knowledge and communication of care preferences. We will ascertain knowledge, treatment preferences, communication of preferences and intervention acceptability via short questionnaires at the time points displayed in figure 2. Specifically, we will use questions from the SUPPORT trial to assess end-of-life (EOL) preferences.41
We will also measure other outcomes including health literacy,42 perceived mental and physical health status,43 44 spiritual well-being,45 perceived stress46 and quality of life,47 using validated surveys (table 2). Patient demographics, whether patients have completed advance directives, and comorbidities will be ascertained via medical record review and surveys.
Table 2.
Other patient outcomes
| Questionnaire | Items | Domain |
| Cognition Short Portable Mental Status Questionnaire | 10 | Cognition |
| Rapid Estimate of Adult Literacy in Medicine | 66 | Health literacy |
| Perceived Stress Scale | 4 | Perceived stress |
| Multidimensional Scale of Perceived Support | 12 | Social support |
| Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being | 12 | Spiritual well-being |
| Modified Yorkshire Dialysis Decision Aid Usefulness Scale | 4 | Program usefulness |
| Patient Activation Measure | 13 | Patient activation |
| McGill Quality of Life Questionnaire: Part A | 1 | Quality of life |
| Satisfaction of Educational Program | 1 | Program satisfaction |
Analysis
Feasibility and acceptability
We will consider that the intervention has adequate feasibility if at least 70% of eligible patients who are approached provide consent and enroll in the study. Additionally, we will determine that adequate acceptability is achieved if at least 80% of patients have a mean score of ≥4.9 using the modified YoDDA usefulness scale.39
CKM and ACP knowledge, communication and preferences
We will describe patient characteristics using proportions for categorical variables and means (±SD) or medians (IQR) for continuous variables as appropriate. We will test for differences in outcomes between study arms regarding: (1) change in conservative kidney management/ACP knowledge score, (2) kidney failure treatment preference, (3) EOL preference and (4) communication of preferences with clinicians and family members using univariate analyses (two-sample t-test, Wilcoxon rank-sum or χ2 test). Given the possibility of imbalance of baseline characteristics between study arms due to small sample size, we will perform secondary analyses using multivariate linear and logistic regression to measure the independent association of the study arm with all outcomes adjusting for measured patient characteristics (age, sex, race, ethnicity, income level, education level, health literacy and Charleston comorbidity index). We will check for collinearity and interactions between variables and determine significance by a two-sided alpha level of 0.05.
Racial disparities
To determine whether the intervention reduces racial disparities in outcomes between black and white patients, we will add an interaction term between race and study arm in the multivariate analyses. A p value of 0.15 or less will be considered statistically significant when testing for interaction. All analyses will be done in SAS (V.9.4, Cary, North Carolina, USA).
Power and sample size
Based on the published data demonstrating poor knowledge of conservative kidney management among patients with advanced kidney disease,48 we anticipate that recruitment of 50 patients to each arm will provide 85% power to detect an effect size of 0.5 SD when comparing the change in knowledge of conservative kidney management and ACP between the two groups.49 50
Patient and public involvement
We performed a qualitative study among older patients with advanced CKD and their caregivers to learn more about their experiences with dialysisdecision-making and ACP discussions. These data were integral to developing the intervention script and educational brochure. We further piloted the intervention script and brochure among older patients with advanced CKD and their caregivers before modifying and finalising these materials. Prior to initiation of the pilot RCT, we will assess feasibility and acceptability of COPE (including timing and burden of the intervention and survey materials) among older patients with advanced CKD.
Discussion
COPE aims to improve knowledge about conservative kidney management and ACP as well as communication of care preferences for patients with advanced CKD who are older and/or who have poor functional status. Additionally, we expect that the intervention will reduce racial disparities in these outcomes among black and white patients. We anticipate that COPE will ultimately improve informed decision-making about kidney failure treatments and encourage patients to engage in timely ACP discussions with their clinicians and family members.
This pilot RCT is designed to specifically evaluate an educational intervention for patients who are older and/or with poor functional status about conservative kidney management and ACP. Our intervention is informed by qualitative work among patients, caregivers and clinicians and by a comprehensive review of the existing literature. COPE consists of three novel components. First, we are targeting educational efforts towards patients who are older and/or with poor functional status, a group for whom there is often considerable uncertainty about the benefits versus the harms of dialysis. We will use questionnaires to identify knowledge gaps among patients to improve conservative kidney management and ACP education. Second, patients will receive conservative kidney management and ACP education that is integrated with rather than siloed from other aspects of advanced CKD care. Studies focused on dialysis decision-making among patients with CKD are lacking.29 30 51–54 Fully informing patients with advanced CKD of conservative kidney management options as well as discussing their preferences for care at EOL allows patients to focus on values and goals that are most important to them. Third, we aim to reduce racial disparities in knowledge and communication of conservative kidney management and EOL preferences among patients with advanced CKD. Compared with white patients with CKD, black patients have lower health literacy, less knowledge about treatment options for advanced kidney disease and tend to have less access to support resources to cope with disease.55 56 Racial differences in knowledge outcomes may in part be due to the notion that educational interventions are developed to achieve a ‘one size fits all’ standard. However, COPE has been developed with input from a diverse population of patients with CKD and with specific attention to communication style and health literacy barriers. There are few existing ACP and conservative kidney management educational tools that account for knowledge differences among patients, which could ultimately help reduce racial disparities in patients’ understanding of these aspects of care.31 57
There are a few limitations to this study. This is a single-centre study and we will enroll patients who self-identify as white or black. Thus, conclusions may not be generalisable to patients of different racial backgrounds or who live in other geographical locations. In addition, shared decision-making includes patients, clinicians and families, but our study will only measure patient outcomes. Finally, we acknowledge that this study will focus on short-term outcomes and, therefore, we will be unable to comment on the downstream effects of the intervention. Future studies will confirm whether COPE has broad relevance and usefulness for similar patients with different demographics, feasibility and acceptability among clinicians and caregivers, and long-term outcomes such as treatment decision-making confidence and conflict.
Educating patients with advanced CKD who are older or seriously ill about kidney failure treatment options (including conservative kidney management) and ACP is central to promoting shared decision-making and goal-concordant care. We anticipate that our study findings will improve informed decision-making for patients with advanced CKD and create an opportunity for clinicians to provide comprehensive patient-centred care.
Ethics and dissemination
This protocol has been approved by the Institutional Review Board at the University of Pennsylvania. Written informed consent will be obtained from all participants. The findings from this work will be disseminated through peer-reviewed publications and will be presented at academic conferences.
Supplementary Material
Footnotes
Twitter: @annmohare, @AmakaEMD
Contributors: Research idea and study design: NE, JT MP-O, MA, AO'; preparation of manuscript: TS, NE; critical revision of manuscript: TS, JT, TK, MP-O, MA, AO', NO', LD, SDH, NE; supervision or mentorship: NE, JT, LD, SDH. All authors take responsibility for the integrity and accuracy of this manuscript’s content and have approved the final draft for submission.
Funding: This study is supported by grant K23DK114526 (NDE) from the National Institutes of Health.
Disclaimer: The funder did not have a role in the design of the study.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.United States Renal Data System 2018 USRDS annual data report: epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2018. [Google Scholar]
- 2.Kurella M, Covinsky KE, Collins AJ, et al. . Octogenarians and nonagenarians starting dialysis in the United States. Ann Intern Med 2007;146:177–83. 10.7326/0003-4819-146-3-200702060-00006 [DOI] [PubMed] [Google Scholar]
- 3.Kurella Tamura M, Covinsky KE, Chertow GM, et al. . Functional status of elderly adults before and after initiation of dialysis. N Engl J Med 2009;361:1539–47. 10.1056/NEJMoa0904655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weisbord SD, Fried LF, Arnold RM, et al. . Prevalence, severity, and importance of physical and emotional symptoms in chronic hemodialysis patients. J Am Soc Nephrol 2005;16:2487–94. 10.1681/ASN.2005020157 [DOI] [PubMed] [Google Scholar]
- 5.McAdams-DeMarco MA, Law A, Salter ML. Frailty as a novel predictor of mortality and hospitalization in hemodialysis patients of all ages. J Am Geriatr Soc 2013;61:896–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Verberne WR, Geers ABMT, Jellema WT, et al. . Comparative survival among older adults with advanced kidney disease managed conservatively versus with dialysis. Clin J Am Soc Nephrol 2016;11:633–40. 10.2215/CJN.07510715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pugh J, Aggett J, Goodland A, et al. . Frailty and comorbidity are independent predictors of outcome in patients referred for pre-dialysis education. Clin Kidney J 2016;9:324–9. 10.1093/ckj/sfv150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Song M-K Quality of life of patients with advanced chronic kidney disease receiving conservative care without dialysis. Semin Dial 2016;29:165–9. 10.1111/sdi.12472 [DOI] [PubMed] [Google Scholar]
- 9.Da Silva-Gane M, Wellsted D, Greenshields H, et al. . Quality of life and survival in patients with advanced kidney failure managed conservatively or by dialysis. Clin J Am Soc Nephrol 2012;7:2002–9. 10.2215/CJN.01130112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roshanravan B, Khatri M, Robinson-Cohen C, et al. . A prospective study of frailty in nephrology-referred patients with CKD. Am J Kidney Dis 2012;60:912–21. 10.1053/j.ajkd.2012.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schmidt RJ, Landry DL, Cohen L, et al. . Derivation and validation of a prognostic model to predict mortality in patients with advanced chronic kidney disease. Nephrol Dial Transplant 2019;34:1517–25. 10.1093/ndt/gfy305 [DOI] [PubMed] [Google Scholar]
- 12.Morton RL, Snelling P, Webster AC, et al. . Factors influencing patient choice of dialysis versus conservative care to treat end-stage kidney disease. CMAJ 2012;184:E277–83. 10.1503/cmaj.111355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foote C, Morton RL, Jardine M, et al. . Considerations of nephrologists when suggesting dialysis in elderly patients with renal failure (consider): a discrete choice experiment. Nephrol Dial Transplant 2014;29:2302–9. 10.1093/ndt/gfu257 [DOI] [PubMed] [Google Scholar]
- 14.Tonkin-Crine S, Okamoto I, Leydon GM, et al. . Understanding by older patients of dialysis and conservative management for chronic kidney failure. Am J Kidney Dis 2015;65:443–50. 10.1053/j.ajkd.2014.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eneanya ND, Paasche-Orlow MK, Volandes A. Palliative and end-of-life care in nephrology: moving from observations to interventions. Curr Opin Nephrol Hypertens 2017;26:327–34. 10.1097/MNH.0000000000000337 [DOI] [PubMed] [Google Scholar]
- 16.Kurella Tamura M, Goldstein MK, Pérez-Stable EJ. Preferences for dialysis withdrawal and engagement in advance care planning within a diverse sample of dialysis patients. Nephrol Dial Transplant 2010;25:237–42. 10.1093/ndt/gfp430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fried TR, Redding CA, Robbins ML, et al. . Development of personalized health messages to promote engagement in advance care planning. J Am Geriatr Soc 2016;64:359–64. 10.1111/jgs.13934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eneanya ND, Wenger JB, Waite K, et al. . Racial disparities in end-of-life communication and preferences among chronic kidney disease patients. Am J Nephrol 2016;44:46–53. 10.1159/000447097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goff SL, Eneanya ND, Feinberg R, et al. . Advance care planning: a qualitative study of dialysis patients and families. Clin J Am Soc Nephrol 2015;10:390–400. 10.2215/CJN.07490714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sudore RL, Schickedanz AD, Landefeld CS, et al. . Engagement in multiple steps of the advance care planning process: a descriptive study of diverse older adults. J Am Geriatr Soc 2008;56:1006–13. 10.1111/j.1532-5415.2008.01701.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Detering KM, Hancock AD, Reade MC, et al. . The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ 2010;340:c1345. 10.1136/bmj.c1345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Douglas C, Sloan J, Cathcart S. The impact of a renal supportive care service on symptom control, advance care planning and place of death for patients with advanced chronic kidney disease managed without dialysis. BJRM 2019;24:60–5. [Google Scholar]
- 23.Greer JA, Pirl WF, Jackson VA, et al. . Effect of early palliative care on chemotherapy use and end-of-life care in patients with metastatic non-small-cell lung cancer. J Clin Oncol 2012;30:394–400. 10.1200/JCO.2011.35.7996 [DOI] [PubMed] [Google Scholar]
- 24.Temel JS, Greer JA, Admane S, et al. . Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non-small-cell lung cancer: results of a randomized study of early palliative care. J Clin Oncol 2011;29:2319–26. 10.1200/JCO.2010.32.4459 [DOI] [PubMed] [Google Scholar]
- 25.Braddock CH, Edwards KA, Hasenberg NM, et al. . Informed decision making in outpatient practice: time to get back to basics. JAMA 1999;282:2313–20. 10.1001/jama.282.24.2313 [DOI] [PubMed] [Google Scholar]
- 26.Mack JW, Cronin A, Taback N, et al. . End-Of-Life care discussions among patients with advanced cancer: a cohort study. Ann Intern Med 2012;156:204–10. 10.7326/0003-4819-156-3-201202070-00008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Davison SN End-Of-Life care preferences and needs: perceptions of patients with chronic kidney disease. Clin J Am Soc Nephrol 2010;5:195–204. 10.2215/CJN.05960809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moss AH Revised dialysis clinical practice guideline promotes more informed decision-making. Clin J Am Soc Nephrol 2010;5:2380–3. 10.2215/CJN.07170810 [DOI] [PubMed] [Google Scholar]
- 29.Moss AH Ethical principles and processes guiding dialysis decision-making. Clin J Am Soc Nephrol 2011;6:2313–7. 10.2215/CJN.03960411 [DOI] [PubMed] [Google Scholar]
- 30.Kurella Tamura M, Meier DE. Five policies to promote palliative care for patients with ESRD. Clin J Am Soc Nephrol 2013;8:1783–90. 10.2215/CJN.02180213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Song M-K, Ward SE, Lin F-C, et al. . Racial differences in outcomes of an advance care planning intervention for dialysis patients and their surrogates. J Palliat Med 2016;19:134–42. 10.1089/jpm.2015.0232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thomas BA, Rodriguez RA, Boyko EJ, et al. . Geographic variation in black-white differences in end-of-life care for patients with ESRD. Clin J Am Soc Nephrol 2013;8:1171–8. 10.2215/CJN.06780712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eneanya ND, Olaniran K, Xu D, et al. . Health literacy mediates racial disparities in cardiopulmonary resuscitation knowledge among chronic kidney disease patients. J Health Care Poor Underserved 2018;29:1069–82. 10.1353/hpu.2018.0080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q 1988;15:175–83. 10.1177/109019818801500203 [DOI] [PubMed] [Google Scholar]
- 35.Eneanya ND, Labbe AK, Stallings TL, et al. . Caring for older patients with advanced chronic kidney disease and considering their needs: a qualitative study. BMC Nephrol 2020;21:213. 10.1186/s12882-020-01870-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Institute of Medicine (US) Committee on Health Literacy Nielsen-Bohlman L, Panzer AM, Kindig DA, Health literacy: a prescription to end confusion. US: National Academies Press, 2004. http://www.ncbi.nlm.nih.gov/books/NBK216032/ [PubMed] [Google Scholar]
- 37.Levey AS, Bosch JP, Lewis JB, et al. . A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. modification of diet in renal disease Study Group. Ann Intern Med 1999;130:461–70. 10.7326/0003-4819-130-6-199903160-00002 [DOI] [PubMed] [Google Scholar]
- 38.Pfeiffer E A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 1975;23:433–41. 10.1111/j.1532-5415.1975.tb00927.x [DOI] [PubMed] [Google Scholar]
- 39.Winterbottom AE, Gavaruzzi T, Mooney A, et al. . Patient acceptability of the Yorkshire dialysis decision aid (YODDA) booklet: a prospective Non-Randomized comparison study across 6 predialysis services. Perit Dial Int 2016;36:374–81. 10.3747/pdi.2014.00274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.The National Kidney Foundation If you choose not to start dialysis treatment, 2008. Available: https://www.kidney.org/sites/default/files/11-10-0330_ifyouchoose.pdf [Accessed 15 Apr 2020].
- 41.Connors AF, Dawson NV, Desbiens NA. A controlled trial to improve care for seriously ill hospitalized patients. the study to understand prognoses and preferences for outcomes and risks of treatments (support). The support principal Investigators. JAMA 1995;274:1591–8. [PubMed] [Google Scholar]
- 42.Cavanaugh KL, Wingard RL, Hakim RM, et al. . Low health literacy associates with increased mortality in ESRD. J Am Soc Nephrol 2010;21:1979–85. 10.1681/ASN.2009111163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. conceptual framework and item selection. Med Care 1992;30:473–83. [PubMed] [Google Scholar]
- 44.Wight JP, Edwards L, Brazier J, et al. . The SF36 as an outcome measure of services for end stage renal failure. Qual Health Care 1998;7:209–21. 10.1136/qshc.7.4.209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Peterman AH, Fitchett G, Brady MJ, et al. . Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy--Spiritual Well-being Scale (FACIT-Sp). Ann Behav Med 2002;24:49–58. 10.1207/S15324796ABM2401_06 [DOI] [PubMed] [Google Scholar]
- 46.Taylor JM Psychometric analysis of the Ten-Item perceived stress scale. Psychol Assess 2015;27:90–101. 10.1037/a0038100 [DOI] [PubMed] [Google Scholar]
- 47.Cohen SR, Mount BM, Bruera E, et al. . Validity of the McGill quality of life questionnaire in the palliative care setting: a multi-centre Canadian study demonstrating the importance of the existential domain. Palliat Med 1997;11:3–20. 10.1177/026921639701100102 [DOI] [PubMed] [Google Scholar]
- 48.Prakash S, McGrail A, Lewis SA, et al. . Behavioral stage of change and dialysis decision-making. Clin J Am Soc Nephrol 2015;10:197–204. 10.2215/CJN.05560614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care 2003;41:582–92. 10.1097/01.MLR.0000062554.74615.4C [DOI] [PubMed] [Google Scholar]
- 50.Cohen J Statistical power analysis for the behavioral sciences. Taylor and Francis, 2013. http://www.123library.org/book_details/?id=107447 [Google Scholar]
- 51.Saeed F, Adams H, Epstein RM. Matters of life and death: why do older patients choose conservative management? Am J Nephrol 2020;51:35–42. 10.1159/000504692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Saeed F, Sardar M, Rasheed K, et al. . Dialysis decision making and preferences for end-of-life care: perspectives of Pakistani patients receiving maintenance dialysis. J Pain Symptom Manage 2020;60:336–45. 10.1016/j.jpainsymman.2020.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Verberne WR, Konijn WS, Prantl K, et al. . Older patients' experiences with a shared decision-making process on choosing dialysis or conservative care for advanced chronic kidney disease: a survey study. BMC Nephrol 2019;20:264. 10.1186/s12882-019-1423-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Saeed F, Sardar MA, Davison SN, et al. . Patients' perspectives on dialysis decision-making and end-of-life care. Clin Nephrol 2019;91:294–300. 10.5414/CN109608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kazley AS, Johnson E, Simpson K, et al. . African American patient knowledge of kidney disease: a qualitative study of those with advanced chronic kidney disease. Chronic Illn 2015;11:245–55. 10.1177/1742395314556658 [DOI] [PubMed] [Google Scholar]
- 56.Grubbs V, Gregorich SE, Perez-Stable EJ, et al. . Health literacy and access to kidney transplantation. Clin J Am Soc Nephrol 2009;4:195–200. 10.2215/CJN.03290708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Song M-K, Ward SE, Fine JP, et al. . Advance care planning and end-of-life decision making in dialysis: a randomized controlled trial targeting patients and their surrogates. Am J Kidney Dis 2015;66:813–22. 10.1053/j.ajkd.2015.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.