Abstract
We present the case of a 47-year-old woman with neurofibromatosis type 1 (NF1) with subarachnoid haemorrhage (SAH) from the left vertebral arteriovenous fistula, along with a review of previous cases. Our patient had a family history of NF1 and presented to the emergency department with a sudden-onset severe headache and neck pain. CT scan showed SAH. CT angiography revealed a left vertebral arteriovenous fistula and an epidural haematoma. She underwent direct surgery and was discharged without neurologic deficits. To our knowledge, this is the first case of SAH caused by perimedullary drainage of a vertebral arteriovenous fistula associated with NF1. In a literature search, we identified 40 cases of vertebral arteriovenous fistula associated with NF1. The majority of vertebral arteriovenous fistulas occurred on the left side and in women. Patients with vertebral arteriovenous fistula typically experience neck pain, radiculopathy, radiculomyelopathy and bruits.
Keywords: dermatology, general practice / family medicine, coma and raised intracranial pressure, headache (including migraines)
Background
Neurofibromatosis type 1 (NF1), also known as von Recklinghausen disease, is an autosomal dominant genetic disorder with generalised neuroectodermal and mesodermal dysplasia that affects the skin, nervous system, skeleton and vascular system.1 Vascular abnormalities associated with NF1 occur in 0.4%–6.4% of patients and most commonly involve the aorta and renal arteries.2–4 Vertebral arteriovenous fistula related to NF1 is relatively rare; however, its incidence is reportedly increasing. Here, we report a patient with NF1 who presented with subarachnoid haemorrhage (SAH) caused by bleeding from the left vertebral arteriovenous fistula, and review 40 previous cases of vertebral arteriovenous fistula with NF1. To our knowledge, this is the first case of SAH caused by perimedullary drainage of a vertebral arteriovenous fistula associated with NF1.
Case presentation
A 47-year-old woman with a family history of NF1 presented to the emergency department with a sudden-onset severe headache and neck pain. NF1 was diagnosed at the age of 20 years on the basis of pathological examination. She had a medical history of left vertebral arteriovenous fistula and was treated with endovascular treatment (coil embolisation) 8 years prior at another hospital. She was alert and oriented to person, place and time. Physical examination revealed multiple neurofibromas and café-au-lait spots across the trunk (figure 1). She had cervical bruit on the left side and neck stiffness. Other neurological examinations were unremarkable. CT scan showed SAH predominantly in the ambient cistern and the prepontine cistern (figure 2). She was diagnosed with SAH and was transferred to another tertiary emergency hospital with a neurosurgical unit.
Figure 1.
Subcutaneous neurofibroma and diffuse café-au-lait spot on the trunk.
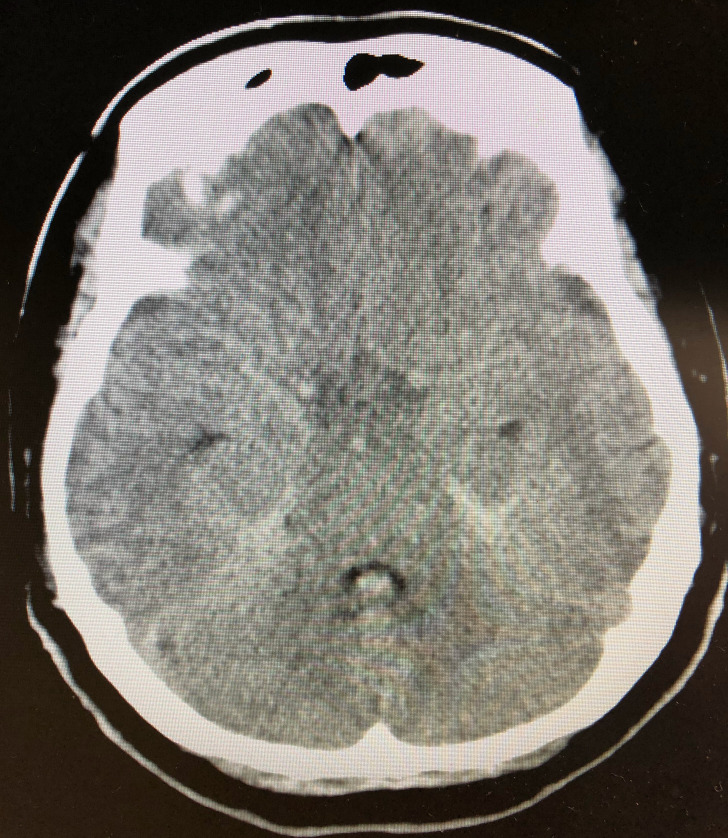
Figure 2.
Subarachnoid haemorrhage in the ambient cistern and the prepontine cistern.
Investigations
CT angiography did not indicate any apparent intracranial aneurysm or any intracranial vascular malformation, but revealed a recurrent left vertebral arteriovenous fistula arising from the left vertebral artery and an epidural haematoma. Angiography demonstrated maintained blood flow through the branches of the left vertebral artery, which had not been completely occluded after coiling, right vertebral artery and left internal carotid artery (figure 3). The fistula point was located at the C2-3 level. The drainage route consisted of the epidural and perimedullary veins. Bleeding appeared to have occurred from the left vertebral arteriovenous fistula with epidural and perimedullary venous drainage. In this case, the incomplete occlusion of the feeder of the previous fistula, which was embolised 8 years prior, resulted in new vertebral arteriovenous fistula, complicating the endovascular treatment. Therefore, she underwent emergent direct surgery to identify the lesion.
Figure 3.

(A) Left vertebral angiogram demonstrated the left vertebral arteriovenous fistula fed by the branches of the left vertebral artery, which had not been completely occluded after coiling. (B) Left carotid angiogram revealed the feeder from left internal carotid artery. (C) Right vertebral angiogram showed the feeder from the right vertebral artery.
Differential diagnosis
The differential diagnosis of non-aneurysmal SAH includes perimesencephalic haemorrhage, intracranial or spinal vascular malformations, intracranial or vertebral arterial dissection and other causes. In this case, the CT findings were not consistent with perimesencephalic haemorrhage. CT angiography did not show any intracranial vascular malformation or any arterial dissection, but revealed a left vertebral arteriovenous fistula. Angiography demonstrated that bleeding appeared to have occurred from the left vertebral arteriovenous fistula. The direct surgery confirmed that in this case, SAH was caused by the bleeding from the left vertebral arteriovenous fistula with epidural and perimedullary venous drainage.
Outcome and follow-up
The patient tolerated the surgical procedure. She was discharged with an uneventful postoperative period. However, she presented with mild memory impairment and was diagnosed with normal pressure hydrocephalus 1 month after discharge. After she was treated with ventriculoperitoneal shunt, she had no neurologic deficits. At the 3-month follow-up, she had no neck pain, radiculopathy, radiculomyelopathy or cervical bruit.
Discussion
NF1 is an autosomal dominant genetic disorder caused by mutations in the NF1 gene on the long arm of chromosome 17.1 These mutations cause dysplastic disorders affecting the vascular system. Patients with NF1 present with a spectrum of vascular lesions ranging from occlusive disease to acute haemorrhage.5
The literature was reviewed using the PubMed database. We identified 40 cases of vertebral arteriovenous fistula associated with NF1 (table 1).5–37 The majority of these cases were reported in Asia. The mean age at diagnosis of the vertebral arteriovenous fistula was 39.8 years. The majority of fistulae occurred on the left side (65%) and in women (75%). Patients with vertebral arteriovenous fistula typically present with neck pain (40%), radiculopathy (30%) and radiculomyelopathy (28%). On physical examination, >50% of the patients experienced cervical bruit. After direct surgery or endovascular coil embolisation, the bruit resolved in all cases of successful treatment.
Table 1.
Literature review of cases of vertebral arteriovenous fistula associated with NF-15–37
| Reference | Country | Age | Sex | Side | Symptoms |
| Su et al6 | China | 33 | Female | Left | Neck pain |
| Maki et al7 | Japan | 59 | NR | Left | Coma |
| Rai et al8 | USA | 39 | Female | Right | Difficulty walking |
| Uneda et al9 | Japan | 35 | Female | Right | Neck pain, shoulder pain, radiculopathy |
| Gao et al10 | China | 24 | Female | Left | Neck pain |
| Gao et al10 | China | 46 | Female | Left | Neck mass, neck pain |
| Hughes and Alleyne 11 | USA | 29 | Female | Left | Difficulty walking, spasticity, neck pain, radiculopathy |
| Takegami et al12 | Japan | 28 | Male | Left | Neck pain, radiculopathy |
| Ng et al13 | Germany | 37 | Male | Left | Radiculopathy, neck pain, numbness |
| Higa et al14 | USA | 60 | Female | Left | Neck pain, swelling, difficulty breathing |
| Patro et al15 | India | 29 | Female | Left | Tinnitus, radiculopathy, radiculomyelopathy, bruit |
| Paolini et al16 | Italy | 26 | Male | Left | Sensory disturbances, weakness of all limbs |
| Guzel et al17 | Turkey | 36 | Male | Right | Arm and leg weakness, arm pain, hoarseness |
| Hauck and Nauta5 | USA | 51 | Female | Left | Tinnitus, radiculomyelopathy, bruit |
| Siddhartha et al18 | India | 36 | Female | Bilateral | Radiculopathy, radiculomyelopathy, neck pain |
| Tanaka et al19 | Japan | 20 | Male | Left | Neck mass |
| Maheshwari et al20 | Canada | 30 | Female | NR | Neck pain, loss of bowel/bladder control, radiculomyelopathy |
| Kāhārā et al21 | Finland | 38 | Male | Right | Neck pain, numbness, muscular weakness |
| Benndorf et al22 | Germany | 59 | Male | Right | Neck mass, neck pain, bruit |
| Hori et al23 | Japan | 41 | Female | Right | Tinnitus, bruit |
| Hori et al23 | Japan | 51 | Female | Left | Bruit, tinnitus |
| Hori et al23 | Japan | 29 | Female | Left | Bruit, radiculopathy |
| Hori et al23 | Japan | 66 | Female | Left | Bruit |
| Hori et al23 | Japan | 51 | Female | Right | Radiculopathy, radiculomyelopathy, bruit |
| Roth et al24 | USA | 36 | Female | Left | Shoulder pain, radiculopathy, radiculomyelopathy, neck mass |
| Ma et al25 | USA | 32 | Female | Left | Radiculomyelopathy, neck pain, loss of bladder control, bruit |
| Sampei et al26 | Japan | 41 | Male | Left | Headache, neck pain |
| Ushikoshi et al27 | Japan | 40 | Female | Left | Bruit, occipitalgia, cervical haematoma |
| Murayama et al28 | Japan | 27 | Female | Right | Bruit, radiculopathy |
| Koenigsberg et al29 | USA | 34 | Female | Right | Neck pain, radiculopathy, difficulty walking, loss of bladder control |
| Anegawa et al30 | Japan | 54 | Female | Left | Radiculomyelopathy, loss of bowel/bladder control |
| Schievink and Piepgras31 | USA | 28 | Female | Right | Bruit, neck swelling |
| Johnson et al32 | USA | 11 | Female | Right | Bruit, tinnitus |
| Wada et al33 | Japan | 24 | Female | Left | Radiculopathy, radiculomyelopathy, bruit |
| Hasegawa et al34 | Japan | 47 | Male | Right | Suboccipital pain, bruit, myelopathy |
| Parkinson and Hay35 | Canada | 54 | Female | Left | Bruit, tinnitus |
| Kamiyama et al36 | Japan | 58 | Female | Left | Bruit, tinnitus |
| Deans et al37 | USA | 53 | Female | Left | Myelopathy, numbness, bruit |
| Deans et al37 | USA | 45 | Female | Left | Bruit, neck pain, shoulder pain |
| Deans et al37 | USA | 58 | Female | Left | Neck pain, neck mass, bruit |
NF-1, neurofibromatosis type 1; NR, not reported.
The clinical symptoms caused by vertebral arteriovenous fistula are variable,5–37 but only one case of SAH related to vertebral arteriovenous fistula in a patient with NF1 has been reported.7 In this previous case, SAH was caused by epidural drainage of the vertebral arteriovenous fistula, but SAH is typically caused by perimedullary drainage of the fistula.38 Maki et al suggested that haemodynamic stress to the epidural drainage system and tissue fragility of the dura due to NF1 could have caused the SAH in their case.7 Our current case is considered to be the first case of SAH caused by perimedullary drainage of an NF1-associated vertebral arteriovenous fistula.
There are two possible mechanisms underlying NF1-associated arteriovenous fistula.33 First, dysplastic smooth muscle in the blood wall might lead to aneurysm formation, leakage and rupture into adjacent veins. Second, arteriovenous malformation could arise congenitally as a mesodermal dysplasia. In our patient, the incomplete occlusion of the feeder of the previous fistula, which was embolised 8 years prior, likely resulted in flow redistribution and abnormal arterial flow. This could have led to mural weakening, leakage perforation and rupture into the adjacent vein, which resulted in the formation of new fistulae.10
Clinicians should consider vertebral arteriovenous fistula and auscultate cervical bruits in patients with NF1, particularly on the left side in female patients. The presence of a cervical bruit in patients with NF1 who present with neurologic symptoms should prompt further vascular imaging.
Patient’s perspective.
Patient’s husband: I am grateful for the help of all doctors at various hospitals. I was surprised to learn that she is at risk of developing a vertebral arteriovenous fistula because of neurofibromatosis type 1. I hope that people around the world will know this fact, which contribute to medicine. I want to trust that nothing will happen to my wife in the future.
Learning points.
Patients with vertebral arteriovenous fistula typically present with neck pain, radiculopathy and radiculomyelopathy.
Clinicians should auscultate the cervical bruits in patients with neurofibromatosis type 1 (NF1), particularly on the left side in female patients.
Vertebral arteriovenous fistula related to NF1 is relatively rare; however, it could cause subarachnoid haemorrhage, as in this case.
Acknowledgments
The authors would like to thank Toyota Kosei Hospital, Toyota, Aichi, Japan, for taking care of the patient and for providing clinical information and images.
Footnotes
Contributors: TN took care of the patient and wrote the report. TN and TT reviewed 40 cases of vertebral arteriovenous fistula associated with neurofibromatosis type 1 in a literature search. YT and YO read and approved the final version of the report.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hirbe AC, Gutmann DH. Neurofibromatosis type 1: a multidisciplinary approach to care. Lancet Neurol 2014;13:834–43. 10.1016/S1474-4422(14)70063-8 [DOI] [PubMed] [Google Scholar]
- 2.Friedman JM, Arbiser J, Epstein JA, et al. Cardiovascular disease in neurofibromatosis 1: report of the NF1 cardiovascular Task force. Genet Med 2002;4:105–11. 10.1097/00125817-200205000-00002 [DOI] [PubMed] [Google Scholar]
- 3.Hamilton SJ, Friedman JM. Insights into the pathogenesis of neurofibromatosis 1 vasculopathy. Clin Genet 2000;58:341–4. 10.1034/j.1399-0004.2000.580501.x [DOI] [PubMed] [Google Scholar]
- 4.Lin AE, Birch PH, Korf BR, et al. Cardiovascular malformations and other cardiovascular abnormalities in neurofibromatosis 1. Am J Med Genet 2000;95:108–17. [DOI] [PubMed] [Google Scholar]
- 5.Hauck EF, Nauta HJW. Spontaneous spinal epidural arteriovenous fistulae in neurofibromatosis type-1. Surg Neurol 2006;66:215–21. 10.1016/j.surneu.2006.01.018 [DOI] [PubMed] [Google Scholar]
- 6.Su X-J, Li Q, Shen H-X. Arteriovenous fistula inside cervical spinal canal associated with neurofibromatosis type 1. World Neurosurg 2019;123:283–5. 10.1016/j.wneu.2018.12.045 [DOI] [PubMed] [Google Scholar]
- 7.Maki Y, Ishibashi R, Fukuda H, et al. Subarachnoid hemorrhage from vertebral arteriovenous fistula without perimedullary drainage: rare stroke hemorrhagic event in a patient of neurofibromatosis type 1. Neurol Med Chir 2018;58:185–8. 10.2176/nmc.cr.2017-0241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rai R, Iwanaga J, Wang B, et al. Atraumatic vertebral arteriovenous fistula: a rare entity with two case reports. World Neurosurg 2018;120:66–71. 10.1016/j.wneu.2018.08.160 [DOI] [PubMed] [Google Scholar]
- 9.Uneda A, Suzuki K, Okubo S, et al. Neurofibromatosis type 1-associated extracranial vertebral artery aneurysm complicated by vertebral arteriovenous fistula after rupture: case report and literature review. World Neurosurg 2016;96:609 10.1016/j.wneu.2016.09.036 [DOI] [PubMed] [Google Scholar]
- 10.Gao P, Chen Y, Zhang H, et al. Vertebral arteriovenous fistulae (AVF) in neurofibromatosis type 1: a report of two cases. Turk Neurosurg 2013;23:289–93. 10.5137/1019-5149.JTN.4993-11.0 [DOI] [PubMed] [Google Scholar]
- 11.Hughes DG, Alleyne CH. Rare giant traumatic cervical arteriovenous fistula in neurofibromatosis type 1 patient. BMJ Case Rep 2012;2012:bcr1220115354. 10.1136/bcr.12.2011.5354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Takegami T, Imai K, Umezawa K, et al. [Endovascular trapping using a tandem balloon technique for a spontaneous vertebrovertebral fistula associated with neurofibromatosis type 1]. No Shinkei Geka 2012;40:705–9. [PubMed] [Google Scholar]
- 13.Ng ES-T, Ong CK, Wilder-Smith E. Neurological picture. traumatic upper limb weakness in a man with type 1 neurofibromatosis. J Neurol Neurosurg Psychiatry 2011;82:883–4. 10.1136/jnnp-2011-300230 [DOI] [PubMed] [Google Scholar]
- 14.Higa G, Pacanowski JP, Jeck DT, et al. Vertebral artery aneurysms and cervical arteriovenous fistulae in patients with neurofibromatosis 1. Vascular 2010;18:166–77. 10.2310/6670.2010.00032 [DOI] [PubMed] [Google Scholar]
- 15.Patro SN, Gupta AK, Arvinda HR, et al. Combined transarterial and percutaneous coiling of a spontaneous vertebrovertebral fistula associated with neurofibromatosis type 1. Case report. J Neurosurg 2009;111:37–40. 10.3171/2008.12.JNS081209 [DOI] [PubMed] [Google Scholar]
- 16.Paolini S, Colonnese C, Galasso V, et al. Extradural arteriovenous fistulas involving the vertebral artery in neurofibromatosis type 1. J Neurosurg Spine 2008;8:181–5. 10.3171/SPI/2008/8/2/181 [DOI] [PubMed] [Google Scholar]
- 17.Guzel A, Tatli M, Er U, et al. Surgical treatment of cervical arteriovenous fistula in a patient with neurofibromatosis type 1. A case report. Neuroradiol J 2007;20:566–9. 10.1177/197140090702000515 [DOI] [PubMed] [Google Scholar]
- 18.Siddhartha W, Chavhan GB, Shrivastava M, et al. Endovascular treatment for bilateral vertebral arteriovenous fistulas in neurofibromatosis 1. Australas Radiol 2003;47:457–61. 10.1046/j.1440-1673.2003.01221.x [DOI] [PubMed] [Google Scholar]
- 19.Tanaka T, Hasegawa Y, Kanki T, et al. [Combination of intravascular surgery and surgical operation for occipital subcutaneous arteriovenous fistula in a patient with neurofibromatosis type I]. No Shinkei Geka 2002;30:309–13. [PubMed] [Google Scholar]
- 20.Maheshwari S, Kale HA, Desai SB, et al. Magnetic resonance imaging findings in an unusual case of atlanto axial dislocation and vertebral artery-vein fistulas in a patient of neurofibromatosis-1. Australas Radiol 2002;46:316–8. 10.1046/j.1440-1673.2002.01069.x [DOI] [PubMed] [Google Scholar]
- 21.Kāhārā V, Lehto U, Ryymin P, et al. Vertebral epidural arteriovenous fistula and radicular pain in neurofibromatosis type I. Acta Neurochir 2002;144:493–6. 10.1007/s007010200071 [DOI] [PubMed] [Google Scholar]
- 22.Benndorf G, Assmann U, Bender A, et al. Vertebral arteriovenous fistula associated with neurofibromatosis type I misdiagnosed as a giant aneurysm. Interv Neuroradiol 2000;6:67–74. 10.1177/159101990000600109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hori Y, Goto K, Ogata N, et al. Diagnosis and endovascular treatment of vertebral arteriovenous fistulas in neurofibromatosis type 1. Interv Neuroradiol 2000;6:239–50. 10.1177/159101990000600310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roth TC, Manness WK, Hershey BL, et al. Complex vertebral arteriovenous fistula and ruptured aneurysm in neurofibromatosis: a therapeutically challenging case. Skull Base Surg 2000;10:35–42. 10.1055/s-2000-6786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ma X, Aminina M, Rozen TD. Arteriovenous fistula in neurofibromatosis. Neurology 2000;55:288. 10.1212/wnl.55.2.288 [DOI] [PubMed] [Google Scholar]
- 26.Sampei T, Yugami H, Sumii T, et al. [A case of neurofibromatosis type 1 associated with arteriovenous fistula caused by re-bleeding of a vertebral dissecting aneurysm]. No Shinkei Geka 1999;27:927–31. [PubMed] [Google Scholar]
- 27.Ushikoshi S, Goto K, Uda K, et al. Vertebral arteriovenous fistula that developed in the same place as a previous ruptured aneurysm: a case report. Surg Neurol 1999;51:168–73. 10.1016/S0090-3019(98)00011-1 [DOI] [PubMed] [Google Scholar]
- 28.Murayama Y, Usami S, Abe T, et al. Transvenous Doppler guidewire sonographic monitoring during treatment of a complex vertebral arteriovenous fistula associated with neurofibromatosis type 1. Neuroradiology 1999;41:328–33. 10.1007/s002340050758 [DOI] [PubMed] [Google Scholar]
- 29.Koenigsberg RA, Aletich V, Debrun G, et al. Cervical vertebral arteriovenous fistula balloon embolization in a patient with neurofibromatosis type 1. Surg Neurol 1997;47:265–73. 10.1016/S0090-3019(96)00254-6 [DOI] [PubMed] [Google Scholar]
- 30.Anegawa S, Hayashi T, Torigoe R, et al. [Symptomatic arteriovenous fistula in a patient with neurofibromatosis type I]. No Shinkei Geka 1997;25:373–8. [PubMed] [Google Scholar]
- 31.Schievink WI, Piepgras DG. Cervical vertebral artery aneurysms and arteriovenous fistulae in neurofibromatosis type 1: case reports. Neurosurgery 1991;29:760–5. 10.1227/00006123-199111000-00020 [DOI] [PubMed] [Google Scholar]
- 32.Johnson CE, Russell EJ, Huckman MS. Resolution of spinal epidural vascular pseudotumor following balloon occlusion of a postoperative vertebral arteriovenous fistula. Neuroradiology 1990;31:529–32. 10.1007/BF00340135 [DOI] [PubMed] [Google Scholar]
- 33.Wada K, Ohtsuka K, Terayama K, et al. Neurofibromatosis with spinal paralysis due to arteriovenous fistula. Arch Orthop Trauma Surg 1989;108:322–4. 10.1007/BF00932324 [DOI] [PubMed] [Google Scholar]
- 34.Hasegawa H, Bitoh S, Katoh A, et al. Bilateral vertebral arteriovenous fistulas and atlantoaxial dislocation associated with neurofibromatosis--case report. Neurol Med Chir 1989;29:55–9. 10.2176/nmc.29.55 [DOI] [PubMed] [Google Scholar]
- 35.Parkinson D, Hay R. Neurofibromatosis. Surg Neurol 1986;25:109–13. 10.1016/0090-3019(86)90128-X [DOI] [PubMed] [Google Scholar]
- 36.Kamiyama K, Endo S, Horie Y, et al. [Neurofibromatosis associated with intra- and extracranial aneurysms and extracranial vertebral arteriovenous fistula]. No Shinkei Geka 1985;13:875–80. [PubMed] [Google Scholar]
- 37.Deans WR, Bloch S, Leibrock L, et al. Arteriovenous fistula in patients with neurofibromatosis. Radiology 1982;144:103–7. 10.1148/radiology.144.1.6806851 [DOI] [PubMed] [Google Scholar]
- 38.Kinouchi H, Mizoi K, Takahashi A, et al. Dural arteriovenous shunts at the craniocervical junction. J Neurosurg 1998;89:755–61. 10.3171/jns.1998.89.5.0755 [DOI] [PubMed] [Google Scholar]