Abstract
The aims of this study were to describe how people living with HIV (PLWH) perceive hope and illustrate implications for HIV care and treatment. This is a qualitative study done to explore perceptions and meanings of hope among PLWH attending care and treatment clinics in Dar es Salaam, Tanzania. In all, 10 focus group discussions and 9 in-depth interviews were conducted. People living with HIV described the following 3 dimensions of hope: cognitive, positive emotions, and normalization. Being cognizant of the effectiveness of antiretroviral treatment (ART) often led to positive emotions, such as feeling comforted or strengthened, which in turn was related to positive actions toward normalizing life. Improved treatment outcomes facilitated hope, while persistent health problems, such as ART side effects, were sources of negative emotions contributing to loss of hope among PLWH. Hope motivated positive health-seeking behaviors, including adherence to ART, and this may guide interventions to help PLWH cope and live positively with HIV.
Keywords: hope, hopelessness, cognitive, coping, HIV, Tanzania
Introduction
Efforts to scale up access to antiretroviral treatment (ART) have been successful in improving life expectancy for people living with HIV (PLWH) and transforming HIV/AIDS disease from a death sentence into a chronic health condition.1–7 However, access to care for comorbidities commonly occurring with HIV/AIDS, especially care for mental health conditions, is still limited.8–10 There is evidence that the mental health conditions of hopelessness and depression are of high prevalence in PLWH and can contribute to poor outcomes of ART care as well as deter the public health efforts of preventing HIV transmission. A recent report from a study conducted in South Africa among PLWH showed that rates of hopelessness and depression among newly diagnosed PLWH were 29% and 80%, respectively. The same study found that depressed PLWH were more likely than those not depressed to demonstrate suicidal ideation.11 An overview presented by Leserman found that depression among PLWH increased HIV disease progression.12 In addition, Locke and Newcomb reported that depression among PLWH was associated with an increased risk of HIV transmission.13 A recent report from a study conducted in Spain to explore depression and health-related quality of life among PLWH showed that depression was associated with poor health outcomes.14 Other evidence suggests that hopelessness among PLWH delays action in seeking health care and is related to poor adherence to ART.15,16 Without appropriate interventions to address mental health comorbidities, PLWH may continue to have poor quality of life despite increased access to ART globally.
In low-income countries, the consequences of depression and hopelessness among PLWH may be exacerbated by the lack of interventions to effectively enhance coping skills and alleviate distress. This indicates the need for more efforts to evaluate interventions targeted at addressing these conditions among PLWH. Existing evidence from both low- and high-resourced settings shows that mental health conditions of depression at mild to moderate levels can often be addressed through appropriate psychological interventions that facilitate coping strategies for the challenges of living with HIV.17 In a 2007 review, which included studies from both high- and low-resource countries, Bernaysa and colleagues argued that the concept of hope/hopefulness within the context of HIV treatment has the potential to inform care, particularly in low-income countries.18 Among patients with chronic, difficult to treat, or terminal illnesses, promoting hope has been found to enhance coping, reduce depression, and hopelessness.19,20 Among PLWH in Tanzania, there is still limited information available on interventions that can reduce depression and hopelessness as well as enhance coping to promote mental well-being and quality of life for PLWH. A better understanding of hope among PLWH in such contexts can shed light on strategies to improve coping, mental health, and quality of life.
This study aimed to explore the concept of hope and consider its potential to inform the development of feasible approaches to promoting mental well-being and quality of life as well as improving HIV-related health outcomes in PLWH. In this article, we describe meaning and experiences of PLWH with building hope and overcoming hopelessness after their HIV diagnosis.
Methods
Study Design and Sampling
We conducted the study using qualitative methods from February to June 2012, including focus group discussions (FGDs) and in-depth interviews with key informant (KI) PLWH, to describe experiences with hope and hopelessness as well as explore its core essence/phenomenon in Dar es Salaam, Tanzania. The study was implemented at 8 large HIV care and treatment clinics (CTCs) that are supported by the US President’s Emergency Plan for AIDS Relief (PEPFAR) from the 3 municipalities of Dar es Salaam city. The locations for the study were selected purposively at recruitment sites, because they are large sites (site had more than 5000 registered PLWH) and would allow greater access to eligible study participants.
We sampled participants for the FGDs from PLWH receiving HIV health care services in PEPFAR-supported CTCs in Dar es Salaam, Tanzania, for at least 6 months before the study began. This criterion was used to ensure that the period of time was sufficient for participants to feel comfortable sharing their experiences of distress or hope in living with HIV.
The in-depth interview KIs were also sampled from among PLWH registered and receiving care in PEPFAR-supported CTCs in Dar es Salaam for at least 6 months. In addition, they also had a documented recent diagnosis of depression or depression was indicated as a reason for their loss to follow-up or for a missed clinic visit in their medical records. This criterion was used to select the KIs who could share more in-depth information on some constructs that emerged from the FGD participants, mainly on study topics such as sonona (depression) and hopelessness. However, they also described their experiences of hope in order to see how PLWH with diagnosed psychological distress perceived and experienced hope.
Data Collection Process
Trained social scientist interviewers accessed selected HIV CTCs through hospital managers who had provided permission to conduct the study. Interviewers used Swahili semi-structured interview/FGD guides with 2 thematic areas to identify aspects of hope and hopelessness. Translated FGD and KI guides were piloted among PLWH from nonparticipating sites before the study initiated. Based on the findings from the pilot, the guides were revised for the main study, resulting in 1 to 1½ hour FGDs and KI interviews. An equivalent of US$5 was provided to all participants to compensate them for their time and transport.
Selection of FGD Participants and Collection of Data
Focus group discussion participants were eligible if they were PLWH, aged 18 years or older and had been receiving HIV care and treatment services for at least 6 months at the participating PEPFAR-supported public CTCs in Dar es Salaam, Tanzania. Focus group discussion information allows for understanding of culturally normative values and practices as these relate to the concept of hope.
The interviewers worked with patient social support groups available at all of the sites during routine patients’ clinic visits to identify and invite eligible patients to the FGDs. A total of 100 eligible participants were contacted for FGDs and all agreed to participate. However, we had to limit the average number of participants to 6 to 8 people per FGD to ensure maximum engagement of all participants in the discussions. A total of 10 FGDs were conducted before saturation was reached. Of the 10 FGDs, 3 each comprised men and women who were 35 years or older and 2 each included men and women who were between 18 and 34 years of age. Each FGD constituted 6 to 8 participants with a total of 78 PLWH participants. Two interviewers, one facilitating discussions and the other documenting detailed field notes on nonverbal aspects of communication, audiorecorded FGDs, and KI interviews. Participants in all of the FGDs and in all but one KI provided permission for audiorecording sessions.
Selection of KIs and Data Collection Process
Key informants were sampled from the same population of PLWH, having the same criteria as FGD participants but with an additional criterion of having been diagnosed recently with any form of depression (mild moderate or severe) or having documented evidence that depression was a reason for missing scheduled clinic visits in their medical records. This was determined from the care database of National HIV care electronic patients available in all participating sites. In-depth interviews with KIs were conducted after some data of the FGDs had been completed, intending both to inform in-depth understandings at experiential levels of emerging constructs from FGD narratives relating to topics of hope and hopelessness. This also provided information regarding similarities and differences in characteristics of hope described by PLWH with and without documented depression. Nine in-depth interviews were conducted with KIs before saturation was reached, including 4 with women aged 18 to 34 years, 2 with women aged 35 years or older, 2 with men aged 35 years or older, and 1 with a man aged 18 to 34 years. Information provided by 1 woman participant of the in-depth interview aged 18 to 34 years was not analyzed as she had also participated in an FGD study and of the 3 men, only 1 man between the ages of 18 and 34 years was included because 2 had travelled outside Dar es Salaam and didn’t return within the time period the study was being conducted.
Data clerks at the study sites worked with the interviewers to provide lists of eligible KIs, with documented recently diagnosed depression or depression as a reason for missing a clinic visit from the electronic national database available at each site. The interviewers then used the lists to work with nurse counselors to contact potential KIs.
In order to remove potential cultural barriers of communication and ensure adequate representation from different age and gender groups, FGD and KI participants were selected to attain equal numbers of the following 4 groups: women 18 to 34 years of age, women aged 35 years or older, men 18 to 34 years of age, and men aged 35 years or older. The rationale for this sampling strategy was also related to the observation that age and gender have been reported to affect psychological distress and coping. Women living with HIV were found to be twice as likely to have psychological distress, including depression, compared to men.21 In South Africa, men were reported to be more likely than women to become dependent, engage in more risk behaviors and consume alcohol.22
All narrative data from FGDs and KI interviews in the form of field notes and audiorecordings were transcribed by interviewers within 48 hours of data collection and reviewed by study investigators soon after transcription to inform new probes in the guide as well as to facilitate an iterative process between data collection and analysis. This process also allowed provision of feedback to interviewers aimed at improving the quality of interviewing and data integrity.
Data Analysis
We used an iterative approach to analyze data from the outset of data collection. In weekly meetings between study social scientist interviewers and investigators, relevance of emergent narrative data themes to study questions was explored as were areas for further probing to increase clarity and depth of provided information. Changes to guides were incorporated prior to the next set of FGDs and KI interviews. Organization and coding of narrative data were assisted by NVIVO version 8 software. Analysis was based on grounded theory 23 including developing as a team initial lists of descriptive codes after reading through the transcripts, sharing and refining code descriptions and agreeing on a set of initial topic codes pertaining to meanings, determinants, characteristics, and circumstances in which PLWH experienced hope, and identifying common local idioms used to describe hope. The topic coding process also allowed for introduction of additional topic codes to the initial code book that pointed to particularly useful meanings or refinement of earlier agreed upon code definitions. Two members of the team were centrally involved in coding, after which the team met again to review emergent topics. These were developed into broader unique categories/themes, with minimal overlap based on the meaning they conveyed. Illustrative examples were sought from narratives that increased clarity and depth of category descriptions. Finally, analytic codes were developed for some categories, based on the demographic characteristics of study participants.
Results
Characteristics of Study Participants
A total of 78 PLWH participated in the FGD and in-depth interviews. All the participants had been diagnosed with HIV disease 6 months or longer before the study began and were taking ART. Overall, 47 (59%) were above the age of 35 years and 45 (57%) were women. Six participants (7.66%) were in World Health Organization (WHO) stage I, 11 (14.47%) were in WHO stage II, 41 (52.34%) were in WHO stage III, and 20 (25.52%) were in WHO stage IV. All the study participants were taking antiretroviral (ARV) medications and had physical functioning status of “walking” and none was in a “bed ridden” or “ambulatory physical functioning status.” The median CD4 count for the study participants was 218 cells/mm.3
Themes
Three themes emerged from the data which robustly conveyed the experiences of hope as involving emotions, cognitive approaches, and coping/normalization. Items characterizing hope and those describing conflicting meanings of hope among PLWH are described. The theme of emotions included positive feelings of joy, happiness, security, and relief. The emotional theme also had a spiritual dimension of feeling comforted, uplifted, assured, and at peace. The cognitive theme included positive thoughts of a good future and for promotion of longevity. The theme of coping/normalization included acceptance of HIV-positive status, seeking, and adhering to medical care as well as making and implementing future plans.
Attaining anticipated treatment outcomes after receiving HIV treatment including improved health from a previous status of being ill was the major source of developing the positive emotions as described previously. On the other hand, coping/normalization after an HIV-positive diagnosis was influenced by both cognitive approaches and emotions, including emotion attached to a deity or religious believe. Both positive emotions and cognitive approaches brought about a sense of renewed inner strength or motivation which then served as a drive to cope/normalize life after contacting HIV/AIDS disease. This is similar to the earlier descriptions of elements of hope, known as agency or “a driving force” described by Snyder in 1991 where hope served as a booster for people to engage in activities to achieve their goals,24 which in this case can lead to activities to cope/normalize one’s life. A more recent definition of hope is an emotional function of yearning to fulfill a goal.25 From these analyses, PLWH participants view adhering to treatment as related to the desire to remain healthy and engage in activities considered “normal” prior to an HIV diagnosis. The following quotations are examples that illustrate each of the 3 themes that emerged from the data.
Hope described as emotions.
Both the groups of women and men between the ages of 18 and 34 years described the terror and fear of ending their lives early which they had initially thought would happen to them because of HIV. They describe what they felt after this fear was erased through receiving treatment as hope. The women between the ages of 18 and 35 years had feelings of satisfaction resulting from responding well to ART and other treatment for HIV-related comorbidities.
What I know with experiencing hope? It means … aah …mmmhhm. To me truly it is the feeling of satisfaction one can have based on what they are expecting and if they got it or not. Like the satisfaction I felt after I had started the ART and tuberculosis treatment. I became better, felt well, and I gained weight, even much more than the HIV uninfected people. Because of this I started to realize that I won’t die as I had thought before treatment, I will recover. Now I am doing well and not falling sick all of the times anymore. This is why I feel satisfied even if you look at me now I don’t look stressed. That is the meaning of hope to me. (participant, in-depth interview/woman between the ages of 18 and 34 years)
This was similar to what the group of men between the ages of 18 and 34 years experienced and described in the following quotation: “For me I will say hope is what lifted me up when I was not sure of continuing with my life anymore. Mmmhh I mean when this problem of [HIV] came my way, I lost all my strength [inner strength], but I sat down one day with my brother and he called a nurse he once knew, who assured us that I can be treated! That, the treatment is available. Suddenly I knew this is not the end of my life! I can be treated … huh! And so it gave me much joy and happiness that caused my heart [to] gain strength again. See because I had thought HIV could just kill me anytime and there was nothing I could do. So I came to this hospital and that is where I was started [on] treatment [ART]” (FGD participant/man between the ages of 18 and 34 years).
For this age group, to be made aware that HIV doesn’t cause immediate death and that life can continue because of the availability of treatment also acted as an inner-driving force for seeking health care as illustrated in the above-mentioned quotation.
Similar to the groups with participants aged between 18 and 34 years, the groups of men and women aged 35 years or older also described having positive feelings of security which came after they were able to freely access ART as hope. This is probably because ART provided PLWH with improved prognosis and survival. “When we come to this clinic (CTC) we felt assured to live because this is where ART is available. We got ART for free so you know without this clinic there will be no hope for us. Therefore we do not feel hopeless anymore, but rather we feel secured knowing we can get these ARV medications to guarantee continuity of our good health for free. To feel this secure about my health is what we call hope!” (FGD participant/man aged 35 years or older).
Additionally among men aged 35 years or older, spiritual and/or religious beliefs brought feelings of security and assurance of living without the threat of one’s life ending early due to HIV as illustrated in the following quotation: “when I look at myself … mh … all my classmates are dead now and we are remaining only three of us from that group. One person teased me and said “all your colleagues are dead, for you what are you doing that keeps you alive?” “I said I have confidence I will live because I know God loves me and therefore he will keep me to continue living … I will die later in old age like anyone else but not now due to HIV” (key informant in-depth interview/man aged 35 years or older).
Hope described as positive cognitive process.
The second emergent category of positive cognitive thoughts seems to precede the theme of emotions and results from PLWH understanding that HIV does not mean immediate death. This knowledge leads to positive emotions and motivation to seek treatment and cope. To know about the availability of ARV medications and the possibility of longevity and a normal life with HIV (living healthy and continuing with activities before contacting HIV) infection facilitated hope. Newly diagnosed PLWH seemed more likely to develop this pattern of belief after counseling or observing improvements in health status and well-being of other PLWH who had a longer period of knowledge of their status and being on ART. Such visible testimony removed their notion that a positive HIV diagnosis was a death sentence generating a sense of relief and resulted in positive emotions among newly diagnosed PLWH accessing care and treatment. These quotations are illustrative:
I was frustrated with my HIV diagnosis; my life had really ended for me … After I saw many people living very long lives under the ART program; like I saw a person who got HIV infection since 1991 … and … and then I saw him again in 2007 he was fine … walking and doing his job, I felt comforted and happy … I can also live like him. (FGD participant/woman between 18 and 34 years of age)
Before I registered to this clinic I was downcast, but I saw many people at the clinic, they too had a condition like mine [HIV] and they kept telling me … you see us alive? … We have been HIV positive for many years, not just today … and we have been taking ARVs), one said since 1995! I felt assured to live … I am not alone, there are people truly living for long with this disease [HIV], so I realized I too will live and became very happy. (FGD participant/woman between 18 and 34 years of age)
For some, fear acted as an impetus to seek information from others similarly infected with HIV. Information was sought particularly on their experiences with care as noted by this informant.
After discovering I was positive with HIV I was terrified! … I decided to visit places where I could meet people with this condition [HIV] who were providing seminars about HIV infection. I learned that when you are infected [with HIV] it is not the end of the world … Uhuuh! I sighed with the relief I felt … So I knowing that was hope to me! I saw that even me if I start to use the medication, I can continue to live and I can reach my goals which I have already set. (KI, in-depth interview/woman between 18 and 34 years of age)
Outcomes of hope among PLWH.
The third emergent thematic area was coping/normalization; this was facilitated by the positive emotions that came after one developed positive cognitive aspects toward HIV diagnosis. People living with HIV having positive thoughts accepted their HIV-infected status in a positive way. They equated HIV with an accident, living in complete health (clean health), and seeing oneself as no different to uninfected people.
To me now HIV it is just a normal thing which can happen to anyone … just like a person who got into an accident … should not say ‘I have already died’ …, so I live and feel happy and I live a normal way. I follow all advice for my medications [ART] I have been taking ART since September 2009 when I was discovered HIV positive. [FGD participant/man aged 35 years or older]
This state of acceptance in turn facilitated thinking about the future, planning, believing in oneself, and having confidence in one’s owns ability to reach the targets set in life (self-efficacy). This developed into implementing normalization plans leading to positive actions. The coping/normalization actions were focused mainly on taking voluntary steps to engage/continue with routine activities in life as before HIV diagnosis such as working to support a family and having ongoing plans to run one’s life. Others involved positive behavior change of taking responsibility for one’s own health through seeking health care and complying with health care services.
For me since I knew I was infected, and learned how to handle it. I live like others; I am doing my routine work, looking after my children I have no concerns, I live like any other person who doesn’t have HIV infection. (FGD participant/woman 35 year of age or older)
People who knew the extent to which I was downcast when I was sick some days back, now they say they don’t believe when they see me now because when I wake up in the morning nowadays I can bathe well, dress and walk as I want, I can help others as well and I am doing all my work as I want, I am not sick at all, so why shouldn’t I feel very happy? This is hope to me. (KI, in-depth interview, /man 35 years of age or older)
Therefore after getting this counseling from the nurse/counselor I was taken to register at the clinic, truly I was comforted, I decided that I must stay in those conditions (comply with HIV care and treatment services) as I was told by the counselor, and now I see this issue (being HIV positive) as a normal thing I live just like other non-infected people. (KI in-depth interview/man 35 years of age or older)
Such findings emphasize the importance of providing both education and counseling to PLWH after HIV diagnosis and could mean tailoring counseling to involve group discussions of older and newly diagnosed PLWH. Clinic-based HIV counseling support can promote more hope and positive behaviors as described in the above-mentioned quotations.
In contrast, our study reveals that PLWH experience social alienation, poor treatment outcomes characterized by health problems such as suffering from opportunistic infections, side effects of ART, and inability to work due to ill health were sources of negative emotions such as distress, depression, and hopelessness among PLWH. Also, the study participants who had experienced failure to live a normal life or continue with routine activities as it was before they contacted HIV infection reported experiencing distress and discouragement. Continued illness such as having opportunistic infections and side effects of ART as well as nonadherence to ART caused much fear and despair for PLWH as illustrated in the following quotations.
Mmh! hope? Really are you asking me if I have experienced hope? [Pointing her finger to herself]. No! I haven’t yet reached a state of being hopeful with this disease [HIV]; I am sick every day even after starting ART, my husband left me … I can’t take care of my children and I am not sure I will make it … mh (Crying) … but calling me here at the bigger CTC today (this was a CTC located within a the referral hospital) has given me hope because I will be helped to solve this problem of being too sick every day which came after [I] started ART. I am really encouraged that the problem of palpitations will end … at least it can be treated by the doctor. The doctor here, the one who has just seen me here before I come to speak with you, said I will be sent to the ward to be admitted and receive blood and she has also given me another type of ARVs to replace the ones I am taking currently, because she said they are making me lose blood that is why I am feeling very ill. You know I have been on the ART for 3 months and I go to my local CTC each month, I wish they had seen this problem of the ART making me loose blood earlier. (KI in-depth interview/woman 35 years of age or older)
Another participant expressed hopelessness as she felt life had ended with the HIV-positive diagnosis, “for me after I received my HIV diagnosis my life hit the end at that point when I discovered I had HIV. I wasn’t living anymore even though I was walking around. Life was meaningless to me, I wasn’t able to sleep or do my routine work. But afterwards I got support from many people counseling me and encouraging me not to give up, to move on and they also told me that there is medicine (ART) that can treat me. I became happy again and I got a strength in my heart to live like other people … mmmh that is how I got hope” (FGD participant/woman 35 year of age or older).
This emphasizes the need for not only early recognition and treatment of ART-related side effects but also providing education about ART-related side effects to PLWH in order to maintain the positive attitude that PLWH quickly develop toward ART when they first hear about it after receiving an HIV-positive diagnosis. Antiretroviral treatment serves as a major source of hope among PLWH.
Discussion
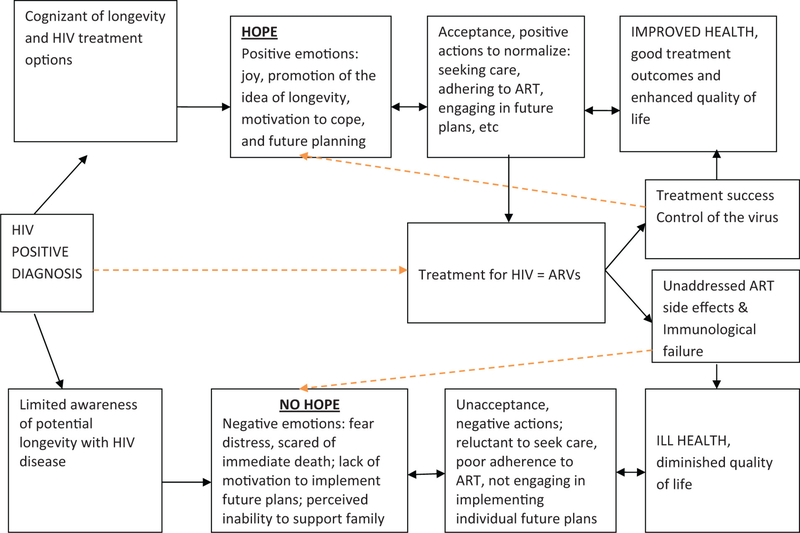
The aim of this descriptive study was to gain insight on experiences of hope in individuals living with HIV/AIDS. Many examples presented illustrate experiences and meanings that PLWH perceive hope to be in the course of being diagnosed HIV positive and life thereafter. The PLWH in this study experienced hope or hopefulness as positive emotions that stimulated inner strength which acted as a drive to cope and normalize their lives. This drive led PLWH to comply with HIV care, adhere to their medications, engage in activities they had planned, and see themselves no different from those individuals not infected with HIV. Figure 1 elaborates a potential pathway of hope among PLWH as described by participants in this study.
Figure 1.
Pathway to developing hope and hopelessness and related outcomes among people living with HIV (PLWH).
Awareness of and access to available treatment (ART) and good treatment outcomes were the main facilitators of hope. In our study, participants viewed HIV to be a life-threatening illness with the possibility of sudden death or having a very short time to live, as soon as they got diagnosed. This changed, however, when PLWH saw other PLWH at the clinics or in the community and when they became aware/knowledgeable of not only treatment options but also counseling on how to live with HIV conditions such as medication, food, and so on as illustrated in the quotations. The findings are similar to the study by Lynch who described imagination as a healer of hopelessness and urged that if the dreaded possibility does occur, hope functions as a creative process that seeks to imagine another way of dealing with these circumstances.26 This suggests the importance of improving the commonly practiced culture of promoting health education on HIV prevention to PLWH and to the general population and begins to add issues of education about HIV disease and available treatment options.
In this study, religiosity aided the development of hope among the older participants. Our study revealed that belief or having faith and a perceived sense of love from a superior being added to bring the positive feelings of hope in some PLWH. This belief in a supernatural being is similar to what was previously defined as religiosity by D’Souza et al27 in their study on spirituality, religion, psychiatry, and the application to clinical practice that was conducted in 2006 in Australia. They defined religiosity as beliefs and behaviors that are related to a supernatural or sacred being and which are grounded in a religious community or tradition. Religiosity has also been reported to have a potential role in the management of depression.28,29 In our study, it was the individual-level religiosity that promoted hope. Such religiosity has been reported in previous studies to facilitate HIV preventive behaviors in the general population and good treatment outcomes among PLWH.30–33 In the context of HIV care in Tanzania currently, individual religiosity issues are not often looked at. This could easily be addressed during individual counseling sessions to increase its potential benefits to PLWH.
This study shows that helping PLWH to develop and maintain hope can be an important aspect of care. This can improve quality of life as reported previously by Akinsola, especially if used as an approach to combat the current challenge of poor adherence with care and high incidences of lost to follow up among PLWH in many ART care programs.34
In addition, the study findings unfold some of the key factors that facilitate hope among PLWH and the conditions to which such factors can bring about hope. One of the main functions of hope reported in the previous literature is to deal with discouraging situations or desperation happening in one’s life, by allowing the person to psychologically find a way to get out of such an encounter.35
The data from this study show that the pathway for PLWH to develop hope includes first having a cognitive shift—lived experience, observation, or education that HIV does not necessarily cause immediate death which generates cognition/awareness of HIV treatment options, service availability, and the effectiveness of treatment. The result of this is positive emotion that also can generate a spiritual cognitive–emotional dimension of peace, uplifting, and positive future expectations. In turn, this fosters motivation to re-engage in pursuing pre-HIV diagnosis life goals in directions that include more positive HIV disease coping/normalization actions. This pathway is explained partly by incentive theory of motivation whereby people are pulled/motivated by external goals or incentives. In this theory, any stimulus object that people have learned to associate with positive or negative outcomes can serve as an incentive, for example, a relief from pain and partly by perceived benefits as reflected in the Health Belief Model (HBM; see Figure 1).
In this current study, accessing ART was viewed by PLWH as an opportunity to bypass HIV/AIDS-related ill health and the perceived consequences of shortened life in order to continue with life as it was before contacting HIV. However, ART was mentioned to facilitate hope only when it resulted in positive health outcomes of the user and if it was not associated with lasting side effects (Figure 1). If there were no signs of improvement from ill health after starting ART and if there were any unmanaged side effects, a poor prognosis or premature death may result. The described negative outcomes of care such as experiencing side effects of ARV medications for a long time as well as the inability to improve and return to work were facilitators of hopelessness and despair. Uncertainty of life was noted among PLWH who were experiencing illnesses most frequently. This further shows the importance of ensuring availability of quality standard ART care for PLWH that includes targeted counseling and timely recognition and treatment of side effects of ART in improving the overall health of PLWH. Also, boosting and maintaining hope as an assurance to sustain their plans and activities comes when they experience good treatment outcomes as elaborated in a number of examples stated previously.
Another implication this might have for the current HIV care programs, especially in resource-limited countries, is the need to build capacity to frequently monitor patients who are on ART in order to ensure positive treatment outcomes and avoid prolongation of side effects or worsening of HIV-related illnesses.
Furthermore, this work depicts a cognitive aspect of hope known as agency described by Snyder in the work published in 1991 and 1994 where hope was found to boost engagement in actions toward achieving a certain goal,24 an aspect that may be useful in improving adherence to medications and to visit schedules among PLWH. There is a desire to remain with the kind of life style that they used to live prior to diagnosis of HIV among PLWH in this study, and as it is known the stability and good health in an individual who is living with HIV is largely determined by taking ART,36 this aspect of hope could be promoted during routine counseling sessions as part of HIV care. For example, patients could be helped during counseling sessions to relate their improved CD4 counts to taking ART often continued their life style as before they were diagnosed with HIV/AIDS disease, the agency aspect of hope could then be facilitated to continue with the long-term demands of adhering to ART and to clinic visits.
Conclusion
Although the use of ARV medications has greatly succeeded in improving the health status of PLWH worldwide, more effort is needed in other aspects of care including psychological well-being for PLWH to experience quality life. In this study, hope was an inner drive for PLWH to engage in positive behavior of seeking and complying with HIV treatment and health care programs. Knowledge or awareness of HIV disease and the possibility to leave longer with HIV under the available treatments were keys to developing hope. Experiences of good treatment outcomes and religion also added to facilitate hope while continued ill health and treatment side effects deterred hope among PLWH. Although our study involved a subgroup of PLWH who are on ART in urban areas and lacks PLWH not taking ART or living in rural areas, the findings point to a possibility of positive benefits of promoting aspects of hope among PLWH attending ART care programs in complementing ART care on improving the quality of lives for PLWH.
Acknowledgements
The authors wish to thank all participants, staff, and the administration of the following hospitals and health centers: Sinza, Mwananyamala, Mbagala Rangi tatu, Amana, Temeke, Amtulubai Karimjee Clinic (AKC), Tandale and Buguruni which participated in the study. The Management and Development for Health (MDH) and Muhimbili University of Health and Allied Sciences departments of Psychiatry, Epidemiology contributed significantly to this study. Special thanks are extended to Deiya Mpanze, Magreats Somba, Neema Mleli, Janet Kamala, Francis Ngomba, and Donald Kakuru.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Tanzania HIV/AIDS and TB remove the center and through. it is just known as Tanzania HIV and TB ICORTA program International Clinical, Operational, and Health Services Research and Training (ICOHRTA) program at Muhimbili University of Health and Allied Sciences, Dar es Salaam Tanzania, which is funded by the Fogarty funded by Fogarty International Center, National Institutes of Health [Grant Number 5U2RTW008258].
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Chan KC, Wong KH, Lee SS. Universal decline in mortality in patients with advanced HIV-1 disease in various demographic subpopulations after the introduction of HAART in Hong Kong, from 1993 to 2002. HIV Med. 2006;7(3):186–192. [DOI] [PubMed] [Google Scholar]
- 2.Braitstein P, Brinkhof MW, Dabis F, et al. Mortality of HIV-1-infected patients in the first year of antiretroviral therapy: comparison between low-income and high-income countries. Lancet. 2006;367(9513):817–824. [DOI] [PubMed] [Google Scholar]
- 3.Palella FJ Jr, Delaney KM, Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338(13):853–860. [DOI] [PubMed] [Google Scholar]
- 4.Chene G, Sterne JA, May M, et al. Prognostic importance of initial response in HIV-1 infected patients starting potent antiretroviral therapy: analysis of prospective studies. Lancet. 2003;362(9385):679–686. [DOI] [PubMed] [Google Scholar]
- 5.King JT Jr, Justice AC, Roberts MS, Chang CC, Fusco JS. Long-term HIV/AIDS survival estimation in the highly active antiretroviral therapy era. Med Decis Making. 2003;23(1):9–20. [DOI] [PubMed] [Google Scholar]
- 6.Siegfried N, Uthman OA, Rutherford GW. Optimal time for initiation of antiretroviral therapy in asymptomatic, HIV-infected, treatment-naive adults. Cochrane Database Syst Rev. 2010;(3):CD008272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Siegfried N, Uthman OA, Rutherford GW. Optimal time for initiation of antiretroviral therapy in asymptomatic, HIV-infected, treatment-naive adults. Cochrane Database Syst Rev. 2010;(3):CD008272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harding Dr Richard, Simms Victoria, Penfold Suzanne, et al. Higginson, PEPFAR Public Health Evaluation - Care and Support: Phase 2 Kenya report. http://www.cpc.unc.edu/measure/publications/tr-10-74c. [accessed on March 2, 2014]
- 9.Simms Victoria, Harding Richard, Penfold Suzanne, et al. Higginson, PEPFAR Public Health Evaluation -Care and Support: Phase 2 Uganda, 2010. http://www.cpc.unc.edu/measure/publications/tr-10-74d. [accessed on March 2014]
- 10.Samuel Likindikoki. Knowledge, attitude and self-efficacy to diagnose and treat depression Preliminary Report of Unpublished Study. Tanzania: Department of psychiatry, Muhimbili University of Health and allied sciences; 2010. [Google Scholar]
- 11.Govender RD, Schlebusch L. Hopelessness, depression and suicidal ideation in HIV-positive persons. South Afr J Psychiatry. 2012;18(1):17–21. [Google Scholar]
- 12.Leserman J Role of depression, stress, and trauma in HIV disease progression. Psychosom Med. 2008;70(5):539–545. [DOI] [PubMed] [Google Scholar]
- 13.Locke TF, Newcomb MD. Correlates and predictors of HIV risk among inner-city African American female teenagers. Health Psychol. 2008;27(3):337–348. [DOI] [PubMed] [Google Scholar]
- 14.Briongos-Figuero LS, Bachiller-Luque P, Palacios-Martín T, De Luis-Román D, Eiros-Bouza JM. Depression and health related quality of life among HIV-infected people. Eur Rev Med Pharmacol Sci. 2011;15(8):855–862. [PubMed] [Google Scholar]
- 15.Raveis VH, Siegel K, Gorey E. Factors associated with HIV-infected women’s delay in seeking medical care. AIDS Care. 1998;10(5):549–562. [DOI] [PubMed] [Google Scholar]
- 16.Ngarina M, Popenoe R, Kilewo C, Biberfeld G, Ekstrom AM. Reasons for poor adherence to antiretroviral therapy postnatally in HIV-1 infected women treated for their own health: experiences from the Mitra Plus study in Tanzania, BMC Public Health. 2013;13(1):450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith Fawzi MC, Eustache E, Oswald C, et al. Psychosocial support intervention for HIV-affected families in Haiti: implications for programs and policies for orphans and vulnerable children. Soc Sci Med. 2012;74(10):1494–1503. [DOI] [PubMed] [Google Scholar]
- 18.Bernaysa Sarah, Rhodesa Tim, Barnettb Tony. Hope: a new way to look at the HIV epidemic AIDS. 2007;21(suppl 5):S5–S11. [DOI] [PubMed] [Google Scholar]
- 19.Schaufel Margrethe Aase, Nordrehaug Jan Erik, Malterud Kirsti. Hope in action—facing cardiac death: a qualitative study of patients with life-threatening disease. Int J Qual Stud Health Well-being. 2011;6(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kaye A The relationship between levels of hope and level of coping response and other variables in patients with Cancer. Oncol Nurs Forum. 1989;16(1):67–72. [PubMed] [Google Scholar]
- 21.Evans DL, Ten Have TR, Douglas SD, et al. Association of depression with viral load, CD8 lymphocytes and natural killer cells in women with HIV infection. Am J Psychiatry. 2002;159(10):1752–1758. [DOI] [PubMed] [Google Scholar]
- 22.Olley BO, Gxamza F, Seedat S, et al. , Psychopathology, and coping in recently diagnosed HIV/AIDS patients–the role of gender. S Afr Med J. 2003;93(12):928–931. [PubMed] [Google Scholar]
- 23.Glaser BG. Basics of Grounded Theory Analysis. Mill Valley, CA: Sociology Press; 1992. [Google Scholar]
- 24.Snyder CR1, Harris C, Anderson JR, et al. The will and the ways: development and validation of an individual differences measure of hope. J Pers Soc Psychol. 1991:60(4);570–585. [DOI] [PubMed] [Google Scholar]
- 25.MacInnis Deborah J, Chun Hae Eun. Understanding hope and its implications for consumer behavior: i hope therefore i consume: understanding hope and its implications for consumer behavior. Found Trends Mark 2007;1(2):97–189. [Google Scholar]
- 26.Lynch WF. Images of Hope: Imagination as Healer of Hopelessness. Baltimore: Helicon; 1965. [Google Scholar]
- 27.D’Souza R, George K. Spirituality, religion and psychiatry: its application to clinical practice. Australas Psychiatry. 2006;14(4):408–412. [DOI] [PubMed] [Google Scholar]
- 28.Razali SM, Hasanah CI, Aminah K, Subramaniam M. Religious–sociocultural psychotherapy in patients with anxiety and depression. Aust N Z J Psychiatry. 1998;32(6):867–872. [DOI] [PubMed] [Google Scholar]
- 29.Thearle MJ, Vance JC, Najman JM, Embelton G, Thearle MJ, Hodgen FM. Church attendance, religious affiliation and parental responses to sudden infant death, neonatal death and stillbirth. Omega (Westport). 1995;31(1):51–58. [Google Scholar]
- 30.Gray PB. HIV and Islam: is HIV prevalence lower among Muslims? Soc Sci Med. 2004;58(9):1751–1756. [DOI] [PubMed] [Google Scholar]
- 31.Kagimu M, Guwatudde D, Rwabukwali C, Kaye S, Walakira Y, Ainomugisha D. Religiosity for promotion of behaviors likely to reduce new HIV infections in Uganda: a study among muslim youth in Wakiso District. J Relig Health. 2013;52(4): 1211–1227. [DOI] [PubMed] [Google Scholar]
- 32.McCree DH, Wingood GM, DiClemente R, Davies S, Harrington KF. Religiosity and risky sexual behavior in African-American adolescent females. J Adolesc Health. 2003;(33):(1):2–8. [DOI] [PubMed] [Google Scholar]
- 33.Mueller PS, Plevak DJ, Rummans TA. Religious involvement, spirituality, and medicine: implications for clinical practice. Mayo Clin Proc. 2001;76(12):1225–1235. [DOI] [PubMed] [Google Scholar]
- 34.Akinsola HA. Fostering hope in people living with AIDS in Africa: The role of primary health-care workers [review]. Aust J Rural Health. 2001;9(4):158–165. [DOI] [PubMed] [Google Scholar]
- 35.Korner JN. Hope as a method of coping. J Consult Clin Psychol. 1970;34(20):134–139. [DOI] [PubMed] [Google Scholar]
- 36.Paterson DL, Swindells S, Mohr J, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133(1):21–30. [DOI] [PubMed] [Google Scholar]