Abstract
The pandemic novel coronavirus disease (COVID-19) has become a global concern in which the respiratory system is not the only one involved. Previous researches have presented the common clinical manifestations including respiratory symptoms (i.e., fever and cough), fatigue and myalgia. However, there is limited evidence for neurological and psychological influences of SARS-CoV-2. In this review, we discuss the common neurological manifestations of COVID-19 including acute cerebrovascular disease (i.e., cerebral hemorrhage) and muscle ache. Possible viral transmission to the nervous system may occur via circulation, an upper nasal transcribrial route and/or conjunctival route. Moreover, we cannot ignore the psychological influence on the public, medical staff and confirmed patients. Dealing with public psychological barriers and performing psychological crisis intervention are an important part of public health interventions.
Keywords: Brain, indirect influence, neurological, SARS-COV-2, psychological, mental health, COVID-19, transmission
1. Introduction
Severity and prognosis of the 2019 novel coronavirus disease (COVID-19), also known as novel coronavirus pneumonia (NCP), have become global concerns in terms of how to treat the patients because this novel disease affects many organs beyond lung [1, 2].
COVID-19 is caused by infection with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2 named by WHO), which resembles and differs from SARS-CoV. One of the similarities is both viruses exploit the angiotensin converting enzyme 2 (ACE2) receptor to gain entry inside cells [3]. One main difference is that the former affects the lung as NCP in every patient but the later, not in every patient developing atypical pneumonia. The most characteristic symptom of NCP is respiratory distress, with a typical chest computer tomography (CT) finding of ground-glass opacity, similar to that of SARS [4]. Previous researches have presented the common clinical manifestations including respiratory symptoms (i.e., fever and cough), fatigue and myalgia.
However, other less common symptoms indicated the influence on other organs and systems. Recent retrospective case series study of Dr. Mao and colleagues [5] discussed neurological manifestations of hospitalized patients with COVID-19. Dr. Li et al reasoned that the respiratory failure may partly be due to a neuroinvasive potential of SARS-CoV-2 [6].
If the NCP onset seemed mainly about nervous system diseases, it could be easily misdiagnosed. And these patients might become invisible sources of transmission. Therefore, it is important to understand the neurological symptoms and possible underlying mechanisms in patients with SARS-CoV-2. In addition, it has been reported that there is a panic among both the sick and the healthy about this new pandemic [7, 8]. Besides the conventional treatment of COVID-19, we should pay attention to the patients' brain health at the same time.
2. Common Neurological Manifestations
Neurological symptoms can be categorized into three main areas: central nervous system (CNS) symptoms or disease, peripheral nervous system (PNS) symptoms and muscular symptoms. In patients with CNS symptoms, the most common complaints were dizziness and headache. In patients with PNS symptoms, the most common complaints were hypogeusia and hyposmia [5]. Muscle injury was defined when a patient had myalgia and elevated serum creatine kinase (CK) level above 200 U/L. The common neurological manifestations of COVID-19 patients are summarized in Table 1 [9].
Table 1.
Neurological manifestations: a summary of published articles.
| Total Patients | Dizziness/Confusion | Headache | Muscle Ache | |
|---|---|---|---|---|
| Xiaobo Yang et al. [13] | 52 | / | 3(6%) | 6(11.5%) |
| Xiao-Wei Xu et al. [14] | 62 | / | 21(34%) | 32(52%) |
| Dawei Wang et al. [15] | 138 | 13(9.4%) | 9(6.5%) | 48 (34.8%) |
| Chaolin Huang et al. [16] | 41 | / | 3/38(8%) | 18(44%) |
| Nanshan Chen et al. [17] | 99 | 9(9%) | 8(8%) | 11(11%) |
| Weijie Guan et al. [9] | 1099 | / | 150(13.6%) | 163(14.8%) |
| De Chang et al. [18] | 13 | / | 3(23.1%) | 3(23.1%) |
| Zhenwei Wang et al. [19] | 4 | 2(50%) | / | / |
| Liu Kui et al. [20] | 137 | / | 13(9.5%) | 44(32.1%) |
| Michael Chuang et al. [21] | 21 | / | 3(14.3%) | 3(14.3%) |
| Feng Pan et al. [22] | 21 | / | / | 5(24%) |
| Fengxiang Song et al. [23] | 51 | 8(16%) | / | 16(31%) |
| Lili Ren et al. [24] | 5 | / | 1(20%) | 3(60%) |
Some patients with conscious disturbance require a head CT examination to exclude acute cerebrovascular disease (i.e., ischemic stroke and cerebral hemorrhage). Older severe patients with elevated D-dimer [9], which is indicative of the consumptive coagulation system, are more likely to have vascular thrombosis, leading to ischemic stroke. SARS-CoV-2 can bind to the ACE2 receptor so the blood pressure of some hypertension patients may elevate abnormally, increasing the risk for cerebral hemorrhage [10, 11]. In NCP patients, symptoms of headache, epilepsy and impaired consciousness could be also investigated [12]. Additionally, symptoms of sore limbs and muscle weakness can be seen in COVID-19 patients. High levels of CK in these patients indicate muscle damage caused by SARS-CoV-2.
3. Transmission Mechanisms of Nervous Systems
Viremia et al discussed the dissemination of the COVID-19 virus SARS-CoV-2 throughout the body via the bloodstream. The neuroinvasive propensity has been demonstrated as a common feature of coronavirus so that neurotropism may occur via circulation, an upper nasal trancribrial route and/or conjunctival route [25-27].
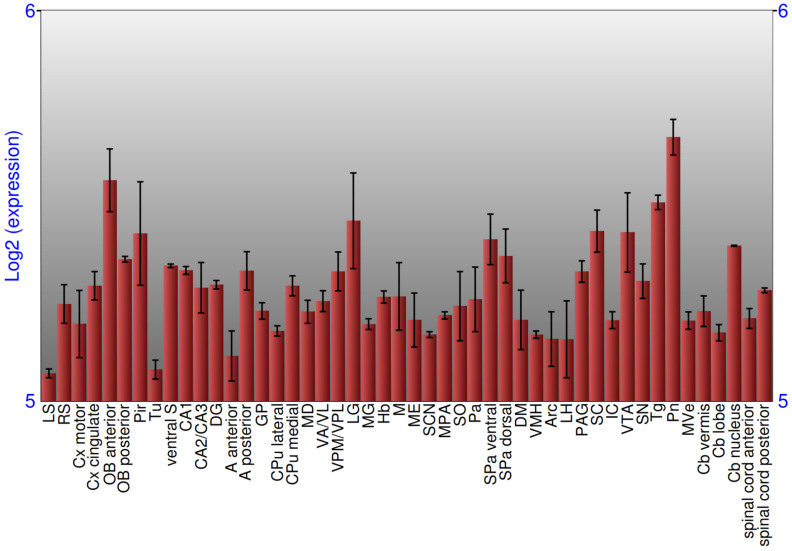
The presence of SARS-CoV-2 in the circulation understandably enables it passing into the cerebral circulation. Patients with SARS have also demonstrated the presence of SARS-CoV in their cerebrospinal fluid, and autopsy findings of such patients have become strong evidence for the viral presence in the brain. The viruses were localized almost exclusively in the neurons, confirming that these viruses can cross the blood-brain barrier and enter the CNS. Once within the milieu of the neuronal tissues, its interaction with ACE2 receptors expressed on the plasma membrane of neurons can initiate a cycle of viral budding accompanied by neuronal damage without substantial inflammation as has been seen with cases of SARS-CoV in the past [25]. ACE2 receptors are targets of SARS-CoV-2 as well [28, 29]. SARS-CoV-2 uses its spike protein S1 that enables the attachment of the virion to the cell membrane by interacting with the host ACE2. The latest study showed that the ACE2 binding affinity for the SARS-CoV-2 spike protein ectodomain was 10 - 20 - fold higher than that of the SARS-CoV [30], partly explaining why COVID-19 has been so highly contagious. Of the note, the brain expresses ACE2 receptors, on glial cells and neurons [25]. The expression of ACE2 in the brain is shown in Fig. 1.
Fig. (1).
Expression of ACE2 in brain. (From BrainStars, http://brainstars.org/probeset/?keyword=ace2). (A higher resolution / colour version of this figure is available in the electronic copy of the article).
Previous studies in transgenic mice revealed that either SARS-CoV [27] or MERS-CoV [31], when given intranasally, could enter the brain, possibly via the olfactory nerves, and thereafter rapidly spread to some specific brain areas such as the brainstem [32]. The spread of SARS-CoV-2 to the brain has been supported by a case with hyposmia and cases with acute respiratory failure in COVID-19 [6]. Additionally, SARS-CoV-2 transmission through the ocular surface was reported. Infectious droplets and body fluids can easily contaminate the human conjunctival epithelium [26].
4. Psychological Influence
Numerous patients have been infected with SARS-CoV-2 since the outbreak of COVID-19 in Wuhan, China. For health-care sectors, dealing with public psychological barriers and performing psychological crisis intervention are an important part of public health interventions. Besides the public, confirmed patients and frontline medical staff were affected to various degrees. The National Health Commission of China has released guidelines for local authorities to promote psychological crisis intervention in related patients, medical personnel, and others under medical observation [33].
4.1. The Public
In order to swiftly contain the spread of SARS-CoV-2, the Chinese government took a firm measure of the entire country quarantined, which has been extreme, astounding and unprecedented [34]. The epidemic brought to people in China and the world not only the risk of death due to the viral infection, but also unbearable psychological pressure which could not be ignored. Quarantine against COVID-19 on the one hand increases the possibility of psychological and mental problems. With interpersonal communication restricted under the introduction of quarantine, depression and anxiety are more likely to occur and worsen. On the other hand, quarantine reduces the availability of timely psychological intervention, and routine psychological counseling is also difficult to carry out in the current situation [35]. As reported on February 14th, 2020, a male patient with common cold committed suicide in India because he suspected he had COVID-19 and was fearing of infecting his family members [36]. A recent survey of the public in China was conducted to understand their levels of psychological impact, anxiety, depression, and stress during the initial stage of the COVID-19 outbreak. The results of the survey indicated that more than a half of the respondents rated themselves with psychological impact as moderate-to-severe and about one-third reported moderate-to-severe anxiety [37].
4.2. Medical Staff
To reduce the medical burden following the outbreak, a large number of medical staff were sent from other provinces to Wuhan city and Hubei province. These healthcare workers are caring for the either severely ill, scared, or lost of beloved but themselves also exposed to the trauma. The challenges and stress they experience could also induce common mental disorders, including anxiety and depressive disorders, and posttraumatic stress disorder [33]. It has been pointed out that a unique feature of some mental health doctors’ work is that through their role as therapists, they are exposed to the description and response of clients to trauma, which may indirectly cause pain and trauma to therapists. This is the proposed phenomenon known as “alternative trauma” or “vicarious traumatization (VT)” [38]. A previous study of VT during COVID-19 control examined frontline nurses engaged in the process of providing care for patients. The results showed that the VT scores for frontline nurses including scores for physiological and psychological responses were significantly worse than those of non-frontline nurses [39]. However, the VT scores for the general public were significantly higher than those of frontline nurses [39]. This study confirmed the psychological influence of COVID-19.
4.3. Confirmed Patients
During disease progression, clinical symptoms become severe and psychological problems in infected patients evolve at the same time [40]. Studies have confirmed that individuals who have experienced public health emergencies still have varying degrees of stress disorders, even after the event is over, or they have been cured and discharged from a hospital [41]. In this way, frontline healthcare workers again become the main personnel providing psychological interventions to patients in hospitals [40].
5. What neurologists need to know
Neurologists should pay more attention to COVID-19 patients with abnormal blood clotting function as a high risk factor of stroke. Head CT and/or MRI should be performed to exclude the symptoms of acute cerebrovascular events and intracranial infection. With symptoms of muscle damage, nutritional support therapy is essential and gamma globulin (15 - 20 g/d, 3 - 5 d) can be used if necessary. Lumbar puncture is feasible for the detection of SARS-CoV-2 in cerebrospinal fluid to help confirm the infectious situation.
Conclusion
For patients with COVID-19, especially those with great severity, there is an urgent need to understand the neurologic manifestations and neurotropic potential of COVID-19 in order to prioritize and individualize the treatment protocols based on particular cases and predominant organ involvement. Neurologists should consider SARS-CoV-2 infection as a differential diagnosis of patients with these neurologic manifestations, to avoid delayed diagnosis or misdiagnosis and ensure prevention of viral transmission. Moreover, psychological intervention measures should be introduced and adapted as appropriate.
Acknowledgements
Declared none.
Consent for Publication
Not applicable.
Funding
This work was supported by grants 2016YFC1306600 and 2018YFC1314700 from the National Key R&D Program of China, grants 81873782 from the National Natural Science Foundation of China, grant 2016CFB624 from Natural Science Foundation of Hubei Province, grant 2017050304010278 from The Youth Science and Technology Morning Light Program of Wuhan City, 2018 Hubei medical research project WJ2019F030, 2018 Wuhan medical research project S201802140011, 2018 Wuhan Young and Middle-aged Medical Talents Program and 2017 Hubei Provincial Party Committee Organization Department the second batch of Hubei youth elite development plan (all to NX).
Conflict of Interest
The authors declare no conflict of interest, financial or otherwise.
References
- 1.Yao X.H., Li T.Y., He Z.C., Ping Y.F., Liu H.W., Yu S.C., Mou H.M., Wang L.H., Zhang H.R., Fu W.J., Luo T., Liu F., Chen C., Xiao H.L., Guo H.T., Lin S., Xiang D.F., Shi Y., Li Q.R., Huang X., Cui Y., Liu X.Z., Tang W., Pan P.F., Huang X.Q., Ding Y.Q., Bian X.W. A pathological report of three COVID-19 cases by minimally invasive autopsies Zhonghua bing li xue za zhi = Chinese J. Pathalogy. 2020;49:E9. doi: 10.3760/cma.j.cn112151-20200312-00193. [DOI] [PubMed] [Google Scholar]
- 2.Wang T., Du Z., Zhu F., Cao Z., An Y., Gao Y., Jiang B. Comorbidities and multi-organ injuries in the treatment of COVID-19. Lancet. 2020;395(10228):e52. doi: 10.1016/S0140-6736(20)30558-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S., Schiergens T.S., Herrler G., Wu N.H., Nitsche A., Müller M.A., Drosten C., Pöhlmann S. SARS-CoV-2 cell entry depends on ace2 and tmprss2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xie X., Zhong Z., Zhao W., Zheng C., Wang F., Liu J. Chest CT for typical 2019-nCoV pneumonia: Relationship to negative rt-pcr testing. Radiology. 2020;296(2):E41–E45. doi: 10.1148/radiol.2020200343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mao L., Jin H., Wang M., Hu Y., Chen S., He Q., Chang J., Hong C., Zhou Y., Wang D., Miao X., Li Y., Hu B. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan. JAMA Neurol. 2020;77(6):683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li Y.C., Bai W.Z., Hashikawa T. The neuroinvasive potential of SARS‐CoV2 may be at least partially responsible for the respiratory failure of COVID‐19 patients. J. Med. Virol. 2020;92(6):552–555. doi: 10.1002/jmv.25728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The Lancet. COVID-19: fighting panic with information. Lancet. 2020;395(10224):537. doi: 10.1016/S0140-6736(20)30379-2. [Editorial]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Depoux A., Martin S., Karafillakis E., Preet R., Wilder-Smith A., Larson H. The pandemic of social media panic travels faster than the COVID-19 outbreak. J. Travel Med. 2020;27(3) doi: 10.1093/jtm/taaa031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X., Liu L., Shan H., Lei C.L., Hui D.S.C., Du B., Li L.J., Zeng G., Yuen K.Y., Chen R.C., Tang C.L., Wang T., Chen P.Y., Xiang J., Li S.Y., Wang J.L., Liang Z.J., Peng Y.X., Wei L., Liu Y., Hu Y.H., Peng P., Wang J.M., Liu J.Y., Chen Z., Li G., Zheng Z.J., Qiu S.Q., Luo J., Ye C.J., Zhu S.Y., Zhong N.S. China medical treatment expert group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang B., Zhou X., Qiu Y., Song Y., Feng F., Feng J., Song Q., Jia Q., Wang J. 2020.
- 11.Huang Y., Yang R., Xu Y., Gong P. 2020.
- 12.Clinical strategies for prevention and treatment neurologist consensus editorial group, corona.c., 2019 clinical prevention and treatment of coronavirus disease (covid-19). Chin. J. Neurol. 2020;•••:e001–e001. [Google Scholar]
- 13.Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H., Wu Y., Zhang L., Yu Z., Fang M., Yu T., Wang Y., Pan S., Zou X., Yuan S., Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 2020;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xu X.W., Wu X.X., Jiang X.G., Xu K.J., Ying L.J., Ma C.L., Li S.B., Wang H.Y., Zhang S., Gao H.N., Sheng J.F., Cai H.L., Qiu Y.Q., Li L.J. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020;368:m606. doi: 10.1136/bmj.m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., Wang B., Xiang H., Cheng Z., Xiong Y., Zhao Y., Li Y., Wang X., Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., Qiu Y., Wang J., Liu Y., Wei Y., Xia J., Yu T., Zhang X., Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chang D., Liu M.G., Wei L., Xie L.X., Zhu G.F., Cruz C.S., Sharm L. Epidemiologic and clinical characteristics of novel coronavirus infections involving 13 patients outside wuhan. JAMA. 2020;323(11):1092–1093. doi: 10.1001/jama.2020.1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang Z., Chen X., Lu Y., Chen F., Zhang W. Clinical characteristics and therapeutic procedure for four cases with 2019 novel coronavirus pneumonia receiving combined Chinese and Western medicine treatment. Biosci. Trends. 2020;14(1):64–68. doi: 10.5582/bst.2020.01030. [DOI] [PubMed] [Google Scholar]
- 20.Liu K., Fang Y.Y., Deng Y., Liu W., Wang M.F., Ma J.P., Xiao W., Wang Y.N., Zhong M.H., Li C.H., Li G.C., Liu H.G. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin. Med. J. (Engl.) 2020;133(9):1025–1031. doi: 10.1097/CM9.0000000000000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chung M., Bernheim A., Mei X., Zhang N., Huang M., Zeng X., Cui J., Xu W., Yang Y., Fayad Z.A., Jacobi A., Li K., Li S., Shan H. CT imaging features of 2019 novel Coronavirus (2019-nCoV). Radiology. 2020;295(1):202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pan F., Ye T., Sun P., Gui S., Liang B., Li L., Zheng D., Wang J., Hesketh R.L., Yang L., Zheng C. Time course of lung changes on chest ct during recovery from 2019 novel coronavirus (COVID-19) Pneumonia. Radiology. 2020;295(3):715–721. doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Song F., Shi N., Shan F., Zhang Z., Shen J., Lu H., Ling Y., Jiang Y., Shi Y. Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295(1):210–217. doi: 10.1148/radiol.2020200274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ren L.L., Wang Y.M., Wu Z.Q., Xiang Z.C., Guo L., Xu T., Jiang Y.Z., Xiong Y., Li Y.J., Li X.W., Li H., Fan G.H., Gu X.Y., Xiao Y., Gao H., Xu J.Y., Yang F., Wang X.M., Wu C., Chen L., Liu Y.W., Liu B., Yang J., Wang X.R., Dong J., Li L., Huang C.L., Zhao J.P., Hu Y., Cheng Z.S., Liu L.L., Qian Z.H., Qin C., Jin Q., Cao B., Wang J.W. Identification of a novel coronavirus causing severe pneumonia in human: a descriptive study. Chin. Med. J. (Engl.) 2020;133(9):1015–1024. doi: 10.1097/CM9.0000000000000722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baig A.M. Khaleeq, A; Ali, U; Syeda, H. Evidence of the COVID-19 Virus targeting the CNS: Tissue distribution, host–virus iInteraction, and proposed neurotropic mechanisms. ACS Chem. Neurosci. 2020;11(7):995–998. doi: 10.1021/acschemneuro.0c00122. [DOI] [PubMed] [Google Scholar]
- 26.Lu C.W., Liu X.F. Jia, Z.F. -nCoV transmission through the ocular surface must not be ignored. Lancet. 2019;395(10224):e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Netland J., Meyerholz D.K., Moore S., Cassell M., Perlman S. Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J. Virol. 2008;82(15):7264–7275. doi: 10.1128/JVI.00737-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.AC W.; YJ, P.; MA, T. A W, AT M, D V. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020;181(2):281–292.e6. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yan R.H., Zhang Y.Y., Li Y.N., Xia L., Guo Y.Y., Zhou Q. Structural basis for the recognition of the SARS-CoV-2 by full-length human ACE2. Science. 2020;367(6485):1444–1448. doi: 10.1126/science.abb2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wrapp D., Wang N., Corbett K.S., Goldsmith J.A., Hsieh C.L., Abiona O., Graham B.S., McLellan J.S. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367(6483):1260–1263. doi: 10.1126/science.abb2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li K., Wohlford-Lenane C., Perlman S., Zhao J., Jewell A.K., Reznikov L.R., Gibson-Corley K.N., Meyerholz D.K., McCray P.B., Jr Middle east respiratory syndrome coronavirus causes multiple organ damage and lethal disease in mice transgenic for human dipeptidyl peptidase 4. J. Infect. Dis. 2016;213(5):712–722. doi: 10.1093/infdis/jiv499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McCray P.B., Jr, Pewe L., Wohlford-Lenane C., Hickey M., Manzel L., Shi L., Netland J., Jia H.P., Halabi C., Sigmund C.D., Meyerholz D.K., Kirby P., Look D.C., Perlman S. Lethal infection of K18-hACE2 mice infected with severe acute respiratory syndrome coronavirus. J. Virol. 2007;81(2):813–821. doi: 10.1128/JVI.02012-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395(10224):e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang Y., Peng F., Wang R., Yange M., Guan K., Jiang T., Xu G., Sun J., Chang C. The deadly coronaviruses: The 2003 SARS pandemic and the 2020 novel coronavirus epidemic in China. J. Autoimmun. 2020;109:102434. doi: 10.1016/j.jaut.2020.102434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xiao C. A Novel Approach of Consultation on 2019 novel coronavirus (COVID-19)-related psychological and mental problems: structured letter therapy. Psychiatry Investig. 2020;17(2):175–176. doi: 10.30773/pi.2020.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. https://news.sina.com.cn/w/2020-02-14/doc-iimxyqvz2844605.shtml
- 37.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sabin-Farrell R., Turpin G. Vicarious traumatization: implications for the mental health of health workers? Clin. Psychol. Rev. 2003;23(3):449–480. doi: 10.1016/S0272-7358(03)00030-8. [DOI] [PubMed] [Google Scholar]
- 39.Li Z., Ge J., Yang M., Feng J., Qiao M., Jiang R., Bi J., Zhan G., Xu X., Wang L., Zhou Q., Zhou C., Pan Y., Liu S., Zhang H., Yang J., Zhu B., Hu Y., Hashimoto K., Jia Y., Wang H., Wang R., Liu C., Yang C. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav. Immun. 2020;88:916–919. doi: 10.1016/j.bbi.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Duan L., Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4):300–302. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cheng S.K., Wong C.W., Tsang J., Wong K.C. Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS). Psychol. Med. 2004;34(7):1187–1195. doi: 10.1017/S0033291704002272. [DOI] [PubMed] [Google Scholar]