Abstract
Suicide is the second leading cause of death for people aged 10–34 years old. Limited research has documented extant heterogeneities in suicide across the life course and among diverse sociodemographic groups. There is also limited research on the influences of mental health utilization on suicidal trajectories across the life course. This study aims to: (1) identify racial/ethnic, sex, sexual orientation, socioeconomic status, and intersectional differences in suicidal trajectories among adolescents transitioning to adulthood; and (2) examine influences of mental health service utilization on disparities in suicidal trajectories. The study included 9421 respondents (Mage = 14.99 [SD = 1.61]) from Waves I–IV National Longitudinal Study of Adolescent to Adult Health (1994–2008). Latent class growth analyses were used to identify trajectories of suicidal ideation and suicide attempts. Multivariate multinomial logistic regression was used to examine the influences of mental health treatment and sociodemographic characteristics on suicidal trajectories. Three suicidal ideation (low-stable, high-decreasing, moderate-decreasing-increasing) and two suicide attempt (low-stable, moderate-decreasing) trajectories were identified. Compared with the low-stable trajectories, the risks of being in high-decreasing suicidal ideation trajectories were higher among females (AOR = 1.45, 95% CI 1.01–2.13) and sexual minorities (AOR = 1.82, 95% CI 1.21–2.74). Sexual minorities (AOR = 2.63, 95% CI 1.69–4.08) and low-SES adolescents (AOR = 1.79, 95% CI 1.08–2.98) were more likely to be in the moderate-decreasing suicide attempt group. Mental health service utilization predicted engagement in high-risk suicidal trajectories. Sociodemographic disparities in suicidal trajectories initiate early and persist over time. Individuals in high-risk trajectories received mental health treatment during adolescence. Suicide prevention should target vulnerable subpopulations and mental health service utilization in the early stage.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10488-021-01122-w.
Keywords: Suicidal trajectories, Suicidal ideation, Suicide attempt, Health disparities, Mental health treatment, Life course
Introduction
Suicide continues to be a serious public health problem (Lindsey et al. 2019; Nock et al. 2019). Suicide ranks as the second leading cause of death for people ages 10–34 years old in the US (Curtin et al. 2016). From a life course perspective, the likelihood of engaging in nonfatal suicide behaviors (i.e., suicide ideation and suicide attempts) vary across developmental stages (Bridge et al. 2018; Lindsey and Xiao 2019; Ruch et al. 2019; Yu and Chen 2019). It is important, therefore, to understand the onset and changing patterns of suicidal behaviors to guide effective suicide preventative efforts (Allan et al. 2019; Czyz and King 2015; Kerr et al. 2013; Shakya et al. 2019).
Existing studies examining suicidal ideation and suicide attempts have mostly focused on estimating the prevalence and risks at specific, static points in time (Allan et al. 2019; Franklin et al. 2017), rather than examining suicidal trajectories from a life course perspective (Rueter et al. 2008; Thompson and Swartout 2018). A single-timepoint approach cannot provide clinicians and researchers with two types of critical information: factors amendable to suicide prevention, and high-risk subgroups who may exhibit different patterns of suicidal ideation and attempts at specific developmental stages (Kerr et al. 2013; Marshal et al. 2013; Rueter et al. 2008; Thompson and Swartout 2018). Existing longitudinal studies, however, are also limited by short follow-up periods (Borowsky et al. 2001; Rueter et al. 2008), geographical generalizability (e.g., beyond state or region; Kerr et al. 2013; Rueter et al. 2008), diversity of sample characteristics (e.g., most were conducted among single category of racial group, patients in clinical settings, or military personnel; Czyz and King 2015; Rueter et al. 2008) and small sample size (Kerr et al. 2013; Rueter et al. 2008). We address this gap by identifying 13-year trajectories of suicidal ideation and suicide attempt among a nationally representative and diverse adolescent sample. Our study contributes to identifying critical risk periods and subpopulations from adolescence to young adulthood in the greatest need for suicide prevention.
During adolescence, higher use of mental health treatment utilization has been shown to associate with the risks of suicide behaviors (McClellan et al. 2020). Most studies, however, were conducted using cross-sectional design (Nock et al. 2013) or followed up over a short term (e.g., 6-month follow up; Moskos et al. 2007). Relatively little is known about the long-term effect of mental health service utilization on the latter development or course of suicidal behaviors. This is noteworthy as recent predictive modeling using intensive ecological momentary assessment found that variability of suicidal trajectories (i.e., changes in suicidal ideation over time) might be trait-like after stressful events and will not manifest risks on suicidal behaviors after at least two years (Oquendo et al. 2020). A prior longitudinal study conducted in rural China found a nonsignificant mental health treatment effect in preventing psychiatric patients from suicide risks after 14 years (Ran et al. 2018). Besides, suicidal adolescents typically enter treatment before rather than after their onset of suicide (55.3–73.2% across suicidal behaviors), while some treatment may not be specific enough to target suicide behaviors (Nock et al. 2013). A longitudinal examination is needed to clarify the influences of early mental health treatment on individual variation in temporal patterns of suicidal ideation and suicide attempts, i.e., whether mental health treatment disrupts suicide trajectories (Mou et al. 2020; Nock et al. 2019; Xiao et al. 2019a, b).
Researchers increasingly suggested disparities in the prevalence and risk of suicide in terms of race/ethnicity, sex, sexual orientation, and socioeconomic status (SES; Bridge et al. 2018; Lindsey et al. 2019; Shakya et al. 2019; Xiao et al. 2019a, b). Such disparities may further differ over time. For example, Black children ages 5–12 had nearly twice the completed suicide rates than their White counterparts, whereas suicide risks were lower among Black adolescents than White adolescents ages 13–17 (Bridge et al. 2018). Sex differences in suicidal behaviors found among adolescents ages 14–17 were not observed for participants ages 18–21 or 22 + years (Wunderlich et al. 2001). Sexual minority youth had a substantially higher level of suicidality than their heterosexual counterparts during early adolescence, and that gap persisted over time (Marshal et al. 2012). Additionally, living in a low SES family was associated with higher risks of suicidal behaviors during adolescence, but not adulthood (Chau et al. 2014; Zaborskis et al. 2016). Extant research, however, fails to address sociodemographic disparities in suicidal trajectories (Alegria et al. 2010). Moreover, with increasing awareness of diversity and inclusion in suicide research (Moutier 2020; Park et al. 2020), growing evidence demonstrates disproportionately and routinely greater risks of suicidal behaviors among individuals with intersecting identities across sex, race/ethnicity, sexual orientation, and socioeconomic status (Liu et al. 2020; Moutier 2020; Mueller et al. 2015). The growing rates of suicide attempts among Black adolescents, for example, were faster among Black girls than their male counterpart. Yet, little is known about how various social identities intersect and affect suicidal trajectories and how intersectionality can guide equity-focused implementation efforts (Aby 2020).
In this study, we identified the trajectories of suicidal ideation and suicide attempts. We further documented the impact of mental health treatment on suicidal trajectories over time. We investigated whether suicidal trajectories differ across sociodemographic characteristics (i.e., racial/ethnic, sex, sexual orientation, SES) and intersectional social identities. Identifying disparities in suicidal trajectories and the influence of early mental health treatment will not only help provide a greater understanding of at-risk critical periods and sub-populations but inform tailored interventions to narrow health disparities in suicidal trajectories (Moutier 2020; Park et al. 2020; Zimmerman and Anderson 2019).
Methods
Study Design and Participants
This study used the restricted-use data from Waves I–IV of the National Longitudinal Study of Adolescent to Adult Health (Add Health), a prospective cohort study using a multistage stratified cluster design to recruit a nationally representative sample from 132 schools associated with 80 communities across the USA (Harris et al. 2019). Wave I in-home survey was completed during the 1994–1995 school year with 20,745 7th–12th-grade students (ages 11–19 years). The adolescents were followed up through four face-to-face surveys, with Wave IV (2007–2008) conducting at ages 24–32 years (Harris 2013; UNC Carolina Population Center 2018).
At-home interviews, conducted at baseline and follow-up, lasted approximately 90 min. Computer-Assisted Personal Interview and Audio Computer-Assisted Self-Interviews were used to respond to a potentially sensitive question, which enhances the quality of self-reporting of sensitive and illegal information (Turner et al. 1998). Written informed consent was obtained from parents when participants were younger than 18 years, or from participants who were 18 years or older. The New York University IRB (IRB-FY2018-1561) approved all procedures to acquire the Add Health dataset.
Procedures
Measures of suicidal ideation and suicide attempts across all four waves were used to identify trajectories of these suicide behavior indices, respectively. Suicidal ideation was assessed by one question with a response option of yes or no: “During the past 12 months, did you ever seriously think about committing suicide?” Suicide attempts were assessed by one item with response options of zero, one, two, three, and four or more: “During the past 12 months, how many times did you attempt suicide?” Answers were dichotomized (zero as no attempt, one as one or more attempts).
Sociodemographic characteristics included non-exclusive categorical measures for race/ethnicity (non-Hispanic White, non-Hispanic Black, Latinx, non-Hispanic Asians, non-Hispanic American Indian or Native American, other, and multiracial), sex (female, male), sexual orientation (sexual minorities, heterosexual), and SES assessed by maternal educational level and receipt of public assistance. A continuous measure of the participant’s age at each wave was included. We further included interaction terms of sociodemographic characteristics to assess intersections across social identities (i.e., race/ethnicity, sex, sexual orientation, SES) to address whether the impact of one factor differed across the level of another (Bridge et al. 2008; Lindsey et al. 2019; Ruch et al. 2019; Sheftall et al. 2016; Xiao 2019).
Mental health treatment during adolescence was assessed using one item at Wave I, which asked participants whether they have received psychological or emotional counseling in the past year. Responses were dichotomized (yes or no).
Given the evidence of depression as a significant risk factor for suicidal behaviors (Cha et al. 2018; Franklin et al. 2017), we included a continuous measure of depression, constructed by the mean scores of a shortened nine-item version of the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff 1977), regarding participants’ experiences in the past week (Cronbach's α = 0.79).
Statistical Analysis
This study carefully adjusted for clustering effects and sampling weights. Preliminary analyses, including identification of and adjustments for missing data using multiple imputation, outliers, and non-normality, were completed. During the analyses, non-linearity, measurement error, moderation effects, statistical power, equivalent models, and specification errors were examined (See Appendix 1 for details on overall consideration and preliminary analysis, Appendix 2 for details on missing data and sensitivity analyses).
Four stages of analyses were conducted. First, before assessing suicidal trajectories, descriptive statistics were computed and reported for suicidal behaviors in each wave and sociodemographic characteristics (e.g., race/ethnicity, sex, sexual orientation, SES). Mean and standard deviation (SD) were used to describe continuous variables (e.g., age). Unweighted frequencies and weighted percentages were used to describe categorical variables (e.g., suicidal behaviors, race/ethnicity, and gender). Rao Scott χ2 tests for weighted data and t-tests were used to examine the cross-sectional relationships between sociodemographic characteristics, depression, and suicidal behaviors at baseline. These analyses were performed using SAS 9.4.
Second, latent class growth analysis (LCGA) was used to characterize the distinct and unobserved subgroups representing varying trajectories of suicidal ideation and likelihood of suicide attempt across four waves (Waves I–IV) and to examine differences in change among these unobserved subgroups. Traditional longitudinal models (e.g., multilevel modeling, random-effect ANOVA, random coefficient modeling, and hierarchical linear modeling) define average estimates of growth trajectories and variance and assume a uniform influence of covariates on the growth trajectories and variance for all individuals (Duncan and Duncan 2009; Raudenbush and Bryk 2002). Therefore, these models assume that all individuals are drawn from a single population characterized by a single set of common parameters (e.g., means, variances, covariances; Ram and Grimm 2009). However, they fail to address the differences between individual subgroups whose growth trajectories are significantly different from the overall estimate. Growth mixture modeling (GMM) allows for exploring differences in growth trajectories across unobserved subpopulations and identifying individual differences in growth trajectories (Muthen and Asparouhov 2008).
LCGA is a special form of a GMM where within-class variances are fixed at zero, implying that all individuals in a particular class are homogeneous (Jung and Wickrama 2008; Nagin 2005). LCGA adopts a person-centered approach, which focuses on the relationships among individuals. By categorizing individuals into distinct groups based on individual response patterns (Muthen and Muthén 2000), LCGA is more effective than traditional longitudinal methods at highlighting changes in and development of behaviors over time (Duncan and Duncan 2009). LCGA is especially suitable for highly skewed and categorical data (Feldman et al. 2009), which are often found in suicide data (e.g., Tidemalm et al. 2008). In this analysis, suicidal behaviors (suicidal ideation and suicide attempts at each time period) were treated as categorical variables to estimate continuous latent intercepts as well as growth patterns for each class (details in Appendix 1).
This analysis followed four steps: (1) problem definition, (2) model specification, (3) model estimation, and (4) model selection and interpretation. Based on the research questions, analysis began with a single-class LCGA model, and then estimated two-, three-, four-, and five- class models (Jung and Wickrama 2008; Ram and Grimm 2009). The number of random starts values was increased several times to assess non-convergence or local maxima (Jung and Wickrama 2008). Our decision for the final model was made based on comparing various statistical indicators and clinical relevance after stepwise increasing the number of classes (Berlin et al. 2013; Curran et al. 2010; Feldman et al. 2009; Jung and Wickrama 2008; Nylund et al. 2007). The final number of trajectories was selected based on conceptual meaning (Xiao et al. 2019a, b), statistical model fit indices (Nylund et al. 2007), entropy (Asparouhov and Muthen 2014) and the smallest estimated class proportions (Nylund et al. 2007). To compare model fit, Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), and adjusted BIC were used. Lower values on AIC and BIC were indicative of better-fitting models (Nagin 1999, 2005; Nylund et al. 2007). Entropy was used to compare how distinctly each model classified individuals into discrete suicidal behavior trajectories, with a value of 0.60 indicating good separation, and higher values till 1.00 suggesting even better separation (Muthen 2004). Latent class models that produced classes with less than 1% of the sample or that did not converge were not considered due to the risk of poor generalizability (Finch and Bolin 2017), given the non-normal distribution of data (Bauer and Curran 2003a). The Lo-Mendell-Rub adjusted likelihood ratio test (LMR-LRT; Lo et al. 2001) was used to test further whether a proposed model with more classes significantly improved model fit relative to a model with fewer classes, indicated by a significant LMR-LRT value. While there is no consensus regarding the smallest size of the latent class (Bollen and Curran 2006; Curran et al. 2010), classes with less than 1% of the population was considered substantially less parsimonious and thus not considered (Agley and Xiao 2020; Geary et al. 2009; Rose et al. 2017; Xiao et al. 2019; Xiao et al. 2020). LCGA analyses were conducted using Mplus version 8 (Muthén and Muthén 1998–2017). During LCGA, full information maximum likelihood (FIML) estimation, a widely accepted approach, was used to handle missing data (Bollen and Curran 2006; Curran and Hussong 2002).
Third, to examine whether individuals’ sociodemographic characteristics predicted suicidal trajectories, bivariate analyses were conducted. We first performed summaries and statistical tests using SAS and compared latent classes (using χ2 tests for categorical variables and t-tests for continuous variables) with respect to sociodemographic characteristics (i.e., sex, race/ethnicity, sexual orientation, SES). Association between categorical variables and suicidal trajectories was assessed using χ2 tests. Analysis of variance (ANOVA) was used to compare sociodemographic differences across suicidal ideation trajectories. Bonferroni correction for multiple comparisons was applied. A series of t-tests were used to compare sociodemographic differences across suicide attempt trajectories.
Fourth, bivariate and multivariate multinomial logistic regression (for suicidal ideation trajectories) and logistic regression (for suicide attempt trajectories) were used to predict the class membership of the identified trajectories. Four steps were conducted, successively: (a) Model 1 adjusted for all sociodemographic variables, including race/ethnicity, sex, sexual orientation, and SES, (b) Model 2 adjusted for sociodemographic characteristics and depression, (c) two-way interactions among sociodemographic variables were included, and (d) three-way interaction terms were examined in each model to investigate the role of intersections across social identities (i.e., race/ethnicity, sex, sexual orientation, SES) in engaging different suicidal trajectories.
We compared classes with respect to mental health service use by bivariate- and multivariable logistic regressions, adjusting for sex, race/ethnicity, sexual orientation, SES. Lastly, we addressed the importance of intersectionality by including the intersection terms between each of the two social identities (i.e., sex, race/ethnicity, sexual orientation, SES). Models were compared using differences in R-squares. These analyses were performed in SAS, adjusting for complex sampling design.
The strategies in the third and fourth stages followed the recommended manual three-step approach (Vermunt 2010) to test for associations between class membership and our covariates of interest, where logits for the classification’s probabilities were used to account for individuals’ likelihood of membership in classes other than their most likely class (King et al. 2020). Significance testing was two-sided and carried out at the 5% significance level. To improve the robustness of our estimation and analyses, we conducted several sensitivity analyses. We conducted sensitivity analyses (e.g., with and without imputed datasets, covariates) and cross-validation through trained subsample and validation subsample (Xiao et al. 2018). Results were consistent. We reported results with imputed datasets, with auxiliary variables adjustment, and the whole sample in the following sections.
Results
There were 9421 respondents who participated in all four waves of data collection (53.15% female, mean age at baseline 14.99 [SD = 1.61], 14.30% sexual minorities, 70.48% White, 16.21% low maternal education, and 26.32% received public assistance, Appendix 3). At baseline, there were 1276 (13.82%) adolescents who thought about suicide, and 366 (4.13%) who reported suicide attempts. Older, sexual minority and low-SES adolescents reported more suicidal ideation. Female and sexual minorities were more likely to attempt suicide (Appendix 3).
The 3-class solution was optimal for suicidal ideation trajectories, and the 2-class solution was optimal for suicide attempt trajectories based on the joint evaluation of fit indices and the conceptual meaning (Table 1). These class solutions were based on the joint evaluation of fit indices and conceptual meaningfulness. Specifically, for suicidal ideation trajectories, the adjusted BIC values were smallest among 3- and 4-class solutions, but the 4-class solution contained one class that contained only 0.62% of the sample, which was too small to be generalizable to a broader population. The nonsignificant LRT statistic, produced by comparing 3-class and 4-class solution, also suggested that there were no statistical differences between 3- and 4-class models, and thus supported rejecting the fourth trajectory. The entropy of the 3-class solution (0.846) also exceeded the criterion for good class separation (i.e., entropy ≥ 0.60). For suicide attempt trajectories, the adjusted BIC was lowest for the 2-class solution, which also produced good class separation (entropy = 0.816) and a generalizable proportion of the sample in each class. Starting with the 3-class solution, all model fit indices increased, and the p-value of the LRT became nonsignificant. Hence, the 2-class solution was selected for the suicide attempt trajectories. For both LCGA models, estimation over five classes produced zero samples in at least one class (e.g., an empty class), and thus, 1- to 4-class solutions were presented. Examination of theoretical cohesiveness also supported the selection of 3-class and 2-class solutions for suicidal ideation and suicide attempts, respectively.
Table 1.
Summary of latent class growth analysis model identification and fit statistics
| No. of classes | AIC | BIC | Adjusted BIC | Smallest class, % | Entropy | LMR-LRT | P |
|---|---|---|---|---|---|---|---|
| Suicidal ideation | |||||||
| 1 | 24,147.4 | 24,333.3 | 24,250.7 | – | – | N/A | N/A |
| 2 | 22,966.8 | 23,174.1 | 23,082.0 | 8.95 | 0.713 | 1156.05 | < 0.001 |
| 3 | 22,892.2 | 23,121.1 | 23,019.4 | 3.42 | 0.846 | 76.85 | 0.13 |
| 4 | 22,870.5 | 23,120.8 | 23,009.5 | 0.83 | 0.881 | 27.36 | 0.05 |
| 5 | 22,875.9 | 23,147.6 | 23,026.9 | 0.00 | 0.800 | 0.21 | 0.45 |
| Suicide attempt | |||||||
| 1 | 9254.1 | 9440.0 | 9357.4 | – | – | N/A | N/A |
| 2 | 8939.3 | 9146.6 | 9054.5 | 2.21 | 0.816 | 306.95 | < 0.001 |
| 3 | 8935.7 | 9164.6 | 9062.9 | 0.71 | 0.870 | 8.99 | 0.49 |
| 4 | 8939.6 | 9189.9 | 9078.7 | 0.06 | 0.900 | 2.05 | 0.60 |
| 5 | 8945.4 | 9217.1 | 9096.4 | 0.04 | 0.902 | 0.21 | 0.58 |
AIC Akaike Information Criterion; BIC Bayesian Information Criteria; Adjusted BIC Sample size adjusted Bayesian Information Criteria; LMR-LRT Lo-Mendell-Rubin adjusted likelihood ratio test. Bolded models were selected
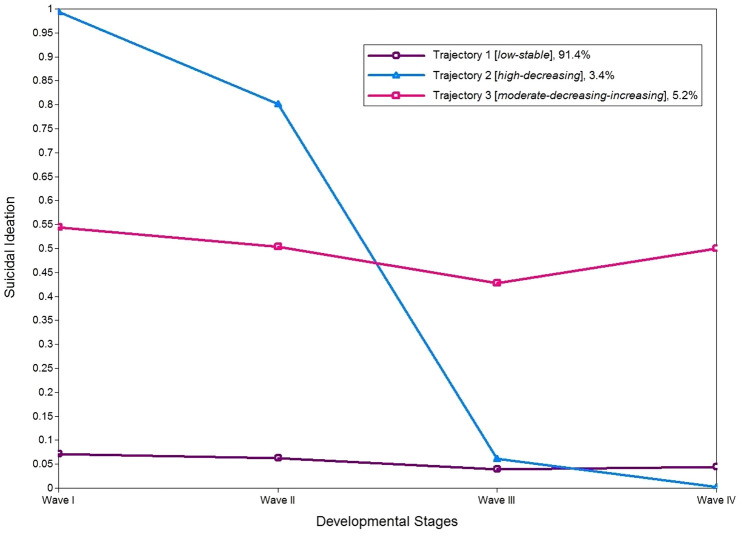
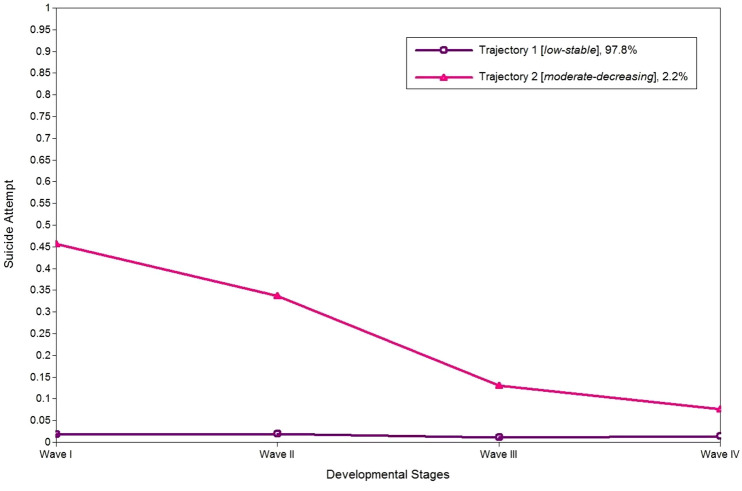
The largest class (Trajectory 1, low-stable, 8608 [91.37%] of 9421), was characterized by participants consistently reporting a low likelihood of suicidal ideation from adolescence to adulthood (Fig. 1). Trajectory 2 (high-decreasing, 322 [3.42%]) consisted of youth reporting a high likelihood of suicidal ideation during early adolescence, followed by a substantial decrease as youth transitioned to emerging adulthood and continued to decrease thereafter. Trajectory 3 (moderate-decreasing-increasing, 491 [5.21%]) included participants reporting a relatively moderate level of suicidal ideation during adolescence (Waves I and II), which decreased when they transitioned to emerging adulthood (Wave III), but then increased again in young adulthood (Wave IV). For suicide attempts trajectories (Fig. 2, most of the sample (9213 [97.79%]) was classified into Trajectory 1 (low-stable) with a consistently low likelihood of attempting suicide across time. Trajectory 2 (moderate-decreasing, 208 [2.21%]) had individuals who indicated a moderate likelihood of attempting suicide during early adolescence but decreased during the transition to adulthood.
Fig. 1.
Trajectories of suicidal ideation likelihood
Fig. 2.
Trajectories of suicide attempt likelihood
Bivariate analyses identified significant differences in the distribution of suicidal trajectories across race/ethnicity, sex, sexual orientation, and SES (Appendix 4). Multivariate multinomial logistic regression showed (Table 2) that for suicidal ideation trajectories, adolescents who were female (Model 1: adjusted odds ratio [AOR] 2.10, 95% confidence interval [CI] 1.46–3.02; Model 2: AOR = 1.45, 95% CI 1.01–2.13), sexual minorities (Model 1: AOR = 1.98, 95% CI 1.35–2.90; Model 2: AOR = 1.82, 95% CI 1.21–2.74), older (Model 1: AOR = 1.12, 95% CI 1.03–1.23), and received mental health treatment (Model 2: AOR = 1.89, 95% CI 1.27–2.84) were significantly more likely to have a high risk of suicidal ideation before emerging adulthood (Trajectory 2, high-decreasing). Sexual minority youth (AOR = 2.86, 95% CI 2.00–4.09) and adolescents receiving mental health treatment (AOR = 2.49, 95% CI 1.82–3.40) were also more likely to have a moderate likelihood of suicidal ideation during adolescence, with an elevated likelihood of experiencing suicidal ideation during the transition to adulthood (Wave III to Wave IV, Trajectory 3, moderate-decreasing-increasing), even after controlling for depression. Across all racial/ethnic groups, Black adolescents were less likely to belong to Trajectory 2 (high-decreasing) and Trajectory 3 (moderate-decreasing-increasing). Adolescents of other races (i.e., non-Hispanic American Indian or Native American, other, and multiracial) were less likely to be in Trajectory 2 (high-decreasing).
Table 2.
Results of the multinomial logistic regression
| Suicidal ideation trajectoriesa | Suicide attempt trajectoriesa | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |||||||||
| Trajectory 2 | Trajectory 3 | Trajectory 2 | Trajectory 3 | Trajectory 2 | Trajectory 2 | |||||||
| (High-decreasing) | (Moderate-decreasing-increasing) | (High-decreasing) | (Moderate-decreasing–increasing) | (Moderate-decreasing) | (Moderate-decreasing) | |||||||
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | |
| Sex | ||||||||||||
| Male | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Female | 2.10 (1.46–3.02) | < 0.001 | 1.03 (0.72–1.48) | 0.86 | 1.45 (1.01–2.12) | 0.05 | 0.83 (0.56–1.21) | 0.33 | 0.80 (0.51–1.25) | 0.32 | 0.50 (0.31–0.80) | .004 |
| Sexual orientation | ||||||||||||
| Heterosexual | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Sexual minority | 1.98 (1.35–2.90) | < 0.001 | 3.02 (2.14–4.27) | < 0.001 | 1.77 (1.17–2.67) | 0.007 | 2.75 (1.91–3.97) | < 0.001 | 2.86 (1.82–4.51) | < 0.001 | 2.46 (1.53–3.97) | < .001 |
| Age (Wave I) | 1.12 (1.03–1.23) | 0.01 | 1.00 (0.93–1.08) | 0.93 | 1.04 (0.95–1.15) | 0.37 | 0.95 (0.88–1.03) | 0.23 | 1.02 (0.90–1.15) | 0.78 | 0.95 (0.83–1.08) | .39 |
| Race/ethnicity | ||||||||||||
| White | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Black | 0.61 (0.39–0.95) | 0.03 | 0.63 (0.43–0.94) | 0.02 | 0.48 (0.30–0.78) | 0.003 | 0.59 (0.40–0.86) | 0.007 | 0.67 (0.33–1.35) | 0.26 | 0.59 (0.27–1.28) | 0.18 |
| Latinx | 1.06 (0.59–1.90) | 0.85 | 0.82 (0.58–1.17) | 0.27 | 0.96 (0.52–1.77) | 0.90 | 0.75 (0.53–1.08) | 0.12 | 1.04 (0.62–1.74) | 0.89 | 0.87 (0.50–1.50) | 0.60 |
| Asian | 1.28 (0.52–3.14) | 0.59 | 0.78 (0.39–1.54) | 0.48 | 1.06 (0.40–2.85) | 0.90 | 0.72 (0.35–1.47) | 0.36 | 0.44 (0.11–1.78) | 0.25 | 0.37 (0.07–1.94) | 0.24 |
| All other race | 0.16 (0.04–0.63) | 0.009 | 0.73 (0.30–1.79) | 0.50 | 0.15 (0.04–0.52) | 0.003 | 0.74 (0.31–1.76) | 0.49 | 0.67 (0.23–1.93) | 0.45 | 0.72 (0.27–1.92) | 0.51 |
| Maternal education | ||||||||||||
| No school/less than high school | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| High school or equivalent | 0.66 (0.42–1.04) | 0.08 | 1.07 (0.73–1.57) | 0.75 | 0.82 (0.52–1.29) | 0.38 | 1.19 (0.79–1.77) | 0.41 | 1.28 (0.77–2.12) | 0.33 | 1.57 (0.92–2.67) | 0.10 |
| Some college | 0.70 (0.35–1.40) | 0.31 | 1.11 (0.66–1.88) | 0.69 | 0.94 (0.46–1.92) | 0.86 | 1.31 (0.76–2.24) | 0.33 | 1.25 (0.61–2.57) | 0.54 | 1.67 (0.81–3.46) | 0.17 |
| Graduate school and higher | 0.82 (0.48–1.40) | 0.47 | 1.02 (0.65–1.59) | 0.94 | 1.23 (0.71–2.12) | 0.45 | 1.24 (0.76–2.02) | 0.39 | 1.08 (0.60–1.95) | 0.79 | 1.46 (0.82–2.61) | 0.19 |
| Public assistance | ||||||||||||
| None | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| At least one | 0.91 (0.62–1.36) | 0.66 | 1.14 (0.85–1.54) | 0.38 | 0.83 (0.57–1.23) | 0.36 | 1.01 (0.74–1.38) | 0.94 | 1.87 (1.14–3.06) | 0.01 | 1.67 (1.01–2.74) | 0.05 |
| Depression | 6.87 (5.23–9.02) | < 0.001 | 3.40 (2.68–4.31) | < 0.001 | 5.83 (4.14–8.21) | < 0.001 | ||||||
| Mental health treatment (W1) | 1.89 (1.27–2.84) | 0.002 | 2.49 (1.82–3.40) | < 0.001 | 3.42 (2.08–5.62) | < 0.001 | ||||||
SI suicidal ideation; SA suicide attempts; OR odds ratio; 95% CI 95% confidence interval.
aReference group = Trajectory 1. W1 = Wave I. ref = reference group
For suicide attempt trajectories (Table 2), sexual minority youth were more likely to be in Trajectory 2 (moderate-decreasing) than Trajectory 1 (low-stable), both before (Model 1: AOR = 2.86, 95% CI 1.82–4.51) and after (Model 2: AOR = 2.63, 95% CI 1.69–4.08) controlling for depression. Adolescents who lived in families receiving public assistance were also more likely to be in Trajectory 2 (moderate-decreasing; Model 1: AOR = 1.87, 95% CI 1.14–3.06; Model 2: AOR = 1.79, 95% CI 1.08–2.98). Receiving mental health treatment was associated with a greater likelihood of being in Trajectory 2 (moderate-decreasing; Model 2: AOR = 3.42, 95% CI 2.08–5.62). Female adolescents, on the other hand, were less likely to be in Trajectory 2 (moderate-decreasing) after controlling for depression (Model 2: AOR = 0.51, 95% CI 0.33–0.81).
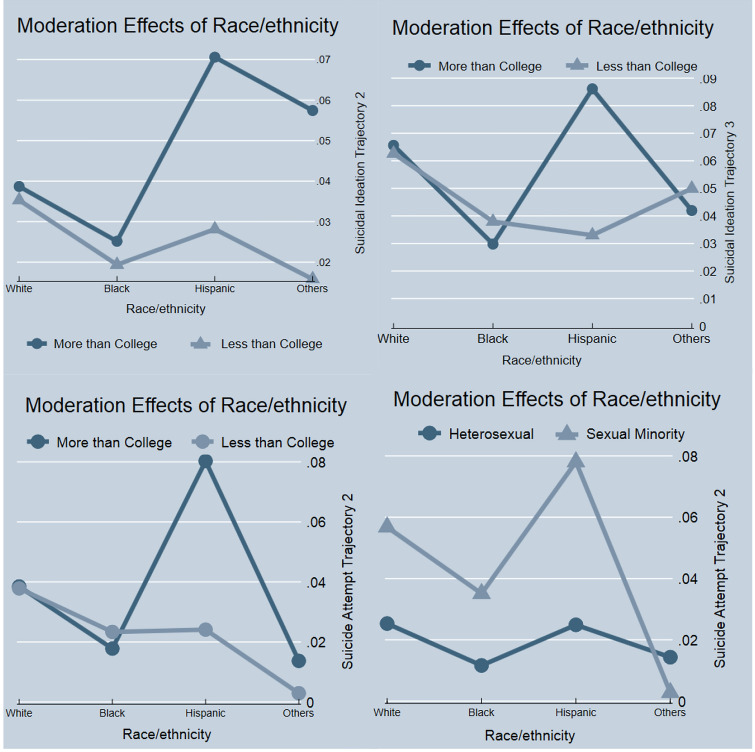
We detected significant two-way interactions across mental health service utilization, race/ethnicity, sexual orientation, and SES (Appendix 5). Compared to Trajectory 1, Black adolescents receiving mental health treatment were 3.41 times (95% CI 1.50–7.80) more likely than White adolescents to be in suicidal ideation Trajectory 3 (moderate-decreasing-increasing). Latinx adolescents with mothers whose highest educational level was less than college were less likely to be in suicidal ideation Trajectory 2 (high-decreasing, AOR = 0.33, 95% CI 0.11–0.96, Fig. 3). Trajectory 3 (moderate-decreasing-increasing, AOR = 0.29, 95% CI 0.14–0.61, Fig. 3). Latinx adolescents with mothers who had less than college-educated were also less likely to be in the suicide attempt Trajectory 2 (moderate-decreasing, AOR = 0.26, 95% CI 0.08–0.78, Fig. 3). Sexual minority adolescents in other racial/ethnic groups (i.e., non-Hispanic American Indian or Native American, other, and multiracial) were less likely to be in Trajectory 2 (moderate-decreasing) of the suicide attempt model (AOR = 0.07, 95% CI 0.01–0.47, Fig. 3). We did not find significant any three-way interactions (e.g., whether Black sexual minorities receiving mental health treatment were more likely to belong to different suicidal trajectories than their White counterparts).
Fig. 3.
Moderation of race/ethnicity on suicidal trajectories
Discussion
This study adds to the body of suicide research by demonstrating the heterogeneity of suicidal trajectories from adolescence to adulthood across sociodemographic characteristics and examining the effect of mental health service utilization. We identified three suicidal ideation trajectories and two suicide attempts trajectories. Receiving mental health treatment was associated with greater odds of being in trajectories showing high risks of suicidal behaviors during adolescence. Sociodemographic and intersectional differences in suicidal trajectories address the health disparities and the potential for more fine-grained risk assessment.
Nock et al. (2013) reported that most suicidal adolescents received mental health treatment, which is in line with our findings that mental health service utilization was significantly associated with being a member of the high-decreasing and moderate-decreasing–increasing suicidal ideation trajectories and moderate-decreasing suicide attempt trajectory. Adolescents with significant levels of psychiatric risk (i.e., reporting suicidal ideation or an attempt), may require mental health treatment, hence the significant association between Wave I mental health service utilization and the suicide behavior trajectories. The decreases in likelihood of suicidal ideation and attempts over time may reflect suicide risk mitigation over time.
Despite evidence of racial/ethnicity, sex, sexual orientation, and SES differences in the prevalence and risk of suicide, few longitudinal studies account for disparities in suicidal trajectories (Needham 2012; Thompson and Swartout 2018). Black adolescents were less likely than other racial/ethnic groups to be categorized in Trajectory 2 (high-decreasing) and Trajectory 3 (moderate-decreasing-increasing). Possible explanations include misclassification (Phillips and Ruth 1993), under-reporting of suicidal ideation due to mistrust of medical and mental health care systems (Shain 2019), and cultural influences on the tendency to “tough-it-out” and hide emotions (Lindsey et al. 2017). For instance, Black adolescents tended to have fewer disclosures of suicidal ideation than their White counterparts (Lindsey et al. 2017; Willis et al. 2003). Lower representation among Black adolescents in the Trajectories 2 and 3 may also be a result that the Add Health baseline sample recruited only students attending high schools. Since Black adolescents had a higher dropout rate than their White counterparts (Rose et al. 2017), those at risk of suicidal ideation (e.g., those experiencing adverse childhood experiences, poverty, racial discrimination; Bridge et al. 2008; Joe et al. 2008; Lindsey et al. 2019) may not be included in the sample.
Our study further identified that Black individuals who received mental health treatment reported a greater likelihood of being in moderate-decreasing–increasing suicidal ideation group. One explanation might be that mental health service utilization increased the likelihood among Black adolescents to report suicidal behaviors or experience higher surveillance of their psychiatric needs via their receipt of treatment (Scott et al. 2007). Conversely, this finding might suggest that the effects of treatment might dissipate over the long term, particularly if early treatment utilization was uneven in terms of attendance or questionable in terms of quality, which has been reported elsewhere among Blacks transitioning to adulthood (Munson et al. 2012). Future research is warranted to determine the risks and tailored interventions to address suicide behaviors among transition-age and young adult Blacks (Davis 2003).
Females were more likely to be in a high-decreasing suicidal ideation trajectory (Trajectory 2). One potential explanation is female adolescents tend to mature earlier, both emotionally and cognitively (Goddings et al. 2014; Yu and Chen 2019) and report greater susceptibility to cyberbully, particularly through social media (Livingstone 2018; Xiao 2019; Xiao et al. 2019). These risk factors could contribute to the early initiation of and changes in suicidal behaviors (Callina et al. 2017; Cha et al. 2018). Future research should investigate more age-related risk factors associated with the widening gap in suicidal ideation and attempts across sex (Bridge et al. 2008; Lindsey et al. 2019; Ruch et al. 2019; Sheftall et al. 2016).
Sexual minorities were more likely to be in the moderate or high suicidal ideation and suicide attempt trajectories (Trajectories 2 and 3), which is consistent with previous studies (Marshal et al. 2013; Nkansah-Amankra 2013). Our results add to a growing body of research documenting the temporal changes of suicidal behaviors from a life course perspective (Liu et al. 2020). Sexual minority youth experienced higher-risk suicidal trajectories than their heterosexual counterparts starting from early adolescence. We identified a subgroup with an alarming relapse of suicidal ideation when transitioning from adolescence to young adulthood. Minority stressors (Meyer 2003) and structural stigma (Hatzenbuehler 2009) are particularly relevant to the sexual disparities in suicidal trajectories and deserve more attention to improve health equity in the suicide prevention agenda (Baiden et al. 2020; Hatzenbuehler 2009). Innovative and peer-led gatekeeper suicide prevention programs (e.g., “A Promise for Tomorrow” gatekeeper program) are encouraged to improve service utilization (Totura et al. 2019).
Adolescents living in low SES families (i.e., receiving public assistance) had greater odds of being in suicide attempt Trajectory 2 (moderate-decreasing). Previous cross-sectional studies found that insufficient family income was a risk factor for higher suicidal ideation and suicide attempts among early adolescents (ages 11–15 years), but not among adults (Chau et al. 2014; Zaborskis et al. 2016). Receiving public assistance may be associated with low social support and high family stress among adolescents transitioning to adulthood (Spirito et al. 2003).
Examining intersectionality in suicidal trajectories provided more nuanced information to understand health disparities. Latinx adolescents with lower SES (lower maternal educational level, in particular) were more likely to report consistently low risks of suicidal ideation and attempts over time. Cultural factors such as familism (i.e., high commitment and loyalty to family) may protect against the negative effect of living in low SES families for Latinx participants (Oscos-Sanchez et al. 2010; Peña et al. 2011). For example, Latinx adolescents may still experience the protective effects of high family cohesion and parental closeness while living in low-SES families compared to other racial/ethnic groups (Xiao and Lu 2019a).
Our results point to the need for future work to improve the long-term effect of mental health treatment with greater attention to the social determinants of health, especially in early adolescence and in the transition to adulthood (Xiao and Lu 2019b; Xiao et al. 2019), especially regarding the mental health treatment experiences of Blacks (Lindsey et al. 2019; Nock et al. 2013). It is also important to engage diversity and inclusion. Integrating mental health into primary care settings and school mental health programs, as well as providing mandatory suicidal risk screening in schools, could facilitate better monitoring of at-risk subpopulations and provision of timely interventions (Gadomski et al. 2015). Reducing the stigma of mental health help-seeking, particularly for minority individuals from culturally diverse backgrounds, could significantly increase public awareness and help-seeking behaviors among vulnerable populations (Batterham et al. 2013). Hence, multilevel intervention approaches, such as combining broad public health campaigns using mass media and gatekeeper training, could improve the effectiveness of suicide prevention initiatives (Li et al. 2021; Niederkrotenthaler et al. 2014; Xiao et al. 2019; Xiao et al. 2021). Additionally, for sexual minority youth, peer gatekeeping programs through social networks, such as the Trevor Project, are encouraged (Gould et al. 2012).
Our study has limitations. First, our measures were self-reported, adolescents may underreport or over-report suicidal behaviors due to social desirability (Miotto and Preti 2008), and there may be measurement bias (Howard 1980), despite the previously established reliability and validity of Add Health measures (Chen and Chantala 2014). Second, this study focused on suicidal ideation and suicide attempts instead of completed suicide. Third, the Add Health data use standard race/ethnic categories, which may mask within-group race/ethnic heterogeneity. Fourth, we assessed suicidal behaviors in longer intervals rather than shorter time intervals (e.g., weeks, months), which may limit the generalizability of changes in suicidal behaviors in short transition periods. Fifth, Add Health collected data from students who attended school, and thus, adolescents who dropped out of high school, were homeless, or who ran away from home are at increased risk of having suicidal behaviors but may not be included (Daniel et al. 2006). Sixth, although LCGA is a robust statistical method, misclassification and possible over-extraction may occur (Bauer and Curran 2003b). We considered missing data, comprehensive lists of indicators for model selection, trained-calibration approach, and practical implications. Future studies are suggested to utilize different nationally representative samples with larger sample sizes to examine the replicability. Seventh, we did not have data about type, amount, or quality of mental health care. Future research should assess and examine the impact of mental health services with detailed information. Finally, Add Health data were collected between 1994 and 2008. Add Health is the only nationally representative longitudinal dataset; however, that contains the measurement of suicidal behaviors over developmental stages. Further, while the prevalence of suicidal behaviors may change over time, the changes in suicidal behaviors over developmental stages may be similar. Thus, our findings are still relevant to the current suicide research agenda.
Conclusion
During the past two decades, one of the overarching goals of Healthy People 2020 has focused on health disparities (U.S. Department of Health and Human Services, 2014). Racial/ethnic, sex, sexual orientation, and SES disparities, however, remain evident in suicidal trajectories over time. Understanding the relations among sociodemographic characteristics and risks of suicidal behaviors over time is critical, not only for reducing suicidal behaviors during adolescence but also for developing effective suicide intervention and prevention programs that are developmentally sensitive and culturally tailored to address the unique needs among high-risk subpopulations.
This study suggests no single suicide prevention policy can effectively address all individuals in need (Alegria et al. 2010). The long-term effect of mental health treatment calls for early connections to treatment among adolescents exhibiting suicide behavior risks as an effective strategy of suicide prevention. Clinicians can identify suicide trajectories by asking their patients and clients about prior history of suicidal behaviors and using screening instruments during early adolescence. Given the possible relapse of suicidal ideation in emerging adults, understanding each distinct trajectory may facilitate more effective clinical screening and treatment.
Our results further suggest a need for a new research agenda to address health disparities in suicidal trajectories at the individual, school, and neighborhood levels. Structural interventions at the policy level are needed to address the racial/ethnic, sex, sexual orientation, and SES disparities in suicidal trajectories. To improve health equity, community structural factors that affect the availability, accessibility, affordability, and acceptability of mental health services should be addressed (Park et al. 2020). Given the little evidence effectiveness of existing curriculum-based suicide prevention programs at the school levels among minority students (Garland et al. 1989; Shaffer et al. 1991; Vieland et al. 1991), suicide research and intervention addressing the health disparities and social determinants of health are encouraged. Future preventative efforts should be multimodal, evidence-based, hypothesis-guided, implemented with sufficient population size, and consider efficient case identification with individualized evaluation (Mann et al. 2005; Shaffer et al. 1990). Incorporating technology to provide behavioral health services (e.g., app-based interventions, videoconferencing), particularly during periods with restricted personal contact such as the COVID-19 pandemic, also holds promise in addressing access-related barriers and improving assessment, diagnosis, and treatment of predisposing factors of suicide among vulnerable youth (Toscos et al. 2019).
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
The authors did not receive support from any organization for the submitted work.
Compliance with Ethical Standards
Conflict of interest
The authors have no financial or proprietary interests in any material discussed in this article.
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Research Involving Human Rights
The current study was not categorized as human subjects research because the data were completely de-identified at the time of study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Aby MJ. Race and equity in statewide implementation programs: An application of the policy ecology of implementation framework. Administration and Policy in Mental Health and Mental Health Services Research. 2020;47(6):946–960. doi: 10.1007/s10488-020-01033-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agley J, Xiao Y. Misinformation about COVID-19: Evidence for differential latent profiles and a strong association with trust in science. BMC Public Health. 2020;21(1):1–12. doi: 10.1186/s12889-020-10103-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Atkins M, Farmer E, Slaton E, Stelk W. One size does not fit all: taking diversity, culture and context seriously. Administration and Policy in Mental Health and Mental Health Services Research. 2010;37(1–2):48–60. doi: 10.1007/s10488-010-0283-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allan NP, Gros DF, Lancaster CL, Saulnier KG, Stecker T. Heterogeneity in short-term suicidal ideation trajectories: Predictors of and projections to suicidal behavior. Suicide and Life-Threatening Behavior. 2019;49(3):826–837. doi: 10.1111/sltb.12480. [DOI] [PubMed] [Google Scholar]
- Asparouhov T, Muthen B. Auxiliary variables in mixture modeling: Three-step approaches using Mplus. Structural Equation Modeling: A Multidisciplinary Journal. 2014;21(3):329–341. doi: 10.1080/10705511.2014.915181. [DOI] [Google Scholar]
- Baiden P, Xiao Y, Asiedua-Baiden G, LaBrenz CA, Boateng GO, Graaf G, Muehlenkamp JJ. Sex differences in the association between sexual violence victimization and suicidal behaviors among adolescents. Journal of Affective Disorders Reports. 2020;1:100011. doi: 10.1016/j.jadr.2020.100011. [DOI] [Google Scholar]
- Batterham PJ, Calear AL, Christensen H. Correlates of suicide stigma and suicide literacy in the community. Suicide and Life-Threatening Behavior. 2013;43(4):406–417. doi: 10.1111/sltb.12026. [DOI] [PubMed] [Google Scholar]
- Bauer DJ, Curran PJ. Distributional assumptions of growth mixture models: Implications for overextraction of latent trajectory classes. Psychological Methods. 2003;8(3):338–363. doi: 10.1037/1082-989x.8.3.338. [DOI] [PubMed] [Google Scholar]
- Bauer DJ, Curran PJ. Overextraction of latent trajectory classes: Much ado about nothing? Reply to Rindskopf (2003), Muthén (2003), and Cudeck and Henly (2003) Psychological Methods. 2003;8(3):384–393. doi: 10.1037/1082-989X.8.3.384. [DOI] [PubMed] [Google Scholar]
- Berlin KS, Parra GR, Williams NA. An introduction to latent variable mixture modeling (part 2): Longitudinal latent class growth analysis and growth mixture models. Journal of Pediatric Psychology. 2013;39(2):188–203. doi: 10.1093/jpepsy/jst085. [DOI] [PubMed] [Google Scholar]
- Bollen KA, Curran PJ. Latent curve models: A structural equation perspective. Hoboken, NJ: Wiley; 2006. pp. 1–293. [Google Scholar]
- Borowsky IW, Ireland M, Resnick MD. Adolescent suicide attempts: Risks and protectors. Pediatrics. 2001;107(3):485–493. doi: 10.1542/peds.107.3.485. [DOI] [PubMed] [Google Scholar]
- Bridge JA, Greenhouse JB, Weldon AH, Campo JV, Kelleher KJ. Suicide trends among youths aged 10 to 19 years in the United States, 1996–2005. JAMA. 2008;300(9):1025–1026. doi: 10.1001/jama.300.9.1025. [DOI] [PubMed] [Google Scholar]
- Bridge JA, Horowitz LM, Fontanella CA, et al. Age-related racial disparity in suicide rates among US youths from 2001 through 2015. JAMA Pediatrics. 2018;172(7):697–699. doi: 10.1001/jamapediatrics.2018.0399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callina KS, Johnson SK, Tirrell JM, Batanova M, Weiner MB, Lerner RM. Modeling pathways of character development across the first three decades of life: An application of integrative data analysis techniques to understanding the development of hopeful future expectations. Journal of Youth and Adolescence. 2017;46(6):1216–1237. doi: 10.1007/s10964-017-0660-1. [DOI] [PubMed] [Google Scholar]
- Cha CB, Franz PJ, Guzmán ME, Glenn CR, Kleiman EM, Nock MK. Annual research review: Suicide among youth—Epidemiology, (potential) etiology, and treatment. Journal of Child Psychology and Psychiatry. 2018;59(4):460–482. doi: 10.1111/jcpp.12831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chau K, Kabuth B, Chau N. Gender and family disparities in suicide attempt and role of socioeconomic, school, and health-related difficulties in early adolescence. BioMed Research International. 2014 doi: 10.1155/2014/314521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, P., & Chantala, K. (2014). Guidelines for analyzing Add Health data. Chapel Hill: Carolina Population Center, University of North Carolina. Retrieved from http://www.cpc.unc.edu/projects/addhealth/documentation/guides/wt_guidelines_20161213.pdf
- Curran PJ, Hussong AM. Structural equation modeling of repeated measures data: Latent curve analysis. In: Moskowitz DS, Hershberger SL, editors. Multivariate applications book series. Modeling intraindividual variability with repeated measures data: Methods and applications. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2002. pp. 59–85. [Google Scholar]
- Curran PJ, Obeidat K, Losardo D. Twelve frequently asked questions about growth curve modeling. Journal of Cognition and Development. 2010;11(2):121–136. doi: 10.1080/15248371003699969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtin SC, Warner M, Hedegaard H. Increase in suicide in the United States, 1999–2014. NCHS Data Brief. 2016;241:1–8. [PubMed] [Google Scholar]
- Czyz EK, King CA. Longitudinal trajectories of suicidal ideation and subsequent suicide attempts among adolescent inpatients. Journal of Clinical Child and Adolescent Psychology. 2015;44(1):181–193. doi: 10.1080/15374416.2013.836454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniel SS, Walsh AK, Goldston DB, Arnold EM, Reboussin BA, Wood FB. Suicidality, school dropout, and reading problems among adolescents. Journal of Learning Disabilities. 2006;39(6):507–514. doi: 10.1177/00222194060390060301. [DOI] [PubMed] [Google Scholar]
- Davis M. Addressing the needs of youth in transition to adulthood. Administration and Policy in Mental Health and Mental Health Services Research. 2003;30(6):495–509. doi: 10.1023/A:1025027117827. [DOI] [PubMed] [Google Scholar]
- Duncan TE, Duncan SC. The ABC’s of LGM: An introductory guide to latent variable growth curve modeling. Social and Personality Psychology Compass. 2009;3(6):979–991. doi: 10.1111/j.1751-9004.2009.00224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman BJ, Masyn KE, Conger RD. New approaches to studying problem behaviors: A comparison of methods for modeling longitudinal, categorical adolescent drinking data. Developmental Psychology. 2009;45(3):652–676. doi: 10.1037/a0014851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch H, Bolin J. Multilevel modeling using Mplus. Boca Raton, FL: CRC Press; 2017. [Google Scholar]
- Franklin, J. C., Ribeiro, J. D., Fox, K. R., Bentley, K. H., Kleiman, E. M., Huang, X., … Nock, M. K. (2017). Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychological Bulletin, 143(2), 187–232. https://doi.org/10.1037/bul0000084 [DOI] [PubMed]
- Gadomski, A. M., Fothergill, K. E., Larson, S., Wissow, L. S., Winegrad, H., Nagykaldi, Z. J., … Roter, D. L. (2015). Integrating mental health into adolescent annual visits: Impact of previsit comprehensive screening on within-visit processes. Journal of Adolescent Health, 56(3), 267–273. [DOI] [PMC free article] [PubMed]
- Garland ANN, Shaffer D, Whittle B. A national survey of school-based, adolescent suicide prevention programs. Journal of the American Academy of Child and Adolescent Psychiatry. 1989;28(6):931–934. doi: 10.1097/00004583-198911000-00019. [DOI] [PubMed] [Google Scholar]
- Geary DC, Bailey DH, Littlefield A, Wood P, Hoard MK, Nugent L. First-grade predictors of mathematical learning disability: A latent class trajectory analysis. Cognitive Development. 2009;24(4):411–429. doi: 10.1016/j.cogdev.2009.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goddings A-L, Dumontheil I, Blakemore S-J, Viner R. The relationship between pubertal status and neural activity during risky decision-making in male adolescents. Journal of Adolescent Health. 2014;54(2):S84–S85. doi: 10.1016/j.jadohealth.2013.10.182. [DOI] [Google Scholar]
- Gould MS, Munfakh JL, Kleinman M, Lake AM. National suicide prevention lifeline: enhancing mental health care for suicidal individuals and other people in crisis. Suicide and Life-Threatening Behavior. 2012;42(1):22–35. doi: 10.1111/j.1943-278X.2011.00068.x. [DOI] [PubMed] [Google Scholar]
- Harris, K. M. (2013). The add health study: Design and accomplishments. Chapel Hill, NC. Retrieved from https://www.cpc.unc.edu/projects/addhealth/documentation/guides/DesignPaperWave_IIV.pdf
- Harris KM, Halpern CT, Whitsel EA, Hussey JM, Killeya-Jones LA, Tabor J, Dean SC. Cohort Profile: The national longitudinal study of adolescent to adult health (add health) International Journal of Epidemiology. 2019;48(5):1415–1415k. doi: 10.1093/ije/dyz115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML. How does sexual minority stigma "get under the skin"? A psychological mediation framework. Psychological Bulletin. 2009;135(5):707–730. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard GS. Response-shift bias: A problem in evaluating interventions with pre/post self-reports. Evaluation Review. 1980;4(1):93–106. doi: 10.1177/0193841X8000400105. [DOI] [Google Scholar]
- Joe S, Canetto SS, Romer D. Advancing prevention research on the role of culture in suicide prevention. Suicide and Life-Threatening Behavior. 2008;38(3):354–362. doi: 10.1521/suli.2008.38.3.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung T, Wickrama K. An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass. 2008;2(1):302–317. doi: 10.1111/j.1751-9004.2007.00054.x. [DOI] [Google Scholar]
- Kerr DCR, Reinke WM, Eddy JM. Trajectories of depressive symptoms and externalizing behaviors across adolescence: Associations with histories of suicide attempt and ideation in early adulthood. Suicide and Life-Threatening Behavior. 2013;43(1):50–66. doi: 10.1111/j.1943-278X.2012.00127.x. [DOI] [PubMed] [Google Scholar]
- King, C. A., Brent, D., Grupp-Phelan, J., Shenoi, R., Page, K., Mahabee-Gittens, E. M., … Casper, T. C. (2020). Five profiles of adolescents at elevated risk for suicide attempts: Differences in mental health service use. Journal of the American Academy of Child and Adolescent Psychiatry, 59(9), 1058–1068.e1055. https://doi.org/10.1016/j.jaac.2019.10.015 [DOI] [PMC free article] [PubMed]
- Li, H., Han, Y., Xiao, Y., Liu, X., Li, A., & Zhu, T. (2021). Suicidal ideation risk and socio-cultural factors in China: A longitudinal study on social media from 2010 to 2018. International Journal of Environmental Research and Public Health, 18(3), 1098. Retrieved from https://www.mdpi.com/1660-4601/18/3/1098 [DOI] [PMC free article] [PubMed]
- Lindsey MA, Brown DR, Cunningham M. Boys do (n’t) cry: Addressing the unmet mental health needs of African American boys. American Journal of Orthopsychiatry. 2017;87(4):377. doi: 10.1037/ort0000198. [DOI] [PubMed] [Google Scholar]
- Lindsey, M. A., Sheftall, A. H., Xiao, Y., & Joe, S. (2019). Trends of suicidal behaviors among high school students in the United States: 1991–2017. Pediatrics, e20191187. doi:10.1542/peds.2019-1187 [DOI] [PMC free article] [PubMed]
- Lindsey MA, Xiao Y. Depression, trauma, and suicide among adolescent and young adult males. In: Griffith DM, Bruce MA, Thorpe RJ Jr, editors. Men’s health equity: A handbook. New York, NY: Routledge; 2019. [Google Scholar]
- Liu RT, Walsh RF, Sheehan AE, Cheek SM, Carter SM. Suicidal ideation and behavior among sexual minority and heterosexual youth: 1995–2017. Pediatrics. 2020 doi: 10.1542/peds.2019-2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingstone S. iGen: Why today’s super-connected kids are growing up less rebellious, more tolerant, less happy–and completely unprepared for adulthood. New York, NY: Taylor & Francis; 2018. [Google Scholar]
- Lo YT, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001;88(3):767–778. doi: 10.1093/biomet/88.3.767. [DOI] [Google Scholar]
- Mann, J. J., Apter, A., Bertolote, J., Beautrais, A., Currier, D., Haas, A., … Marusic, A. (2005). Suicide prevention strategies: A systematic review. JAMA, 294(16), 2064–2074. https://doi.org/10.1001/jama.294.16.2064 [DOI] [PubMed]
- Marshal MP, Dermody SS, Cheong J, Burton CM, Friedman MS, Aranda F, Hughes TL. Trajectories of depressive symptoms and suicidality among heterosexual and sexual minority youth. Journal of Youth and Adolescence. 2013;42(8):1243–1256. doi: 10.1007/s10964-013-9970-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal, M. P., King, K. M., Stepp, S. D., Hipwell, A., Smith, H., Chung, T., … Markovic, N. (2012). Trajectories of alcohol and cigarette use among sexual minority and heterosexual girls. Journal of Adolescent Health, 50(1), 97–99. https://doi.org/10.1016/j.jadohealth.2011.05.008 [DOI] [PMC free article] [PubMed]
- McClellan C, Ali MM, Mutter R. Impact of mental health treatment on suicide attempts. The Journal of Behavioral Health Services & Research. 2020 doi: 10.1007/s11414-020-09714-4. [DOI] [PubMed] [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129(5):674. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miotto P, Preti A. Suicide ideation and social desirability among school-aged young people. Journal of Adolescence. 2008;31(4):519–533. doi: 10.1016/j.adolescence.2007.08.004. [DOI] [PubMed] [Google Scholar]
- Moskos MA, Olson L, Halbern SR, Gray D. Utah youth suicide study: Barriers to mental health treatment for adolescents. Suicide and Life-Threatening Behavior. 2007;37(2):179–186. doi: 10.1521/suli.2007.37.2.179. [DOI] [PubMed] [Google Scholar]
- Mou D, Kleiman EM, Nock MK. Proposed directions for suicide research: Incorporating successful approaches from other disciplines. The British Journal of Psychiatry. 2020 doi: 10.1192/bjp.2020.58. [DOI] [PubMed] [Google Scholar]
- Moutier C. Suicide prevention in the COVID-19 era: Transforming threat into opportunity. JAMA Psychiatry. 2020 doi: 10.1001/jamapsychiatry.2020.3746. [DOI] [PubMed] [Google Scholar]
- Mueller AS, James W, Abrutyn S, Levin ML. Suicide ideation and bullying among US adolescents: Examining the intersections of sexual orientation, gender, and race/ethnicity. American Journal of Public Health. 2015;105(5):980–985. doi: 10.2105/AJPH.2014.302391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munson MR, Jaccard J, Smalling SE, Kim H, Werner JJ, Scott LD. Static, dynamic, integrated, and contextualized: A framework for understanding mental health service utilization among young adults. Social Science & Medicine. 2012;75(8):1441–1449. doi: 10.1016/j.socscimed.2012.05.039. [DOI] [PubMed] [Google Scholar]
- Muthen B. Latent variable analysis: Growth mixture modeling and related techniques for longitudinal data. In: Kaplan D, editor. The Sage handbook of quantitative methodology for the social sciences. Newbury Park, CA: Sage Publications; 2004. pp. 345–368. [Google Scholar]
- Muthen B, Asparouhov T. Growth mixture modeling: Analysis with non-Gaussian random effects. In: Fitzmaurice G, Davidian M, Verbeke G, Molenberghs G, editors. Longitudinal data analysis. Boca Raton, FL: Chapman and Hall/CRC Press; 2008. pp. 143–165. [Google Scholar]
- Muthen B, Muthén LK. Integrating person-centered and variable-centered analyses: Growth mixture modeling with latent trajectory classes. Alcoholism: Clinical and Experimental Research. 2000;24(6):882–891. doi: 10.1111/j.1530-0277.2000.tb02070.x. [DOI] [PubMed] [Google Scholar]
- Muthén, L. K., & Muthén, B. O. (1998–2017). Mplus User's Guide (8th ed.). Los Angeles, CA: Muthén & Muthén
- Nagin DS. Analyzing developmental trajectories: A semiparametric, group-based approach. Psychological Methods. 1999;4(2):139–157. doi: 10.1037//1082-989x.4.2.139. [DOI] [PubMed] [Google Scholar]
- Nagin DS. Group-based modeling of development. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- Needham BL. Sexual attraction and trajectories of mental health and substance use during the transition from adolescence to adulthood. Journal of Youth and Adolescence. 2012;41(2):179–190. doi: 10.1007/s10964-011-9729-4. [DOI] [PubMed] [Google Scholar]
- Niederkrotenthaler T, Reidenberg DJ, Till B, Gould MS. Increasing help-seeking and referrals for individuals at risk for suicide by decreasing stigma: The role of mass media. American Journal of Preventive Medicine. 2014;47(3):S235–S243. doi: 10.1016/j.amepre.2014.06.010. [DOI] [PubMed] [Google Scholar]
- Nkansah-Amankra S. Adolescent suicidal trajectories through young adulthood: Prospective assessment of religiosity and psychosocial factors among a population-based sample in the United States. Suicide and Life-Threatening Behavior. 2013;43(4):439–459. doi: 10.1111/sltb.12029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, Kessler RC. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70(3):300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Ramirez F, Rankin O. Advancing our understanding of the who, when, and why of suicide risk. JAMA Psychiatry. 2019;76(1):11–12. doi: 10.1001/jamapsychiatry.2018.3164. [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal. 2007;14(4):535–569. doi: 10.1080/10705510701575396. [DOI] [Google Scholar]
- Oquendo, M. A., Galfalvy, H. C., Choo, T.-H., Kandlur, R., Burke, A. K., Sublette, M. E., … Stanley, B. H. (2020). Highly variable suicidal ideation: A phenotypic marker for stress induced suicide risk. Molecular Psychiatry. https://doi.org/10.1038/s41380-020-0819-0 [DOI] [PMC free article] [PubMed]
- Oscos-Sanchez MA, Lesser J, Berndt A, Oscos-Flores LD, Pineda D, Tinitigan M, Tran A. Exposure to community violence, male privilege, depression, and familismo are correlates of substance use among high-risk Latino youth. Journal of Adolescent Health. 2010;46(2):S61–S62. [Google Scholar]
- Park KY, Chaiet SR, Greenberg CC. Diversity and inclusion—One size does not fit all. JAMA Surgery. 2020;155(1):30–31. doi: 10.1001/jamasurg.2019.4082. [DOI] [PubMed] [Google Scholar]
- Peña JB, Kuhlberg JA, Zayas LH, Baumann AA, Gulbas L, Hausmann-Stabile C, Nolle AP. Familism, family environment, and suicide attempts among Latina youth. Suicide and Life-Threatening Behavior. 2011;41(3):330–341. doi: 10.1111/j.1943-278X.2011.00032.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips DP, Ruth TE. Adequacy of official suicide statistics for scientific research and public policy. Suicide and Life-Threatening Behavior. 1993;23(4):307–319. [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Ram N, Grimm KJ. Methods and measures: Growth mixture modeling: A method for identifying differences in longitudinal change among unobserved groups. International Journal of Behavioral Development. 2009;33(6):565–576. doi: 10.1177/0165025409343765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ran, M.-S., Xiao, Y., Chui, C. H. K., Hu, X.-Z., Yu, Y.-H., Peng, M.-M., … Chan, C. L.-W. (2018). Duration of untreated psychosis (DUP) and outcome of people with schizophrenia in rural China: 14-year follow-up study. Psychiatry Research, 267, 340–345. https://doi.org/10.1016/j.psychres.2018.06.043 [DOI] [PubMed]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Rose T, Lindsey MA, Xiao Y, Finigan-Carr NM, Joe S. Mental health and educational experiences among Black Youth: A latent class analysis. Journal of Youth and Adolescence. 2017;46(11):2321–2340. doi: 10.1007/s10964-017-0723-3. [DOI] [PubMed] [Google Scholar]
- Ruch DA, Sheftall AH, Schlagbaum P, Rausch J, Campo JV, Bridge JA. Trends in suicide among US youth aged 10 to 19 years, 1975 to 2016. JAMA Network Open. 2019;2(5):e193886–e193886. doi: 10.1001/jamanetworkopen.2019.3886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rueter MA, Holm KE, McGeorgf CR, Conger RD. Adolescent suicidal ideation subgroups and their association with suicidal plans and attempts in young adulthood. Suicide and Life-Threatening Behavior. 2008;38(5):564–575. doi: 10.1521/suli.2008.38.5.564. [DOI] [PubMed] [Google Scholar]
- Scott LD, Munson MR, McMillen JC, Snowden LR. Predisposition to seek mental health care among Black males transitioning from foster care. Children and Youth Services Review. 2007;29(7):870–882. doi: 10.1016/j.childyouth.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Garland A, Vieland V, Underwood M, Busner C. The impact of curriculum-based suicide prevention programs for teenagers. Journal of the American Academy of Child and Adolescent Psychiatry. 1991;30(4):588–596. doi: 10.1097/00004583-199107000-00010. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Vieland V, Garland A, Rojas M, Underwood M, Busner C. Adolescent suicide attempters: Response to suicide-prevention programs. JAMA. 1990;264(24):3151–3155. doi: 10.1001/jama.1990.03450240053039. [DOI] [PubMed] [Google Scholar]
- Shain BN. Increases in rates of suicide and suicide attempts among Black adolescents. Pediatrics. 2019;144(5):e20191912. doi: 10.1542/peds.2019-1912. [DOI] [PubMed] [Google Scholar]
- Shakya HB, Domingue B, Nagata JM, Cislaghi B, Weber A, Darmstadt GL. Adolescent gender norms and adult health outcomes in the USA: A prospective cohort study. The Lancet Child & Adolescent Health. 2019;3(8):529–538. doi: 10.1016/S2352-4642(19)30160-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheftall AH, Asti L, Horowitz LM, Felts A, Fontanella CA, Campo JV, Bridge JA. Suicide in elementary school-aged children and early adolescents. Pediatrics. 2016;138(4):e20160436. doi: 10.1542/peds.2016-0436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spirito, A., Valeri, S., Boergers, J., & Donaldson, D. (2003). Predictors of continued suicidal behavior in adolescents following a suicide attempt. Journal of Clinical Child and Adolescent Psychology, 32(2), 284–289. Retrieved from http://proxy.library.nyu.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=mnh&AN=12679287&site=ehost-live [DOI] [PubMed]
- Thompson M, Swartout K. Epidemiology of suicide attempts among youth transitioning to adulthood. Journal of Youth and Adolescence. 2018;47(4):807–817. doi: 10.1007/s10964-017-0674-8. [DOI] [PubMed] [Google Scholar]
- Tidemalm D, Långström N, Lichtenstein P, Runeson B. Risk of suicide after suicide attempt according to coexisting psychiatric disorder: Swedish cohort study with long term follow-up. BMJ. 2008;337:a2205. doi: 10.1136/bmj.a2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toscos, T., Coupe, A., Flanagan, M., Drouin, M., Carpenter, M., Reining, L., … Mirro, M. J. (2019). Teens using screens for help: Impact of suicidal ideation, anxiety, and depression levels on youth preferences for telemental health resources. JMIR mental health, 6(6), e13230 [DOI] [PMC free article] [PubMed]
- Totura CMW, Labouliere CD, Gryglewicz K, Karver MS. The role of youth trainee–trainer alliance and involvement in school-based prevention: A moderated-mediation model of student gatekeeper suicide prevention training. Administration and Policy in Mental Health and Mental Health Services Research. 2019;46(2):209–219. doi: 10.1007/s10488-018-0907-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: Increased reporting with computer survey technology. Science. 1998;280(5365):867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. (2014). Disparities. Retrieved from https://www.healthypeople.gov/2020/about/foundation-health-measures/Disparities
- UNC Carolina Population Center. (2018). Add Health Research Design [PowerPoint slides]. Retrieved from https://www.cpc.unc.edu/projects/addhealth/design/researchdesign_3618_regular.pdf
- Vermunt JK. Latent class modeling with covariates: Two improved three-step approaches. Political Analysis. 2010;18(4):450–469. doi: 10.1093/pan/mpq025. [DOI] [Google Scholar]
- Vieland V, Whittle B, Garland A, Hicks R, Shaffer D. The impact of curriculum-based suicide prevention programs for teenagers: An 18-month follow-up. Journal of the American Academy of Child and Adolescent Psychiatry. 1991;30(5):811–815. [PubMed] [Google Scholar]
- Willis LA, Coombs DW, Drentea P, Cockerham WC. Uncovering the mystery: Factors of African American suicide. Suicide and Life-Threatening Behavior. 2003;33(4):412–429. doi: 10.1521/suli.33.4.412.25230. [DOI] [PubMed] [Google Scholar]
- Wunderlich U, Bronisch T, Wittchen H-U, Carter R. Gender differences in adolescents and young adults with suicidal behaviour. Acta Psychiatrica Scandinavica. 2001;104(5):332–339. doi: 10.1111/j.1600-0447.2001.00432.x. [DOI] [PubMed] [Google Scholar]
- Xiao, Y. (2019). Cumulative health risk behaviors, future orientation, and mental health among adolescents. Paper presented at the The American Academy of Health Behavior 2019 Annual Scientific Meeting: Theory and Applications of Multiple Health Behavior Change, Greenville, SC.
- Xiao Y, Bowen NK, Lindsey MA. Racial/ethnic measurement invariance of the School Success Profile (SSP)'s future orientation scale. Journal of School Psychology. 2018;71:85–107. doi: 10.1016/j.jsp.2018.10.003. [DOI] [PubMed] [Google Scholar]
- Xiao, Y., & Lu, W. (2019a). Social network risks and multiple health behaviors among adolescents: The moderating role of future orientation. Paper presented at the The American Academy of Health Behavior 2019 Annual Scientific Meeting: Theory and Applications of Multiple Health Behavior Change, Greenville, SC.
- Xiao Y, Lu W. Cumulative health risk behaviors and adolescent suicide: The moderating role of future orientation. American Journal of Health Behavior. 2019;43(6):1086–1102. doi: 10.5993/AJHB.43.6.7. [DOI] [PubMed] [Google Scholar]
- Xiao Y, Romanelli M, Lindsey MA. A latent class analysis of health lifestyles and suicidal behaviors among US adolescents. Journal of Affective Disorders. 2019;255:116–126. doi: 10.1016/j.jad.2019.05.031. [DOI] [PubMed] [Google Scholar]
- Xiao Y, Romanelli M, Vélez-Grau C, Lindsey MA. Unpacking racial/ethnic differences in the associations between neighborhood disadvantage and academic achievement: Mediation of future orientation and moderation of parental support. Journal of Youth and Adolescence. 2021;50(1):103–125. doi: 10.1007/s10964-020-01319-6. [DOI] [PubMed] [Google Scholar]
- Xiao Y, Wong K, Cheng QJ, Yip PS. Understanding the better than average effect on altruism. Frontiers in Psychology. 2020 doi: 10.3389/fpsyg.2020.562846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu B, Chen X. Age and birth cohort–adjusted rates of suicide mortality among US male and female youths aged 10 to 19 years from 1999 to 2017. JAMA Network Open. 2019;2(9):e1911383–e1911383. doi: 10.1001/jamanetworkopen.2019.11383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaborskis A, Sirvyte D, Zemaitiene N. Prevalence and familial predictors of suicidal behaviour among adolescents in Lithuania: A cross-sectional survey 2014. BMC Public Health. 2016 doi: 10.1186/s12889-016-3211-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman FJ, Anderson NW. Trends in health equity in the United States by race/ethnicity, sex, and income, 1993–2017. JAMA Network Open. 2019;2(6):e196386–e196386. doi: 10.1001/jamanetworkopen.2019.6386. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.