The European Hematology Association (EHA) Guideline Committee recently agreed to review the Global Guideline for the Diagnosis and Management of Rare Mold Infection of the European Confederation of Medical Mycology (ECMM) in cooperation with International Society for Human and Animal Mycology (ISHAM) and American Society for Microbiology (ASM).1 External reviews from independent experts were obtained in a standardized review process and the EHA decided to endorse the guideline.
With increasing numbers of immunosuppressed patients at risk for opportunistic infections, mycoses caused by molds other than Aspergillus or Mucorales are on the rise.2 Infections with rare molds possess several challenges for diagnosis and treatment and require complex multidisciplinary management.3 All invasive fungal diseases meet the definition of orphan diseases—an absolute frequency in the population of less than 1 in 2000—and therefore, resources remain more limited than in other areas of medicine. Guidance for optimal management is urgently needed. On that background, the ECMM has set out an unprecedented orphan diseases guidance initiative including all disciplines involved in diagnosis and treatment of invasive fungal infections.4,5
Previous guidelines on rare molds were limited to individual pathogens, focused on specific groups of patients such as those with hematological malignancies, or were missing altogether for infections caused by many of the very rare, but emerging pathogenic molds. The current ECMM Guideline is therefore an ambitious and unprecedented effort, as invasive mold infections caused by Fusarium spp., Lomentospora spp., Scedosporium spp., dematiaceous molds causing phaeohyphomycosis, Rasamsonia spp., Scopulariopsis spp., Penicillium spp., nonmarneffei Talaromyces spp., Paecilomyces spp., Purpureocillium spp., and Schizophyllum spp. as well as other basidiomycetes have been covered in detail.1
The endorsement of the EHA is of particular importance as fungal infections significantly contribute to morbidity and mortality in patients with hematological malignancies or those undergoing hematopoietic stem cell transplantation.6 Although numerically rare in the general population, frequencies of invasive fungal infections are much higher in immunocompromised patients and with treatment advances for underlying diseases as well as more common fungal infections such as invasive aspergillosis, treating physicians are increasingly confronted with less common and often multiresistant molds. The epidemiology of many of these rare and emerging infections is still not well studied, as data on incidence and prevalence are scarce and show high variability depending on geographical region and availability of diagnostic approaches. However, the ubiquitous environmental distribution of filamentous fungi and expanding patient populations with immunosuppression fosters the emergence of these infections, changing the epidemiological landscape lately (Figure 1). Various other drivers, such as new diagnostic utilities and the selective pressure caused by widespread antifungal use, including antifungal prophylaxis, accelerate this process.7
Figure 1.
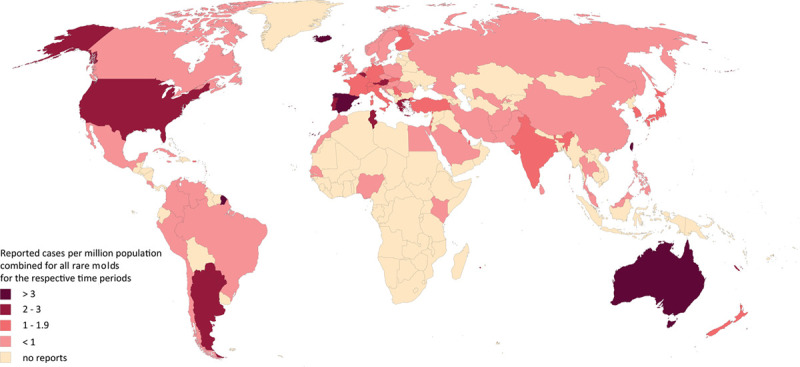
Worldwide distribution of reported rare mold infections. Number of reported cases of severe fungal infections caused by fungi of the genera Fusarium, Paecilomyces, Penicillium, Phaeohyphomycetes, Purpureocillium, Rasamsonia, Scedosporium, Lomentospora, Schizophyllum, Scopulariopsis, and Talaromyces in humans as provided for each pathogen separately in the Rare Mold Global Guideline are presented in a concatenated format for a general overview of the worldwide distribution. The map provides a current view on published cases that is likely related to the medical infrastructure and economic resources in some countries. Numbers are not supposed to predict incidences per country.
Most of the emerging molds cause severe disseminated disease in critically ill and immunocompromised patients and possess multiple challenges in diagnosis and management. Diagnosis requires a high index of clinical suspicion, mycological expertise, and accurate diagnostic methods. Knowledge on epidemiology, risk factors, and clinical characteristics can facilitate diagnosis. In hematological patients, fusariosis frequently manifests systemically with positive blood cultures and disseminated disease characteristically presents with necrotic erythematous skin lesions.8 Hematological malignancy and its treatment are also major risk factors for infection with Lomentospora spp. and Scedosporium spp. Dissemination of lomentosporiosis is detected in more than 80% of hematological patients, and mortality is devastating, mostly above 90%. Endocarditis and cerebral infection are frequently seen in disseminated lomentosporiosis, while patient with scedosporiosis predominantly present with pulmonary or cutaneous infections. Underlying malignancy predicts worse outcome for both lomentosporiosis and scedosporiosis.9 Infections caused by Rasamsonia spp. have been reported mainly in patients with chronic granulomatous disease or underlying malignancy and predominantly affect the lungs with high mortality rates.10 These examples demonstrate the importance of rare molds as etiological agents of life-threatening infections in a hematological setting. Appropriate prophylaxis and treatment in this vulnerable group of patients are complicated by the fact that several rare molds are intrinsically resistant against classes of antifungals. This includes Fusarium, Lomentospora, and Scedosporium spp. as well as even less common emerging molds such as Rasamsonia, Scopulariopsis, Paecilomyces, and Purpureocillium spp. Prompt and accurate classification at species level is therefore indispensable to tailor treatment based on individual susceptibility profiles. Optimization of the complex multidisciplinary management of these infections has the potential to improve prognosis.
The present ECMM recommendations are part of the “One World – One Guideline” initiative to incorporate regional differences in epidemiology and management.4,5 Available diagnostic and therapeutic options differ across global regions and guidance needs to reflect this to optimize patient management. Utilizing the global network of the ECMM and together with the International Society for Human and Animal Mycology and the American Society for Microbiology, medical professionals from around the world contributed their expertise and analyzed published evidence to develop global guidance for diagnosis and management of rare mold infections. Guidance is stratified for high- and low-resource countries and therefore applicable worldwide.
Due to the rarity and heterogeneity of emerging molds, the field still lacks high quality of evidence in several critical areas affecting the management of our patients. Nevertheless, medical professionals representing the fields of dermatology, infectious diseases, intensive care, hematology, microbiology, pathology, pediatrics, pharmacology, radiology, and surgery, and have put maximum effort to generate a balanced and effective tool to facilitate clinical decision-making. This guideline is therefore expected to be of substantial help to clinicians dealing with rare mold infections worldwide. Simultaneously, the guideline provides an overview of the areas of uncertainty for invasive mold infections and new directions of future research. The endorsement of the EHA is very encouraging and emphasizes the importance of rare mold infections in patients with hematological malignancies.
Disclosures
The authors declare no conflicts of interest.
Footnotes
R. Sprute, O. A. Cornely, and M. Hoenigl contributed equally.
References
- 1.Hoenigl M, Salmanton-García J, Walsh TJ, et al. Global guideline for the diagnosis and management of rare mould infections: an initiative of the European Confederation of Medical Mycology in cooperation with the International Society for Human and Animal Mycology and the American Society for Microbiology. Lancet Infect Dis. 2021February 16. [Epub ahead of print]. doi: 10.1016/S1473-3099(20)30784-2 [DOI] [PubMed] [Google Scholar]
- 2.Salmanton-García J, Koehler P, Kindo A, et al. Needles in a haystack: extremely rare invasive fungal infections reported in FungiScope®-Global Registry for Emerging Fungal Infections. J Infect. 2020; 81:802–815 [DOI] [PubMed] [Google Scholar]
- 3.Jenks JD, Seidel D, Cornely OA, et al. Voriconazole plus terbinafine combination antifungal therapy for invasive Lomentospora prolificans infections: analysis of 41 patients from the FungiScope® registry 2008-2019. Clin Microbiol Infect. 2020; 26:784.e781–784.e5 [DOI] [PubMed] [Google Scholar]
- 4.Cornely OA, Alastruey-Izquierdo A, Arenz D, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019; 19:e405–e421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoenigl M, Gangneux JP, Segal E, et al. Global guidelines and initiatives from the European Confederation of Medical Mycology to improve patient care and research worldwide: new leadership is about working together. Mycoses. 2018; 61:885–894 [DOI] [PubMed] [Google Scholar]
- 6.Pagano L, Caira M, Candoni A, et al. The epidemiology of fungal infections in patients with hematologic malignancies: the SEIFEM-2004 study. Haematologica. 2006; 91:1068–1075 [PubMed] [Google Scholar]
- 7.Lamoth F, Chung SJ, Damonti L, et al. Changing epidemiology of invasive mold infections in patients receiving azole prophylaxis. Clin Infect Dis. 2017; 64:1619–1621 [DOI] [PubMed] [Google Scholar]
- 8.Nucci M, Anaissie E. Fusarium infections in immunocompromised patients. Clin Microbiol Rev. 2007; 20:695–704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seidel D, Meißner A, Lackner M, et al. Prognostic factors in 264 adults with invasive Scedosporium spp. and Lomentospora prolificans infection reported in the literature and FungiScope®. Crit Rev Microbiol. 2019; 45:1–21 [DOI] [PubMed] [Google Scholar]
- 10.Stemler J, Salmanton-García J, Seidel D, et al. Risk factors and mortality in invasive Rasamsonia spp. infection: analysis of cases in the FungiScope® registry and from the literature. Mycoses. 2020; 63:265–274 [DOI] [PubMed] [Google Scholar]


