Abstract
Among the difficulties associated with Autism Spectrum Disorder (ASD) are those related to adaptation to changes and new situations, as well as anxious-depressive symptoms frequently related to excessive environmental requirements. The main objective of this research is to study the psychological impact of the lockdown due to the social emergency situation (COVID-19) in children/adolescents and adults diagnosed with ASD. Participants were 37 caregivers of children/adolescents with ASD, also 35 ASD adults and 32 informants. Evaluation was conducted through a web survey system and included standardized clinical questionnaires (CBCL and SCL-90-R), which were compared with results before lockdown start, and a brief self-reported survey addressing the subjective perception of changes in daily functioning areas. The results revealed a reduction of psychopathological symptoms in both age groups, but only reaching statistical significance in the adult group, except for Somatization, Anxiety, and Obsessive-Compulsive domains. ASD severity Level 2 showed greater improvement after lockdown onset in the children/adolescent group when compared to ASD Level 1 participants. Younger adults (18–25 yoa) reported greater improvement than older adults (=>25 yoa). Survey results indicate an improvement of feeding quality and a reduction in the number of social initiations during the lockdown. Adult ASD participants perceived a decrease in stress levels after the lockdown onset, whereas caregivers reported higher stress levels at the same point in both age groups. Limitations included the small number of participants and a heterogeneous evaluation window between measures. Pyschopathological status after two months of social distancing and lockdown seems to improve in ASD young adult population.
Keywords: Autism Spectrum Disorder, COVID-19, Mental health, Caregivers, Pre-post design, Survey
1. Introduction
The SARS-CoV-2 virus (COVID-19) has been rapidly spreading throughout the world, with Spain being one of the countries most affected by the pandemic (World Health Organization (WHO), 2020), with its transmission reaching the maximum capacity response of the public health system (Legido-Quigley et al., 2020) as well as forcing the public authorities to decree the state of alarm throughout the national territory and establishing a lockdown for a large part of the population. Mobility was reduced to avoid interpersonal contact and lower the chances of contagion, apart from exceptions considered force majeure such as buying food, pharmaceuticals, and basic necessities; attending health centers, services, and establishments; traveling to the work place; allowed professional or business services; returning to one’s habitual residence; assisting and caring for older people, minors, dependents, people with disabilities or especially vulnerable people; travelling to financial and insurance entities; due to force majeure or a situation of need (such as emergencies at home); any other similar activity that must be done individually, unless accompanied by people with disabilities or for other justified reasons.
This exceptional situation potentially activated a series of psychological responses in the general population, in reaction to COVID-19 and lockdown. In such an extraordinary setting like this, both the spread of the virus and the lockdown substantially increase emotions of fear, nervousness, sadness, or guilt (Pompili et al., 2014; Reynolds et al., 2008; Serafini et al., 2012). A recent systematic review on the mental health impact of the COVID-19 outbreak in specific groups of population found higher levels of post-traumatic stress symptoms and depression among COVID-19 patients, while increased depression/depressive symptoms, anxiety, psychological distress, and poor sleep quality were found in health care workers (Vindegaard & Benros, 2020). This review also reported that the clinical status of patients with psychiatric conditions worsened. Concerning the general population, survey studies revealed lower psychological well-being and higher anxiety and depression scores than before the pandemic outbreak (Rajkumar, 2020; Vindegaard & Benros, 2020). Also, the lockdown itself has led to an increase in psychological symptoms, emotional disturbance, depression, stress, hypothymia, irritability, post-traumatic symptoms, and anger (Brooks et al., 2020).
In this complex situation, people with previous psychiatric diagnoses are a particularly vulnerable population, both for the threat of SARS-CoV-2 for their general health status and environmental changes that can lead to a relapse of their psychiatric diagnosis. Within these groups, Autism Spectrum Disorder (ASD) is a particularly vulnerable group for the development of psychiatric symptoms during the pandemic. According to the DSM-5 (American Psychiatric Association, 2013), one of the main characteristics of ASD is flexibility difficulties, and therefore, the difficulty of adapting to new situations such as the lockdown. Moreover, people with ASD have a higher rate of psychiatric comorbidity than their counterparts (Lugo-Marín et al., 2019; Mannion & Leader, 2013), with anxiety, depression, and behavioral disorders being the most prevalent (Greenlee et al., 2016; Hollocks et al., 2019; Van Steensel & Heeman, 2017). These findings indicate an increased vulnerability for this group and their families, for whom the consequences of the pandemic, such as the loss of structured routines and the learning of new ones, can pose additional difficulties. The lockdown situation can also reduce academic and social requirements, which promote high daily stress for individuals with ASD (Khor, Melvin, Reid, & Gray, 2014). Hence, in some cases, an improvement could be detected in some specific aspects of both mental and general health status.
Some studies have been recently published on ASD and COVID-19-related issues regarding supporting recommendations for lockdown period (Eshraghi et al., 2020; Narzisi, 2020a; Smile, 2020), distance-based supporting challenges (Ameis, Lai, Mulsant, & Szatmari, 2020; Narzisi, 2020b; Stenhoff, Pennington, & Tapp, 2020) and world wide perception of ASD researchers (Amaral & de Vries, 2020). Also, a number of observational studies have been conducted in order to explore changes in mental and physical status of ASD individuals and their caregivers during this period. Colizzi et al. (2020) conducted an online survey in parents/caregivers of ASD children and found that most of the families considered COVID-19 emergency period difficult, especially when trying to manage structure activities and leisure time. Also, it was reported an increasement of the intensity and frequency of behavioral problems in ASD children. Moreover, prior diagnosed behavior difficulties predicted worse outcome of behavioral problems during lockdown period. When addressing parents/caregivers’ stress, higher levels have been reported since the onset of the COVID-19 pandemic (Manning, Billian, Matson, Allen, & Soares, 2020; Mutluer, Doenyas, & Genc, 2020). Identified stress factors were mostly related with therapeutical services shutdown and behavioral problems of ASD children during lockdown period. More specifically, Alhuzimi (2021) found that age and gender characteristics of the ASD individual, as well as their severity, directly impacted in parental stress and parental emotional well-being. Also, frequency and perceived usefulness of ASD therapeutic services negatively impacted parental stress and emotional well-being. Despite the evidence pointing to a worsening of mental and general status after the pandemic onset, to date, there is no published empirical study that directly compares after-lockdown-onset psychopathological outcomes with previous self-reported standardized measures in ASD individuals. Moreover, studies have focused on children and adolescents and their parents/caregivers’ subjective perception, while knowledge on self-perception of mental and general status of adults with ASD after the pandemic onset is yet to explore.
The main objective of this research is to study the psychological impact of lockdown due to the social emergency situation in children/adolescents and adults diagnosed with ASD. Specific hypotheses were: (i) Changes in psychopathological measures compared to those obtained before the lockdown onset, with higher scores expected in the post-lockdown evaluation; (ii) differences in ASD severity level and age, with people with more severe ASD forms and younger participants obtaining higher scores in the psychopathological measures; (iii) subjective perception of changes in ASD participants’ general status, as well as of caregivers’ level of stress will show a poorer status and greater stress levels at the post-lockdown evaluation.
2. Method
2.1. Participants
A sample of participants with ASD was recruited from the population monitored within the Comprehensive Care Program for Autism Spectrum Disorder (PAITEA), from the Hospital Vall d'Hebron Psychiatry Department. The study sample included patients who had been evaluated in our program and were subsequently invited to participate in the present study. The sample was subdivided into two groups, children/adolescents (3 years and 0 months - 17 years and 11 months), and adults (18 years or older). Inclusion criteria were having a diagnosis of ASD according to DSM-5 diagnostic criteria, user-level computer skills, and participants’ agreement to take part in the study. Language and cognitive barriers in respondents were exclusion criteria.
The estimated sample size is 100 participants, considering the total population of people with ASD attending PAITEA at the specified ages and calculated based on the prevalence described for this condition, assuming an error percentage (alpha) of 5%, with the same standard deviation value and a 95% confidence level, and loss values of 25% of the study participants.
2.2. Instruments
The following socio-demographic data and clinical characteristics of ASD participants were collected: age, gender, ASD severity level, psychiatric status, and medication changes during the lockdown period. In caregivers, the following data were collected: age, gender, relationship with the ASD participant, psychiatric history, working and socio-economic status changes after lockdown onset.
The evaluation instruments were self-informed questionnaires that measured psychopathological symptoms frequently found in both age groups at psychiatric settings.
2.2.1. Children/adolescents
The Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001) is a caregiver-reported measure that assesses a variety of childhood behavior problems. The syndrome scales combine to form a composite score of Internalization Problems, Externalization Problems, and Total Problems. A T-score of 65 (or above) is generally considered "clinically significant." This questionnaire has been widely reported for use in children and adolescents with ASD (Hoffmann, Weber, König, Becker, & Kamp-Becker, 2016; Magyar & Pandolfi, 2017).
2.2.2. Adults
The Symptom Checklist 90 Revised (SCL-90-R; Derogatis, 1994) is a 90-item, multidimensional, self-informed questionnaire developed to screen for a range of psychopathological symptoms in adult population (somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism). A T-score of 60 or above is considered “clinically significant.” This questionnaire has been used in ASD population to measure psychopathological status (Deprey & Ozonoff, 2018; Lever & Geurts, 2016; Spek, Van Ham, & Nyklíček, 2013).
As a result of the lack of a standardized survey to assess the outcomes of social distancing and lockdown in general health status, we decided to develop a survey. Thus, we designed a 10-point semantic differential scale assessing the following aspects of the functioning of a person with ASD: Mood/Irritability, Sleep quality, Feeding quality, Weight, Number of social initiations, Anxiety, and Externalizing/Internalizing behaviors. Also, stress levels (pre- and post-lockdown start) and general condition (post-lockdown start) were examined. For this purpose, answers on the 10-point semantic differential scale were coded as follows: answers ranging from 1 to 4 were coded as worse, less, or low, depending on the variable; answers ranging from 7 to 10 were coded as better, more, or high, depending on the variable; answers 5 and 6 were coded as no changes. A copy of this survey can be found in Appendix 1.
2.3. Procedure
Potential participants were contacted via telephone exactly 8 weeks after lockdown onset. After a textual explanation of the study goals, participants were asked for their consent to participate. If they consented, a digitalized version of the questionnaires and survey was provided through a web survey application. Caregivers of participants in the children/adolescent group were asked to complete the CBCL and the survey. In the adult group, both the informant (a relative/caregiver/partner) and the ASD participant were asked to complete the survey, whereas only the SCL-90-R was completed by the ASD participant. Medical records of each ASD participant were searched to retrieve similar evaluation measures conducted before lockdown onset.
2.4. Statistic analysis
Statistical analysis was carried out on the results of the questionnaires. First, a descriptive synthesis of the main variables (frequencies and means) was performed. The evaluation window was calculated as the difference between the first visit date and the completion date of the questionnaires/survey. For the analysis of differences in clinical variables (CBCL and SCL-90-R) between evaluation times, pre-lockdown (T1) and post-lockdown (T2), a non-parametric test (Wilcoxon signed-rank) of each independent variable was conducted. Also, for group differences in the ASD level of severity (Level 1 vs. Level 2) and age (young vs. older), a non-parametric test (Mann-Whitney Wilcoxon test) of each independent variable was conducted. Analysis of survey responses consisted of the calculation of frequencies for each variable assessed. In the adult group, a set of Chi-square tests was conducted to compare categorical variables between participants of the adult group (ASD vs. Informant). The level of significance was set at .05 in all analyses.
2.5. Ethics
Ethical approval was obtained from Hospital Universitari Vall d’Hebron Ethics Committee of Research and Medication.
3. Results
A total of 100 participants was contacted (50 in each group). Of these, 37 caregivers of the children/adolescent group completed the questionnaire and survey. In the adult group, a total of 35 ASD adults completed the questionnaire and survey, and 32 informants completed the survey. The mean evaluation window was estimated at 14.07 months (SD = 7.58; 95% CI [11.6, 16.5]) in the children/adolescent group and 9.41 months (SD = 4.42; 95% CI [7.95, 10.9]) in the adult group. No significant differences were found either in the demographic or clinical characteristics in children/adolescents (age: Z = −.61, p = .54; gender: Z = −.17, p = .87; ASD severity: Z = -.46, p = .65; psychiatric history: Z = −.109, p = .91) or adults (age: Z = −1.35, p = .18; gender: Z = −.52, p = .60; ASD severity: Z = .00, p = 1; psychiatric history: Z = −.52, p = .61) groups. A synthesis of these results can be found in Table 1 .
Table 1.
Demographic and clinical characteristics of participants.
| ASD participant | Children/Adolescents (n = 37) | Adults (n = 35) |
|---|---|---|
| Age (mean, sd) | 10.7 (3.4) | 32.8 (13.1) |
| Gender (male %) | 86.5 | 65.7 |
| ASD severity (%) | ||
| Level 1 | 70.3 | 100 |
| Level 2 | 29.7 | 0 |
| Level 3 | 0 | 0 |
| Psychiatric history (%) | ||
| At least one psychiatric disorder | 67.6 | 80 |
| No past history of psychiatric disorders | 32.4 | 20 |
| Changes in pharmacological treatment during confinement (%) | ||
| Yes | 19 | 6 |
| No | 81 | 94 |
| Caregiver/Informant | Children/Adolescents (n = 37) | Adults (n = 32) |
|---|---|---|
| Age (mean, sd) | 42.5 (11.7) | 52.7 (5.3) |
| Gender (male %) | 13.5 | 18.8 |
| Relationship with ASD participant (%) | ||
| Mother | 89.2 | 68.8 |
| Father | 10.8 | 6.3 |
| Partner | – | 25 |
| Psychiatric history (%) | ||
| At least one psychiatric disorder | 67.6 | 71.9 |
| No past history of psychiatric disorders | 32.4 | 28.1 |
| Familiar psychiatric history (other than Caregiver/Informant) (%) | ||
| At least one psychiatric disorder | 73 | 81.3 |
| No past history of psychiatric disorders | 27 | 18.8 |
| Employment status changes post-confinement start (%) | ||
| Subsidized unemployment | 16.2 | 6.2 |
| Non-subsidized unemployment | 2.7 | 12.5 |
| Teleworking | 19 | 18.8 |
| No changes | 60 | 71.9 |
| Income level changes post-confinement start (%) | ||
| Better | 10.8 | 0 |
| Worse | 35.1 | 43.8 |
| No changes | 54.1 | 56.3 |
3.1. Children/adolescents
3.1.1. Psychopathology assessment
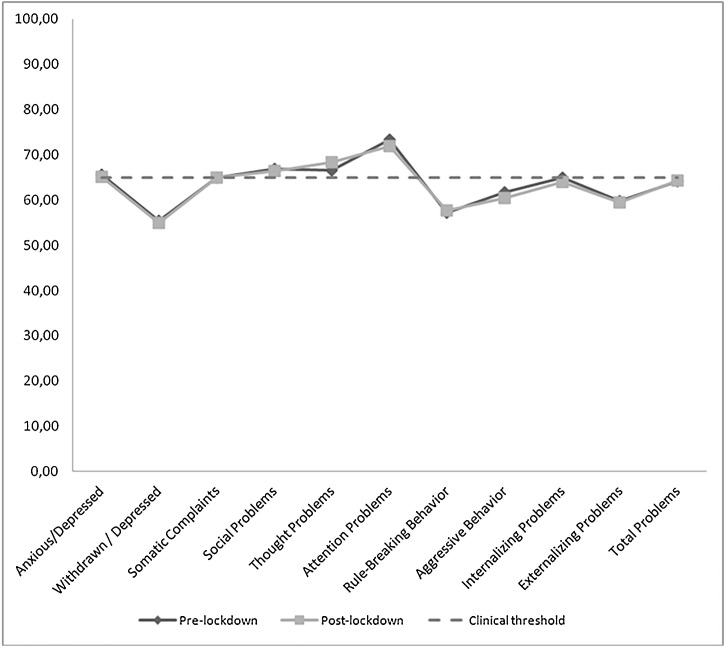
Table 2 shows the mean CBCL scores of ASD participants at both evaluation times. At T1, participants scored below the clinical threshold in all subscales, except for Anxious/Depressed (M = 65.7, SD = 14.8), Social Problems (M = 67, SD = 16.4), Thought Problems (M = 66.7, SD = 15), and Attention Problems (M = 73.3, SD = 16). At T2, participants scored above the clinical threshold in the same subscales. The result of the mean comparison test found no subscale significantly lower after the lockdown start (Table 2). Fig. 1 shows the line graph comparing both evaluation times.
Table 2.
CBCL means (sd) for children/adolescents group (n = 36).
| Pre-lockdown (T1) | Post-lockdown (T2) | Wilcoxon signed-rank test | |
|---|---|---|---|
| Anxious/Depressed | 65,65 (14.8) | 65,08 (10.7) | −1.12 |
| Withdrawn/Depressed | 55,46 (11.5) | 54,86 (6.3) | −1.72 |
| Somatic Complaints | 64,95 (15.6) | 64,92 (10.7) | −.84 |
| Social Problems | 66,95 (16.4) | 66,41 (10.4) | −1.11 |
| Thought Problems | 66,65 (15) | 68,32 (9.5) | −0.27 |
| Attention Problems | 73,30 (15.9) | 71,95 (8.9) | −1.8 |
| Rule-Breaking Behavior | 57,22 (12.3) | 57,68 (7.4) | −0.11 |
| Aggressive Behavior | 61,68 (15.1) | 60,35 (9.2) | −1.03 |
| Internalizing Problems | 64,97 (14.4) | 63,92 (10.9) | −1.81 |
| Externalizing Problems | 59,81 (13) | 59,49 (9.2) | −1.17 |
| Total Problems | 64,22 (14) | 64,35 (9.7) | −0.64 |
Fig. 1.
Comparison CBCL Pre vs Post lockdown (n = 37 children/adolescents).
3.1.2. Differences by ASD severity
Regarding ASD severity level, inter-group analysis showed significant differences, indicating lower scores in the ASD Level 2 group for Withdrawn/Depressed (Z = −2.62, p = .01) at T1, whereas Anxious/Depressed (Z = −2.5, p = .01), Somatic Complaints (Z = −2.85, p = .00), Rule-Breaking Behavior (Z = −2.1, p = .04), Internalizing Problems (Z = −2.99, p = .00), and Total Problems (Z = −2.25, p = .02) showed statistically significant differences at T2, with lower scores in the ASD Level 2 group. The within-group comparison showed significantly lower differences between the pre- and post-lockdown CBCL scores at T2 only for the Withdrawn/Depressed subscale (Z = −2.61, p = .01) in the ASD Level 1 group.
3.1.3. Differences by age
Regarding differences by age group, inter-group differences showed significant results only for Social Problems (Z = −2.22, p = .03), with higher scores in the adolescent group (=>12 yoa) at T1. Within-group analyses revealed no significant differences in CBCL scores for any subscales between evaluation times.
3.1.4. General status and subjective perception of stress level
Survey results are shown in Table 3 . Caregivers reported significant improvement (=>45%) only in feeding quality (49%), whereas significant worsening was reported for Mood/Irritability (57%), and a lower number of social initiations (49%). Caregivers’ stress after lockdown onset was evaluated as high in 62% of the participants, although it was considered high before the lockdown start in 38% of the respondents.
Table 3.
Survey results for children/adolescents group (n = 36).
| Worse | No changes | Better | |
|---|---|---|---|
| Mood/Irritability | 57 | 19 | 24 |
| Sleep quality | 30 | 38 | 32 |
| Feeding quality | 22 | 30 | 49 |
| Anxiety | 38 | 32 | 30 |
| Externalizing | 30 | 35 | 35 |
| Internalizing | 27 | 30 | 43 |
| ASD participant general status post-confinement | 38 | 30 | 32 |
| Low | No changes | High | |
|---|---|---|---|
| Weight | 14 | 60 | 27 |
| *Stress pre-confinement | 32 | 30 | 38 |
| *Stress post-confinement | 16 | 22 | 62 |
| Less | No changes | More | |
|---|---|---|---|
| Number of social initiations | 49 | 14 | 38 |
3.2. Adults
3.2.1. Psychopathology assessment
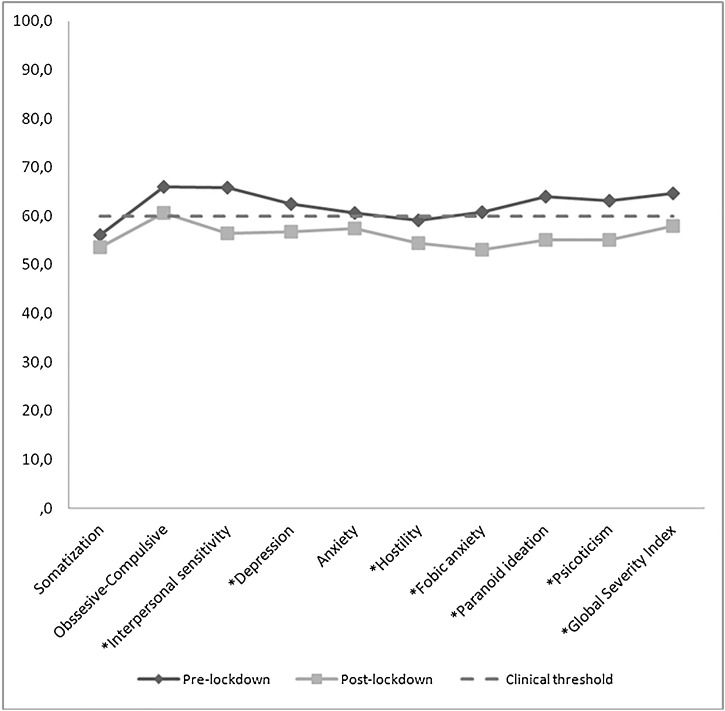
Table 4 shows the mean SCL-90-R scores of ASD adult participants both at T1 and T2. Before the lockdown start (T1), participants scored above the clinical threshold in all subscales, except for Somatization (M = 56, SD = 11.7) and Hostility (M = 59.1, SD = 8.6). At T2, participants scored below the clinical threshold in all subscales, except for Obsessive-Compulsive, which remained close to the clinical threshold (M = 61.7, SD = 13.7). The result of the mean comparison test found that all the subscales were significantly lower after the lockdown start, except for Somatization (Z = −1.02, p = .31), Obsessive-Compulsive (Z = −1.88, p = .06), and Anxiety (Z = −1.26, p = .21) (Table 4). Fig. 2 shows the line graph comparing both evaluation times.
Table 4.
SCL-90-R means (sd) for adult group (n = 35).
| Pre-lockdown | Post-lockdown | Wilcoxon signed-rank test | |
|---|---|---|---|
| Somatization | 56 (11.7) | 54,6 (12.8) | −1.02 |
| Obssesive-Compulsive | 66,1 (9) | 61,7 (13.7) | −1.88 |
| Interpersonal sensitivity | 65,9 (10.5) | 56,5 (15.8) | −4.04* |
| Depression | 62,4 (12.1) | 57,9 (15.1) | −2.29* |
| Anxiety | 60,7 (10.9) | 58,2 (13.7) | −1.26 |
| Hostility | 59,1 (8.6) | 54,9 (12.6) | −2.51* |
| Fobic anxiety | 60,9 (12.6) | 53,5 (15.9) | −2.28* |
| Paranoid ideation | 63,9 (10.4) | 55,6 (15.6) | −4.02* |
| Psicoticism | 63,1 (11.9) | 56,3 (17.6) | −2.38* |
| Global Severity Index | 64,7 (10.6) | 58,7 (14.9) | −3.28* |
p < .05.
Fig. 2.
Comparison SCL-90 Pre vs Post lockdown (n = 35 adults).
*p<.05.
3.2.2. Differences by ASD severity
Due to a lack of participants with ASD severity Level 2, analysis of the differences between ASD severity levels could not be conducted.
3.2.3. Differences by age
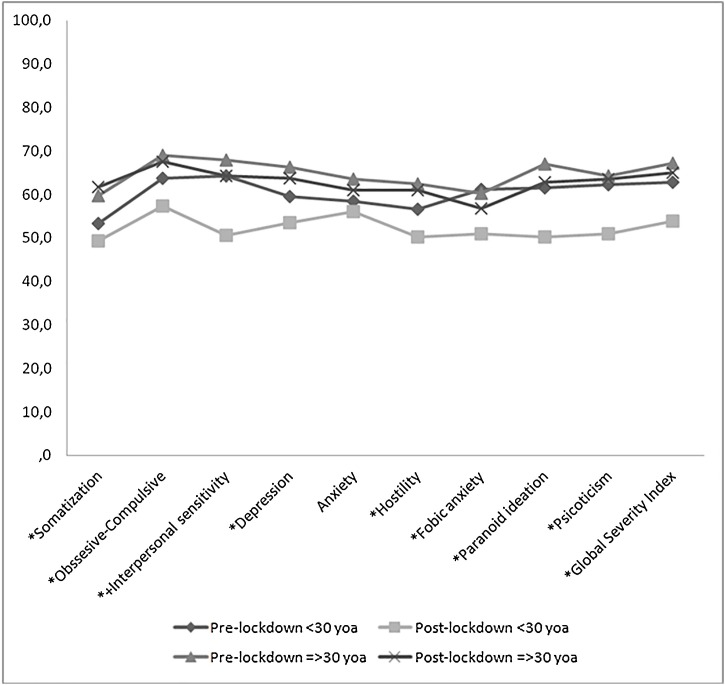
Regarding age differences, inter-group analysis revealed significant differences in all mean SCL-90-R subscale scores between the young adult group (<30 yoa) and the older adult group (> = 30 yoa), except for Anxiety (Z = −1.09, p = .28) and Phobic Anxiety (Z = −1.15, p = .25), with lower scores in younger adults at T2. Within-group analysis showed a significant decrease in all mean SCL-90-R subscale scores at T2 in the young adult group, except for Anxiety (Z = −.52, p = .60). For older adults, the mean SCL-90-R scores showed a significant decrease only for Interpersonal Sensitivity (Z = −2.1, p = .04) (Fig. 3 ).
Fig. 3.
Comparison SCL-90 Pre vs Post lockdown across ages (n = 20 younger ASD adults; n = 15 older ASD adults).
<30 yoa (n = 20) *p<.05.
=>30 yoa (n = 15) +p<.05.
3.2.4. General status and subjective perception of stress level
Survey results are shown in Table 5 . The areas of daily functioning that were self-perceived as very improved (=>45%) for the ASD adults were Feeding quality (51%) and Externalizing behaviors (47%), whereas the number of social initiations was reported as lower for half the sample (51%). ASD adults rated their stress before lockdown onset as high in approximately half the sample (47%), whereas it was perceived as high after lockdown onset in a little more than one-third of the sample (37%). Finally, general status post-lockdown onset was perceived as better by almost half of the ASD adult participants (49%).
Table 5.
Survey results (%) for adult group ASD participant (n = 35) and caregiver/informant (n = 32).
| Worse |
No changes |
Better |
||||
|---|---|---|---|---|---|---|
| ASD participant | Caregiver/Informant | ASD participant | Caregiver/Informant | ASD participant | Caregiver/Informant | |
| Mood/Irritability | 37 | 41 | 26 | 25 | 37 | 34 |
| Sleep quality | 44 | 56 | 19 | 25 | 37 | 19 |
| Feeding quality | 21 | 22 | 28 | 41 | 51 | 38 |
| Anxiety | 35 | 41 | 28 | 31 | 37 | 28 |
| Externalizing | 21 | 34 | 33 | 41 | 47 | 25 |
| Internalizing | 28 | 22 | 35 | 47 | 37 | 32 |
| ASD participant general status post-confinement | 30 | 31 | 21 | 31 | 49 | 36 |
| Low |
No changes |
High |
||||
|---|---|---|---|---|---|---|
| ASD participant | Caregiver/Informant | ASD participant | Caregiver/Informant | ASD participant | Caregiver/Informant | |
| Weight | 14 | 25 | 54 | 44 | 33 | 31 |
| *Stress pre-confinement | 30 | 25 | 23 | 34 | 47 | 41 |
| *Stress post-confinement | 37 | 31 | 26 | 19 | 37 | 50 |
| Less |
No changes |
More |
||||
|---|---|---|---|---|---|---|
| ASD participant | Caregiver/Informant | ASD participant | Caregiver/Informant | ASD participant | Caregiver/Informant | |
| Number of social initiations | 51 | 34 | 14 | 44 | 35 | 22 |
For each respondant, item refers to their own stress level.
In the case of Caregiver/Informants’ subjective perception, none of the evaluated areas of daily functioning reached at least 45% of improvement after the lockdown onset, whereas sleep quality worsened in half the sample (56%). Caregiver/Informants’ stress level after the lockdown was evaluated as high in 50% of participants, whereas it was considered high before lockdown start in 41% of the respondents. General status after the lockdown onset was perceived as better by 36% of the Caregiver/Informants, whereas 31% considered it worse than before the lockdown start.
Chi-square tests showed no significant differences in ratings between ASD participants and their caregivers/informants in any survey outcome.
4. Discussion
To our knowledge, this is the first study addressing the psychological impact after the COVID-19 pandemic outbreak in ASD population and their caregivers. Moreover, this study includes a comparison with a standardized self-informed instrument prior to the start of social distancing and lockdown measures. The main findings indicate a decrease in psychopathological problems in this population during the lockdown, with a greater improvement found in the young adult ASD population. Feeding quality also seemed to improve, as reported by both age groups. Finally, stress levels were found to be lower in adults with ASD, whereas caregivers perceived an increase in their stress level after the lockdown onset.
Regarding children and adolescents with ASD, results show a general improvement in psychopathological status after the lockdown start, although not reaching statistical significance. Unexpectedly, caregivers reported greater improvement in the psychopathological status for ASD Level 2 participants when compared to ASD 1 Level participants. This result may be explained by changes in pharmacological treatment during the lockdown period. In fact, 27% of the ASD Level 2 participants in the children/adolescent group reported changes in pharmacological treatment after the lockdown onset, due to a deterioration of their clinical status, whereas only 15% of the participants in the ASD Level 1 group reported changes in pharmacological treatment. Thus, this general improvement in results should be considered within the context of a change in medication, probably due to an initial worsening of ASD participants’ clinical status. Also, there is an imbalance between the number of participants in each ASD severity level group, with the ASD Level 1 group representing two-thirds of the total sample. Regarding ASD Level 1 participants, they seem to benefit from social distancing measures in withdrawn/depressed symptoms. Many of the items on this scale are sensitive to the differences in social reciprocity present in ASD, such as shyness, withdrawal, and preference for being alone. Thus, a lockdown situation improved this area due to the drastic decrease in social demands.
Concerning adult ASD participants, the global results suggest a significant improvement in psychopathological symptoms after the lockdown start. Only for few variables (Somatization, Anxiety, and Obsessive-Compulsive), differences were not significant. In any case, both Somatization and Anxiety scored below the clinical threshold in the post-lockdown evaluation, while Obsessive-Compulsive remained at the limit of significance. Moreover, when divided by age, young adults (under 30 yoa) seem to be the group with more improvement. Interestingly, older adults (30 yoa or above) benefited from the social distancing measures, improving their scores on SCL-90-R “Interpersonal Sensitivity”, which refers to feelings of inferiority and inadequacy, especially when comparing oneself with peers. Overall, these results suggest that psychopathological status seems to improve in adults with ASD when environmental requirements decrease. Only anxiety symptoms, which may be related to adaptation to changes of the so-called “new normality” (hygiene measures, new social rules, etc.), may not have improved in the lockdown situation.
Finally, general status assessed through survey indicates an improvement in feeding quality in the two age groups. This may be due to the fact that, during lockdown, people stayed at home and had more time for indoor activities like cooking, which allowed subjects with ASD to explore this area and even dare to extend certain previous restrictions. Another possible explanation would be the fact that, in some families, having more time at home has led to more elaborate menus, translating into improvements in the diet of the whole family. Also, the number of social interactions was reported as lower in both age groups, which can be explained by the social distancing setting, which did not allow direct contact with other people and resembles what was observed in the general population (Elmer, Mepham, & Stadtfeld, 2020; Smith & Limb, 2020). Although there was a clear decrease in face-to-face personal relationships, there has been an increase in social contact through virtual settings (e.g., videophone, online chats) (Gammon & Ramshaw, 2020; Luchetti et al., 2020). As people with ASD tend to prefer social interactions through virtual media (Benford & Standen, 2009), they may have made use of these non-physical mechanisms to interact with others during the lockdown period. These interactions may have increased when compared to before the lockdown, and the families may be unaware of this improvement in socialization because it belongs to the intimacy of the person with ASD.
Concerning stress, both children/adolescent caregivers and adult informants reported an increased level of stress after lockdown onset, whereas adults with ASD reported a decrease in their self-perceived stress levels. This can be explained because the caregivers/informants increased the time spent on this task during the lockdown, leading to higher levels of self-perceived stress, whereas ASD adults reduced their environmental requirements and, therefore, their efforts to fit in a neurotypical setting.
Survey results show that caregivers/informants’ reports are congruent with those of ASD participants in all the variables evaluated. Sleep quality was reported to worsen during the lockdown by informants, whereas the adults with ASD perceived the opposite outcome. This discrepancy can be explained by analyzing ASD sleep profiles, which are known to show insomnia and sleep phase delay (Cortese, Wang, Angriman, Masi, & Bruni, 2020). During the lockdown period, environmental requirements of time schedules almost completely disappeared, making it unnecessary to get up at a certain time in the morning. Thus, adults with ASD may have translated this into an improvement, as they could go to bed as soon as they started to feel sleepy and get up when they felt sufficiently rested. Conversely, informants may have considered this as a worsening because they may have changed sleep routines in terms of pre-lockdown standards.
4.1. Limitations
Among the limitations, the small number of participants could compromise the generalizability of the findings. Also, the heterogeneity of each participant’s evaluation window could also affect the interpretation of the results. In this line, the effects of previous pharmacological and non-pharmacological treatments applied since the baseline data were collected could have influenced changes in the participants’ psychopathological scores. Thus, improvement in this outcome may not be directly associated with lockdown onset. Nevertheless, differences between age groups indicate an effect of lockdown and social distancing measures, at least in the young adult group, which strongly suggests that environmental demands underlie this particular population’s psychiatric status.
4.2. Conclusions
The COVID-19 pandemic outbreak has partially benefited the psychopathological status of adults with ASD Level 1, and especially for those of younger age. This improvement may not be shared by caregivers/informants, who seem to have increased their stress levels since the lockdown period. These findings should be considered when designing future interventions for this specific population, attending to social and environmental adaptations and not neglecting all the therapeutical requirements in people with ASD and their caregivers. Also, longitudinal measures are needed to evaluate this seeming improvement once neurotypical normality is re-established. After the present study was concluded, the lockdown scenario began to change, as people were allowed to go out again, and many socially related activities (e.g., shops, cafeterias) were re-established. Over time, we followed the evolution of these participants through clinical visits and verbal reports, concluding that the progressive return to the situation before the lockdown has changed the participants’ clinical status. In any case, this assessment is based on clinical judgment, and in no case should it be considered scientific evidence. Also, this assumption may not apply to all the ASD population.
Finally, the authors would like to emphasize the increased burden for caregivers of ASD individuals during the lockdown situation, having to cope with both their own and others’ needs during this exceptional time. This reflects how vulnerable this population is and the importance of the role of caregivers in ensuring the well-being of ASD individuals. Policy-makers must address this issue to fulfill their requests and prevent the emergence of psychological distress (e.g., Anxiety) in caregivers of people with ASD.
CRediT authorship contribution statement
Jorge Lugo-Marín: Conceptualization, Methodology, Formal analysis, Investigation, Resources, Writing - original draft. Laura Gisbert-Gustemps: Conceptualization, Methodology, Formal analysis, Investigation, Resources, Writing - original draft. Imanol Setien-Ramos: Conceptualization, Methodology, Formal analysis, Investigation, Resources, Writing - review & editing. Gemma Español-Martín: Conceptualization, Methodology, Writing - review & editing. Pol Ibañez-Jimenez: Conceptualization, Methodology, Writing - review & editing. Mireia Forner-Puntonet: Writing - review & editing. Gara Arteaga-Henríquez: . Albert Soriano-Día: Writing - review & editing. Juan David Duque-Yemail: Writing - review & editing. Josep Antoni Ramos-Quiroga: Writing - review & editing, Supervision.
Declaration of Competing Interest
The author L.G. received travel awards for taking part in psychiatric meetings from Shire in the last 3 years. The author J.A.R.Q was on the speakers’ bureau and/or acted as consultant for Eli-Lilly, Janssen-Cilag, Novartis, Shire, Takeda, Lundbeck, Almirall, Braingaze, Sincrolab, Medice and Rubió in the last 5 years. He also received travel awards (air tickets+hotel) for taking part in psychiatric meetings from Janssen-Cilag, Rubió, Shire, Takeda, Medice and Eli- Lilly. The Department of Psychiatry chaired by him received unrestricted educational and research support from the following companies in the last 5 years: Eli-Lilly, Lundbeck, Janssen- Cilag, Actelion, Shire, Ferrer, Oryzon, Roche, Psious, and Rubió.
Acknowledgments
Dr. Gara Arteaga Henríquez is currently funded by the Innovative Medicine Initiative (IMI2)-Call 2 under grant agreement no. 853966. The funders played no part in study design, collection, management, analysis, and interpretation of the data; writing of the report; or the decision to submit the report for publication.
The authors want to thank Dr. Virginia Navascues for her diligent proofreading of this paper.
Number of completed reviews is 2
References
- Achenbach T.M., Rescorla L.A. University of Vermont, Research Center For Children Youth & Families; 2001. Manual for the ASEBA school-age forms & profiles: Child behavior checklist for ages 6-18, teacher’s report form, youth self-report: An integrated system of multi-informant assessment. [Google Scholar]
- Alhuzimi T. Stress and emotional wellbeing of parents due to change in routine for children with Autism Spectrum Disorder (ASD) at home during COVID-19 pandemic in Saudi Arabia. Research in Developmental Disabilities. 2021;108 doi: 10.1016/j.ridd.2020.103822. [DOI] [PubMed] [Google Scholar]
- Amaral D.G., de Vries P.J. COVID‐19 and autism research: Perspectives from around the globe. Autism Research. 2020;13(6):844. doi: 10.1002/aur.2329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ameis S.H., Lai M.C., Mulsant B.H., Szatmari P. Coping, fostering resilience, and driving care innovation for autistic people and their families during the COVID-19 pandemic and beyond. Molecular Autism. 2020;11(1):1–9. doi: 10.1186/s13229-020-00365-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . American Psychiatric Pub; 2013. Diagnostic and statistical manual of mental disorders (DSM-5®) [Google Scholar]
- Benford P., Standen P.J. The Internet: A comfortable communication medium for autistic people? I: Journal of Assistive Technologies. 2009;3(2):44–53. [Google Scholar]
- Brooks S., Webster R., Smith L., Woodland L., Wessely S., Greenberg N., et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colizzi M., Sironi E., Antonini F., Ciceri M.L., Bovo C., Zoccante L. Psychosocial and behavioral impact of COVID-19 in autism spectrum disorder: An online parent survey. Brain Sciences. 2020;10(6):341. doi: 10.3390/brainsci10060341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortese S., Wang F., Angriman M., Masi G., Bruni O. Sleep disorders in children and adolescents with autism spectrum disorder: Diagnosis, epidemiology, and management. CNS Drugs. 2020:1–9. doi: 10.1007/s40263-020-00710-y. [DOI] [PubMed] [Google Scholar]
- Deprey L., Ozonoff S. 2018. Assessment of comorbid psychiatric conditions in autism spectrum disorder. [Google Scholar]
- Derogatis L.R. National Computer Systems. Inc.; Minneapolis: 1994. Scl-90-r: Administration, scoring and procedures manual. [Google Scholar]
- Elmer T., Mepham K., Stadtfeld C. Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PloS One. 2020;15(7) doi: 10.1371/journal.pone.0236337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eshraghi A.A., Li C., Alessandri M., Messinger D.S., Eshraghi R.S., Mittal R., et al. COVID-19: Overcoming the challenges faced by individuals with autism and their families. The Lancet Psychiatry. 2020;7(6):481–483. doi: 10.1016/S2215-0366(20)30197-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gammon S., Ramshaw G. Distancing from the present: Nostalgia and leisure in lockdown. Leisure Sciences. 2020:1–7. [Google Scholar]
- Greenlee J.L., et al. Medical and behavioral correlates of depression history in children and adolescents with autism spectrum disorder. Pediatrics. 2016;137(Supplement 2):S105–S114. doi: 10.1542/peds.2015-2851I. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann W., Weber L., König U., Becker K., Kamp-Becker I. The role of the CBCL in the assessment of autism spectrum disorders: An evaluation of symptom profiles and screening characteristics. Research in Autism Spectrum Disorders. 2016;27:44–53. [Google Scholar]
- Hollocks M.J., et al. Anxiety and depression in adults with autism spectrum disorder: A systematic review and meta-analysis. Psychological Medicine. 2019;49(4):559–572. doi: 10.1017/S0033291718002283. [DOI] [PubMed] [Google Scholar]
- Khor A.S., Melvin G.A., Reid S.C., Gray K.M. Coping, daily hassles and behavior and emotional problems in adolescents with high-functioning autism/Asperger’s disorder. Journal of Autism and Developmental Disorders. 2014;44(3):593–608. doi: 10.1007/s10803-013-1912-x. [DOI] [PubMed] [Google Scholar]
- Legido-Quigley H., Mateos-García J.T., Campos V.R., Gea-Sánchez M., Muntaner C., McKee M. The resilience of the Spanish health system against the COVID-19 pandemic. Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30060-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lever A.G., Geurts H.M. Psychiatric co-occurring symptoms and disorders in young, middle-aged, and older adults with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2016;46(6):1916–1930. doi: 10.1007/s10803-016-2722-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luchetti M., Lee J.H., Aschwanden D., Sesker A., Strickhouser J.E., Terracciano A., et al. The trajectory of loneliness in response to COVID-19. American Psychologist. 2020;75(7):897–908. doi: 10.1037/amp0000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lugo-Marín J., et al. Prevalence of psychiatric disorders in adults with autism spectrum disorder: A systematic review and meta-analysis. Research in Autism Spectrum Disorders. 2019;59:22–33. [Google Scholar]
- Magyar C.I., Pandolfi V. Utility of the CBCL DSM-oriented scales in assessing emotional disorders in youth with autism. Research in Autism Spectrum Disorders. 2017;37:11–20. doi: 10.1016/j.rasd.2017.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manning J., Billian J., Matson J., Allen C., Soares N. Perceptions of families of individuals with Autism Spectrum Disorder during the COVID-19 crisis. Journal of Autism and Developmental Disorders. 2020:1–9. doi: 10.1007/s10803-020-04760-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannion A., Leader G. Comorbidity in autism spectrum disorder: A literature review. Research in Autism Spectrum Disorders. 2013;7(12):1595–1616. [Google Scholar]
- Mutluer T., Doenyas C., Genc H.A. Behavioral Implications of the Covid-19 process for autism spectrum disorder, and individuals’ comprehension of and reactions to the pandemic conditions. Frontiers in Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.561882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narzisi A. 2020. Handle the autism spectrum condition during coronavirus (COVID-19) stay at home period: Ten tips for helping parents and caregivers of young children. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narzisi A. Phase 2 and later of COVID-19 lockdown: Is it possible to perform remote diagnosis and intervention for autism spectrum disorder? An online-mediated approach. Journal of Clinical Medicine. 2020;9(6):1850. doi: 10.3390/jcm9061850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pompili M., Innamorati M., Lamis D.A., Erbuto D., Venturini P., Ricci F., et al. The associations among childhood maltreatment,“male depression” and suicide risk in psychiatric patients. Psychiatry Research. 2014;220(1–2):571–578. doi: 10.1016/j.psychres.2014.07.056. [DOI] [PubMed] [Google Scholar]
- Rajkumar R.P. COVID-19 and mental health: A review of the existing literature. Asian Journal of Psychiatry. 2020 doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds D., Garay J., Deamond S., Moran M., Gold W., Styra R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiology and Infection. 2008;136(7):997–1007. doi: 10.1017/S0950268807009156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serafini G., Pompili M., Innamorati M., Gentile G., Borro M., Lamis D.A., et al. Gene variants with suicidal risk in a sample of subjects with chronic migraine and affective temperamental dysregulation. European Review for Medical and Pharmacological Sciences. 2012;16(10):1389–1398. [PubMed] [Google Scholar]
- Smile S.C. Supporting children with autism spectrum disorder in the face of the COVID-19 pandemic. CMAJ. 2020;192(21) doi: 10.1503/cmaj.75399. E587-E587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B.J., Limb M.H. How the COVID-19 pandemic is focusing attention on loneliness and social isolation. Public Health Research & Practice. 2020;30(2) doi: 10.17061/phrp3022008. [DOI] [PubMed] [Google Scholar]
- Spek A.A., Van Ham N.C., Nyklíček I. Mindfulness-based therapy in adults with an autism spectrum disorder: A randomized controlled trial. Research in Developmental Disabilities. 2013;34(1):246–253. doi: 10.1016/j.ridd.2012.08.009. [DOI] [PubMed] [Google Scholar]
- Stenhoff D.M., Pennington R.C., Tapp M.C. Distance education support for students with autism spectrum disorder and complex needs during covid-19 and school closures. Rural Special Education Quarterly. 2020;39(4):211–219. [Google Scholar]
- Van Steensel F.J.A., Heeman E.J. Anxiety levels in children with autism spectrum disorder: A meta-analysis. Journal of Child and Family Studies. 2017;26(7):1753–1767. doi: 10.1007/s10826-017-0687-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain, Behavior, and Immunity. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) 2020. Coronavirus disease (COVID-19) technical guidance: Infection prevention and control/WASH.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical- Retrieved March 26, at: [Google Scholar]