Abstract
Introduction
The reopening of schools during the COVID-19 pandemic has raised concern for the safety of staff and students, their families and the wider community. We monitored SARS-CoV-2 infection rates in school-aged children and compared them with adult infection rates before and after schools reopened in England.
Methods
Public Health England receives daily electronic reports of all SARS-CoV-2 tests nationally. SARS-CoV-2 infection rates by school year from July to December 2020 were analysed, including the effect of a national month-long lockdown whilst keeping schools open in November 2020
Results
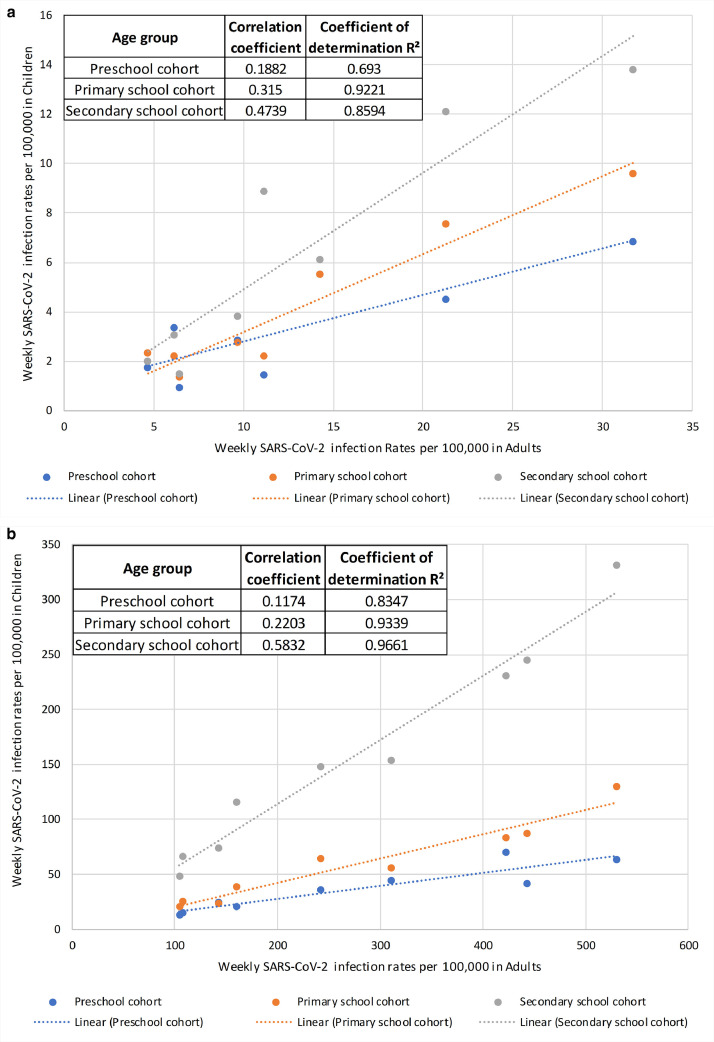
SARS-CoV-2 infections rates were low during early summer but started increasing in mid-August, initially in young adults followed by secondary and then primary school-aged children prior to schools reopening in September 2020. Cases in school-aged children lagged behind and followed adult trends after schools reopened, with a strong age gradient in weekly infection rates. There was a strong (P<0.001) correlation in regional infection rates between adults and secondary (R2=0.96–0.98), primary (R2=0.93–0.94) and preschool-aged (R2=0.62–0.85) children. The November lockdown was associated with declines in adult infection rates, followed a week later, by declines in student cases. From 23 November 2020, cases in adults and children increased rapidly following the emergence of a more transmissible novel variant of concern (VOC-202,012/01; B.1.1.7).
Conclusions
In school-aged children, SARS-CoV-2 infections followed the same trajectory as adult cases and only declined after national lockdown was implemented whilst keeping schools open. Maintaining low community infection rates is critical for keeping schools open during the pandemic.
Keywords: SARS-CoV-2, COVID-19, Schools, Children, Transmission
Introduction
The rapid spread of the SARS-CoV-2, the virus responsible for COVID-19, led many countries to impose strict national lockdowns which, in most countries, included school closures, even though children were relatively spared by the pandemic.1 School closures not only disrupt the education of students, but also affect their physical, mental and social development and wellbeing, as well as restricting access to health visiting, social care and school-based vaccinations, all of which disproportionately impact children from disadvantaged backgrounds, thus exacerbating inequalities.2 , 3
In England, COVID-19 cases started increasing rapidly from March 2020, leading to school closures on 20 March and wider national lockdown on 26 March. Cases eventually plateaued in mid-April and then declined gradually in May, allowing for phased easing of national lockdown.4 From June 2020, preschool children and some primary and secondary school years returned to school until mid-July 2020. Strict infection control and physical distancing measures were implemented,5 resulting in very few cases or outbreaks in educational settings.6 These findings, together with experiences of other countries,1 led to the full reopening of all school years during the Autumn term.5 Unlike the summer half-term, however, community infection rates were higher across England,4 and, while extensive national guidelines were issued for educational settings,5 the large number of children attending school provided unprecedented challenges, particularly for maintaining physical distancing within the educational environment. Additionally, the full reopening of schools increases the number of contacts students had both within and outside educational settings, increasing the risk of infection and transmission among school children, staff, their household members and potentially the wider community. We analysed age-specific regional and national trends of SARS-CoV-2 infections in England from the start of the summer holidays in July 2020 to the full reopening of schools in September 2020 until the end of 2020 to better understand risks and trends in SARS-CoV-2 infections in school-aged children. We also assessed the impact of local restrictions and national lockdown whilst keeping the schools open during November 2020 on SARS-CoV-2 infection rates in students and adults.
Methods
Public Health England (PHE) conducts SARS-CoV-2 surveillance in England and receives daily electronic notifications of SARS-CoV-2 tests through ‘Pillars’.7 In Pillar 1, SARS-CoV-2 RT-PCR tests are undertaken by PHE laboratories and National Health Service (NHS) hospitals for those with a clinical need and for health and care workers. Pillar 2 includes results of Lateral Flow and SARS-CoV-2 RT-PCR tests in the community, which can be requested by anyone with COVID-19 symptoms (fever, new onset cough or loss of smell or taste). The data are collated electronically in the Second-Generation Surveillance System (SGSS).
Timelines
SARS-CoV-2 infections confirmed by RT-PCR in England between 13 July (start of school summer holidays) and 27 December 2020 were analysed. This period included the start of the Autumn term on 07 September, a week-long half-term break from 26 October for most schools and the end of term on 18 December 2020. Because of increasing numbers of cases across different regions in England, local tier restrictions were announced on 12 October 2020,8 with Tier 1 representing medium alert, Tier 2 high alert and Tier 3 very high alert.9 Many parts of northern England and the Midlands were placed in Tier 3 restrictions. Schools remained open in all tiers. With cases continuing to increase nationally, national lockdown was imposed from 05 November to 02 December 2020, whilst keeping schools open.
Data analysis
SARS-CoV-2 tests in school-aged children were categorised by corresponding school year; children born between 01 September and 31 August of the following calendar year were assigned to their respective school years, including nursery [2–3 year-olds], pre-school [3–4 year-olds], reception [4–5 year-olds], primary school years 1 [5–6 year-olds] to 6 [10–11 year-olds], and secondary school years 7 [11–12 year-olds] to 13 [17–18 year-olds]. School years were then categorised into three educational settings: preschools (nursery, preschool), primary schools (reception, years 1–6) and secondary schools (years 7–13). In England, children are educated in secondary schools until school year 11 (15–16 year-olds) and then opt for higher education in school or college, apprenticeships or traineeship, as well as being employed, self-employed or volunteering work. For this analysis, they were grouped as a single cohort in school year 12 (16–17 year-olds) or 13 (17–18 year-olds).
SARS-CoV-2 infection rates in school-aged children were compared to two adult age-groups: all adults (16–64 year-olds representing working-age adults) and young adults (18–29 year-olds, the age group with the earliest, most rapid and highest increase in SARS-CoV-2 infection rates during the second pandemic wave).4 Weekly SARS-CoV-2 infections were calculated using positive cases from Monday to Sunday for each week. Positivity rates were calculated by dividing the number of positive cases with total number of tests performed in that week. Mid-year estimates using 2019/2020 census data (www.statistics.gov) were used as denominators for age and the nine PHE regions.10 Infection rate ratios (IRRs) were used to compare weekly infection rates between age-groups, educational settings and regions, using the group with the lowest weekly infection rate as baseline.
Confidence intervals were calculated as follows:
where e1 and e2 are the number of events in those populations and
95% Confidence Interval (95%CI) = exp(LnIR ± 1.96*SE(LnIR)
Linear regression was used to assess correlation between weekly infection rates in the educational cohorts and adults (18–64 year-olds) in individual English regions. Correlation was assessed for the week of 27 July 2020 (very low infection rates) and 12 October 2020 (very high infection rates). Daily growth rates and doubling times were calculated using statistical software R with the “i2extras” package and included positive cases from the last four weeks before 31 August 2020 and before 19 October 2020.
Results
Infection rate during summer holidays
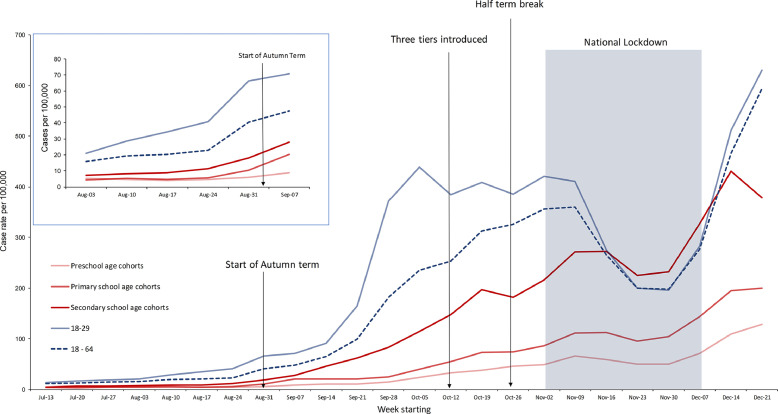
In England, the weekly SARS- CoV-2 infections rate during the summer holidays (13 July to 30 August 2020) was low across all age-groups. There was a consistent trend of increasing SARS-CoV-2 infection rates with increasing age, from preschool-aged children to young adults (18–29 years old) (Fig 1 a), apart from school year 11 having higher weekly infection rates than school year 12 (Fig. 2 ). During the four weeks prior to the start of the school Autumn term (up to and including week beginning 31 August 2020), the daily growth rate of SARS-CoV2 infection rates was relatively stable in preschool-aged and primary school-aged children, but was increasing slowly in secondary school-aged children (daily growth rate, r = 0.00947; 95% CI: 0.00439 to 0.0146) (Supplement Table S1). In young adults, cases had been increasing since 13 July 2020 and accelerated after 03 August 2020 (Fig. 1 b).
Fig. 1.
Weekly infection rates of confirmed COVID-19 cases per 100,000 population per age cohort, England.
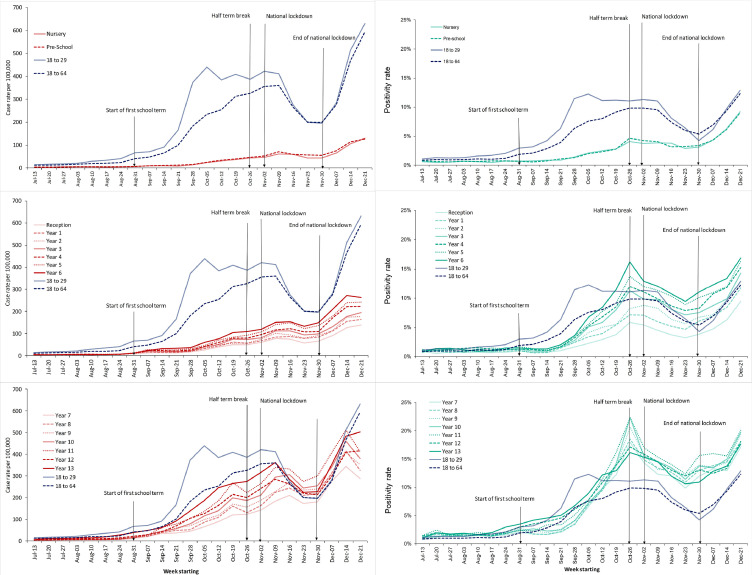
Fig. 2.
Weekly infection rates of confirmed COVID-19 cases per 100,000 population for each school cohort and adult age groups, England.
Infection rates after schools reopening
During the week beginning 24 August 2020, there was an upward inflection in weekly SARS-CoV-2 infection rates in both secondary and primary school-aged children but not in preschool children. Weekly infection rates were higher in young adults than in the three educational cohorts and increased rapidly after 14 September 2020, peaking during the week of 05 October 2020 when infection rates in young adults were 18.32 times (95%CI, 16.42–20.44) higher than in preschool children and then plateaued (Fig. 1 , Supplement Table S2). During the week beginning 19 October 2020, just before the school half-term holidays, the doubling time for SARS-CoV-2 infection rates was 18.2 (95%CI, 15–22.3) days in preschool-aged children, 20.4 (18.8–22.2) days in primary school-aged and 30.1 (28.0–32.5) days in secondary school-aged children (Supplement Table S1).
Age-specific incidence
From the time of schools reopening in September until the week of 16 November 2020, SARS-CoV-2 infection rates remained highest in young adults, followed by secondary, primary and then preschool-aged children (Fig. 2), as evidenced by the weekly IRR trends between these cohorts (Supplement Table S2). During the week of 13 July 2020 (start of summer school holidays), the relative weekly SARS-CoV-2 infection rates compared to preschool-aged children were 1.20 (95%CI, 0.88–1.64) for primary school-aged children, 1.26 (95%CI, 0.92–1.72) for secondary school-aged children and 3.91 (95%CI, 2.93–5.21) for young adults. These rates increased to 1.91 (95%CI, 1.74–2.09), 5.17 (95%CI 4.73–5.65) and 10.73 (95%CI, 9.84–11.71), respectively, during the week of 19 October 2020 (week before half-term holidays) (Supplement Table S2).
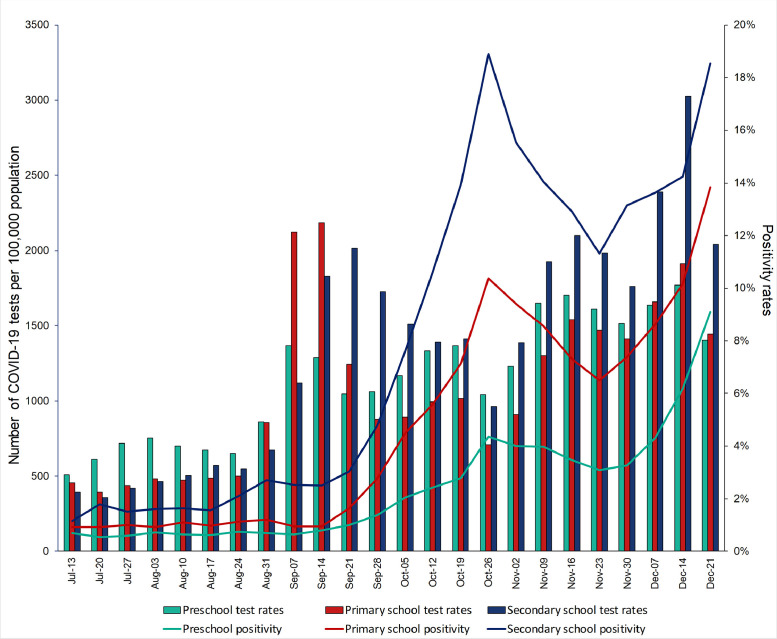
The same trends in weekly SARS-CoV-2 infection rates were also observed in the weekly SARS-CoV-2 infection positivity rates for the three educational settings, which increased throughout the autumn half-term and peaked during the half-term week beginning 26 October 2020, when positivity rates were 4.35% in preschool-aged children, 10.37% in primary school-aged children and 18.89% in secondary school-aged children (Fig. 3 ). This compares with 0.70%, 1.21% and 2.70% during the week prior to schools reopening (August 31, 2020).
Fig. 3.
Weekly COVID-19 test rates per 100,000 population and weekly COVID-19 positivity rates for preschool, primary and secondary school birth cohorts, England.
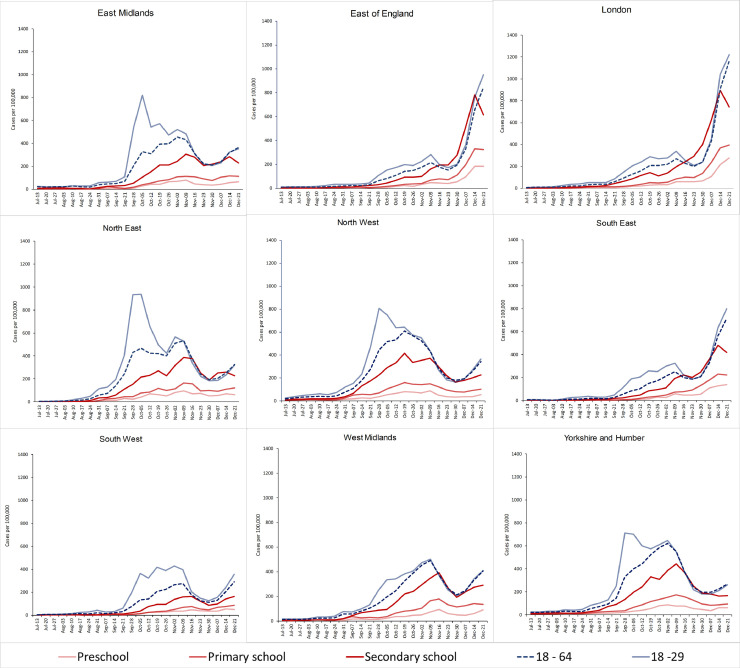
Regional infection rates
The national trends in SARS-CoV-2 infection rates were also observed across the nine English regions although peak infection rates varied in the different regions. A strong and statistically significant (P<0.001) correlation was observed between weekly SARS-CoV-2 infection rates in adults and the three educational cohorts, during both low (27 July 2020) and high (19 October 2020) national weekly incidence, with the strongest correlation observed for secondary school-aged children (Fig. 5).
Fig. 5.
Correlation between weekly SARS-CoV-2 infection rates in adults (18–64 years old) and school cohorts across the nine different regions in England, along with linear regression, correlation coefficient and coefficient of determination R² for the week starting (A) 27 July 2020 (low community infection rates) and (B) 19 October 2020 (low community infection rates).
Impact of school closure during half-term and national lockdown
SARS-CoV-2 infection rates dipped during the half-term school break (week of 26 October 2020) and was associated with fewer tests performed for all three educational cohorts, although positivity rates were highest during this week. The re-opening of schools after the half-term was associated with continuing increase in SARS-CoV-2 infection rates across all educational settings and at the same rate as the weeks prior to the half-term holiday (Fig. 1). In adults, trends in SARS-CoV-2 infection rates remained unchanged.
Following national lockdown in 05 November 2020, cases in adults plateaued and then fell rapidly. Similar trends were observed in secondary and primary educational settings but with a one-week lag, such that, for the first time in England, adult infection rates fell below secondary school-aged children (Fig. 1). Concomitant reductions in SARS-CoV-2 test numbers and positivity rates were observed (Fig. 3).
From 23 November, weekly infection rates plateaued in adults and school-aged children, and then increased rapidly a week later (Fig. 1). SARS-CoV-2 infection positivity rates, too, reached a nadir in the same week and then increased rapidly until the end of the year (Fig. 3). Regionally, the decline in weekly infection rates following national lockdown was most marked in areas with high SARS-CoV-2 infection rates (>350/100,000), especially northern England, where large declines were first observed in young adults followed by secondary school-aged children, with smaller declines in primary schools-aged and preschool-aged children (Fig. 4 ). In the East of England, South East and in the London region, SARS-CoV-2 infection rates were relatively low (<350/100,000) during the second wave and, whilst national lockdown in November was also associated with an initial decline in adult infection rates, these declines were more moderate. In these regions, however, weekly infection rates plateaued temporarily in school-aged children and then increased rapidly across all three educational cohorts until the end of the year (Fig. 4).
Fig. 4.
Regional weekly infection rates of confirmed COVID-19 cases per 100,000 population for school cohorts and adult age groups, England.
Discussion
We used national surveillance data to monitor trends in weekly SARS-CoV-2 infection rates in school-aged children following the full reopening of all school years in September 2020. We found that SARS-CoV-2 infection rates In England were very low during early summer 2020, but started to increase from August 2020, initially in young adults, followed by secondary and primary school-aged children, with little change in preschool-aged children. These increases started before schools reopened and continued across all educational cohorts until the end of the year. SARS-CoV-2 infections rates increased with age across the three educational settings and lagged behind trends in young adults. There was a strong correlation in regional weekly infection rates between adults and secondary school-aged children, during periods of both low and high community incidence. The correlation was weaker but remained statistically significant for primary school-aged and preschool-aged children. National lockdown in November 2020 whilst keeping schools open was associated with rapid declines in SARS-CoV-2 infection rates, initially in young adults followed a week later by declines by secondary school-aged children and then primary school-aged children. These trends were most noticeable in English regions with moderate-to-high infection rates prior to lockdown. Infection rates in children, however, reached a nadir during the week of 23 November 2020 and, in regions with lower SARS-CoV-2 infection rates during the second wave, namely the South East, East of England and the London region, increased in all three educational cohorts until the end of the year with the highest increases observed in secondary school-aged children.
In England, SARS-CoV-2 RT-PCR testing is free and available to individuals of any age with COVID-19 symptoms of fever, new onset cough, anosmia or ageusia. Whilst acknowledging that asymptomatic infections will not be captured in this dataset and that asymptomatic infections may vary across the age-groups, with young children more likely to have asymptomatic and mild, transient infections than older children or adults,11 the observed trends over time, especially relative to adults, should not be affected. We observed a strong age effect, with SARS-CoV-2 infection rates increasing with each school year-group, except in school year 12 (higher education/college) which was lower than in year 11 (final year of secondary school). We speculate that the students in the final year of secondary schools were more likely to have a wider network of contacts compared to those in the year 12, who may be starting higher education in a different school, attending college or beginning an apprenticeship outside the educational setting.
The full reopening of school during the Autumn term raised important questions about the risk of SARS-CoV-2 infection and transmission both within and outside educational settings. Even if very few children became infected, the large numbers of children returning to school significantly increased their average number of contacts and, therefore, opportunities for transmission. So far, investigations focusing on individual outbreaks generally reported low rates of transmission among pupils and staff, especially in preschool and primary school settings.6 , 12 , 13 Some countries had kept their schools open during their lockdown and did not see any increase in cases among children or in the wider community.1 Large outbreaks have, however, been reported in secondary schools, possibly because older children may be more susceptible and more efficient transmitters of the virus than younger children, as well as having different behavioural contact patterns with each other and those around them.14, 15, 16
During the summer half-term in England, the reopening of preschools and some primary school years, along with strict infection control measures,5 was associated with very few cases or outbreaks, with more than half the outbreaks affecting staff only.6 Similar experiences were reported in Germany, Netherlands and other European countries during summer 2020.17 , 18
It has been proposed that the decision to reopen schools should be based on indicators of low community infection rates (based on incidence or test positivity rates) and the ability of schools to implement safe physical distancing and infection control measures.1 , 19 We found a strong correlation in weekly infection rates between adults and all three educational cohorts during periods of both low and high community infection rates. This correlation was strongest for secondary school-aged children and less so for preschool-aged children, which is plausible because secondary school-aged students are only just younger than the young adults and likely to have similar social contacts and behaviour patterns as young adults.
Notably, too, the implementation of a second national lockdown whilst keeping schools open in November 2020 was associated with rapid and large declines in adult infection rates nationally and across most English regions, especially those experiencing the highest infection rates. In these regions, it is likely that the 3-tier system, where regions with the highest infection rates were placed into Tier 3 (very high alert) from 12 October 2020, also helped control the spread of the virus and could explain the rapid decline in infection rates as soon as national lockdown was announced.9 By the end of November 2020, infection rates in secondary school-aged children were, for the first time in England, higher than in young adults but, soon after, infection rates started increasing rapidly across all age-groups until the end of the year, especially in the South East, East of England and the London region. These increases were subsequently associated with rapid spread of a novel variant of concern (VOC-202012/01; B.1.1.7), which is more transmissible than pre-existing strains.20
Strengths and limitations
The strength of this analysis lies in the near real-time availability of national and regional surveillance data during a period when widespread testing was available. The large volume of tests and the consistency of reporting have provided a wealth of information on (symptomatic) disease burden, whilst the consistency of testing has provided useful insight on disease trends across age-groups and over time. We, however, do not have information on the reason for testing, potential source of infection among positive cases or illness severity. Additionally, our data, however, only included cases that presented to a national testing centre, primarily because they had COVID-19 symptoms, and may be subject to bias testing behaviour in the different age-groups and, potentially, over time. It is, for example, likely that the incentive to get tested will be low, especially for mild or atypical symptoms, because of the self-imposed isolation period for positive cases and their household members. These, along with lack of testing in asymptomatic individuals, would have had an impact on the analysis, especially because asymptomatic infections are likely to be different across the age-groups.11 The contribution of asymptomatic infections in each age-group, however, remains uncertain. A recent school infection survey, for example, identified asymptomatic infections in 1.5% of secondary school students compared to 0.9% of primary school students in England, although this difference was not statistically significant.21 We also analysed data according to the age of the children and their corresponding school year, but without knowledge of whether they were attending school, although school attendance rates in state-funded remained very high throughout the autumn term.22 Another important limitation is that schools closed soon after the emergence of the novel SARS-CoV-2 variant of concern in late November and are yet to re-open in England. Ongoing surveillance, ideally supplemented with genomic surveillance of circulating strains, will be critical for monitoring SARS-CoV-2 infection and transmission when schools reopen in 2021.
Conclusions
Our data show that, in England, childhood cases closely followed adult infection rates and national lockdown whilst keeping schools open was associated with large declines in SARS-CoV-2 infection rates, first in adults and then in school-aged children. The strong regional correlation between adult and childhood infection rates highlights the important of maintaining low community infection rates to allow schools to remain open safely through the pandemic.
Declaration of Competing Interest
We declare no conflicts of interest.
Acknowledgments
Funding
This surveillance was internally funded by PHE. SAI is supported by a Wellcome Trust Clinical Training Fellowship (Ref No 215654/Z/19/Z).
Ethical approval
PHE has legal permission, provided by Regulation 3 of The Health Service (Control of Patient Information) Regulations 2002, to process patient confidential information for national surveillance of communicable diseases.
Contributors
AAM: Methodology; Formal analysis; Investigation; Data curation; Writing the original draft; Writing – review and editing; Visualisation
MS, AZ, LC, RS: Data curation; Writing- review and editing
SAI: Methodology, Writing – review and editing
VS, MER and SNL: Conceptualisation; Methodology; Supervision; Writing – review and editing
Data sharing
Applications for relevant anonymised data should be submitted to the Public Health England Office for Data Release: https://www.gov.uk/government/publications/accessing-public-health-england-data/about-the-phe-odr-and-accessing-data.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jinf.2021.02.022.
Appendix. Supplementary materials
References
- 1.Levinson M., Cevik M., Lipsitch M. Reopening primary schools during the pandemic. N Engl J Med. 2020;383:981–985. doi: 10.1056/NEJMms2024920. [DOI] [PubMed] [Google Scholar]
- 2.Snape M.D., Viner R.M. COVID-19 in children and young people. Science. 2020;370:286–288. doi: 10.1126/science.abd6165. [DOI] [PubMed] [Google Scholar]
- 3.Viner R.M., Bonell C., Drake L. Reopening schools during the COVID-19 pandemic: governments must balance the uncertainty and risks of reopening schools against the clear harms associated with prolonged closure. Arch Dis Child. 2020 doi: 10.1136/archdischild-2020-319963. Aug 3;archdischild-2020-319963Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Public Health England (PHE). Weekly coronavirus disease 2019 (COVID-19) surveillance report: summary of COVID-19 surveillance systems. 2020. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/880925/COVID19_Epidemiological_Summary_w17.pdf. Accessed: 12 February 2021.
- 5.Department for Education (DfE). Guidance for full opening: schools. 2020. Available at: https://www.gov.uk/government/publications/actions-for-schools-during-the-coronavirus-outbreak/guidance-for-full-opening-schools. Accessed: 12 February 2021.
- 6.Ismail S., Saliba V., Lopez-Bernal J., Ramsay M., Ladhani S. SARS-CoV-2 infection and transmission in educational settings: cross-sectional analysis of clusters and outbreaks in England. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30882-3. Published Online December 8, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang Y., Ma Z.F. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning province, China: a cross-sectional study. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17072381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prime Minister's Office. Prime minister announces new local COVID alert levels, 12 October 2020. 2020. Available at https://www.gov.uk/government/news/prime-minister-announces-new-local-covid-alert-levels. Accessed: 12 February 2021.
- 9.Department of Health and Social Care (DHSC). Local restriction tiers: what you need to know 2020. Available at: https://www.gov.uk/guidance/local-restriction-tiers-what-you-need-to-know. Accessed: 12 February 2021.
- 10.Office for National Statistics (ONS). Dataset: population projections for regions - Table 1. 2020. Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections/datasets/regionsinenglandtable1. Accessed: 12 February 2021.
- 11.Buitrago-Garcia D., Egli-Gany D., Counotte M.J. Occurrence and transmission potential of asymptomatic and presymptomatic SARS-CoV-2 infections: a living systematic review and meta-analysis. PLoS Med. 2020;17 doi: 10.1371/journal.pmed.1003346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Viner R.M., Russell S.J., Croker H. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Health. 2020;4:397–404. doi: 10.1016/S2352-4642(20)30095-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Macartney K., Quinn H.E., Pillsbury A.J. Transmission of SARS-CoV-2 in Australian educational settings: a prospective cohort study. Lancet Child Adolesc Health. 2020;4:807–816. doi: 10.1016/S2352-4642(20)30251-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stein-Zamir C., Abramson N., Shoob H. A large COVID-19 outbreak in a high school 10 days after schools' reopening, Israel, May 2020. EuroSurveill. 2020;25(29) doi: 10.2807/1560-7917.ES.2020.25.29.2001352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fontanet A., Tondeur L., Madec Y. Cluster of COVID-19 in northern France: a retrospective closed cohort study. MedRxiv. 2020 doi: 10.1101/2020.04.18.20071134. [DOI] [Google Scholar]
- 16.Fontanet A., Grant R., Tondeur L. SARS-CoV-2 infection in primary schools in northern France: a retrospective cohort study in an area of high transmission. MexRxIV. 2020 doi: 10.1101/2020.06.25.20140178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Otte Im Kampe E., Lehfeld A.S., Buda S., Buchholz U., Haas W. Surveillance of COVID-19 school outbreaks, Germany, March to August 2020. EuroSurveill. 2020;25(38) doi: 10.2807/1560-7917.ES.2020.25.38.2001645. pii=2001645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Couzin-Frankel J., Vogel G., Weiland M. Not open and shut. Science. 2020;369:241–245. doi: 10.1126/science.369.6501.241. [DOI] [PubMed] [Google Scholar]
- 19.Center for Disease Control and Prevention (CDC). Indicators for dynamic school decision-making, updated September 15, 2020 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/indicators.html#thresholds. Accessed: 12 February 2021.
- 20.Public Health England (PHE). Investigation of novel SARS-COV-2 variant: variant of concern 202012/01 (21 December 2020). 2020. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/959438/Technical_Briefing_VOC_SH_NJL2_SH2.pdf. Accessed: 12 February 2021.
- 21.Office for National Statistics (ONS). COVID-19 schools infection survey round 1, England: November 2020. 17 December 2020. Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/covid19schoolsinfectionsurveyround1england/november2020. Accessed: 12 February 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.