Abstract
The novel coronavirus disease 2019 (COVID-19) pandemic has been an overwhelming challenge for worldwide health systems. Since the beginning of year 2020, COVID-19 has represented a potential harm for cancer patients and has often hindered oncology care. The Collegio Italiano dei Primari Oncologi Medici (CIPOMO) is an Italian association of head physicians in oncology departments, which promotes working and research activities in oncology on a national basis. During the second wave of COVID-19 pandemic, the CIPOMO promoted a national survey aiming to evaluate the impact of COVID-19 on oncologists' clinical activity and what changes have been made compared with the Italian situation during the first wave of the pandemic. Overall, 138 heads of medical oncology departments participated in this survey: 75 (54%) from the North, 24 (17%) from the Centre and 39 (28%) from the South of Italy and islands. This survey provides an overview of Italian oncologists facing the second wave of COVID-19 pandemic. The lesson learned during the first wave of COVID-19 pandemic has led to a better organisation of clinical activities, and regular testing among healthcare practitioners, with better chances to grant patients' protection. However, the lack of standardised informatic platforms results in serious challenges in replacing frontal visits, often making a concrete reduction of patients' hospital accesses unfeasible.
Oncologists need to keep preserving the continuum of care of patients. Standardisation of safety measures, together with the implementation of informatic platforms, can significantly improve oncology pathways during this second wave of COVID-19 pandemic.
Keywords: Cancer, COVID-19, Pandemic, Health care, Oncology
From the beginning of year 2020, the coronavirus disease 2019 (COVID-19) pandemic has been an overwhelming challenge for worldwide health systems [1]. As with other serious infectious diseases, available data suggest that patients with cancer might be more at risk for an increased mortality in case of COVID-19 [2,3]. Namely selected populations of patients with cancer, as elderly subjects and those affected by haematological malignancies or lung cancer seem to be at increased risk of poor outcomes [4]. During the first wave of COVID-19 pandemic, several efforts have been made to reduce the risk of infection among patients with cancer accessing oncology facilities, with the aid of structured recommendations and guidelines [5,6]. The use of telemedicine has frequently allowed effective remote monitoring of patients, even in case of confirmed COVID-19 diagnosis [7]. Nevertheless, oncology activities have been severely endangered by this infectious threat, also due to the significant reduction of healthcare activities related to the contamination of physicians and caregivers [8].
Since March 2020, Italy has been heavily hit by COVID-19 [9,10]. The subsequent overburden of the national health system required oncologists to implement measures to safely carry on the everyday clinical activity [[11], [12], [13]]. At the beginning of COVID-19 pandemic in Italy, the Italian college of directors of the National Health System of the Hospital Department of Medical Oncology (Collegio Italiano dei Primari Oncologi Medici Ospedalieri [CIPOMO]) promoted a nationwide survey regarding the reorganisation of Italian oncology departments [14]. The results of this survey suggested that Italian oncology departments promptly set a proactive approach to the COVID-19 emergency, however with significant differences due to the lack of clear indications provided to healthcare practitioners in oncology [14].
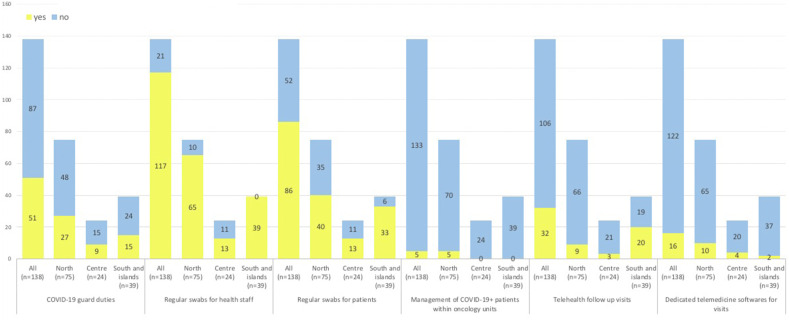
As the second wave of COVID-19 pandemic has approached, the CIPOMO launched another nationwide survey aiming to evaluate the oncology pathways in Italy during COVID-19. The survey was sent online on November 17th and closed on December 9th 2020. Overall, 138 heads of medical oncology departments participated in this survey: 75 (54%) from the North, 24 (17%) from the Centre, and 39 (28%) from the South of Italy and islands. The results of the survey are shown in Fig. 1 .
Fig. 1.
Overview of survey result.
The survey focused on six key points. The first question regarded the organisation of oncology staff during the pandemic, and specifically whether oncologists had been assigned COVID-19 ward duties. Answers to this question suggest that medical oncologists have been largely spared from this activity (63%); still, a significant proportion of them were committed to COVID-19 ward duties (37%), with a superimposable distribution on the national territory (36% in the North, 37.5% in the Centre and 38% in the South of Italy and islands). Compared with the results of the previous survey, there has been a substantial increase in the employment of oncology resources in COVID-19 dedicated wards, which are now equal to those observed in the high-risk areas (so-called ‘red zone’) during the first wave [14].
The following two questions focused on testing methods for patients and healthcare practitioners within oncology facilities. At the present time, regional council decisions have stated that healthcare practitioners should undergo COVID-19 rhinopharyngeal swabs on a regular basis (ideally every 14 days) only in 7 of 20 Italian regions (4 in the North, 2 in the Centre, and 1 in the South of Italy). However, based on the results of our survey, after hospital recommendations the majority of oncology departments perform regular (i.e. every 14 days) COVID-19 surveillance among healthcare practitioners (85%). However, there is a significant difference among Italian regions, with the totality of oncology departments in the South, 87% in the North,and 54% in the Centre of Italy performing regular COVID-19 swabs. Regarding COVID-19 testing measures among patients, more than half of oncology departments regularly test patients accessing Day Hospitals (62%), usually 15–21 days before cancer treatment administration. Similarly, there is a high discrepancy over the National territory, with 53% and 54% of patients undergoing regular swabs in the North and Centre, respectively, compared with 85% of patients in the South of Italy and islands. Because these two items were not specifically addressed in the previous survey, it is not possible to compare the actual situation with the first wave of COVID-19 pandemic. However, these data suggest that even in this second wave, COVID-19 surveillance practices are inhomogeneously distributed through the Italian territory, presumably due to the lack of standardised procedures but also to limited resources.
The fourth question addressed whether COVID-19-positive patients diagnosed by means of surveillance procedures are managed within the oncology units, or rather addressed to family doctors and territory health services. The near totality of COVID-19 cancer patients is managed on a territory basis (96%), with only a minority monitored by oncologists (4%, all in the North of Italy). The possibility to entrust patients with cancer to general doctors has significantly reduced the burden of oncologists' activities, allowing adequate observation of patients with COVID-19 during the course of disease, and potential indication for hospitalisation in case of more severe cases.
The last part of the survey regarded alternative modalities to keep in touch with patients, to reduce direct access to hospitals for follow up (non-urgent) visits. Over the first wave of COVID-19 pandemic, telehealth has been proposed as an adequate surrogate to replace frontal visits. However, results from our survey suggest that the majority of Italian oncology departments still perform frontal visits and do’ not rely on telehealth devices (23%), with a superimposable distribution in the North and Centre (12% and 12.5%, respectively), compared with 51% in the South of Italy. Consistent with these results, most oncology department do n’t have access to a dedicated informatic platform to exchange medical information with patients to replace frontal visits. Indeed, only 11% of oncology departments over the National territory have access to this kind of informatic facility (13% in the North, 17% in the Centre and only 5% in the South of Italy), suggesting that implementation of such resources has not substantially changed from the first wave of COVID-19 pandemic. Overall, these results suggest that optimisation of preventive measures to reduce the risk of COVID-19 diffusion (e.g. avoiding the hospital access to caregivers, performing triage procedures to patients) might allow to carry on clinical activity in oncology.
This survey provides an overview of Italian oncologists facing the second wave of COVID-19 pandemic. Overall, the lesson learned during the first wave of COVID-19 pandemic has led to a better organisation of clinical activities, and regular testing among healthcare practitioners, with better chances to grant patients' protection. However, the lack of standardised informatic platforms results in serious challenges in replacing frontal visits, often making a concrete reduction of patients' hospital accesses unfeasible.
COVID-19 has revolutionised healthcare worldwide, with unprecedented impact on cancer care. Clinical practice has substantially changed with the implementation of protective and preventive measures [15]. In most cases, during the first wave of COVID-19 pandemic, routine oncology care for patients with metastatic cancer has been maintained without significant difference before and after the COVID-19 outbreak [16]. As an example, strategic countermeasures to maintain the continuity of cancer care in South Korea based on the following elements: rapid implementation of nationwide healthcare protocols; establishment of widespread diagnostic capacities; effective spreading of preventive measures against COVID-19 community transmission (e.g. contact tracing, quarantine, and isolation); redesigning triage and treatment systems; and mobilisation of resources for case management [16]. However, dealing with this emergency has often collided with the challenges of healthcare systems to face the shortage of human resources, and with the impact of the pandemic on the economic systems [5].
Results of this survey suggest there are several issues that need to be further implemented, with the aid of standardised procedures. First, there is need to preserve patients with cancer and cancer-related activities. This includes preservation of medical staff, whose commitment to COVID-19 wards should be minimised, and of patients with cancer by ensuring triage procedures and regular COVID-19 testing for both healthcare practitioners and patients [17]. The psychological impact of COVID-19 on patients with cancer should not be underestimated, and psycho-oncological support for patients and caregivers should be considered, as forthcoming COVID-19 outbreaks are expected in the next future [18]. Cancer research should also be preserved, as the COVID-19 has prolonged over months with potentially negative impact on the conduction of clinical trials [19].
Second, adequate allocation of working resources should be implemented, to reinforce territory health services thus reducing the working burden of medical oncologists and allowing to carry on hospital activities. Finally, data are needed regarding risk categorisation of patients with cancer, as well as prioritisation of treatment procedures, to better define oncology pathway over the second wave of COVID-19 pandemic. Available data suggest that, with due precautions and dedicated devices, oncology care can be safely preserved during COVID-19 emergency situation [20]. Over the last months, a novel clinical care has been established with the aid of continuous research and international cooperation, and will be implemented to successfully face COVID-19.
Authors’ contribution
Alice Indini: Writing – original draft, Formal Analysis, Data Curation. Graziella Pinotti: Conceptualization, Methodology, Supervision. Fabrizio Artioli: Visualization, Validation, Writing – review & editing. Carlo Aschele: Visualization, Investigation, Writing – review & editing. Daniele Bernardi: Visualization, Validation, Writing – review & editing. Alfredo Butera: Visualization, Data curation, Writing – review & editing. Efisio Defraia: Visualization, Validation, Writing – review & editing. Gianpiero Fasola: Visualization, Investigation, Writing – review & editing. Teresa Gamucci: Visualization, Data curation, Writing – review & editing. Monica Giordano: Visualization, Data curation, Writing – review & editing. Antonino Iaria: Visualization, Validation, Writing – review & editing. Silvana Leo: Visualization, Validation, Writing – review & editing. Angela Stefania Ribecco: Visualization, Validation, Writing – review & editing. Riccardo Rossetti: Visualization, Investigation, Writing – review & editing. Clementina Savastano: Visualization, Validation, Writing – review & editing. Marina Schena: Visualization, Data curation, Writing – review & editing. Rosa Rita Silva: Visualization, Validation, Writing – review & editing. Francesco Grossi: Conceptualization, Methodology, Supervision, Writing – review & editing. Livio Blasi: Conceptualization, Methodology, Supervision.
Funding
No funding was obtained for the present investigation.
Conflict of interest statement
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this article.
Acknowledgements
The authors thank all the CIPOMO members for participating in the present survey, thereby making this work possible to be shared in the oncologists' community.
References
- 1.The World Health Organization (WHO). Available at:: https://www.who.int/health-topics/coronavirus#tab=tab_1. Accessed December 21st 2020.
- 2.Guan W.J., Ni Z.Y., Hu Y., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saini K.S., Tagliamento M., Lambertini M., et al. Mortality in patients with cancer and coronavirus disease 2019: a systematic review and pooled analysis of 52 studies. Eur J Canc. 2020;139:43–50. doi: 10.1016/j.ejca.2020.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Joode K., Dumoulin D.W., Tol J., et al. Dutch Oncology COVID-19 consortium: outcome of COVID-19 in patients with cancer in a nationwide cohort study. Eur J Canc. 2020;141:171–184. doi: 10.1016/j.ejca.2020.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Raymond E., Thieblemont C., Alran S., Faivre S. Impact of the COVID-19 outbreak on the management of patients with cancer. Targeted Oncol. 2020;15(3):249–259. doi: 10.1007/s11523-020-00721-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Giesen N., Sprute R., Rüthrich M., et al. Evidence-based management of COVID-19 in cancer patients: guideline by the infectious diseases working party (AGIHO) of the German society for haematology and medical oncology (DGHO) Eur J Canc. 2020;140:86–104. doi: 10.1016/j.ejca.2020.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scotté F., Minvielle E., Mir O., et al. A patient reported outcome platform, a useful tool to improve monitoring and effective management of Covid-19-positive patients with cancer. Eur J Canc. 2020;132:1–4. doi: 10.1016/j.ejca.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fauci A.S., Lane H.C., Redfield R.R. Covid-19 - navigating the uncharted. N Engl J Med. 2020;382(13):1268–1269. doi: 10.1056/NEJMe2002387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aschele C., Negru M.E., Pastorino A., et al. Incidence of SARS-CoV-2 infection among patients undergoing active antitumor treatment in Italy. JAMA Oncol. 2020 doi: 10.1001/jamaoncol.2020.6778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guarneri V., Bassan F., Zagone V., et al. Epidemiology and clinical course of severe acute respiratory syndrome coronavirus 2 infection in cancer patients in the Veneto Oncology Network: The Rete Oncologica Veneta covID19 study. Eur J Canc. 2021;147:120–127. doi: 10.1016/j.ejca.2021.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Indini A., Cattaneo M., Ghidini M., et al. Triage process for the assessment of coronavirus disease 2019-positive patients with cancer: the ONCOVID prospective study. Cancer. 2020 Dec 3 doi: 10.1002/cncr.33366. Epub ahead of print. PMID: 33270908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Trapani D., Marra A., Curigliano G. The experience on coronavirus disease 2019 and cancer from an oncology hub institution in Milan, Lombardy Region. Eur J Canc. 2020;132:199–206. doi: 10.1016/j.ejca.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zuliani S., Zampiva I., Tregnago D., et al. Organisational challenges, volumes of oncological activity and patients' perception during the severe acute respiratory syndrome coronavirus 2 epidemic. Eur J Canc. 2020;135:159–169. doi: 10.1016/j.ejca.2020.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Indini A., Aschele C., Cavanna L., et al. Reorganisation of medical oncology departments during the novel coronavirus disease-19 pandemic: a nationwide Italian survey. Eur J Canc. 2020;132:17–23. doi: 10.1016/j.ejca.2020.03.024. [DOI] [PubMed] [Google Scholar]
- 15.Dong S., Luo C., Hu X., et al. Expert consensus for treating cancer patients during the pandemic of SARS-CoV-2. Front Oncol. 2020;10:1555. doi: 10.3389/fonc.2020.01555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee S., Lim A.R., Kim M.J., et al. Innovative countermeasures can maintain cancer care continuity during the coronavirus disease-2019 pandemic in Korea. Eur J Canc. 2020;136:69–75. doi: 10.1016/j.ejca.2020.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arpino G., De Angelis C., De Placido P., et al. Optimising triage procedures for patients with cancer needing active anticancer treatment in the COVID-19 era. ESMO Open. 2020;5(5) doi: 10.1136/esmoopen-2020-000885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Joode K., Dumoulin D.W., Tol J., et al. Dutch Oncology COVID-19 consortium: outcome of COVID-19 in patients with cancer in a nationwide cohort study. Eur J Canc. 2020;141:171–184. doi: 10.1016/j.ejca.2020.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pinto C., Cagnazzo C. Indications regarding the management of interventional clinical trials with drugs during the current COVID-19 emergency in Italy. ESMO Open. 2020;5(2) doi: 10.1136/esmoopen-2020-000782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Omarini C., Maur M., Luppi G., et al. Cancer treatment during the coronavirus disease 2019 pandemic: do not postpone, do it! Eur J Canc. 2020;133:29–32. doi: 10.1016/j.ejca.2020.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]