Abstract
Objectives:
Knee injury prevention programs (IPPs) reduce knee and anterior cruciate ligament (ACL) injury rates in female athletes, however, implementation of IPPs is low. The purpose of this study was to identify barriers to implementation of IPPs among collegiate women’s soccer coaches.
Design:
Cross-sectional survey.
Methods:
A custom survey based on the RE-AIM (reach, effectiveness, adoption, implementation, maintenance) framework and existing literature was sent to 151 out of 153 women’s National Collegiate Athletic Association (NCAA) soccer coaches in the NCAA’s Eastern Region.
Results:
Ten respondents reported that they did not use an IPP (Non-users), and nineteen respondents reported that they did use an IPP (Users). “Cost” was the most highly ranked barrier (median rank: 2) to implementing an IPP among Non-users. For the statement, “Who should be responsible for completing an IPP,” Users said “Coaches” (47%) and “Other” (21%), while Non-users said “Strength and conditioning” (50%) and “Athletic trainers” (30%). Respondents who marked “Other”, elaborated that it was the responsibility of coaches, athletes, and additional staff members.
Conclusions:
Cost was the primary barrier to implementation of an IPP. Since the majority of Non-users indicated that implementation of an IPP was the responsibility of a non-coaching staff member, cost may be a surrogate for the expense of hiring an additional staff member rather than the cost of performing the IPP itself. Additionally, using a team-based approach that encompasses athletes, coaches, and non-coaching staff members may support long-term implementation of IPPs.
Keywords: Athletic injuries, Knee injuries, Anterior cruciate ligament, Exercise therapy
1. Introduction
Lower extremity injuries are a significant problem for soccer players.1 For example, for a National Collegiate Athletic Association (NCAA) women’s soccer team with twenty-two players, on average, at least player will incur an anterior cruciate ligament (ACL) injury every two seasons.2 Consequently, a number of exercise-based injury prevention programs (IPPs) have been designed to reduce the rate of lower extremity injuries among women’s soccer players by addressing biomechanical technique and neuromuscular control.3 Many IPPs are free to users and have been designed so that they can be implemented by coaches who do not have a background in the health sciences.4,5
Strong evidence exists that the rate of traumatic knee injuries and other lower extremity injuries can be reduced through participation in an IPP.6–8 There is limited research on adherence and fidelity to IPPs among coaches and athletes, but the existing research suggests that these programs are underused.4 A survey of 101 youth soccer coaches reported that only 29% utilized an IPP.9 Lack of education and exposure to IPPs has been suggested as a potential barrier to implementation.9 In a trial of an educational intervention in a youth soccer club with a mandate for all coaches to adhere to an IPP, however, only 53% of coaches were adherent to the IPP at the end of the soccer season.10 This suggests that barriers to implementation of IPPs beyond education exist.
The time commitment needed to complete an IPP has also been cited as a perceived barrier to implementation among youth soccer coaches.11–14 In a survey of Norwegian girls’ soccer coaches, coaches were 87% less likely to be compliant with completing an IPP if they thought it was time-consuming.12 The impact of time commitment on implementation of IPPs among NCAA women’s soccer coaches have not been studied before. NCAA soccer is unique as players are restricted to a maximum of 20 hours per week of participation in soccer-related activities. Therefore, it is possible that time commitment is a perceived barrier to implementation that persists at the NCAA level.
The impact of IPPs on athletic performance is also a growing area of research. Participation in the 11+ for a single season led to significant improvements in dynamic balance among female youth soccer players in one study, and led to an improvement in static plank hold time in another.15 Some hypothesize that if participation in IPPs can be directly linked to improvements in performance, coaches may be more willing to implement and adhere to IPPs.15–17 Lower injury rates have been associated with better team placements in professional soccer, and teams with lower injury incidence and fewer severe injuries had higher league placements, suggesting that injury prevention is an advantageous investment.17,18 However, whether performance or league placement influences collegiate soccer coaches’ willingness to implement an IPP has not been studied before.
Implementation does not solely refer to adoption of an intervention, but also encompasses long-term adherence to the intervention and fidelity to using the intervention as it was intended to be used.4 Higher adherence to an IPP is associated with greater efficacy of the IPP.19 For coaches who do choose to implement an IPP, many end up modifying the content of the IPP overtime, losing fidelity.10,20–22 In a study of adolescent Swedish soccer teams, only 26% of coaches reported using an IPP without modifications three years after originally implementing it.20 It is unknown whether modifications to established IPPs influence their efficacy, however, players who have a higher adherence rate to an IPP demonstrate lower injury rates.4,19,20
Barriers to implementation and adoption of IPPs among youth, high school, and professional soccer teams have been studied before.9,21,22 Collegiate soccer players represent a unique population as teams may have more resources and auxiliary personnel to support implementation of an IPP when compared to youth and high school teams. Players are also closer to the age-range where IPPs are most effective when compared to professional players.6 Therefore, our primary aim for this study was to identify barriers for implementation of IPPs among NCAA women’s soccer coaches, and our secondary aim was to identify barriers to adherence to IPPs for NCAA women’s soccer coaches who are currently using them. We hypothesized that coaches would identify lack of time and minimal impact on sport performance as primary barriers to implementation of IPPs.
2. Methods
A custom survey based on the RE-AIM framework and existing studies on implementation science was created to explore the attitudes, beliefs, and behaviors of soccer coaches regarding injury prevention programs (Appendix 1).9,22,23 RE-AIM framework is an implementation science framework that consists of 5 dimensions (reach, effectiveness, adoption, implementation, maintenance) (Appendix 1 in Supplementary material). This framework is helpful in improving the transparency and the external and internal validity of implementation research. Coaches who indicated in the survey that they use an IPP were asked additional questions about their use of and fidelity to the IPP. Prior to distribution, the survey was pilot-tested for question face validity by three physical therapists each PhD trained, all with a background in sports medicine, and one who also had a background in implementation science. The survey was then pilot-tested for question face validity by three women’s NCAA soccer coaches who were either retired or outside of the Eastern Region.
The University of Delaware Human Subjects Review Board determined that this research met the US Federal criteria as research exempt from review prior to survey distribution. All survey responses were anonymous. The survey was distributed via the online platform Qualtrics. The survey link was emailed to all Division 1 (D1), Division 2 (D2), and Division 3 (D3) women’s soccer coaches in the NCAA’s Eastern Region five times during the 2019–2020 academic year. Email addresses were obtained from school’s publicly available athletics websites. Prior to participation in the survey, all participants were required to complete a digital consent form. Logic-based testing was utilized to avoid question redundancy, and consequently some coaches were asked a slightly different set of questions than others. The survey link was single-use so that duplicate answers would not be obtained from coaches.
3. Results
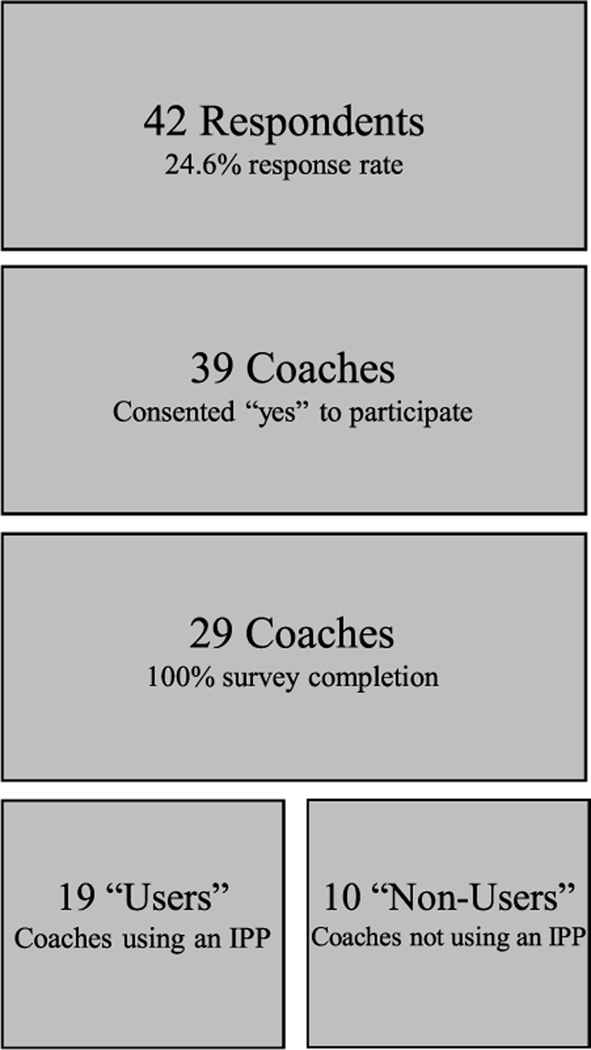
A total of 171 out of 173 women’s soccer coaches in the NCAA Eastern Region were contacted at least one time during the 2019–2020 school year. Forty-two responses were recorded (25% response rate), with 41 respondents consenting to participate and 1 respondent declining to participate. One respondent was a strength and conditioning coach and that data will not be reported. Twenty-nine coaches fully completed the survey, and reported that they were the head soccer coach for their team (Fig. 1). Demographic characteristics of coaches with 100% completion rate of the survey can be found in Table 1.
Fig. 1.
Diagram of survey response rate and participant distribution (IPP: injury prevention program).
Table 1.
Demographics of respondents with 100% survey completion rate. *NAIA: National Association of Intercollegiate Athletics.
| Users (N=19) | Non-users (N=10) | |
|---|---|---|
| D1: 10 | D1: 2 | |
| Division | D2: 2 | D2: 2 |
| D3: 7 | D3: 6 | |
| Highest level played | *NAIA: 0 | NAIA: 1 |
| NCAA: 10 | NCAA: 8 | |
| Semi-professional: 1 | Semi-professional: 0 | |
| Professional: 8 | Professional: 1 | |
| Coaching experience (years) | 19.9±8.9 | 16.4±10.2 |
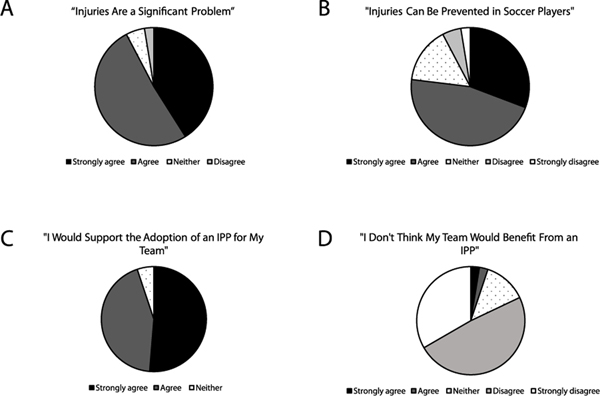
Thirty-nine coaches answered introductory survey items regarding IPP beliefs and attitudes. For the statement, “Injuries are a significant problem for soccer players,” 92% of coaches strongly agreed or agreed, 5% neither agreed or disagreed, and 3% disagreed (Fig. 2A). For the statement, “Injuries can be prevented in soccer players,” 77% of coaches strongly agreed or agreed, 15% neither agreed or disagreed, and 8% disagreed or strongly disagreed (Fig. 2B). For the statement, “I would support the adoption of an injury prevention program for my team,” 95% of coaches strongly agreed or agreed, and 5% of coaches neither agreed or disagreed, none disagreed (Fig. 2C). For the statement, “I don’t think my team would benefit from an injury prevention program,” 5% of coaches strongly agreed or agreed, 13% of coaches neither agreed or disagreed, and 82% of coaches disagreed or strongly disagreed (Fig. 2D). 31 coaches stated that they were aware of an injury prevention program, and 7 coaches stated that they were not aware of an injury prevention program. 12 coaches stated that they did not use an injury prevention program, and 22 coaches stated that they used an injury prevention program. Of the 12 coaches who reported not using an injury prevention program, 10 had a 100% completion rate of the survey (“Non-users”) and only their data will be reported. Of the 22 coaches who reported that they do use an injury prevention program, 19 had a 100% completion rate of the survey (“Users”) and only their data will be reported. For the Users, 1 coach reported using an IPP once per week, 8 coaches reported using an IPP 2–3 times per week, and 10 respondents reported using an IPP every practice/game.
Fig. 2.
Participant responses (N=39) to statements about beliefs and attitudes regarding injury prevention programs (IPPs).
Demographic data of the Non-users were compared to the Users. The majority of Users were coaches at D1 schools (53%), while the majority of Non-users were coaches at D3 schools (54%) Table 1. For the statement “Who should be responsible for completing an injury prevention program?,” Users responded: “Coaches” (47%), “Strength and Conditioning” (21%), “Other” (21%), and “Athlete” (11%). For the statement “Other”, respondents elaborated that it was a joint responsibility among coaches, athletes and auxiliary staff. Non-users responded to this statement with: “Strength and Conditioning” (50%), “Athletic training” (30%), “Athlete” (10%), and “Coaches” (10%).
The Non-users were asked to rank order (1–7 (1=highest rank, 7=lowest rank)) reasons they do not use an injury prevention program (“Barrier” (median rank)). “Costs too much” (2) was the most highly ranked barrier to implementing an injury prevention program followed by, “Not trained in instructing the program” (2.5), “Takes too much time” (3), “Did not know that programs exist” (4), “Not effective in preventing injuries” (4.5), “Does not improve player performance” (5), and “Other” (7). For the statement “Other”, coaches were allowed to enter free-text answers. The free-text answers included, “Most injuries occur because of players being hit by opposing players”, and “We have a great athletic trainer that I trust and can confide with.” Coaches were also asked to rank order (1–7 (1=highest rank, 7=lowest rank)) statements that would make them more likely to implement an injury prevention program. “Free of cost” (2) was the most highly ranked statement followed by “Effective in preventing injuries” (3), “Improves player performance” (3.5), “Training in instructing programs” and “Shorter duration” (4, 4), “Education on available programs” (5), and “Other” (7).
The Users were asked, “Do you think that using an injury prevention program has prevented injuries for your team?” 73.7% stated “yes” and 26.3% stated “maybe”. For the statement, “Do you think that using an injury prevention program has improved player performance?” 57.9% of coaches stated “yes” and 42.1% of coaches stated “maybe”. 12 coaches reported that they used a named program (11+ or portions of the 11+) and 7 reported that they do not use a named program. Of the coaches who stated they use a named program 75.0% reported that they have modified the program, 16.7% reported that they were unsure if they had modified the program, and 8.3% reported that they had not modified the program.
4. Discussion
The purpose of this study was to identify barriers to implementation of IPPs among NCAA women’s soccer coaches. Overall, survey respondents’ expressed supportive attitudes regarding IPPs, which is consistent with previous studies.10 Non-users of IPPs identified cost as the primary barrier to initiating an IPP. Although time and impact on player performance were recognized by the respondents as factors influencing adoption of an IPP, our hypothesis that they would be the primary barriers reported by our sample was not supported. Fidelity was identified as a limitation to long-term implementation of an IPP.
Cost was the primary barrier to implementing an IPP reported by our respondents. Coaches stated that that they would be more likely to implement an IPP if it was free of cost. In a systematic review of studies on barriers to implementation of ACL injury prevention programs, cost was also reported to be a consistent barrier to implementation.13 Although there are IPPs that require purchase of learning materials or training, there are also evidence-based IPPs such as the 11+ with freely available training materials online.1,24,25 Therefore, although cost is a self-reported barrier to implementation of an IPP, this survey response may represent other barriers such as education regarding access to IPPs or self-efficacy in leading an IPP.9,11 “Cost” may also represent a multifaceted construct, beyond educational materials and equipment. Since the majority of Non-users identified strength and conditioning coaches as being responsible for completion of an IPP, this may indicate that the cost of hiring additional staff is a barrier to implementation rather than the cost of an actual IPP. However, further research, such as completion of qualitative interviews, is needed to identify specific cost-related barriers to implementation of IPPs.
Although the majority of our sample reported being aware of an IPP, education on how to teach an IPP was indicated as another barrier to implementation among the Non-users. While high levels of awareness of IPPs is reported among youth soccer coaches, awareness does not necessarily translate to adoption and implementation of an IPP.10 Perhaps future educational interventions should focus on practical instruction of how to teach IPPs rather than further increasing awareness of them. Participation in a coaching workshop on instruction of the 11+ has reportedly led to higher adherence to the program versus solely providing instructional materials.26 Additionally, “takes too much time” was identified as the third most important barrier for not using an IPP and “improves player performance” was identified as the third most important factor in adopting an IPP. This may indicate that these factors are still influential in a coach’s decision to implement an IPP, but are not the primary barriers to implementation as we hypothesized.
Fidelity was a limitation to long-term implementation of IPPs among Users. The majority of coaches stated that they had either definitively modified the IPP that they use, or may have modified the IPP that they use. Long-term follow-up studies on implementation have also reported low fidelity to IPPs overtime.20,22 One of our survey respondents reported adding in additional stretches to the IPP that they followed, and other common modifications include progressing exercises beyond the established IPP.27 One study has reported increased efficacy of and improved adherence to the 11+ after re-ordering its components.28 However, modifying the actual content of an IPP could reduce its efficacy, especially if modifications are not guided by existing evidence on ACL injury prevention.19,27
Asking coaches to identify who should be responsible for completion of an IPP was a unique feature of this survey. Although the response rate to the survey was too low to compare the responses between Users and Non-users statistically, there appears to be a difference between these two groups. The majority of IPP Users reported that it was the team/head coach’s responsibility to make sure an IPP was completed, while the majority of Non-users reported that it was the strength and conditioning staff’s responsibility. The role of the coach has been indicated as a strong factor for adopting an IPP.5,9 However, previous research has identified that having a strength and conditioning coach associated with a soccer team strongly increases the odds that the team uses an IPP.14 Studies of team handball have also reported increased IPP compliance when a physical therapist assists in the application of an IPP.29 The coaches that responded “Other” and elaborated that it is the responsibility of coaches, athletes, and support personnel to complete an IPP may have the most insightful response. A collaborative approach to IPP implementation may be key for ACL injury prevention. It is unlikely that players will have coaches with consistent IPP approaches throughout their athletic careers.30 Perhaps, the focus of implementing IPPs should not be solely on the coach, but include all team personnel, and players too so that they can integrate injury prevention strategies throughout their individual athletic journeys.
Our study has several limitations. The survey has not undergone formal validation testing. At this time, however, there are no standardized surveys for examining barriers to implementation of interventions. The questions asked in our survey and the responses we received were also commensurate with existing literature. Another potential limitation is our sample. We had a response rate of 25%, but only 29 respondents had a 100% completion rate of the survey. This number of respondents as well as the overall response rate is similar though to comparable studies.9,21,30 Additionally, only coaches in the NCAA Eastern region were contacted, so beliefs and attitudes about IPPs could vary in different regions or countries. Furthermore, the majority of survey respondents were from D1 and D3 schools, so these beliefs and attitudes may not fully represent D2 schools. Future research should include national and international sampling of coaches to address these limitations, and should also consider use of qualitative research strategies to gain a deeper understanding of the barriers to implementation of IPPs.
5. Conclusion
This study identified several barriers to implementation of IPPs among NCAA women’s soccer coaches, some surprising. Coaches who do not currently use an IPP cited the cost of implementing an IPP as the primary barrier to implementation of an IPP, and education on instructing an IPP as another significant barrier. Coaches who do use an IPP identified adherence as a barrier to long-term implementation of IPPs. A team-based approach to implementation of IPPs may be a facilitator of long-term implementation of IPPs. Many coaches who currently use an IPP cited that a team-based approach should be used, and incorporation of additional support personnel such as rehabilitation and strength and conditioning professionals may facilitate implementation.14,29 Furthermore, incorporating the athletes themselves into implementation responsibilities could support life-long use of IPPs and ultimately reduce ACL injury rates.
Supplementary Material
Practical implications.
Although many injury prevention programs are freely available, “cost” was cited as the principal barrier to initiating an injury prevention program among coaches who do not use a prevention program.
The majority of coaches reported being aware of an injury prevention program, but indicated that lack of practical training in instructing a program was a barrier to implementation among coaches who do not use a prevention program.
This paper adds to the body of evidence that suggests injury prevention program implementation might need to incorporate all team personnel for long-term adherence.
Acknowledgements
Thank you to the coaches who participated in this survey. The work of Celeste Dix was supported by National Institutes of Health [T32 HD007490].
Footnotes
Appendix A. Supplementary data
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.jsams.2020.09.016.
References
- [1].Thorborg K, Krommes KK, Esteve E et al. Effect of specific exercise-based football injury prevention programmes on the overall injury rate in football: a systematic review and meta-analysis of the FIFA 11 and 11+ programmes. Br J Sports Med 2017; 51(7):562–571. 10.1136/bjsports-2016-097066. [DOI] [PubMed] [Google Scholar]
- [2].Prodromos CC, Han Y, Rogowski J et al. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthrosc J Arthrosc Relat Surg 2007; 23(12):1320–1325. 10.1016/j.arthro.2007.07.003. [DOI] [PubMed] [Google Scholar]
- [3].Soligard T, Myklebust G, Steffen K et al. Comprehensive warm-up programme to prevent injuries in young female footballers: cluster randomised controlled trial. BMJ 2009; 338(7686):95–99. 10.1136/bmj.a2469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Finch CF, Donaldson A. A sports setting matrix for understanding the implementation context for community sport. Br J Sports Med 2010; 44(13):973–978. 10.1136/bjsm.2008.056069. [DOI] [PubMed] [Google Scholar]
- [5].Bizzini M, Junge A, Dvorak J. Implementation of the FIFA 11+ football warm up program: how to approach and convince the football associations to invest in prevention. Br J Sports Med 2013; 47(12):803–806. 10.1136/bjsports-2012-092124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Arundale AJH, Bizzini M, Giordano A et al. Exercise-based knee and anterior cruciate ligament injury prevention. J Orthop Sport Phys Ther 2018; 48(9):A1–A42. 10.2519/jospt.2018.0303. [DOI] [PubMed] [Google Scholar]
- [7].Crossley KM, Patterson BE, Culvenor AG et al. Making football safer for women: a systematic review analysis of injury prevention programmes in 11 773 female football (soccer) players. Br J Sports Med 2020;(2):1–12. 10.1136/bjsports-2019-101587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Webster KE, Hewett TE. Meta-Analysis of Meta-Analyses of anterior cruciate ligament injury reduction training programs. J Orthop Res 2018:2696–2708. 10.1002/jor.24043. [DOI] [PubMed] [Google Scholar]
- [9].Mawson R, Creech MJ, Peterson DC et al. Lower limb injury prevention programs in youth soccer : a survey of coach knowledge, usage, and barriers. J Exp Orthop 2018; 5:43 10.1186/s40634-018-0160-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Frank BS, Register-Mihalik J, Padua DA. High levels of coach intent to integrate a ACL injury prevention program into training does not translate to effective implementation. J Sci Med Sport 2015; 18(4):400–406. 10.1016/j.jsams.2014.06.008. [DOI] [PubMed] [Google Scholar]
- [11].McKay CD, Merrett CK, Emery CA. Predictors of FIFA 11+ implementation intention in female adolescent soccer: an application of the health action process approach (HAPA) model. Int J Environ Res Public Health 2016; 13(7). 10.3390/ijerph13070657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Soligard T, Nilstad A, Steffen K et al. Compliance with a comprehensive warm-up programme to prevent injuries in youth football. Br J Sports Med 2010; 44(11):787–793. 10.1136/bjsm.2009.070672. [DOI] [PubMed] [Google Scholar]
- [13].Bogardus RL, Martin RJ, Richman AR et al. Applying the socio-ecological model to barriers to implementation of ACL injury prevention programs: a systematic review. J Sport Heal Sci 2019; 8(1):8–16. 10.1016/j.jshs.2017.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Joy EA, Taylor JR, Novak MA et al. Factors influencing the implementation of anterior cruciate ligament injury prevention strategies by girls soccer coaches. J Strength Cond Res 2013; 27(8):2263–2269. [DOI] [PubMed] [Google Scholar]
- [15].Steffen K, Emery CA, Romiti M et al. High adherence to a neuromuscular injury prevention programme (FIFA 11+) improves functional balance and reduces injury risk in Canadian youth female football players: a cluster randomised trial. Br J Sports Med 2013;47(12):794–802. 10.1136/bjsports-2012-091886. [DOI] [PubMed] [Google Scholar]
- [16].Parsons JL, Carswell J, Nwoba IM et al. Athlete perceptions and physical performance effects of the FIFA 11 + program in 9–11 year-old female soccer players. Int J Sports Phys Ther 2019; 14(5):740–752. 10.26603/ijspt20190740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Hägglund M, Waldén M, Magnusson H et al. Injuries affect team performance negatively in professional football: an 11-year follow-up of the UEFA Champions League injury study. Br J Sports Med 2013; 47(12):738–742. 10.1136/bjsports-2013-092215. [DOI] [PubMed] [Google Scholar]
- [18].Waldén M, Hägglund M, Ekstrand J. Football injuries during European Championships 2004–2005. Knee Surg Sport Traumatol Arthrosc 2007; 15(9):1155–1162. 10.1007/s00167-007-0290-3. [DOI] [PubMed] [Google Scholar]
- [19].Hagglund M, Atroshi I, Wagner P et al. Superior compliance with a neuromuscular training programme is associated with fewer ACL injuries and fewer acute knee injuries in female adolescent football players: secondary analysis of an RCT. Br J Sports Med 2013; 47(15):986–991. 10.1136/bjsports-2013-092676. [DOI] [PubMed] [Google Scholar]
- [20].Lindblom H, Waldén M, Carlfjord S et al. Implementation of a neuromuscular training programme in female adolescent football: 3-year follow-up study after a randomised controlled trial. Br J Sports Med 2014; 48(19):1425–1430. 10.1136/bjsports-2013-093298. [DOI] [PubMed] [Google Scholar]
- [21].O’Brien J, Finch CF. Injury prevention exercise programmes in professional youth soccer: understanding the perceptions of programme deliverers. BMJ Open Sport Exerc Med 2016; 2(1):e000075. 10.1136/bmjsem-2015-000075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Norcross MF, Johnson ST, Bovbjerg VE et al. Factors influencing high school coaches’ adoption of injury prevention programs. J Sci Med Sport 2016; 19(4):299–304. 10.1016/j.jsams.2015.03.009. [DOI] [PubMed] [Google Scholar]
- [23].O’Brien J, Finch CF. Injury prevention exercise programs for professional soccer: Understanding the perceptions of the end-users. Clin J Sport Med 2017; 27(1):1–9. 10.1097/JSM.0000000000000291. [DOI] [PubMed] [Google Scholar]
- [24].Mandelbaum BR, Silvers HJ, Watanabe DS et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med 2005; 33(7):1003–1010. 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- [25].Sportsmetrics. Sportsmetrics.
- [26].Steffen K, Meeuwisse WH, Romiti M et al. Evaluation of how different implementation strategies of an injury prevention programme (FIFA 11+) impact team adherence and injury risk in Canadian female youth football players: a cluster-randomised trial. Br J Sports Med 2013; 47(8):480–487. 10.1136/bjsports-2012-091887. [DOI] [PubMed] [Google Scholar]
- [27].O’Brien J, Young W, Finch CF. The delivery of injury prevention exercise programmes in professional youth soccer: comparison to the FIFA 11+. J Sci Med Sport 2017; 20(1):26–31. 10.1016/j.jsams.2016.05.007. [DOI] [PubMed] [Google Scholar]
- [28].Whalan M, Lovell R, Steele JR et al. Rescheduling part 2 of the 11+ reduces injury burden and increases compliance in semi-professional football. Scand J Med Sci Sport 2019; 29(12):1941–1951. 10.1111/sms.13532. [DOI] [PubMed] [Google Scholar]
- [29].Myklebust G, Skjølberg A, Bahr R. ACL injury incidence in female handball 10 years after the Norwegian ACL prevention study: Important lessons learned. Br J Sports Med 2013; 47(8):476–479. 10.1136/bjsports-2012-091862. [DOI] [PubMed] [Google Scholar]
- [30].Lindblom H, Carlfjord S, Hägglund M. Adoption and use of an injury prevention exercise program in female football: a qualitative study among coaches. Scand J Med Sci Sport 2018; 28(3):1295–1303. 10.1111/sms.13012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.