Abstract
Objective:
Mirrored psychophysiological change in cognitive workload indices may reflect shared mental models and effective healthcare team dynamics. In this exploratory analysis, we investigated the frequency of mirrored changes, defined as concurrent peaks in heart rate variability (HRV) across team members, during cardiac surgery.
Design:
Objective cognitive workload was evaluated via HRV collected from the primary surgical team during cardiac surgery cases (N=15). Root mean square of the successive differences (RMSSD) was calculated as the primary HRV measure. Procedures were divided into consecutive non-overlapping 5-minute segments, and RMSSD along with deviations from RMSSD were calculated for each segment. Segments with positive deflections represent above-average cognitive workload. Positive deflections and peaks across dyads within the same segment were counted.
Setting:
Data collection for this study took place in the cardiovascular operating room during live surgeries.
Participants:
Physiological data was collected and analyzed from the attending surgeon, attending anesthesiologist, and primary perfusionist involved with the recorded cases.
Results:
Of the 641 five-minute segments analyzed, 325 (50.7%) were positive deflections above average, concurrently across at least two team members. Within the 325 positive deflections, 26 (8%) represented concurrent peaks in HRV across at least two active team members. Mirrored peaks across team members was observed most commonly during the coronary anastomoses or valve replacement phase (N=12).
Conclusions:
In this pilot study, mirrored physiological responses representing peaks in cognitive workload were observed uncommonly across dyads of cardiac surgery team members (1.73 peaks/case on average). Almost half of these occurred during the most technically demanding phases of cardiac surgery, which may underpin teamwork quality. Future work should investigate interactions between technical and non-technical performance surrounding times of mirrored peaks and expand the sample size.
ACGME Competencies:
Systems-based practice
Keywords: Heart rate variability, cognitive workload, cardiac surgery, patient safety
Introduction
Effective teamwork and non-technical skill are critical when performing complex procedural care.1,2 In the face of extreme cognitive demands, surgical and procedural teams are required to maintain close cooperation and high standards of care to avoid preventable adverse events (PAEs). Recent evidence suggests a previously underappreciated influence of cognitive factors on the occurrence of surgical PAEs, contributing up to 51.6% of all PAEs in a recent multi-site study.3 Given this evidence, alongside existing theoretical frameworks,4 identifying peaks of cognitive workload statuses may facilitate the development of new error-prevention strategies.
While cognitive workload approaches tend to focus on individuals, the complex socio-technical nature of the operating room (OR) warrants evaluation of multiple team members working towards the same goal. Within team organizations, previous work has established the presence of neurodynamic synchrony among dyads in surgery, and in particular among actively involved members. These results suggest that presence in the OR is insufficient to achieve synchrony across team members, but rather active involvement is required.5,6 The cardiac OR in particular is an exemplary setting due to the distinct but inter-dependent teams delivering patient care, comprised of teams of surgeons, anesthesiologists, perfusionists, and OR nurses. Typical approaches to measuring cognitive workload include self-report and psychophysiological measures. Self-report measures, however, are not adequately designed or equipped to evaluate team-based dynamics in all cases. Self-report measures also tend to be less temporally accurate and more susceptible to various cognitive biases. Objective, real-time psychophysiological measures of cognitive workload are therefore appealing.
Heart rate variability (HRV) as a measure of cognitive workload is a strong candidate, and is the most often relied upon measure of cognitive workload during surgery.7 HRV captures the dynamic fluctuations in heart rate by quantifying beat-to-beat changes detected from R-peaks within the electrocardiogram, which result from complex interactions among physiological systems (e.g. autonomic neural activity, blood pressure, respiratory control, etc.).8 Individual HRV has been used extensively as a measure of cognitive workload, and capturing HRV of multiple team members simultaneously provides the opportunity to evaluate team-based patterns of psychophysiological change over time.9-12 One pattern of particular interest is that reflecting mirrored physiological change, defined as concurrent peaks in cognitive workload across team members. Mirrored psychophysiological change in cognitive workload indices may be indicative of effective healthcare team dynamics,12 including enhanced coordination and shared mental models.
In addition to observing the relationship between physiological changes and non-technical team outcomes such as coordination of care, knowledge of HRV in real time could contribute a previously untapped data source to enhance self-insight for surgeons. A greater interest in emotional intelligence among healthcare providers in recent years presents ample educational opportunities to incorporate self-awareness and self-regulation practices into surgical care.13 Along these lines, both intentional self-reflection14 and gaining insight into one’s own physiological response (e.g. through biofeedback15) can be powerful methods of augmenting traditional surgical educational approaches with HRV monitoring. More broadly, a greater awareness of the frequency and influence of mirrored psychophysiological changes in the OR could be leveraged to improve system processes involved in surgical care, for both senior surgical team members and trainees.
Through this exploratory analysis, we aim to leverage HRV acquisition during live surgery to assess team-wide interactions across multiple individuals. Our goal is to determine the characteristics and frequency of simultaneous mirrored changes in intra-operative cognitive workload across at least two members of the cardiac surgery team (dyads). With this information we aim to classify on a high-level the surgical phase during which these mirrored changes occur over the course of the procedure, as well as the general composition of individual roles within dyads. We also aimed to explore the relationship between the frequency of mirrored changes and proxies of surgical risk and complexity, with the expectation that a higher frequency mirrored changes would be associated with riskier and more complex procedures, thereby indicating enhanced coordination among team members under ambiguous circumstances.
Material and Methods
Participants
This project received approval from the Institutional Review Boards of VA Boston Healthcare System and Harvard Medical School (IRB#3047). Participants in this study were all individuals who entered the OR at any time during audio/video recording set up for this project, which includes patients and all staff involved with or observing the case. All participants provided a written informed consent prior to the start of surgery. This preliminary analysis evaluated data from 15 surgical cases in total (N=7 coronary artery bypass graft (CABG) and N=8 aortic valve replacement (AVR) surgeries), all of which were elective surgeries.
Equipment
OR recordings included audio capture via three Sony ICD-PX440 microphones (Tokyo, Japan) worn on the surgical mask by three of the core cardiac surgical team members (attending surgeon, attending anesthesiologist, and primary perfusionist) and video capture via two GoPro HERO4 Black Edition high-definition cameras (San Mateo, CA) in the cardiac OR (wide angle of OR and narrow angle of surgical field).
Objective cognitive workload was evaluated wirelessly via HRV by fitting a Polar V800 chest strap with H10 sensors (Kempele, Finland) to each of the three cardiac surgery team members included in this study.
Analysis
Procedures were divided into consecutive non-overlapping 5-minute segments, and the root mean square of the successive differences (RMSSD), an HRV measure reflective of cognitive workload, was calculated for each segment using R-R intervals entered into Kubios software.16 Calculating consecutive non-overlapping segments is an approach which was originally proposed by the Task Force of The European Society of Cardiology and The North American Society of Pacing and Electrophysiology, and has been adopted across multiple analytical approaches. The formula for calculating RMSSD based on R-R intervals can be seen in Equation 1, where “R” signifies an individual R-peak on the electrocardiogram.
| (Equation 1) |
The RMSSD component of HRV is classified as time-domain measure17 and is known to be vagally-mediated, reflecting parasympathetic activity of the autonomic nervous system.18 RMSSD has the advantage of being exceptionally temporally sensitive and robust against certain external influences, including the impact of breathing on HRV.19
Because RMSSD is parasympathetically driven, its values reflect a state of rest. Thus, higher RMSSD values indicate higher states of relaxation, or overall lower workload. For the ease of interpretation, RMSSD was inverted in this analysis such that higher values now represent higher cognitive workload states. In addition to averaging RMSSD values of all consecutive segments within a surgery together to arrive at an average value per case, individuals’ deviations from their average RMSSD were also calculated for each segment in such a way that inverted the value (Equation 2).
| (Equation 2) |
Due to this inversion, segments with positive deflections represent above-average cognitive workload. Positive deflections across at least two team members within the same segment were counted. The total count of concurrent positive deflections included any segment during which at least two data points, representing at least two team members physically present in the OR for the entire 5-minute segment, reflected normalized RMSSD values greater than zero. Because each deflection is a point in time, it cannot speak to the directionality or change in patterns in relation to other points in time. In an effort to detect patterns of change, positive deflections were further considered in relation to the points in time surrounding them. Thus, within deflections, matching patterns reflecting the same directional change and pattern in RMSSD across at least two team members concurrently were counted (Figure 1), which we refer to as peaks in cognitive workload.
Figure 1.
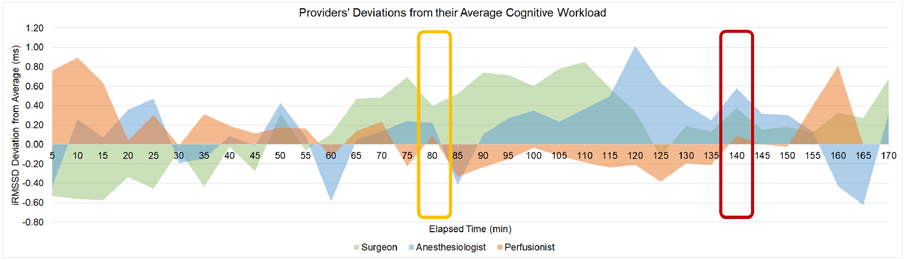
provides an example of how concurrent positive deflections and positive peaks were identified across cases. Elapsed time is shown on the x-axis For every 5 minutes of elapsed time, RMSSD was calculated and inverted such that higher values on the y-axis represent higher levels of cognitive workload. Because these values were normalized to each individual’s average RMSSD over the course of the surgery, deviations from the x-axis indicate increases (positive y-values) and decreases (negative y-values) in cognitive workload. This figure highlights one example of concurrent positive deflections (80 minutes elapsed, yellow square) and one example of concurrent positive peaks (140 minutes elapsed, red square). iRMSSD = inverted root mean square of the successive differences
All data sources collected throughout this project (audio, video, HRV) were integrated and time-synchronized. Data were trimmed to start when the patient was transferred onto the operating table, and end when the patient left the OR. Using previously developed standardized process models of CABG and AVR procedures,20,21 each case was divided into the following phases: 1) Pre-induction, 2) Anesthesia Induction, 3) Sterile Prepping, 4) Pre-incision Time-out, 5) Sternotomy, 6) Vessel Harvesting (for CABG only), 7) Heparinization, 8) Aortic Cannulation, 9) Initiation of Bypass, 10) Aortic Clamp and Cardioplegia, 11) Anastomoses or Valve Replacement, 12) Separation from Bypass, 13) Sternal Closure, and 14) Post-operative Debrief. On a case-by-case basis, timestamps of segments corresponding to peaks in cognitive workload across actively-involved dyads were traced to the phase in which they occurred. Videos were consulted to ensure the presence and active, primary involvement of all monitored team members represented in each segment of elevated cognitive workload. Although trainee involvement was not standardized across cases, each segment was reviewed, confirming that the attending surgeon and attending anesthesiologist were actively involved in 68.42% of the segments demonstrating concurrent peaks. For our analysis to capture physiological changes of the attending surgeons and attending anesthesiologists when they are the primary actors, the 31.58% of segments with primary involvement of the trainee were excluded from further analysis.
To lend support for the underlying hypothesis that a higher frequency of mirrored physiological peaks reflects higher levels of team performance and thereby outcomes, preliminary validity analysis compared outcome measures of procedures with less concurrent peaks to those of procedures with a greater number of concurrent peaks. Cases were considered to have a low number of concurrent peaks if there were less than 3 peaks observed, while cases with ≥ 3 peaks observed were considered to have a high number of concurrent peaks. Relevant outcome measures including post-operative length of hospital stay and total surgery duration, collected during the course of this study, were selected. Patient-specific factors, including the patient’s age and STS Predicted Risk of Mortality (PROM) calculated risk scores, were also selected, to provide additional contextual information.
Given the exploratory nature of this study, descriptive statistics were calculated and are reported in terms of frequencies and percentages. Preliminary validation was analyzed with an independent samples t-test, and results are reported as (mean ± standard deviation, p-value).
Results and Discussion
Results
Participants.
Across the 15 cardiac cases analyzed, participants representing the core surgical team included three attending surgeons, three attending anesthesiologists, and three primary perfusionists. Table 1 provides an overview of participant demographics.
Table 1.
shows participant characteristics of cardiac surgery team members recorded in the cases analyzed.
| Surgeon | Anesthesiologist | Perfusionist | |
|---|---|---|---|
| N of Participants | 3 | 3 | 3 |
| Sex: M (%) | 2 (66.6) | 2 (66.6) | 3 (100) |
| Age: Ave (Range) | 56.67 (53-61) | 46.33 (38-54) | 46 (32-60) |
| Years of Experience Post-Training: Ave (Range) | 26.33 (18-34) | 13.83 (3.5-25) | 19.33 (9-32) |
| Approximate Cardiac Surgeries | 5,000 | 1,008.33 | 1,933 |
| Performed: Ave (Range) | (1,000-10,000) | (275-1,500) | (700-3,500) |
Physiological Analysis.
In total, 641 five-minute segments were analyzed (average: 42.73 segments/case). Of the 641 segments, 325 (50.7%) were positive deflections above average, concurrently across at least two team members. Within the 325 positive deflections, 26 (8%) represented peaks in RMSSD such that at least two actively involved team members saw the same mirrored change, creating a simultaneous peak of above-average cognitive workload. While five cases included more than three mirrored peaks over the course of the procedure, seven cases included less than three mirrored peaks, and the remaining three of the 15 cases did not reveal any concurrent peaks in cognitive workload across any dyad combination. Overall, 12 cases (N=6 CABG, N=6 AVR) revealed a total of 26 peaks (1.73 peaks/case on average).
Surgical Phase Analysis.
The 26 concurrent peaks in cognitive workload observed occurred during seven of the possible 14 phases. Overall, mirroring of peaks across actively involved dyads was observed most commonly during the Anastomoses or Valve Replacement phase (N=12), followed by Cannulation (N=7), Separation from Bypass (N=2) and Sternotomy (N=2), Heparinization (N=1), Initiation of Bypass (N=1), and Sternal Closure (N=1) phases.
Provider Role Analysis.
Roles involved in each dyad throughout the 26 concurrent peaks identified were relatively evenly represented, with the attending surgeon involved in the greatest number of dyad peaks (N=20, 76.92% of all peaks), followed by the primary perfusionist (N=19, 73.08% of all peaks) and the attending anesthesiologist (N=14, 53.85% of all peaks). When considering individual providers within each category, one surgeon was disproportionately represented (10/20 or 50% of all peaks involving surgeons), as well as one perfusionist (10/19 or 52.63% of all peaks involving perfusionists), and one anesthesiologist (7/14 or 50% of all peaks involving anesthesiologists).
Within all surgeon-perfusionist dyads (Surg-Perf), a relatively even distribution was observed among individual providers. In contrast, 50% of all surgeon-anesthesiologist dyads (Surg-Anes) involved the same two individuals, while 42.86% of all anesthesiologist-perfusionist dyads (Anes-Perf) involved the same two individuals.
Dyad Analysis Within Surgical Phases.
Of three possible dyad combinations (Surg-Perf, Surg-Anes, Anes-Perf), the attending surgeon and primary perfusionist experienced the greatest number of concurrent peaks in general (N=12/26, 46.15%), and notably, during the Anastomoses or Valve Replacement phase (N= 10/12, 83.33%). Concurrent peaks among the attending surgeon and attending anesthesiologist appeared in seven of the 26 segments (26.92%) and were most prevalent during the Cannulation phase (N=3/7, 42.86%). Finally, concurrent peaks between the attending anesthesiologist and primary perfusionist were observed least frequently in six of the 26 segments (23.08%) and was most common during the Cannulation phase (N=3/6, 50%). One segment (3.85%) revealed mirroring of HRV across all three team members, which was noted during the Separation from Bypass phase.
Preliminary Validation.
Seven of the 12 procedures (58.33%) revealed less than three peaks across dyads, while the remaining five procedures (41.67%) revealed at least three concurrent peaks. Length of hospital stay was slightly, but non-significantly, higher in cases with fewer concurrent peaks (8.86 ± 2.97 days) compared to cases with more concurrent peaks (7.80 ± 1.79 days, t(10)=0.705, P=0.249). Similarly, surgery duration was slightly longer in cases with fewer concurrent peaks (245.43 ± 80.92 minutes) compared to cases with more concurrent peaks (238.20 ± 57.97 minutes, t(10)=0.170, P=0.434).
In terms of patient-specific factors analyzed, the patient’s age tended to be higher on average, though not reaching statistical significance, in cases with fewer concurrent peaks (69.00 ± 2.27) compared to cases with more concurrent peaks (65.40 ± 11.67, t(10)=0.810, P=0.218). Significant differences were detected between groups between STS-PROM calculated risk scores. In particular, risk of 30-day mortality was significantly lower in cases demonstrating fewer concurrent peaks (1.14 ± 0.01%) compared to cases with a greater number of concurrent peaks (2.37 ± 0.02%, t(10)=−141.934, P<0.0001). The risk of 30-day morbidity was similarly significantly lower in cases with fewer concurrent peaks (2.34 ± 0.01%) compared to cases with more concurrent peaks (4.42 ± 0.04%, t(10)=−134.048, P<0.0001). Finally, the risk of 30-day surgical site infection was significantly higher in cases with less concurrent peaks (3.04 ± 0.04%) compared to cases with more concurrent peaks (2.41 ± 0.02%, t(10)=32.117, P<0.0001). Despite predicted risk values, no patients enrolled in the study suffered from any observed morbidities or mortality, eliminating the need for statistical testing for actual mortality outcomes.
Based on analysis of key words from self-reports and operative notes, there was no observed difference in intraoperative difficulties concerned with patient anatomy or teaching responsibilities across cases with less versus more concurrent peaks. In both categories, there were reports of “bad veins” and frustration with teaching new residents or nursing staff, but these comments were unrelated to the number of observed peaks.
Discussion
Existing evidence suggests concurrent/mirrored peaks across multiple team members may reflect enhanced non-technical skills, including shared mental models, converging during times of ambiguity or crisis. In our pilot study, we have demonstrated the novelty of utilizing HRV to capture and assess interactions on the team level during cardiac surgery. Primary findings suggest that mirrored psychophysiological responses representing peaks in cognitive workload occur infrequently across all dyad combinations within cardiac surgery team members (26 peaks across 15 cases; average: 1.73 peaks/case). Isolated peaks in HRV, representing above-average cognitive workload, could be indicative of moments of overload when considered on an individual basis. While this may be the case on a collective basis as well, concurrent/mirrored peaks across multiple team members may reflect critical non-technical skills, including problem-solving mentalities, focused attention, task coordination, and shared mental models, converging during times of ambiguity or crisis.12 Notably, a greater number of mirrored peaks across dyads in our small sample was associated with significantly higher predicted risk compared to cases with fewer mirrored peaks, with the exception of the predicted risk of surgical site infection. This finding, in conjunction with the lack of observed mortalities in either group, offers strong support that team members’ physiological convergence may represent more effective teamwork and non-technical skills under conditions of greater ambiguity.
Critically, almost half of the observed mirrored peaks in cognitive workload occurred during an extremely technically demanding phase of cardiac surgery: coronary anastomoses (CABG) or valve replacement (AVR). Mirrored peaks occurring during these phases were almost exclusively observed between the attending surgeon and primary perfusionist (83.33%), suggesting that those roles that tend to be more directly involved in patient care and monitoring during this phase may be experiencing converging mental states. Unexpectedly, there was only one observed instance reflecting concurrent peaks in cognitive workload across all three providers monitored. Perhaps expectedly, this occurred during the Separation from Bypass phase, a phase of cardiac surgery requiring high levels of situation awareness and shared mental models across the entire team to ensure successful performance and outcomes. These observed peaks, while they cannot be automatically considered signs of psychophysiological synchrony due to distinct analytical approaches, may reflect a shared mental model for a similar process given the common underlying physiological system. Psychophysiological synchrony in high-consequence, ambiguous domains, including healthcare, has been associated with enhanced team effectiveness and the resolution of uncertainty.11 This becomes significant in light of the literature supporting the powerful impact of non-technical skills on technical performance.22
Attending surgeons and primary perfusionists appeared slightly more frequently in segments involving mirrored peaks in cognitive workload compared to anesthesiologists (N=20, 19, and 14, respectively). This pattern does not seem very surprising, given the more frequent nature of attending anesthesiologists’ absences while the patient is on bypass. Similarly, the greater proportion of specific individuals appearing in dyads through this analysis can largely be attributed to specific cases presenting with more concurrent peaks than others (range: 0-5 peaks/case; average: 1.73)
In both categories, notable reports included “bad veins” and frustration with teaching new residents or nursing staff, but these comments were unrelated to the number of observed peaks. Comments about thin-walled veins and difficulty deciding on grafts, especially when coinciding with concurrent peaks during the anastomoses phase of CABG procedures, may play a role in the higher number of peaks appearing during this phase of the surgery. It is difficult to interpret too strongly, however, given that this study was not specifically designed to evaluate the source of potential stressors.
Separating out cases with low frequency of observed peaks (less than 3) and those with a higher frequency of observed peaks (≥3 peaks) revealed interesting relationships between the number of mirrored peaks and measures of surgical complexity. Though not statistically significant, the relationship between frequency of mirrored peaks among dyads of cardiac surgery team members and length of hospital stay and total surgical duration offer some support towards the underlying hypothesis that concurrent moments of elevated cognitive workload across team members may have a positive effect on facilitating performance. Cases with a higher frequency of mirrored peaks in cognitive workload were somewhat associated with lower surgery times, shorter post-operative lengths of stay, and less variability among both outcomes compared to cases with a lower frequency of mirrored peaks, though this association was not significant.
Anticipated risk scores (e.g. STS-PROM calculated risks of 30-day mortality and 30-day morbidity) were significantly higher in cases with a greater number/frequency of concurrent peaks over the course of the surgery, compared to cases with a lower number/frequency of concurrent peaks. Patients enrolled in this study did not suffer from any observed morbidities or mortality, but larger sample sizes would benefit from investigating the relationship between mirrored cognitive workload and outcomes metrics such as these. These findings lend more substantial support for the potential facilitating role mirrored peaks may have on outcomes, despite poorer anticipated outcomes.
The potential to demonstrate an objective, team-wide psychophysiological signature representative of an improvement in non-technical skill presents the opportunity to anticipate and support associated technical performance. With this knowledge comes the potential to intervene in real time to prevent performance decrement by supporting non-technical interactions at critical moments. For example, during time periods known for high cognitive workload with high technical skill requirements, cognitive engineering approaches could support the OR environment by providing situation awareness support.23
In addition to the real-time benefits of approaches such as biofeedback, HRV indices are also sensitive enough to distinguish between levels of expertise among healthcare providers, and can be readily incorporated into post-hoc debriefs.15 However, for physiology-based interventions to improve performance successfully, users must also display a level of emotional intelligence conducive to detecting and coping with physiological changes.24 Prior work has demonstrated that high levels of emotional intelligence are associated with effective recognition of and recovery from stressful experiences in the simulated OR.25 Fostering an environment that values self-reflection and insights into physiological changes can be embedded into residency curricula and systems-based practice to enhance emotional intelligence levels, an area especially critical to address in trainees and surgical teams.
This study has a number of limitations. The primary limitation is the small sample size, but given the exploratory and descriptive nature of this study, the interpretations are not vastly affected. Another limitation is the lack of contextual information identified and classified surrounding the peaks of cognitive workload present. This limitation can be resolved with detailed analysis of the recordings, which will be included in future work. With more detailed annotation of environmental, social, and procedural context, this type of analysis could be generalized more widely. The initial study design limited the number of team members monitored and did not include key demographics of those monitored, which would have aided interpretation. The ability to monitor additional team members (e.g. surgery and anesthesiology trainees, nurses) would greatly enhance the interpretability and impact of this work, especially given the importance of understanding the entire team dynamic. Additionally, we were unable to collect data regarding medication use, such as beta blockers, which has the capacity to directly influence HRV. The scope of this analysis has limited interpretation to moments reflecting simultaneous isolated peaks in cognitive workload across team members and did not investigate the potential presence and impact of transference of heightened states of cognitive workload between team members over time. Finally, utilizing five-minute time windows to calculate RMSSD segments may have masked differences occurring on shorter time-scales. Analysis involving shorter time windows may reveal more nuanced trends and patterns in physiological responses from individuals and the team.
Conclusions
Overall, the results from this exploratory analysis suggest that moments of mirrored changes in above-average cognitive workload, derived from team-wide HRV data, occur rarely during cardiac surgery procedures. However, when these moments are observed, they primarily occur within surgical phases reliant on high technical performance. Findings support further classification of inputs contributing to mirrored psychophysiological peaks in cognitive workload across cardiac surgery team members. Knowledge and awareness of the interactive nature of the OR system at large could inform trainees of the greater context, and factors influencing the context at any given time. Ultimately, this could result in greater management and coping abilities during surgical care.
Avenues for future work should include: investigating and characterizing notable events surrounding times of mirrored peaks to determine potential contributors to individual and team-wide changes in cognitive workload; monitoring trainees and nursing staff to ascertain a more comprehensive snapshot of OR staff workload; and characterizing and further investigating additional patterns of temporal- and role-specific changes (i.e. successive peaks rather than strictly concurrent peaks in cognitive workload). Given this preliminary theoretical basis underpinning team interactions during surgery, additional future studies are also expected to inform development of aforementioned training activities.
Highlights.
Heart rate variability is an effective objective measure of team cognitive workload
Mirrored changes in heart rate variability may indicate effective team dynamics
Mirrored changes occurred most often during technically demanding phases of surgery
Acknowledgments
Funding: This work was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health [R01HL126896, PI Marco A. Zenati]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Meeting Presentation: This research was presented at the 15th annual Academic Surgical Congress conference in Orlando, FL on February 6, 2020.
Declaration of Interest
None.
References
- 1.Agha RA, Fowler AJ, Sevdalis N. The role of non-technical skills in surgery. Ann Med Surg. 2019;4(4):422–427. doi: 10.1016/j.amsu.2015.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yule S, Paterson-Brown S. Surgeons’ Non-technical Skills. Surg Clin North Am. 2012;92(1):37–50. doi: 10.1016/j.suc.2011.11.004 [DOI] [PubMed] [Google Scholar]
- 3.Suliburk JW, Buck QM, Pirko CJ, et al. Analysis of Human Performance Deficiencies Associated With Surgical Adverse Events. JAMA Netw Open. 2019;2(7):e198067. doi: 10.1001/jamanetworkopen.2019.8067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel VL, Kannampallil TG, Shortliffe EH. Role of cognition in generating and mitigating clinical errors. BMJ Qual Saf. 2015;24(7):468–474. doi: 10.1136/bmjqs-2014-003482 [DOI] [PubMed] [Google Scholar]
- 5.Stevens RH, Galloway T, Willemsen-Dunlap A. Advancing Our Understandings of Healthcare Team Dynamics From the Simulation Room to the Operating Room: A Neurodynamic Perspective. Front Psychol. 2019;10(August):1–14. doi: 10.3389/fpsyg.2019.01660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stevens RH, Galloway TL. Teaching Machines to Recognize Neurodynamic Correlates of Team and Team Member Uncertainty. J Cogn Eng Decis Mak. 2019;13(4):310–327. doi: 10.1177/1555343419874569 [DOI] [Google Scholar]
- 7.Dias RD, Ngo-Howard MC, Boskovski MT, Zenati MA, Yule SJ. Systematic review of measurement tools to assess surgeons’ intraoperative cognitive workload. Br J Surg. 2018;105(5):491–501. doi: 10.1002/bjs.10795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shaffer F, McCraty R, Zerr CL. A healthy heart is not a metronome: An integrative review of the heart’s anatomy and heart rate variability. Front Psychol. 2014;5(September):1–19. doi: 10.3389/fpsyg.2014.01040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dias RD, Zenati MA, Stevens RH, Gabany JM, Yule SJ. Physiological synchronization and entropy as measures of team cognitive load. J Biomed Inform. 2019;96(June 2018):103250. doi: 10.1016/j.jbi.2019.103250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kennedy-Metz LR, Dias RD, Conboy HM, Nudel J, Stock EM, Zenati MA. Quantifying Intraoperative Team Cognitive Workload in Complex Surgical Environments. Proceedings, 2019 Int Conf Robot Autom (ICRA), Full-Day Work Next Gener Surg Seamless Integr Robot Mach Learn Knowl Represent within Oper Rooms, Montr Quebec, Cana 2019:17–19. [Google Scholar]
- 11.Stevens RH, Galloway T, Halpin D, Willemsen-Dunlap A. Healthcare teams neurodynamically reorganize when resolving uncertainty. Entropy. 2016;18(12):1–15. doi: 10.3390/e18120427 [DOI] [Google Scholar]
- 12.Zenati MA, Leissner K, Zorca S, Kennedy-Metz L, Yule S, Dias RD. First Reported Use of Team Cognitive Workload for Root Cause Analysis in Cardiac Surgery. Semin Thorac Cardiovasc Surg. 2019;31(3):394–396. doi: 10.1053/J.SEMTCVS.2018.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grewal D, Davidson HA. Emotional intelligence and graduate medical education. JAMA. 2008;300(10):1200–1202. [DOI] [PubMed] [Google Scholar]
- 14.Bose S, Oliveras E, Edson WN. How Can Self-Assessment Improve the Quality of Healthcare. Oper Res Issue Pap. 2001;2(4). [Google Scholar]
- 15.Normahani P, Makwana N, Rosenberg W Von, et al. Self-assessment of surgical ward crisis management using video replay augmented with stress biofeedback. Patient Saf Surg. 2018;12(6):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tarvainen MP, Niskanen JP, Lipponen JA, Ranta-aho PO, Karjalainen PA. Kubios HRV - Heart rate variability analysis software. Comput Methods Programs Biomed. 2014;113(1):210–220. doi: 10.1016/j.cmpb.2013.07.024 [DOI] [PubMed] [Google Scholar]
- 17.Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Eur Heart J. 1996;17:354–381. doi: 10.1161/01.CIR.93.5.1043 [DOI] [PubMed] [Google Scholar]
- 18.Shaffer F, Ginsberg JP. An Overview of Heart Rate Variability Metrics and Norms. Front Public Heal. 2017;5(September):1–17. doi: 10.3389/fpubh.2017.00258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Penttila J, Helminen A, Jartti T, Kuusela T. Time domain, geometrical and frequency domain analysis of cardiac vagal outflow: effects of various respiratory patterns. Clin Physiol. 2001;1:365–376. http://www.blackwell-synergy.com/doi/abs/10.1046/j.1365-2281.2001.00337.x. [DOI] [PubMed] [Google Scholar]
- 20.Conboy HM, Avrunin GS, Clarke LA, et al. Cognitive support during high-consequence episodes of care in cardiovascular surgery. 2017 IEEE Conf Cogn Comput Asp Situat Manag CogSIMA 2017. 2017. doi: 10.1109/COGSIMA.2017.7929610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Avrunin GS, Clarke LA, Conboy HM, et al. Toward Improving Surgical Outcomes by Incorporating Cognitive Load Measurement into Process-Driven Guidance. 2018 IEEE/ACM Int Work Softw Eng Healthc Syst 2018:2–9. doi: 10.1145/3194696.3194705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hull L, Arora S, Aggarwal R, Darzi A, Vincent C, Sevdalis N. The Impact of Nontechnical Skills on Technical Performance in Surgery: A Systematic Review. J Am Coll Surg. 2012;214(2):214–230. doi: 10.1016/j.jamcollsurg.2011.10.016 [DOI] [PubMed] [Google Scholar]
- 23.Zenati MA, Kennedy-Metz L, Dias RD. Cognitive Engineering to Improve Patient Safety and Outcomes in Cardiothoracic Surgery. Semin Thorac Cardiovasc Surg. 2019;32(1):1–7. doi: 10.1053/j.semtcvs.2019.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kennedy-Metz L, Weiss P, Parker SH. Results of exploratory investigation into adherence to auditory coping instructions during an acutely stressful task. Stress. 2020;23(2):144–152. doi: 10.1080/10253890.2019.1660317 [DOI] [PubMed] [Google Scholar]
- 25.Arora S, Russ S, Petrides K V., et al. Emotional intelligence and stress in medical students performing surgical tasks. Acad Med. 2011;86(10):1311–1317. doi: 10.1097/ACM.0b013e31822bd7aa [DOI] [PubMed] [Google Scholar]


