Abstract
Background:
The associations between ambient NO2 and diabetes and dyslipidemia have been controversial, and data is especially lacking in developing countries.
Objective:
This study aimed to assess the associations of long-term exposure to NO2 with diabetes and dyslipidemia in China.
Methods:
We conducted a cross-sectional study including 13,013 participants from the China Health and Retirement Longitudinal Study. The annual average concentrations of NO2 were estimated based on land-use regression, satellite measurements, and universal kriging. We applied logistic regression models to evaluate the associations of NO2 with diabetes and dyslipidemia, and linear regression models to assess the associations with blood biomarkers.
Results:
A total of 1,933 diabetes cases (14.85%) and 1,935 (14.87%) dyslipidemia cases were identified. Significant associations were observed between NO2 and risk of diabetes and dyslipidemia independent of PM2.5 and O3. For an interquartile range (IQR) increase in NO2 (12.39 μg/m3), we observed a 13% [odds ratio (OR): 1.13; 95% confidence interval (CI): 1.01, 1.26] increased risk of diabetes, 1.48% (95%CI: 0.51%, 2.46%) increase in glucose, 0.74% (95%CI: 0.19%, 1.29%) increase in glycosylated hemoglobin (HbA1c), 17% (OR: 1.17; 95% CI: 1.05, 1.31) increased risk of dyslipidemia, 4.62% (95%CI: 2.49%, 6.79%) increase in triglyceride, and a decrease of 2.96% (95%CI: 2.13%, 3.79%) in high-density lipoprotein. The associations of NO2 with glucose disorders were stronger among smokers.
Conclusions:
Our study indicated long-term exposure to NO2 might contribute to the development of diabetes and dyslipidemia, and the associations were potentially independent of O3 and PM2.5.
Keywords: air pollution, nitrogen dioxide, diabetes, dyslipidemia, glucolipid metabolism
Introduction
Glucose and lipid metabolism disorders are the primary risk factors for cardiovascular and cerebrovascular diseases, the leading cause of deaths worldwide. The prevalence of glucose and lipid metabolism-related diseases, including diabetes and dyslipidemia, has been rising rapidly, especially in developing countries (World Health Organization, 2016). It was estimated that the overall prevalence of diabetes and dyslipidemia were as high as 11.6% and 34.0%, respectively, among the Chinese adult population in 2010 (Xu et al., 2013; Pan et al., 2016).
Accumulating studies indicated that long-term exposure to air pollution can act as facilitators of glucose and lipid metabolism-related diseases (Pearson et al., 2010; Liu et al., 2016; Wang et al., 2018; Lao et al., 2019). While most previous studies put more emphasis on particulate matter, air pollution is a rather complex mixture consisting of both solid particles and various toxic gases. NO2 is a noxious gaseous pollutant and an important precursor in the formation of secondary aerosols and ozone, with ubiquitous sources mainly from fossil fuels. Only a limited number of studies were available on the toxicity of NO2 on glucose and lipid metabolic diseases, and the results were mixed, with positive associations found in some (Cai et al., 2017; Yang et al., 2018b) but null in others (Chen et al., 2016; Eze et al., 2017). It is also unclear whether the associations between NO2 and health outcomes are independent or are rather indicators of the impact of other air pollutants. In an integrated science assessment for NO2 in 2016, the United States Environmental Protection Agency concluded that “Available studies have not distinguished an independent effect of NO2 on cardiovascular diseases and diabetes.” However, recent studies demonstrated that the adverse health effects caused by NO2 were likely to be independent of other co-pollutants such as fine particulate matter (PM2.5) and ambient ozone (O3) (Wooding et al., 2019).
The associations between NO2 and blood biomarkers of glucose and lipid metabolism (e.g., HbA1c, cholesterol) were only investigated in a few studies and mostly in developed countries (Cai et al., 2017; Lucht et al., 2018). China’s rapid economic development has been accompanied by massive consumption of fossil fuels, resulting in high levels of air pollution. However, only a few single-center studies have explored the associations of long-term exposure of NO2 with health outcome in China (Yang et al., 2018a; Yang et al., 2018b; Mao et al., 2020). Most of these studies used the single-pollutant model without adjustment for the confounding co-pollutants such as PM2.5 and O3, thus they were unable to isolate the independent role of NO2. Also, some previous studies relied on self-report for case identification of diabetes and dyslipidemia, which would inevitably be biased due to the poor sensitivity of self-report (Yuan et al., 2015). It was estimated that nearly 50% of diabetes cases failed to be diagnosed (International Diabetes Federation, 2017). Therefore, national studies on associations between long-term NO2 exposure and metabolic diseases are needed in China, where air pollution levels are high, and prevalence rates of diabetes and dyslipidemia have been accelerating.
In this study, we utilized data from the third wave of a nationwide project, the China Health and Retirement Longitudinal Study (CHARLS), to investigate the associations of long-term exposure to NO2 with glucose and lipid metabolic diseases and six key biomarkers.
2. Materials and Methods
2.1. Study population
CHARLS aims to collect a high quality nationally representative sample of Chinese residents. Using a four-staged, stratified, cluster sampling method, participants were selected randomly from 450 villages or neighborhoods (the smallest administrative unit in China) in 150 counties or districts within 28 provinces (Zhao et al., 2014). Baseline information was collected during 2011 and 2012 through in-person interviews, and follow-up was conducted every two years. In this study, we used data collected in the third wave of CHARLS in 2015. A total of 21,095 participants completed face-to-face interviews and were encouraged to donate venous blood samples for blood tests. A standardized questionnaire was used to obtain individual information including demographics (e.g., age, sex, educational level, body mass index [BMI]), behavioral factors (smoking status, pack-years of smoking, and alcohol consumption), types of energy used for heating and cooking, and history of chronic diseases (e.g., diabetes and dyslipidemia) (Chen et al., 2019a). Finally, 13,013 participants who completed both questionnaires and blood tests were included in the current analysis.
2.2. Health data
A total of 13,013 participants donated blood samples, among which 85% (11,025) reported to have fasted overnight as required. Both fasting and non-fasting subjects were included in the current study. The transportation and storage of blood samples were strictly in accordance with the protocol (Chen et al., 2019a). Boronate affinity high-performance liquid chromatography method was used to examine glycosylated hemoglobin (HbA1c) level. Standard enzymatic colorimetric methods were used to measure levels of glucose (Hexokinase), HDL (Direct method), LDL (Direct method), cholesterol (Oxidase method), and triglyceride (Oxidase method).
The primary definition of diabetes was meeting at least one of the following criteria: a fasting blood glucose > 126 mg/dl, a non-fasting blood glucose > 200 mg/dl, HbA1c > 6.5%, or using antidiabetic medications including insulin, modern medicine or traditional Chinese medicine (Yuan et al., 2015). These cut-off points were in accordance with the recommendation from the American Diabetes Association (American Diabetes Association, 2014). Self-reported diabetes was defined as answering “Yes” to the question “Have you been diagnosed with diabetes or high blood sugar?”. The primary definition for dyslipidemia was the ratio of cholesterol to HDL ≥ 5.0 (Allison et al., 2008) or using lipid-lowering medications(Wang et al., 2017). Self-reported dyslipidemia was evaluated based on the question: “Have you ever been diagnosed with dyslipidemia?”.
2.3. Air pollution data
The annual average concentrations of NO2 in 2015 at the participants’ residential addresses were estimated using a national empirical model. Details on the exposure model has been described elsewhere (Xu et al., 2019). Briefly, this model was built incorporating land-use and meteorological data, ground-level NO2 concentrations from China’s regulatory monitors, and satellite-based measurements of NO2, at 1 km× 1 km spatial resolution. The model showed good predictive power with a 10-fold CV R2 of 0.78. We obtained the concentrations of PM2.5 and O3 in 2015 at a spatial resolution of 0·1° × 0·1° (approximately 11 km x 11 km at the equator) fro m the Global Burden of Disease project. The annual average concentrations of PM2.5 were estimated by combining satellite-based aerosol optical depth (AOD) data and simulations from chemical transport models, and the predictions were calibrated with ground-level monitoring data (Shaddick et al., 2018). The concentrations of O3 were estimated using the global chemical transport models and corrected with ground measurements (Shaddick et al., 2018). The concentrations of NO2, PM2.5, and O3 in the grids were assigned to the participants if their residential addresses fell into the corresponding grids.
2.4. Statistical analysis
We used multivariable logistic regression models to examine the associations between NO2 and diabetes/dyslipidemia and multivariable linear regression models to investigate the associations between NO2 and glucose levels (glucose and HbA1c) and lipid levels (HDL, LDL, cholesterol, and triglyceride). All biomarkers were log transformed to improve the normality before statistical analysis. We established four models to explore these associations. Model 1 adjusted for age, sex, educational level (low, ≤ 5years; medium, 6–9 years; high, >9 years), body mass index (BMI, <18.5 kg/m2,18.5 – 24.9 kg/m2, ≥ 25 kg/m2), smoking status (current smokers, ex-smoker and non-smoker), pack-years for current smokers (pack per day multiplied by years of smoking), frequency of alcohol consumption (never, < 1 / month, > 1 / month), energy types for cooking and heating (clean, central heating, solar energy, electricity natural gas; unclean, coal or biomass). We additionally adjusted for ambient O3 (model 2), PM2.5 (model 3), or both (model 4, the primary model). There was no significant collinearity among the three air pollutants according to the variance inflation factor, so they could be simultaneously adjusted in the models.
In order to evaluate potential effect modifiers, we conducted stratification analyses by age (21–64 years and ≥65 years), sex (male and female), BMI (<18.5 kg/m2,18.5 – 24.9 kg/m2, ≥ 25 kg/m2), smoking status (current or former smokers, never smokers), and alcohol consumption (ever/never). The statistical significance of the potential effect modifier was tested by calculating the 95% CIs of the effect differences between strata using the following formula , where Q1 and Q2 were the estimates in each strata and Se1 and Se2 were the corresponding standard errors (Schenker and Gentleman, 2001; Payton et al., 2003). P values for the potential effect modifiers were calculated based on 95% CIs (Altman and Bland, 2011).
We did sensitivity analyses by repeating the above analyses using self-reported diabetes and dyslipidemia. We also did sensitivity analyses by excluding diabetes cases defined only by non-fasting glucose to test the stability of the associations.
The effect estimates were presented per interquartile range (IQR) increase in NO2. We reported odds ratios (ORs) and 95%CIs for logistic regression models and percent changes (95%CI) for all biomarkers. All statistical tests were two-sided, and a p-value less than 0.05 was considered statistically significant.
3. Results
3.1. Descriptive statistics
Location of the CHARLS study sites distributed in 450 villages or neighborhoods (the smallest administrative unit in China) in 150 counties or districts within 28 provinces (Figure 1). Baseline characteristics, the prevalence of diabetes and dyslipidemia, mean concentrations of biomarkers, and air pollutants were summarized in Table 1. A total of 13,013 subjects were included in the current analysis. The mean age was 61.88 years, 46.04% were men, and the mean BMI was 23.95 kg/m2. A total of 1,933 (14.85%) diabetes cases and 1,935 (14.87%) dyslipidemia cases were identified using the primary outcome definitions. The average levels of glucose, HbA1c, HDL, LDL, cholesterol, and triglyceride were 103.6 mg/dl, 5.98%, 51.21 mg/dl, 102.22 mg/dl, 183.94 mg/dl, and 143.20 mg/dl, respectively. Strong correlations were observed between LDL and cholesterol (r=0.87) as well as between glucose and HbA1c (r=0.70). The remaining correlations among the biomarkers were weak (Table S1). The demographic characteristics of the excluded population were similar to those of the included population (Table S2). The annual average concentrations of NO2 varied greatly among participants from 6.77 μg/m3 to 58.41 μg/m3, with a mean of 24 μg/m3 (IQR, 12.39 μg/m3). The average of the annual mean concentrations of PM2.5 and O3 at residential addresses were 57.32 μg/m3 and 68.27 μg/m3, respectively. There were moderate to high correlations among air pollutants (r = 0.72 for NO2 and PM2.5, r = 0.56 for NO2 and O3, r= 0.71 for PM2.5 and O3) (Table S3).
Figure 1 :
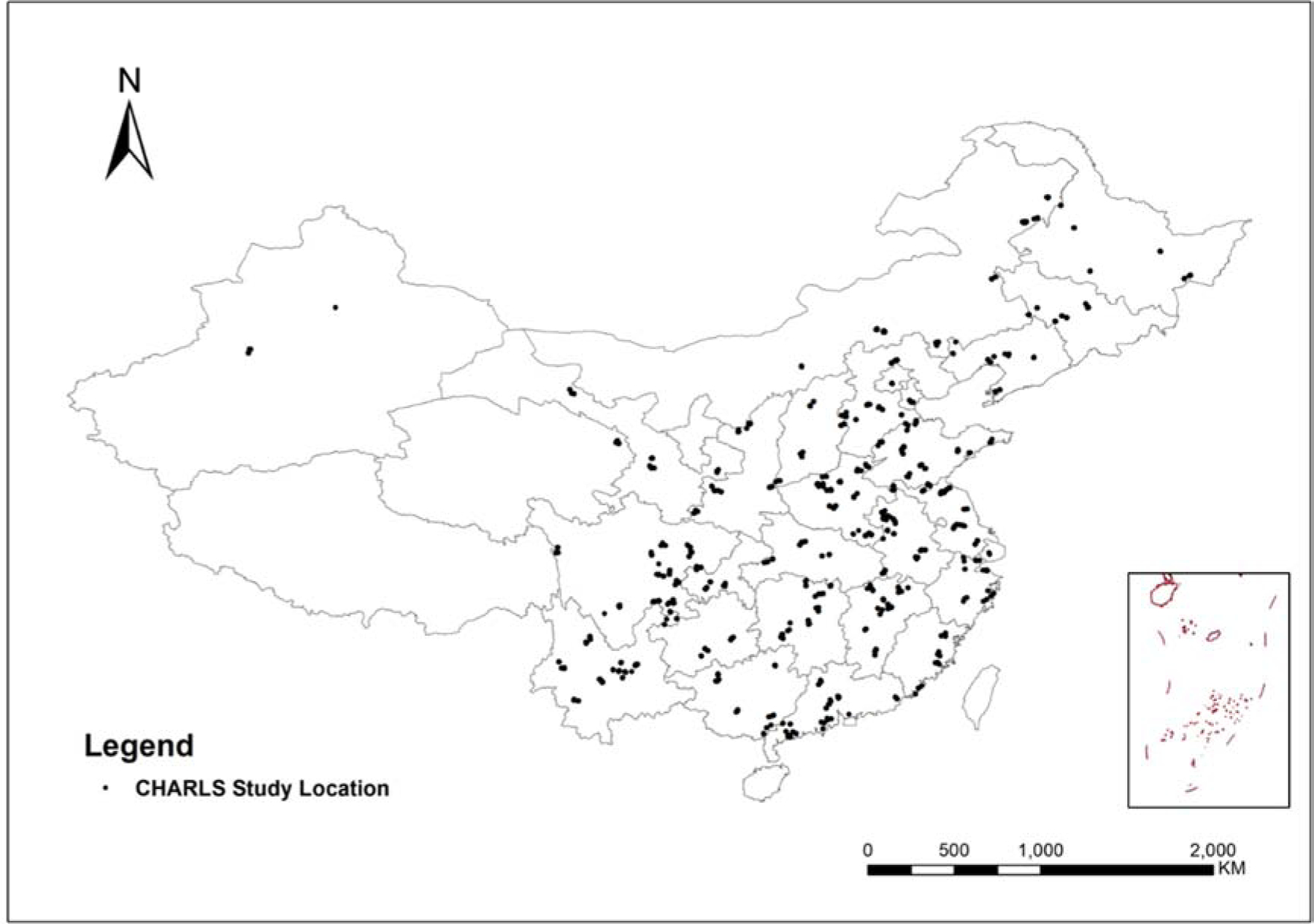
Locations of the study sites in the CHARLS project.
Table 1.
Baseline characteristics of the study participants.
| Characteristics | Value |
|---|---|
| Age (year, mean ± SD) | 61.88 ± 10.02 |
| Sex N (%) | |
| Female | 7021 (53.96) |
| Male | 5991 (46.04) |
| Educational level N (%) | |
| Low | 2927 (27.40) |
| Medium | 4418 (41.36) |
| High | 3336 (31.23) |
| BMI (kg/m2, mean ± SD) | 23.94 ± 3.74 |
| Smoking status N (%) | |
| Never | 7758 (59.68) |
| Former | 1746 (13.43) |
| Current | 3496 (26.89) |
| Pack-years of cigarette for current smokers | 32.73 ± 10.02 |
| Drinking frequency N (%) | |
| Never | 8481 (65.26) |
| <1/month | 1134 (8.73) |
| >1/month | 3380 (26.01) |
| Type of energy N (%) | |
| Clean (central heating, solar energy, electricity, natural gas) | 6657 (51.42) |
| Unclean (coal or biomass) | 6290 (48.58) |
| Diabetes | |
| Prevalence of diabetes (%) | 1933 (14.85) |
| Glucose (mg/dL mean ± SD) | 103.6 ± 35.4 |
| HbA1c (%, mean ± SD) | 5.98 ± 0.99 |
| Dyslipidemia | |
| Prevalence of dyslipidemia (%) | 1935 (14.87) |
| HDL (mg/dL mean ± SD) | 51.21 ± 11.58 |
| LDL (mg/dL mean ± SD) | 102.22 ± 29.01 |
| Cholesterol (mg/dL mean ± SD) | 183.94 ± 36.62 |
| Triglyceride (mg/dL mean ± SD) | 143.20 ± 91.30 |
| Exposure to air pollutants | |
| NO2 (μg/m3, mean (IQR)) | 24.00 (17.84 – 30.22) |
| PM2.5 (μg/m3, mean (IQR)) | 57.32 (40.31 – 71.78) |
| O3 (μg/m3, mean (IQR)) | 68.27 (60.30 – 74.41) |
Abbreviations: SD, standard deviation; BMI, Body mass index; HbA1c, glycosylated hemoglobin, %; HDL, high density lipoprotein; LDL, low density lipoprotein; IQR, interquartile range (P75–P25); NO2, nitrogen dioxide; PM2.5, particulate matter with an aerodynamic diameter less than or equal to 2.5 μm; O3, ozone
3.2. Regression results
Table 2 presents the associations between NO2 exposure and diabetes and dyslipidemia. We found significant positive associations of NO2 concentration and diabetes, blood glucose, and HbA1c in all models. The associations remained after adjustment of O3, while were attenuated but remained statistically significant after adjustment of PM2.5. In model 4, an IQR increase in NO2 was associated with a 13% increase in risk of diabetes (OR=1.13, 95%CI: 1.01, 1.26), a 1.48% (95%CI: 0.51%, 2.46%) increment in glucose, and a 0.74% (95%CI: 0.19%, 1.29%) elevation in HbA1c. Higher NO2 exposure was also associated with increased risk of dyslipidemia, increased concentrating of triglyceride, and decreased concentration of HDL. Each IQR increase in NO2 was associated with a 17% (OR 1.17, 95%CI, 1.05, 1.31) increased risk of dyslipidemia, a 4.62% (95%CI: 2.49%, 6.79%) increase in triglyceride and a 2.96% (95%CI: 2.13%, 3.79%) decrease in HDL (model 4). No associations were observed between NO2 exposure and LDL or cholesterol after full adjustment.
Table 2.
Changes (point estimates and 95% confidence intervals) in health indicators associated with an interquartile range increase in NO2.
| Health indicators | point estimates and 95%
confidence intervals |
|||
|---|---|---|---|---|
| Model1 | Model2 | Model3 | Model4 | |
| Diabetes | ||||
| Prevalence of diabetes (odds ratio) | 1.17 (1.09, 1.26) | 1.17 (1.06, 1.28) | 1.12 (1.01, 1.25) | 1.13 (1.01, 1.26) |
| Fasting glucose (% change) | 2.25 (1.59, 2.91) | 2.23 (1.42, 3.05) | 1.38 (0.43, 2.35) | 1.48 (0.51, 2.46) |
| HbA1c (% change) | 0.85 (0.48, 1.22) | 1.00 (0.55, 1.46) | 0.66 (0.11, 1.20) | 0.74 (0.19, 1.29) |
| Dyslipidemia | ||||
| Prevalence of dyslipidemia (odds ratio) | 1.14 (1.06, 1.23) | 1.26 (1.15, 1.38) | 1.13 (1.01, 1.26) | 1.17 (1.05, 1.31) |
| HDL (% change) | −2.57 (−3.13, −2.01) | −3.12 (−3.80, −2.44) | −2.76 (−3.57, −1.94) | −2.96 (−3.79, −2.13) |
| LDL (% change) | −1.86 (−2.62, −1.09) | 0.61 (−0.35, 1.58) | 0.08 (−1.07, 1.23) | 0.85 (−0.32, 2.03) |
| Cholesterol (% change) | −1.81 (−2.32, −1.30) | −0.06 (−0.70, 0.58) | −0.65 (−1.40, 0.12) | −0.08 (−0.85, 0.70) |
| Triglyceride (% change) | 0.49 (−0.88, 1.89) | 3.42 (1.68, 5.19) | 3.83 (1.74, 5.95) | 4.62 (2.49, 6.79) |
Abbreviations:NO2, nitrogen dioxide; HbA1c, glycosylated hemoglobin; HDL, high density lipoprotein; LDL, low density lipoprotein. Note: Model1, adjusted age, sex, educational level (low, medium, high), BMI (<18.5, 18.5–24.9, ≥25), smoking status (current smokers, ex-smoker and non-smoker), pack-years for current smokers, drinking frequency (never, < 1 / month, > 1 / month), energy types for cooking and heating (clean, unclean); Model2, Model1 + O3; Model3, Model1 + PM2.5; Model4, Model1 + O3 + PM2.5. All biomarkers were log transformed in the association analysis.
Results of stratified analyses were shown in Table 3 and Table 4. For dyslipidemia or related biomarkers, we did not find any significant modifying effects based on current stratified analysis. However, we found the associations between NO2 and glucose disorders were significantly stronger among smokers (Table 3)
Table 3.
Changes (point estimates and 95% confidence intervals) in health indicators for diabetes associated with an interquartile range increase in NO2 stratified by potential modifiers.
| Variables | Categories | N | Diabetes |
Fasting glucose |
HbA1c |
|||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p | % change (95% CI) | p | % change (95% CI) | p | |||
| Age | 21–64 | 7844 | 1.19 (1.02, 1.39) | 0.43 | 1.46 (0.20, 2.74) | 0.76 | 0.94 (0.22, 1.66) | 0.58 |
| ≥65 | 5023 | 1.09 (0.93, 1.28) | 1.80 (0.27, 3.36) | 0.61 (−0.24, 1.47) | ||||
| Sex | Female | 7021 | 1.06 (0.91, 1.24) | 0.27 | 1.28 (−0.04, 2.63) | 0.66 | 0.35 (−0.42, 1.12) | 0.12 |
| Male | 5991 | 1.21 (1.02, 1.42) | 1.74 (0.31, 3.19) | 1.22 (0.44, 2.01) | ||||
| BMI kg/m2 | <18.5 | 717 | 1.21 (0.60, 2.44) | 0.83 | 5.52 (0.87, 10.39) | 0.10 | 1.36 (−1.37, 4.17) | 0.72 |
| 18.5–24.9 | 7442 | 1.11 (0.95, 1.31) | 1.45 (0.21, 2.70) | 0.81 (0.12, 1.50) | ||||
| ≥25 | 4854 | 1.12 (0.96, 1.31) | 1.12 (−0.55, 2.81) | 0.55 (−0.41, 1.51) | ||||
| Smoking status | No | 7758 | 1.01 (0.87, 1.17) | 0.03 | 0.55 (−0.70, 1.82) | 0.03 | 0.25 (−0.47, 0.97) | 0.04 |
| Yes | 5242 | 1.29 (1.09, 1.54) | 2.78 (1.24, 4.34) | 1.40 (0.55, 2.25) | ||||
| Drinking | No | 8481 | 1.11 (0.97, 1.27) | 0.69 | 1.44 (0.20, 2.69) | 0.89 | 0.82 (0.11, 1.54) | 0.80 |
| Yes | 4514 | 1.17 (0.96, 1.42) | 1.59 (0.02, 3.18) | 0.67 (−0.17, 1.52) | ||||
Abbreviations: NO2, nitrogen dioxide; BMI, Body mass index; HbA1c, glycosylated hemoglobin; OR, odds ratio.
Note: categories for education (low ≤ 9 years; high ≥ 9 years); models adjusted for age, sex, educational level (low, medium, high), BMI (<18.5 kg/m2, 18.5–24.9 kg/m2, ≥25 kg/m2), smoking status (current smokers, ex-smoker and non-smoker), pack-years for current smokers, drinking frequency (never, < 1 / month, > 1 / month), energy types for cooking and heating (clean, unclean), O3, PM2.5. All biomarkers were log transformed in the association analysis.
Table 4.
Changes (point estimates and 95% confidence intervals) in health indicators for dyslipidemia associated with an interquartile range increase in NO2 stratified by potential modifiers.
| Variables | Categories | N | Dyslipidemia |
HDL |
LDL |
Cholesterol |
Triglyceride |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR and 95%CI | p | % change (95% CI) | p | % change (95% CI) | p | % change (95% CI) | p | % change (95% CI) | p | |||
| Age | 21–64 | 7844 | 1.10 (0.95, 1.28) | 0.16 | −2.96 (−4.02, −1.89) | 0.92 | 1.51 (−0.04, 3.08) | 0.33 | −0.06 (−1.08, 0.96) | 0.89 | 3.71 (0.84, 6.67) | 0.38 |
| ≥65 | 5023 | 1.29 (1.09, 1.52) | −3.05 (−4.36, −1.72) | 0.31 (−1.47, 2.12) | 0.06 (−1.13, 1.26) | 5.67 (2.56, 8.86) | ||||||
| Sex | Female | 7021 | 1.11 (0.95, 1.29) | 0.35 | −2.30 (−3.38, −1.20) | 0.08 | 1.29 (−0.26, 2.87) | 0.38 | 0.20 (−0.82, 1.24) | 0.33 | 3.15 (0.33, 6.04) | 0.20 |
| Male | 5991 | 1.24 (1.05, 1.46) | −3.79 (−5.04, −2.52) | 0.23 (−1.52, 2.01) | −0.57 (−1.72, 0.59) | 5.94 (2.77, 9.21) | ||||||
| BMI kg/m2 | <18.5 | 717 | 1.17 (0.48, 2.85) | 0.99 | −3.93 (−8.27, 0.61) | 0.82 | −1.40 (−6.94, 4.48) | 0.53 | −2.58 (−6.27, 1.27) | 0.23 | 5.49 (−2.88, 14.58) | 0.92 |
| 18.5–24.9 | 7442 | 1.18 (1.00, 1.39) | −3.37 (−4.51, −2.23) | 0.56 (−0.97, 2.12) | −0.13 (−1.15, 0.89) | 6.01 (3.19, 8.92) | ||||||
| ≥25 | 4854 | 1.16 (0.99, 1.34) | −2.10 (−3.32, −0.86) | 1.45 (−0.45, 3.38) | 0.28 (−0.97, 1.55) | 2.44 (−1.02, 6.02) | ||||||
| Smoking status | No | 7758 | 1.11 (0.95, 1.29) | 0.21 | −2.76 (−3.78, −1.72) | 0.59 | 0.99 (−0.49, 2.49) | 0.69 | −0.23 (−1.21, 0.76) | 0.88 | 2.73 (0.05, 5.48) | 0.08 |
| Yes | 5242 | 1.24 (1.05, 1.46) | −3.24 (−4.60, −1.87) | 0.48 (−1.40, 2.39) | −0.10 (−1.34, 1.15) | 6.66 (3.25, 10.18) | ||||||
| Drinking | No | 8481 | 1.17 (1.02, 1.33) | 0.92 | −2.87 (−3.86, −1.86) | 0.69 | 0.69 (−0.75, 2.15) | 0.68 | −0.06 (−1.03, 0.92) | 0.91 | 4.59 (1.98, 7.27) | 0.88 |
| Yes | 4514 | 1.18 (0.97, 1.44) | −3.24 (−4.70, −1.77) | 1.23 (−0.75, 3.24) | −0.15 (−1.42, 1.13) | 4.20 (0.59, 7.94) | ||||||
Abbreviations: NO2, nitrogen dioxide; BMI, Body mass index; HDL, high density lipoprotein; LDL, low density lipoprotein.
Note: categories for education (low ≤ 9 years; high ≥ 9 years); models adjusted for age, sex, educational level (low, medium, high), BMI (<18.5 kg/m2, 18.5–24.9 kg/m2, ≥25 kg/m2), smoking status (current smokers, ex-smoker and non-smoker), pack-years for current smokers, drinking frequency (never, < 1 / month, > 1 / month), energy types for cooking and heating (clean, unclean), O3, PM2.5. All biomarkers were log transformed in the association analysis. All biomarkers were log transformed in the association analysis.
When using self-report for definitions, the prevalence of diabetes was appreciably lower (9.00%) than that using the primary definition (14.85%). The sensitivity of self-reported diabetes was 49%, and the specificity was 81%. While the prevalence of dyslipidemia remained similar, the sensitivity and specificity of self-reported dyslipidemia were 62% and 63%, respectively. The associations between NO2 and both self-reported diabetes and self-reported dyslipidemia remained significant (Table S4). After excluding diabetes cases that were diagnosed only by non-fasting glucose, the association remained stable. An IQR increase in NO2 was associated with a 13% increase in risk of diabetes (OR=1.13, 95%CI: 1.01, 1.26) (Table S4).
4. Discussion
In this nationwide cross-sectional study, we found that exposure to NO2 air pollution was significantly associated with diabetes and dyslipidemia independent of other co-pollutants (PM2.5 and O3). The associations were consistent when using different definitions of diabetes and dyslipidemia. The associations between NO2 and risks of diabetes and glucose biomarkers were stronger among ever smokers compared to never smokers. To our knowledge, this is the largest nationwide study to explore the associations between long-term exposure of NO2 and glucose and lipids levels in developing countries.
The association between ambient NO2 exposure and diabetes has been investigated in several epidemiological studies (Andersen et al., 2012; Yang et al., 2018b; Yang et al., 2020). A recent meta-analysis including 11 studies primarily from developed countries reported that the OR of diabetes was 1.07 (95%CI: 1.04, 1.11) per 10 μg/m3 increment in NO2 exposure (Yang et al., 2020). In line with these results, our study in China also suggested a significantly positive association between NO2 and diabetes with a comparable effect size (OR=1.13, 95%CI: 1.01, 1.26, per an IQR (12.39 μg/m3) increment of NO2). Fasting glucose and HbA1c are both important biomarkers of glucose-homeostasis and are used for diabetes diagnosis. However, very few studies have assessed the associations of NO2 with blood glucose and HbA1c, and the results were inconsistent. Consistent with our results, Chuang et al., found elevated fasting glucose and HbA1c were positively associated with long-term exposure to NO2 in an analysis among 1,023 elderly subjects in Taiwan (Chuang et al., 2011). Similarly, in a cross-sectional study including 15,477 adults from mainland China, Yang et al., observed NO2 was associated with a higher concentration of plasma glucose (Yang et al., 2018b). In contrast, a study including 7,108 observations in Germany found no association between NO2 and blood glucose or HbA1c (Lucht et al., 2018). The inconsistency of these results might be attributable to differences in geographic locations, study populations, and exposure levels. The associations of NO2 with diabetes and glucose metabolism appear to be biologically plausible. Preliminary evidence from toxicological studies and some epidemiological studies suggested that long-term exposure to NO2 was positively associated with low-grade systemic inflammation (including adipose tissue inflammation) and oxidative stress (Li et al., 2011; Riedl et al., 2012). These effects can further lead to impaired insulin signaling, which plays a key role in glucose homeostasis (Sun et al., 2009; Chen et al., 2016).
Dyslipidemia plays a key role in the development of cardiovascular diseases (Brunham et al., 2008). The positive associations we observed between NO2 exposure and dyslipidemia were largely consistent with previous studies, though mixed findings existed. The Chinese Health Study of 33 Communities found that long-term NO2 exposure was associated with risk of hypercholesterolemia, higher cholesterol and triglyceride levels, and lower HDL-C level (Yang et al., 2018a). Consistent results were also reported from the Korean Community Health Survey (Shin et al., 2019). A pooled study of 144,082 European participants reported that NO2 was significantly associated with elevated triglycerides and HDL cholesterol, but not with total cholesterol (Cai et al., 2017). Another study among 1,023 Mexican Americans reported no associations between NO2 exposure and any lipids concentration (Chen et al., 2016). The geographic differences, varying health status of participants, and variables included in statistical models complicated the comparison across studies. The biological mechanism underlying these associations remains unclear. One possible explanation is that systemic inflammation and oxidative stress induced by inhaled NO2 might trigger lipid oxidation and impair lipid metabolism (Chen et al., 2019b).
In this study, we observed that associations between NO2 and glucose disorders appeared to be stronger among smokers than non-smokers, which were consistent with the findings from an Italian study (Orioli et al., 2018). On the contrary, another study in Denmark that investigated the modification effect of smoking status reported stronger associations among non-smokers (Andersen et al., 2012). Smoking and air pollution were both identified as important risk factors for diabetes and shared similar biological pathways triggering glucose metabolic disorder, such as systemic inflammation and oxidative stress. Some studies also suggested preexisting subclinical inflammation might enhance the diabetogenic effects of air pollution (Kramer et al., 2010). These findings, along with our results, supported that smokers, who had chronic low-level inflammation, might be more susceptible to NO2.
Few epidemiological studies explored whether the associations of NO2 with diabetes or dyslipidemia were independent of other co-pollutants. A study conducted in Northwest China among 3,912 type-2 diabetes patients found that the associations between NO2 and triglyceride disappeared after adjustment of PM2.5 and sulfur dioxide, while the associations with HDL and LDL remained statistically significant (Wang et al., 2018). In the current study, adjustment for O3 did not materially change the associations between NO2 and glucose and lipid indicators. The associations with glucose disorders weakened after adjustment for PM2.5 but remained statistically significant even in three-pollutants models. The results in this study supported that the associations of NO2 with glucose and lipid metabolism could be potentially independent of O3 or PM2.5.
Some limitations of this study should be noted. First, exposure misclassification was likely as we obtained the exposure of NO2 from a prediction model rather than personal monitoring, and indoor environment air pollution was not considered. Second, although our study adjusted for multiple individual-level confounders, residual confounding from unmeasured factors such as physical activity, noise, and other traffic-related pollutants, could not be ruled out. Finally, this study was based on a cross-sectional design, thus it was not possible to determine temporal precedence or to establish causality. Future studies with prospective cohort study design and full adjustment of co-pollutants would be valuable to verify the associations between NO2 and glucose and lipid metabolic diseases.
Conclusion
Our study suggests that long-term exposure to NO2 air pollution was significantly associated with glucose and lipids metabolic diseases in China, and the associations were potentially independent of O3 and PM2.5. The associations of NO2 with diabetes and glucose biomarkers were stronger among smokers. Our findings have important public health implications for the prevention of diabetes and dyslipidemia.
Supplementary Material
Highlights.
Long-term exposure to NO2 was associated with diabetes and dyslipidemia.
Associations of NO2 with blood glucose and lipid were independent of O3 and PM2.5.
The associations between NO2 and glucose disorders were stronger among smokers.
Acknowledgment
This work was funded by the National Natural Science Foundation of China (91843302 and 71603013), China Medical Board Collaborating Program (16–250 and 16–249) and National Institute on Aging (R01 AG-037031 and R01AG-053228).The authors thank Dr. Julian D. Marshall at the University of Washington for sharing the data of NO2 and Dr.Michael Brauer at the University of British Columbia for sharing the data of PM2.5 and O3.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interests
The authors declared no conflicts of interest.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Reference:
- Allison MA, Budoff MJ, Wong ND, Blumenthal RS, Schreiner PJ, Criqui MH, 2008. Prevalence of and risk factors for subclinical cardiovascular disease in selected US Hispanic ethnic groups: the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol 167, 962–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altman DG, Bland JM, 2011. How to obtain the P value from a confidence interval. BMJ 343, d2304. [DOI] [PubMed] [Google Scholar]
- American Diabetes Association, 2014. Diagnosis and classification of diabetes mellitus. Diabetes care 37 Suppl 1, S81–S90. [DOI] [PubMed] [Google Scholar]
- Andersen ZJ, Raaschou-Nielsen O, Ketzel M, Jensen SS, Hvidberg M, Loft S, Tjonneland A, Overvad K, Sorensen M, 2012. Diabetes incidence and long-term exposure to air pollution: a cohort study. Diabetes Care 35, 92–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunham LR, Kruit JK, Verchere CB, Hayden MR, 2008. Cholesterol in islet dysfunction and type 2 diabetes. J Clin Invest 118, 403–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Y, Hansell AL, Blangiardo M, Burton PR, BioShaRe, de Hoogh K, Doiron D, Fortier I, Gulliver J, Hveem K, Mbatchou S, Morley DW, Stolk RP, Zijlema WL, Elliott P, Hodgson S., 2017. Long-term exposure to road traffic noise, ambient air pollution, and cardiovascular risk factors in the HUNT and lifelines cohorts. Eur Heart J 38, 2290–2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X, Crimmins E, Hu PP, Kim JK, Meng Q, Strauss J, Wang Y, Zeng J, Zhang Y, Zhao Y, 2019a. Venous Blood-Based Biomarkers in the China Health and Retirement Longitudinal Study: Rationale, Design, and Results From the 2015 Wave. Am J Epidemiol 188, 1871–1877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z, Newgard CB, Kim JS, Iikayeva O, Alderete TL, Thomas DC, Berhane K, Breton C, Chatzi L, Bastain TM, McConnell R, Avol E, Lurmann F, Muehlbauer MJ, Hauser ER, Gilliland FD, 2019b. Near-roadway air pollution exposure and altered fatty acid oxidation among adolescents and young adults - The interplay with obesity. Environ Int 130, 104935–104935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z, Salam MT, Toledo-Corral C, Watanabe RM, Xiang AH, Buchanan TA, Habre R, Bastain TM, Lurmann F, Wilson JP, Trigo E, Gilliland FD, 2016. Ambient Air Pollutants Have Adverse Effects on Insulin and Glucose Homeostasis in Mexican Americans. Diabetes care 39, 547–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang KJ, Yan YH, Chiu SY, Cheng TJ, 2011. Long-term air pollution exposure and risk factors for cardiovascular diseases among the elderly in Taiwan. Occup Environ Med 68, 64–68. [DOI] [PubMed] [Google Scholar]
- Eze IC, Foraster M, Schaffner E, Vienneau D, Heritier H, Rudzik F, Thiesse L, Pieren R, Imboden M, von Eckardstein A, Schindler C, Brink M, Cajochen C, Wunderli JM, Roosli M, Probst-Hensch N, 2017. Long-term exposure to transportation noise and air pollution in relation to incident diabetes in the SAPALDIA study. Int J Epidemiol 46, 1115–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Diabetes Federation, 2017. IDF Diabetes Atlas. 8th Edition, International Diabetes Federation, Brussels. [Google Scholar]
- Kramer U, Herder C, Sugiri D, Strassburger K, Schikowski T, Ranft U, Rathmann W, 2010. Traffic-related air pollution and incident type 2 diabetes: results from the SALIA cohort study. Environ Health Perspect 118, 1273–1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lao XQ, Guo C, Chang L-Y, Bo Y, Zhang Z, Chuang YC, Jiang WK, Lin C, Tam T, Lau AKH, Lin C-Y, Chan T-C, 2019. Long-term exposure to ambient fine particulate matter (PM(2.5)) and incident type 2 diabetes: a longitudinal cohort study. Diabetologia 62, 759–769. [DOI] [PubMed] [Google Scholar]
- Li H, Han M, Guo L, Li G, Sang N, 2011. Oxidative stress, endothelial dysfunction and inflammatory response in rat heart to NO inhalation exposure. Chemosphere 82, 1589–1596. [DOI] [PubMed] [Google Scholar]
- Liu C, Yang C, Zhao Y, Ma Z, Bi J, Liu Y, Meng X, Wang Y, Cai J, Chen R, Kan H, 2016. Associations between long-term exposure to ambient particulate air pollution and type 2 diabetes prevalence, blood glucose and glycosylated hemoglobin levels in China. Environ Int 92–93, 416–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucht SA, Hennig F, Matthiessen C, Ohlwein S, Icks A, Moebus S, Jockel KH, Jakobs H, Hoffmann B, 2018. Air Pollution and Glucose Metabolism: An Analysis in Non-Diabetic Participants of the Heinz Nixdorf Recall Study. Environ Health Perspect 126, 047001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao S, Chen G, Liu F, Li N, Wang C, Liu Y, Liu S, Lu Y, Xiang H, Guo Y, Li S, 2020. Long-term effects of ambient air pollutants to blood lipids and dyslipidemias in a Chinese rural population. Environ Pollut 256, 113403. [DOI] [PubMed] [Google Scholar]
- Orioli R, Cremona G, Ciancarella L, Solimini AG, 2018. Association between PM10, PM2.5, NO2, O3 and self-reported diabetes in Italy: A cross-sectional, ecological study. PLoS One 13, e0191112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan L, Yang Z, Wu Y, Yin R-X, Liao Y, Wang J, Gao B, Zhang L, China National Survey of Chronic Kidney Disease Working, G., 2016. The prevalence, awareness, treatment and control of dyslipidemia among adults in China. Atherosclerosis 248, 2–9. [DOI] [PubMed] [Google Scholar]
- Payton ME, Greenstone MH, Schenker N, 2003. Overlapping confidence intervals or standard error intervals: what do they mean in terms of statistical significance? J Insect Sci 3, 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson JF, Bachireddy C, Shyamprasad S, Goldfine AB, Brownstein JS, 2010. Association between fine particulate matter and diabetes prevalence in the U.S. Diabetes care 33, 2196–2201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riedl MA, Diaz-Sanchez D, Linn WS, Gong H Jr., Clark KW, Effros RM, Miller JW, Cocker DR, Berhane KT, 2012. Allergic inflammation in the human lower respiratory tract affected by exposure to diesel exhaust. Res Rep Health Eff Inst, 5–43; discussion 45–64. [PubMed] [Google Scholar]
- Schenker N, Gentleman JF, 2001. On judging the significance of differences by examining the overlap between confidence intervals. Am Stat 55, 182–186. [Google Scholar]
- Shaddick G, Thomas ML, Amini H, Broday D, Cohen A, Frostad J, Green A, Gumy S, Liu Y, Martin RV, Pruss-Ustun A, Simpson D, van Donkelaar A, Brauer M, 2018. Data Integration for the Assessment of Population Exposure to Ambient Air Pollution for Global Burden of Disease Assessment. Environ Sci Technol 52, 9069–9078. [DOI] [PubMed] [Google Scholar]
- Shin J, Choi J, Kim KJ, 2019. Association between long-term exposure of ambient air pollutants and cardiometabolic diseases: A 2012 Korean Community Health Survey. Nutr Metab Cardiovasc Dis 29, 144–151. [DOI] [PubMed] [Google Scholar]
- Sun Q, Yue P, Deiuliis JA, Lumeng CN, Kampfrath T, Mikolaj MB, Cai Y, Ostrowski MC, Lu B, Parthasarathy S, Brook RD, Moffatt-Bruce SD, Chen LC, Rajagopalan S, 2009. Ambient air pollution exaggerates adipose inflammation and insulin resistance in a mouse model of diet-induced obesity. Circulation 119, 538–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M, Zheng S, Nie Y, Weng J, Cheng N, Hu X, Ren X, Pei H, Bai Y, 2018. Association between Short-Term Exposure to Air Pollution and Dyslipidemias among Type 2 Diabetic Patients in Northwest China: A Population-Based Study. Inter J Env Res Pub Heal 15, 631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z, Li C, Yang Z, Ma J, Zou Z, 2017. Fetal and infant exposure to severe Chinese famine increases the risk of adult dyslipidemia: Results from the China health and retirement longitudinal study. BMC Public Health 17, 488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wooding DJ, Ryu MH, Hüls A, Lee AD, Lin DTS, Rider CF, Yuen ACY, Carlsten C, 2019. Particle Depletion Does Not Remediate Acute Effects of Traffic-related Air Pollution and Allergen. A Randomized, Double-Blind Crossover Study. Am J Respir Crit Care Med 200, 565–574. [DOI] [PubMed] [Google Scholar]
- World Health Organization, 2016. Global report on diabetes. World Health Organization. [Google Scholar]
- Xu H, Bechle MJ, Wang M, Szpiro AA, Vedal S, Bai Y, Marshall JD, 2019. National PM2.5 and NO2 exposure models for China based on land use regression, satellite measurements, and universal kriging. Sci Total Environ 655, 423–433. [DOI] [PubMed] [Google Scholar]
- Xu Y, Wang L, He J, Bi Y, Li M, Wang T, Wang L, Jiang Y, Dai M, Lu J, Xu M, Li Y, Hu N, Li J, Mi S, Chen C-S, Li G, Mu Y, Zhao J, Kong L, Chen J, Lai S, Wang W, Zhao W, Ning G, China Noncommunicable Disease Surveillance, G., 2013. Prevalence and control of diabetes in Chinese adults. JAMA 310, 948–959. [DOI] [PubMed] [Google Scholar]
- Yang B-Y, Bloom MS, Markevych I, Qian ZM, Vaughn MG, Cummings-Vaughn LA, Li S, Chen G, Bowatte G, Perret JL, Dharmage SC, Heinrich J, Yim SH-L, Lin S, Tian L, Yang M, Liu K-K, Zeng X-W, Hu L-W, Guo Y, Dong G-H, 2018a. Exposure to ambient air pollution and blood lipids in adults: The 33 Communities Chinese Health Study. Environ Int 119, 485–492. [DOI] [PubMed] [Google Scholar]
- Yang BY, Fan S, Thiering E, Seissler J, Nowak D, Dong GH, Heinrich J, 2020. Ambient air pollution and diabetes: A systematic review and meta-analysis. Environ Res 180, 108817. [DOI] [PubMed] [Google Scholar]
- Yang BY, Qian ZM, Li S, Chen G, Bloom MS, Elliott M, Syberg KW, Heinrich J, Markevych I, Wang SQ, Chen D, Ma H, Chen DH, Liu Y, Komppula M, Leskinen A, Liu KK, Zeng XW, Hu LW, Guo Y, Dong GH, 2018b. Ambient air pollution in relation to diabetes and glucose-homoeostasis markers in China: a cross-sectional study with findings from the 33 Communities Chinese Health Study. Lancet Planet Health 2, e64–e73. [DOI] [PubMed] [Google Scholar]
- Yuan X, Liu T, Wu L, Zou ZY, Li C, 2015. Validity of self-reported diabetes among middle-aged and older Chinese adults: the China Health and Retirement Longitudinal Study. BMJ Open 5, e006633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y, Hu Y, Smith JP, Strauss J, Yang G, 2014. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol 43, 61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


