Abstract
Post Traumatic Stress Disorder (PTSD) is a condition which causes great sufferance to the individuals affected. The occurrence of comorbidities in PTSD is a frequent event with a negative impact on outcome. This study investigated the frequency of PTSD in relation to comorbidities by analyzing the results of the 2007 ‘Adult Psychiatric Morbidity Survey’ in the English population, which included data on comorbidities. A population study conducted in the United Kingdom, this survey investigated the frequency of PTSD in the community and the relationship to comorbidities by adopting a random design to minimize selection bias, stratified by region and socioeconomic characteristics, and weighted according to design and non-response. The survey interviewed 7403 adults living in private households. Socio-demographic characteristics and psychiatric morbidity were systematically assessed. Results indicated that PTSD prevalence was 2.9%, with an excess in women (3.3%) compared to men (2.4%) as reported by the 2007 survey. Comorbidity was a very frequent occurrence in PTSD reaching 78.5% in affected cases. Major depression was the commonest condition and its frequency increased with symptoms severity up to 54%. Among anxiety disorders, social phobia was the most frequent, followed by generalized anxiety disorder, obsessive-compulsive disorder, agoraphobia and panic disorder. Substance use disorders were also common. The presence of psychotic symptoms was particularly significant with over 30% prevalence in PTSD. These results indicate that attention needs to be devoted to the presence of comorbidities. In view of the impact of comorbidities on PTSD severity, chronicity and functional impairment, early detection and treatment are likely to improve outcome.
Electronic supplementary material
The online version of this article (10.1007/s11126-020-09797-4) contains supplementary material, which is available to authorized users.
Keywords: Psychiatry, Post traumatic stress disorder, Comorbidities, Major depressive disorders, Survey
Introduction
The co-occurrence of psychiatric morbidity is significant in PTSD [1–5] with concerning estimates for major depression reaching 48% of PTSD cases [6], often coexisting with suicidal ideation [7], the frequent presence of symptoms of generalized anxiety disorder [8] and of alcohol dependence with increased levels of aggression and impulsivity [6, 9–12]. The association between PTSD and psychosis is also recognized as contributing to the burden and quality of life of patients with schizophrenia [13] and in some studies is related to negative symptoms [14]. Despite evidence of a significant negative interaction between comorbidities and the outcome of PTSD [15], there is limited information available in the literature from sufficiently powered studies to appraise the frequencies of comorbidities at population level [16] particularly from European samples. This is relevant because differences in PTSD prevalence shown globally [1, 16] might also reflect on comorbidities [17]. More accurate information, based on data from local samples, is essential for devising more precise care models and tailored services for more complex forms of PTSD [18]. This work reports PTSD comorbidity data from the 2007 ‘Adult Psychiatric Morbidity Survey’ in the English population and provides a detailed description of the concomitant psychopathology when PTSD criteria are met.
Methods
Patient Population
Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement guidelines for reporting observational studies were followed [19]. This study presents data from the 2007 adult psychiatric morbidity survey [20] which included individuals aged 16–64 living in the UK. The survey interviewed 7403 individuals, a sample size sufficient to detect less common psychiatric disorders (0.5–1.0%) by taking into account age, sex and UK region [20].
Assessment and Data Collection
Adults living in private households were sampled using a population-based multi-phase probability sampling (Small User Postcode Address File approach). Well trained survey interviewers identified private households after one person in the household had been selected at random to minimize selection bias (Kish grid method) [21]. Furthermore, the sample was stratified by region and socioeconomic characteristics and weighted for survey design and non-response [22]. Ethnic categories were classified as ‘white’ which included all white participants independent of their country of origin, ‘black’ comprising Caribbean, black African, black other, and mixed white/black, and a residual ‘Other’ group. Social class was classified according to the UK Registrar General’s classification, and divided into three groups: social classes I and II, social class III, and social classes IV and V (this last group also included members of the armed forces).
During phase 1 of the survey, socio-demographic characteristics were collected and suitability for phase 2 was established with a detailed questionnaire. In phase 2 interviews were carried out by clinically trained researchers. The Revised Clinical Interview Schedule (CIS-R) [23] was used to establish the presentation of prevalent current mental disorders. A diagnostic algorithm was utilized to establish ICD-10 diagnoses including depressive episodes, generalized anxiety disorder, mixed anxiety and depressive disorder, panic disorder, phobias and obsessive–compulsive disorder [21]. The possible presence of psychotic symptoms was assessed during phase 1 by using the Psychosis Screening Questionnaire (PSQ) [24] and subsequently confirmed at phase 2 in a formal assessment based on set criteria (see Supplementary material). The experience of a traumatic events was systematically assessed with the non-patient version of the Structured Clinical Interview for DSM-IV (SCID) [25]. If any event occurred from the age of 16 onwards, PTSD experiences were explored by using the Trauma Screening Questionnaire (TSQ) [26]. The TSQ is a valid instrument to screen for PTSD symptoms in primary care according to the National Institute of Clinical Excellence aligned with DSM IV criteria [21] with a sensitivity of 84%, a specificity of 95% and a positive predictive value for PTSD vs. other forms of trauma of 90% [21, 26]. The Alcohol Use Disorders Identification Test (AUDIT) [27], the community version of the Severity of Alcohol Dependence Questionnaire (SADQ-C) [28] and the Comprehensive Addiction Severity, based on the Diagnostic Interview Schedule [29] were used to assess and identify alcohol misuse over the preceding 6 months and drug use over the past year.
Statistical Analysis
Data from each survey were weighted to allow for design and response rates [21, 30, 31] and analyzed using the Data Analysis & Statistical Software (STATA 15; StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC.). Binary logistic regression analyses were used to calculate the odds ratios (ORs) and 95% confidence intervals (CIs).
Patient and Public Involvement
Patients or public were not involved in the design of this study.
Compliance with Ethical Standards
The Royal Free Medical School Research Ethics Committee (London, UK) granted Ethical approval for the Adult Psychiatric Morbidity Survey 2007 (Ref.: 06/Q0501/71).
Results
Characteristics of the Sample and Prevalence of PTSD
Overall 7325 participants were eligible, 3163 men (43.2%) and 4162 women (56.8%). Two hundred and thirteen individuals (2.9%), 75 men (2.4%) and 138 women (3.3%) met the criteria for a probable PTSD diagnosis (mean age 42.9 years, SD = 15.0). White middle class participants were more represented in the groups (see Table 1 for details).
Table 1.
Characteristics of the sample
| Probable PTSD | ||
|---|---|---|
| Not Present (n = 7112) | Present (n = 213) | |
| Males % | 97.4% | 2.6% |
| Females % | 96.8% | 3.2% |
| Age, mean (SD) | 51.3 (18.5) | 42.9 (15.0) |
| Upper class N (%) | 2570 | 64 (2.2) |
| Middle class N (%) | 3724 | 124 (3.1) |
| Lower class N (%) | 354 | 6 (2.0) |
| White N (%) | 6575 | 191 (2.8) |
| Black N (%) | 180 | 8 (6.1) |
| Other ethnicities N (%) | 337 | 12 (2.2) |
Co-Morbid Psychiatric Diagnoses
The co-existence of comorbid psychiatric diagnoses in the individuals with probable PTSD was 78.5% compared to 14.5% in those who did meet PTSD criteria. Table 2 and Fig. 1 show the distribution and frequency of comorbid conditions. The odds ratio indicated a significant association with most conditions except for specific isolated phobias. Depressive disorders were the most represented with increasing severity (16.2%–53.6%), followed by social phobia (36.3%), psychotic symptoms (30.4%), obsessive-compulsive disorder (27.7%), agoraphobia/panic disorders (17.9%), generalized anxiety disorder (9.8%), alcohol misuse and dependency (9.5%), and use of substances (12.6%).
Table 2.
Psychiatric diagnoses predicting the occurrence of probable Post Traumatic Stress Disorder (PTSD); OR = Odds Ratio
| Other psychiatric comorbidities | Probable PTSD | Odds Ratio | z | P value | Confidence Interval | |
|---|---|---|---|---|---|---|
| Not Present (N = 7112) % |
Present (N = 213) % |
|||||
|
No other mental disorder N = 6066 |
99.3 | 0.7 | ||||
|
Mixed Anxiety and Depression N = 665 |
91 | 9 | 13.3 | 11.0 | <0.001 | 8.4–21.1 |
|
Mild depression N = 55 |
83.8 | 16.2 | 25.9 | 7.1 | <0.001 | 10.6–63.8 |
|
Moderate depression N = 122 |
70.1 | 29.9 | 57.2 | 14.0 | <0.001 | 32.5–100.6 |
|
Severe depression N = 7 |
46.4 | 53.6 | 155.4 | 6.0 | <0.001 | 30.0–804.2 |
|
Agoraphobia/Panic disorder N = 84 |
82.1 | 17.9 | 29.3 | 11.0 | <0.001 | 14.0–61.1 |
|
Obsessive Compulsive Disorder N = 34 |
72.3 | 27.7 | 51.5 | 7.8 | <0.001 | 19.1–138.9 |
|
Social phobia N = 37 |
63.7 | 36.3 | 76.6 | 10.11 | <0.001 | 33.1–177.8 |
| Generalized Anxiety Disorder N = 205 | 90.2 | 9.8 | 14.6 | 8.6 | <0.001 | 7.9–27.0 |
|
Specific Isolated Phobias N = 13 |
100 | 0.0 | 1.0 | NA | NA | NA |
|
Psychosis N = 37 |
69.6 | 30.4 | 58.7 | 9.7 | <0.001 | 25.8–133.7 |
|
Alcohol misuse/dependence N = 20 |
90.5 | 9.5 | 4.1 | 6.6 | <0.001 | 2.7–6.4 |
|
Substance use disorders N = 27 |
87.4 | 12.6 | 5.5 | 6.5 | <0.001 | 3.3–9.3 |
Fig. 1.
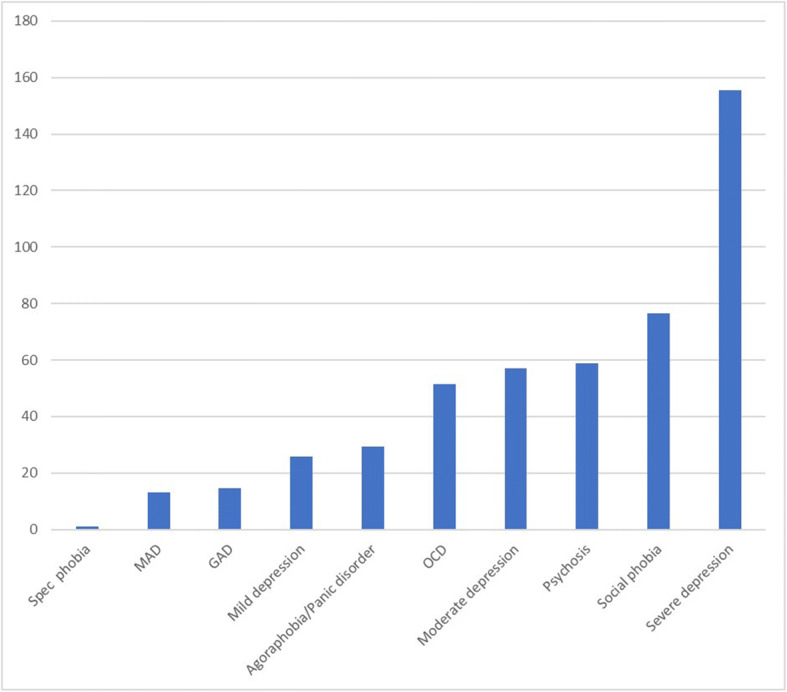
Strength of association between PTSD diagnosis and other comorbidities as indicated by their odds ratio (OR)
Discussion
We set out to investigate the frequencies of PTSD and explore its comorbidities. As reported by the 2007 ‘Adult Psychiatric Morbidity Survey’ in the English population the prevalence of PTSD equaled 2.9%, with an excess in women (3.3%) compared to men (2.4%). White middle class participants were more represented in the groups. In agreement with previous research, we found that comorbidity is a very frequent occurrence in PTSD reaching 78.5% in this survey. Major depression was the commonest condition and its frequency raised with increasing severity, up to 54% in case of severe symptoms. We also found that among anxiety disorders, social phobia had the highest comorbidity with PTSD compared to generalized anxiety disorder, obsessive-compulsive disorder, agoraphobia and panic disorder. We also found significant levels of substance use disorders. The presence of psychotic symptoms was particularly significant with over 30% prevalence in PTSD. This is of interest given the small number of large surveys, which systematically assessed the presence of psychotic symptoms in individuals with PTSD. It is possible that this finding is related to the design of this study powered to detect less common psychopathology combined with the psychometric tools used.
It is not possible for this work to explain the high rate of comorbidities and provide potential etiological explanations. It is plausible that depressive disorders as well as anxiety symptoms can be a consequence of PTSD as well as an independent risk factor for PTSD following trauma exposure. Both conditions could also be a vulnerability factor for developing PTSD once exposure to traumatic events occurs. The relationship between PTSD and the use of alcohol and substances could be understood as a coping strategy to attenuate disturbing PTSD symptoms according to the self-medication hypothesis [32]. Regarding psychotic symptoms, there is a complex relationship with PTSD. Firstly, some of the psychotic symptoms can occur in case of severe PTSD. For example, thoughts which could be described as persecutory, the occurrence of abnormal multimodal perceptions [33] and the phenomenon of depersonalization/derealisation have been described in PTSD [34, 35]. This has led to conceiving a subtype of PTSD with psychotic symptoms as a way of explaining psychopathology. Other explanations are however possible, including that trauma could trigger PTSD as well schizophrenia and there is evidence that PTSD could be a prodromal manifestation of Schizophrenia [35, 36]. It is not to underestimate though that psychotic symptoms could be related to misusing substances, and associated with intoxication, be the result of withdrawal symptoms or complications related to chronic use (e.g. alcohol hallucinosis) [32].
It is essential to reflect on the possible overlap of the diagnostic criteria between PTSD and other mental disorders. The significantly high rates of comorbidity detected may be a reflection of the limitations of the diagnostic criteria used [32]. This is particularly relevant when it is not possible to establish a temporal relationship with the onset of the symptoms. Kessler and colleagues in their landmark survey also reported high rates of comorbidities in their study and similarly to this study, could not establish the primacy of PTSD [16]. It is possible that the high degree of symptoms overlap across syndromes contributes to under diagnose PTSD, particularly when detailed histories of traumatic events are not fully elicited. It is therefore important in routine clinical practice to specifically ascertain or exclude the presence and significance of traumatic events to avoid underestimating or overestimating PTSD in relation to other disorders. It may increase discriminative power to focus on the more distinctive symptoms of PTSD, particularly those not overlapping with other psychiatric conditions e.g. history of trauma, the presence of flashback and the individual response to traumatic events [16]. Algorithms that implement numerical weights for counting repeated items in assessment inventories could help reduce diagnostic overlap [37]. Another way might be to amend the diagnostic overlap by re-examining the constructs that define PTSD [38]. Rosen and Lilienfeld focused on the absence of valid empirical support for diagnostic criteria for the disorder [37]. This observation would be consistent with some studies that have referred to the fact that the onset of the classic form of trauma as a main diagnostic component is neither sufficient nor necessary for the onset of PTSD [39, 40]. Furthermore, some of the current literature alludes to the diagnostic boundaries of PTSD not being as specific as it is purported to be [38, 39, 41]. For example, many non-traumatic stressors (e.g. divorce of one’s parents, relationship problems) could lead to a higher number of PTSD symptoms when compared to the typical trauma described by diagnostic manuals, although extending the diagnostic boundaries of PTSD by lowering the threshold for the definition of trauma may not result in better precision [40, 42].
Limitations
Large surveys such as this one offer the great opportunity to appraise conditions such as PTSD at population level by estimating disease prevalence over a time period. The main limitation of this approach is that cross sectional data do not allow for a prognostic evaluation and cannot establish primacy. This information can only be obtained from longitudinal data. Nevertheless, it is known that meeting criteria for more than one psychiatric disorder increases severity, prolongs illness, service utilisation, and negatively affects functionality [3, 43]. In this context, early intervention and recognition of comorbidities is likely to have a significant public health impact to reduce morbidity and improve outcome.
Conclusion
In conclusion, this large population based survey reports a frequency of PTSD around 3% in the English population with an excess in women compared to men. Comorbidity in PTSD is highly prevalent and major depression is the most frequent among the detected mental health conditions. Psychotic symptoms were surprisingly common in PTSD. Exploration of comorbidities warrants further investigation because early recognition might prove beneficial to reduce morbidity, chronicity and loss of function. Addressing comorbid conditions in PTSD might also provide an insight into optimizing diagnostic criteria in view of the diagnostic overlap with some of the frequently occurring syndromes. Furthermore, a better understanding of the role of co-morbidities in PTSD could provide a rationale for subtyping PTSD to optimize treatment outcomes. Some attention could also be devoted to understanding some of the potential moderating factors including those of biological nature e.g. the relationship between immunology and the stress response [44], which might explain the overlap between PTSD and some of the comorbid conditions. Further studies with a longitudinal design assessing the primacy of one disorder over the other could help disentangle temporal associations.
Electronic supplementary material
(DOCX 15.2 kb)
Acknowledgements
TQ would like to thank Paul Bebbington, Nicola Spiers and Sally McManus and the team that designed the National Psychiatric Morbidity Survers for the opportunity to access the data for re-analysis and for their help in data interpretation. All authors would like to thank the participants and interviewers of the Adult Psychiatric Morbidity Surveys.
Biographies
T. Qassem
: Consultant Psychiatrist and Associate Professor of Psychiatry
D. Aly-ElGabry
: Consultant Psychiatrists and Associate Professor of Psychiatry
A. Alzarouni
: MA student
K. Abdel-Aziz
: Consultant Psychiatrist and Assistant Professor of Psychiatry
Danilo Arnone
: Consultant Psychiatrist and Associate Professor of Psychiatry
Authors’ Contributions
TQ analyzed the data and prepared the first draft of the manuscript with the contribution of DAE, AA and KAA. DA contributed to data interpretation and to the final draft of the manuscript. All authors approved the submission.
Funding Information
The Adult National Psychiatric Morbidity surveys were funded by the Department of Health, England, to the University of Leicester (1993–2007) and to the Office for National Statistics (1993–2000) and NatCen Social Research (2007), and via the Health and Social Care. Information Centre, Leeds (2007). This paper was made Open Access by support from King’s College London.
Compliance with Ethical Standards
Declaration of Interest
DA has received travel grants from Jansen-Cilag and Servier and sponsorship from Lundbeck.
Data Statement
Data can be requested by contacting the authors.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Koenen KC, Ratanatharathorn A. Ng L3, et al. posttraumatic stress disorder in the world mental health surveys. Psychol Med. 2017;47(13):2260–2274. doi: 10.1017/S0033291717000708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arkowitz H, Lilienfeld, SO. Chichester, West Sussex, UK, 2017: Wiley Blackwell.
- 3.Alonso J, Angermeyer MC, Bernert S, et al. 12-month comorbidity patterns and associated factors in Europe: results from the European study of the epidemiology of mental disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004;420:28–37. doi: 10.1111/j.1600-0047.2004.00328.x. [DOI] [PubMed] [Google Scholar]
- 4.Diagnostic and statistical manual of mental disorders. American Psychiatric Association (2013). (5th ed.). Arlington, VA: American Psychiatric Publishing.
- 5.Galatzer-Levy IR, Nickerson A, Litz BT, Marmar CR. Patterns of lifetime PTSD comorbidity: a latent class analysis. Depress Anxiety. 2013;30:489–496. doi: 10.1002/da.22048. [DOI] [PubMed] [Google Scholar]
- 6.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cougle JR, Resnick H, Kilpatrick DG. PTSD, depression, and their comorbidity in relation to suicidality: cross-sectional and prospective analyses of a national probability sample of women. Depress Anxiety. 2009;26(12):1151–1157. doi: 10.1002/da.20621. [DOI] [PubMed] [Google Scholar]
- 8.Price M, van Stolk-Cooke K. Examination of the interrelations between the factors of PTSD, major depression, and generalized anxiety disorder in a heterogeneous trauma-exposed sample using DSM 5 criteria. J Affect Disord. 2015;186:149–155. doi: 10.1016/j.jad.2015.06.012. [DOI] [PubMed] [Google Scholar]
- 9.Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from wave 2 of the National Epidemiologic Survey on alcohol and related conditions. J Anxiety Disord. 2011;25(3):456–465. doi: 10.1016/j.janxdis.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Felson RB, Staff J. The effects of alcohol intoxication on violent versus other offending. Crim Justice Behav. 2010;37(12):1343–1360. doi: 10.1177/0093854810382003. [DOI] [Google Scholar]
- 11.Modesto-Lowe V, Brooks D, Ghani M. Alcohol dependence and suicidal behavior: from research to clinical challenges. Harv Rev Psychiatry. 2006;14(5):241–248. doi: 10.1080/10673220600975089. [DOI] [PubMed] [Google Scholar]
- 12.Tull MT, Jakupcak M, Paulson A, Gratz KL. The role of emotional inexpressivity and experiential avoidance in the relationship between posttraumatic stress disorder symptom severity and aggressive behavior among men exposed to interpersonal violence. Anxiety Stress Coping. 2007;20(4):337–351. doi: 10.1080/10615800701379249. [DOI] [PubMed] [Google Scholar]
- 13.Braga RJ, Mendlowicz MV, Marrocos RP, Figueira IL. Anxiety disorders in outpatients with schizophrenia: prevalence and impact on the subjective quality of life. J Psychiatr Res. 2005;39(4):409–414. doi: 10.1016/j.jpsychires.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 14.Strauss GP, Duke LA, Ross SA, Allen DN. Posttraumatic stress disorder and negative symptoms of schizophrenia. Schizophr Bull. 2009;37(3):603–610. doi: 10.1093/schbul/sbp122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Green BL, Krupnick JL, Chung J, Siddique J, Krause ED, Revicki D, et al. Miranda. Impact of PTSD comorbidity on one-year outcomes in a depression trial. J Clin Psychol. 2006;62(7):815–35. [DOI] [PubMed]
- 16.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 17.Burri A, Maercker A. Differences in prevalence rates of PTSD in various European countries explained by war exposure, other trauma and cultural value orientation. BMC Res Notes. 2014;7:407. doi: 10.1186/1756-0500-7-407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rojas SM, Bujarski S, Babson KA, Dutton CE, Feldner MT. Understanding PTSD comorbidity and suicidal behavior: associations among histories of alcohol dependence, major depressive disorder, and suicidal ideation and attempts. J Anxiety Disord. 2014;28(3):318–325. doi: 10.1016/j.janxdis.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 19.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–808. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McManus S, Meltzer H, Brugha T, et al. Adult psychiatric morbidity in England, 2007: Results of a household survey, 2009 10.13140/2.1.1563.5205
- 21.Kish L. Survey sampling. New York: Wiley; 1965. [Google Scholar]
- 22.Lewis G, Pelosi AJ, Araya R, Dunn G. Measuring psychiatric disorder in the community: a standardized assessment for use by lay interviewers. Psychol Med. 1992;22(2):465–486. doi: 10.1017/s0033291700030415. [DOI] [PubMed] [Google Scholar]
- 23.Bebbington, P., & Nayani, T. Psychosis screening questionnaire . PsycTESTS Dataset. American Psychological Association (APA), 1995. 10.1037/t30040-000.
- 24.First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition. (SCID-I/NP) New York: Biometrics Research, 2002 New York State Psychiatric Institute.
- 25.Brewin CR, Rose S, Andrews B, Green J, Tata P, McEvedy C, et al. Brief screening instrument for post-traumatic stress disorder. Br J Psychiatry. 2002;181(2):158–62. [DOI] [PubMed]
- 26.Saunders JB, Aasland OG, Babor TF, et al. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 27.Stockwell T, Sitharthan T, McGrath D, et al. The measurement of alcohol dependence and impaired control in community samples. Addiction. 1994;89(2):167–184. doi: 10.1111/j.1360-0443.1994.tb00875.x. [DOI] [PubMed] [Google Scholar]
- 28.Malgady RG, Rogler LH, Tryon WW. Issues of validity in the diagnostic interview schedule. J Psychiatr Res. 1992;26(1):59–67. doi: 10.1016/0022-3956(92)90016-H. [DOI] [PubMed] [Google Scholar]
- 29.Meltzer H, Gill B, Petticrew M. OPCS Surveys of Psychiatric Morbidity in Great Britain, Bulletin No.1: The prevalence of psychiatric morbidity among adults aged 16–64, living in private households, in Great Britain, 1994 OPCS: London.
- 30.Singleton N, Bumpstead R, O'Brien M, Lee A, Meltzer H. Psychiatric morbidity among adults living in private households. Int Rev Psychiatry. 2003;15(1–2):65–73. doi: 10.1080/0954026021000045967. [DOI] [PubMed] [Google Scholar]
- 31.Brady KT, Killeen TK, Brewerton T, Lucerini S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J Clin Psychiatry. 2000;61(Suppl 7):22–32. [PubMed] [Google Scholar]
- 32.Braakman MH, Kortmann FA, van den Brink W. Validity of ‘posttraumatic stress disorder with secondary psychotic features’: a review of the evidence. Acta Psychiatr Scand. 2009;119:15–24. doi: 10.1111/j.1600-0447.2008.01252.x. [DOI] [PubMed] [Google Scholar]
- 33.Blevins CA, Weathers FW, Witte TK. Dissociation and posttraumatic stress disorder: a latent profile analysis. J Trauma Stress. 2014;27:388–396. doi: 10.1002/jts.21933. [DOI] [PubMed] [Google Scholar]
- 34.OConghaile A, DeLisi LE. Distinguishing schizophrenia from posttraumatic stress disorder with psychosis. Curr Opin Psychiatry. 2015;28(3):249–255. doi: 10.1097/YCO.0000000000000158. [DOI] [PubMed] [Google Scholar]
- 35.Gaudiano BA, Zimmerman M. Evaluation of evidence for the psychotic subtyping of posttraumatic stress disorder. Br J Psychiatry. 2010;197:326–327. doi: 10.1192/bjp.bp.110.078824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosen GM, Lilienfeld SO. Posttraumatic stress disorder: an empirical evaluation of core assumptions. Clin Psychol Rev. 2008;28(5):837–868. doi: 10.1016/j.cpr.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 37.Bonanno GA, Westphal M, Mancini AD. Resilience to loss and potential trauma. Annu Rev Clin Psychol. 2011;7(1):511–535. doi: 10.1146/annurev-clinpsy-032210-104526. [DOI] [PubMed] [Google Scholar]
- 38.Gold SD, Marx BP, Soler-Baillo JM, Sloan DM. Is life stress more traumatic than traumatic stress? J Anxiety Disord. 2005;19(6):687–698. doi: 10.1016/j.janxdis.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 39.Andrews G, Slade T, Issakidis C. Deconstructing current comorbidity: data from the Australian National Survey of mental health and well-being. Br J Psychiatry. 2002;181:306–314. doi: 10.1192/bjp.181.4.306. [DOI] [PubMed] [Google Scholar]
- 40.Rosen GM. Posttraumatic stress disorder: issues and controversies. Chichester, West Sussex, England, 2005: J. Wiley.
- 41.Henderson S, Andrews G, Hall W. Australia's mental health: an overview of the general population survey. Aust N Z J Psychiatry. 2000;34(2):197–205. doi: 10.1080/j.1440-1614.2000.00686.x. [DOI] [PubMed] [Google Scholar]
- 42.Karam EG, Andrews G, Bromet E, Petukhova M, Ruscio AM, Salamoun M, et al. The role of criterion A2 in the DSM-IV diagnosis of posttraumatic stress disorder. Biol Psychiatry. 2010;68(5):465–73. 10.1016/j.biopsych.2010.04.032. [DOI] [PMC free article] [PubMed]
- 43.Sareen J. Posttraumatic stress disorder in adults: impact, comorbidity, risk factors, and treatment. Can J Psychiatr. 2014;59(9):460–467. doi: 10.1177/070674371405900902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Michopoulos V, Powers A, Gillespie CF, Ressler KJ, Jovanovic T. Inflammation in fear and anxiety-based disorders: PTSD, GAD, and beyond. Neuropsychopharmacology. 2016;42(1):254–270. doi: 10.1038/npp.2016.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 15.2 kb)


