Abstract
Simulated hypobaric hypoxia (SHH) training has been used to enhance running performance. However, no studies have evaluated the effects of a single SHH exposure on healthy mice performance and analyzed the changes of mitochondria-related genes in the central nervous system. The current study used a mouse decompression chamber to simulate mild hypobaric hypoxia at the high altitude of 5000 m or severe hypobaric hypoxia at 8000 m for 16 h (SHH5000 & SHH8000, respectively). Then, the mouse behavioral tests were recorded by a modified Noldus video tracking. Third, the effects of SHH on 8 mitochondria-related genes of Drp1, Mfn1, Mfn2, Opa1, TFAM, SGK1, UCP2 and UCP4, were assessed in cerebellum, hippocampus and gastrocnemius muscles. The results have shown that a single mild or severe HH improves healthy mice performance. In cerebellum, 6 of all 8 detected genes (except Mfn2 and UCP4) did not change after SHH. In hippocampus, all detected genes did not change after SHH. In muscles, 7 of all 8 detected genes (except Opa1) did not change after SHH. The present study has indicated the benefit of a single SHH in healthy mice performance, which would due to the stabilized mitochondria against a mild stress state.
Subject terms: Neuroscience, Medical research
Introduction
Hypoxia is defined as oxygen deprivation at the tissue level1. High altitude causes hypoxia due to decreased inspired oxygen pressure, which is called hypobaric hypoxia (HH)2. This atmospheric pressure is composed of the partial pressures of the constituent gases, oxygen, nitrogen, and water vapor (6.3 kPa at 37 ℃). As oxygen accounts for 21% of the dry air, the formula of inspired oxygen pressure is 0.21 '(100 − 6.3) = 19.6 kPa at sea level3. Atmospheric pressure and inspired oxygen pressure decrease linearly with altitude. The inspired oxygen pressure at 5000 m or at 8000 m decreases to be 56.2% or 38.3% of the sea level value, respectively3. Hence at 5000 m or 8000 m above sea level, the inspired oxygen pressure decreases to 19.6 × 0.562 = 11.01 kPa or 19.6 × 0.383 = 7.51 kPa, respectively.
Many previous results have indicated that HH could induce neurological damages, including high-altitude headache, acute mountain sickness, and high-altitude cerebral edema4. HH could result in impairment in arithmetic5 memory and metamemory language6, perception, learning, cognitive flexibility, and psychomotor skills7. On the contrary, HH training has been used by endurance athletes in the pursuit of performance enhancement after returning to sea level. Short-term “live high” training will increase O2 transport and delay hypoxic ventilatory responses, enhancing the 3000/5000 m run-time trial time8. The use of HH or simulated hypobaric hypoxia (SHH) has become increasingly popular sincerity was discussed in the first international symposium on altitude training and team sports held in 20139. The beneficial effects of HH or SHH on athletes have focused on skeletal tissues and the cardiac system, such as hypobaric hypoxic exercise superimposed on hypoxic residence, which could boost the skeletal muscle mitochondrial transcriptional response in elite port athletes10. However, it should be noted that the neurological physiological responses under HH remain debated.
A fall in inspired oxygen pressure reduces the driving pressure for gas exchange in the lungs and in turn produces a cascade of effects right down to the level of the mitochondria, the final destination of the oxygen11. In the central nervous system, mitochondria are involved in neuronal impairment induced by HH. It has been shown that dihydromyricetin improved mitochondrial function and reduced oxidative stress under HH12. Mironova GD et al. found that cortical mitochondria responded to HHconditions with typical and progressive changes in the structure and function of mitochondrial enzymes13. Therefore, the capability of mitochondrial stress is closely related to HH-induced stress.
The mitochondria-directed interventions affecting brain susceptibility to injury including mitochondrial dynamics, mitochondrial biogenesis, mitophagy, and morphogenesis. The mitochondrial fusion–fission cycle is important for the maintenance of organelle function. The process of mitochondrial fission is driven by dynamin-related protein 1 (Drp1), a cytosolic protein that upon activation translocates to the outer mitochondrial membrane14. Fusion depends on mitofusin 1 (Mfn1) and mitofusin 2 (Mfn2) in the outer mitochondrial membranes15. Optic atrophy 1 (Opa1) mediates mitochondrial inner membrane fusion16. Mitochondrial biogenesis is a highly regulated process, and mitochondrial transcription factor A (TFAM) is needed17. Mitophagy is an important mechanism controlling mitochondrial quality, and serum and glucocorticoid-regulated protein kinase 1 (SGK1) induces the autophagic degradation of mitochondria18. Mitochondrial uncoupling proteins (UCPs) are present in neurons, and UCP2 & UCP4can directly influence neurotransmission, synaptic plasticity and neuronal processes by regulating mitochondrial biogenesis, calcium flux, and free radical production19.
In the current study, we first used a mouse decompression chamber to simulate mild hypobaric hypoxia at the high altitude of 5000 m or severe hypobaric hypoxia at 8000 m for 16 h, which are named as SHH5000 & SHH8000 in the present study, respectively. Then, the mouse behavioral tests were recorded by a modified Noldus video tracking. Third, the effects of hypobaric hypoxia on 8 mitochondria-related genes of Drp1, Mfn1, Mfn2, Opa1, TFAM, SGK1, UCP2 and UCP4, were assessed in cerebellum, hippocampus and gastrocnemius muscle. The aim of the present work was to describe the changes in mitochondrial dynamics in the central nervous system of healthy mice caused by exposure to a single hypobaric hypoxia event.
Results
A single SHH improves healthy mice performance detected by a modified Noldus video tracking
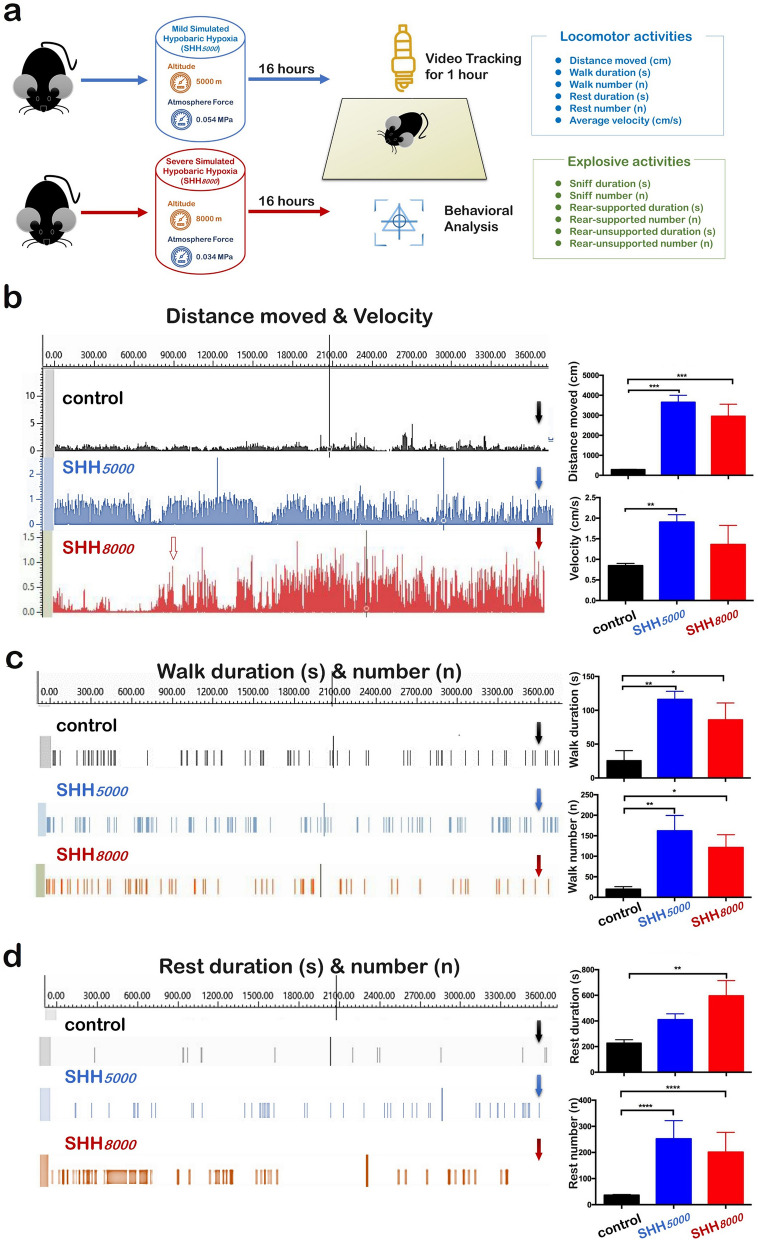
As above mentioned research revealed, the athletes short-term “live high” training will increase in O2 transport and delay hypoxic ventilatory responses, enhancing 30005000 m run-time trial time8. Therefore, we tested whether single 16 h exposure to mild environmental hypoxia (breathing the oxygen with the decreased pressure from 19.6 kPa to 11.01 kPa and equivalent to 5000 m altitude) or the severe environmental hypoxia (breathing the oxygen with the decreased pressure 7.51 kPa and equivalent to 8000 m altitude) could improve behavioral performance on healthy mice. Scheme of 3600 s of video tracking and behavioral analysis was shown in Fig. 1a.
Figure 1.
Locomotor activity and exploratory behavior were improved by a short-term simulated hypobaric hypoxia in healthy mice. (a) Scheme of 3600 s of video tracking and behavioral analysis after 16 h of SHH5000 or SHH8000 treatment, aimed to examine the cerebellum susceptibility to hypoxia. Most locomotor activities [(b) distance moved and velocity; (c) walk duration and walk number; (d) Rest duration and rest number] were significantly increased by SHH5000and SHH8000treatment. Several exploratory behaviors [(e) sniff duration and sniff number; (f) rear-supported duration and sniff number; (g) rear-unsupported duration] were increased by SHH5000 and SHH8000 treatment. The left column in each figure from B to G shows the representative ground truth and generated annotation over time (3600 s) for test video tracking; the solid arrow represents the time point of termination for statistical analysis (3600 s); the hollow arrow represents the time point for changing behavioral activity in the SHH8000 group. The right column in each figure from B to G shows the comparison of the means of behavior activities over the 3600 s for the treated animals (SHH5000 or SHH8000) and their respective control. Each value is expressed as the mean ± standard error of the mean. Multiple comparisons between groups were carried out with Tukey’s post hoc test. *P value < 0.05; **P value < 0.01; ***P value < 0.001, n = 10 per group.
First, we analyzed spontaneous locomotor activities. Laboratory studies showed a total distance moved of 286.5 ± 8.1 cm in normal mice (n = 10), as shown in Fig. 1b. SHH5000 and SHH8000 significantly increased distance traveled to 12.7 times (P = 0.0002) and 10.3 times (P = 0.0008) as much as that of normal mice, respectively. It should be noted that distance moved began to increase only 500 s after SHH8000, indicated by the hollow arrow representing the time point for changing in Fig. 1b. And there was no difference between the increase by SHH5000 and by SHH8000.
In Fig. 1b and supplementary Video 1, laboratory studies showed average velocity of 0.8 ± 0.03 cm/s in normal mice. SHH5000 significantly increased average velocity to 2.4 times as much as that of normal mice (Supplementary Video 2) (P = 0.0099). SHH8000 average velocity of to 1.7 times as much as that of normal mice, but there was no difference between control versus SHH8000.
In Fig. 1c, the video tracking studies showed a total walk duration of 25.4 ± 8.7 s and walk number of 19.7 ± 3.7 in normal mice. SHH5000 and SHH8000 significantly increased walk duration to 4.6 times and 3.4 times, as well as 8.2 times and 6.2 times as much as that of normal mice, respectively.
Next, we analyzed spontaneous rest states. As shown in Fig. 1d and Supplementary Video 1, laboratory studies showed a total rest duration of 226.4 ± 15.9 s in normal mice. SHH5000 increased rest duration to 1.8 times as much as that of normal mice (Supplementary Video 2), but there was no significance between control and SHH5000 (P = 0.0558). Interestingly, SHH8000 significantly increased rest duration to 2.6 times as much as that of normal mice (Supplementary Video 3) (P = 0.0023). It was logical to observe a significant increase of average velocity in SHH5000 group, but no statistical difference between the control and SHH8000 groups in the average velocity.
Then we assessed the exploratory behavior of hypobaric hypoxia at altitude 5000 m or 8000 m using a battery of behavioral tests.
As shown in Fig. 1e and Supplementary Video 1, laboratory studies showed a total sniff duration of 85.7 ± 8.5 s in normal mice. SHH5000 and SHH8000 significantly increased sniff duration to 5.3 times (Supplementary Video 2) and 4.3 times (Supplementary Video 3) as much as that of normal mice (P = 0.0144 and P = 0.0462), respectively.
In Fig. 1f and Supplementary Video 1, laboratory studies showed a total rear supported duration of 18.7 ± 1.8 s and number of 12.0 ± 2.3 in normal mice. Unexpectedly, SHH5000 and SHH8000 significantly increased rear supported duration to 6.0 times (Supplementary Video 2) and 5.2 times (Supplementary Video 3) as much as that of normal mice, respectively. SHH5000 significantly increased rear supported number to 9.3 times as much as that of normal mice. SHH8000 could not significantly increase rear supported number.
Finally, as shown in Fig. 1g, laboratory studies showed a total rear unsupported duration of 35.7 ± 3.5 s and number of 47.0 ± 3.5 in normal mice (Supplementary Video 1). SHH5000 and SHH8000 significantly increased the duration to 5.2 and 3.6 times, and increased the number to 3.2 and 2.7 times, respectively. There was no significant difference between the increase by SHH5000 and SHH8000.
In conclusion, SHH improved mice locomotor under SHH condition. Effects of mild SHH is higher than severe SHH.
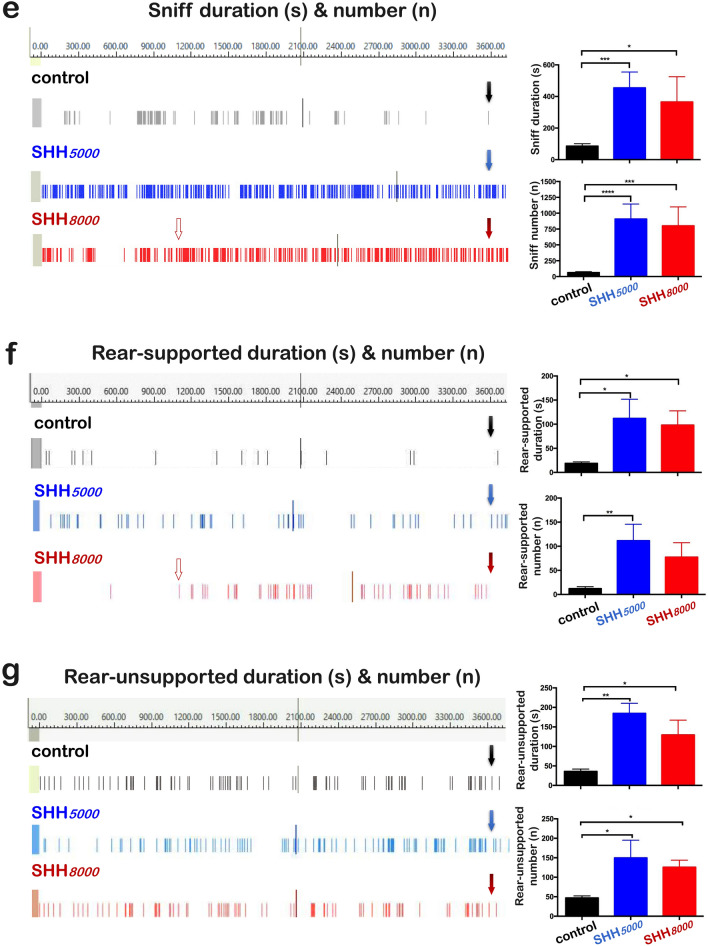
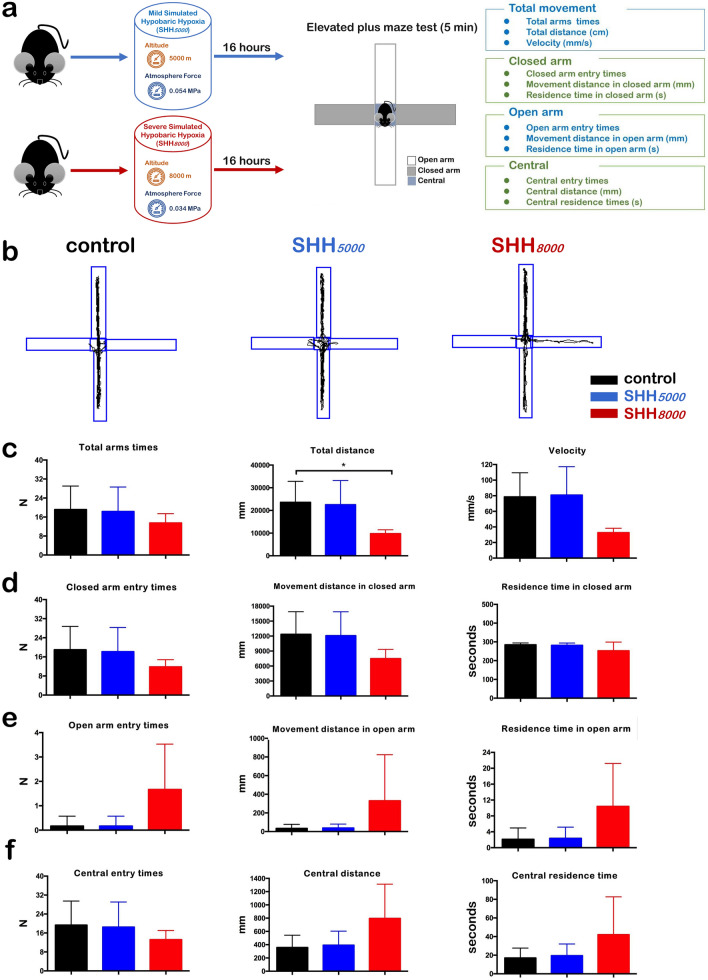
Results of rotarod tests and elevated plus maze (EPM) tests
In order to observe the effects of the SHH on the balance ability of mice, rotarod test was performed (Fig. 2a). As shown in Fig. 2b, both SHH5000 and SHH8000 could not change the two items significantly. Moreover, in the 5 min duration time of rotarod tests, the average velocity in normal mice decreased to be 95.0% in mice of SHH8000 group (P = 0.0022); although SHH5000 could not significantly change the average velocity.
Figure 2.
Mice presented an improved balance ability under SHH conditions. (a) Scheme of the rotarod test after 16 h of SHH5000 or SHH8000 treatment aiming to examine the balance ability of mice. (b) Run time, distance and average speed after SHH5000 and SHH8000 treatment. Each value is expressed as the mean ± standard error of the mean. Multiple comparisons between groups were carried out with Tukey’s post hoc test. *P value < 0.05; **P value < 0.01; ***P value < 0.001, n = 5 per group.
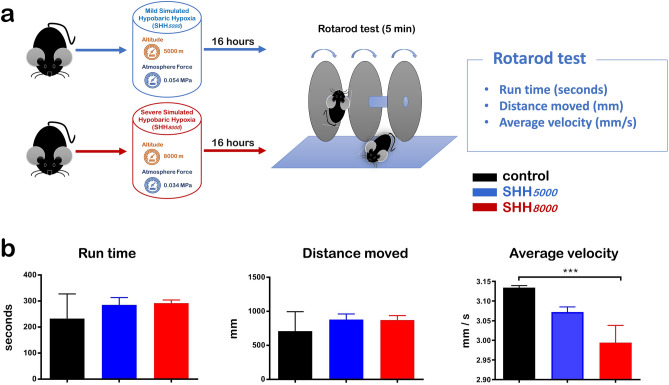
At the same time, the exploratory behaviors of SHH mice were assessed by elevated plus maze (EPM) test (Fig. 3a,b). Compared to control group, all eleven items of mice after SHH5000 treatment or SHH8000 treatment did not show significant difference, including total arms time and velocity in Fig. 3c, three items in closed arm (Fig. 3d), three items in open arm (Fig. 3e), and three items in central area (Fig. 3f). Only the total distance (mm) of normal mice decreased to be 41.5% in mice of SHH8000 group; although SHH5000 could not significantly change it (Fig. 3c).
Figure 3.
Mice presented improved exploratory behaviors under SHH conditions. (a) Scheme of the elevated plus maze test after 16 h of SHH5000 or SHH8000 treatment aiming to examine the exploratory behaviors of mice. (b) Trajectory pattern diagram after SHH5000 or SHH8000 treatment. (c) Total arms times, total distance and speed (from left to right). (d) Closed arm entry times, movement distance in the closed arm and residence time in the closed arm (from left to right). (e) Open arm entry times, movement distance in the open arm and residence time in the open arm (from left to right). (f) Central entry times, central distance and central residence time (from left to right). Each value is expressed as the mean ± standard error of the mean. Multiple comparisons between groups were carried out with Tukey’s post hoc test. *P value < 0.05; **P value < 0.01; ***P value < 0.001, n = 5 per group.
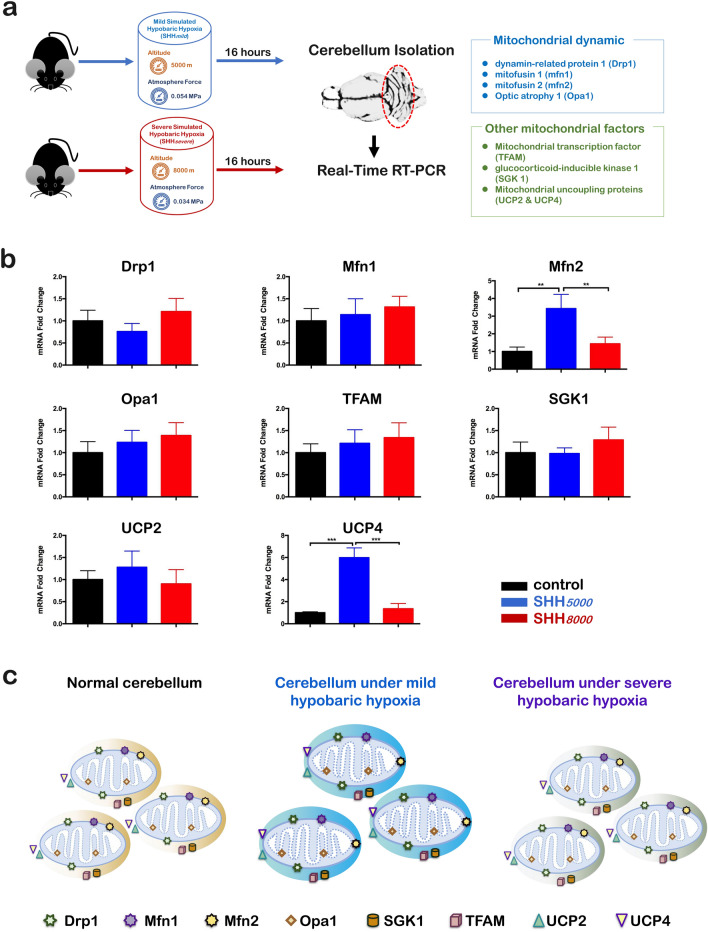
In cerebellum, 6 of all 8 detected mitochondria-related genes did not change after a single SHH
We further investigated whether hypoxia-treated mice showed any changes in multiple mitochondrial genes, including Drp1, Mfn1, Mfn2, Opa1, TFAM, SGK1, UCP2 and UCP4 in cerebellum by qRT-PCRs (Fig. 4a). It was shown that SHH5000 increased significantly the levels of two genes, Mfn2 (P = 0.0124) and UCP4 (P < 0.0001), but did not change the mRNA levels of Drp1, Mfn1, Opa1, TFAM, SGK1, and UCP2 (Fig. 4b). Therefore, only the levels of Mfn2 and UCP4 were significantly increased in cerebellum under SHH5000, whereas the levels of other genes in either SHH5000 or SHH8000 were detected no changes (Fig. 4c).
Figure 4.
In the cerebellum of mice with simulated hypobaric hypoxia treatment, only the levels of Mfn2 and UCP4 were statistically increased by SHH5000, whereas all other genes were almost the same as those in the normal control group. (a) Normal mice were sacrificed at SHH5000 or SHH8000 for 16 h. The mice were sacrificed and the cerebellum was collected, immediately stored in liquid nitrogen. Real-time quantitative PCR was then performed to detect mitochondrial-related molecules (Drp1, Mfn1, Mfn2, Opa1, TFAM, SGK1, UCP2, UCP4) mRNA expression levels differences. (b) Simulated hypobaric hypoxia induced mitochondrial dynamic altering in cerebellum of mice. qRT-PCR analyses of Drp1, Mfn1, Mfn2, Opa1, TFAM, SGK1, UCP2, UCP4 in cerebellum of mice. In the cerebellum of mice with SHH treatment, only the levels of Mfn2 and UCP4 were statistically increased by SHH5000, whereas all other genes, including DRP1, other mfn1 and Opa1, TFAM, SGK1 and UCP2 were almost the same as those in the normal control group. Data are presented as mean SD. *P < 0.05, **P < 0.01, ***P < 0.001, compared with the control group. n = 5 per group. (c) Schematic depiction of the mitochondrial dynamics within the cerebellum of mice in different conditions including normal control, exposed at SHH5000 and SHH8000, respectively. It can be found the mRNAs levels of six mitochondria-related genes including Drp1, Mfn1, Opa1, SGK1, TFAM and UCP2 remained stable except that the mRNAs levels of Mfn2 and UCP4 increased significantly only at SHH5000. Drp1, dynamin-related protein 1, mitochondrial fission factor on the mitochondrial outer membrane; Mfn1, mitochondrial fusion protein 1, mitochondrial fusion factor on the mitochondrial outer membrane; Mfn2, mitochondrial fusion protein 2, mitochondrial fusion factor on the mitochondrial outer membrane; Opa1, Optic atrophy 1, mitochondrial fusion factor on the mitochondrial inner membrane; SGK1, serum and glucocorticoid-regulated protein kinase 1, mitophagy-related factor; TFAM, mitochondrial transcription factor; UCP2, uncoupling protein 2, mitochondrial stress factor; UCP4, uncoupling protein 4, mitochondrial stress factor; SHH5000, simulated hypobaric hypoxia at altitude 5000 m; SHH8000, simulated hypobaric hypoxia at altitude 8000 m.
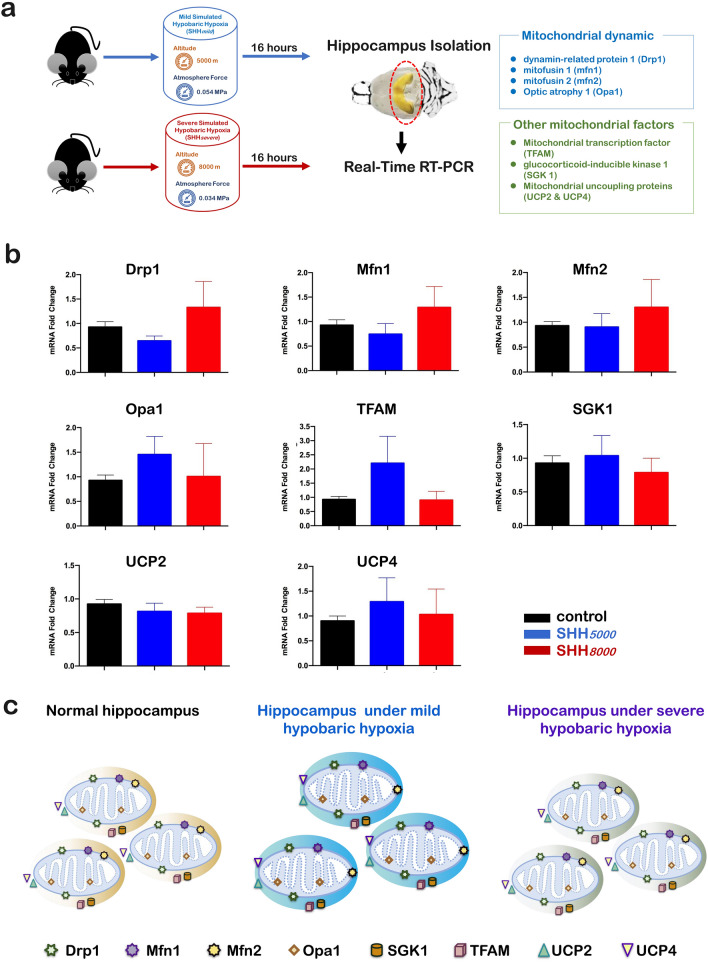
In hippocampus, all 8 detected mitochondria-related genes did not change after a single SHH
Also the changes of mRNAs in 8 mitochondria-related genes in hippocampus were detected by qRT-PCRs (Fig. 5a). As shown in Fig. 5b, it was shown that both SHH5000 and SHH8000 did not increase or decrease the levels of Drp1, Mfn1, Mfn2, Opa1, TFAM, SGK1, UCP2, and UCP4. There was also no significant difference between the increase by SHH5000 and SHH8000. Therefore, all eight detected mitochondria-related genes within the hippocampus maintained stable under both SHH5000 and SHH8000 conditions (Fig. 5c).
Figure 5.
In the hippocampus, no changes in any gene mRNA levels were detected after SHH5000 and SHH8000 treatment. (a) Normal mice were sacrificed after SHH5000 or SHH8000 treatment for 16 h. The mice were sacrificed, and each hippocampus was collected and immediately stored in liquid nitrogen. Real-time quantitative PCR was then performed to detect differences in the mRNA expression levels of mitochondrial-related genes (Drp1, Mfn1, Mfn2, Opa1, TFAM, SGK1, UCP2, UCP4). (b) Simulated hypobaric hypoxia-induced mitochondrial dynamic alterations in the hippocampus of mice. qRT-PCR analyses of Drp1, Mfn1, Mfn2, Opa1, TFAM, SGK1, UCP2, and UCP4 in the hippocampus of mice. In the hippocampus of mice after SHH treatment, no changes in the mRNA levels of any of the genes examined were detected. Data are presented as the mean ± SD. *P < 0.05, **P < 0.01, ***P < 0.001, compared with the control group. n = 5 per group. (c) Schematic depiction of the mitochondrial dynamics within the hippocampus of mice after different treatments, including the normal control and after to SHH5000 and SHH8000 treatment. Drp1, dynamin-related protein 1, a mitochondrial fission factor on the mitochondrial outer membrane; Mfn1, mitochondrial fusion protein 1, a mitochondrial fusion factor on the mitochondrial outer membrane; Mfn2, mitochondrial fusion protein 2, a mitochondrial fusion factor on the mitochondrial outer membrane; Opa1, Optic atrophy1, a mitochondrial fusion factor on the mitochondrial inner membrane; SGK1, serum and glucocorticoid-regulated protein kinase 1, a mitophagy-related factor; TFAM, mitochondrial transcription factor; UCP2, uncoupling protein 2, a mitochondrial stress factor; UCP4, uncoupling protein 4, a mitochondrial stress factor; SHH5000, simulated hypobaric hypoxia at an altitude of 5000 m; SHH8000, simulated hypobaric hypoxia at an altitude of 8000 m.
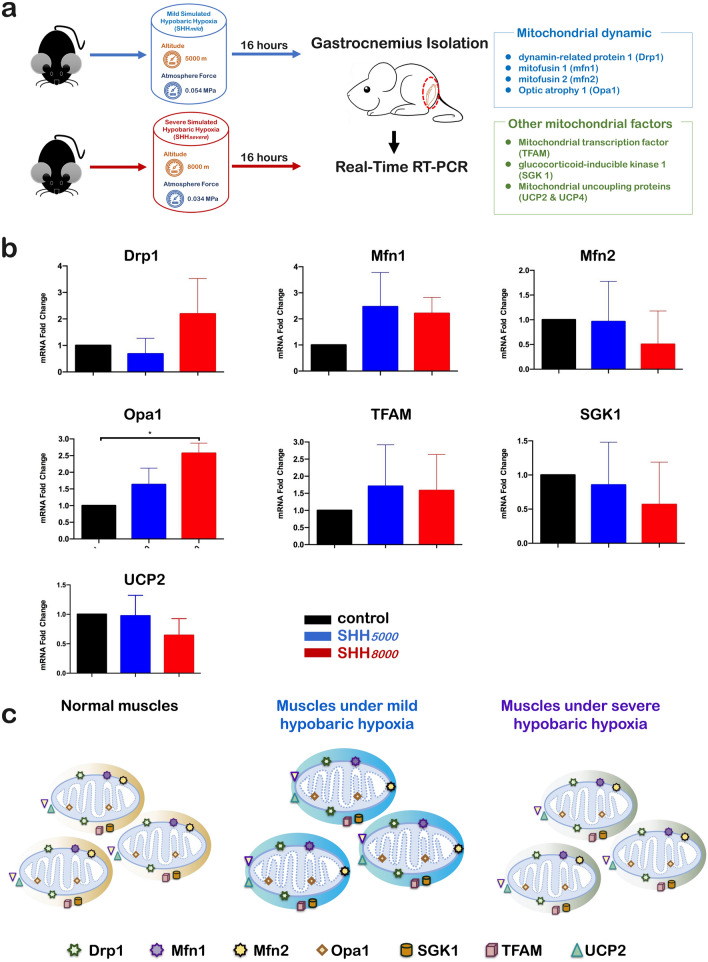
In gastrocnemius muscle, 7 of all 8 detected mitochondria-related genes did not change after a single SHH
In addition, the eight mitochondrial genes in gastrocnemius muscle were detected by qRT-PCRs (Fig. 6a). It should be indicated that UCP4 was a brain-specific mitochondrial protein, which could not be detected in the skeletal muscles. The present qRT-PCR results have confirmed UCP4 mRNAs could not be detected at normal control and SHH conditions. And as shown in Fig. 6b, it was shown that both SHH5000 and SHH8000 did not increase or decrease the levels of Drp1, Mfn1, Mfn2, Opa1, TFAM, SGK1 and UCP2. Therefore, all eight detected mitochondria-related genes within the muscles maintained stable under both SHH5000 and SHH8000 conditions (Fig. 6c).
Figure 6.
Only the levels of Opa1 significantly increased in the muscles after SHH8000 treatment, whereas the levels of the other examined genes in the muscles showed no changes. (a) Normal mice were sacrificed after SHH5000 or SHH8000 treatment for 16 h. The muscles were collected and immediately stored in liquid nitrogen. Real-time quantitative PCR was then performed to detect differences in the mRNA expression levels of mitochondrial-related genes (Drp1, Mfn1, Mfn2, Opa1, TFAM, SGK1, UCP2, and UCP4). (b) Simulated hypobaric hypoxia-induced mitochondrial dynamic alterations in the muscles of mice. qRT-PCR analyses of Drp1, Mfn1, Mfn2, Opa1, TFAM, SGK1, UCP2, and UCP4 in the muscles of mice. In the muscles of mice with SHH treatment, only the level of Opa1 was significantly increased by SHH8000 treatment, whereas the levels of all other genes examined in muscles and all genes examined in the hippocampus showed no changes compared to the control. Data are presented as the mean ± SD. *P < 0.05, **P < 0.01, ***P < 0.001, compared with the control group, n = 5 per group. (c) Schematic depiction of the mitochondrial dynamics within the cerebellum of mice in different conditions including normal control, exposed at SHH5000 and SHH8000, respectively. It can be found the mRNAs levels of six mitochondria-related genes including Drp1, Mfn1, Opa1, SGK1, TFAM and UCP2 remained stable except that the mRNAs levels of Mfn2 and UCP4 increased significantly only at SHH5000. Drp1, dynamic-related protein 1, mitochondrial fission factor on the mitochondrial outer membrane; Mfn1, mitochondrial fusion protein 1, mitochondrial fusion factor on the mitochondrial outer membrane; Mfn2, mitochondrial fusion protein 2, mitochondrial fusion factor on the mitochondrial outer membrane; Opa1, Optic atrophy1, mitochondrial fusion factor on the mitochondrial inner membrane; SGK1, serum and glucocorticoid-regulated protein kinase 1, mitophagy-related factor; TFAM, mitochondrial transcription factor; UCP2, uncoupling protein 2, mitochondrial stress factor; UCP4, uncoupling protein 4, mitochondrial stress factor; SHH5000, simulated hypobaric hypoxia at altitude 5000 m; SHH8000, simulated hypobaric hypoxia at altitude 8000 m.
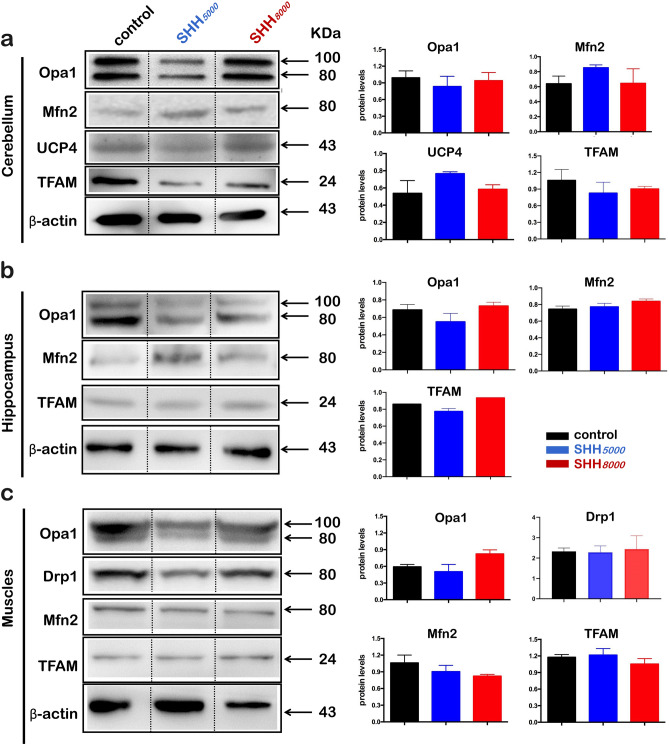
Western blot results
Because we have detected the significant increases of mRNAs of Mfn2 & UCP4 in cerebellum, as well as Opa1 in gastrocnemius muscle, we further performed Western blot to explore the protein expression changes of five mitochondria-related genes, including Drp1, Mfn2, Opa1, TFAM and UCP4, in the cerebellum, hippocampus and gastrocnemius muscle tissues (Fig. 7). Opa1 protein level in muscle tissues under SHH8000 is higher than other group, but with no significant difference (Fig. 7c). All other four protein levels under both SHH5000 and SHH8000 did not change whenever in cerebellum (Fig. 7a), hippocampus (Fig. 7b) and gastrocnemius muscle tissues (Fig. 7c).
Figure 7.
Protein expression levels showed a trend similar to those of the mRNA levels. (a) Normal mice were sacrificed after SHH5000 or SHH8000 treatment for 16 h. Each cerebellum was collected and immediately stored in liquid nitrogen. Western blotting was then performed to detect differences in mitochondrial-related protein expression levels (Mfn2, Opa1, TFAM, UCP4). (b) Western blotting was performed to detect differences in mitochondrial-related protein expression levels (Mfn2, Opa1, TFAM) in each mouse hippocampus after SHH5000 or SHH8000 treatment. (c) Western blotting was performed to detect differences in mitochondrial-related protein expression levels (Mfn2, Opa1, TFAM) in the muscles of mice after SHH5000 or SHH8000 treatment. Data are analyzed by Image J software, and are presented as the mean ± SD. *P < 0.05, **P < 0.01, ***P < 0.001, compared with the control group, n = 5 per group. Full-length blots/gels are presented in Supplementary Fig. 1a–c. Mfn2, mitochondrial fusion protein 2, a mitochondrial fusion factor on the mitochondrial outer membrane; Opa1, Optic atrophy1, a mitochondrial fusion factor on the mitochondrial inner membrane; TFAM, mitochondrial transcription factor; UCP4, uncoupling protein 4, a mitochondrial stress factor; SHH5000,simulated hypobaric hypoxia at an altitude of 5000 m; SHH8000, simulated hypobaric hypoxia at an altitude of 8000 m.
Morphology of cerebellar mitochondria did not change after SHH treatment
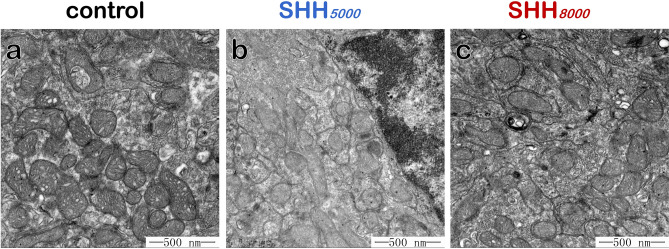
Since the Mfn2, UCP4 were found enhancing after SHH treatment, we further observed mitochondrial structure in cerebellum under TEM after SHH treatment. Results showed that mitochondrial morphology in cerebellum did not significantly change after SHH5000 (Fig. 8b) or SHH8000 (Fig. 8c) treatment, compared with that in normal control group (Fig. 8a).
Figure 8.
Representative transmission electron microscopy (TEM) images of cerebellar mitochondria. The circular, granular and tubular shaped mitochondria were frequently observed in the mice in normal control group (a), SHH5000 group (b), and SHH8000 group (c). Results showed that mitochondrial morphology in cerebellum did not significantly change after SHH treatment. Scale bars, 500 nm.
Discussion
The current study used a mouse decompression chamber to simulate mild hypobaric hypoxia at the high altitude of 5000 m or severe hypobaric hypoxia at 8000 m for 16 h (SHH5000 & SHH8000, respectively). Firstly, it has been shown that a single mild or severe SHH could improve healthy mice performance by using a combination of modified Noldus video tracking system, rotarod test and elevated plus maze (EPM) test. Secondly, the results by using qRT-PCR and Western blot have shown that 5 important mitochondria-related genes of Drp1, Mfn1, TFAM, SGK1 and UCP2 haven’t significant changes in cerebellum, hippocampus or gastrocnemius muscle after SHH. Thirdly, cerebellar mitochondria detected by transmission electron microscopy (TEM) haven’t morphological changes after SHH treatment. The present study has indicated the benefit of a single SHH in healthy mice performance, which would due to the stabilized mitochondria against a mild stress state.
The present beneficial effect of SHH on performance is seemingly counterintuitive. In fact, hypobaric hypoxia have long been used for training pilots, mountaineers, and athletes and even applied for the treatment and prevention of human diseases such as hypertension14, ischemic coronary artery diseases20, Parkinson’s disease21, and acute myeloid leukemia22. Kiers D et al. have demonstrated that short-term hypoxia (3.5 h) dampens the systemic pro-inflammatory cytokine response through enhancing purinergic signaling in mice and men23. Serebrovska et al. have revealed that intermittent hypoxia-hyperoxia training improves cognitive function and decreases circulating biomarkers of Alzheimer’s disease. Similarly, hypoxic exposure can enhance both physical and mental capacities, resulting in increased aerobic performance capacity24. Evidence has demonstrated that mild hypoxic preconditioning and hypoxia-mimetic agents are beneficial to cerebral stroke and some neurodegenerative disorders25. Recently, it has been shown that hypoxia promotes neurogenesis in vitro26. All these results have indicated a role of a single hypoxia exposure for the potential therapeutic effects, at least on mice.
It is notable that in the rotarod tests, mice with SHH8000 treatment had decreased average velocity; also in the EPM tests, mice with SHH8000 treatment had decreased total distance. But we should consider the duration of both rotarod and EPM tests is only within 5 min, which is much shorter than the duration of 60 min in the modified Noldus video tracking system. Our Noldus recordings had evidenced that the distance moved, the sniff number and the rear-supported number indeed decreased at the early 8 min (indicated by the hollow arrow in Fig. 1). However, after a short recovery from the hypoxia, these three items began to increase and exceeded the normal level after then on. Some research has reported that short-term athletic training at an altitude of 1860 m can significantly improve 150 m running speed times27. And a single short-term traditional “live high-train high” or contemporary “live high-train low” training will lead to a 3% increase in O2 transportation and a 1.1–1.2% improve in sea level 3000 m run time8. Based on the data, it is tempting to speculate SHH indeed has beneficial effect on performance outcome.
Mitochondria-related genes are an important basis for the homeostasis of the central nervous system and physiological functions. Once the body is stimulated by extreme environments, mitochondrial UCPs immediately function to ensure normal mitochondrial function and maintain the body's normal living environment. Hypoxia can be regarded as an extreme environment that is accompanied by physiological metabolic challenges in normal tissues. Exercise or training increases expression levels of UCP228 and UCP329. Previous studies have shown that the UCP4 expression level in the cerebellum may potentially function as a protective factor to enhance neuronal survival30. The present qRT-PCR results showed that, after SHH5000 treatment, only the levels of Mfn2 and UCP4 within the cerebellum increased; in both hippocampus and gastrocnemius muscle, all 8 detected mitochondria-related genes did not change. UCP4 is a brain-specific isoform and its function in the neuron have not been established yet. Previous studies reported that UCP4 exhibits a competence of decrease mitochondrial membrane potential in cultured cells in vitro19. Xu et al. have found that UCP4 could lead to enhanced proton leak in cerebral mitochondrial membrane and stabilize mitochondrial Ca2+ homeostasis31. Our ultrastructural analysis further indicates cerebellar mitochondria show normal characteristics and do not display vacuolization of the cristae or distorted morphology. So we propose that cerebellum is sensitive to the physiological metabolic challenges and the elevated UCP4 upon hypoxia might contribute to its neuroprotective actions.
Mitochondrial dynamics has been recently linked to energy demand and supply balance32. At the molecular level, mitochondrial fusion depends on three fusion proteins: Mfn1 and Mfn2 at outer mitochondrial membranes and Opa1 at inner mitochondrial membranes32. Mfn2 is more abundant in the brain and skeletal muscle. Previous studies have shown that Mfn2 agonists could reverse mitochondrial defects in preclinical models of neurodegenerative disease of Charcot Marie Tooth disease type 2A (CMT2A) by mechanistically ameliorating mitochondrial trafficking33. The present results of the table Mfn2 mRNA levels within hippocampus and gastrocnemius tissues after SHH5000 and SHH8000, as well as the cerebellum after SHH8000, may imply that the mitochondrial fusion or trafficking in these areas maintains in balanced state after SHH stress.
Opa1 can promote the fusion of mitochondria32 and the defect of the Opa1 gene leads to the malformation of the mitochondrial cristae morphology, which has a serious influence on the proliferation of the cells34. Patten et al. have revealed that Opa1-dependent modulation of cristae structure is necessary for cellular adaptation to energy substrate availability and is required for cell survival34. The present results of the stable Opa1 mRNA level, as well as unchanged mitochondrial morphology and cristae structures, within the cerebellum after both SHH5000 and SHH8000, may imply the benefit of a single SHH in healthy mice performance is due to mitochondrial homeostasis. Rizo-Roca et al. have reported that the soleus muscles of the rats with 7 days exposure to intermittent hypobaric hypoxia at 4000 m have increased Opa1 protein expressions and activities35. We have also observed increased Opa1 mRNA level within the gastrocnemius skeletal tissues after SHH8000. These results would suggest a protective role of Opa1 against oxidative stress.
However, the present beneficial effect of SHH is challenged by two papers. Firstly, Chitra et al. have reported that the rats exposed to acute and severe hypobaric hypoxia (9142 m, 6 h) have had pulmonary oedema and the decreased Mfn2 expressions in lung tissue36. The controversy might be due to two points: altitudes and animal types. The hyobaric condition used by Chitra et al. has simulated much higher altitude (more than 9000 m) than that in the present study (SHH5000 and SHH8000 equal to 5000 and 8000 m, respectively). In addition, the study of Chitra et al. has imposed on rats, the present study on mice. Secondly, Zou et al. have reported that the rats subjected to SHH condition (5000 m) have had the decreased physical performance, as well as the decreased Mfn1 & Mfn2 mRNAs and increased drp1 mRNA in gastrocnemius tissues37. The controversy might be due to two points: SHH duration and animal types. The SHH used by Zou et al. lasted for 24 h, which was longer than the duration of 16 h in the present study. Also, the study of Zou et al. has imposed on rats. More importantly, we have noticed that the poor performance provided by Zou et al. is based on the results of rotarod tests. We have explained above that the duration of rotarod test is only within 5 min, which is much shorter than the duration of 60 min in the present modified Noldus video tracking system. We think the better physical performance under SHH condition in the present study is convincing.
In summary, the present findings open the door for further studies in hypobaric hypoxia effect in the field of the central nervous system and muscles. The benefit of a single SHH in healthy mice performance would due to the stabilized mitochondria against a mild stress state. Considering of the fact that being in the simulated hypobaric chambers has been already used in humans to improve exercise performance, it is deserved to detect the exact effects of SHH on mitochondrial dynamics, biogenesis, and activity of electron transporter chain.
Materials and methods
Mice
Adult male C57BL/6J mice with an average body weight of 20 ± 25 g were obtained from the Experimental Animal Center of the Air Force Medical University, Xi'an, Shaanxi, China. Mice were maintained on a 12:12 h light/dark cycle at 25 ± 1 °C with free access to standard laboratory feed and water. All animal protocols were approved by the Ethical Committee of the Air Force Medical University (permission number IACUC-20190107) and followed our institutional guidelines for the use of laboratory animals.
Experimental design
To explore the influence of mild to severe SHH, mice were randomly divided into three groups (n = 35 pergroup): control normoxia group (control), mild SHH group (SHH5000), and severe SHH group (SHH8000). All mice but those in the control group were subjected to SHH for 16 h. Following treatment, 20 mice (n = 20) in each group were used for behavioral tests, and 15 mice (n = 15) in each group were sacrificed for tissue collections. In behavioral tests, 10 mice were video tracked to assess both their locomotor and exploratory behaviors (as shown in Fig. 1a), 5 mice measured by Rotarod test to assess their balance abilities (as shown in Fig. 2a), and 5 mice measured by Elevated plus maze test to assess their exploratory abilities (as shown in Fig. 3a). 20 mice were not sacrificed but be used for other relevant research by our research group other members.
We chose the humane endpoint after SHH exposure in mice, 15 mice in each group were humanely sacrificed with sodium pentobarbital (50 mg/kg body weight) by intraperitoneal injection and cervical dislocation. Then 10 mice were used for Quantitative Real Time—PCR (qRT-PCR) (as shown in Figs. 4a, 5a, 6a) and Western blot to analyze changes in mRNA and protein levels of mitochondria-related genes within the cerebellum, the hippocampus and the gastrocnemius muscle. At the same time, 5 mice were perfused for transmission electron microscopy (TEM) analysis.
Simulated hypobaric hypoxia (SHH) treatment
To simulate a hypobaric hypoxia environment, a 12 mm thick stainless steel cabin (300 × 400 × 500 cm) was used38. An enclosed cabin, an exhaust valve and an intake valve leading into the cabin were installed and then connected to a vacuum pump. The hypobaric hypoxia cabin was designed by Professor Jin Ma, and the instrument was provided by the Department of Aerospace Medicine, Air Force Medical University, Xi’an, China. After normal mice were placed into the SHH chamber, the vacuum pump was turned on, and the gas in the cabin was continuously drawn out, resulting in low air pressure in the cabin. Environmental hypoxia was generated by adjusting the relative concentrations of nitrogen and oxygen in the input gas mixture. This created environmental oxygen tensions similar to those found in the high mountain communities of Nepaland Peru39. Continuous gas flow and CO2 absorption by Ca(OH)2 within the hypoxic chamber maintained CO2 levels below 0.4% with continuous monitoring. According to the method described by Paul H Holloway et al.40, the cabin pressure was adjusted to drop within 20 min to a vacuum of minus 11.01 kPa in the SHH5000 group, which was equivalent to an altitude of 5000 m atmosphere force; and the cabin pressure was adjusted to drop within 20 min to a vacuum of minus 7.51 kPa in the SHH8000 group, which was equivalent to an altitude of 8000 m atmosphere force. A control ambient environment for breathing 21% O2 was created with an identical chamber setup. During the experiment, the temperature was maintained at 20 ± 3 °C, and the humidity was 65 ± 5%.
Modified Noldus video tracking and tests
To observe the behavioral changes of the mice after SHH exposure, locomotor functionswere assessed using a set of modified Noldus PhenoTyper (Model 3000) chambers (Leeburg, VA) with shock floors as previously described41 (as shown in Fig. 1A).The PhenoTyper Model 3000 chamber has a 30 cm × 30 cm floor and is 40 cm in height. The PhenoTyper chamber is equipped with a top unit including a matrix of infrared LED lights and an infrared CCD camera with a high-pass filter blocking visible light. The floor of the cages was modified to include a stainless steel grid (interbar separation: 0.9 cm) connected to an electric shock generator (Shock Scrambler ENV-414S; Med Associates, St. Alvans; VT). Automated tracking and shock delivery control were performed using EthoVision 3.1 software (Noldus, Wageningen, the Netherlands)42. Individual mice were introduced into each chamber andacclimated to the apparatus for 60 min. Then, all mice were removed and left undisturbed inside their home cages. Subsequently, the mice were placed individually in the same cages they had experienced and were tested for 60 min. Behavioral data were collected, and then digital data were analyzed. Twelve items of observed behavioral elements were grouped into two categories. The first category is mainly related to locomotor activity and includes six items: distance moved (cm), average velocity (cm/s), walk duration (s), walk number (n), rest duration (s) and rest number (n). The walk state indicates that the mouse moves to another place with the hind legs moving as well. The rest state indicates resting without any movement, either sitting or lying down, including sleeping. The duration (s) and the number of walks or resting states were analyzed. The second category is mainly related to exploratory behavior, including duration (s) and number (n) of rear supported, rear unsupported or sniff states. The rear supported state indicates exploring while standing in an upright posture while leaning with the front paws against the cage wall or another object. The rear unsupported state indicates exploring while standing in an upright posture. The sniff state indicates slight movements of the head in order to gather information about the environment, possibly with slight, discontinuous displacement. The supplementary videos illustrate the performance of the behavioral tests.
Rotarod test
To assess the influence of SHH on the balance ability of mice, the rotarod test was performed (as shown in Fig. 2a). The rotarod test system from Shanghai Jiliang Software Technology Co., Ltd (Shanghai, China) was used. Before the test, mice were trained for three successive days at a constant speed (8 rpm on the first day, 11 rpm on the second day and 15 rpm on the third day). For the test, the mice were placed on the rotarod apparatus, with rotation starting at 8 rpm and progressing to a maximum of 20 rpm. The maximum speed allowed was 300 s per trial, and the falling latency of the mice was recorded. Three items were assessed including run time (s), distance moved (mm) and average velocity (mm/s). Each mouse was measured three times.
Elevated plus maze test
To assess the influence of SHH on the exploratory behavior of mice, the elevated plus maze test (Med Associates, St. Albans, Vermont) was performed (as shown in Fig. 3a). Animals were placed in the center square (10 × 10 cm) with their head towards a closed arm (40 × 10 cm), recorded for 5 min and analyzed with the motion tracking system. The total traveling distance and the central distance were recorded using the motion tracking system and analyzed by JLBehv-EPMG software (Shanghai Jiliang Software Technology Co., Ltd). Scoring was performed blinded to treatment type. Twelve items were assessed, including total arms times, total distance (cm), velocity (mm/s), closed arm entry times, movement distance in closed arm (mm), resistance time in closed arm (s), open arm entry times, movement distance in open arm (mm), resistance time in open arm (s), central entry times, central distance (mm), central resistance time (s). Each mouse was measured three times.
Quantitative real time-PCR (qRT-PCR)
To assess the influence of SHH on 8 mitochondria-related genes, quantitative Real Time-PCR (qRT-PCR) was performed. The tissues of cerebellum (as shown in Fig. 4a), hippocampus (as shown in Fig. 5a) and gastrocnemius muscle (as shown in Fig. 6a) of mice in three groups were collected, homogenized and processed to measure total RNA using Trizol reagent (Invitrogen, CA) in accordance with the manufacturer's instructions. The corresponding cDNA was synthesized using the extracted RNA as a template and detected by qRT-PCR. The detected eight genes include4 mitochondrial dynamic-related genes of Drp1, Mfn1, Mfn2 and Opa1, as well as 4 other mitochondrial factors of TFAM, SGK1, UCP2 and UCP4. The primer sequences are shown in Table 1. The internal reference is β-actin (Biotech, Shanghai). The reaction conditions: set the program as a two-step real-time quantification, pre-denaturation 95 °C, 15 s, and then each step denatures 95 °C, 5 s, annealing, extension 60 °C for 30 s for 40 cycles. After amplification, a dissolution curve was performed to check the homogeneity of the product. The relative content was calculated using the 2−△△Ct method for statistical analysis.
Table 1.
Sequences of the primers employed for amplification of mRNAs encoding Drp1, Mfn1, Mfn2, Opa1, TFAM, SGK1, UCP2 and UCP4 by qRT-PCR.
| mRNA | Sequences (5′–3′) | Length | Annealing temperature (°C) | |
|---|---|---|---|---|
| Drp1 |
Forward: Reverse: |
5′-AACAGGCAACTGGAGAGGAA-3′ 5′-GCAACTGGAACTGGCACAT-3′ |
144 | 58 |
| Mfn1 |
Forward: Reverse: |
5′-GGTCTGCTTTCCTGCTCTCT-3′ 5′-CTTTCTGCTCCCATTTCACC-3′ |
117 | 60 |
| Mfn2 |
Forward: Reverse: |
5′-CCTGGGATCGATGTTACCAC-3′ 5′-AACTGCTTCTCCGTCTGCAT-3′ |
119 | 62 |
| Opa1 |
Forward: Reverse: |
5′-GCCTTCCTCTTCGTCTCTCC-3′ 5′-CTCACTTGCTTCCACACCAA-3′ |
111 | 60 |
| TFAM |
Forward: Reverse: |
5′-GCAGGCACTACAGCGATACA-3′ 5′-TACCTTTCCCATTCCCTTCC-3′ |
128 | 58 |
| SGK1 |
Forward: Reverse: |
5′-GGTGGACTGGTGGTGTCTTG-3′ 5′-GAAGGAATCCACAGGAGGTGC-3′ |
122 | 62 |
| UCP2 |
Forward: Reverse: |
5′-TGGGAGGTAGCAGGAAATCA-3′ 5′-GCGGTATCCAGAGGGAAAGT-3′ |
135 | 60 |
| UCP4 |
Forward: Reverse: |
5′-CTCAGAGCCAACCGAATAGC-3′ 5′-GGCTGACAGATGCAACAGAA-3′ |
142 | 58 |
Western blotting
To assess the influence of SHH on mitochondria-related gene expressions, western blotting was performed. The tissues of cerebellum, hippocampus and gastrocnemius muscle of mice in three groups were collected into ice-cold homogenization buffer (50 mM Tris–HCl, pH 7.4, 150 mM NaCl, 1 mM EDTA, 0.5% Triton X, protease inhibitor cocktail) and homogenized before centrifugation (14,000g). Aliquots of the supernatant were incubated for 30 min at 37 °C in Laemmli SDS sample buffer (Invitrogen, Carlsbad, CA, USA). 20 μg of protein extracts were loaded on 10% acrylamide gel and blotted onto a methanol-activated PVDF membrane (Millipore, USA). The detected 5 gene proteins include 3 mitochondrial dynamic-related genes of Drp1, Mfn2 and Opa1, as well as 2 mitochondrial factors of TFAM and UCP4. Immunoblots were soaked in 5% nonfat milk 2 h at room temperature and subsequently probed with following primary antibodies overnight at 4 °C: rabbit-anti-Drp1 (1:250, Abcam, CA), rabbit-anti-Mfn2 (1:1000, Abcam, CA), rabbit-anti-Opa1 (1:1000, Abcam, CA), rabbit-anti-TFAM (1:1000, Abcam, CA), mouse-anti-UCP4 (1:200, Santa, CA), mouse-anti-β-actin (1:5000, Beijing, China). The immunoblots were then incubated with corresponding horseradish peroxidase (HRP)-conjugated secondary antibodies (1:5000, Beijing, China). The bands were detected with enhanced chemiluminescence (Beyotime, China) followed by exposure to luminometer (Bio-Rad, USA) and analyzed by ImageJ software. Target protein levels were normalized against β-actin levels and expressed as fold changes relative to those of the naive control group43.
Transmission electron microscopy (TEM) analysis
To observe the mitochondrial morphological changes after SHH treatment, transmission electron microscopy (TEM) analysis within the cerebellum was performed. After anesthesia, mice were perfused with 0.01 M PBS and 4% formaldehyde with 0.1% glutaraldehyde in PBS successively. The cerebellums were removed and placed into 4% glutaraldehyde solution for tissue fixation. After fixation, each cerebellum was rinsed twice with 0.1 M PB. Then, 1% osmic acid (TED PELLA, Inc. No.18451) was used for staining for 2 h. Then, 50%, 70%, and 90% ethanol and 100% acetone were used successively for dehydration, followed by acetone: embedding agent (Embed812, DDSA, NMA, DMP-30) = 1: 1 for 2 h at room temperature. Finally, the cerebellar tissue was removed from the embedding agent and stored at room temperature overnight. On the next day, the tissue was placed into a special electron microscope plate at 60 °C for 48 h. An ultrathin microtome was used to make 70 nm thick slices. The slices were placed on a copper network and stained with lead nitrate and uranium acetate for 10 min each. Images were recorded using a transmission electron microscope (JEM1400, Olympus, Japan).
Statistical analysis
Statistical analyses were performed with SPSS 15.0. Quantitative data are expressed as mean ± SD. The data are analyzed by one-way ANOVA (and nonparametric test). P < 0.05 was considered statistically significant.
Supplementary Information
Acknowledgements
This work was supported by State Key Laboratory of Military Stomatology Open project to Prof. Ya-Yun Wang (2018KA01), Scientific and technological research projects on major issues in aviation medicine from school to Prof. Ya-Yun Wang (2019ZTC03), grants from the National Natural Science Foundation of China to Prof. Yan-Ling Yang (81870415) and Key R&D Projects in Shaanxi Province to Prof. Ya-Yun Wang (2018ZDXM-SF-082,2018JZ8003). We thank Prof. Jin Ma, Department of Aerospace Physiology, AFMU, to provide hypobaric hypoxia chamber, also Prof. Jia-Yong Fan Department of Foreign Language, AFMU, for polishing the English.
Abbreviations
- Drp1
Dynamic-related protein 1 (mitochondrial fission factor)
- EPM
Elevated plus maze
- HH
Hypobaric hypoxia
- HIF
Hypoxia inducible factor
- Mfn1
Mitochondrial fusion protein 1 (mitochondrial fusion factor)
- Mfn2
Mitochondrial fusion protein 2 (mitochondrial fusion factor)
- Opa1
Optic atrophy1 (mitochondrial fusion factor)
- qRT-PCR
Quantitative real time-PCR
- SGK1
Serum and glucocorticoid-regulated protein kinase 1 (mitophagy-related factor)
- SHH
Simulated hypobaric hypoxia
- SHH5000
Simulated hypobaric hypoxia 5000 m
- SHH8000
Simulated hypobaric hypoxia 8000 m
- TFAM
Mitochondrial transcription factor A
- UCPs
Uncoupling proteins
- UCP2
Uncoupling protein2 (mitochondrial stress factor)
- UCP4
Uncoupling protein 4 (mitochondrial stress factor)
- TEM
Transmission electron microscopy
Author contributions
F.-F.W. and K.-L.Z. contributed to conception and design. All authors were involved in analysis and interpretation of the data. Y.-L.Y., H.-F.Z., Y.-Y.W. drafted manuscript, Z.-M.W., Y.Y. and J.-Q.W. provided to experiments, professional drawings and statistical expertise. J.M. and S.-H.L. provide hypobaric hypoxia chamber. All authors approved the final version.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Fei-Fei Wu and Kun-Long Zhang.
Contributor Information
Yan-Ling Yang, Email: yangyanl@fmmu.edu.cn.
Hai-Feng Zhang, Email: hfzhang@fmmu.edu.cn.
Ya-Yun Wang, Email: wangyy@fmmu.edu.cn.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-020-80425-8.
References
- 1.Kicken CH, et al. Hypobaric hypoxia causes elevated thrombin generation mediated by FVIII that is balanced by decreased platelet activation. Thromb. Haemost. 2018;118:883–892. doi: 10.1055/s-0038-1641566. [DOI] [PubMed] [Google Scholar]
- 2.West JB. Physiological effects of chronic hypoxia. N. Engl. J. Med. 2017;376:1965–1971. doi: 10.1056/NEJMra1612008. [DOI] [PubMed] [Google Scholar]
- 3.Peacock, A. J. ABC of oxygen Oxygen at high altitude. (1998). [DOI] [PMC free article] [PubMed]
- 4.Wilson MH, Newman S, Imray CH. The cerebral effects of ascent to high altitudes. Lancet Neurol. 2009;8:175–191. doi: 10.1016/S1474-4422(09)70014-6. [DOI] [PubMed] [Google Scholar]
- 5.Wu X, Li X, Han L, Wang T, Wei Y. Effects of acute moderate hypoxia on human performance of arithmetic. Space Med. Med. Eng. (Beijing) 1998;11:391–395. [PubMed] [Google Scholar]
- 6.Pelamatti G, Pascotto M, Semenza C. Verbal free recall in high altitude: Proper names vs common names. Cortex. 2003;39:97–103. doi: 10.1016/s0010-9452(08)70077-7. [DOI] [PubMed] [Google Scholar]
- 7.Bouquet CA, Gardette B, Gortan C, Abraini JH. Psychomotor skills learning under chronic hypoxia. NeuroReport. 1999;10:3093–3099. doi: 10.1097/00001756-199909290-00040. [DOI] [PubMed] [Google Scholar]
- 8.Millet GP, Roels B, Schmitt L, Woorons X, Richalet JP. Combining hypoxic methods for peak performance. Sports Med. 2010;40:1–25. doi: 10.2165/11317920-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 9.Girard O, et al. Position statement–altitude training for improving team-sport players' performance: Current knowledge and unresolved issues. Br. J. Sports Med. 2013;47(Suppl 1):i8–16. doi: 10.1136/bjsports-2013-093109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brocherie F, et al. Repeated maximal-intensity hypoxic exercise superimposed to hypoxic residence boosts skeletal muscle transcriptional responses in elite team-sport athletes. Acta Physiol. (Oxf.). 2018 doi: 10.1111/apha.12851. [DOI] [PubMed] [Google Scholar]
- 11.Jurgens KD, Gros G. Phylogeny of gas exchange systems. Anasthesiol. Intensivmed. Notfallmed. Schmerzther. 2002;37:185–198. doi: 10.1055/s-2002-25080. [DOI] [PubMed] [Google Scholar]
- 12.Liu P, et al. Dihydromyricetin improves hypobaric hypoxia-induced memory impairment via modulation of SIRT3 signaling. Mol. Neurobiol. 2016;53:7200–7212. doi: 10.1007/s12035-015-9627-y. [DOI] [PubMed] [Google Scholar]
- 13.Mironova GD, et al. Effect of hypoxia on mitochondrial enzymes and ultrastructure in the brain cortex of rats with different tolerance to oxygen shortage. J. Bioenergy Biomembr. 2019;51:329–340. doi: 10.1007/s10863-019-09806-7. [DOI] [PubMed] [Google Scholar]
- 14.Serebrovskaya TV, Manukhina EB, Smith ML, Downey HF, Mallet RT. Intermittent hypoxia: Cause of or therapy for systemic hypertension? Exp. Biol. Med. (Maywood) 2008;233:627–650. doi: 10.3181/0710-MR-267. [DOI] [PubMed] [Google Scholar]
- 15.Franco A, et al. Correcting mitochondrial fusion by manipulating mitofusin conformations. Nature. 2016;540:74–79. doi: 10.1038/nature20156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Delettre C, et al. Nuclear gene OPA1, encoding a mitochondrial dynamin-related protein, is mutated in dominant optic atrophy. Nat. Genet. 2000;26:207–210. doi: 10.1038/79936. [DOI] [PubMed] [Google Scholar]
- 17.Picca A, Lezza AM. Regulation of mitochondrial biogenesis through TFAM-mitochondrial DNA interactions: Useful insights from aging and calorie restriction studies. Mitochondrion. 2015;25:67–75. doi: 10.1016/j.mito.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 18.Sierra-Ramos C, et al. SGK1 activation exacerbates diet-induced obesity, metabolic syndrome and hypertension. J. Endocrinol. 2020;244:149–162. doi: 10.1530/JOE-19-0275. [DOI] [PubMed] [Google Scholar]
- 19.Liu D, et al. Mitochondrial UCP4 mediates an adaptive shift in energy metabolism and increases the resistance of neurons to metabolic and oxidative stress. Neuromol. Med. 2006;8:389–414. doi: 10.1385/NMM:8:3:389. [DOI] [PubMed] [Google Scholar]
- 20.Zhu M, et al. Ischemic postconditioning protects remodeled myocardium via the PI3K-PKB/Akt reperfusion injury salvage kinase pathway. Cardiovasc. Res. 2006;72:152–162. doi: 10.1016/j.cardiores.2006.06.027. [DOI] [PubMed] [Google Scholar]
- 21.Liu J, Ames BN. Reducing mitochondrial decay with mitochondrial nutrients to delay and treat cognitive dysfunction, Alzheimer's disease, and Parkinson's disease. Nutr. Neurosci. 2005;8:67–89. doi: 10.1080/10284150500047161. [DOI] [PubMed] [Google Scholar]
- 22.van Oosterwijk JG, et al. Hypoxia-induced upregulation of BMX kinase mediates therapeutic resistance in acute myeloid leukemia. J. Clin. Investig. 2018;128:369–380. doi: 10.1172/JCI91893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kiers D, et al. Short-term hypoxia dampens inflammation in vivo via enhanced adenosine release and adenosine 2B receptor stimulation. EBioMedicine. 2018;33:144–156. doi: 10.1016/j.ebiom.2018.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Serebrovska ZO, et al. Intermittent hypoxia-hyperoxia training improves cognitive function and decreases circulating biomarkers of Alzheimer's disease in patients with mild cognitive impairment: A pilot study. Int. J. Mol. Sci. 2019 doi: 10.3390/ijms20215405. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 25.Davis CK, Jain SA, Bae ON, Majid A, Rajanikant GK. Hypoxia mimetic agents for ischemic stroke. Front. Cell Dev. Biol. 2018;6:175. doi: 10.3389/fcell.2018.00175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sun C, et al. Chronic mild hypoxia promotes hippocampal neurogenesis involving Notch1 signaling in epileptic rats. Brain Res. 2019;1714:88–98. doi: 10.1016/j.brainres.2019.02.011. [DOI] [PubMed] [Google Scholar]
- 27.Karvonen J, Peltola E, Saarela J, Nieminen MM. Changes in running speed, blood lactic acid concentration and hormone balance during sprint training performed at an altitude of 1860 metres. J. Sports Med. Phys. Fitness. 1990;30:122–126. [PubMed] [Google Scholar]
- 28.Busquets-Cortés C, et al. Training and acute exercise modulates mitochondrial dynamics in football players' blood mononuclear cells. Eur. J. Appl. Physiol. 2017;117:1977–1987. doi: 10.1007/s00421-017-3684-z. [DOI] [PubMed] [Google Scholar]
- 29.Morales FE, et al. BAIBA does not regulate UCP-3 expression in human skeletal muscle as a response to aerobic exercise. J. Am. Coll. Nutr. 2017;36:200–209. doi: 10.1080/07315724.2016.1256240. [DOI] [PubMed] [Google Scholar]
- 30.Erden Y, et al. Effects of central irisin administration on the uncoupling proteins in rat brain. Neurosci. Lett. 2016;618:6–13. doi: 10.1016/j.neulet.2016.02.046. [DOI] [PubMed] [Google Scholar]
- 31.Xu Y, Liu Y, Xia C, Gao P, Liu JZ. Evidence for involvement of uncoupling proteins in cerebral mitochondrial oxidative phosphorylation deficiency of rats exposed to 5,000 m high altitude. Neurochem. Res. 2013;38:282–289. doi: 10.1007/s11064-012-0917-8. [DOI] [PubMed] [Google Scholar]
- 32.Schrepfer E, Scorrano L. Mitofusins, from mitochondria to metabolism. Mol. Cell. 2016;61:683–694. doi: 10.1016/j.molcel.2016.02.022. [DOI] [PubMed] [Google Scholar]
- 33.Rocha AG, et al. MFN2 agonists reverse mitochondrial defects in preclinical models of Charcot-Marie-Tooth disease type 2A. Science. 2018;360:336–341. doi: 10.1126/science.aao1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Patten DA, et al. OPA1-dependent cristae modulation is essential for cellular adaptation to metabolic demand. EMBO J. 2014;33:2676–2691. doi: 10.15252/embj.201488349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rizo-Roca D, et al. Modulation of mitochondrial biomarkers by intermittent hypobaric hypoxia and aerobic exercise after eccentric exercise in trained rats. Appl. Physiol. Nutr. Metab. 2017;42:683–693. doi: 10.1139/apnm-2016-0526. [DOI] [PubMed] [Google Scholar]
- 36.Chitra L, Boopathy R. Adaptability to hypobaric hypoxia is facilitated through mitochondrial bioenergetics: An in vivo study. Br. J. Pharmacol. 2013;169:1035–1047. doi: 10.1111/bph.12179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zou D, et al. Dihydromyricetin improves physical performance under simulated high altitude. Med. Sci. Sports Exerc. 2014;46:2077–2084. doi: 10.1249/MSS.0000000000000336. [DOI] [PubMed] [Google Scholar]
- 38.Judd E, Calhoun DA. Apparent and true resistant hypertension: Definition, prevalence and outcomes. J. Hum. Hypertens. 2014;28:463–468. doi: 10.1038/jhh.2013.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Beran D, et al. Moving from formative research to co-creation of interventions: Insights from a community health system project in Mozambique, Nepal and Peru. BMJ Glob. Health. 2018;3:e001183. doi: 10.1136/bmjgh-2018-001183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Holloway PH, Pritchard DG. Effects of ambient temperature and water vapor on chamber pressure and oxygen level during low atmospheric pressure stunning of poultry. Poult. Sci. 2017;96:2528–2539. doi: 10.3382/ps/pex066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Spink AJ, Tegelenbosch RA, Buma MO, Noldus LP. The EthoVision video tracking system—a tool for behavioral phenotyping of transgenic mice. Physiol. Behav. 2001;73:731–744. doi: 10.1016/s0031-9384(01)00530-3. [DOI] [PubMed] [Google Scholar]
- 42.Pham J, Cabrera SM, Sanchis-Segura C, Wood MA. Automated scoring of fear-related behavior using EthoVision software. J. Neurosci. Methods. 2009;178:323–326. doi: 10.1016/j.jneumeth.2008.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bai Y, et al. Targeted upregulation of uncoupling protein 2 within the basal ganglia output structure ameliorates dyskinesia after severe liver failure. Free Radic. Biol. Med. 2018;124:40–50. doi: 10.1016/j.freeradbiomed.2018.05.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.