Abstract
Preoperative anaemia is common in the Asia-Pacific. Iron deficiency anaemia (IDA) is a risk factor that can be addressed under patient blood management (PBM) Pillar 1, leading to reduced morbidity and mortality. We examined PBM implementation under four different healthcare systems, identified challenges and proposed several measures: (a) Test for anaemia once patients are scheduled for surgery. (b) Inform patients about risks of preoperative anaemia and benefits of treatment. (c) Treat IDA and replenish iron stores before surgery, using intravenous iron when oral treatment is ineffective, not tolerated or when rapid iron replenishment is needed; transfusion should not be the default management. (d) Harness support from multiple medical disciplines and relevant bodies to promote PBM implementation. (e) Demonstrate better outcomes and cost savings from reduced mortality and morbidity. Although PBM implementation may seem complex and daunting, it is feasible to start small. Implementing PBM Pillar 1, particularly in preoperative patients, is a sensible first step regardless of the healthcare setting.
Keywords: anaemia, Asia Pacific, iron deficiency, patient blood management, preoperative
INTRODUCTION
Anaemia is a global health problem, affecting 30% of the world’s population in 2015.(1) In 2010, there were 68.4 million years lived with disability from anaemia worldwide, and 56% of these were in Asia-Pacific countries.(2) Anaemia, which is characterised by a decrease in total red blood cell (RBC) mass, is accompanied by reduced haemoglobin (Hb) levels and altered RBC morphology. As its symptoms are nonspecific and develop gradually, it often goes unnoticed and therefore untreated. Iron deficiency (ID) is the most common cause of anaemia (> 50%),(2) manifesting in decreased production of Hb and activity of iron-dependent enzymes.(3) Iron deficiency anaemia (IDA) often presents in young children and pregnant women in developing countries due to malnutrition, multiparity, postpartum haemorrhage and infectious diseases; and in the elderly due to bleeding from gastrointestinal conditions.(4)
Preoperative anaemia represents a significant healthcare problem in Asia-Pacific countries.(5-8) This is compounded by the limited supply of blood products: 19 (23%) out of 82 countries with low donation rates (< 10 donations per 1,000 population) are in the Asia-Pacific.(9) These are typically developing countries with growing populations and a high demand for transfusions.(10) Their blood services also face difficulties in safeguarding blood stocks from risks posed by pathogens in the blood supply.(11) On the other hand, the developed countries, and even some of the less developed countries with ageing populations, have to confront the decreasing numbers of eligible donors. In addition, older persons, who have higher risks of malignancies and chronic diseases, are more likely to require complex surgical interventions.(12)
POORER OUTCOMES FOR PATIENTS WITH PREOPERATIVE ANAEMIA
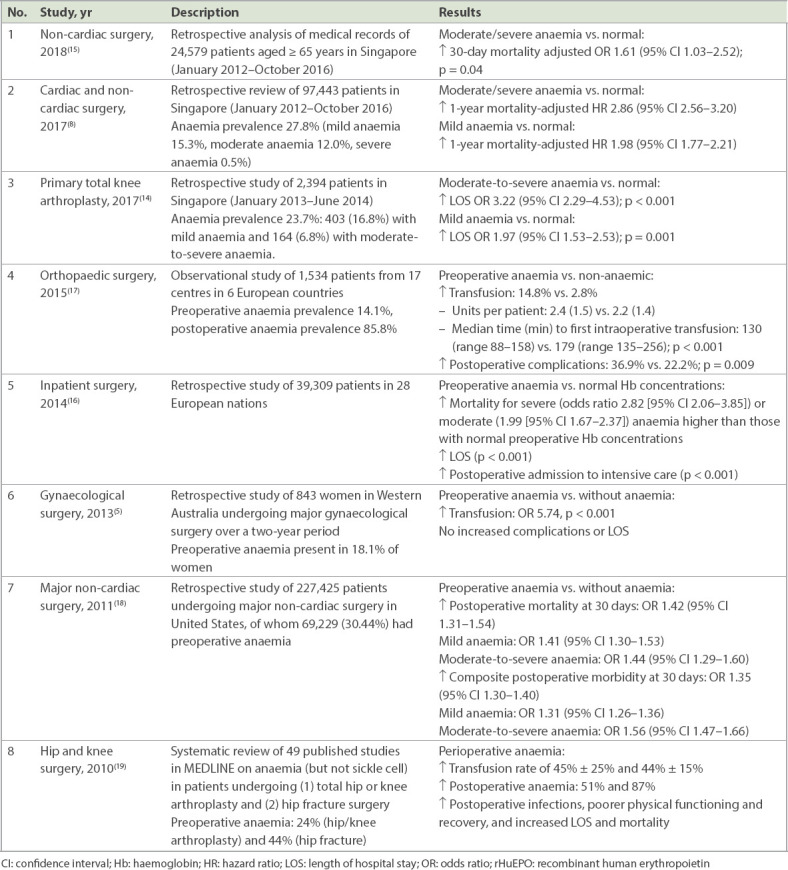
IDA is an independent risk factor for poor outcomes among patients scheduled for surgery. In a meta-analysis of observational studies, 39.1% of 949,445 patients undergoing surgery were found to be anaemic.(13) This study and others (Table I) found preoperative anaemia to be associated with greater risks of transfusion, morbidity, mortality and increased length of hospital stay (LOS).(5,8,14-19) Despite these risks and the exacerbation of anaemia by surgical blood loss, preoperative anaemia is deemed acceptable by many physicians.(20) Consequently, many patients receive allogeneic RBC transfusions, which have remained the mainstay of perioperative anaemia management in many settings. This may be undesirable, as RBC transfusion is another independent risk factor for adverse outcomes such as infections and lung injury.(21)
Table I.
Outcomes in patients with preoperative anaemia.
Patient blood management (PBM) improves patient outcomes by applying evidence-based medical and surgical concepts across its three pillars, namely: Pillar 1 – optimise RBC mass; Pillar 2 – minimise blood loss; and Pillar 3 – optimise anaemia tolerance of the patient to improve outcomes by clinically managing and preserving the patient’s own blood.(22) In May 2010, the World Health Organization (WHO) formally recognised the importance of PBM and recommended it to its 193 member states.(23) Under PBM Pillar 1, a key strategy for optimising the total RBC mass of patients undergoing surgery is to identify anaemia and treat its underlying causes preoperatively.(22) For example, the Australian PBM guidelines recommend that doctors perform early evaluation and treatment of preoperative ID/IDA and its underlying causes as part of preparation for elective surgery.(24) In most cases, preoperative IDA can be corrected with iron replacement therapy.(22)
Successful PBM implementation in Western Australia was associated not only with reduced blood use (i.e. RBC units/admission declined by 26% despite a 22% rise in admissions),(25) but also significant reductions in preoperative anaemia, hospital-acquired complications, in-hospital mortality and LOS, with cost savings of > AUD 6 million per year.(26) Such observations give weight to recommendations that elective surgeries be delayed until after anaemia correction.(27) Despite these reasons and the availability of therapeutic strategies and pharmacologic interventions for reducing transfusion in the perioperative setting, PBM implementation has varied widely, even in Europe and Canada where PBM has been practised for many years.(28,29)
CHALLENGES AND PROPOSED SOLUTIONS
We examined PBM implementation in the Asia-Pacific countries of Australia, Malaysia, Republic of Korea and Singapore, discussing specific challenges of implementing PBM in these countries and suggesting potential solutions (Table II).
Table II.
Challenges to PBM implementation and proposed solutions.
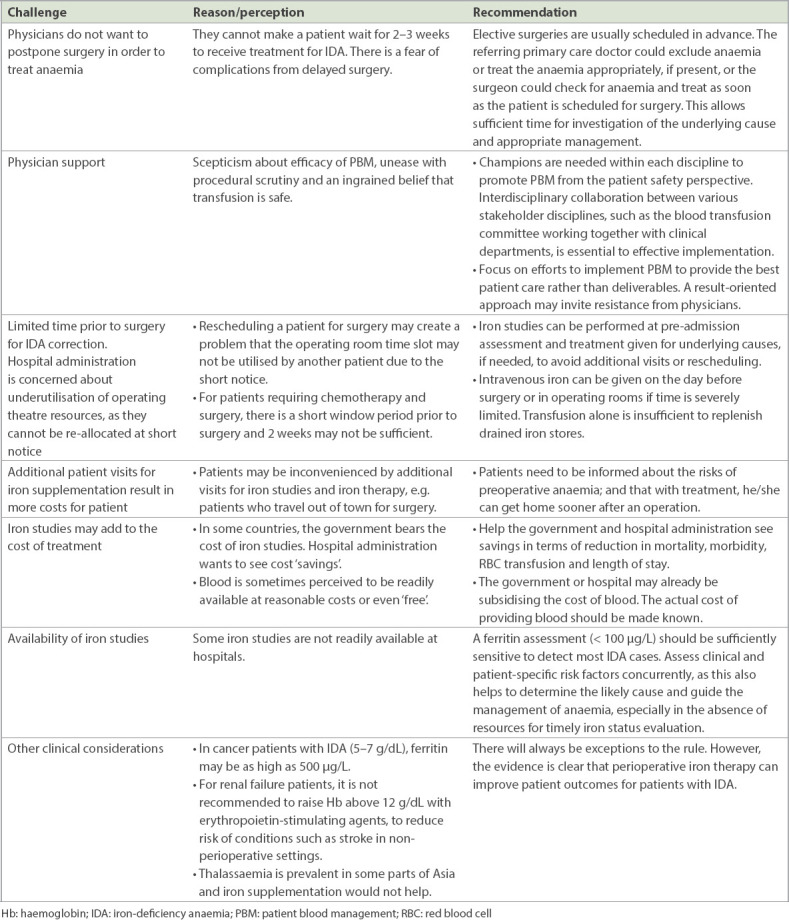
Postponement of surgery due to preoperative anaemia is usually not well received. Hospital administrators are concerned about optimising the utilisation of operating theatres, while physicians are resistant to changes to their clinical practice and concerned that delaying surgery may result in medical complications. Patients do not want to delay treatment, particularly for major illnesses, and are concerned about the cost and time needed for additional visits. Understanding that appropriate changes to current clinical practice can deliver better patient care and educating patients on the potential risks and benefits can help to overcome these challenges. Physicians should initiate anaemia investigations early, while patients should also be informed about the benefits of treating preoperative anaemia. We proposed an algorithm for the diagnosis and treatment of preoperative anaemia (Fig. 1).
Fig. 1.
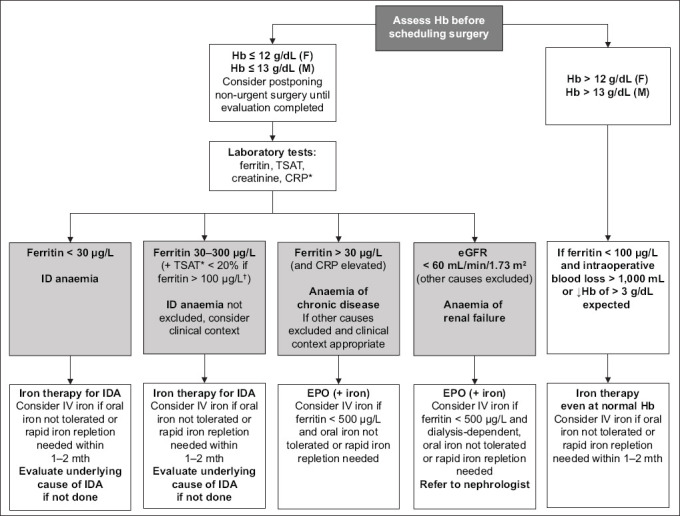
Chart shows proposed algorithm to evaluate and treat perioperative anaemia. *If TSAT is unavailable, assess clinical context for conditions that may falsely elevate ferritin despite ID. †If ferritin is > 100 μg/L, TSAT < 20% is required to support diagnosis of IDA. If anaemia cannot be classified based on these, contact a haematologist. CRP: C-reactive protein; eGFR: estimated glomerular filtration rate; EPO: erythropoietin; F: female; Hb: haemoglobin; ID: iron deficiency; IDA: iron deficiency anaemia; IV: intravenous; M: male; TSAT: transferrin saturation
Although formal iron studies are needed prior to iron therapy, some tests may not be readily available in resource-limited settings. We suggest that an assessment of ferritin together with clinical and patient-specific risk factors can identify most IDA cases. When IDA is detected early, oral iron supplementation is usually the first-line treatment. Some side effects from the use of oral iron include nausea, constipation and vomiting,(4) which may lead to poor compliance to treatment. A systematic review has concluded that patients administered with intravenous (IV) iron experienced fewer gastrointestinal side effects compared to oral iron treatments.(30)
When time is limited, IV iron infusions can be used to rapidly and effectively replenish iron stores without compromising outcomes.(31) However, in patients who urgently require reliable and rapid iron replacement, IV iron formulations such as iron sucrose, ferric gluconate, iron isomaltoside, low-molecular-weight iron dextran (LMW-ID) or ferric carboxymaltose may be better suited, as they allow the slow release of iron with marginal or no toxicity-related adverse events.(4,32-34) Incidence rates of adverse drug events were found to be lower with modern IV iron formulations, including LMW-ID, than with older high-molecular-weight iron dextran preparations.(35) Whereas iron sucrose and ferric gluconate infusions need to be administered across several sessions, iron isomaltoside, LMW-ID or ferric carboxymaltose, which bind iron more tightly, can replenish total iron deficit in one or two doses.(4,32)
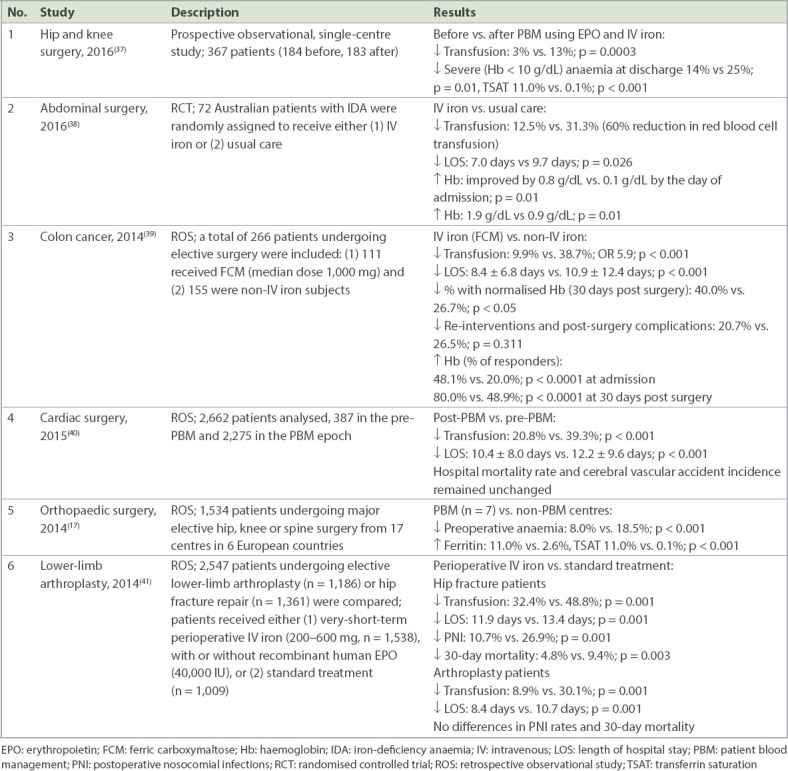
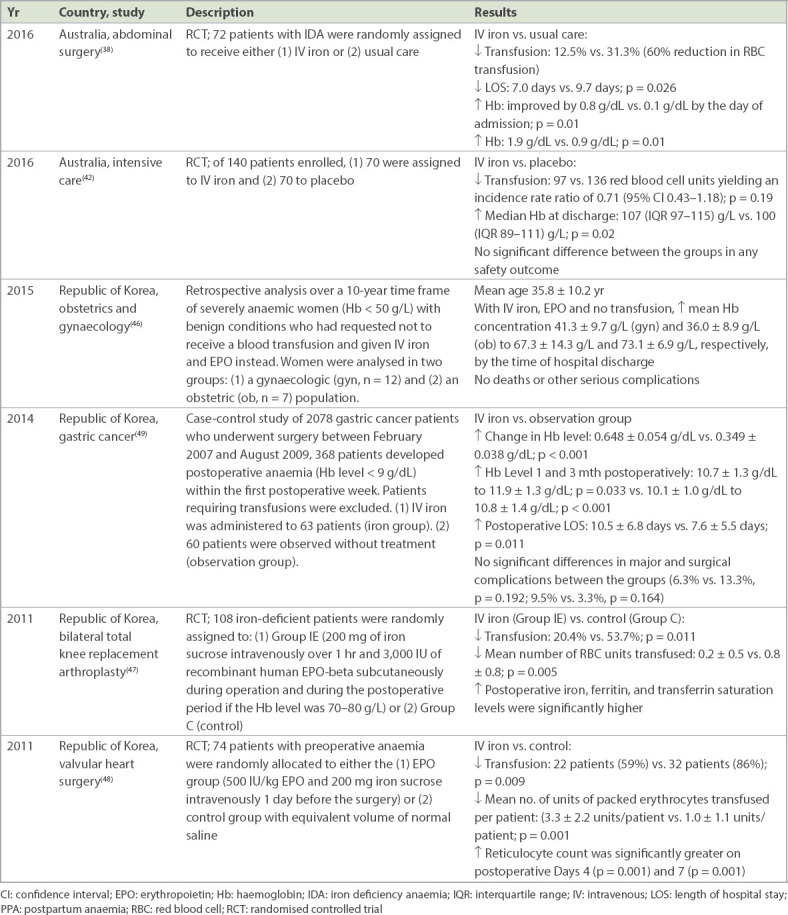
IV iron is applicable in certain instances, including immediately before surgery, post trauma, and in cases of inability to tolerate or absorb oral iron, iron loss exceeding absorption rates, and late pregnancy.(4) When there is insufficient preoperative time (e.g. trauma and emergency surgical cases), postoperative IV iron therapy has also been shown to improve Hb recovery with fewer RBC transfusions, shorter LOS and, importantly, fewer infections.(36) Clinical evidence (Table III) suggests that the use of IV iron increases the total RBC mass of patients undergoing surgery and improves outcomes.(17,37-41) Even in critically ill patients, early IV iron therapy raised discharge Hb levels despite lower transfusion triggers (< 7.5 g/dL) without compromising safety.(42)
Table III.
Improvement in patient outcomes from perioperative IV iron therapy.
EXPERIENCE IN THE ASIA-PACIFIC
PBM champions such as national health authorities and/or blood services, professional medical organisations, hospital administrators and, crucially, physicians are pivotal in promoting PBM implementation. They provide the strong leadership needed to sustainably establish effective programmes and create collaborative environments for healthcare professionals from the surgical, medical, transfusion medicine, and nursing departments, laboratory and pharmacy with guidelines, communication tools and education.(43) We herein discuss examples from Australia and Singapore, the Republic of Korea and Malaysia and illustrate how different PBM champions can positively influence the practice of PBM in their respective countries.
National health authorities
In Australia, the National Blood Authority has published comprehensive PBM guidelines since 2012.(24) In addition, the Australian Commission on Safety and Quality in Health Care “requires that blood and blood product policies, procedures and/or protocols are consistent with national evidence-based guidelines for pre-transfusion practices, prescribing and clinical use of blood and blood products” (Action 7.1.1).(24) From mid-2010 to mid-2015, the number of RBC units issued saw a 15.8% reduction.(44) A multidisciplinary National Patient Blood Management Collaborative, led by the Department of Health, Australia, was established in 2015 to further promote appropriate care for patients and reduce exposure to transfusion. 12 hospitals were selected and supported with federal funding. They identified and implemented changes in preoperative practice in areas that were at risk for anaemia. Monthly data for 8,758 procedures (May 2015–September 2016) showed that 98% of patients were assessed for preoperative anaemia, an increase from 90%; 71% had their anaemia managed, up from 28%; 90% were assessed for ID, from 25%; and 53% had their ID managed, from 39%.(44)
In Singapore, the Blood Services Group of the Health Sciences Authority, a statutory board of the Ministry of Health, supplies blood nationwide. With an ageing population (11.8% were aged > 65 years) and life expectancy of 82.7 years, blood demand is expected to increase even as eligible donors decrease.(45) To mitigate this, the Ministry of Health and Blood Services Group have actively promoted PBM at public hospitals since 2013. Regular national audits of PBM-related efforts have been performed since 2017 to promote appropriate clinical indications for RBC transfusion and preoperative anaemia screening for elective surgeries. We herein describe these PBM efforts at two major public hospitals: National University Hospital and Singapore General Hospital, Singapore.
National University Hospital’s anaemia clinic was started in 2014 and is integral to its PBM programme. A preliminary survey showed that 23% of patients had preoperative anaemia, with 57% requiring transfusion subsequently, compared to 18% for patients without anaemia. Surgeons were encouraged to refer patients for anaemia management if patients had Hb < 10 g/dL, any degree of anaemia and poor cardiopulmonary reserve; or when the surgery had a potential for high blood loss. IDA management was initiated with oral iron if ferritin < 100 μg/L (< 200 μg/L in non-dialysis-dependent chronic kidney disease) and transferrin saturation < 20%. IV iron was given as soon as was feasible if there was no response after two weeks, intolerance to oral iron or the surgery was scheduled within four weeks; or after surgery if therapy was not started earlier. Erythropoietin was used on an individualised basis, e.g. chronic kidney disease Stage III/V or chemotherapy-induced anaemia in a palliative setting.
At Singapore General Hospital, formal PBM implementation was started in 2013 as part of the national initiative. The hospital had a number of existing measures to support PBM, i.e. a multidisciplinary blood transfusion committee, transfusion guidelines and an early preoperative anaemia assessment clinic. In August 2017, a preoperative anaemia management pathway was instituted in which anaemic patients undergoing surgery were given either oral iron (ferrous fumarate) or single-dose IV iron (ferric carboxymaltose) depending on the severity of anaemia, invasiveness of surgery and time available for optimisation. Mandatory documentation of indications for RBC transfusion was also instituted, while inappropriate indications generated alerts via the computerised physician order entry (CPOE) system. A preliminary one-month audit of the system showed that 21% of CPOEs generated alerts for inappropriate indications and were subsequently cancelled.
Professional medical organisations
The Korean Research Society of Transfusion Alternatives of the Republic of Korea began promoting PBM in 2006. In 2014, the Korean Patient Blood Management (KPBM) Research Group was formed to further promote greater PBM use. Its active participation saw PBM included in the Korean Transfusion Guidelines of 2016 for the first time. In 2016, the KPBM organised a new steering committee comprising > 40 leading physicians from various specialties to promote PBM in their respective clinical fields.
The Korean Society of Blood Transfusion, representing practitioners in blood banking and transfusion medicine, including laboratory physicians, haematologists and anaesthetists, supported PBM with the creation of its PBM committee in 2016. A KPBM survey showed that 70%–80% of practising surgeons supported the use of PBM and had held special PBM symposia within their respective society meetings. A number of Korean hospitals that adopted PBM as part of their clinical practice have already demonstrated its benefits in improved postoperative Hb levels, with reductions in transfusions (Table IV).(46-49)
Table IV.
Studies documenting benefits of PBM in Asia-Pacific countries.
Physicians
In Malaysia, PBM is practised at the local level (e.g. maternal and fetal medicine department at the Sultan Haji Ahmad Shah Hospital, Pahang, Malaysia). Postpartum haemorrhage (PPH) remains one of the main causes of maternal mortality in Malaysia. High parity is common among local women and access to affordable healthcare remains a key challenge. Women at high risk of anaemia are tested for Hb levels and ferritin in early pregnancy. Patients who are found to be iron-deficient are treated with low-dose elemental iron (20–80 mg daily); those with anaemia are given higher-dose elemental iron orally (100–200 mg daily) and their response is monitored. In this resource-constrained setting, IV iron is used when time is limited or when oral iron is ineffective or poorly tolerated. Despite its efficacy, IV iron is used sparingly due to the higher cost of iron sucrose compared to oral iron. Other practical measures to minimise the risk of anaemia included providing dietary advice and advice on increasing the interval period between pregnancies as well as treating comorbidities.
For PPH, patients who were not actively bleeding were managed in the following ways based on their Hb levels: (a) > 9 g/L – transfusion was deemed inappropriate and discouraged; (b) 7–9 g/L – transfusion was based on the need to relieve clinical signs and symptoms of anaemia, and the availability of anaemia treatment, expected delivery date and risk factors for haemorrhage; and (b) < 7 g/L – transfusion could be used but might not be required for well-compensated patients, or other therapies were available. When indicated, a single RBC unit was given followed by clinical assessment to determine further need.
BENEFITS OF PBM PILLAR 1
Our article has described the practice of PBM in four different healthcare settings. Although these examples are certainly not exhaustive, they illustrate a range of implementation approaches that can be applied in both developed and developing countries. As we and others have noted, there is an urgent need for action.(50) The anaemia burden in the Asia-Pacific region is high, with growing numbers of elderly patients who are more likely to be anaemic.(2) Without PBM, a third to half (30%–54%)(16,18,47) of patients undergoing surgery could require transfusion, increasing the demand for blood and potentially leading to poorer patient outcomes. Shrinking blood donor pools puts a strain on the blood supply system and may result in cancellation or postponement of elective surgery in some countries.
On the other hand, studies in the region have shown that the application of PBM Pillar 1 has led to shorter LOS, improved Hb/ferritin levels and fewer adverse events, besides reduced transfusion rates (Table IV).(38,42,46-49) Implementation of PBM also has a significant positive impact on healthcare costs. A 2012 study of > 100,000 patients in the canton of Zurich, Switzerland, showed a 27% reduction in RBC transfusion in the first year of implementation with direct savings of USD 2.0 million on blood products alone.(43,51) In Australia, the National Blood Authority estimated that a 5% reduction in RBC use would save AUD 14.6 million nationally.(51) Cost savings from the use of IV iron to treat preoperative IDA were reported at USD 730 per patient (Singapore)(52) and USD 22,192 per quality-adjusted life-year for patients with chronic heart failure (Republic of Korea)(53) in 2014. There is also the intangible cost of RBC transfusion-associated adverse outcomes and prolonged LOS.(54)
While each country may face different challenges in implementing PBM, the concept is applicable everywhere. Notwithstanding its urgency, the implementation process should proceed stepwise in a manner that is appropriate to the healthcare setting and acceptable to stakeholders. Post implementation, it is also essential to apply quality assurance measures of good benchmarking, monitoring and feedback,(54) and demonstrate improved patient outcomes and safety benefits. Although this review presents PBM Pillar 1 for perioperative settings, the same principles of implementation can be extended to the other two pillars of PBM and to the non-surgical fields of medicine.
CONCLUSION
IDA is common and it is an independent modifiable risk factor for patient outcomes. Physicians and patients need to be aware of the risks of preoperative anaemia and appreciate that early treatment of IDA preoperatively can help to improve patient safety and outcomes. The most feasible way of implementing PBM is to start with small steps and expand efforts over time. Getting PBM Pillar 1 right by using iron replacement therapy to preoperatively optimise red cell mass in patients with IDA is a sensible first step to take when embarking on PBM implementation, regardless of the healthcare setting.
AUTHOR CONTRIBUTIONS
Froessler B and Spahn DR co-chaired the PBM workshop and presented data on current Pillar 1 practice. Froessler B presented data for Australia; Lim KKC for Malaysia; Ang AL, Lee SY and Singh G for Singapore; and Kim YW for the Republic of Korea. All of the authors participated in the workshop discussion, contributed equally to the drafting, reviewed the manuscript and approved its submission.
ACKNOWLEDGEMENTS AND DISCLOSURE OF COMPETING INTERESTS
This manuscript was developed following a workshop supported by Vifor Pharma Asia Pacific and Vifor (International) AG in October 2016. Vifor Pharma Asia Pacific provided support in respect of publication costs but had no influence on the content of the work. Abdullah HR received travel support, speaking honoraria and research grant support from Vifor Pharma. Lee SY, Lim KKC and Um TH received travel support from Vifor Pharma to attend the workshop. Ang AL and Lee JJ have received speaker or lecture honoraria in the past and travel support from Vifor Pharma. Froessler B has received lecture honoraria or travel support in the past five years from the New South Wales Department of Health; South Australia Department of Health; Australian Red Cross Blood Service; National Blood Authority, Australia; Vifor Pharma Ltd, Glattbrugg, Switzerland; Fresenius Kabi GmbH, Bad Homburg, Germany; and CSL Behring Biotherapies for Life™ Victoria, Australia. Hofmann A has received honoraria and/or travel support for professional services related to programme implementation, health economic analyses, outcomes research and lecturing from Vifor Fresenius Medical Care Renal Pharma Ltd , Vifor Pharma AG, Switzerland. Kim YW has received a research grant from Vifor Pharma and JW Pharmaceutical and travel support from Vifor Pharma. Spahn DR’s academic department is receiving grant support from the Swiss National Science Foundation, Berne, Switzerland; the Ministry of Health (Gesundheitsdirektion) of the Canton of Zurich, Switzerland for Highly Specialized Medicine; the Swiss Society of Anesthesiology and Reanimation (SGAR), Berne, Switzerland; the Swiss Foundation for Anesthesia Research, Zurich, Switzerland; CSL Behring, Berne, Switzerland; Vifor SA, Villars-sur-Glâne, Switzerland. Spahn DR is co-chair of the ABC-Trauma Faculty, sponsored by unrestricted educational grants from Novo Nordisk Health Care AG, Zurich, Switzerland; CSL Behring GmbH, Marburg, Germany; LFB Biomédicaments, Courtaboeuf Cedex, France; and Octapharma AG, Lachen, Switzerland. Spahn DR has received honoraria or travel support for consulting or lecturing from: Danube University of Krems, Austria; US Department of Defense, Washington, USA; European Society of Anesthesiology, Brussels, Belgium; Korean Society for Patient Blood Management, Seoul, Korea; Korean Society of Anesthesiologists, Seoul, Korea; Baxter AG, Volketswil, Switzerland; Baxter S.p.A., Roma, Italy; Bayer AG, Zürich, Switzerland; Bayer Pharma AG, Berlin, Germany; B Braun Melsungen AG, Melsungen, Germany; Boehringer Ingelheim GmbH, Basel, Switzerland; Bristol-Myers-Squibb, Rueil-Malmaison Cedex, France, and Baar, Switzerland; CSL Behring GmbH, Hattersheim am Main, Germany, and Berne, Switzerland; Celgene International II Sàrl, Couvet, Switzerland; Curacyte AG, Munich, Germany; Daiichi Sankyo AG, Thalwil, Switzerland; GlaxoSmithKline GmbH & Co KG, Hamburg, Germany; Haemonetics, Braintree, MA, USA; Instrumentation Laboratory (Werfen), Bedford, MA, USA; LFB Biomédicaments, Courtaboeuf Cedex, France; Merck Sharp & Dohme, Kenilworth, New Jersey, USA; Octapharma AG, Lachen, Switzerland; Organon AG, Pfäffikon/SZ, Switzerland; PAION Deutschland GmbH, Aachen, Germany; Pharmacosmos A/S, Holbaek, Denmark; Photonics Healthcare B.V., Utrecht, Netherlands; Roche Diagnostics International Ltd, Reinach, Switzerland; Roche Pharma AG, Reinach, Switzerland; Sarstedt AG & Co, Sevelen, Switzerland, and Nümbrecht, Germany; Schering-Plough International, Inc, Kenilworth, New Jersey, USA; Tem International GmbH, Munich, Germany; Verum Diagnostica GmbH, Munich, Germany; Vifor Pharma, Munich, Germany, Vienna, Austria, and Villars-sur-Glâne, Switzerland; and Vifor (International) AG, St Gallen, Switzerland. Lasocki S has received consultancy fees from Vifor Pharma and hospice and travel support from Sandoz.
The authors also acknowledge editorial and manuscript-drafting support funded by Vifor Pharma Asia-Pacific, provided by Sen-Kwan Tay and Geraldine Toh, Tech Observer Asia-Pacific Pte Ltd; and would like to thank Sze Min Loh, Vifor Pharma Asia-Pacific, for critical reading and discussion.
REFERENCES
- 1.GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries 1990-2015:a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kassebaum NJ, Jasrasaria R, Naghavi M, et al. A systematic analysis of global anemia burden from 1990 to 2010. Blood. 2014;123:615–24. doi: 10.1182/blood-2013-06-508325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. [Accessed October 20 2017]. Available at:https://www.who.int/vmnis/indicators/haemoglobin/en/
- 4.Camaschella C. Iron-deficiency anemia. N Engl J Med. 2015;372:1832–43. doi: 10.1056/NEJMra1401038. [DOI] [PubMed] [Google Scholar]
- 5.Browning RM, Trentino K, Nathan EA, Hashemi N Western Australian Patient Blood Management Program. Preoperative anaemia is common in patients undergoing major gynaecological surgery and is associated with a fivefold increased risk of transfusion. Aust N Z J Obstet Gynaecol. 2012;52:455–9. doi: 10.1111/j.1479-828X.2012.01478.x. [DOI] [PubMed] [Google Scholar]
- 6.Kassebaum NJ GBD 2013 Anemia Collaborators. The global burden of anemia. Hematol Oncol Clin North Am. 2016;30:247–308. doi: 10.1016/j.hoc.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Lee JO, Lee JH, Ahn S, et al. Prevalence and risk factors for iron deficiency anemia in the Korean population:results of the fifth Korea National Health and Nutrition Examination Survey. J Korean Med Sci. 2014;29:224–9. doi: 10.3346/jkms.2014.29.2.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sim YE, Wee HE, Ang AL, et al. Prevalence of preoperative anemia, abnormal mean corpuscular volume and red cell distribution width among surgical patients in Singapore, and their influence on one year mortality. PLoS One. 2017;12:e0182543. doi: 10.1371/journal.pone.0182543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Blood safety:key global fact and figures in 2011. [Accessed October 20 2017]. Available at:https://www.who.int/worldblooddonorday/media/who_blood_safety_factsheet_2011.pdf .
- 10.Schantz-Dunn J, M N. The use of blood in obstetrics and gynecology in the developing world. Rev Obstet Gynecol. 2011;4:86–91. [PMC free article] [PubMed] [Google Scholar]
- 11.Garraud O, Filho LA, Laperche S, Tayou-Tagny C, Pozzetto B. The infectious risks in blood transfusion as of today - A no black and white situation. Presse Med. 2016;45(7-8 Pt 2):e303–11. doi: 10.1016/j.lpm.2016.06.022. [DOI] [PubMed] [Google Scholar]
- 12.Farmer SL, Towler SC, Leahy MF, Hofmann A. Drivers for change:Western Australia Patient Blood Management Program (WA PBMP), World Health Assembly (WHA) and Advisory Committee on Blood Safety and Availability (ACBSA) Best Pract Res Clin Anaesthesiol. 2013;27:43–58. doi: 10.1016/j.bpa.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 13.Fowler AJ, Ahmad T, Phull MK, et al. Meta-analysis of the association between preoperative anaemia and mortality after surgery. Br J Surg. 2015;102:1314–24. doi: 10.1002/bjs.9861. [DOI] [PubMed] [Google Scholar]
- 14.Abdullah HR, Sim YE, Hao Y, et al. Association between preoperative anaemia with length of hospital stay among patients undergoing primary total knee arthroplasty in Singapore:a single-centre retrospective study. BMJ Open. 2017;7:e016403. doi: 10.1136/bmjopen-2017-016403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abdullah HR, Sim YE, Sim YT, et al. Preoperative Red Cell Distribution Width and 30-day mortality in older patients undergoing non-cardiac surgery:a retrospective cohort observational study. Sci Rep. 2018;8:6226. doi: 10.1038/s41598-018-24556-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baron DM, Hochrieser H, Posch M, et al. European Surgical Outcomes Study (EuSOS) group for Trials Groups of European Society of Intensive Care Medicine;European Society of Anaesthesiology. Preoperative anaemia is associated with poor clinical outcome in non-cardiac surgery patients. Br J Anaesth. 2014;113:416–23. doi: 10.1093/bja/aeu098. [DOI] [PubMed] [Google Scholar]
- 17.Lasocki S, Krauspe R, von Heymann C, et al. PREPARE:the prevalence of perioperative anaemia and need for patient blood management in elective orthopaedic surgery:a multicentre, observational study. Eur J Anaesthesiol. 2015;32:160–7. doi: 10.1097/EJA.0000000000000202. [DOI] [PubMed] [Google Scholar]
- 18.Musallam KM, Tamim HM, Richards T, et al. Preoperative anaemia and postoperative outcomes in non-cardiac surgery:a retrospective cohort study. Lancet. 2011;378:1396–407. doi: 10.1016/S0140-6736(11)61381-0. [DOI] [PubMed] [Google Scholar]
- 19.Spahn DR. Anemia and patient blood management in hip and knee surgery:a systematic review of the literature. Anesthesiology. 2010;113:482–95. doi: 10.1097/ALN.0b013e3181e08e97. [DOI] [PubMed] [Google Scholar]
- 20.Isbister JP, Shander A, Spahn DR, et al. Adverse blood transfusion outcomes:establishing causation. Transfus Med Rev. 2011;25:89–101. doi: 10.1016/j.tmrv.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 21.Spahn DR, Goodnough LT. Alternatives to blood transfusion. Lancet. 2013;381:1855–65. doi: 10.1016/S0140-6736(13)60808-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Isbister JP. The three-pillar matrix of patient blood management--an overview. Best Pract Res Clin Anaesthesiol. 2013;27:69–84. doi: 10.1016/j.bpa.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 23.63rd World Health Assembly. Resolution WHA63.12:Availability, safety and quality of blood products. 2010. May 21, [Accessed August 15 2018]. Available at:http://apps.who.int/gb/ebwha/pdf_files/WHA63/A63_R12-en.pdf .
- 24.National Blood Authority Australia. National Standard for Blood and Blood Products Safety and Quality. [Accessed August 16 2017]. Available at:https://www.blood.gov.au/national-standard .
- 25.Leahy MF, Roberts H, Mukhtar SA, et al. Western Australian Patient Blood Management Program. A pragmatic approach to embedding patient blood management in a tertiary hospital. Transfusion. 2014;54:1133–45. doi: 10.1111/trf.12362. [DOI] [PubMed] [Google Scholar]
- 26.Leahy MF, Hofmann A, Towler S, et al. Improved outcomes and reduced costs associated with a health-system-wide patient blood management program:a retrospective observational study in four major adult tertiary-care hospitals. Transfusion. 2017;57:1347–58. doi: 10.1111/trf.14006. [DOI] [PubMed] [Google Scholar]
- 27.Klein AA, Arnold P, Bingham RM, et al. AAGBI guidelines:the use of blood components and their alternatives 2016. Anaesthesia. 2016;71:829–42. doi: 10.1111/anae.13489. [DOI] [PubMed] [Google Scholar]
- 28.Baron DM, Metnitz PG, Fellinger T, et al. Evaluation of clinical practice in perioperative patient blood management. Br J Anaesth. 2016;117:610–6. doi: 10.1093/bja/aew308. [DOI] [PubMed] [Google Scholar]
- 29.Van der Linden P, Hardy JF. Implementation of patient blood management remains extremely variable in Europe and Canada:the NATA benchmark project:an observational study. Eur J Anaesthesiol. 2016;33:913–21. doi: 10.1097/EJA.0000000000000519. [DOI] [PubMed] [Google Scholar]
- 30.Avni T, Bieber A, Grossman A, et al. The safety of intravenous iron preparations:systematic review and meta-analysis. Mayo Clin Proc. 2015;90:12–23. doi: 10.1016/j.mayocp.2014.10.007. [DOI] [PubMed] [Google Scholar]
- 31.Bhandari S. Beyond efficacy and safety:the need for convenient and cost-effective iron therapy in health care. NDT Plus. 2011;4(Suppl 1):i14–i19. doi: 10.1093/ndtplus/sfr044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Auerbach M, Deloughery T. Single-dose intravenous iron for iron deficiency:a new paradigm. Hematology Am Soc Hematol Educ Program. 2016;2016:57–66. doi: 10.1182/asheducation-2016.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Auerbach M, Goodnough LT, Shander A. Iron:the new advances in therapy. Best Pract Res Clin Anaesthesiol. 2013;27:131–40. doi: 10.1016/j.bpa.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 34.Rognoni C, Venturini S, Meregaglia M, Marmifero M, Tarricone R. Efficacy and safety of ferric carboxymaltose and other formulations in iron-deficient patients:a systematic review and network meta-analysis of randomised controlled trials. Clin Drug Investig. 2016;36:177–94. doi: 10.1007/s40261-015-0361-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chertow GM, Mason PD, Vaage-Nilsen O, Ahlmén J. Update on adverse drug events associated with parenteral iron. Nephrol Dial Transplant. 2006;21:378–82. doi: 10.1093/ndt/gfi253. [DOI] [PubMed] [Google Scholar]
- 36.Khalafallah AA, Yan C, Al-Badri R, et al. Intravenous ferric carboxymaltose versus standard care in the management of postoperative anaemia:a prospective, open-label, randomised controlled trial. Lancet Haematol. 2016;3:e415–25. doi: 10.1016/S2352-3026(16)30078-3. [DOI] [PubMed] [Google Scholar]
- 37.Rineau E, Chaudet A, Chassier C, Bizot P, Lasocki S. Implementing a blood management protocol during the entire perioperative period allows a reduction in transfusion rate in major orthopedic surgery:a before-after study. Transfusion. 2016;56:673–81. doi: 10.1111/trf.13468. [DOI] [PubMed] [Google Scholar]
- 38.Froessler B, Palm P, Weber I, et al. The important role for intravenous iron in perioperative patient blood management in major abdominal surgery:a randomized controlled trial. Ann Surg. 2016;264:41–6. doi: 10.1097/SLA.0000000000001646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Calleja JL, Delgado S, del Val A, et al. Ferric carboxymaltose reduces transfusions and hospital stay in patients with colon cancer and anemia. Int J Colorectal Dis. 2016;31:543–51. doi: 10.1007/s00384-015-2461-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gross I, Seifert B, Hofmann A, Spahn DR. Patient blood management in cardiac surgery results in fewer transfusions and better outcome. Transfusion. 2015;55:1075–81. doi: 10.1111/trf.12946. [DOI] [PubMed] [Google Scholar]
- 41.Muñoz M, Gómez-Ramirez S, Cuenca J, et al. Very-short-term perioperative intravenous iron administration and postoperative outcome in major orthopedic surgery:a pooled analysis of observational data from 2547 patients. Transfusion. 2014;54:289–99. doi: 10.1111/trf.12195. [DOI] [PubMed] [Google Scholar]
- 42.Litton E, Baker S, et al. I RONMAN nvestigators. Intravenous iron or placebo for anaemia in intensive care:the IRONMAN multicentre randomized blinded trial:a randomized trial of IV iron in critical illness. Intensive Care Med. 2016;42:1715–22. doi: 10.1007/s00134-016-4465-6. [DOI] [PubMed] [Google Scholar]
- 43.Mbanya D. Barriers and enablers to introducing comprehensive patient blood management in the hospital. Biologicals. 2012;40:205–8. doi: 10.1016/j.biologicals.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 44.Australian Commission on Safety and Quality in Healthcare. The National Patient Blood Management Collaborative. [Accessed August 16 2016]. Available at:https://www.safetyandquality.gov.au/national-priorities/pbm-collaborative/
- 45.Ministry of Health Singapore Population and vital statistics. [Accessed August 16 2017]. Available at:https://www.moh.gov.sg/resources-statistics/singapore-health-facts/population-and-vital-statistics .
- 46.Lee ES, Kim MJ, Park BR, et al. Avoiding unnecessary blood transfusions in women with profound anaemia. Aust N Z J Obstet Gynaecol. 2015;55:262–7. doi: 10.1111/ajo.12329. [DOI] [PubMed] [Google Scholar]
- 47.Na HS, Shin SY, Hwang JY, et al. Effects of intravenous iron combined with low-dose recombinant human erythropoietin on transfusion requirements in iron-deficient patients undergoing bilateral total knee replacement arthroplasty. Transfusion. 2011;51:118–24. doi: 10.1111/j.1537-2995.2010.02783.x. [DOI] [PubMed] [Google Scholar]
- 48.Yoo YC, Shim JK, Kim JC, et al. Effect of single recombinant human erythropoietin injection on transfusion requirements in preoperatively anemic patients undergoing valvular heart surgery. Anesthesiology. 2011;115:929–37. doi: 10.1097/ALN.0b013e318232004b. [DOI] [PubMed] [Google Scholar]
- 49.Yoon HM, Kim YW, Nam BH, et al. Intravenous iron supplementation may be superior to observation in acute isovolemic anemia after gastrectomy for cancer. World J Gastroenterol. 2014;20:1852–7. doi: 10.3748/wjg.v20.i7.1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Muñoz M, Acheson AG, Auerbach M, et al. International consensus statement on the peri-operative management of anaemia and iron deficiency. Anaesthesia. 2017;72:233–47. doi: 10.1111/anae.13773. [DOI] [PubMed] [Google Scholar]
- 51.Mehra T, Seifert B, Bravo-Reiter S, et al. Implementation of a patient blood management monitoring and feedback program significantly reduces transfusions and costs. Transfusion. 2015;55:2807–15. doi: 10.1111/trf.13260. [DOI] [PubMed] [Google Scholar]
- 52.Ong DEH, Hadi F, Stevens V. Health economic evaluation comparing IV iron ferric carboxymaltose, iron sucrose and blood transfusion for treatment of patients with iron deficiency anemia (IDA) in Singapore. Value Health. 2014;17:A784. doi: 10.1016/j.jval.2014.08.395. [DOI] [PubMed] [Google Scholar]
- 53.Lim EA, Sohn HS, Lee H, Choi SE. Cost-utility of ferric carboxymaltose (Ferinject®) for iron-deficiency anemia patients with chronic heart failure in South Korea. Cost Eff Resour Alloc. 2014;12:19. doi: 10.1186/1478-7547-12-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hofmann A, Ozawa S, Farrugia A, Farmer SL, Shander A. Economic considerations on transfusion medicine and patient blood management. Best Pract Res Clin Anaesthesiol. 2013;27:59–68. doi: 10.1016/j.bpa.2013.02.001. [DOI] [PubMed] [Google Scholar]


