Abstract
A 48-year-old woman presented with chronic right heel pain and paraesthesia over the foot. Magnetic resonance imaging of the right foot demonstrated isolated atrophy of the abductor digiti minimi. A diagnosis of Baxter’s neuropathy was made and the patient was managed successfully via surgical release. We describe the clinical and radiological features of Baxter’s neuropathy and, with brief examples, outline other causes of chronic heel pain.
Keywords: abductor digiti minimi, Baxter’s nerve, inferior calcaneal nerve, nerve entrapment, plantar fasciitis
CASE PRESENTATION
A 48-year-old woman presented with chronic right heel pain of two months’ duration that had responded poorly to physiotherapy and conservative measures. Clinical assessment revealed exquisite tenderness over the medial calcaneal tuberosity as well as paraesthesia over the sole of the forefoot. Relative weakness of the abductor digiti minimi (ADM) was elicited. The Achilles tendon, alignment of the hindfoot, and the longitudinal arches were assessed to be normal. Magnetic resonance (MR) imaging of the right foot was performed. What do the MR images (Figs. 1 & 2) and lateral radiograph (Fig. 3) of the right foot show?
Fig. 1.
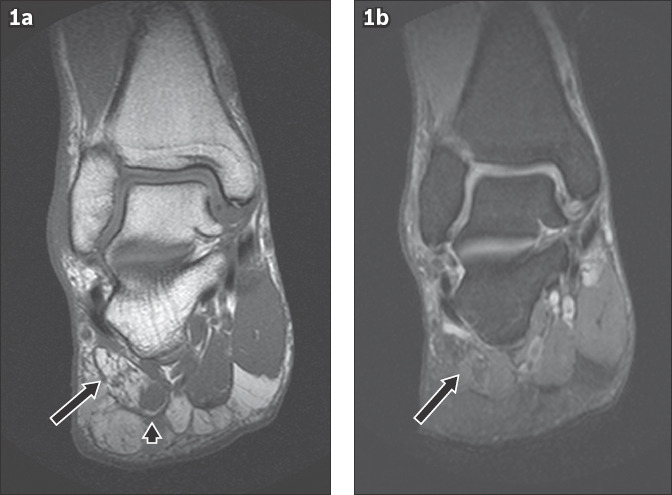
(a) Coronal T1-weighted and (b) T2-weighted fat-suppressed images of the right foot.
Fig. 2.
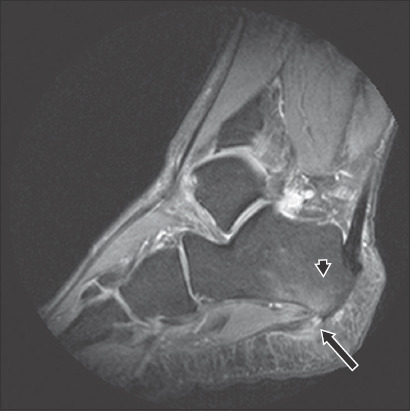
Sagittal T2-weighted fat-suppressed image of the right foot.
Fig. 3.

Lateral radiograph of the foot.
IMAGE INTERPRETATION
Coronal T1-weighted sequence shows isolated atrophy and fatty infiltration of the ADM (arrow, Fig. 1), with only the medial portion of the muscle belly retaining normal muscle architecture (arrowhead). There is faint muscle oedema on the corresponding coronal T2-weighted fat-suppressed (FS) sequence (Fig. 1b). The findings are compatible with chronic denervation change in the ADM. Sagittal T2-weighted FS sequence shows a thickened, oedematous plantar fascia with partial tear (arrow, Fig. 2) and reactive marrow oedema in the calcaneal tuberosity (arrowhead, Fig. 2). A prominent plantar calcaneal spur is noted on the lateral radiograph (Fig. 3).
DIAGNOSIS
Baxter’s neuropathy.
CLINICAL COURSE
The patient initially underwent conservative treatment with footwear modification and physiotherapy, followed by corticosteroid injection. However, the substantial clinical symptoms were largely refractory despite treatment. The decision was made to proceed with open tarsal tunnel release of Baxter’s nerve. Intraoperatively, the Baxter’s nerve was found to be tightly compressed as it crossed the abductor hallucis muscle belly, and it was released to as far distally as possible. The patient was then kept on a plaster of Paris cast for two weeks. This was then converted to a long Aircast boot, and physiotherapy was commenced. The patient eventually achieved good symptomatic relief and return to normal function.
DISCUSSION
Baxter’s neuropathy is a compressive neuropathy of the inferior calcaneal nerve (ICN). It presents clinically with a mixed sensory-motor pattern. Recalcitrant heel pain is typical, with maximal tenderness over the medial border of the calcaneus where the entrapment occurs. Clinical features overlap with those of plantar fasciitis, which is often concurrently present. The ICN entrapment, estimated to involve 20% of patients suffering from chronic heel pain,(1) eventually leads to motor impairment with loss of resistive strength of the ADM. Consideration should be given to this diagnosis if symptoms persist for longer than six months without improvement despite conservative treatment.
The ICN arises as the first branch of the lateral plantar nerve. The origin of the ICN is always distal to the origin of the medial calcaneal nerve.(2) The ICN first descends with the lateral plantar nerve covered medially by the posterior tibial vein. It then takes an inferior, anterior and lateral course, passing between the upper edge of the abductor hallucis and medial edge of the quadratus plantae. The nerve then continues between the quadratus plantae above and the flexor digitorum brevis below. Finally, the nerve crosses over the lateral edge of the quadratus plantae to run just anterior to the medial calcaneal tuberosity before terminating in the proximal portion of the ADM.(2-4) Along its course, the ICN also gives off branches to the calcaneal periosteum, long plantar ligament and, occasionally, the flexor digitorum brevis and quadratus plantae.(3) Two possible sites of nerve entrapment have been described.(4-6) The first site is where the nerve crosses the deep fascia of the abductor hallucis between the abductor hallucis and medial caudal margin of the quadratus plantae; contributory factors include altered biomechanics such as pes cavus or excessive pronation as well as muscle hypertrophy. The second is where the nerve passes just anterior to the medial calcaneal tuberosity. Contributory factors include plantar fasciitis or a plantar calcaneal spur.
MR imaging is the imaging modality of choice for the evaluation of Baxter’s neuropathy, and its imaging hallmark is denervation changes in the ADM. Acute to subacute denervation manifests as muscle oedema, which is best evaluated on fluid-sensitive sequences such as T2-weighted or proton-density FS and short-tau inversion recovery sequences. With chronicity, frank muscle atrophy and fatty infiltration develop; these changes are best assessed using a T1-weighted sequence. Another important role of imaging is in the detection of commonly associated features such as plantar fasciitis, prominent plantar calcaneal spur and hindfoot deformities, which may be considered for treatment.
The mainstay of treatment consists of conservative measures such as stretching, splints/orthoses, nonsteroidal anti-inflammatory drugs and local steroid injections.(7,8) The majority of patients respond well to conservative measures, failing which other measures such as extracorporeal shockwave therapy, radiofrequency nerve ablation and surgical release may be considered.(9) Operative treatment is generally reserved for symptoms that have failed a minimum of six months of conservative measures, with several studies reporting excellent outcomes following targeted surgical release of the ICN.(10,11)
Causes of heel pain are myriad and run the gamut of pathologies involving bone, enthesis, fascia and other soft tissues. Plantar fibromatosis is a known cause of chronic heel pain. A skilled clinician may be able to palpate the nodular deposits, but these are often small and may evade detection. MR imaging or ultrasonography is often employed to identify and confirm the diagnosis (Fig. 4). In the local context, gout is relatively prevalent in the local population and should be considered in cases of recalcitrant heel pain with no other conclusive identifiable cause. Dual-energy computed tomography has proven to be an effective problem-solving technique for both the referring clinician and radiologist for this condition by showing corresponding monosodium urate deposits in the afflicted region (Fig. 5). It is known that even small deposits can initiate a localised inflammatory response.(12) An important differential in cases of neuropathic heel pain is tarsal tunnel syndrome, in which clinical manifestations relate to compression of the posterior tibial nerve. These include paraesthesia and sensory deficits over the sole of the foot, usually concentrated over the posteromedial region. A positive Tinel sign may also be elicited over the tarsal tunnel. MR imaging facilitates the detection of compressive lesions within the tarsal tunnel (Fig. 6). Muscle denervation is less commonly encountered.(13)
Fig. 4.
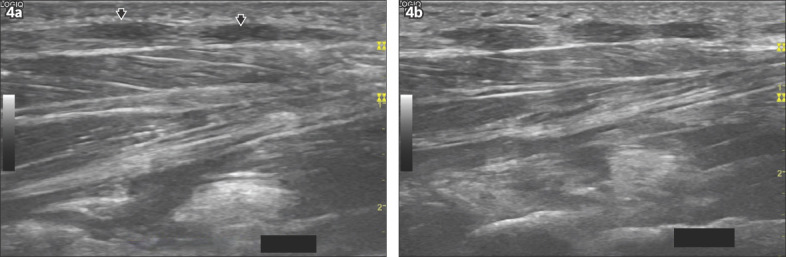
A 65-year-old man presented with chronic bilateral heel pain. US image of the (a) right and (b) left plantar fasciae shows multiple small circumscribed hypoechoic nodules (arrows) compatible with plantar fibromatosis.
Fig. 5.
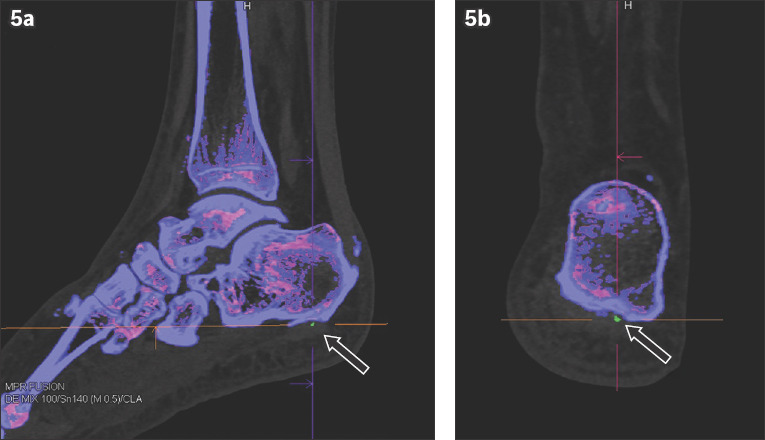
A 67-year-old man with a history of hyperuricaemia presented with chronic intermittent left heel pain. (a) Sagittal and (b) coronal post-processed dual-energy CT images show monosodium urate deposition, depicted in green, in the plantar fascia (arrows).
Fig. 6.
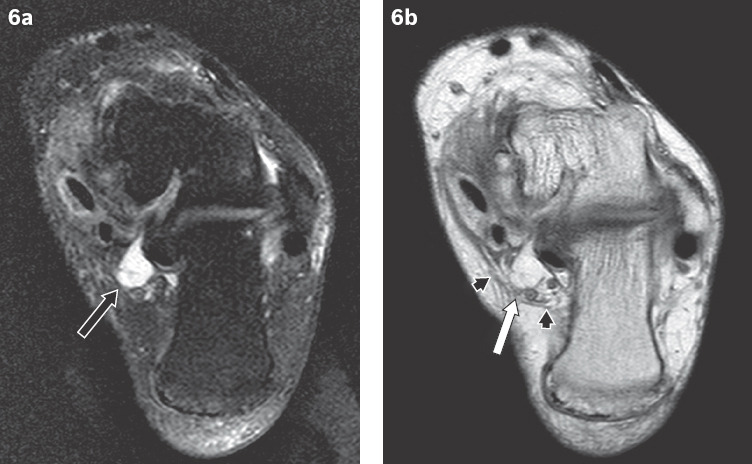
A 60-year-old woman presented with chronic left heel pain and paraesthesia over the sole of the foot. (a) T2-weighted fat-suppressed and (b) proton density-weighted axial images at the level of the tarsal tunnel show a ganglion cyst (black arrow) impinging on the tibial nerve (white arrow). The tarsal tunnel space is constrained by the flexor retinaculum (arrowheads).
In summary, although heel pain is usually managed conservatively, Baxter’s neuropathy should be considered in cases that are recalcitrant despite conservative treatment. MR imaging plays an important role in such situations by accurately characterising the disease pattern along with other associated pathologies, enabling optimised patient care and management.
REFERENCES
- 1.Shon LC, Easly ME. Chronic pain. In: Myerson M, editor. Foot and ankle disorders. Philadelphia, PA: WB Saunders; 2000. pp. 815–81. [Google Scholar]
- 2.Louisia S, Masquelet AC. The medial and inferior calcaneal nerves:an anatomic study. Surg Radiol Anat. 1999;21:169–73. doi: 10.1007/BF01630895. [DOI] [PubMed] [Google Scholar]
- 3.del Sol M, Olave E, Gabrielli C, Mandiola E, Prates JC. Innervation of the abductor digiti minimi muscle of the human foot:anatomical basis of the entrapment of the abductor digiti minimi nerve. Surg Radiol Anat. 2002;24:18–22. doi: 10.1007/s00276-002-0001-1. [DOI] [PubMed] [Google Scholar]
- 4.Recht MP, Grooff P, Ilaslan H, et al. Selective atrophy of the abductor digiti quinti:an MRI study. AJR Am J Roentgenol. 2007;189:W123–7. doi: 10.2214/AJR.07.2229. [DOI] [PubMed] [Google Scholar]
- 5.De Maeseneer M, Madani H, Lenchik L, et al. Normal anatomy and compression areas of nerves of the foot and ankle:US and MR imaging with anatomic correlation. Radiographics. 2015;35:1469–82. doi: 10.1148/rg.2015150028. [DOI] [PubMed] [Google Scholar]
- 6.Rodrigues RN, Lopes AA, Torres JM, et al. Compressive neuropathy of the first branch of the lateral plantar nerve:a study by magnetic resonance imaging. Radiol Bras. 2015;48:368–72. doi: 10.1590/0100-3984.2013.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosenbaum AJ, DiPreta JA, Misener D. Plantar heel pain. Med Clin North Am. 2014;98:339–52. doi: 10.1016/j.mcna.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 8.Lui TH. Endoscopic decompression of the first branch of the lateral plantar nerve and release of the plantar aponeurosis for chronic heel pain. Arthrosc Tech. 2016;5:e589–94. doi: 10.1016/j.eats.2016.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thomas JL, Christensen JC, Kravitz SR, et al. The diagnosis and treatment of heel pain:a clinical practice guideline-revision 2010. J Foot Ankle Surg. 2010;49(3 Suppl):S1–19. doi: 10.1053/j.jfas.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 10.Baxter DE, Pfeffer GB. Treatment of chronic heel pain by surgical release of the first branch of the lateral plantar nerve. Clin Orthop Relat Res. 1992;279:229–36. [PubMed] [Google Scholar]
- 11.Watson TS, Anderson RB, Davis WH, Kiebzak GM. Distal tarsal tunnel release with partial plantar fasciotomy for chronic heel pain:an outcome analysis. Foot Ankle Int. 2002;23:530–7. doi: 10.1177/107110070202300610. [DOI] [PubMed] [Google Scholar]
- 12.Chou H, Chin TY, Peh WC. Dual-energy CT in gout - a review of current concepts and applications. J Med Radiat Sci. 2017;64:41–51. doi: 10.1002/jmrs.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Donovan A, Rosenberg ZS, Cavalcanti CF. MR imaging of entrapment neuropathies of the lower extremity Part 2. The knee, leg, ankle, and foot. Radiographics. 2010;30:1001–19. doi: 10.1148/rg.304095188. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


