Abstract
Objective:
The Australian federal government introduced new COVID-19 psychiatrist Medicare Benefits Schedule (MBS) telehealth items to assist with providing private specialist care. We investigate private psychiatrists’ uptake of video and telephone telehealth, as well as total (telehealth and face-to-face) consultations for Quarter 3 (July–September), 2020. We compare these to the same quarter in 2019.
Method:
MBS-item service data were extracted for COVID-19-psychiatrist video and telephone telehealth item numbers and compared with Quarter 3 (July–September), 2019, of face-to-face consultations for the whole of Australia.
Results:
The number of psychiatry consultations (telehealth and face-to-face) rose during the first wave of the pandemic in Quarter 3, 2020, by 14% compared to Quarter 3, 2019, with telehealth 43% of this total. Face-to-face consultations in Quarter 3, 2020 were only 64% of the comparative number of Quarter 3, 2019 consultations. Most telehealth involved short telephone consultations of ⩽15–30 min. Video consultations comprised 42% of total telehealth provision: these were for new patient assessments and longer consultations. These figures represent increased face-to-face consultation compared to Quarter 2, 2020, with substantial maintenance of telehealth consultations.
Conclusions:
Private psychiatrists continued using the new COVID-19 MBS telehealth items for Quarter 3, 2020 to increase the number of patient care contacts in the context of decreased face-to-face consultations compared to 2019, but increased face-to-face consultations compared to Quarter 2, 2020.
Keywords: COVID-19, telepsychiatry, telehealth, psychiatrist, private practice
The first confirmed case of COVID-19 in Australia was identified late January 2020. Cases rose rapidly such that on 20 March, the federal government closed the international border, followed shortly by lockdowns at state level. Although case numbers levelled and then fell, there was a second wave of infections in Victoria mid-June, necessitating a further lockdown. In response to concerns about possible mental health consequences, the federal government introduced COVID-19 Medicare Benefits Schedule (MBS) item numbers for video and telephone psychiatric consultations.1 This is because private psychiatric practice is mainly office-based, providing 50%–60% of specialist psychiatric care.2 Consequently, telehealth was rapidly adopted.3 Therefore, we analyse the ongoing usage of telehealth by psychiatrists during the third quarter of COVID-19 public health measures in Australia to inform contemporaneous mental health policy. We determined the amount of telehealth as well as face-to-face office-based consultations during Quarter 3, 2020, compared to the equivalent pre-COVID-19 period of Quarter 3, 2019, which was of predominantly face-to-face consultations. We also compared Quarter 3, 2020 with previously published data from Quarter 2, 2020.3
Methods
MBS item service data were extracted from the Services Australia Medicare Item Reports (http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp) for psychiatrist practice office-based face-to-face consultations, COVID-19 video and telephone telehealth consultations for Quarter 3 (July–September) 2020, in Microsoft Excel format, and transferred to a purpose-built Excel database and analysed (totals, proportions, percentages) using Excel (Microsoft Office Home and Student 2019, Microsoft Corporation, Seattle, WA, USA). We extracted, as a baseline comparator, face-to-face consultation data from Quarter 3 (July–September), 2019 (Table 1).
Table 1.
Overall Data Summary
| Face-to-Face | F2F 2020 | Video Item | VideoTele2020 | Telephone Item | TeleTele2020 | F2F 2019 | F2F20/19 | Vid+Tel2020 | Vid+Tel+F2F2020 | Vid/TotalTeleh2020 | TotalTelheal+F2F2020/F2F2019 | Telehealth2020/TotalTelehealthF2F2020 | TotalTelehealth2020/F2F2019 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 289 | 38 | 92434 | 24 | 92474 | 1 | 94 | 40.43 | 25 | 63 | 96.00 | 67.02 | 39.68 | 26.60 |
| 291 | 6583 | 92435 | 1907 | 92475 | 1850 | 11,013 | 59.77 | 3757 | 10,340 | 50.76 | 93.89 | 36.33 | 34.11 |
| 293 | 1375 | 92436 | 254 | 92476 | 750 | 2269 | 60.60 | 1004 | 2379 | 25.30 | 104.85 | 42.20 | 44.25 |
| 296 | 21,606 | 92437 | 5531 | 92477 | 1629 | 32,149 | 67.21 | 7160 | 28,766 | 77.25 | 89.48 | 24.89 | 22.27 |
| 300 | 3969 | 91827 | 1466 | 91837 | 8867 | 6639 | 59.78 | 10,333 | 14,302 | 14.19 | 215.42 | 72.25 | 155.64 |
| 302 | 35,405 | 91828 | 9256 | 91838 | 31,562 | 56,196 | 63.00 | 40,818 | 76,223 | 22.68 | 135.64 | 53.55 | 72.64 |
| 304 | 104,702 | 91829 | 27,037 | 91839 | 53,592 | 157,698 | 66.39 | 80,629 | 185,331 | 33.53 | 117.52 | 43.51 | 51.13 |
| 306 | 89,968 | 91830 | 45,853 | 91840 | 30,962 | 151,558 | 59.36 | 76,815 | 166,783 | 59.69 | 110.05 | 46.06 | 50.68 |
| 308 | 5437 | 91831 | 1278 | 91841 | 1237 | 8531 | 63.73 | 2515 | 7952 | 50.82 | 93.21 | 31.63 | 29.48 |
| 342 | 6621 | 92455 | 830 | 92495 | 43 | 10,355 | 63.94 | 873 | 7494 | 95.07 | 72.37 | 11.65 | 8.43 |
| 344 | 34 | 92456 | 20 | 92496 | 8 | 131 | 25.95 | 28 | 62 | 71.43 | 47.33 | 45.16 | 21.37 |
| 346 | 584 | 92457 | 350 | 92497 | 80 | 1273 | 45.88 | 430 | 1014 | 81.40 | 79.65 | 42.41 | 33.78 |
| 348 | 6467 | 92458 | 754 | 92498 | 1105 | 8118 | 79.66 | 1859 | 8326 | 40.56 | 102.56 | 22.33 | 22.90 |
| 350 | 4894 | 92459 | 495 | 92499 | 424 | 5440 | 89.96 | 919 | 5813 | 53.86 | 106.86 | 15.81 | 16.89 |
| 352 | 9255 | 92460 | 1052 | 92500 | 2570 | 11,394 | 81.23 | 3622 | 12,877 | 29.04 | 113.02 | 28.13 | 31.79 |
| TOTAL | 296,938 | 96,107 | 134,680 | 462,858 | 64.15 | 230,787 | 527,725 | 41.64 | 114.01 | 43.73 | 49.86 |
Note. Face-to-Face: Psychiatrist Office-Based Face-to-Face MBS-Item-Number:
• New patient assessment items are telehealth items for new patients for an individual psychiatrist corresponding to face-to-face consultations 289 (assessment of new patient with autism), 291 (comprehensive assessment and 12-month treatment plan), 293 (review of 291 plan), 296 (new patient for a psychiatrist or patient not seen in last two calendar years).
• Standard office-based consultation items are time-based items for current and ongoing patients for an individual psychiatrist, corresponding to face-to-face consultations: 300 (<15 min), 302 (15–30 min), 304 (30–45 min), 306 (45–75 min) and 308 (75+ min).
• Group psychotherapy provided by a psychiatrist item equivalents: 342 (group psychotherapy 1 h plus of 2–9 unrelated patients), 344 (group psychotherapy 1 h plus of family of 3 patients) and 346 (group psychotherapy 1 h plus of family group of 2 patients).
• Items for interview of a person other than the patient, by a psychiatrist, for the care of the patient: 348 (initial diagnostic evaluation, 20–45 min), 350 (initial diagnostic evaluation, 45+ min) and 352 (20+ min, not exceeding 4 consultations).
Totals and percentages were calculated for combined video and telephone telehealth as a proportion Quarter 3, 2019 face-to-face consultations, as well as the combined total of video–telephone telehealth and face-to-face consultations for Quarter 3, 2020. Video telehealth consultations were calculated as a percentage of total of video–telephone telehealth consultations for Quarter 3, 2020. The sum total of video–telephone telehealth and face-to-face consultations for Quarter 3, 2020 was calculated as a percentage of Quarter 3, 2019 face-to-face consultations:
• F2F 2020: Face-to-face consultations for Quarter 3, 2020: (count)
• Video Item: Psychiatrist video telehealth MBS item number
• VideoTele2020: Psychiatrist video telehealth MBS item number services (count)
Telephone Item: Psychiatrist telephone telehealth MBS item number
• TeleTele2020: Psychiatrist telephone telehealth MBS item number services (count)
• F2F 2019: Face-to-face consultations for Quarter 3, 2019 (count)
• F2F20/19%: [(F2F 2020)] divided by (F2F 2019)] multiplied by 100: (percentage)
• Vid+Tel2020: [(VideoTele2020)] plus (TeleTele2020]: (count)
• Vid+Tel+F2F2020: [(VideoTele2020) plus (TeleTele2020) plus (F2F 2020)]: (count)
• Vid/TotalTeleh2020%: {VideoTele2020 divided by Vid+Tel2020} multiplied by 100: (percentage)
• TotalTelheal+F2F2020/F2F2019%: [(Vid+Tel+F2F2020) divided by (F2F 2019)] multiplied by 100: (percentage)
• Telehealth2020/TotalTelehealthF2F2020%: [(Vid+Tel2020) divided by (Vid+Tel+F2F2020)] multiplied by 100: (percentage)
• TotalTelehealth2020/F2F2019%: [(Vid+Tel2020) divided by (F2F 2019)] multiplied by 100: (percentage)
• Telehealth2020/TotalTelehealth+F2F2020%: [(Vid+Tel2020) divided by (Vid+Tel+F2F2020)] multiplied by 100: (percentage).
Results
Overall findings for Quarter 3, 2020
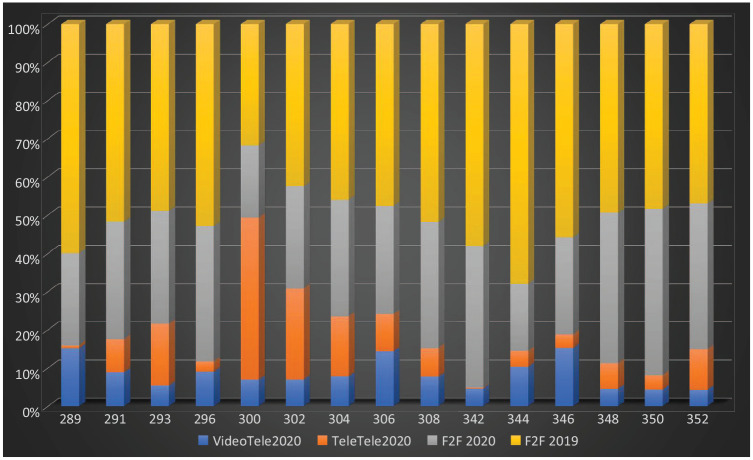
For Quarter 3, 2020, the total combined use of telehealth and face-to-face consultations increased by 14% compared to the equivalent pre-COVID-19 period in 2019 (Table 1 and Figure 1).
Figure 1.
Quarter 3 individual psychiatrist MBS item usage by modality and year.
Note. MBS-equivalent item numbers on y-axis; percentage of total consultations on x-axis; VideoTele2020: Video telehealth count; TeleTele2020: Telephone telehealth count; F2F2020: Face-to-face consultations for Quarter 3, 2020: (count); F2F 2019: Face-to-face consultations for Quarter 3, 2019 (count).
However, this increase masked ongoing reduction in face-to-face consultations, which were only 64% of those in the equivalent quarter of 2019. When used, face-to-face consultations were most frequently used for specific new patient for individual psychiatrist assessments (Items 289, 291, 293, 296) and longer consultations for previously seen, ongoing patients for an individual psychiatrist ⩾30 min (Items 304, 306, 308).
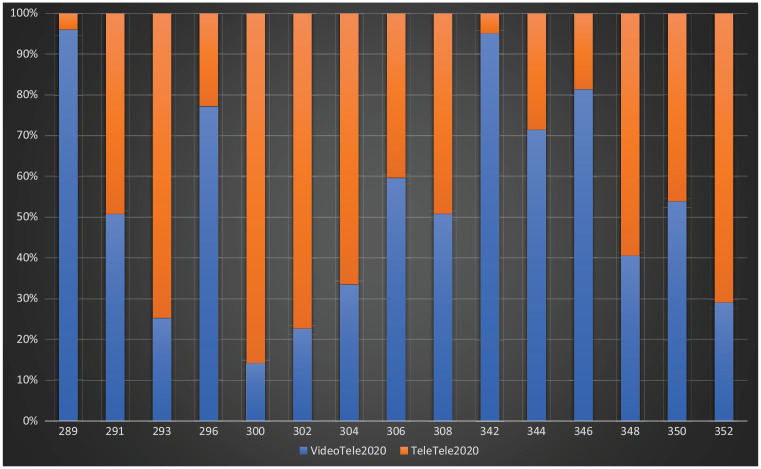
Video and telephone telehealth constituted 43% of the combined total of telehealth and face-to-face consultation for Quarter 3, 2020 (Figure 1). Telephone telehealth was predominantly used for shorter consultations (⩽15–30 min) with correspondingly greater video telehealth usage in longer consultations (⩾30–75 min) (Figure 2). The decrease in telehealth usage corresponds with the increase in face-to-face consultations, with an increase in video telehealth for longer consultations perhaps due to increased familiarity with video meeting platforms. Telephone telehealth remained prominent, likely due to patient and psychiatrist preferences for shorter consultations, obviating the need for transit time and travel to appointments.
Figure 2.
Quarter 3, 2020 video versus telephone telehealth.
Note. MBS-equivalent item numbers on y-axis; percentage of total consultations on x-axis; VideoTele: Video telehealth consultations; TeleTele: Telephone telehealth consultations.
COVID-19-psychiatrist-MBS-telehealth-item usage
New patient assessment for individual psychiatrist telehealth items
Specific MBS telehealth-equivalent items for assessment of a new patient for an individual psychiatrist were rarely used at 22%–44% of the combined total of (telehealth and face-to-face) consultations for Quarter 3, 2019 (Table 1; Figures 1–2).
For new patient assessments for an individual psychiatrist:
Telehealth new patient assessments for autism spectrum disorders (289 equivalents) were 27% of the pre-COVID-19 Quarter 3, 2019 face-to-face consultations in the same quarter of 2019, with video telehealth used in 96% of these consultations, representing a large increase in usage of video telehealth, compared to Quarter 2, 2020.3
Telehealth new patient assessment and 12-month treatment plans (291 equivalents) were 34% of 2019 face-to-face consultations, with video telehealth used in 51% of telehealth consultations representing an increased usage of video telehealth, compared to Quarter 2, 2020.3
Telehealth follow-up assessment of previously new patient seen for a 12-month treatment plan (293 equivalents – patients previously seen using a 291 equivalent) were 44% of 2019 face-to-face consultations, with video telehealth used in 25% of these consultations.
Telehealth new patient assessment items without the requirement for a 12-month treatment plan (296 equivalents) were 22% of 2019 face-to-face consultations, with video telehealth used in 77% of these consultations.
The combined total of (telehealth and face-to-face) new patient assessments for Quarter 3, 2020 was commensurate with 2019 face-to-face consultations, from the lowest of 67% for assessment for autism (289) to 89%–104% for new assessments and reviews (291, 293, 296).
Standard office-based consultations psychiatrist telehealth items
For MBS telehealth-equivalent items to time-based office consultations for previously seen and ongoing patients of an individual psychiatrist, the majority of the overall increase in telehealth consultations comprised item 300 equivalents, that is, consultations <15 min, representing an 55% increase above the 2019 face-to-face consultations. For 300-equivalent telehealth consultations, >86% were via telephone (Table 1; Figures 1–2).
For time-based consultations of previously seen and ongoing patients of individual psychiatrists:
Telehealth for 15–30 min (302 equivalents) were ⩾72% of the face-to-face consultations for Quarter 3, 2019. Of these consultations, 78% were by telephone.
Telehealth for 30–45 min (304 equivalents) were 51% of the face-to-face consultations for 2019, with video used in 33% of consultations.
Telehealth for 45–75 min (306 equivalents) were 51% of the face-to-face consultations for 2019 and use of video was 60% of all telehealth.
Telehealth for 75 min plus (308 equivalents) were 29% of the face-to-face consultations for 2019, with video used in 51% of telehealth consultations.
Telehealth consultations – interview of a person other than a patient to provide ongoing care of a patient – (348, 350, 352 equivalents) were used for 23%–32% compared to the face-to-face consultations for 2019, with video used in 29%–54% of telehealth consultations.
Fifteen-to-thirty-minute telehealth consultations (300–302 equivalents) represented the majority of telehealth usage. Less telehealth was used for 30–75 min (304–308 equivalents) consultations. Shorter consultations are used to provide urgent care as quantified in telephone telehealth consultations. Video telehealth may be more effective for longer consultations involving assessment, management and psychological therapy.
The combined total of (telehealth and face-to-face) standard office-based consultations for Quarter 3, 2020 equalled/exceeded Quarter 3, 2019 consultations, from the lowest of 93% for >75 min (308) to 110%–215% for items 300–306.
Group psychotherapy psychiatrist telehealth items
Group psychotherapy telehealth consultations remained little used, likely because face-to-face consultations, were preferred for psychotherapy (Table 1; Figures 1 and 2). The combined total of (telehealth and face-to-face) group psychotherapy for Quarter 3, 2020 was between 47% and 80% of Quarter 3, 2019 face-to-face psychotherapy consultations.
Comparison to Quarter 2, 2020 data
The 14% increase in face-to-face and telehealth consultations from Quarter 3 of 2019 to that of 2020 was identical to the increase in Quarter 2, 2020 relative to the respective 2019 quarters.3 However, relative proportions of face-to-face and telehealth consultations were different. The ratio of face-to-face consultations from Quarter 3 of 2020 to that of 2019 (64%) was greater than that from Quarter 2 of the same years (56%).3 This may be partially explained with the end of the first wave and lockdowns of the COVID-19 pandemic in Australia, with the exception of the Victorian second wave (warranting further investigation). By contrast, video and telephone telehealth use was less with comparable proportions of 43% and 51%, respectively.3
As in Quarter 2, 2020, face-to-face consultations were generally preferred for new patient assessment items in Quarter 3, 2020, and when telehealth was used, increasing video telehealth was used, likely to establish empathy and rapport more effectively for new patients.3 The combined total of (telehealth and face-to-face) new patient assessments were commensurate with Quarter 2, 2020, and Quarter 2, 2019.3
In comparison to Quarter 2, 2020 data,3 Quarter 3 results show a relative increase in face-to-face consultation, while there is maintenance of telephone telehealth for short consultations and increasing use of video telehealth for longer consultations.
Group psychotherapy telehealth was little used, similar to Quarter 2, 2020.3
Discussion
Psychiatrist MBS telehealth services have formed an important part of mental healthcare during Quarter 3, 2020. This resulted in a 14% increase in the overall level of service (telehealth and face-to-face combined) compared to face-to-face-office-based consultations in Quarter 3, 2019. This increase is similar to that seen in the second quarter of 2020 compared to the same period in 2019.3 Higher numbers of services might have resulted from a combination of: COVID-19-related distress, shorter telehealth consultations, as well as the limited capacity for expansion of services by private psychiatrists due to existing caseload.
Telephone telehealth remains predominant for shorter consultations (⩽15–30 min) as in Quarter 2, 2020. Provision of in-depth care during new patient assessment, as well as for ongoing patients, interview of a person other than a patient, and longer consultations (⩾30–75 min) increasingly involved more video telehealth, perhaps reflecting increasing experience and confidence with telehealth technology. Overall, face-to-face consultations increased in Quarter 3, 2020 compared to Quarter 2, 2020, likely reflecting the nationally improving COVID-19 situation (with the exception of Victoria’s second wave) and a consequent return to face-to-face appointments for longer consultations and continued use of telehealth for shorter appointments.
Implications for future private psychiatric care
These Quarter 3, 2020 results, together with those from Quarter 2, 2020,3 show that the private practice system adapted rapidly in Australia, mirroring the US experience.4 These adaptations may reduce emergency department attendance, increase the care of isolated patients and create opportunities for telehealth-enhanced shared care.5 Sensitivity to cultural, health and socioeconomic disparities is also needed to avoid inequities in access.5 Patients and psychiatrists, while still preferring face-to-face interaction, appreciate the complementary effectiveness, accessibility and convenience of telehealth, with reduced opportunity costs for consultations.6 The particular usefulness of shorter telephone telehealth consultations has been demonstrated during COVID-19.
Limitations
COVID-19-psychiatrist-telehealth usage needs to be cautiously interpreted, due to jurisdictional variations in private practice. Phased introduction of COVID-19-psychiatrist-telehealth-items and restrictions to bulk billing until April 20, 2020 are likely to have limited usage by private psychiatrists, in Quarter 2, 2020, due to income reduction, and thus encouraged maintenance of face-to-face consultations, with a tailing-off effect in Quarter 3, 2020.
Conclusions
Future research should investigate the relative proportions of newly referred and existing patients on the face-to-face and telehealth groups, as well as their demographic details such as age, gender and geographical distribution. These data should be supplemented by information on service outcomes, satisfaction with services and patient/psychiatrist consultation preferences.
Ongoing use of COVID-19-psychiatrist-MBS-telehealth-items, by patients and practitioners, beyond the first wave of the pandemic, indicates their effectiveness, complementary to face-to-face care. Furthermore, the Productivity Commission Report on Mental Health recommends making permanent the COVID-19-MBS-telehealth-consultation-items.7
Footnotes
Disclosure: The authors report no conflict of interest. The authors alone are responsible for the content and writing of the paper.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iDs: Jeffrey C.L. Looi  https://orcid.org/0000-0003-3351-6911
https://orcid.org/0000-0003-3351-6911
Stephen Allison  https://orcid.org/0000-0002-9264-5310
https://orcid.org/0000-0002-9264-5310
Rebecca Reay  https://orcid.org/0000-0001-9497-5842
https://orcid.org/0000-0001-9497-5842
Stephen R. Kisely  https://orcid.org/0000-0003-4021-2924
https://orcid.org/0000-0003-4021-2924
Contributor Information
Jeffrey CL Looi, Academic Unit of Psychiatry and Addiction Medicine, Australian National University Medical School, Canberra Hospital, Canberra, ACT, Australia; Private Psychiatry, Canberra, ACT, Australia.
Stephen Allison, College of Medicine and Public Health, Flinders University, Adelaide, SA, Australia.
Tarun Bastiampillai, College of Medicine and Public Health, Flinders University, Adelaide, SA, Australia; Department of Psychiatry, Monash University, Clayton, VIC, Australia.
William Pring, Monash University, VIC, Australia; Centre for Mental Health Education and Research at Delmont Private Hospital, Melbourne, VIC, Australia; Private Psychiatry, Melbourne, VIC, Australia.
Rebecca Reay, Academic Unit of Psychiatry and Addiction Medicine, Australian National University Medical School, Canberra Hospital, Canberra, ACT, Australia; Private Practice, Canberra, ACT, Australia.
Stephen R Kisely, School of Medicine, The University of Queensland, Princess Alexandra Hospital, Woolloongabba, Brisbane, QLD, Australia; Departments of Psychiatry, Community Health and Epidemiology, Dalhousie University, Halifax, Nova Scotia, Canada.
References
- 1. Department_of_Health. Australians embrace telehealth to save lives during COVID-19, https://www.health.gov.au/ministers/the-hon-greg-hunt-mp/media/australians-embrace-telehealth-to-save-lives-during-covid-19 (accessed 17 June 2020).
- 2. Keks NA, Hope J, Pring W, et al. Characteristics, diagnoses, illness course and risk profiles of inpatients admitted for at least 21 days to an Australian private psychiatric hospital. Australas Psychiatry 2019; 27: 25–31. [DOI] [PubMed] [Google Scholar]
- 3. Looi JCL, Allison S, Bastiampillai T, et al. Australian private practice metropolitan telepsychiatry during the Covid-19 pandemic: analysis of Quarter 2, 2020 usage of new MBS-telehealth-item psychiatrist services. Australas Psychiatry. In Press. [DOI] [PMC free article] [PubMed]
- 4. Yellowlees P, Nakagawa K, Pakyurek M, et al. Rapid conversion of an outpatient psychiatric clinic to a 100% virtual telepsychiatry clinic in response to COVID-19. Psychiatr Serv 2020; 71: 749–752. [DOI] [PubMed] [Google Scholar]
- 5. Kannarkat JT, Smith NN, McLeod-Bryant SA. Mobilization of telepsychiatry in response to COVID-19-moving toward 21(st) century access to care. Adm Policy Ment Health 2020; 47: 489–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Reay R, Looi JCL, Keightley P. Telehealth mental health services during COVID-19: summary of evidence and clinical practice. Australas Psychiatry 2020; 28: 514–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Productivity_Commission. Mental Health - Report No. 95. Canberra, ACT, Australia, 2020. [Google Scholar]