Key Points
Question
What are the real-world outcomes for Medicare patients with metastatic cancer receiving recently approved oncology drugs and how do they compare with pivotal clinical trial outcomes?
Findings
In this retrospective cohort study, outcomes were compared between clinical trial participants and treated Medicare patients across 22 cancer drugs approved by the US Food and Drug Administration for 29 indications. Median duration of therapy and overall survival among treated Medicare patients were generally shorter than among trial participants, and dose reductions were common among Medicare patients.
Meaning
Pivotal clinical trials may provide inadequate data for the purpose of clinical decision-making among Medicare beneficiaries with advanced cancer.
Abstract
Importance
A lack of generalizability of pivotal cancer clinical trial data to treatment of older adults with Medicare could affect therapeutic decision-making in clinical practice.
Objective
To evaluate the differences in survival, duration of therapy, and treatment patterns between clinical trial patients and older adults with Medicare receiving cancer drugs for metastatic solid cancers in usual practice.
Design, Setting, and Participants
This retrospective cohort study, performed from May 1, 2018, to August 30, 2020, used the linked Surveillance, Epidemiology, and End Results (SEER) program and Medicare database to examine sequential US Food and Drug Administration (FDA)–approved cancer drug indications (2008-2013) for locally advanced or metastatic solid tumors to assess whether pivotal trials reflect the outcomes of Medicare patients with cancer treated in usual practice.
Exposures
Treatment with FDA-approved cancer drugs for metastatic solid cancers in pivotal clinical trials and in the SEER-Medicare database.
Main Outcomes and Measures
Overall survival, duration of treatment, and dose reductions among trial participants and treated Medicare patients.
Results
A total of 11 828 trial participants (mean age, 61.8 years; 6718 [56.8%] male; and 7605 [64.3%] White) and 9178 SEER-Medicare patients (mean age, 72.7 years; 4800 [52.3%] male; and 7437 [81.0% White]) were compared. Twenty-nine indications for 22 cancer drugs were included. Median overall survival among Medicare patients was shorter than among patients in the clinical trial intervention arm for 28 of 29 indications (median difference, −6.3 months; range, −28.7 to 2.7 months). Median duration of therapy among Medicare patients was shorter for 23 of the 27 indications with data available (median difference, −1.9 months; range, −12.4 to 1.4 months). For 9 indications, there was information available regarding dose reductions in the package insert or trial publication. In all but 1 instance, dose reductions or single prescriptions were more common in the Medicare population compared with dose reductions among the clinical trial patients; for example, in the Medicare patients, 600 of 1032 (58.1%) received dose reduction or a single prescription and 172 of 1032 (16.7%) received a single prescription vs 734 of 3416 (21.5%) in the trial intervention arm. The exception was afatinib for non–small cell lung cancer: 34 of 71 (47.9%) received dose reduction or a single prescription and 15 of 71 (21.1%) received a single prescription among the Medicare patients vs 120 of 230 (52.2%) receiving dose reductions among the trial intervention group.
Conclusions and Relevance
In this cohort study, patients receiving Medicare who were treated with FDA-approved cancer drugs did not live as long as treated clinical trial participants and commonly received treatment modifications. This study suggests that cancer clinical data relevant to newly approved drugs lack generalizability to Medicare beneficiaries with cancer; therefore, these agents should be used with caution.
This cohort study evaluates the differences in survival, duration of therapy, and treatment patterns between clinical trial patients and older adults with Medicare receiving cancer drugs for metastatic solid cancers in usual practice.
Introduction
Differences between clinical trial participants and the broader patient population they are intended to represent can impair the generalizability of study results.1,2,3,4,5,6 Elderly, minority, poor, and chronically ill patients, for instance, are often underrepresented in cancer clinical trials.7,8,9,10,11,12 Lack of generalizability of clinical trials for cancer drugs used to treat patients with metastatic cancers may be of particular concern. Such therapies tend to have modest efficacy and produce substantial toxic effects even in young, fit clinical trial participants. Thus, additional scrutiny is warranted when applying these trial data to patients at a higher risk of harm from therapy.13,14
Adults 65 years and older are projected to account for 70% of cancer diagnoses by 2030. Medicare, the US federal health insurance program for elderly and disabled people, provides coverage for more than 50 million older adults, including nearly 7.5 million with cancer. In 2018, more than 40% of prescription dispensations for oral cancer drugs used to treat metastatic cancers were to Medicare beneficiaries.15 However, trial representation of patients in this age group is routinely lower, and age disparities between trial participants and the incident disease population is widening.16,17,18
Adequate power for subgroup analyses is needed for clinical trial results to be generalizable. Although this is not the same as representativeness—the extent to which a clinical trial cohort reflects the underlying disease population—improving the representation of older patients could increase the sample size sufficiently to perform these subgroup analyses needed for scientific inference. Given that older patients may experience more toxic effects when receiving cancer treatments, inadequate generalizability may be of clinical consequence.19
Prior research20 suggests that outcomes of cancer treatment differ between clinical studies and patients treated in usual clinical practice. Sanoff et al21 found that patients receiving sorafenib for advanced hepatocellular carcinoma had shorter survival than their clinical trial counterparts (median survival, 3 vs 10.3 months). Khozin et al22 also found a survival deficit among patients with metastatic non–small cell lung cancer (NSCLC) treated with nivolumab or pembrolizumab (median survival, 8 vs 9.2-12.2 months). Schmidinger et al,23 however, found that patients receiving pazopanib for advanced renal cell carcinoma in everyday practice lived longer than individuals in the pivotal clinical trial (median, 29.9 vs 22.9 months).
Using the Surveillance, Epidemiology, and End Results (SEER)–Medicare database, we conducted a study aimed to examine the generalizability of pivotal cancer clinical trial data. First, we compared the survival of Medicare patients treated with new drugs with that among pivotal clinical trial participants. Second, we examined whether the duration of treatment differed between Medicare patients and pivotal clinical trial participants. Third, we assessed the frequency of early discontinuation of drug use and dose reductions among Medicare patients treated with new drugs. We did not assess the incremental survival benefit of newly approved cancer drugs among Medicare patients.
Methods
This retrospective cohort study was conducted from May 1, 2018, to August 30, 2020, using the linked SEER-Medicare database. The study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline. Given that the SEER database contains deidentified data, informed consent was not possible, and the study was approved as exempt research by the institutional review board at Memorial Sloan Kettering Cancer Center.
Approved Cancer Drug Indications
We abstracted sequential cancer drug approvals for metastatic and locally advanced indications without curative intent approved between January 1, 2008, and December 31, 2013, from the US Food and Drug Administration (FDA) Hematology/Oncology (Cancer) Approvals and Safety Notifications website24 (eFigure 1 in the Supplement). We only included drugs for which median overall survival in the intervention arm of the pivotal trial, defined as the trial cited on the package insert (the label) and the FDA approval announcement, was published in a peer-reviewed journal. Median duration of therapy, dose reductions, and age-specific survival results were recorded from the trial publication or FDA package insert when available.
Medicare Patient Outcomes
We identified patients in the SEER-Medicare database diagnosed with cancer between January 1, 2006, and December 31, 2015, whose disease type and stage matched the FDA indication and who received at least 1 dose of the relevant cancer drug via intravenous infusion or filled 1 prescription for oral therapy (eTable 1 in the Supplement). We did not further limit the patient population to those who met trial eligibility criteria because our goal was to study those treated in general. We assumed the presence of biomarkers when relevant because SEER does not routinely capture such information. SEER is a population-based cancer registry that covers 28% of the US population. Medicare claims capture health care use and date of death.25
Patients had stage IV disease at diagnosis unless the indication included patients with locally advanced disease not amenable to curative surgery or radiotherapy. In such cases, patients with stage III disease at diagnosis were included if they had no cancer-directed surgery and/or radiotherapy documented in the SEER-Medicare database. Treatment was determined from J codes in Medicare Part B for intravenous drugs and generic and brand names in Medicare Part D for oral drugs. Median duration of therapy was measured from the date of first fill to the end of the days supplied of the last fill for oral drugs and from the first to last date of drug administration, unless the trial duration of therapy was reported in cycles, for the intravenous drugs. If so, we approximated number of cycles in the SEER-Medicare database and converted to months of therapy for more accurate comparison (eTable 2 in the Supplement). We restricted the sample to patients with continuous enrollment in Medicare Parts A and B for 6 months before and after diagnosis or until death or end of follow-up. More than 99% of patients receiving oral therapy in our analysis had continuous Medicare Part D enrollment.
Statistical Analysis
We included drug indications for which 30 or more SEER-Medicare patients met eligibility criteria. We compared age by regressing the mean age of patients in the SEER-Medicare database (weighted by sample size) against the mean age in the intervention arm of the pivotal trial because variance was not available for the trial population. A test of proportions was used to examine significant differences in race/ethnicity and sex composition. Statistical significance was defined as a 2-sided P ≤ .05.
Kaplan-Meier survival analyses were used to calculate median overall survival (censoring date December 31, 2016) and cancer-specific survival (censoring date December 31, 2015, the follow-up duration available in SEER-Medicare for this outcome) for SEER-Medicare patients. The burden of comorbidities for SEER-Medicare patients treated for each drug indication was calculated using the Charlson comorbidity index, modified to exclude cancer diagnoses, and categorized into 3 groups according to number of comorbidities (0-1, 2, and ≥3).26,27 For each drug indication, we calculated the absolute and relative differences between median overall survival and duration of therapy and summarized these differences by the median and range of values across indications. Overall survival estimates were also calculated among the subgroup of Medicare patients with 1 or no comorbidities (Charlson comorbidity index, 0-1).
If a prescription for an oral drug was filled for less than any of the approved doses for that indication and there was no later claim for a recommended dose, this was counted as a dose reduction. It is not possible to determine whether intravenous doses match those approved by the FDA.28 When a patient received only 1 prescription claim (for 30-90 days) or a single cycle of an intravenous drug, we labeled this a single treatment.
Results
A total of 11 828 trial participants (mean age, 61.8 years; 6718 [56.8%] male; 7605 [64.3%] White) and 9178 SEER-Medicare patients (mean age, 72.7 years; 4800 [52.3%] male; 7437 [81.0%] White) were compared. The median difference in age across indications was 11 years, with a range of 1 to 20 years. A total of 8031 treated SEER-Medicare patients (87.5%) across indications had 1 or no comorbidities.
A total of 47 drug indications across 33 drugs were approved by the FDA for metastatic or locally advanced, noncurative solid tumor treatment between 2008 and 2013 (eFigure 1 in the Supplement). Overall survival data for the intervention arm of the pivotal trial were available for 38 indications that represented 27 drugs. Of these, there were sufficient numbers of patients in SEER-Medicare to evaluate outcomes for 29 indications across 22 drugs (Table 1).
Table 1. Drug Indications Included in Analysis With Baseline Demographics Among SEER-Medicare Patients and Clinical Trial Intervention Arm.
| Year of FDA approval | Drug | FDA indicationa | SEER-Medicare/trial intervention arm | Modified Charlson comorbidity index, (range, 0-1), No. (%) | |||
|---|---|---|---|---|---|---|---|
| Sample size | Age, median (IQR)/ y | No. (%) | |||||
| White race | Male sex | ||||||
| 2008 | Pemetrexed | NSCLC, first line | 720/862 | 70 (67-73)/61 | 605 (84.0)/672 (78.0) | 382 (53.1)/603 (70.0) | 653 (90.7) |
| 2009 | Everolimus | Kidney cancer | 105/272 | 70 (66-75)/61 | 84 (80.0)/NR | 64 (61.0)/212 (77.9) | 86 (81.9) |
| 2009 | Pazopanib | Kidney cancer | 295/290 | 72 (67-78)/59 | 245 (83.0)/252 (86.9) | 189 (64.1)/197 (67.9) | 235 (79.7) |
| 2009 | Pemetrexed | NSCLC, maintenance | 2192/359 | 73 (69-77)/61 | 1885 (86.0)/337 (93.9) | 1096 (50.0)/201 (56.0) | 1901 (86.7) |
| 2010 | Erlotinib | NSCLC, maintenance | 208/438 | 71 (67-76)/60 | 156 (75.0)/368 (84.0) | 114 (54.8)/320 (73.1) | 165 (79.3) |
| 2010 | Cabazitaxel | Prostate cancer | 220/378 | 71 (68-76)/68 | 187 (85.0)/325 (86.0) | 220 (100.0)/378 (100.0) | 207 (94.1) |
| 2010 | Eribulin | Breast cancer | 43/508 | 68 (66-73)/55 | 36 (83.7)/472 (92.9) | 0/0 | 41 (95.3) |
| 2010 | Trastuzumab | Gastric cancer | 43/294 | 71 (66-74)/59 | 36 (83.7)/115 (39.1) | 32 (74.4)/226 (76.9) | 38 (88.3) |
| 2010 | Sipuleucel-T | Prostate cancer | 331/341 | 73 (69-79)/72 | 285 (86.1)/303 (88.5) | 331 (100.0)/341 (100.0) | 290 (87.6) |
| 2011 | Everolimus | Pancreatic NET | 53/207 | 72 (68-76)/58 | 47 (88.7)/155 (74.9) | 30 (56.6)/110 (53.1) | 45 (84.9) |
| 2011 | Abiraterone | Prostate cancer, prior docetaxel | 122/797 | 72 (68-75)/69 | 78.7 (96.0)/NR | 122 (100.0)/797 (100.0) | 115 (94.3) |
| 2011 | Vemurafenib | Melanoma | 84/337 | 70 (67-77)/56 | 46 (97.6)/199 (99.1) | 82 (54.8)/334 (59.1) | 75 (89.3) |
| 2011 | Cetuximab | Head and neck cancer | 55/222 | 68 (67-74)/56 | 87.3 (48)/NR | 83.4 (46)/89.2 (198) | 46 (83.6) |
| 2011 | Ipilimumab | Melanoma | 32/137 | 73 (68-78)/56 | 32 (100.0)/129 (94.2) | 22 (68.8)/84 (61.3) | 26 (81.3) |
| 2012 | Everolimus | Breast cancer | 97/485 | 71 (68-77)/62 | 79 (81.4)/359 (74.0) | 0/0 | 91 (93.8) |
| 2012 | Axitinib | Kidney cancer | 88/361 | 71 (67-76)/61 | 74 (84.0)/278 (77.0) | 60 (68.2)/264 (73.1) | 75 (85.2) |
| 2012 | Nab-paclitaxel | NSCLC | 179/521 | 75 (68-80)/60 | 141 (78.8)/417 (80.0) | 104 (58.1)/391 (75.0) | 145 (81.0) |
| 2012 | Enzalutamide | Prostate cancer | 215/800 | 72 (68-76)/69 | 215 (78.1)/800 (93.0) | 215 (100.0)/800 (100.0) | 192 (89.3) |
| 2012 | Abiraterone | Prostate cancer | 742/546 | 74 (69-80)/71 | 556 (74.9)/NR | 742 (100.0)/546 (100.0) | 621 (83.7) |
| 2012 | Regorafenib | Colorectal cancer | 295/505 | 70 (66-74)/61 | 224 (75.9)/394 (78.0) | 162 (54.9)/313 (61.9) | 270 (91.5) |
| 2012 | Cetuximab | Colorectal cancer | 280/316 | 70 (67-74)/61 | 227 (81.1)/NR | 174 (62.1)/196 (62.0) | 248 (88.6) |
| 2012 | Pertuzumab | Breast cancer | 88/402 | 70 (66-76)/54 | 67 (76.1)/245 (60.9) | 0/0 | 76 (86.4) |
| 2012 | Ziv-aflibercept | Colorectal cancer | 79/612 | 73 (68-76)/61 | 43 (67.1)/367 (90.0) | 53 (54.4)/551 (60.0) | 71 (89.9) |
| 2013 | Trastuzumab emtansine | Breast cancer | 53/495 | 71 (66-77)/53 | 43 (81.1)/356 (71.9) | 0 (0)/1 (0.2) | 48 (90.6) |
| 2013 | Dabrafenib | Melanoma | 51/187 | 73 (67-79)/53 | 50 (98.0)/187 (100) | 30 (58.8)/112 (59.9) | 44 (86.3) |
| 2013 | Nab-paclitaxel | Pancreatic cancer | 1019/431 | 73 (68-77)/62 | 866 (85.0)/379 (87.9) | 530 (52.0)/246 (57.1) | 853 (83.7) |
| 2013 | Afatinib | NSCLC | 71/230 | 77 (71-84)/62 | 51 (71.8)/62 (27.0) | 19 (26.8)/83 (36.1) | 64 (90.1) |
| 2013 | Erlotinib | NSCLC | 1032/86 | 77 (67-76)/65 | 65.0/90.7 | 299 (29.0)/28 (32.6) | 866 (83.9) |
| 2013 | Bevacizumab | Colorectal cancer | 386/409 | 71 (67-75)/63 | 305 (79.0)/NR | 216 (56.0)/266 (65.0) | 352 (91.2) |
Abbreviations: FDA, US Food and Drug Administration; IQR, interquartile range; nab, nanoparticle albumin-bound; NET, neuroendocrine tumor; NR, not reported in clinical trial publication, FDA package insert, or ClinicalTrials.gov; NSCLC, non–small cell lung cancer; SEER, Surveillance, Epidemiology, and End Results.
Complete FDA-approved indications are listed in eTable 1 in the Supplement.
For 28 of the 29 drug indications (22 drugs), the median survival among treated SEER-Medicare patients was shorter than among clinical trial participants receiving the same treatment for the same indication (14.0 vs 11.8 months) (Figure 1). The exception was pemetrexed for the first-line treatment of NSCLC. The median survival of Medicare patients was 59.9% of the survival of clinical trial patients, corresponding to a difference of 6.3 months at the median (range, −28.7 to 2.7 months). For 12 indications (41.4%), the median survival of SEER-Medicare patients was less than half the duration observed among patients in the clinical trial (median absolute difference, −11.2 months; range, −28.7 to −6.3 months). The median survival of Medicare patients with 1 or no comorbidities was 59.5% of the survival of clinical trial patients (median absolute difference, −6.7 months; range, −24.4 to 2.7 months) (eFigure 2 in the Supplement).
Figure 1. Median Overall Survival (95% CIs) Comparing Surveillance, Epidemiology, and End Results (SEER)–Medicare Patients and Clinical Trial Intervention Arm Participants Receiving the Same US Food and Drug Administration–Approved Cancer Drug for the Same Indication (2008-2013).
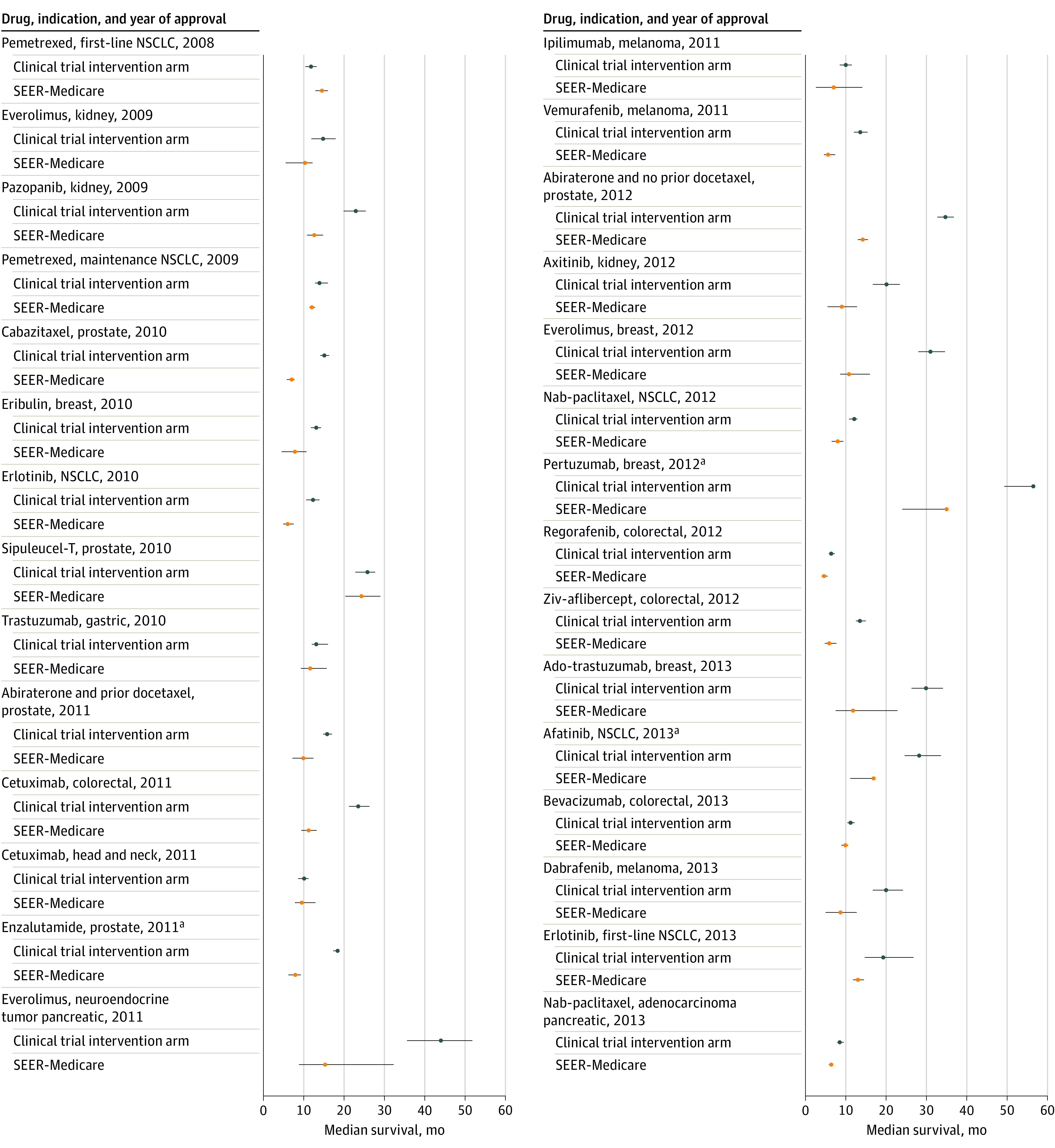
Nab indicates nanoparticle albumin-bound; NSCLC, non–small cell lung cancer.
aUpper confidence bound not met.
In SEER-Medicare (eTable 3 in the Supplement) across all indications, 8141 patient deaths (88.7%) were attributed to cancer (range, 78.5% to 100.0%). Only 6 of the 29 indications (5 drugs) reported age-specific survival in the trial publication or FDA package insert (eTable 4 in the Supplement). The median overall survival for older trial participants was similar to that for younger trial participants and longer than survival among patients in SEER-Medicare for 5 indications (4 drugs). It was similar for patients receiving cetuximab for head and neck cancer (median survival in trial among those ≥65 years of age, 9.1 months; median survival in SEER-Medicare group, 9.7 months).
There were 27 indications (21 drugs) for which median duration of therapy was available for the clinical trial participants in the trial publication or FDA package insert for comparison with Medicare beneficiaries, and it was shorter for Medicare beneficiaries in 23 of them (Figure 2). Median duration of therapy among Medicare patients was 59.0% of treatment duration for clinical trial patients across indications, for a difference of 1.9 months at the median (range, −12.4 to 1.4 months). Across all indications, 1725 SEER-Medicare patients (18.8%) received a single prescription or cycle, ranging from 1 patient (2.3%) (trastuzumab for gastric cancer) to 120 patients (40.7%) (regorafenib for colorectal cancer). Among Medicare patients, 1459 (42.2%) were dose reduced, ranging from 20 (16.4%) to 64 (66.0%) (Table 2) across the 14 oral drug indications (10 drugs) for which this outcome could be evaluated. For 9 of these indications, information was available regarding dose reductions in the package insert or trial publication. In all but 1 instance (afatinib for NSCLC: 34 of 71 [47.9%] receiving dose reduction or a single prescription and 15 of 71 [21.1%] receiving a single prescription in the Medicare patients vs 120 of 230 [52.2%] receiving dose reductions in the trial intervention arm), dose reductions or single prescriptions were more common in the Medicare population compared with dose reductions among the clinical trial patients (eg, 600 of 1032 [58.1%] receiving dose reduction or a single prescription and 172 of 1032 [16.7%] receiving a single prescription in the Medicare patients vs 734 of 3416 [21.5%] in the trial intervention arm) (Table 2). For erlotinib, 18 of 84 patients (21.4%) with first-time NSCLC had dose reduction.
Figure 2. Median Duration of Therapy (DOT) (Interquartile Ranges) Comparing Surveillance, Epidemiology, and End Results (SEER)–Medicare Patients and Clinical Trial Intervention Arm Participants Receiving the Same US Food and Drug Administration–Approved Cancer Drug for the Same Indication (2008-2013).
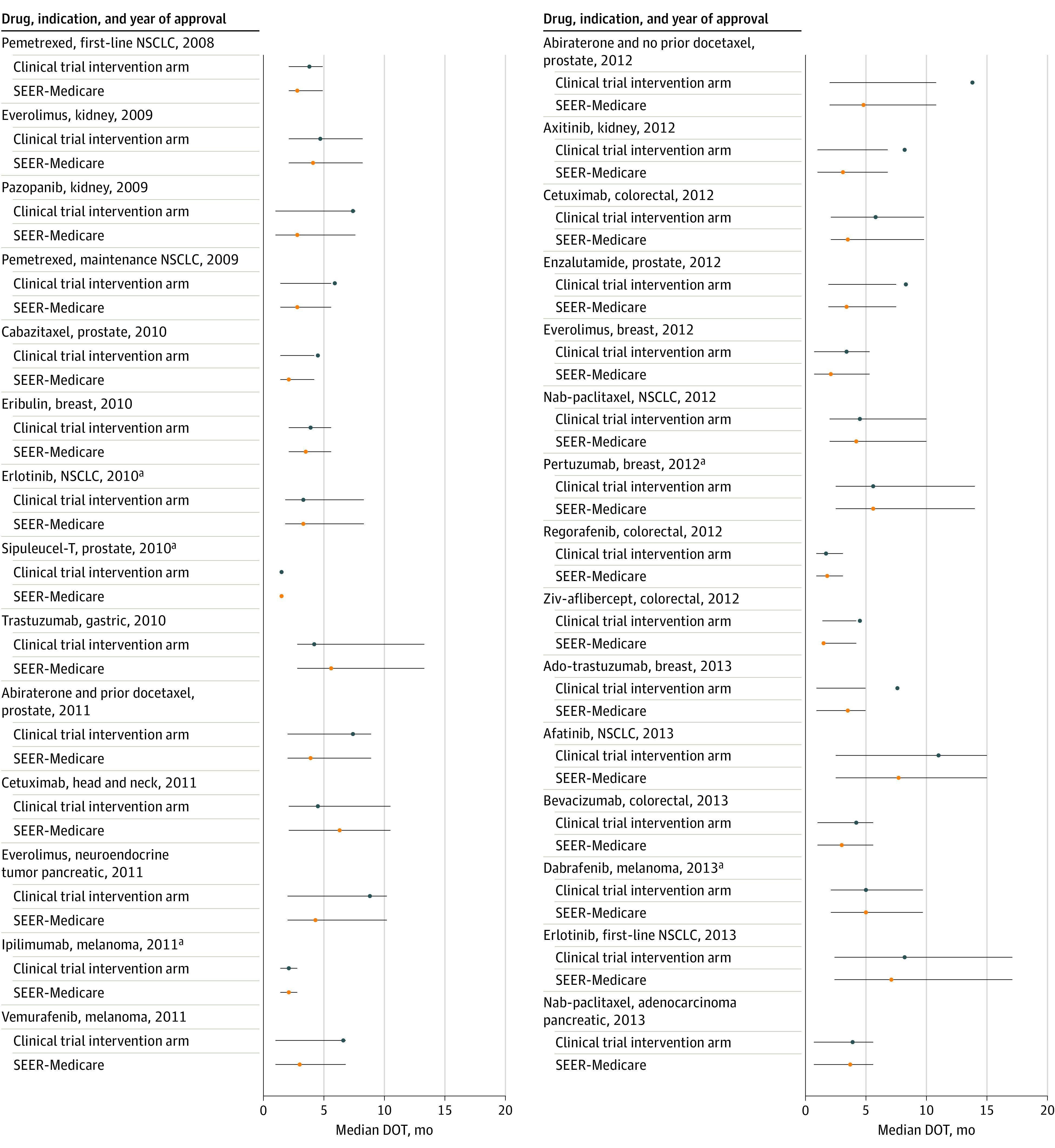
Nab indicates nanoparticle albumin-bound; NSCLC, non–small cell lung cancer.
aUpper confidence bound not met.
Table 2. Dose Reductions or Single Prescriptions Among SEER-Medicare Patients Who Received Oral Medicare Part D Drugs Compared With Dose Reductions in the Clinical Trial Intervention Arm.
| Drug, indication | SEER-Medicare arm, No./total No. (%) | Dose reductions in trial intervention arm, No./total No. (%) | |
|---|---|---|---|
| Dose reduction or single prescription | Single prescription | ||
| Everolimus, breast | 64/97 (66.0) | 22/97 (22.7) | NR |
| Axitinib, RCC | 37/88 (42.0) | 24/88 (27.3) | 121/359 (34.0) |
| Everolimus, RCC | 32/105 (30.5) | 19/105 (18.1) | NR |
| Pazopanib, RCC | 154/295 (52.2) | 89/295 (30.2) | 104/290 (36.0) |
| Erlotinib, NSCLC maintenance | 100/208 (48.2) | 43/208 (20.7) | 70/433 (16.0) |
| Everolimus, pancreatic NET | 26/53 (49.1) | 10/53 (18.9) | NR |
| Enzalutamide, CRPC | 51/215 (23.7) | 45/215 (20.9) | NR |
| Abiraterone, CRPC | 132/742 (17.8) | 111/742 (15.0) | 38/542 (7.0) |
| Abiraterone, CRPC with prior docetaxel | 20/122 (16.4) | 18/122 (14.8) | 23/791 (2.9) |
| Regorafenib, colorectal | 159/295 (53.9) | 120/295 (40.7) | 188/500 (38.0) |
| Vemurafenib, melanoma | 37/84 (44.0) | 32/84 (38.1) | NR |
| Afatinib, NSCLC | 34/71 (47.9) | 15/71 (21.1) | 120/230 (52.0) |
| Dabrafenib, melanoma | 19/51 (37.3) | 11/51 (21.6) | 52/187 (28.0) |
| Erlotinib, NSCLC first line | 600/1032 (58.2) | 172/1032 (16.7) | 18/84 (21.4) |
Abbreviations: CRPC, castration-resistant prostate cancer; NET, neuroendocrine tumor; NR, not reported in clinical trial publication, FDA package insert, or ClinicalTrials.gov; NSCLC, non–small cell lung cancer; RCC, renal cell carcinoma; SEER, Surveillance, Epidemiology, and End Results.
Discussion
This cohort study was conducted to evaluate the generalizability of pivotal trial data to Medicare beneficiaries treated in usual clinical practice. The median overall survival, duration of therapy, and treatment patterns were compared between Medicare patients treated with FDA-approved cancer drugs and the participants in the pivotal trials. With only 1 exception (afatanib), the median survival across drugs and indications was briefer for the Medicare patients, with a median absolute difference in survival of 6.3 months. Medicare patients received shorter durations of therapy than study participants, and sizeable percentages received only a single prescription or cycle (18.8%) or dose reductions (42.2%). The effectiveness or incremental survival benefit cannot be determined from these new treatments for Medicare patients because of the lack of a comparison group of patients who did not receive treatment and because this was not the aim of the study.
Several associated factors are likely to explain these differences. In the analysis, the mean age of Medicare patients receiving treatment exceeded the mean age of clinical trial participants by 11 years (73 vs 62 years). Advanced age is on average associated with frailty and a higher prevalence of comorbidities, which may heighten drug toxicity and reduce patients’ ability to tolerate cancer drugs.29 These factors may lead to earlier discontinuation of therapy, treatment interruptions, or suboptimal dosages, negatively impacting survival. Although this study found that Medicare beneficiaries received shorter durations of therapy than study participants, including a sizeable percentage receiving only a single prescription or cycle as well as dose reductions, this was likely not solely attributable to their age but also to other factors, including comorbidities, performance status, tumor prognostic factors, access to care, racial disparities, systemic discrimination, and other socioeconomic factors that could lead to differential treatment and outcomes in the Medicare population compared with clinical trial participants.
In the few trials in which age-specific survival was reported in the publication or FDA package insert, survival was generally similar between older and younger study participants, suggesting that age alone does not explain our findings. However, this result was only available in 6 (20.7%) of the pivotal trials included. Another reason why advanced age might be associated with poorer outcomes is that older patients die at higher rates from other causes. However, this study found that nearly 90% of deaths among SEER-Medicare patients were associated with cancer.
Beyond older age, comorbidities or illness from more advanced or aggressive cancer that impairs drug tolerability could explain why, among Medicare patients, therapies were routinely discontinued early, doses were reduced, or medication was given for a single prescription or cycle of therapy. Most patients in the Medicare cohort had mild or no comorbidities (87.5%), and only small changes in survival were noted when the analysis was limited to this subgroup. However, the modified Charlson comorbidity index, a weighted score based on chronic disease diagnostic codes, may not be associated with the typical measures of performance status in patients with advanced cancer, such as the Eastern Cooperative Oncology Group and Karnofsky performance status scores, which are not available in the SEER-Medicare database. Furthermore, intrinsic delays in the enrollment process can lead investigators to enroll trial patients with less aggressive disease and thus better prognosis. Patients are often excluded from trials if they are heavily pretreated or their disease is rapidly progressing. In usual practice, patients may receive approved drugs after other prior treatments, when they are sicker or closer to the end of life.
This study found that the median survival and duration of treatment of patients in cancer clinical trials was substantially longer than that of treated Medicare patients. Although possibly expected for reasons outlined, these findings suggest that pivotal trial data do not reflect the experience of Medicare patients treated in usual clinical practice. As a result, the risks vs benefits of treatment are difficult to surmise. In particular, understanding the influence of dose reductions and prescribing patterns on survival outcomes in Medicare beneficiaries is an area for further study. Avoiding subtherapeutic dosages without clear indication for dose reduction may be a modifiable intervention to improve survival in older Medicare patients with cancer; however, the optimal dosing strategy in older adults is poorly defined.30
This study may have implications for clinical trial design to improve the external validity of pivotal trials and regulatory decision-making to ensure that data for clinical prescribing in Medicare patients is informative. Broadening eligibility criteria might improve but cannot ensure the sample size required for generalizability of cancer clinical trial data.31 Allowances for a wider range of performance status, preexisting comorbidities, and organ dysfunction, however, would improve the characterization of toxic effects of treatment. The FDA released guidance to encourage researchers and sponsors to broaden eligibility criteria32; whether these changes are implemented remains to be seen.
The FDA could encourage pharmaceutical firms to design their pivotal trials in a manner that ensures availability of age-specific toxic effects, dosing, and efficacy data, which were inconsistently available in the published literature and often nonspecific in the FDA package inserts. The Institute of Medicine has suggested patent extensions for companies that pursue dedicated trials in older patients or those with comorbidities. These extensions are important for oncologic drugs because more than 40% of prescriptions in 2018 for oral cancer drugs included in this analysis are administered to Medicare patients.15
Real-world data can be used to generate additional information to help guide treatment decisions in understudied patients and could also be required by the FDA as part of postmarketing commitments. However, postapproval trials and mandatory surveillance studies are often underresourced and inconsistently performed.33,34,35 Regardless, evidence of poorer outcomes or increased toxic effects in specific subgroups could lead to a requirement for more formal phase 4 studies.
Limitations
This study has limitations. An important limitation is the lack of a comparator group of Medicare patients who did not receive the treatment being evaluated; therefore, any estimate of the relative survival benefit from these drugs among Medicare patients could not be determined. The generalizability of clinical trial outcomes to younger, non-Medicare patients could also not be assessed, and similar differences may be evident among these patients. Because of limitations of claims-based data, the role of such factors as age, comorbidities, and socioeconomic and demographic variables in the observed differences in clinical trial efficacy in Medicare patients cannot be quantified. This analysis was limited to patients with stage IV or noncurative stage III cancer at diagnosis because these patients can be reliably identified in the SEER database. Many of the pivotal trials also include participants with newly metastatic disease; however, this was unlikely to influence the study findings because the difference in prognosis among patients with recurrence vs stage IV disease at diagnosis is mixed,36,37 and stage IV diagnosis at presentation is common for cancers included in this analysis.38,39,40,41
Conclusions
Among Medicare patients with advanced solid cancers treated with FDA-approved drugs, median survival was shorter than that reported among clinical trial participants treated with the same drugs for all but 1 drug used for 1 indication. Many Medicare patients were also treated for only brief duration, had dose reductions, or received a single prescription or treatment cycle. These findings raise concerns regarding the generalizability of clinical trial data for treatment decision-making in Medicare patients. Furthermore, prescribing patterns in Medicare patients require additional scrutiny to ensure optimal dosing to avoid overtreatment or undertreatment in this population. Pivotal trials can be improved, and regulatory requirements could emphasize the importance of generating data relevant to the older patients who constitute an increasing number of all patients with cancer in the US.11
eFigure 1. Flow Diagram of Selection of Cancer Drug Indications
eFigure 2. Median Overall Survival With 95% Confidence Intervals Comparing SEER-Medicare Patients With Charlson Comorbidity Index 0-1 and the Clinical Trial Intervention Arm Participants Receiving the Same FDA Approved Cancer Drug for the Same Indication
eTable 1. SEER-Medicare Inclusion Criteria for Cohort Selection
eTable 2. Cycle Estimates for Intravenous Cancer Drugs Used to Calculate Duration of Therapy and/or Single Cycles
eTable 3. Median Cancer-Specific Survival and Percent Deaths Due to Cancer Among SEER-Medicare Patients, Censored 12/31/2015
eTable 4. Age-Specific Median Overall Survival or Hazard Ratios for Clinical Trial Intervention Arms
References
- 1.Elting LS, Cooksley C, Bekele BN, et al. . Generalizability of cancer clinical trial results: prognostic differences between participants and nonparticipants. Cancer. 2006;106(11):2452-2458. doi: 10.1002/cncr.21907 [DOI] [PubMed] [Google Scholar]
- 2.Clarey J, Kao SC, Clarke SJ, Vardy J. The eligibility of advanced non-small-cell lung cancer patients for targeted therapy clinical trials. Ann Oncol. 2012;23(5):1229-1233. doi: 10.1093/annonc/mdr443 [DOI] [PubMed] [Google Scholar]
- 3.Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: race-, sex-, and age-based disparities. JAMA. 2004;291(22):2720-2726. doi: 10.1001/jama.291.22.2720 [DOI] [PubMed] [Google Scholar]
- 4.Duma N, Vera Aguilera J, Paludo J, et al. . Representation of minorities and women in oncology clinical trials: review of the past 14 Years. J Oncol Pract. 2018;14(1):e1-e10. doi: 10.1200/JOP.2017.025288 [DOI] [PubMed] [Google Scholar]
- 5.Ford JG, Howerton MW, Lai GY, et al. . Barriers to recruiting underrepresented populations to cancer clinical trials: a systematic review. Cancer. 2008;112(2):228-242. doi: 10.1002/cncr.23157 [DOI] [PubMed] [Google Scholar]
- 6.Gross CP, Filardo G, Mayne ST, Krumholz HM. The impact of socioeconomic status and race on trial participation for older women with breast cancer. Cancer. 2005;103(3):483-491. doi: 10.1002/cncr.20792 [DOI] [PubMed] [Google Scholar]
- 7.Jin S, Pazdur R, Sridhara R. Re-evaluating eligibility criteria for oncology clinical trials: analysis of investigational New Drug Applications in 2015. J Clin Oncol. 2017;35(33):3745-3752. doi: 10.1200/JCO.2017.73.4186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lichtman SM, Harvey RD, Damiette Smit MA, et al. . Modernizing clinical trial eligibility criteria: recommendations of the American Society of Clinical Oncology–Friends of Cancer Research Organ Dysfunction, Prior or Concurrent Malignancy, and Comorbidities Working Group. J Clin Oncol. 2017;35(33):3753-3759. doi: 10.1200/JCO.2017.74.4102 [DOI] [PubMed] [Google Scholar]
- 9.Unger JM, Hershman DL, Fleury ME, Vaidya R. Association of patient comorbid conditions with cancer clinical trial participation. JAMA Oncol. 2019;5(3):326-333. doi: 10.1001/jamaoncol.2018.5953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh H, Kanapuru B, Smith C, et al. FDA analysis of enrollment of older adults in clinical trials for cancer drug registration: a 10-year experience by the U.S. Food and Drug Administration. J Clin Oncol. 2017;35(15 suppl):10009. doi: 10.1200/JCO.2017.35.15_suppl.10009 [DOI] [Google Scholar]
- 11.Smith BD, Smith GL, Hurria A, Hortobagyi GN, Buchholz TA. Future of cancer incidence in the United States: burdens upon an aging, changing nation. J Clin Oncol. 2009;27(17):2758-2765. doi: 10.1200/JCO.2008.20.8983 [DOI] [PubMed] [Google Scholar]
- 12.Baquet CR, Commiskey P, Daniel Mullins C, Mishra SI. Recruitment and participation in clinical trials: socio-demographic, rural/urban, and health care access predictors. Cancer Detect Prev. 2006;30(1):24-33. doi: 10.1016/j.cdp.2005.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mailankody S, Prasad V. Five years of cancer drug approvals: innovation, efficacy, and costs. JAMA Oncol. 2015;1(4):539-540. doi: 10.1001/jamaoncol.2015.0373 [DOI] [PubMed] [Google Scholar]
- 14.Widakowich C, de Castro G Jr, de Azambuja E, Dinh P, Awada A. Review: side effects of approved molecular targeted therapies in solid cancers. Oncologist. 2007;12(12):1443-1455. doi: 10.1634/theoncologist.12-12-1443 [DOI] [PubMed] [Google Scholar]
- 15.Biotech Dashboard: Industry Rx. Bloomberg terminal. Updated 2019. Accessed December 19, 2019. https://www.bloomberg.com/professional/solution/bloomberg-terminal
- 16.Freedman RA, Dockter TJ, Lafky JM, et al. . Promoting accrual of older patients with cancer to clinical trials: an alliance for clinical trials in oncology member survey (A171602). Oncologist. 2018;23(9):1016-1023. doi: 10.1634/theoncologist.2018-0033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dale W, Mohile SG, Eldadah BA, et al. ; Cancer and Aging Research Group . Biological, clinical, and psychosocial correlates at the interface of cancer and aging research. J Natl Cancer Inst. 2012;104(8):581-589. doi: 10.1093/jnci/djs145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ludmir EB, Mainwaring W, Lin TA, et al. . Factors associated with age disparities among cancer clinical trial participants. JAMA Oncol. 2019. doi: 10.1001/jamaoncol.2019.2055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muss HB, Berry DA, Cirrincione C, et al. ; Cancer and Leukemia Group B Experience . Toxicity of older and younger patients treated with adjuvant chemotherapy for node-positive breast cancer: the Cancer and Leukemia Group B Experience. J Clin Oncol. 2007;25(24):3699-3704. doi: 10.1200/JCO.2007.10.9710 [DOI] [PubMed] [Google Scholar]
- 20.Bird ST, Tian F, Flowers N, et al. . Idelalisib for treatment of relapsed follicular lymphoma and chronic lymphocytic leukemia: a comparison of treatment outcomes in clinical trial participants vs Medicare beneficiaries. JAMA Oncol. 2020;6(2):248-254. doi: 10.1001/jamaoncol.2019.3994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sanoff HK, Chang Y, Lund JL, O’Neil BH, Dusetzina SB. Sorafenib effectiveness in advanced hepatocellular carcinoma. Oncologist. 2016;21(9):1113-1120. doi: 10.1634/theoncologist.2015-0478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khozin S, Carson KR, Zhi J, et al. . Real-world outcomes of patients with metastatic non-small cell lung cancer treated with programmed cell death protein 1 inhibitors in the year following U.S. regulatory approval. Oncologist. 2019;24(5):648-656. doi: 10.1634/theoncologist.2018-0307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schmidinger M, Bamias A, Procopio G, et al. ; PRINCIPAL Study Group . Prospective observational study of pazopanib in patients with advanced renal cell carcinoma (PRINCIPAL study). Oncologist. 2019;24(4):491-497. doi: 10.1634/theoncologist.2018-0787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.US Food and Drug Administration. Hematology/Oncology (Cancer) Approvals and Safety Notifications. Accessed January 13, 2021. https://www.fda.gov/drugs/resources-information-approved-drugs/hematologyoncology-cancer-approvals-safety-notifications
- 25.Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF. Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care. 2002;40(8)(suppl):IV-3-IV-18. doi: 10.1097/00005650-200208001-00002 [DOI] [PubMed] [Google Scholar]
- 26.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613-619. doi: 10.1016/0895-4356(92)90133-8 [DOI] [PubMed] [Google Scholar]
- 27.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383. doi: 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 28.Bach PB, Conti RM, Muller RJ, Schnorr GC, Saltz LB. Overspending driven by oversized single dose vials of cancer drugs. BMJ. 2016;352:i788. doi: 10.1136/bmj.i788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Williams GR, Deal AM, Lund JL, et al. . Patient-reported comorbidity and survival in older adults with cancer. Oncologist. 2018;23(4):433-439. doi: 10.1634/theoncologist.2017-0404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Given B, Given CW. Older adults and cancer treatment. Cancer. 2008;113(12)(suppl):3505-3511. doi: 10.1002/cncr.23939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim ES, Bruinooge SS, Roberts S, et al. . Broadening eligibility criteria to make clinical trials more representative: American Society of Clinical Oncology and Friends of Cancer Research Joint Research Statement. J Clin Oncol. 2017;35(33):3737-3744. doi: 10.1200/JCO.2017.73.7916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.US Department of Health and Human Services, US Food and Drug Administration Enhancing the diversity of clinical trial populations—eligibility criteria, enrollment practices, and trial designs guidance for industry. November 20, 2020. Accessed December 1, 2020. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/enhancing-diversity-clinical-trial-populations-eligibility-criteria-enrollment-practices-and-trial
- 33.Vlahakes GJ The value of phase 4 clinical testing. N Engl J Med. 2006;354(4):413-415. doi: 10.1056/NEJMe058272 [DOI] [PubMed] [Google Scholar]
- 34.Suvarna V Consort 2010: a standard for reporting clinical trials revised anew? Perspect Clin Res. 2010;1(3):87-89. [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang X, Zhang Y, Ye X, Guo X, Zhang T, He J. Overview of phase IV clinical trials for postmarket drug safety surveillance: a status report from the ClinicalTrials.gov registry. BMJ Open. 2016;6(11):e010643. doi: 10.1136/bmjopen-2015-010643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Finianos A, Gupta K, Clark B, Simmens SJ, Aragon-Ching JB. Characterization of differences between prostate cancer patients presenting with de novo versus primary progressive metastatic disease. Clin Genitourin Cancer. 2017;S1558-7673(17)30247-1. [DOI] [PubMed] [Google Scholar]
- 37.Malmgren JA, Mayer M, Atwood MK, Kaplan HG. Differential presentation and survival of de novo and recurrent metastatic breast cancer over time: 1990-2010. Breast Cancer Res Treat. 2018;167(2):579-590. doi: 10.1007/s10549-017-4529-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Motzer RJ, Bander NH, Nanus DM. Renal-cell carcinoma. N Engl J Med. 1996;335(12):865-875. doi: 10.1056/NEJM199609193351207 [DOI] [PubMed] [Google Scholar]
- 39.Little AG, Gay EG, Gaspar LE, Stewart AK. National survey of non-small cell lung cancer in the United States: epidemiology, pathology and patterns of care. Lung Cancer. 2007;57(3):253-260. doi: 10.1016/j.lungcan.2007.03.012 [DOI] [PubMed] [Google Scholar]
- 40.Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014;64(1):9-29. doi: 10.3322/caac.21208 [DOI] [PubMed] [Google Scholar]
- 41.Rothman KJ, Gallacher JE, Hatch EE. Why representativeness should be avoided. Int J Epidemiol. 2013;42(4):1012-1014. doi: 10.1093/ije/dys223 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Flow Diagram of Selection of Cancer Drug Indications
eFigure 2. Median Overall Survival With 95% Confidence Intervals Comparing SEER-Medicare Patients With Charlson Comorbidity Index 0-1 and the Clinical Trial Intervention Arm Participants Receiving the Same FDA Approved Cancer Drug for the Same Indication
eTable 1. SEER-Medicare Inclusion Criteria for Cohort Selection
eTable 2. Cycle Estimates for Intravenous Cancer Drugs Used to Calculate Duration of Therapy and/or Single Cycles
eTable 3. Median Cancer-Specific Survival and Percent Deaths Due to Cancer Among SEER-Medicare Patients, Censored 12/31/2015
eTable 4. Age-Specific Median Overall Survival or Hazard Ratios for Clinical Trial Intervention Arms


