Abstract
Background:
Research on how disclosure concerns affect health outcomes for people living with HIV (PLWH) has yielded inconsistent results. Theoretically, disclosure concerns could predict either poorer ART adherence (PLWH worried about disclosure may not want to take their medication in front of others) or better ART adherence (stronger concerns may enhance treatment adherence to avoid unintentional disclosure). Furthermore, internalized stigma (which is positively associated with disclosure concerns) predicts worse ART adherence (an effect potentially in the opposite direction of the direct effect of disclosure concerns).
Setting/Methods:
186 PLWH initiating HIV care at four US clinics completed measures of disclosure concerns, internalized stigma, and ART adherence. Viral load data were obtained from medical records. We examined the indirect effect of disclosure concerns on outcomes, adjusting for the suppressor effect of internalized stigma. That is, we examined whether the association between disclosure concerns and ART adherence/ viral suppression is stronger and positive when controlling for the effect of internalized stigma.
Results:
Disclosure concerns were more strongly associated with better viral suppression and ART adherence when internalized stigma was in the model, suggesting that internalized stigma suppressed this association. Similarly, internalized stigma led to higher disclosure concerns, which in turn led to better ART adherence and higher likelihood of viral suppression. However, internalized stigma also had a direct effect in the opposite direction of this indirect effect.
Conclusions:
Findings highlight the importance of addressing effects of internalized stigma and disclosure concerns jointly when attempting to understand effects on health outcomes among new-to-care PLWH.
Keywords: Disclosure concerns, Internalized stigma, ART adherence, Viral suppression, New-to-care
Introduction
HIV-related stigma is a social process that involves prejudice, devaluation, negative attitudes, and discrimination towards people living with HIV (PLWH).1,2 There is mounting evidence suggesting that HIV-related stigma leads to negative health behaviors and outcomes among PLWH, such as poor antiretroviral therapy (ART) adherence and lower visit adherence.3–9 A variety of HIV-related stigma dimensions have been described in the literature: negative self-image (internalized stigma), disclosure concerns, enacted stigma, anticipated stigma, and perceived stigma in the community.1,10–12
Research has consistently supported associations between all of these dimensions of HIV-related stigma and worse health outcomes, except for one stigma dimension: Extant research has yielded inconsistent—even contradictory—results on the role of “disclosure concerns” in treatment adherence and health outcomes. The construct of disclosure concerns includes worrying about negative consequences of disclosing one’s HIV sero-status to others and trying to keep one’s HIV serostatus a secret.12,13 It is theoretically possible that disclosure concerns lead to worse medication adherence, since PLWH who are worried about unintentional disclosure may not want to take their medication in front of others. However, it is also possible that PLWH who have disclosure concerns are motivated to be (and appear) healthy so others will not suspect their HIV status, which would lead to better ART adherence and viral suppression.
There is empirical support for both of these hypotheses for people who have been living with HIV for some time. Research conducted with PLWH in different settings outside the US such as Ethiopia and Netherlands has found support for a negative effect of disclosure concerns on medication adherence14,15 as well as for a positive effect of disclosure concerns on viral suppression among PLWH who were mostly Hispanic in the US South.16 More importantly, many studies (some unpublished, including several of our own analyses) in the US, Canada or South Africa among demographically diverse PLWH (e.g., in terms of race/ethnicity: African, African American, and White; gender/sexual orientation: men who have sex with men, women; age: those who are 18 years and older, those who are between the ages of 16 and 24 or 29 years) did not find significant associations between disclosure concerns and ART adherence, viral load, or physical and mental health outcomes.14,17–22 The inconsistency in these findings point to the need for elucidating the complex role of disclosure concerns in health outcomes for PLWH in different contexts and via different mechanisms. Furthermore, most studies on the effect of disclosure concerns on health outcomes have been carried out with individuals who have been living with HIV for many years. However, the context of initial linkage to care is a unique and critical part of the HIV care continuum. It is therefore crucial to understand how PLWH newly entering HIV care experience disclosure concerns, as disclosure concerns may be a more salient and important issue for PLWH when they first start ART.21,23
Furthermore, internalized HIV-related stigma, which refers to endorsing and accepting society’s negative views, labels, and perceptions about living with HIV and applying these to oneself,10–12 has been shown to be one of the most important stigma dimensions predicting suboptimal treatment adherence for PLWH.10,11 Both cross-sectional and longitudinal studies have suggested that internalized HIV-related stigma is associated with worse medication adherence7,24–26 and lower HIV care visit adherence.27 Research also suggests that internalized HIV-related stigma leads to negative health outcomes through depression7,26 and other psychosocial mechanisms (e.g., treatment adherence self-efficacy).25
Moreover, the association between one dimension of HIV-related stigma and health outcomes may be mediated by another dimension of HIV-related stigma. For example, Turan et al.28 found that perceived community stigma leads to medication non-adherence, mediated by both internalized stigma and anticipated community stigma. Another study suggested that internalized stigma and anticipated stigma from healthcare workers mediate the association between experienced stigma in healthcare settings and lower trust in physicians,29 which may lead to ART nonadherence.30 However, little is known about the effect of disclosure concerns on health outcomes in the context of internalized HIV-related stigma. Considering that internalized stigma has a robust significant negative effect on health outcomes for PLWH and shows consistent positive correlations with disclosure concerns,12,13,19,22,31,32 examining these two dimensions of HIV-related stigma together may help explain contradictory findings on the role of disclosure concerns in HIV health outcomes.
The purpose of this study was to examine the joint associations that disclosure concerns and internalized stigma have with ART adherence and viral suppression among PLWH newly initiating HIV care. If disclosure concerns are associated with worse ART adherence, does this association remain significant when adjusting for internalized stigma? The picture may be more complicated for the hypothesis that disclosure concerns are associated with better ART adherence. On the one hand, conceptually, it may be expected that stronger disclosure concerns are associated with better ART adherence,16 since PLWH new to treatment who have stronger concerns about disclosure may view treatment adherence as one method of avoiding disclosure. For example, they may set up effective adherence systems such as private dosing reminders that do not alert others to their medication taking. On the other hand, internalized HIV-related stigma has a positive association with disclosure concerns,12,13,19,22,31,32 and internalized HIV-related stigma consistently predicts worse ART adherence (an effect in the opposite direction of the potential direct effect of disclosure concerns).7,24–26 Therefore, it is possible that internalized stigma masks or undermines the effect of disclosure concerns. That is, internalized stigma may act as a suppressor variable in the association between disclosure concerns and ART adherence (or viral suppression). In other words, when controlling for the effect of internalized HIV-related stigma, the association between disclosure concerns and ART adherence (or viral suppression) may be stronger and positive. It should be noted that we considered the suppression hypothesis as one of many possibilities and preliminary analyses veered us to focus on this possibility.
Method
Participants and Procedures
The sample consisted of 186 PLWH at four HIV clinical sites in the United States (see Table 1), who participated in a larger study called “integrating ENGagement and Adherence Goals upon Entry (iENGAGE)”. The iENGAGE was an intervention which aims to facilitate adjustment to living with HIV and improve adherence to care and ART for PLWH initiating HIV care by addressing HIV-related stigma and focusing problem solving, affect management, and communication. In the iENGAGE study,33,34 371 PLWH were either assigned to the intervention including four face-to-face sessions or to the standard clinical care and the effects of the iENGAGE intervention on HIV-related stigma and health outcomes such as ART adherence and viral suppression were examined. The details of the iENGAGE intervention are described elsewhere.33,34 Participants in the present study included those who recently initiated outpatient HIV care for the first time at one of the four HIV clinical sites, namely the University of Alabama at Birmingham (UAB), Johns Hopkins University (JHU), the University of North Carolina at Chapel Hill (UNC), and the University of Washington at Seattle (UW). All participants were enrolled within 14 days of their first outpatient HIV medical care visit at one of the study sites. All patients had confirmed no prior outpatient HIV medical care. Of participants, 16 initiated ART and achieved viral suppression following diagnosis and prior to their first outpatient HIV care provider visit. All viral loads and details of ART were systematically ascertained following enrollment and based upon data available in the electronic health records. ART initiation prior to study enrollment was ascertained by patient self-report as yes vs. no. Participants who previously received outpatient HIV care were excluded from the study. The majority of participants were male (148; 79.6%), 36 (19.4%) were female, and 2 (1.1%) were transgender; 112 were Black or African American, 60 White, 14 other race/ethnicity; with a mean age of 36.33 (SD = 12.78). Cross-sectional data were obtained by asking participants to complete measures using a computer-administered survey. Data on viral load were extracted from clinic records. The study was approved by the Institutional Review Board at each site. Descriptive statistics are presented in Table 1.
Table 1.
Descriptive Statistics
| N | % | |
|---|---|---|
| Race | ||
| Black or African American | 112 | 60.2 |
| White | 60 | 32.3 |
| Other | 14 | 7.5 |
| Gender | ||
| Male | 148 | 79.6 |
| Female | 36 | 19.4 |
| Transgender | 2 | 1.1 |
| Ethnicity | ||
| Hispanic | 12 | 6.5 |
| Non-Hispanic | 174 | 93.5 |
| Insurance | ||
| Public | 92 | 49.5 |
| Private | 53 | 28.5 |
| None | 41 | 22 |
| Site | ||
| JHU | 39 | 21 |
| UAB | 77 | 41.4 |
| UNC | 38 | 20.4 |
| UW | 32 | 17.2 |
| Mean | SD | |
| Age | 36.22 | 12.78 |
JHU: Johns Hopkins University, UAB: University of Alabama at Birmingham, UNC: The University of North Carolina at Chapel Hill, UW: University of Washington.
Measures
HIV-related Internalized Stigma & Disclosure Concerns
We used the 7-item Negative Self-Image and the 8-item Disclosure Concerns subscales of the revised HIV Stigma Scale13 to assess internalized HIV-related stigma and disclosure concerns, respectively. The items of the Negative Self-Image subscale (e.g., “I feel guilty because I have HIV/AIDS”) and Disclosure Concerns subscale (e.g., “I work hard to keep my HIV/AIDS a secret” and “Telling someone I have HIV is risky”) are rated on a Likert-type scale ranging from 1 (strongly disagree) to 4 (strongly agree). Both subscales have high internal consistency and test-retest reliability as shown previously.35 For the Negative Self-Image subscale, higher levels indicate higher levels of internalized stigma and for the Disclosure Concerns subscale, higher levels indicate higher levels of disclosure concerns. In the current study, Cronbach’s alphas were .82 for HIV-related internalized stigma and .75 for disclosure concerns.
HIV Clinical Outcomes
ART Adherence
ART adherence was assessed with the single question,36 “Thinking about the past 4 weeks, on average how would you rate your ability to take all of your HIV antiretroviral medications as your doctor prescribed” with response options ranging from very poor to excellent. Previous evidence suggests that this item is a valid measure of adherence.37 We dichotomized this measure by employing a cutoff as less than perfect adherence versus perfect adherence, as in previous studies using this measure, which is aligned with the robust negative predictive value of any degree of self-reported non-adherence.25
Viral Suppression
Data on viral load were extracted from participants’ most recent clinic visits. In accordance with treatment guidelines, we dichotomized the variable as suppressed (<200 c/mL) versus not suppressed (≥200 c/mL).
Statistical Analyses
Suppression, confounding, and mediation are similar in terms of statistical analyses used to test them.38–43 However, there are important conceptual differences as described by MacKinnon et al.38 Suppression is particularly similar to confounding; the main difference between suppression and confounding is the direction of change in effects. Whereas in confounding, typically the effect of one variable is reduced when controlling for a confounder, in suppression the magnitude of the effect of one variable increases when controlling for a suppressor. An important difference between mediation on the one hand, and suppression/confounding on the other hand is that mediation implies causality (as well as temporality), whereas suppression and confounding do not. Therefore, in mediation the ordering of predictor, mediator, and outcome is determined by theory and is fixed. However, for suppression and confounding, no temporal or causal relationship is hypothesized. Therefore, when one variable serves as a suppressor for the effect of a second variable, it may also be that the second variable serves as a suppressor for the effect of the first variable. This is referred to as mutual, or reciprocal, or cooperative suppression.42,44–46 In our case, examining the suppressor role of both variables are of theoretical importance. Therefore, we examined both the suppressor role of disclosure concerns in the association between internalized stigma and health outcomes as well as the suppressor role of internalized stigma in the association between disclosure concerns and health outcomes.
As mentioned above, statistically, suppression and mediation effects are tested using similar analytic procedures.38,39 When testing for mediation, one examines whether the direct effect (when the mediator is controlled in the model) is weaker compared to the total effect (when the mediator is not in the model). When testing for a suppressor effect, one examines whether the direct effect (when the suppressor is controlled in the model) is stronger compared to the total effect (when the suppressor is not in the model). This is tested by examining the indirect effect; a significant indirect effect suggests the direct effect is stronger compared to the total effect.38,47 Therefore, we tested two models using mediation/suppression analysis; one for each outcome variable (ART adherence and viral suppression). Furthermore, internalized stigma and disclosure concerns may affect viral suppression through ART adherence.
Our analyses included two simple mediation/suppression models. First, we tested whether there is a suppressor effect of HIV-related internalized stigma on the association that HIV-related disclosure concerns have with two outcomes: viral suppression and ART adherence (employing two separate simple mediation/suppression analyses). Second, we tested whether there is a suppressor effect of disclosure concerns on the association that HIV-related internalized stigma has with two outcomes: viral suppression and ART adherence. Additionally, we also tested a serial (sequential) mediation/suppression path model examining whether internalized HIV-related stigma leads to viral suppression, first through disclosure concerns, and then through ART adherence (with a direct effect of internalized stigma in the opposite direction). In these analyses, we calculated 95% percentile confidence intervals (CIs) with 2000 bootstrap resamples for indirect effects using the PROCESS macro for SPSS or SPSS AMOS (which enables us to run a mediation model with a dichotomous variable).48 In this procedure, if the CI does not include the value zero, the indirect effect is significant, suggesting a suppression or mediation effect. In all analyses, we adjusted for race, gender, and age of participants. All analyses conducted were cross-sectional. We computed and used mean scores for each scale.
Results
First, we tested the suppression effect of HIV-related internalized stigma in the association between HIV-related disclosure concerns and either viral suppression or ART adherence, respectively, as the outcome variable. The total effect of HIV-related disclosure concerns on viral suppression was not significant (when internalized stigma is not in the model; B=.01, SE=.04, p=.84, 95% CI [−.06, .08]. However, when internalized stigma was added to the model, the effect of disclosure concerns was significant and positive (direct effect; B=.10, SE=.04, p=.03, 95% CI [.01, .19]). The indirect effect of HIV-related disclosure concerns on viral suppression with internalized HIV-related stigma in the model was also significant (B=−.09, SE=.03, 95% CI [−.16, −.04]), suggesting that the effect of disclosure concerns is significantly stronger when internalized stigma is in the model, compared to when it is not. This finding supports the hypothesis that internalized stigma serves as a suppressor variable in the association between disclosure concerns and viral suppression. That is, adding internalizing stigma unmasks the significant effect of disclosure concerns on viral suppression.
Similarly, the total effect of HIV-related disclosure concerns on ART adherence was not significant (when internalized stigma is not in the model; B=.03, SE=.05, p=.49, 95% CI [−.06, .13]. When internalized stigma was added to the model, the effect of disclosure concerns was significant and positive (direct effect; B=.15, SE=.06, p=.01, 95% CI [.04, .27]). The indirect effect of HIV-related disclosure concerns on ART adherence with internalized HIV-related stigma in the model was also significant (B=−.12, SE=.04, 95% CI [−.21, −.04]), suggesting a significant suppression effect of internalized HIV-related stigma.
Considering the literature indicating that suppressor effects are usually mutual or reciprocal,39,42,45,49 we also hypothesized that there would be a suppressor effect of disclosure concerns on the association that internalized HIV-related stigma has with viral suppression and with ART adherence, employing two separate simple mediation/suppression analyses. The total effect of internalized HIV-related stigma on viral suppression (when disclosure concerns are not added to the model) was significant (B=−.08, SE=.03, p=.01, 95% CI [−.15, −.02]). However, this effect became stronger with disclosure concerns added to the model (the direct effect; B=−.14, SE=.04, p=.00, 95% CI [−.22, −.06]). The indirect effect of internalized HIV-related stigma on viral suppression through HIV-related disclosure concerns was also significant (B=.05, SE=.03, 95% CI [.01, .12], see Figure 1), suggesting a significant suppression effect of HIV-related disclosure concerns. These analyses are in line with one way to understand a suppression effect: The effect through a suppressor is in the opposite direction of the direct effect (and therefore result in these two opposing effects canceling each other and yielding a small total effect).
Figure 1.
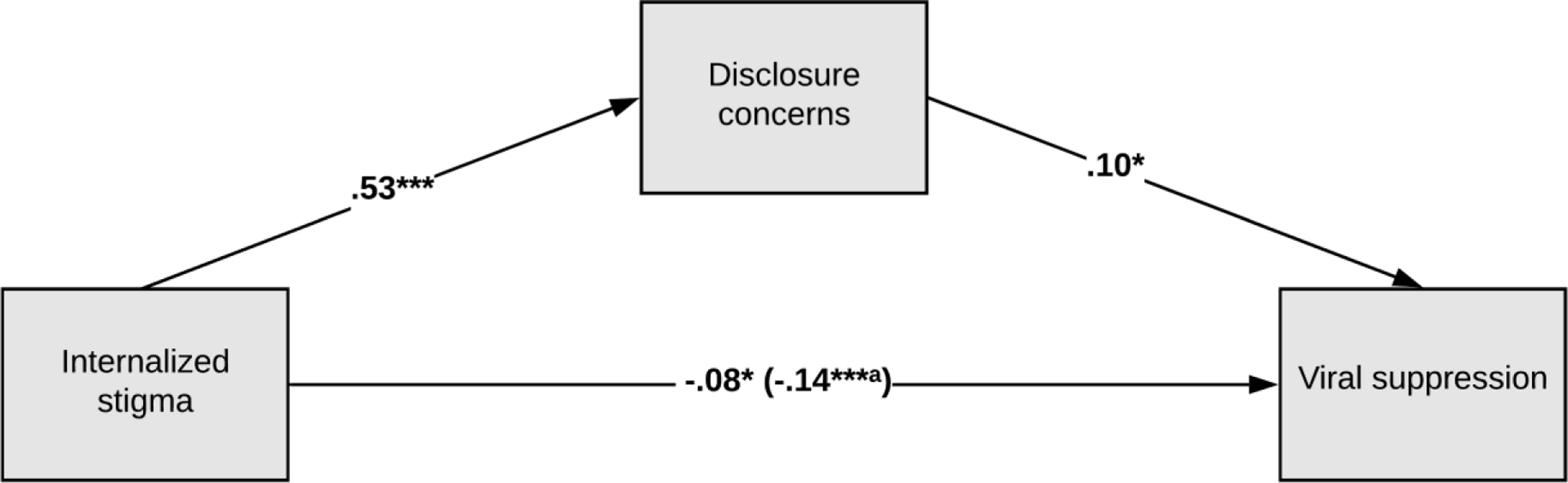
Mediation/Suppression Model of Viral Suppression. *p < .05, ***p < .001. aWhen disclosure concerns are in the model.
Similarly, the total effect of internalized HIV-related stigma on ART adherence was significant (B=−.09, SE=.04, p=.03, 95% CI [−.18, −.01]). However, this effect became stronger when disclosure concerns were added to the model (the direct effect; B=−.18, SE=.05, p=.00, 95% CI [−.28, −.07]). The indirect effect of internalized HIV-related stigma on ART adherence through disclosure concerns was also significant (B=.08, SE=.05, 95% CI [.01, .16], see Figure 2), suggesting a significant suppression effect of HIV-related disclosure concerns.
Figure 2.
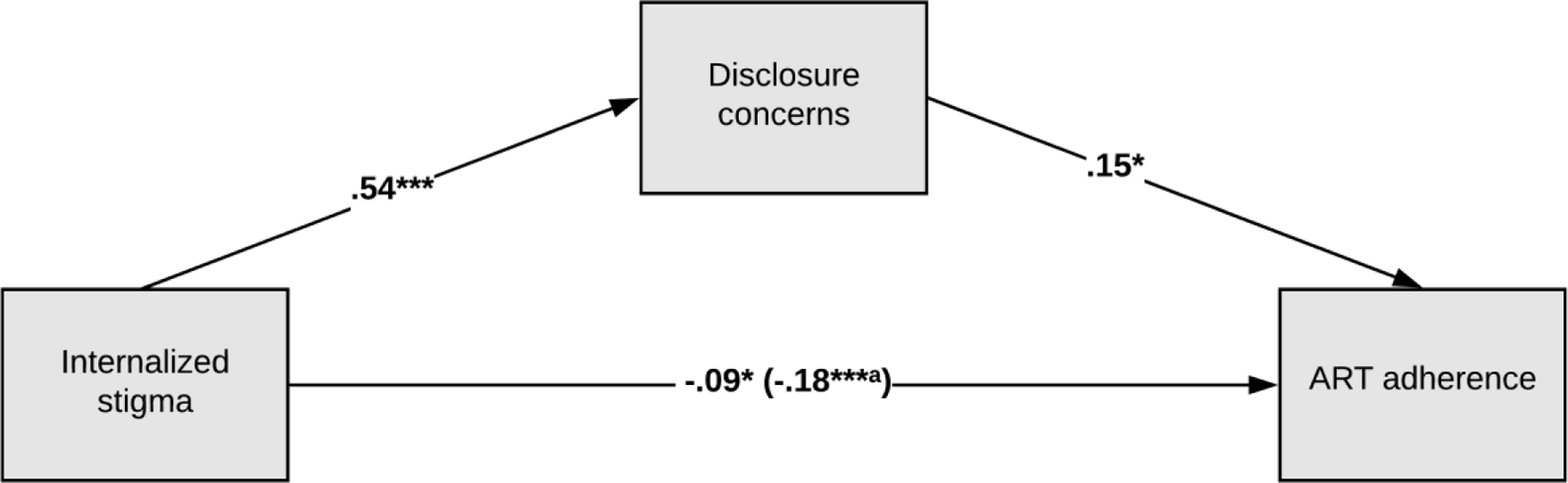
Mediation/Suppression Model of ART Adherence. *p < .05, ***p < .001. aWhen disclosure concerns are in the model.
We also tested a serial mediation/suppression model depicted in Figure 3 using SPSS AMOS, which enables us to run a mediation model with a dichotomous mediator by employing 2000 bootstrap resamples and 95% percentile CIs. The results suggest that internalized HIV-related stigma leads to higher HIV-related disclosure concerns, which leads to better ART adherence. However, there is also a direct effect of internalized stigma that is in the opposite direction: higher internalized stigma leads to worse ART adherence. Worse ART adherence, in turn, is associated with a lower likelihood of viral suppression. The serial indirect effect of internalized HIV-related stigma on viral suppression first through HIV-related disclosure concerns and then through ART adherence was significant and positive (B=.02, SE=.01, 95% CI [.00, .05]; see Figure 3).
Figure 3.
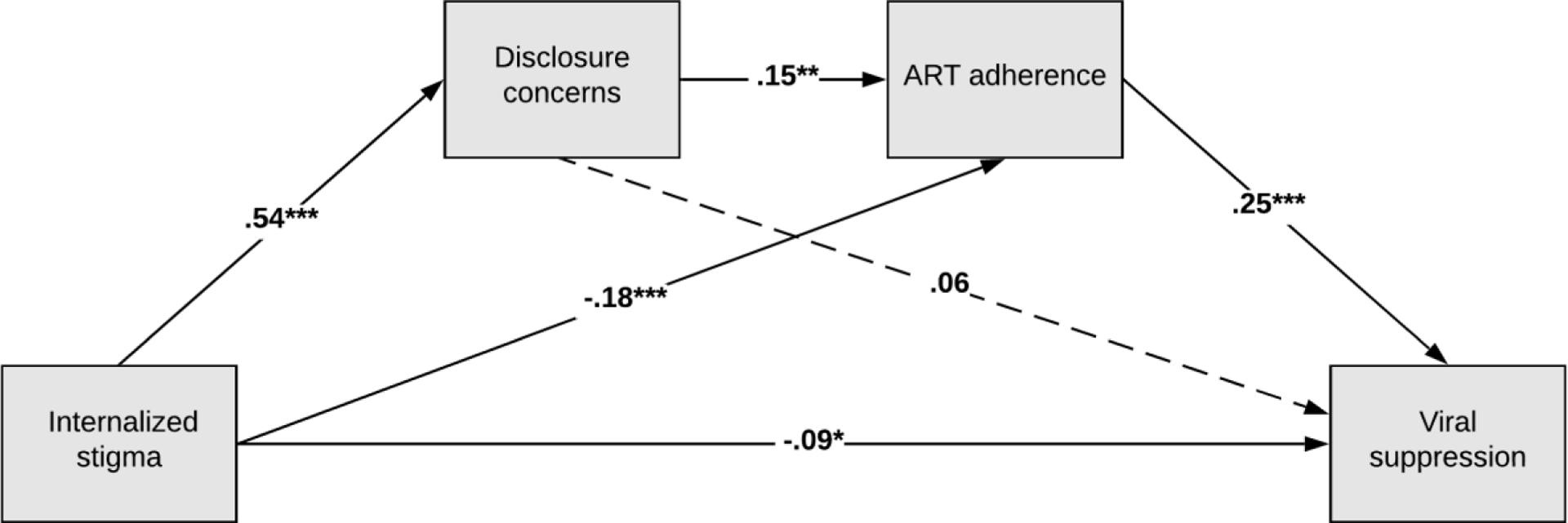
Serial Mediation/Suppression Model of Viral Suppression. *p < .05, **p < .01, ***p < .001.
Discussion
Initial engagement in HIV care is an overwhelming part of HIV care continuum. In the period when PLWH first enter HIV care, it is likely that disclosure concerns are a more salient issue and understanding how disclosure concerns contribute to health outcomes is of critical importance. In the present study, we examined the joint associations of disclosure concerns and internalized stigma with HIV-related health behaviors and outcomes (i.e., ART adherence and viral suppression) in PLWH new to HIV care. Our findings suggest that disclosure concerns are significantly associated with higher levels of ART adherence and viral suppression when the suppressor effect of internalized stigma in this association is taken into account. In other words, adjusting for internalized HIV-related stigma unmasked and revealed a positive effect of disclosure concerns on HIV-related health outcomes. Thus, it appears that PLWH new to care who have concerns about disclosing their HIV status to others may show better adherence to their treatment regimen, possibly because achieving optimal adherence and viral suppression may be viewed as a way to prevent disease progression and thereby to avoid unintentional disclosure.
Prior research suggested that PLWH initiating ART have more stable elevated disclosure concerns over a period of six months than those who did not initiate ART.21 The direction of causality in this association is not clear; however, it is possible that for PLWH who are newly entering HIV care, disclosure concerns may encourage initiating and maintaining ART. Furthermore, some prior research suggests that non-disclosure of HIV serostatus to close family members is associated with better ART adherence,50 and that PLWH who have disclosed their HIV to their mothers and yet received low levels of HIV-specific family support have a higher viral load.51 It is possible that the effect of disclosure concerns on ART adherence (or viral suppression) may also depend on who specifically is the source of disclosure concerns for a person living with HIV. Future studies focusing on the specifics of when and how disclosure concerns may affect health outcomes are needed.
Our findings also suggest that HIV-related disclosure concerns may serve as a suppressor in the association that HIV-related internalized stigma has with ART adherence or with viral suppression. This finding suggests that disclosure concerns mask the effect of internalized stigma on health outcomes, which became stronger (more negative) when adjusting for disclosure concerns. Theoretically, internalized stigma may lead to higher disclosure concerns, which in turn may lead to better ART adherence and a higher likelihood of viral suppression (Figures 1 and 2). However, research strongly suggests that internalized stigma has a direct effect that is in the opposite direction of this effect (of the effect through disclosure concerns described above), resulting in a lower likelihood of optimal ART adherence and viral suppression (possibly through deleterious psychological mechanisms such as depression7,52 or lower self-efficacy25). Furthermore, our serial mediation analyses suggest that the effects of both internalized HIV stigma and disclosure concerns on viral suppression are mediated by ART adherence (Figure 3).
This study had some limitations. First, we used a cross-sectional design, which makes it difficult to infer causality. Future research using longitudinal designs may contribute to our understanding of how changes in disclosure concerns over time are associated with health outcomes for PLWH. Second, our participants were recruited from well-resourced HIV clinics at major academic health centers in the US, which may limit generalizability to other settings or geographical locations. Lastly, there may be unobserved variables (e.g., some moderators) of the associations between disclosure concerns and health outcomes.
Despite these limitations, this study suggests that disclosure concerns positively affect ART adherence and viral suppression among new-to-care PLWH when the effect of internalized stigma is taken into account. On the one hand, internalized stigma directly and negatively affects health outcomes for PLWH; on the other hand, it may improve these outcomes through the pathway of increased disclosure concerns. Thus, our findings highlight the importance of addressing the effects of internalized stigma and disclosure concerns jointly when attempting to understand effects on health behaviors and outcomes, especially among PLWH newly entering HIV care. Services and interventions need to ascertain both internalized stigma and disclosure concerns in new-to-care HIV patients and assist patients in navigating disclosure decisions and protecting their mental health.
Conflict of Interest and Source of Funding:
The authors declare that there is no conflict of interest. This work was supported by the National Institutes of Allergy and Infectious Diseases (NIAID) [grant numbers R01AI103661 and 3R01AI103661-03S1]. This research was also supported by the University of Alabama at Birmingham (UAB) Center for AIDS Research CFAR, and a National Institutes of Health funded program [P30 AI027767] that was made possible by the following institutes: NIAID, NCI, NICHD, NHLBI, NIDA, NIA, NIDDK, NIGMS, and OAR.
M. J. M. has received grant support (to the University of Alabama at Birmingham) from Merck Foundation and consulting fees from Gilead Sciences.
References
- 1.Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS and Behavior. 2009;13(6):1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Herek GM, Capitanio JP. AIDS stigma and contact with persons with AIDS: Effects of direct and vicarious contact. 1. Journal of Applied Social Psychology. 1997;27(1):1–36. [Google Scholar]
- 3.Rice WS, Crockett KB, Mugavero MJ, Raper JL, Atkins GC, Turan B. Association between internalized HIV-related stigma and HIV care visit adherence. Journal of acquired immune deficiency syndromes (1999). 2017;76(5):482–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sayles JN, Wong MD, Kinsler JJ, Martins D, Cunningham WE. The association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. Journal of general internal medicine. 2009;24(10):1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sweeney SM, Vanable PA. The association of HIV-related stigma to HIV medication adherence: a systematic review and synthesis of the literature. AIDS and Behavior. 2016;20(1):29–50. [DOI] [PubMed] [Google Scholar]
- 6.Turan B, Rogers AJ, Rice WS, et al. Association between perceived discrimination in healthcare settings and HIV medication adherence: mediating psychosocial mechanisms. AIDS Behav. 2017;21(12):3431–3439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Turan B, Smith W, Cohen MH, et al. Mechanisms for the negative effects of internalized HIV-related stigma on antiretroviral therapy adherence in women: the mediating roles of social isolation and depression. Journal of Acquired Immune Deficiency Syndromes. 2016;72(2):198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Katz IT, Ryu AE, Onuegbu AG, et al. Impact of HIV‐related stigma on treatment adherence: systematic review and meta‐synthesis. Journal of the International AIDS Society. 2013;16:18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rueda S, Mitra S, Chen S, et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: a series of meta-analyses. BMJ open. 2016;6(7):e011453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Turan B, Hatcher AM, Weiser SD, Johnson MO, Rice WS, Turan JM. Framing mechanisms linking HIV-related stigma, adherence to treatment, and health outcomes. American Journal of Public Health. 2017;107(6):863–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS and Behavior. 2013;17(5):1785–1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale¶. Research in nursing & health. 2001;24(6):518–529. [DOI] [PubMed] [Google Scholar]
- 13.Bunn JY, Solomon SE, Miller C, Forehand R. Measurement of stigma in people with HIV: a reexamination of the HIV Stigma Scale. AIDS Education & Prevention. 2007;19(3):198–208. [DOI] [PubMed] [Google Scholar]
- 14.Sumari-de Boer IM, Sprangers MA, Prins JM, Nieuwkerk PT. HIV stigma and depressive symptoms are related to adherence and virological response to antiretroviral treatment among immigrant and indigenous HIV infected patients. AIDS and Behavior. 2012;16(6):1681–1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tilahun HA, Mariam DH, Tsui AO. Effect of perceived stigma on adherence to highly active antiretroviral therapy and self-confidence to take medication correctly in Addis Ababa, Ethiopia. Journal of HIV/AIDS & Social Services. 2012;11(4):346–362. [Google Scholar]
- 16.Matheu M, Sunil T, Castro-Peña A, et al. Lack of virologic suppression is associated with lower HIV-related disclosure stigma in people living with HIV. AIDS care. 2019:1–7. [DOI] [PubMed] [Google Scholar]
- 17.Golub SA, Tomassilli JC, Parsons JT. Partner serostatus and disclosure stigma: implications for physical and mental health outcomes among HIV-positive adults. AIDS and Behavior. 2009;13(6):1233. [DOI] [PubMed] [Google Scholar]
- 18.Logie CH, Lacombe-Duncan A, Wang Y, et al. Pathways from HIV-related stigma to antiretroviral therapy measures in the HIV care cascade for women living with HIV in Canada. Journal of acquired immune deficiency syndromes (1999). 2018;77(2):144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Logie C, James L, Tharao W, Loutfy M. Associations between HIV-related stigma, racial discrimination, gender discrimination, and depression among HIV-positive African, Caribbean, and Black women in Ontario, Canada. AIDS patient care and STDs. 2013;27(2):114–122. [DOI] [PubMed] [Google Scholar]
- 20.Quinn K, Voisin DR, Bouris A, et al. Multiple dimensions of stigma and health related factors among young black men who have sex with men. AIDS and Behavior. 2017;21(1):207–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chan BT, Maughan-Brown BG, Bogart LM, et al. Trajectories of HIV-related internalized stigma and disclosure concerns among art initiators and noninitiators in South Africa. Stigma and Health. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dowshen N, Binns HJ, Garofalo R. Experiences of HIV-related stigma among young men who have sex with men. AIDS patient care and STDs. 2009;23(5):371–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lambert CC, Tarver WL, Musoke PL, et al. Complexities of HIV Disclosure in Patients Newly Entering HIV Care: A Qualitative Analysis. The Journal of the Association of Nurses in AIDS Care: JANAC. 2020;31(2):208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Helms CB, Turan JM, Atkins G, et al. Interpersonal mechanisms contributing to the association between HIV-related internalized stigma and medication adherence. AIDS and Behavior. 2017;21(1):238–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seghatol-Eslami VC, Dark H, Raper JL, Mugavero MJ, Turan JM, Turan B. Interpersonal and intrapersonal factors as parallel independent mediators in the association between internalized HIV stigma and ART adherence. Journal of acquired immune deficiency syndromes (1999). 2017;74(1):e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Turan B, Rice WS, Crockett KB, et al. Longitudinal association between internalized HIV stigma and antiretroviral therapy adherence for women living with HIV: the mediating role of depression. Aids. 2019;33(3):571–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rice WS, Burnham K, Mugavero MJ, Raper JL, Atkins GC, Turan B. Association between internalized HIV-related stigma and HIV care visit adherence. Journal of acquired immune deficiency syndromes (1999). 2017;76(5):482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Turan B, Budhwani H, Fazeli PL, et al. How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS and Behavior. 2017;21(1):283–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kay ES, Rice WS, Crockett KB, Atkins GC, Batey DS, Turan B. Experienced HIV-related stigma in healthcare and community settings: Mediated associations with psychosocial and health outcomes. Journal of acquired immune deficiency syndromes (1999). 2018;77(3):257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schneider J, Kaplan SH, Greenfield S, Li W, Wilson IB. Better physician-patient relationships are associated with higher reported adherence to antiretroviral therapy in patients with HIV infection. Journal of general internal medicine. 2004;19(11):1096–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Franke MF, Muñoz M, Finnegan K, et al. Validation and abbreviation of an HIV stigma scale in an adult spanish-speaking population in urban Peru. AIDS and Behavior. 2010;14(1):189–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hernansaiz-Garrido H, Alonso-Tapia J. Internalized HIV stigma and disclosure concerns: development and validation of two scales in Spanish-speaking populations. AIDS and Behavior. 2017;21(1):93–105. [DOI] [PubMed] [Google Scholar]
- 33.Yigit I, Modi RA, Weiser SD, et al. Effects of an intervention on internalized HIV-related stigma for individuals newly entering HIV care. In. Vol 34: LWW; 2020:S73–S82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Modi R, Amico K, Knudson A, et al. Assessing effects of behavioral intervention on treatment outcomes among patients initiating HIV care: Rationale and design of iENGAGE intervention trial. Contemporary clinical trials. 2018;69:48–54. [DOI] [PubMed] [Google Scholar]
- 35.Varni SE, Miller CT, Solomon SE. Sexual behavior as a function of stigma and coping with stigma among people with HIV/AIDS in rural New England. AIDS and Behavior. 2012;16(8):2330–2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lu M, Safren SA, Skolnik PR, et al. Optimal recall period and response task for self-reported HIV medication adherence. AIDS and Behavior. 2008;12(1):86–94. [DOI] [PubMed] [Google Scholar]
- 37.Feldman BJ, Fredericksen RJ, Crane PK, et al. Evaluation of the single-item self-rating adherence scale for use in routine clinical care of people living with HIV. AIDS and Behavior. 2013;17(1):307–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prevention science. 2000;1(4):173–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hicks BM, Patrick CJ. Psychopathy and negative emotionality: analyses of suppressor effects reveal distinct relations with emotional distress, fearfulness, and anger-hostility. Journal of abnormal psychology. 2006;115(2):276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Monroe AE, Ysidron DW. Not so motivated after all? Three replication attempts and a theoretical challenge to a morally motivated belief in free will. Journal of Experimental Psychology: General. 2020. [DOI] [PubMed] [Google Scholar]
- 41.Rucker DD, Preacher KJ, Tormala ZL, Petty RE. Mediation analysis in social psychology: Current practices and new recommendations. Social and Personality Psychology Compass. 2011;5(6):359–371. [Google Scholar]
- 42.Akinwande MO, Dikko HG, Samson A. Variance inflation factor: as a condition for the inclusion of suppressor variable (s) in regression analysis. Open Journal of Statistics. 2015;5(07):754. [Google Scholar]
- 43.Nickisch A, Palazova M, Ziegler M. Dark personalities–dark relationships? An investigation of the relation between the Dark Tetrad and attachment styles. Personality and Individual Differences. 2020;167:110227. [Google Scholar]
- 44.Conger AJ. A revised definition for suppressor variables: A guide to their identification and interpretation. Educational and psychological measurement. 1974;34(1):35–46. [Google Scholar]
- 45.Paulhus DL, Robins RW, Trzesniewski KH, Tracy JL. Two replicable suppressor situations in personality research. Multivariate Behavioral Research. 2004;39(2):303–328. [DOI] [PubMed] [Google Scholar]
- 46.Cohen J, Cohen P, West SG, Aiken LS. Applied multiple correlation/regression analysis for the social sciences. In: Hillsdale, NJ: Erlbaum; 2003. [Google Scholar]
- 47.Tzelgov J, Henik A. Suppression situations in psychological research: Definitions, implications, and applications. Psychological Bulletin. 1991;109(3):524. [Google Scholar]
- 48.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Publications; 2017. [Google Scholar]
- 49.Lewis JW, Escobar LA. Suppression and enhancement in bivariate regression. Journal of the Royal Statistical Society: Series D (The Statistician). 1986;35(1):17–26. [Google Scholar]
- 50.Rotzinger A, Locatelli I, Reymermier M, et al. Association of disclosure of HIV status with medication adherence. Patient education and counseling. 2016;99(8):1413–1420. [DOI] [PubMed] [Google Scholar]
- 51.Fekete EM, Antoni MH, Lopez CR, et al. Men’s serostatus disclosure to parents: associations among social support, ethnicity, and disease status in men living with HIV. Brain, behavior, and immunity. 2009;23(5):693–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.DiIorio C, McCarty F, DePadilla L, et al. Adherence to antiretroviral medication regimens: a test of a psychosocial model. AIDS and Behavior. 2009;13(1):10–22. [DOI] [PMC free article] [PubMed] [Google Scholar]


