Abstract
Background:
Limited data exist on the association between circulating suppression of tumorigenicity 2 (ST2) and recurrent hospitalizations and emergency department (ED) encounters in outpatients with heart failure (HF). In addition, data on ST2 in African American patients with HF are scarce.
Methods:
We evaluated 307 outpatients with HF (age, 57±12 years; 64.2% men; 51.5% Caucasian, 45.6% African American; median ejection fraction, 35%; ischemic etiology, 41.4%). Median ST2 was 37.8 ng/mL (29.6–51.4).
Results:
After a median of 3.1 years, there were 584 hospitalizations (224 for HF) and 335 ED visits (80 for HF). Patients (N=176; 57.3%) with elevated (>35 ng/mL) ST2 had 2-fold higher hospitalization rates in adjusted models (rate ratio [RR] 1.97; 95%CI 1.38–2.82; P<0.001), driven by 3.5-fold higher HF hospitalization rates (adjusted RR 3.56; 95%CI 1.69–7.49; P<0.001). These associations persisted after adjusting for baseline B-type natriuretic peptide levels. Findings were similar for elevated ST2 and ED visit rates. Elevated ST2 was associated with the composite of death or HF hospitalization (109 patients; 3-year estimate: 35.4%); risk was 5-fold higher in the first 6 months but declined gradually. The higher hospitalization rates and composite endpoint risk associated with elevated ST2 was similar in African Americans and Caucasians. In landmark analyses in a subset of patients, 6-month (N=112) and 12-month (N=149) changes in ST2 levels from baseline added prognostic information.
Conclusions:
Elevated ST2 in outpatients with HF portends higher healthcare resources utilization and higher risk for accelerated disease progression, regardless of race, especially in the first 6 months.
Keywords: Heart failure, suppression of tumorigenicity 2 (ST2), hospitalization, mortality, outcomes
1. Introduction
Suppression of tumorigenicity 2 (ST2) is a member of the interleukin-1 receptor superfamily [1]. The main biologic isoforms are the transmembrane isoform, which has antihypertrophic and antifibrotic properties on cardiomyocytes via IL-33 ligand [2,3], while the soluble isoform (sST2) acts as a “decoy receptor” blocking, in a dose-dependent fashion, the aforementioned favorable effects [3]. Although the complex biology of the ST2 system has not been fully elucidated, ST2 is upregulated in response to mechanical injury, among other stimuli, and is released from cardiac myocytes, vascular endothelial cells, and fibroblasts [4,5]. Elevated levels of sST2 have been associated with increased mortality in both acute and chronic heart failure (HF) settings [6,7]. The prognostic value of ST2 for mortality in HF is enhanced when measured serially [8–10]. Based on these data, ST2 has been recognized as a potentially useful biomarker for risk stratification in patients with HF [11]. However, the evidence linking ST2 with outcomes in HF comes largely from Caucasian populations, as data on African-Americans with HF have been limited to date [12].
Besides mortality, ST2 has been identified as a strong predictor of hospitalization in chronic HF patients [13] and rehospitalization after admission for acute HF [6]. However, studies to date have focused on time to first HF hospitalization or readmission, alone or combined with mortality [14], ignoring information on recurrent events and eventually healthcare resources utilization. Recent work from large trials [15–18] and cohorts [19,20] has demonstrated that evaluating the totality of information on outcomes, including recurrent events, improves statistical power and provides a more comprehensive view of treatment effects and prognosis. This approach was adopted in the design of the recently reported transcatheter mitral repair trial [21]. To date, no study has examined the longitudinal association of ST2 levels with recurrent events in HF.
In this study, our goal was to evaluate the association of ST2 with (1) hospitalization and ED visit rates (i.e. first and recurrent events) and (2) death or HF hospitalization (time-to-event analysis), a composite endpoint commonly used in clinical trials, in a Stage C, ambulatory HF prospective cohort with adequate representation of African-American patients to detect any differential associations between ST2 levels and outcomes. In exploratory analyses, we provide information on the value of serial ST2 levels in a subset of patients with serial measurements.
2. Methods
2.1. Study Population
Outpatients with HF were recruited from 3 university-affiliated practices in the greater metropolitan Atlanta area as part of a prospective cohort study (The Atlanta Cardiomyopathy Consortium) [22,23]. Inclusion criteria included age >18 years and a diagnosis of HF with either reduced or preserved left ventricular ejection fraction (LVEF). For HF with preserved LVEF, in addition to clinical criteria, a B-type natriuretic peptide (BNP) level >200 ng/L and/or echocardiographic evidence of diastolic dysfunction were required [24,25]. Exclusion criteria included congenital heart disease, previous or pending heart transplant or left ventricular assist device (LVAD), known infiltrative disease (e.g., amyloidosis), previous other solid organ transplantation, and end-stage HF requiring continuous inotrope infusion. All patients had an established HF diagnosis and were stable for at least 3 months before entering the study. Clinical data and blood samples were collected during dedicated visits every 6 months. Because of interim protocol changes, not all patients had repeat blood draws during the 6- and 12-month visits. The Institutional Review Board of Emory University has approved this study. All patients have signed informed consent and the study protocol conformed to ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the institution’s human research committee.
2.2. ST2 Measurements
ST2 concentrations were measured at Critical Diagnostics in stored serum samples, using the Critical Diagnostics Presage® ST2 assay, which is an enzyme-linked immunosorbent assay. The assay is calibrated for a range of 3.1 to 200 ng/mL.
2.3. Assessment of Outcomes and Endpoints
Every six months, the patients were contacted to assess medication changes, procedures, new diagnoses, hospitalizations, and emergency department (ED) visits. Mortality was ascertained through medical records, information from family members, and Social Security Death Index query. Hospitalization data were obtained from electronic medical records, outpatient notes from any encounter for admissions to outside hospitals, and direct patient inquiry during follow-up.
The primary endpoints of our study were the rates of all-cause hospital admissions and ED visits. We have classified these events into cardiovascular and non-cardiovascular. Cardiovascular events were further classified into HF-related and non-HF-related. The reasons for hospital admissions and ED visits have been individually verified by chart review. The secondary endpoint was the composite of a terminal endpoint (death or implantation of LVAD or heart transplant) or hospitalization for HF, on a time-to-first-event basis. The rationale was that this composite and variations thereof are commonly encountered in HF clinical trials.
2.4. Statistical Analysis
We evaluated ST2 levels both as a log2-transformed continuous variable and as a dichotomous variable using a 35-ng/mL cut-off based on several previous studies in chronic HF [4,9,26]. In an exploratory analysis using step functions, the optimal cut-off point for the composite endpoint of death or HF hospitalization in our cohort was 34.5 ng/mL, corroborating previous reports. Rates of hospitalizations and ED visits were examined using negative binomial regression models, which allow for over-dispersed events (i.e. clustering of events) and have been previously validated for these outcomes [27]. We used Cox models for the composite of death or HF hospitalization and tested for proportional hazards using the Schoenfeld residuals and time interaction terms. Because we detected non-proportional association of ST2 levels with this endpoint, we used flexible parametric survival (Royston-Parmar) models to incorporate time-dependent effects [28]. Our hypothesis was that ST2 levels were associated with the primary endpoint (hospitalization rates) at the two-sided α=0.05 level. In adjusted models, we considered the following covariates based on previous literature: age, gender, race, systolic blood pressure, LVEF, presence of coronary artery disease, New York Heart Association (NYHA) class, diabetes mellitus, renal function, presence of atrial fibrillation, and medical and implantable device therapy at baseline (i.e., present at the index visit). Because of the relatively small sample size of our cohort, we opted not to follow a data-driven prognostic model (i.e., derive prognostic variables from our own cohort), as this would have led to under-detection of predictor variables and under-adjustment of the predictive value of ST2. Therefore, we have opted for a literature-driven adjustment model. Because BNP is an established prognostic marker in HF, we repeated the analyses including log-transformed BNP in the adjustment models. For each endpoint, we also evaluated for differential prognostic significance of ST2 levels in race-based subgroups, using appropriate interaction terms. To explore the association of serial ST2 data with outcomes we did landmark analyses at 6 and 12 months using both 6- and 12-month ST2 levels and percent changes from baseline as the exposure of interest. Statistical analysis was conducted using STATA 14.2 (StataCorp, College Station, TX).
3. Results
3.1. Study Population and ST2 Distribution
Baseline ST2 measurements were available in 307 of 325 (94.5%) participants of the study. Among these patients, 185 (60.3%) had LVEF <40% and 42 (13.7%) had LVEF 40%-50%. The median concentration of ST2 in the cohort was 37.8 ng/mL (25th–75th percentile: 29.6–51.4) and 176 patients (57.3%) had ST2 levels above the 35 ng/mL clinical cutoff. Table 1 summarizes the clinical characteristics of the study cohort according to ST2 levels at baseline. Patients with higher ST2 levels (>35 ng/mL) at baseline were younger, had higher heart rate and BNP, and worse NYHA class and renal function. In 112 patients and 146 patients with repeat 6- and 12-month samples, respectively, the corresponding ST2 changes vs. baseline were +2.9 ng/mL (-5.9–8.6; P=0.05) and +2.8 ng/mL (-4.3–9.2; P=0.01).
Table 1.
Baseline Patient Characteristics (N=307)
| Characteristic | All (N=307) | ST2 >35 ng/mL (N=176) | ST2 ≤35 ng/mL (N=131) | P value |
|---|---|---|---|---|
| Age | 57 ± 12 | 55 ± 12 | 59 ± 13 | 0.011 |
| Men, n (%) | 197 (64.2) | 118 (67.0) | 79 (60.3) | 0.231 |
| Race, n (%) | 0.473 | |||
| White | 158 (51.5) | 88 (50.0) | 70 (53.4) | |
| Black | 140 (45.6) | 81 (46.0) | 59 (45.0) | |
| Other | 6 (2.0) | 4 (2.3) | 2 (1.5) | |
| Body mass index, kg/m2 | 29.9 (25.7–35.5) | 30.5 (26.3–36.7) | 29.6 (25.1–33.0) | 0.064 |
| NYHA Class (%) | 0.001 | |||
| I-II | 218 (71.0) | 113 (64.2) | 105 (80.2) | |
| III-IV | 82 (26.7) | 56 (31.8) | 26 (19.8) | |
| LVEF, % | 35 (26, 50) | 35 (26, 49) | 35 (27, 51) | 0.620 |
| LVEF <40%, n (%) | 185 (60.3) | 107 (60.8) | 78 (59.5) | 0.906 |
| Time from HF diagnosis, years | 6.4 (3.1–12.0) | 7.2 (3.4–12.0) | 6.1 (2.6–11.3) | 0.204 |
| Previous hospitalization for HF, n (%) | 105 (34.2) | 65 (36.9) | 40 (30.5) | 0.274 |
| Ischemic heart disease, n (%) | 127 (41.4) | 65 (36.9) | 62 (47.3) | 0.079 |
| Atrial fibrillation, % | 46 (15.0) | 27 (15.3) | 19 (14.5) | 0.873 |
| Diabetes mellitus, % | 103 (33.6) | 66 (37.5) | 37 (28.2) | 0.112 |
| Anemia, % * | 98 (31.9) | 57 (32.4) | 41 (31.3) | 0.902 |
| Systolic blood pressure, mmHg | 113 ± 19 | 112 ± 19 | 114 ± 20 | 0.685 |
| Heart rate, beats/min | 72 ± 11 | 73 ± 11 | 71 ± 11 | 0.028 |
| Hemoglobin, g/dL | 13.2 ± 1.8 | 13.2 ± 1.9 | 13.1 ± 1.6 | 0.231 |
| Serum sodium, mEq/L | 138 ± 3 | 138 ± 3 | 139 ± 3 | 0.226 |
| Serum potassium, mEq/L | 4.2 ± 0.5 | 4.2 ± 0.5 | 4.2 ± 0.5 | 0.787 |
| Serum creatinine, mg/dL | 1.2 (1, 1.5) | 1.2 (1.1, 1.5) | 1.1 (0.9, 1.3) | 0.000 |
| Blood urea nitrogen, mg/dL | 18 (13–26) | 19 (14–27) | 16 (12–25) | 0.002 |
| eGFRMDRD, mL/min/1.73m2 | 66 ± 25 | 62 ± 24 | 70 ± 25 | 0.004 |
| B-type natriuretic peptide, ng/L | 162 (53–548) | 172 (59–611) | 116 (44–307) | 0.019 |
| Therapy | ||||
| ACE inhibitor or ARB, n (%) | 242 (78.8) | 140 (79.5) | 102 (77.9) | 0.778 |
| Beta-blocker, n (%) | 284 (92.5) | 163 (92.6) | 121 (92.4) | 1.000 |
| Aldosterone antagonists, n (%) | 133 (43.3) | 77 (43.8) | 56 (42.7) | 0.908 |
| Nitrates, n (%) | 72 (23.5) | 41 (23.3) | 31 (23.7) | 1.000 |
| Diuretics, n (%) | 254 (82.7) | 141 (80.1) | 113 (86.3) | 0.172 |
| CRT and/or ICD, n (%) | 196 (63.8) | 112 (63.6) | 84 (64.1) | 1.000 |
Continuous variables expressed as median (25th–75th percentile) or mean ± standard deviation.
Defined as hemoglobin <13 g/dL in men and <12 g/dL in women. ACE: angiotensin-converting enzyme; ARB: angiotensin receptor blocker; CRT: cardiac resynchronization therapy; eGFRMDRD: eGFR calculated by the Modification of Diet in Renal Disease study equation; HF: heart failure ICD: implantable cardioverter defibrillator; LVEF: left ventricular ejection fraction; NYHA: New York Heart Association
Echocardiographic data were available in a subset of patients (N=247; 80.5%), as echocardiography was not part of the research protocol. Supplemental Table 1 summarizes the baseline echocardiographic characteristics according to baseline ST2 levels. There was a trend towards worse right ventricular systolic function in patients with elevated ST2 based on fractional area change and ejection time, although this finding should be interpreted cautiously.
3.2. Follow-Up and Outcomes
Median follow-up time was 3.1 years (25th–75th percentile, 1.9–3.9) for a total of 873 patient-years. During this time, there were 584 all-cause hospitalizations (67 per 100 patient-years) in 193 (62.9%) patients. Of these, 420 were for all cardiovascular causes (48 per 100 patient-years) in 157 (51.1%) patients, out of which 224 were for HF specifically (26 per 100 patient-years) in 79 (25.7%) patients. In addition, there was a total of 335 all-cause ED visits (38 per 100 patient-years) in 133 (43.3%) patients. Of these, 178 were for all cardiovascular causes (20 per 100 patient-years) in 88 (28.7%) patients, out of which 80 were for HF specifically (9 per 100 patient-years) in 44 (14.3%) patients.
The secondary composite endpoint (death, LVAD implantation, heart transplant, or HF hospitalization) was met by 109 patients (3-year Kaplan-Meier estimate: 35.4%). Specifically, there were 44 deaths, 4 LVAD, and 7 heart transplants (55 terminal events; 3-year Kaplan-Meier estimate: 17.4%), and 54 additional patients were admitted for HF.
3.3. Baseline ST2 and Rates of Hospitalization and ED Visits
Higher baseline ST2 was associated with higher rates of HF-related, cardiovascular, and all-cause hospitalizations after adjustment for clinical covariates (Table 2). When treated as a dichotomous variable, elevated ST2 (>35 ng/mL) was still associated with higher hospitalization rates after BNP was introduced into the adjustment model. The association between baseline ST2 levels and hospitalization rates was similar in Caucasian and African American patients (Supplemental Table 2).
Table 2.
Baseline ST2 Levels and Hospitalization Rates
| HF Hospitalizations | CV Hospitalizations | Total Hospitalizations | ||||
|---|---|---|---|---|---|---|
| RR (95% CI) | P | RR (95% CI) | P | RR (95% CI) | P | |
| Adjusted - Clinical Model | ||||||
| Continuous ST2 (log2) | 2.31 (1.31–4.07) | 0.004 | 1.75 (1.26–2.44) | 0.001 | 1.63 (1.22–2.18) | 0.001 |
| Dichotomous ST2 (>35 ng/mL) | 3.56 (1.69–7.49) | 0.001 | 2.14 (1.40–3.26) | <0.001 | 1.97 (1.38–2.82) | <0.001 |
| Adjusted - Clinical Model Plus BNP | ||||||
| Continuous ST2 (log2) | 1.62 (0.88–2.99) | 0.121 | 1.43 (1.01–2.02) | 0.045 | 1.38 (1.02–1.87) | 0.036 |
| Dichotomous ST2 (>35 ng/mL) | 3.03 (1.42–6.46) | 0.004 | 1.91 (1.25–2.91) | 0.003 | 1.83 (1.28–2.61) | 0.001 |
Estimates calculated with negative binomial regression models. Adjusted model included age, gender, race, systolic blood pressure, left ventricular ejection fraction, presence of coronary artery disease, New York Heart Association class, diabetes mellitus, renal function, history of atrial fibrillation, medical therapy, and implantable devices. BNP: B-type natriuretic peptide; CI: confidence interval; CV: cardiovascular; HF: heart failure; RR: rate ratio
Higher baseline ST2 was associated with higher rates of HF-related, cardiovascular, and all-cause ED visits after adjustment for clinical covariates (Supplemental Table 3), especially with dichotomous ST2. When ST2 was treated as a dichotomous variable (>35 ng/mL), the association was retained after BNP was introduced into the adjustment model. In exploratory analyses, there were signals towards a stronger association of ST2 levels with ED visits rates in African Americans compared to Caucasians, but the corresponding interaction terms did not meet the significance threshold and therefore these trends must be interpreted with caution (Supplemental Table 4).
3.4. Baseline ST2 and Composite Endpoint (Death or HF Hospitalization)
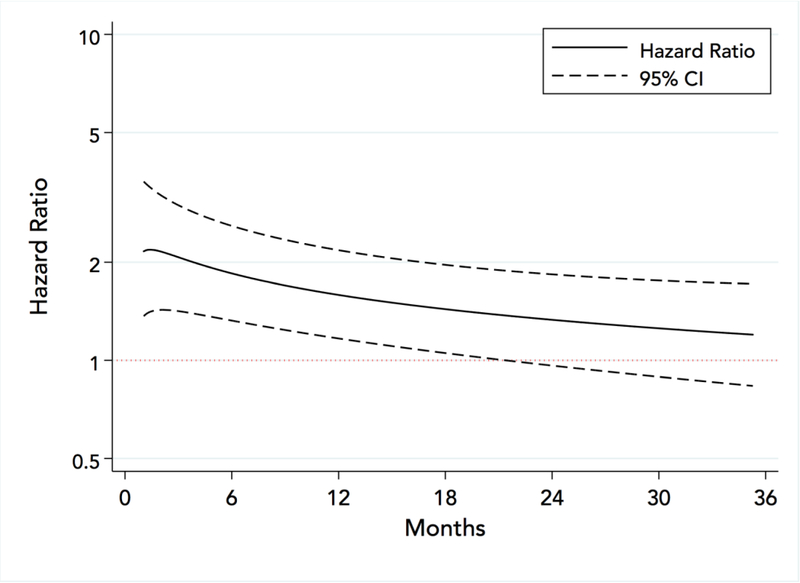
In models with ST2 levels entered as a continuous variable, for every log2 higher (doubling) of ST2, the average hazard ratio (HR) for the composite endpoint (death, LVAD implantation, heart transplant, or HF hospitalization) was 1.58 (95% CI 1.16 to 2.15; P=0.003) in a model adjusting for clinical covariates and 1.34 (95% CI 1.00 to 1.80; P=0.047) in a model additionally adjusting for BNP. The risk associated with baseline ST2 was time-dependent; risk per doubling of concentration was initially 2-fold higher and declined gradually over time, with the 95% confidence interval crossing the unity boundary at about 18 months, Figure 1.
Figure 1.
Hazard ratio for the composite endpoint (death or heart failure related hospitalization) associated with doubling (log2-increase) of ST2 concentrations. Flexible parametric survival model adjusted for age, gender, race, systolic blood pressure, left ventricular ejection fraction, presence of coronary artery disease, New York Heart Association class, diabetes mellitus, renal function, presence of atrial fibrillation, and therapy.
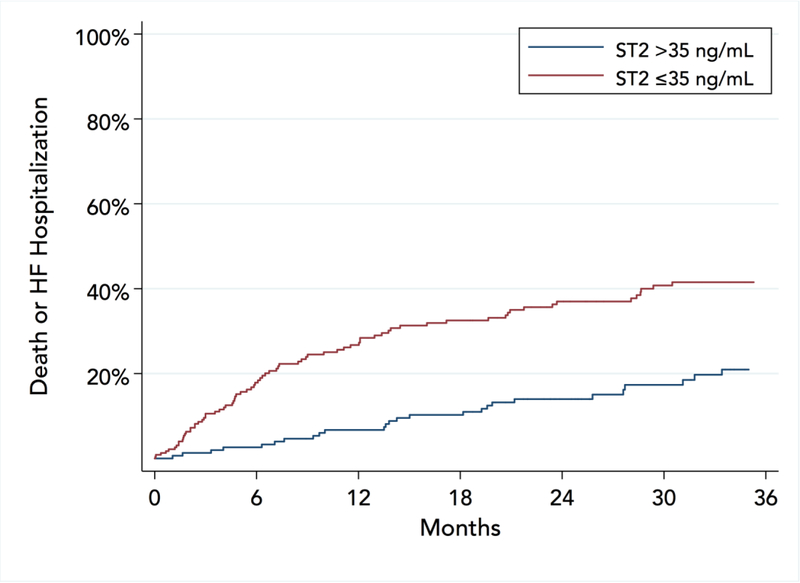
Elevated baseline ST2 (>35 ng/mL) identified a group of patients with significantly higher risk for the composite endpoint, Figure 2. The HR for the entire follow-up period was 2.28 (95% CI 1.38 to 3.78; P=0.001) in a model adjusting for clinical covariates and 2.13 (95% CI 1.25 to 3.61; P=0.005) in a model additionally adjusting for BNP. As in the continuous-variable analysis, the risk was time-dependent. Risk among patients with ST2 >35 ng/mL (vs. those with ST2 ≤35 ng/mL) was 5-fold higher in the first 6 months in adjusted models, but declined gradually over time, with the 95% CI crossing the unity boundary at about 18 months, Supplemental Figure 1.
Figure 2.
Cumulative incidence of death or hospitalization for heart failure according to baseline levels of ST2. Kaplan-Meier curves adjusted for age, gender, race, systolic blood pressure, left ventricular ejection fraction, presence of coronary artery disease, New York Heart Association class, diabetes mellitus, renal function, presence of atrial fibrillation, and therapy.
In exploratory analyses, the optimal cut-off point for the composite endpoint in the entire cohort was 34.5 ng/mL. The association of log2 ST2 with the composite endpoint in adjusted models was similar in African American and Caucasian patients (P for interaction =0.70).
3.5. Serial ST2 Measurements and Event Rates
In 112 patients with repeat ST2 levels available at the 6-month visit, the median increase in ST2 levels was 2.9 ng/mL (-5.9–8.6), corresponding to 6.9% increase (-12.3%, 25.7%; P=0.062) vs. baseline. ST2 at 6 months retained strong prognostic value for subsequent events (Supplemental Table 5). When 6-month changes in ST2 levels vs. baseline were examined in models adjusting for baseline ST2, the change offered incremental prognostic information and was associated with significantly higher risk for subsequent events (Supplemental Table 5).
In 149 patients with ST2 levels available at 12 months, median increase in ST2 levels was 2.8 ng/mL (-4.3–9.2), corresponding to 8.5% increase (-10.1%, 28.1%; P=0.011) vs. baseline. ST2 at 12 months was still prognostic of subsequent events, but power was limited, and the incremental information offered by 12-month changes did not reach statistical significance (Supplemental Table 5).
4. Discussion
In this well-characterized cohort of African American and Caucasian outpatients with HF, we observed a strong association between baseline levels of ST2 and rates of hospitalization and ED visits during a 3-year follow-up. The relative risks associated with elevated ST2 were higher for HF-related events (hospitalizations and ED visits) compared to cardiovascular and all-cause events, but ST2 was still prognostic across the board of outcomes. Elevated baseline ST2 levels (defined as >35 ng/mL based on previous work; we observed a similar cut-off in our cohort) were strongly predictive of death or HF hospitalization, a composite endpoint commonly used in HF clinical trials. There was no differential association of ST2 with hospitalization rates and the composite endpoint between African American and Caucasian patients, which has not been previously demonstrated. Notably, the risk for death or HF hospitalization associated with elevated ST2 levels varied over time, with a 5-fold higher risk initially during the first 6 months and gradual decline over the next 18 months. In a subset of patients with serial measurements available, increases in ST2 levels were associated with excessive risk for subsequent events, especially HF-related events,
In ambulatory patients with HF, elevated ST2 has been associated with increased risk of HF-related hospitalizations and all-cause mortality. In a well-characterized clinical trial cohort of patients with HFrEF [26], doubling of baseline ST2 was associated with 68% higher risk of cardiovascular death or HF hospitalization over a median of 30 months in models adjusting for clinical covariates. A similar magnitude of excess risk (50%) for terminal HF endpoints in clinical models per log2-ST2 was reported by the Penn Heart Study [4]. Those results are directly comparable to the risk we report in our study (58%) for the composite of death or HF hospitalization in clinically adjusted models. In an outpatient HF cohort from Spain, ST2 was a strong predictor of death or HF hospitalization and performed better than galectin-3 [29]. We expand on those findings by providing evidence that elevated ST2 is associated with more utilization of healthcare resources in terms of hospitalizations and ED visits during a 3-year follow-up in a racially diverse cohort that included patients with both HFrEF and HFpEF.
Studies with serial assessment of ST2 are limited. In a study of patients with ischemic HF [30], repeat ST2 levels at 3 months showed minimal change over baseline; however, an >15% increase in ST2 was associated with cardiovascular hospitalization. In the Valsartan Heart Failure Trial cohort, 12-month increases in ST2 significantly compounded risk for HF-related events [31]. In a serial biomarker study among 180 outpatients with HFrEF, only serial ST2 added prognostic information and elevated ST2 was associated with 3-fold higher risk for death or cardiac transplantation [32]. Similarly, in a HF study using serial biomarkers to guide therapy [9], only serial ST2 added prognostic information. In all, as ST2 is a relatively stable marker, increases in ST2 appear to reflect disease progression and portend worse prognosis.
The pathophysiological links between ST2 and adverse cardiovascular outcomes have been previously described in detail [1]. From a practical perspective, elevated levels of ST2 in a stable outpatient signify a patient who is at substantially higher risk for hard clinical events and increased use of healthcare resources in the next few years, beyond what would be expected from their clinical profile alone. Although there is no prospective work or recommendations on ST2-guided therapy, patients with elevated ST2 levels probably warrant closer follow for signs and symptoms of decompensation as they have a substantially higher rate of hospitalizations for HF. From a decision-making perspective, the addition of ST2 may refine patient prognosis when needed for clinical decisions as recommended (IIb) by the updated 2017 HF guidelines [11]. Of note, although serial ST2 values appear to confer incremental information in clinical research, there is no guidance on when to repeat ST2 in clinical practice. Future studies need to focus on how to best use the information provided by ST2. For example, ST2 is a marker of fibrosis [1], among other properties. Therefore, agents with antifibrotic properties, e.g. mineralocorticoid receptor antagonists [33], may provide more benefit for patients with elevated ST2 levels.
5. Limitations
Our study has some limitations. Most participants were enrolled in an academic setting, with a smaller proportion coming from an urban public hospital. Therefore, our patients may not represent the HF population at large. For example, our patients were younger, more likely to be on guideline-based medical therapy, and less likely to have coronary artery disease compared to other cohorts. The number of major clinical events (death, heart transplant, ventricular assist device implantation) was small and therefore power for these events was limited. Also, we did not have detailed information on the cause of death for all patients and thus we could not provide data for cardiovascular vs. non-cardiovascular mortality. Although the total number of hospitalizations (all-cause and specific) and all-cause ED visits was adequate (i.e., >20 events per covariate), subgroup analyses and specific ED visits had reduced power; therefore, we may have missed important effects. Serial measurements were not consistently available, because of interim protocol changes and logistic limitations, and this has reduced our power to detect associations of serial ST2 with outcomes and may also have affected the reliability of these analyses. Despite use of comprehensive clinical adjustment models in our study, unmeasured socioeconomic factors may confound estimates of relative risk for healthcare resources utilization in the context of an observational design.
6. Conclusions
In this prospective cohort, elevated ST2 at index visit was a marker of higher utilization rates of healthcare resources among outpatients with HF and a marker of considerably higher risk for death or HF hospitalization during the first 6 months. The elevated risk associated with ST2 was similar for African American and Caucasian patients. How to use this information to improve outcomes in these patients by e.g. modifying disease management or modifying treatment needs further investigation.
Supplementary Material
Highlights.
In outpatients with HF, ST2 is strongly associated with 3-year hospitalization rates
ST2 levels had similar prognostic impact for African-American and Caucasian patients
The relative risks associated with elevated ST2 were higher for HF vs. non-HF events
Risk for death or HF hospitalization associated with elevated ST2 varied over time
Increases in ST2 after 6 or 12 months in a subset were associated with excessive risk
Funding:
This project was funded by an Emory University Heart and Vascular Board grant and supported in part by Public Health Service grants UL1 RR025008, KL2 RR025009, and TL1 RR025010 from the Clinical and Translational Science Award program, National Institutes of Health, and National Center for Research Resources. Critical Diagnostics (San Diego, CA) measured ST2 concentrations in blinded samples and had no role in the design of the study or the analysis and interpretation of the data.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.McCarthy CP, Januzzi JL Jr. Soluble ST2 in Heart Failure. Heart Fail Clin 2018;14:41–48. [DOI] [PubMed] [Google Scholar]
- 2.Schmitz J, Owyang A, Oldham E et al. IL-33, an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity 2005;23:479–90. [DOI] [PubMed] [Google Scholar]
- 3.Sanada S, Hakuno D, Higgins LJ, Schreiter ER, McKenzie AN, Lee RT. IL-33 and ST2 comprise a critical biomechanically induced and cardioprotective signaling system. J Clin Invest 2007;117:1538–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ky B, French B, McCloskey K et al. High-sensitivity ST2 for prediction of adverse outcomes in chronic heart failure. Circ Heart Fail 2011;4:180–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kakkar R, Lee RT. The IL-33/ST2 pathway: therapeutic target and novel biomarker. Nat Rev Drug Discov 2008;7:827–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aimo A, Vergaro G, Ripoli A et al. Meta-Analysis of Soluble Suppression of Tumorigenicity-2 and Prognosis in Acute Heart Failure. JACC Heart Fail 2017;5:287–296. [DOI] [PubMed] [Google Scholar]
- 7.Aimo A, Vergaro G, Passino C et al. Prognostic Value of Soluble Suppression of Tumorigenicity-2 in Chronic Heart Failure: A Meta-Analysis. JACC Heart Fail 2017;5:280–286. [DOI] [PubMed] [Google Scholar]
- 8.Boisot S, Beede J, Isakson S et al. Serial sampling of ST2 predicts 90-day mortality following destabilized heart failure. J Card Fail 2008;14:732–8. [DOI] [PubMed] [Google Scholar]
- 9.Gaggin HK, Szymonifka J, Bhardwaj A et al. Head-to-head comparison of serial soluble ST2, growth differentiation factor-15, and highly-sensitive troponin T measurements in patients with chronic heart failure. JACC Heart Fail 2014;2:65–72. [DOI] [PubMed] [Google Scholar]
- 10.Tang WH, Wu Y, Grodin JL et al. Prognostic Value of Baseline and Changes in Circulating Soluble ST2 Levels and the Effects of Nesiritide in Acute Decompensated Heart Failure. JACC Heart Fail 2016;4:68–77. [DOI] [PubMed] [Google Scholar]
- 11.Yancy Clyde W, Jessup M, Bozkurt B et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation 2017;136:e137–e161. [DOI] [PubMed] [Google Scholar]
- 12.O’Meara E, Prescott MF, Claggett B et al. Independent Prognostic Value of Serum Soluble ST2 Measurements in Patients With Heart Failure and a Reduced Ejection Fraction in the PARADIGM-HF Trial (Prospective Comparison of ARNI With ACEI to Determine Impact on Global Mortality and Morbidity in Heart Failure). Circ Heart Fail 2018;11:e004446. [DOI] [PubMed] [Google Scholar]
- 13.Emdin M, Aimo A, Vergaro G et al. sST2 Predicts Outcome in Chronic Heart Failure Beyond NT-proBNP and High-Sensitivity Troponin T. J Am Coll Cardiol 2018;72:2309–2320. [DOI] [PubMed] [Google Scholar]
- 14.van Vark LC, Lesman-Leegte I, Baart SJ et al. Prognostic Value of Serial ST2 Measurements in Patients With Acute Heart Failure. J Am Coll Cardiol 2017;70:2378–2388. [DOI] [PubMed] [Google Scholar]
- 15.Pfeffer MA, Claggett B, Assmann SF et al. Regional variation in patients and outcomes in the Treatment of Preserved Cardiac Function Heart Failure With an Aldosterone Antagonist (TOPCAT) trial. Circulation 2015;131:34–42. [DOI] [PubMed] [Google Scholar]
- 16.Braga JR, Tu JV, Austin PC, Sutradhar R, Ross HJ, Lee DS. Recurrent events analysis for examination of hospitalizations in heart failure: insights from the Enhanced Feedback for Effective Cardiac Treatment (EFFECT) trial. Eur Heart J Qual Care Clin Outcomes 2018;4:18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mogensen UM, Gong J, Jhund PS et al. Effect of sacubitril/valsartan on recurrent events in the Prospective comparison of ARNI with ACEI to Determine Impact on Global Mortality and morbidity in Heart Failure trial (PARADIGM-HF). Eur J Heart Fail 2018;20:760–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Claggett B, Pocock S, Wei LJ, Pfeffer MA, McMurray JJV, Solomon SD. Comparison of Time-to-First Event and Recurrent-Event Methods in Randomized Clinical Trials. Circulation 2018;138:570–577. [DOI] [PubMed] [Google Scholar]
- 19.Morris AA, McAllister P, Grant A et al. Relation of Living in a “Food Desert” to Recurrent Hospitalizations in Patients With Heart Failure. Am J Cardiol 2019;123:291–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sokoreli I, Pauws SC, Steyerberg EW et al. Prognostic value of psychosocial factors for first and recurrent hospitalizations and mortality in heart failure patients: insights from the OPERA-HF study. Eur J Heart Fail 2018;20:689–696. [DOI] [PubMed] [Google Scholar]
- 21.Stone GW, Lindenfeld J, Abraham WT et al. Transcatheter Mitral-Valve Repair in Patients with Heart Failure. N Engl J Med 2018;379:2307–2318. [DOI] [PubMed] [Google Scholar]
- 22.Bhalla V, Georgiopoulou VV, Kalogeropoulos AP et al. Contemporary outcomes of optimally treated heart failure patients with sleep apnea. Case for urgency in evaluation of newer interventions? From the Atlanta Cardiomyopathy Consortium. Int J Cardiol 2013;165:366–8. [DOI] [PubMed] [Google Scholar]
- 23.Georgiopoulou VV, Tang WHW, Giamouzis G et al. Renal biomarkers and outcomes in outpatients with heart failure: The Atlanta cardiomyopathy consortium. Int J Cardiol 2016;218:136–143. [DOI] [PubMed] [Google Scholar]
- 24.Paulus WJ, Tschope C, Sanderson JE et al. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J 2007;28:2539–50. [DOI] [PubMed] [Google Scholar]
- 25.McMurray JJ, Adamopoulos S, Anker SD et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 2012;33:1787–847. [DOI] [PubMed] [Google Scholar]
- 26.Felker GM, Fiuzat M, Thompson V et al. Soluble ST2 in ambulatory patients with heart failure: Association with functional capacity and long-term outcomes. Circ Heart Fail 2013;6:1172–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rogers JK, McMurray JJ, Pocock SJ et al. Eplerenone in patients with systolic heart failure and mild symptoms: analysis of repeat hospitalizations. Circulation 2012;126:2317–23. [DOI] [PubMed] [Google Scholar]
- 28.Royston P, Parmar MK. Flexible parametric proportional-hazards and proportional-odds models for censored survival data, with application to prognostic modelling and estimation of treatment effects. Stat Med 2002;21:2175–97. [DOI] [PubMed] [Google Scholar]
- 29.Bayes-Genis A, de Antonio M, Vila J et al. Head-to-head comparison of 2 myocardial fibrosis biomarkers for long-term heart failure risk stratification: ST2 versus galectin-3. J Am Coll Cardiol 2014;63:158–66. [DOI] [PubMed] [Google Scholar]
- 30.Broch K, Ueland T, Nymo SH et al. Soluble ST2 is associated with adverse outcome in patients with heart failure of ischaemic aetiology. Eur J Heart Fail 2012;14:268–77. [DOI] [PubMed] [Google Scholar]
- 31.Anand IS, Rector TS, Kuskowski M, Snider J, Cohn JN. Prognostic value of soluble ST2 in the Valsartan Heart Failure Trial. Circ Heart Fail 2014;7:418–26. [DOI] [PubMed] [Google Scholar]
- 32.Miller WL, Saenger AK, Grill DE, Slusser JP, Bayes-Genis A, Jaffe AS. Prognostic Value of Serial Measurements of Soluble Suppression of Tumorigenicity 2 and Galectin-3 in Ambulatory Patients With Chronic Heart Failure. J Card Fail 2016;22:249–55. [DOI] [PubMed] [Google Scholar]
- 33.Zannad F, Gattis Stough W, Rossignol P et al. Mineralocorticoid receptor antagonists for heart failure with reduced ejection fraction: integrating evidence into clinical practice. Eur Heart J 2012;33:2782–95. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.