Abstract
Introduction: Transgender women (TW) face one of the highest HIV burdens worldwide. In Malaysia, 12.4% of TW are HIV infected, ∼30-fold higher than in the Malaysian adult population. Pre-exposure prophylaxis (PrEP) is a highly effective HIV prevention strategy, however, little is known about TW's willingness to use PrEP or their preferences for receiving PrEP. This study examined the correlates of Malaysian TW's willingness to use PrEP and their attitudes and preferences related to delivery of PrEP and PrEP-related care.
Methods: Between June and August 2017, 361 TW in Malaysia completed an online survey about their knowledge of and willingness to use PrEP for HIV prevention.
Results: Only 20.2% of participants had ever previously heard of PrEP and none were currently taking PrEP. The majority (82.5%) expressed high willingness to take PrEP and most participants met the World Health Organization (WHO) indication for PrEP (82.3%). In the multivariate model, lifetime hormone use, prior postexposure prophylaxis use, and having completed a high school education were associated with higher willingness to use PrEP, while injection drug use, older age, and Chinese ethnicity were associated with lower PrEP willingness.
Conclusion: TW in Malaysia are highly willing to use PrEP for HIV prevention. Differences in willingness to use PrEP identified by education, ethnicity, substance abuse, and age suggest different strategies may be needed to scale-up PrEP for this diverse community of TW.
Keywords: HIV prevention, pre-exposure prophylaxis, transgender women, Malaysia
Introduction
Transgender women (TW) have been disproportionately affected by the HIV epidemic.1 Globally, an estimated 19% of TW are HIV infected—a 49-fold greater odds of being HIV infected compared with the general adult population.1 A recent systematic review on the global epidemiology of HIV in TW found laboratory-confirmed HIV prevalence rates in 33 studies ranging from 13.8% to 34.1%.2 In Malaysia, an estimated 12.4% (95% confidence interval: 7.8–17.1) of TW are living with HIV, compared with only 0.4% in the general population.3 TW in Southeast Asia face a multilevel risk for HIV brought on, in part, by social stigma and discrimination, as well as high engagement with sex work, in turn creating a largely hidden population of at-risk Malaysian TW.4–6 This underscores the urgent need for HIV prevention strategies tailored to the needs of TW.
Oral pre-exposure prophylaxis (PrEP) is a safe and effective tool for the prevention of HIV.7 The World Health Organization (WHO) recommends PrEP as an HIV prevention strategy for TW, and to achieve the Joint United Nations Programme on HIV/AIDS (UNAIDS) 90-90-90 targets, including a 50% reduction in HIV incidence by 2030, PrEP must be scaled up as part of comprehensive HIV prevention programs in key populations, including TW.8,9
There are, however, no evidence-based interventions for HIV prevention that are designed for TW in Malaysia. Moreover, little is known about TW's knowledge of, and willingness to use, PrEP in low- and middle-income countries (LMIC) of Southeast Asia. Of the three studies we found on PrEP among TW in Southeast Asia, PrEP acceptability varied widely, ranging from 37% in Thailand to 72% in Vietnam.10–12 Although PrEP is currently available in Malaysia, it is not included in the government's national formulary of subsidized medications and is only available for purchase with a prescription. On average, 1 month (30 tablets) of PrEP in Malaysia will cost Malaysian Ringgit (MYR) 120 (USD 30). Existing research on PrEP in Malaysia is limited to men who have sex with men (MSM), indicating that 43.6% of MSM had previously heard of PrEP, and 39.0% of respondents were willing to use it.13,14 We were unable to identify any studies exploring attitudes toward PrEP among TW in Malaysia.
Accordingly, we sought to examine Malaysian TW's knowledge about, and willingness to use, PrEP for HIV prevention by conducting a cross-sectional survey of TW in four Malaysian states. The findings reported in this article represent the first data on PrEP acceptability in Malaysian TW.
Methods
Sample and recruitment
In 2017, a total of 361 TW were recruited to complete a questionnaire about their attitudes toward and willingness to use PrEP for HIV prevention. Inclusion criteria were as follows: (1) male sex assigned at birth and reporting gender identity as female or self-identified as a TW; (2) living in Malaysia; (3) 18 years of age or older; (4) able to read or speak Bahasa Malaysia, Tamil, or English; and (5) able to provide informed consent. Interviews were conducted in three states across west Malaysia, including Selangor (inclusive of the Greater Kuala Lumpur region), Penang, and Negeri Sembilan, and in Kuantan, Pahang, in East Malaysia. These three locations were selected based on formative interviews conducted with leaders from the Malaysian transgender community, who provided guidance on selection of regions around Malaysia with established communities of TW.
In total, 381 individuals underwent eligibility screening, 374 were identified as eligible, and 361 enrolled in the study. Study participation was anonymous.
Procedures
After providing informed consent, participants completed a self-administered survey using a laptop computer in a private room. Surveys were administered using Qualtrics® Internet survey software (Qualtrics, Inc., Provo, Utah). A trained research assistant, who was also a member of the TW community, was available to respond to participants' queries. The questionnaire took ∼20 min to complete. After the survey, participants were given the opportunity to ask questions to the research staff about HIV and PrEP. Each participant was provided MYR 20 (USD 4) for their time and thanked for their participation.
Measures
Dependent variable
Before answering the survey questions about PrEP, participants read a brief paragraph explaining PrEP. PrEP was defined as “a once-daily pill that, when taken daily, can prevent you from getting HIV, even if you have sex with someone who has HIV.” The dependent variable, willingness to take PrEP, was measured by a single-item question, “How likely would you be to take PrEP if it were offered to you?” Responses were collected on a Likert-type response ranging from “not at all likely” (1) to “extremely likely” (5), with higher scores indicating greater willingness to initiate PrEP.
Independent variables
Sociodemographic characteristics, including age, ethnicity, income, education, relationship status, and housing status, were measured. Indicators of sexual risk included engagement in sex work during the last 6 months, defined as receiving money in exchange for sexual services. For participants who engaged in sex work, we assessed the average number of customers they engaged in sexual activity with during the last month. Condomless anal sex with a casual partner (defined as a person who is not a primary partner and who does not pay for sex) and regular partner (defined as a primary partner who does not pay for sex) was assessed in the last 6 months.
Sexual and general health measures were also included. Previous diagnosis with a sexually transmitted infection (STI) was defined as having ever been diagnosed with syphilis, chlamydia, or gonorrhea. Recent HIV testing was defined as having received an HIV test in the last 12 months. Lifetime and recent (last 90 days) use of hormone therapy (HT) was defined as any use of feminizing hormones for gender affirmation, including oral and injectable formulations. Recent doctor visit was defined as having been examined by a medical doctor for any reason in the last 12 months. Current depressive symptoms was measured using the 10-item Clinical Epidemiological Scale-Depression, with a score of 10 or higher indicating depressive symptoms.15 Use of amphetamine-type stimulants (ATS), including methamphetamine, and alcohol use in the lifetime and last 30 days were also measured. Lifetime drug injection behavior, excluding hormones, was defined as any previous injection of illicit drugs.
Previous involvement with the criminal justice system was assessed. Previous placement in jail or lockup (pretrial detention) was measured for lifetime. Previous placement in prison (post-trial incarceration) was also measured for experience of childhood, and adulthood physical and sexual trauma was measured using three items from the U.S. Centers for Disease Control and Prevention's Behavioral Risk Factor Surveillance System (BRFSS) questionnaire for violence and victimization.16 One additional question was added to measure adulthood sexual violence, “Since the age of 18, have you ever had any unwanted sexual experiences?”
PrEP-related measures included two binary “yes/no” questions: “Have you previously heard of PrEP” and “are you willing to pay for PrEP?” Participants were also asked, “How much are you willing to pay for your PrEP medication each month?” with a continuous-level response option of MYR 0–200 per month. Any previous use of postexposure prophylaxis (PEP) for HIV prevention was also measured. Participants were screened to determine if they met the WHO's indication for PrEP.17 Specifically, TW were classified as meeting the WHO PrEP indication if they reported any of the following: (1) vaginal or anal sex without a condom with more than one sexual partner in the last 6 months; (2) STI diagnosis in the last 6 months; or (3) any previous use of PEP. Although not specified in the WHO indication, a fourth item, “any engagement in sex work in the last 6 months,” was added to the indication criteria given the evidence associated with sex work and HIV infection. Two additional indications listed by the WHO (“requested PrEP from health care provider” and “sexual partner with one or more HIV risk factors”) were not included in the questionnaire. Participants' concerns about PrEP were also measured, including concerns related to cost, side effects, efficacy, safety, convenience of acquiring the medication, concerns about hormone interactions, convenience of taking the medication, stigma of being on PrEP, and having the support of family members. The type of clinical venue TW preferred for receiving PrEP-related care and PrEP drug dispensing was also measured, with response options of (1) government clinic; (2) private clinic; (3) community-based nongovernmental organization (NGO); (4) government hospital; or (5) other. Reasons for venue preference were also assessed, with response options of (1) privacy; (2) convenience; (3) trustworthiness; or (4) quality of medical care. Finally, participants were informed that a new, injectable formulation of PrEP may become available in the near future. Preference for oral PrEP or injectable PrEP was measured with a single-item question, “Researchers are developing a new form of PrEP that can be injected by a medical profession once every two months. If given the choice, would you prefer to take PrEP once a day as a pill or would you prefer to have an injection of PrEP once every two months?”
Ethics
All participants provided informed consent before enrollment. The study was approved by the Institutional Review Boards of Yale University and the University of Malaya.
Analysis
A series of bivariate linear regression analyses were conducted to identify significant (p<0.05) associations between willingness to use PrEP and each of the independent variables. Bivariate associations that were significant at p<0.05 were selected for inclusion in a multivariable linear regression model. Multicollinearity between independent variables was tested using the variance inflation factor (VIF). All independent variables had a VIF <2.4, indicating nonpresence of collinearity. Data were analyzed using IBM SPSS Statistics for Windows, version 24.0 (IBM Corporation, Armonk, NY).
Results
Participant characteristics
Sample characteristics are presented in Table 1. Participants were mostly of Malay ethnicity (75.1%), single (67.6%), and living in stable housing (95.0%). Participants' mean age was 35.3 years (standard deviation [SD]=9.8) and the mean monthly income was ∼1000 MYR. In the sample, 9.1% of participants had used ATS in the past 30 days, and 32.4% had used ATS in their lifetime. Low occurrence of condomless sex in the past 6 months with casual (23.0%) or primary (25.2%) sexual partners was reported. Most participants (74.5%) reported working in sex work in the past 6 months, seeing an average of 4.8 (SD=6.2) customers per day over the last month.
Table 1.
Descriptive Statistics of the Sample (n=361)
| Variable | n (%) |
|---|---|
| Sociodemographics | |
| Age (mean, SD) | (35.3, 9.8) |
| Ethnicity | |
| Malay | 271 (75.1) |
| Indian | 48 (13.3) |
| Chinese | 9 (2.5) |
| Interview site (state) | |
| Selangor (includes Kuala Lumpur) | 207 (57.3) |
| Penang | 78 (21.6) |
| Pahang | 44 (12.2) |
| Negeri Sembilan | 32 (8.9) |
| Income ≥MYR 1000 per month | 311 (86.1) |
| High school education or higher | 250 (69.3) |
| Single | 244 (67.6) |
| Living in stable housing | 343 (95.0) |
| Sexual risk behaviors | |
| Sex work (last 6 months) | 269 (74.5) |
| Sex work clients per day in last month (mean, SD) | (4.8, 6.2) |
| Solicited sex work clients via mobile app | 153 (42.4) |
| Condomless sex with casual partner(s) (last 6 months) | 83 (23.0) |
| Condomless sex with primary partner (last 6 months) | 91 (25.2) |
| Sexual and general health | |
| Previous STI diagnosis (lifetime) | 35 (9.7) |
| HIV tested (lifetime) | 287 (79.5) |
| HIV tested (last 12 months) | 221 (61.2) |
| Used HT (last 90 days) | 200 (55.4) |
| Used HT (lifetime) | 333 (92.2) |
| Seen by a doctor in last 12 months | 307 (85.0) |
| Current depressive symptoms | 202 (56.0) |
| Drug and alcohol use | |
| ATS use (last 30 days) | 33 (9.1) |
| ATS use (lifetime) | 117 (32.4) |
| Alcohol use (last 30 days) | 63 (17.5) |
| Alcohol use (lifetime) | 222 (61.5) |
| Drug injection behavior (lifetime) | 10 (2.8) |
| Criminal justice history | |
| Previously in lockup/jail (lifetime) | 132 (36.6) |
| Previously in prison (lifetime) | 77 (21.3) |
| Multiple times in lockup | 82 (22.7) |
| Multiple times in prison | 37 (10.2) |
| Physical and sexual trauma | |
| Childhood physical assault | 135 (37.4) |
| Childhood sexual assault | 149 (41.3) |
| Adulthood physical assault | 40 (11.1) |
| Adulthood sexual assault | 78 (21.6) |
| PrEP and PEP | |
| Previously aware of PrEP | 73 (20.2) |
| Meets WHO criteria for PrEP | 297 (82.3) |
| Willing to pay for PrEP | 325 (90.0) |
| Prefer using private doctor for PrEP | 106 (29.4) |
| Amount willing to pay for PrEP monthly (MYR) (mean, SD) | (69.8, 48.6) |
| Previously used PEP | 81 (22.4) |
ATS, amphetamine-type stimulant; HT, hormone therapy; MYR, Malaysian Ringgit; PEP, postexposure prophylaxis; PrEP, pre-exposure prophylaxis; SD, standard deviation; STI, sexually transmitted infection; WHO, World Health Organization.
Most participants reported having been previously HIV tested (79.5%), with 61.2% having been tested in the last 12 months. Among participants who had ever been HIV tested, the most common testing venues were government clinics (30.7%), NGOs (23.3%), government hospitals (11.4%), and private clinics (7.5%). A minority of participants reported having been previously diagnosed with an STI (9.7%), including syphilis (5.8%), gonorrhea (3.9%), and chlamydia (1.4%).
PrEP knowledge and willingness to use PrEP
Only 20.2% of participants had previously heard of PrEP. No participants were currently taking PrEP. Overall, 82% reported being “extremely willing” or “very willing” to use PrEP. Most participants (90.0%) were willing to pay for PrEP. The average amount TW were willing to pay each month for PrEP was MYR 69.8 (SD=48.2), or approximately USD 17.50. The majority of participants met the WHO indication criteria for PrEP (82.3%).
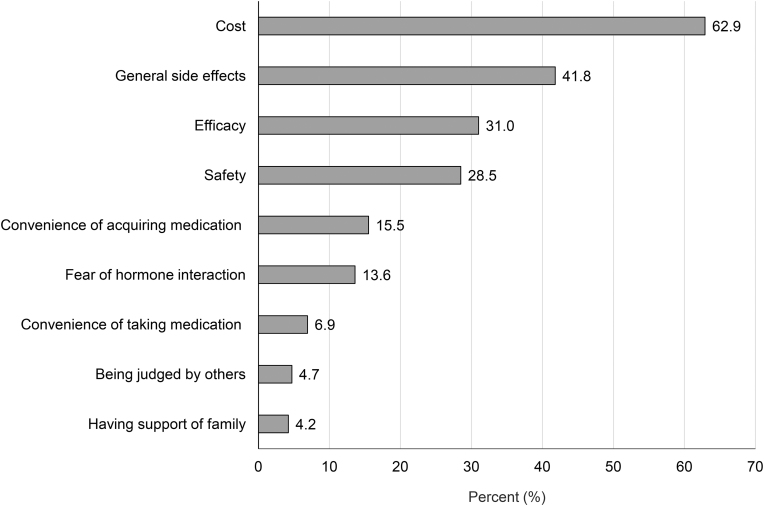
Participants' concerns about taking PrEP are illustrated in Figure 1. Cost (62.9%) was the most reported concern, followed by general side effects (41.8%), efficacy (31.0%), safety (28.5%), convenience of acquiring PrEP (15.5%), and fear that PrEP may interact with gender-affirming hormones (13.6%).
FIG. 1.
Participants' concerns related to taking PrEP (n=361).
Preferences for PrEP-related care and dispensing
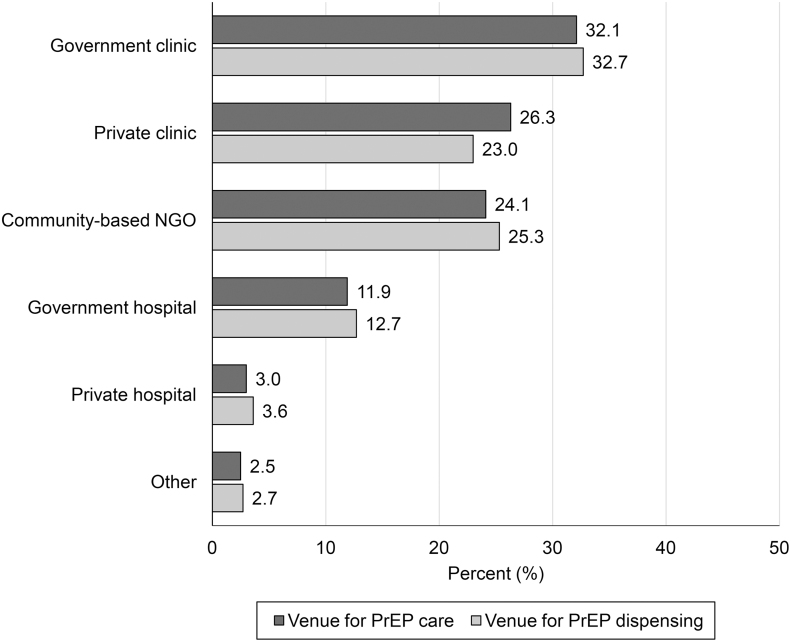
Figure 2 illustrates participants' preferred venue for obtaining PrEP-related medical care and preferred venue for dispensing of PrEP medication. The most preferred venues for PrEP-related care were government clinics (32.1%), private clinics (26.3%), and community-based NGOs (24.1%). Similarly, the most preferred venue for picking up PrEP medication was government clinics (32.7%), community-based NGOs (25.3%), and private clinics (23.0%). Participants generally preferred the same venue for obtaining PrEP-related medical care and picking up their PrEP medication. TW preferred government clinics primarily for reasons of convenience (40.0%) and trustworthiness (26.8%). Nearly half (48.5%) of participants were extremely confident that they could remember to take PrEP every day. The majority of TW said they would prefer oral PrEP (83.1%) over a bimonthly injectable formulation (16.9%), if they were given a choice. Less than a quarter of participants (22.4%) had previously used PEP.
FIG. 2.
Participants' preferred venue for receiving PrEP-related care and PrEP medication dispensing (n=361).
Bivariate and multivariate analyses
Results from the bivariate and multivariable linear regression analyses are presented in Table 2. Bivariate associations with willingness to use PrEP included having a high school education (B=0.38; p=0.003), having more sex work customers (B=0.03; p=0.008), use of mobile phone apps to find sex work customers (B=0.27; p=0.024), hormone use across the lifetime (B=0.64; p=0.003) and last 90 days (B=0.28; p=0.014), having seen a doctor in the last year (B=0.34; p=0.037), willingness to pay for PrEP (B=1.55; p<0.001), prior PEP use (B=0.27; p=0.050), and being concerned about cost (B=0.25; p=0.036). Willingness to use PrEP was lower for ethnic Chinese (B=−1.38; p<0.001), older participants (B=−0.03; p<0.001), recent amphetamine use (B=−0.52; p=0.010), lifetime injection drug use (B=−1.17; p<0.001), previous incarceration (B=−0.04; p=0.015), multiple incarcerations (B=−0.68; p<0.001), and prior knowledge of PrEP (B=−0.38; p=0.009).
Table 2.
Bivariate and Multivariate Linear Regression Analysis of Transgender Women Willingness to Use Pre-Exposure Prophylaxis (n=361)
| Variable | Bivariate analysis |
Multivariable analysis |
||||||
|---|---|---|---|---|---|---|---|---|
| B | SE | 95% CI | p | B | SE | 95% CI | p | |
| Age (mean, SD) | −0.03 | 0.01 | (−0.04 to −0.02) | <0.001 | −0.02 | 0.01 | (−0.03 to −0.01) | 0.002 |
| Ethnicity | ||||||||
| Malay | 0.25 | 0.13 | (−0.01 to 0.51) | 0.062 | ||||
| Indian | −0.32 | 0.17 | (−0.65 to 0.02) | 0.064 | ||||
| Chinese | −1.38 | 0.37 | (−2.10 to −0.66) | <0.001 | −1.08 | 0.35 | (−1.76 to −0.39) | 0.002 |
| Income ≥MYR 1000 per month | 0.27 | 0.17 | (−0.06 to 0.60) | 0.108 | ||||
| High school education or higher | 0.38 | 0.12 | (0.13 to 0.62) | 0.003 | 0.28 | 0.13 | (0.03 to 0.53) | 0.026 |
| Single | 0.04 | 0.12 | (−0.20 to 0.29) | 0.743 | ||||
| Living in stable housing | 0.36 | 0.07 | (−0.16 to 0.89) | 0.175 | ||||
| Sexual risk behaviors | ||||||||
| Sex work (last 6 months) | 0.21 | 0.13 | (−0.05 to 0.47) | 0.115 | ||||
| Sex work clients per day in last month (mean, SD) | 0.03 | 0.01 | (0.01 to 0.05) | 0.008 | 0.01 | 0.01 | (−0.01 to 0.03) | 0.281 |
| Solicited sex work clients via mobile app | 0.27 | 0.12 | (0.04 to 0.50) | 0.024 | 0.10 | 0.11 | (−0.12 to 0.32) | 0.377 |
| Condomless sex with casual partner(s) (last 6 months) | −0.07 | 0.13 | (−0.34 to 0.20) | 0.626 | ||||
| Condomless sex with primary partner (last 6 months) | 0.03 | 0.13 | (−0.24 to 0.29) | 0.841 | ||||
| Sexual and general health | ||||||||
| Previous STI diagnosis (ever) | −0.04 | 0.20 | (0.42 to 0.35) | 0.854 | ||||
| HIV tested in last 12 months | 0.16 | 0.12 | (−0.07 to 0.38) | 0.167 | ||||
| Used HT (last 90 days) | 0.28 | 0.12 | (0.06 to 0.51) | 0.014 | ||||
| Used HT (lifetime) | 0.64 | 0.22 | (0.22 to 1.06) | 0.003 | 0.49 | 0.20 | (0.09 to 0.89) | 0.016 |
| Seen by a doctor in last 12 months | 0.34 | 0.16 | (0.02 to 0.66) | 0.037 | 0.21 | 0.15 | (−0.10 to 0.51) | 0.182 |
| Current depressive symptoms | 0.11 | 0.12 | (−0.12 to 0.34) | 0.338 | ||||
| Drug and alcohol use | ||||||||
| ATS use (last 30 days) | −0.52 | 0.20 | (−0.91 to −0.13) | 0.010 | −0.32 | 0.19 | (−0.69 to 0.05) | 0.092 |
| Alcohol use (last 30 days) | 0.20 | 0.15 | (−0.10 to 0.50) | 0.194 | ||||
| Drug injection behavior (lifetime) | −1.17 | 0.35 | (−1.85 to −0.48) | 0.001 | −0.69 | 0.33 | (−1.34 to −0.03) | 0.041 |
| Criminal justice history | ||||||||
| Previously in lockup/jail (lifetime) | −0.18 | 0.12 | (−0.41 to 0.06) | 0.145 | ||||
| Previously in prison (lifetime) | −0.04 | 0.14 | (−0.62 to −0.07) | 0.015 | ||||
| Multiple times in lockup | −0.21 | 0.14 | (−0.48 to 0.07) | 0.137 | ||||
| Multiple times in prison | −0.68 | 0.19 | (−1.05 to −0.31) | 0.001 | −0.27 | 0.19 | (−0.64 to 0.11) | 0.166 |
| Physical and sexual trauma | ||||||||
| Childhood physical assault | −0.11 | 0.12 | (−0.35 to 0.13) | 0.354 | ||||
| Childhood sexual assault | −0.16 | 0.12 | (−0.39 to 0.08) | 0.186 | ||||
| Adulthood physical assault | −0.32 | 0.19 | (−0.68 to 0.05) | 0.086 | ||||
| Adulthood sexual assault | −0.10 | 0.14 | (−0.38 to 0.18) | 0.477 | ||||
| PrEP and PEP | ||||||||
| Meets WHO criteria for PrEP | 0.17 | 0.15 | (−0.12 to 0.46) | 0.256 | ||||
| Previously heard of PrEP | −0.38 | 0.14 | (−0.66 to −0.10) | 0.009 | −0.25 | 0.13 | (−0.51 to 0.02) | 0.066 |
| Willing to pay for PrEP | 1.55 | 0.18 | (1.21 to 1.90) | <0.001 | ||||
| Prefer using private doctor for PrEP | −0.13 | 0.13 | (−0.38 to 0.12) | 0.312 | ||||
| Amount willing to pay for PrEP each month (MYR) (mean, SD) | 0.01 | 0.01 | (0.01 to 0.01) | 0.015 | 0.01 | 0.01 | (0.01 to 0.01) | 0.116 |
| Previously used PEP | 0.27 | 0.14 | (0.01 to 0.55) | 0.050 | 0.25 | 0.13 | (−0.01 to 0.51) | 0.054 |
| PrEP-related concerns | ||||||||
| Cost | 0.25 | 0.12 | (0.02 to 0.49) | 0.036 | 0.19 | 0.12 | (−0.04 to 0.42) | 0.108 |
| Efficacy | −0.03 | 0.13 | (−0.27 to 0.22) | 0.832 | ||||
| Side effects | 0.22 | 0.12 | (−0.02 to 0.45) | 0.068 | ||||
Bold p-values indicate statistical significance at p<0.05.
B, unstandardized beta; CI, confidence interval; SE, standard error.
In the multivariable linear regression, hormone use (B=0.49; p=0.016) and having a high school education (B=0.28; p=0.026) were significantly associated with higher willingness to use PrEP, while prior PEP use approached significance (B=0.25; p=0.054). Lifetime injection drug use (B=−0.69; p=0.041), older age (B=−0.02; p=0.002), and Chinese ethnicity (B=−1.08; p=0.002) were associated with lower willingness to use PrEP.
Discussion
To our knowledge, this is the first study to assess willingness to use PrEP among TW in Malaysia and only the second study to assess willingness to use PrEP among a key population in Malaysia.13 This study identified high levels of willingness to use PrEP among TW in Malaysia, with 82% of participants meeting the criteria for being willing to use PrEP. This level of willingness is higher than previously surveyed TW in Southeast Asia12,18,19 and it is among the highest measured levels of PrEP acceptability for TW in the world.20–23 Relative social acceptability of identity, particularly marginal identity, bears heavily on the willingness to use PrEP in other key populations.24–26 It is likely that differences in willingness to use PrEP for HIV prevention among TW in a diversity of regional settings may be due to the specific cultural context of transgender identity, differential perception of HIV risk and PrEP utility, and spatiotemporal variations in access to HIV knowledge and sexual health interventions.23,27 Further research must be done to better understand this variation in willingness to use PrEP, and to design PrEP implementation interventions that are context driven.
The present study found that Chinese ethnicity was significantly negatively associated with willingness to use PrEP when compared with ethnic Malay and Indian TW. This result was consistent, even while controlling for other demographic factors, such as income and education. A study assessing willingness to use PrEP among MSM in Malaysia similarly identified Chinese ethnicity to be associated with lower willingness to use PrEP.13 Other studies have identified consistent differences between the health profiles of ethnic Chinese versus ethnic Malay Malaysians, which they attribute to cultural differences around the engagement of health care that drive ethnic Chinese Malaysians to have a lower likelihood of reporting poor health, and of seeking medical care.28 Future studies of PrEP among key populations in Malaysia should be particularly attentive to nuanced sociocultural and ethnoreligious factors that might provide insight into differing willingness to use PrEP among ethnicities.
Moreover, this study identified age to be independently and inversely associated with willingness to use PrEP. This result differs from other studies of PrEP willingness among TW in other LMIC settings,18,23 and also from studies of willingness to use PrEP among Malaysian MSM, in which age and willingness to use PrEP were not associated.13 That older TW were less willing to use PrEP than younger TW, while controlling for income and education level, is concerning and may point to intergenerational differences in HIV risk perception and health care knowledge. This finding necessitates further research to characterize the nature of this relationship.
Another concerning finding is that TW with a lifetime history of injecting drugs are significantly less willing to use PrEP. While a study of willingness to use PrEP among MSM in Malaysia found no relationship between willingness to use PrEP and drug use,13 and little is known about the relationship between drug use in TW and willingness to use PrEP in other settings, a study of TW sex workers in Kuala Lumpur, Malaysia, found high rates of drug use, particularly during sex work.4 The same study also found that drug use tended to increase sexual risk-taking behaviors.4 Our study found in bivariate analyses that participants who were both engaged in sex work and seeing more clients per workday, as well as those who found clients primarily on mobile phone applications were more willing to use PrEP. Although these factors were found to be nonsignificant in the multivariable analysis, these correlations may be explained by evidence that suggests sex workers are more aware of their HIV risk, which may lead them to adopt additional HIV prevention practices.29
An encouraging finding of the present study is that TW who have a lifetime history of gender-affirming hormone use are significantly more willing to use PrEP. Previous studies have posited that TW may prioritize gender-affirming HT at the expense of other health care, and that this may be a barrier to PrEP uptake in this population.30–32 The results of this study suggest that despite social marginalization and a lack of inclusion in targeted health care programming,4 TW who were engaging in gender-affirming hormone use both presently and in the past were also more willing to use PrEP. TW who have taken hormones may be more familiar with the routine of taking a daily medication, which could lead to greater willingness to use PrEP. Moreover, this finding suggests that integration of PrEP into HT, or broader gender-affirming care, could be a promising strategy for engaging TW in HIV prevention. This result highlights the strong potential for the use of PrEP for HIV prevention among Malaysian TW.
Consistent with past studies of PrEP acceptability in LMIC settings,32 cost was overwhelmingly the most frequently cited concern TW had about PrEP. However, in contrast with concerns expressed by UNAIDS that in LMIC settings, out-of-pocket cost of PrEP could present as a barrier to PrEP uptake,14 bivariate analyses found that individuals in this study who were concerned with cost were significantly more willing to use PrEP. Also notably, TW in this study preferred government clinics for acquiring a PrEP prescription. The same government clinics narrowly followed private pharmacies for preferred venue in retrieving PrEP medication. This finding suggests the potential for Malaysia to utilize existing government clinics as settings for scaling up PrEP in TW.
This study had several limitations. First, the study used venue-based and snowball sampling. This, in combination with the fact that the study was carried out primarily in urban cities across Malaysia, may have generated a sample population that was not representative of the broader population of TW in Malaysia. Consequentially, this may have biased estimates of willingness to use PrEP. However, the sociodemographic characteristics of the participants were broadly reflective of other studies of TW in Malaysia,4 and of other key populations in Malaysia.13 Future research should deploy sampling methods that can obtain a more diverse sample of TW across Malaysia.
Also, the methods by which we assessed willingness to use PrEP may have biased these estimates. A study of willingness to use PrEP among MSM in Malaysia reported that spatiotemporal variability in measured willingness to use PrEP may be due, in part, to variability of measurement instruments, with instruments with fewer item choices tending to estimate higher rates of willingness to use PrEP.13,33 However, given that our survey question assessing willingness comprised five item choices, resultant estimates of willingness to use PrEP should be lower than others derived from instruments comprising fewer options. Enthusiasm for PrEP, while high in this sample of TW, may be reduced when additional information about the requirements for routine laboratory tests, regular clinic visits, and wait times to receive PrEP refills is described to participants. Still, our estimate of overall willingness to use PrEP is among the highest measured in any sample of TW from an LMIC setting.
Lastly, we recruited a relatively small number of ethnically Chinese participants, which is an important limitation especially given the fact that Chinese ethnicity was independently negatively correlated with willingness to use PrEP. This issue is echoed by a study of TW sex workers in Kuala Lumpur, Malaysia. In that study, researchers attributed difficulties recruiting ethnically Chinese to the lack of a dedicated Chinese-language recruitment effort, which this study also lacked.4 Still, the result that ethnically Chinese TW are less willing to use PrEP is supported by studies in other key populations,13 and should inform further PrEP research in Malaysia.
Conclusions
This study is the first to assess willingness to use PrEP for HIV prevention among TW in Malaysia. High levels of willingness to use PrEP, as well as positive associations between PEP and hormone use and willingness to use PrEP, emphasize the potential for PrEP to be implemented as an effective HIV prevention strategy for TW. At the same time, negative associations between willingness to use PrEP and Chinese ethnicity, lifetime injection drug use, and age demonstrate the need for further research to more completely understand and address the needs of TW in Malaysia. The results of this study demonstrate that PrEP has the potential to play a central role in Malaysia's plan to reduce HIV transmission in accordance with its National Strategic Plan for Ending AIDS 2016–2030.
Acknowledgments
The authors wish foremost to thank the participants for their participation in this study. They also thank PAMT, IHKLAS, SEED Foundation, WAKE, PT Foundation Kuala Lumpur, FADHA Penang, and DiC Penang for both assisting in data collection and for allowing sampling to occur at their venues. The authors also thank Danisha Tahir, Jeremy Tan, Kristina Talbert-Slagle, and Fredrick L. Altice for their contributions.
Abbreviations Used
- ATS
amphetamine-type stimulant
- B
unstandardized beta
- BRFSS
Behavioral Risk Factor Surveillance System
- CI
confidence interval
- HT
hormone therapy
- LMIC
low- and middle-income countries
- MSM
men who have sex with men
- MYR
Malaysian Ringgit
- NGO
nongovernmental organization
- PEP
postexposure prophylaxis
- PrEP
pre-exposure prophylaxis
- SD
standard deviation
- SE
standard error
- STI
sexually transmitted infection
- TW
transgender women
- UNAIDS
Joint United Nations Programme on HIV/AIDS
- WHO
World Health Organization
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This research was supported by a grant from the Yale Bates Summer Fellowship, the Yale Global Health Seed Funding Award, Global Health Studies Scholarship, and a grant from the National Institute on Drug Abuse (K01 DA038529 for J.A.W.).
Cite this article as: Galka JM, Wang M, Azwa I, Gibson B, Lim SH, Shrestha R, Wickersham JA (2020) Willingness to use pre-exposure prophylaxis (PrEP) for HIV prevention and PrEP implementation preferences among transgender women in Malaysia, Transgender Health 5:4, 258–266, DOI: 10.1089/trgh.2020.0003.
References
- 1. Baral SD, Poteat T, Strömdahl S, et al. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13:214–222 [DOI] [PubMed] [Google Scholar]
- 2. Poteat T, Scheim A, Xavier J, et al. Global epidemiology of HIV infection and related syndemics affecting transgender people. J Acquir Immune Defic Syndr. 2016;72(Suppl. 3):S210–S219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Malaysia Ministry of Health. National Strategic Plan for Ending AIDS: 2016–2030. Putrajaya, Malaysia: Malaysia Ministry of Health, 2015 [Google Scholar]
- 4. Wickersham JA, Gibson BA, Bazazi AR, et al. Prevalence of human immunodeficiency virus and sexually transmitted infections among cisgender and transgender women sex workers in Greater Kuala Lumpur, Malaysia: results from a respondent-driven sampling study. Sex Transm Dis. 2017;44:663–670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Poteat T, Malik M, Scheim A, Elliott A. HIV prevention among transgender populations: knowledge gaps and evidence for action. Curr HIV/AIDS Rep. 2017;14:141–152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Poteat T, Wirtz AL, Radix A, et al. HIV risk and preventive interventions in transgender women sex workers. Lancet. 2015;385:274–286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Force USPST. Prevention of human immunodeficiency virus (HIV) infection: pre-exposure prophylaxis. https://wwwuspreventiveservicestaskforceorg/Page/Document/draft-recommendation-statement/prevention-of-human-immunodeficiency-virus-hiv-infection-pre-exposure-prophylaxis Accessed December3, 2018
- 8. Gallant JE, DeJesus E, Arribas JR, et al. Tenofovir DF, emtricitabine, and efavirenz vs. zidovudine, lamivudine, and efavirenz for HIV. N Engl J Med. 2006;354:251–260 [DOI] [PubMed] [Google Scholar]
- 9. Ristig MB, Crippin J, Aberg JA, et al. Tenofovir disoproxil fumarate therapy for chronic hepatitis B in human immunodeficiency virus/hepatitis B virus-coinfected individuals for whom interferon-alpha and lamivudine therapy have failed. J Infect Dis. 2002;186:1844–1847 [DOI] [PubMed] [Google Scholar]
- 10. Wang Z, Lau JTF, Yang X, et al. Acceptability of daily use of free oral pre-exposure prophylaxis (PrEP) among transgender women sex workers in Shenyang, China. AIDS Behav. 2017;21:3287–3298 [DOI] [PubMed] [Google Scholar]
- 11. Oldenburg CE, Le B, Toan T, et al. HIV pre-exposure prophylaxis indication and readiness among HIV-uninfected transgender women in Ho Chi Minh City, Vietnam. AIDS Behav. 2016;20(Suppl. 3):365–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zablotska I, Grulich AE, Phanuphak N, et al. PrEP implementation in the Asia-Pacific region: opportunities, implementation and barriers. J Int AIDS Soc. 2016;19(7Suppl. 6):21119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lim SH, Mburu G, Bourne A, et al. Willingness to use pre-exposure prophylaxis for HIV prevention among men who have sex with men in Malaysia: findings from an online survey. PLoS One. 2017;12:e0182838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Centers for Disease Control and Prevention. Pre-exposure prophylaxis for the prevention of HIV infection in the United States: a clinical practice guideline. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf Accessed November5, 2017
- 15. Lee AE, Chokkanathan S. Factor structure of the 10-item CES-D scale among community dwelling older adults in Singapore. Int J Geriatr Psychiatry. 2008;23:592–597 [DOI] [PubMed] [Google Scholar]
- 16. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System: BRFSS 2006 Survey Data and Documentation—Questionnaire. https://www.cdc.gov/brfss/annual_data/annual_2006.htm. Accessed November5, 2017
- 17. World Health Organization. Consolidated guidelines on HIV prevention, diagnosis, treatment, and care for key populations. Geneva, Switzerland: World Health Organization, 2016 [PubMed] [Google Scholar]
- 18. Draper BL, Oo ZM, Thein ZW, et al. Willingness to use HIV pre-exposure prophylaxis among gay men, other men who have sex with men and transgender women in Myanmar. J Int AIDS Soc. 2017;20:1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Yang D, Chariyalertsak C, Wongthanee A, et al. Acceptability of pre-exposure prophylaxis among men who have sex with men and transgender women in Northern Thailand. PLoS One. 2013;8:e76650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hoagland B, Moreira RI, De Boni RB, et al. High pre-exposure prophylaxis uptake and early adherence among men who have sex with men and transgender women at risk for HIV Infection: the PrEP Brasil demonstration project. J Int AIDS Soc. 2017;20:1–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kuhns LM, Reisner SL, Mimiaga MJ, et al. Correlates of PrEP indication in a multi-site cohort of young HIV-uninfected transgender women. AIDS Behav. 2016;20:1470–1477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Peinado J, Lama JR, Galea JT, et al. Acceptability of oral versus rectal HIV preexposure prophylaxis among men who have sex with men and transgender women in Peru. J Int Assoc Provid AIDS Care. 2013;12:278–283 [DOI] [PubMed] [Google Scholar]
- 23. Zalazar V, Aristegui I, Kerr T, et al. High willingness to use HIV pre-exposure prophylaxis among transgender women in Argentina. Transgend Health. 2016;1:266–273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. White D, Stephenson R. Identity formation, outness, and sexual risk among gay and bisexual men. Am J Mens Health. 2014;8:98–109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pitpitan EV, Smith LR, Goodman-Meza D, et al. “Outness” as a moderator of the association between syndemic conditions and HIV risk-taking behavior among men who have sex with men in Tijuana, Mexico. AIDS Behav. 2016;20:431–438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chakrapani V, Newman PA, Shunmugam M, et al. Acceptability of HIV pre-exposure prophylaxis (PrEP) and implementation challenges among men who have sex with men in India: a qualitative investigation. AIDS Patient Care STDS. 2015;29:569–577 [DOI] [PubMed] [Google Scholar]
- 27. Young I, McDaid L. How acceptable are antiretrovirals for the prevention of sexually transmitted HIV?: a review of research on the acceptability of oral pre-exposure prophylaxis and treatment as prevention. AIDS Behav. 2014;18:195–216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ismail MN. Obesity in Malaysia. Obes Rev. 2002;3:203–208 [DOI] [PubMed] [Google Scholar]
- 29. Shannon K, Strathdee SA, Goldenberg SM, et al. Global epidemiology of HIV among female sex workers: influence of structural determinants. Lancet. 2015;385:55–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sevelius JM, Deutsch MB, Grant R. The future of PrEP among transgender women: the critical role of gender affirmation in research and clinical practices. J Int AIDS Soc. 2016;19(7(Suppl. 6)):21105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sevelius JM, Keatley J, Calma N, Arnold E. ‘I am not a man’: trans-specific barriers and facilitators to PrEP acceptability among transgender women. Glob Public Health. 2016;11:1060–1075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Galea JT, Kinsler JJ, Salazar X, et al. Acceptability of pre-exposure prophylaxis (PrEP) as an HIV prevention strategy: barriers and facilitators to PrEP uptake among at-risk Peruvian populations. Int J STD AIDS. 2011;22:256–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Holt M. HIV pre-exposure prophylaxis and treatment as prevention: a review of awareness and acceptability among men who have sex with men in the Asia-Pacific region and the Americas. Sexual Health. 2013;11:166–170 [DOI] [PubMed] [Google Scholar]