Abstract
Background
Appropriate infant and young child feeding practices are the basis for child nutrition. In China, WeChat is gradually changing the channels through which people receive information. The paper aims to explore the feasibility of using WeChat to improve infant and young child feeding in rural China.
Methods
A mixed-methods study was carried out in Huzhu County, Qinghai province, China. We conducted two cross-sectional surveys with children aged 6–23 months and their caregivers in 2012 (N = 1804) and 2018 (N = 754), respectively. Quantitative data were collected on feeding knowledge and practices, caregiver’s use of smartphones and WeChat. Qualitative data were from 33 semi-structured interviews with pregnant women and mothers. In addition, we developed a WeChat feeding health education platform and asked women about their experiences with using it.
Results
In both cross-sectional surveys, less than 10% of caregivers knew that breastfeeding can be continued up to two years, less than 50% knew the accurate duration of exclusive breastfeeding, and only around 20% knew meat can be given to children from the age of 6–8 months. Similarly, the feeding practices were suboptimal and most key infant feeding practices did not change over the years. Only around 30% of caregivers ever received feeding information during pregnancy or after delivery in both surveys. Around 50% of caregivers received information from their relatives and friends, followed by 30% from health facilities and communities. More than 80% of mothers were currently using both a smartphone and the WeChat app, and 75.4% of them were willing to receive feeding information from WeChat official accounts. The WeChat feeding health education platform developed by our study team was generally well accepted by women.
Conclusions
There was an absence of accurate information sources on infant feeding and child nutrition. WeChat could be a potential way to deliver infant feeding recommendations to pregnant women and mothers in rural China.
Trial registration
ChiCTR-PRC-11001446 (The controlled intervention trial for complementary food supplements “Yingyangbao”); ChiCTR1800017364 (the randomized controlled trial for WeChat)
Introduction
Appropriate nutrition in the first few years of life is extremely important to childhood growth and development, and has lasting effects on children’s future health [1]. The critical window for child nutrition is within the first 1,000 days between conception and the age of two, and any nutritional deficits (such as anemia and stunting) acquired during this period can cause irreversible damage [2, 3]. The promotion of appropriate feeding practices can reduce the incidence of stunting and lead to better health and growth outcomes [4, 5]. Therefore, the World Health Organization (WHO) and United Nations Children’s Fund (UNICEF) recommend exclusive breastfeeding from birth to six months of age followed by the introduction of adequate complementary foods at six months and continued breastfeeding for up to two years [6].
During the past two decades, the Chinese government has made great efforts to improve infant and young child feeding. In 1998, the Ministry of Health introduced the WHO integrated management of childhood illness (IMCI) guidelines and has since implemented IMCI program in rural areas China, in which infant feeding counseling play an important part [7]. Also the Chinese infant and young child feeding (IYCF) strategy was released in 2007 by the Ministry of Health [8]. Many hospitals have been made baby-friendly to promote breastfeeding and breastfeeding week activities were organized to raise public awareness of breastfeeding in China [9–11]. Moreover, a national program called “Basic Public Health Service” has been implemented in China since 2009, in which health care workers are required to provide face-to-face breastfeeding and complementary feeding counseling to pregnant women and mothers throughout antenatal and postnatal care [12]. However, the exclusive breastfeeding rate of babies aged up to 6 months was only 20.7% in China in 2013 and the prevalence of minimum dietary diversity, meal frequency and acceptable diet among children aged 6–23 months was 53.7%, 69.1%, and 25.1%, respectively [13]. In addition, too early or too late introduction of complementary food is very common; around 20% of children younger than 4 months in poor rural areas were given complementary food, and 15% were introduced to complementary food when they were older than 9 months [13].
Women’s knowledge on infant feeding practices is crucial for the health and nutrition wellbeing of a child, which can be improved by healthcare education messages [14–16]. Currently, infant and young child feeding counseling have generally been implemented through the rural three-tier healthcare system (county-township-village) in China [12]. However, previous studies indicated that caregivers in rural areas receive feeding information mainly from family members, friends or their own experience, and rarely from health facilities [17–19]. Thus, child feeding education need to be enhanced and exploring effective ways to promote feeding practices is greatly needed.
With the widespread use of smartphones, interventions delivered through smartphone apps have been increasingly used for health promotion, such as for providing education on antibiotics or diabetes, reducing alcohol consumption, smoking cessation, or to improve diet, physical activity and reduce sedentary behaviour [20–24]. In China, the most popular smartphone app is WeChat (Tencent), which is regarded as one of the leading social networks worldwide. Founded in 2011, WeChat has 902 million daily users, and about 38 billion messages are sent on the platform every day [25]. Furthermore, in addition to messaging, WeChat offers users functions such as video calls, sharing photos and ‘moments’, games, payment, booking flight or hotels. One of the most popular functional modules of WeChat called ‘WeChat official accounts’ can be used for developers, merchants, celebrities, and organizations to communicate and interact with their audience through text, images, voice, videos and rich-media messages [26]. WeChat is gradually changing the ways people receive information, and has been used as a communication tool to change health behaviors, for example for cancer, malaria, asthma, chronic rhinosinusitis, diabetes and weight loss [27–32]. However, no studies have focused on using WeChat to support caregivers with infant and young child feeding. Therefore, this current paper aims to explore the feasibility of using WeChat as a potential way to improve infant and young child feeding in rural China.
Materials and methods
Study design and data sources
Mixed methods were used to explore the feasibility of using WeChat as a potential way to improve infant and young child feeding in Huzhu County, Qinghai province, China.
Quantitative data were derived from two cross-sectional surveys, which collected data on caregivers’ infant feeding knowledge and practices, information sources, and use of smartphones and WeChat. From 2012 to 2014, we carried out a controlled intervention trial study to evaluate the effectiveness of complementary food supplements and dietary counseling on nutrition of children aged 6–23 months in Qinghai province [33], and a cross-sectional survey was conducted in 2012 in Huzhu County as the baseline of the trial, which was the first survey for this paper. The intervention was continued to be implemented in Huzhu County after the trial study ended, and we carried out another cross-sectional survey in August 2018 to assess sustainability of intervention, which was the second survey for this paper.
Qualitative data were derived from 33 semi-structured interviews with pregnant women in their second and third trimester and mothers who had a child aged 0–6 months. These semi-structured interviews were conducted in September 2018 to obtain a better understanding of mothers’ child feeding knowledge and the feasibility of using WeChat as an infant feeding education platform.
We integrated quantitative and qualitative data to provide insights into the feasibility of using WeChat as potential way to improve infant and young child feeding. We first report quantitative data followed by qualitative data on infant feeding knowledge and practices, information sources and WeChat use.
Study setting
This study was conducted in Huzhu County, Qinghai Province, China, which was the intervention county of the controlled intervention trial study [33]. Qinghai province lies in northwest China, with a total population of 5,838,000 in 2017. There are 34 counties and 439 townships in Qinghai Province. Huzhu County, located in the northeast of Qinghai province, has a total population of 401,540 of which the rural population accounts for 76.0%. Huzhu County has 19 townships and 294 villages. The annual per capita income of rural residents in 2017 was ¥9810 (US$1414.91) [34].
Quantitative study population
Children aged 6–23 months and their caregivers in Huzhu County were participants for the two cross-sectional surveys. Children with a structural or genetic birth defect such as neural tube defects, congenital heart disease or phenylketonuria or caregivers who refused to participate were excluded.
Quantitative sample size and sampling
For the survey in 2012, the sample size calculation and the sampling was based on the study design of the intervention trial [33]. We expected to achieve a 20% reduction in the prevalence of stunting. With a power of 80% and 5% significance level, we calculated that a sample size of 1793 children aged 6–23 months per group would be sufficient. We used a two-stage sampling procedure to select children. At the first stage, we selected 150 villages out of 294 villages using proportional to population size sampling. At the second stage, we randomly selected and interviewed caregivers of 12 children from the name list of all eligible children in each village [33]. For the survey in 2018, the sample size was calculated based on data from survey in 2012 [33]. We expected to achieve a 20%-point reduction of anemia prevalence and 20–50% points increase for knowledge and appropriate feeding practices. With 80% power and 5% significance level, we estimated that a sample size of 554 children aged 6–23 months would be sufficient for all key indicators. We over-sampled 30% of children to compensate for possible refusal and loss to follow-up. We randomly selected 38 villages from the 150 villages and surveyed all eligible children aged 6–23 months in those villages.
The participants in the two surveys were not the same. In each survey, we randomly selected children aged 6–23 in the selected villages.
Quantitative data collection
We used the adapted Maternal, Newborn and Child Health household survey (MNCH HHS) tool to collect quantitative data in two cross-sectional surveys, which included socio-demographic characteristics, infant and young child feeding and common illnesses. In addition, we also collected caregivers’ use of smartphones and WeChat during the survey in 2018. We set up all the questionnaires in the specially developed software on smartphones, which interviewers used to record data [35]. Staff from the Capital Institute of Pediatrics in Beijing acted as supervisors in both surveys, and students were recruited from the School of Public Health, Qinghai University in 2012 and Qinghai Institute of Health Sciences in 2018 as interviewers. Two days’ training for each survey was carried out before the fieldwork, including communication skills, explanation of questionnaires, demonstration, role plays, field practice, and group discussions. During each survey, we asked caregivers first to come to register at village clinics, then interviewers introduced the aim of the survey, obtained written informed consent and conducted interviews with caregivers.
Quantitative data analysis
Data were automatically transferred into a Microsoft Excel sheet. After data cleaning, we converted the database into a database file (dbf) for the analysis. We carried out statistical analysis with SAS 9.2 for Windows. The median (Q1, Q3) was used to describe the age in years of mothers and grandparents. Percentages were presented for binary or categorical variables. We used the Pearson χ2–test and Fisher exact test to compare binary or categorical variables.
Five core feeding practice indicators were used to assess feeding practices according to the WHO guidelines ‘Indicators for assessing infant and young child feeding practices (Box 1) [36].
Box 1. WHO core feeding practice indicators.
Introduction of solid, semi-solid or soft foods: the proportion of infants 6–8 months of age who receive solid, semi-solid or soft foods.
Minimum dietary diversity: the indictor was four out of seven food groups per day. The proportion of children aged 6–23 months who receive foods from four or more food groups was estimated. The food groups were: a) grains, root, and tubers; b) legumes and nuts; c) dairy products (milk, yogurt, cheese); d) meat (meat, fish, poultry and liver/organ meat); e) eggs; f) vitamin-A rich fruits and green vegetables; g) other fruits and vegetables.
Minimum meal frequency: the proportion of breastfed and non-breastfed children aged 6–23 months who received solid, semi-solid, or soft foods (also including milk for non-breastfed children) the minimum number of times or more.
Minimum acceptable diet: Proportion of children aged 6–23 months who reached a minimum dietary diversity and minimum meal frequency.
Consumption of iron-rich or iron-fortified foods: Proportion of children aged 6–23 months who received iron-rich food or iron-fortified food that was specially designed for infants and young children, or that was fortified in the home.
The feasibility of using WeChat as a potential way to improve infant and young child feeding was mainly assessed by samrtphone and WeChat usage coverage among caregivers, and caregivers who were willing to receive IYCF information from WeChat official accounts.
Qualitative semi-structured interview participants and sampling
The participants in the qualitative interviews were independent from the two cross-sectional surveys in the quantitative data collection. We assumed that pregnant and mothers may well accept WeChat to deliver infant feeding recommendations. Therefore pregnant women in their second and third trimester and mothers who had a child aged 0–6 months were the study population for the qualitative semi-structured interviews. Based on our previous data, only around half main caregivers of children aged 6–23 months were mothers, and thus we did not include mothers of children aged 6–23 months in the qualitative semi-structured interviews.
We used convenience sampling to select participants in Huzhu County Maternal and Child Health Family Planning Service Centre. A total of 33 women agreed to participate the qualitative interviews, no one refused. Seventeen pregnant women in second and third trimester who came to the center to receive antenatal care were invited. Seven mothers who just gave birth in the maternity ward of the center and 9 mothers who took their children to receive child health care in the child health care clinic of the center were also invited to be interviewed.
The WeChat feeding health education platform
Before conducting the qualitative interviews, the study team developed a WeChat feeding health education platform on the local WeChat official account “Huzhu County Maternal and Child Health Family Planning Service Centre” in May 2018, which has describe in detail in our previous paper [37, 38]. We used this platform as an infant feeding intervention in a randomized controlled trial to evaluate the effectiveness on exclusive breastfeeding rate under six months in Huzhu County from May 2019 to April 2020 [37, 38].
The WeChat platform includes a feeding messages, feeding knowledge competition, baby growth chart, and online forum. The feeding messages module is for providing key breastfeeding knowledge, recommendations, and breastfeeding problems encountered for both mothers and children in the form of text, videos, and pictures. All the education messages show in the form of text, videos, and pictures. The feeding knowledge competition component aims to test how well mothers know the breastfeeding knowledge. The baby growth chart component is developed based on the WHO growth chart standard. Mothers can enter data on weight and height of their children whenever they want to monitor their children’s growth. The online forum component is designed to enable interaction between mothers and experts. And detailed description of each component was reported in our previous paper [37, 38].
Qualitative data collection
One researcher from the Capital Institute of Pediatrics (HYW (MD, graduate student, female)) conducted the face-to-face semi-structured interviews in September 2018. The researcher had qualitative interview experience before and was trained on the qualitative methodology before the interviews again. The study team developed the interview guides to understand women’s views on exclusive breastfeeding, their sources of feeding information, which were pilot tested in Huzhu County in July 2018. In addition, we also asked each pregnant woman and mothers to use the WeChat feeding health education platform and asked them for their experiences on use and satisfaction. After signing the written informed consent, participants were invited for an interview in a separate room in Huzhu County Maternal and Child Health Family Planning Service Centre, and no one else was present beside the participants and the researcher. Interviews were conducted in Mandarin, typically lasting for around 60 minutes, and were digitally recorded with the permission of each participant. Tape recordings were transcribed verbatim in Chinese by five medical students from Qinghai Institute of Health Sciences, and then the study team member who conducted the in-depth interviews validated the transcripts.
Qualitative data analysis
Content analysis was used to examine the major themes and patterns that emerged from the data. Two Chinese researchers involved in the study (WQ (MD, senior researcher, female, had qualitative interview and data analysis experience) and HYW) first read the transcripts and used MAXQDA 11 to identify themes from the data and code them independently. Then the researchers compared the themes and discussed areas of agreement and discrepancies. They further refined the themes until consensus was reached on the themes and interpretation of the findings. A total of 1053 data coders were coded. We listed all the key themes that we identified. The main coding tree was as follows: the feeding information they wanted to know, the sources of feeding knowledge, exclusive breastfeeding conception and duration, exclusive breastfeeding practice, smartphone usage, access the internet by phones, WeChat usage, WeChat official account usage, WeChat platform usage.
Ethical considerations
The study was approved by the Ethics Committee of the Capital Institute of Pediatrics. All interviewees read the Information Sheet and provided written consent. For participants who were illiterate or could not write, they asked village doctors to help them to sign their name on the sheets.
Results
Quantitative surveys’ results
Participants
A total of 1804 caregivers of children were surveyed in 2012 and 754 in 2018. In both surveys, mothers and grandparents were the main caregivers, accounting for around 50% and 45% respectively (Table 1). For the 6–11 months child age group, more than 65% of main caregivers were mothers in both surveys. Mothers who attended junior high school or above increased from 59.8% in 2012to 79.0% in 2018 (P<0.001) and only 4.0% of mothers were illiterate in 2018. The illiteracy rate for grandparents decreased over time but was still very high; 69.1% in 2012 and 60.3% in 2018, and this decrease was not significant (P = 0.057).
Table 1. Children’s main caregivers and their education in both surveys.
| Survey in 2012 | Survey in 2018 | P-valuesa | |||||
|---|---|---|---|---|---|---|---|
| 6–11 months (N = 610) | 12–23 months (N = 1194) | Total (N = 1804) | 6–11 months (N = 247) | 12–23 months (N = 507) | Total (N = 754) | ||
| Main caregivers | <0.001 | ||||||
| Mother | 65.6 | 46.9 | 53.2 | 66.4 | 40.0 | 48.7 | |
| Grandparents | 33.9 | 50.7 | 45.0 | 27.5 | 55.6 | 46.4 | |
| Father | 0.0 | 0.9 | 0.6 | 6.1 | 4.2 | 4.8 | |
| Other | 0.5 | 1.5 | 1.2 | 0.0 | 0.2 | 0.1 | |
| Mothers | |||||||
| Age in years (median (Q1, Q3)) | 25 (23, 30) | 26 (23, 30) | 26 (23, 30) | 28 (26,31) | 29 (26, 32) | 29 (26, 31) | <0.001 |
| Education, % (n)* | <0.001 | ||||||
| Illiterate | 14.1 | 14.7 | 14.5 | 3.7 | 4.2 | 4.0 | |
| Primary school | 21.4 | 24.0 | 23.1 | 12.2 | 14.5 | 13.8 | |
| Junior high school school | 52.6 | 48.9 | 50.2 | 58.9 | 57.4 | 57.9 | |
| Senior high school school or above | 9.9 | 9.4 | 9.6 | 24.0 | 19.7 | 21.1 | |
| Did not know | 2.0 | 3.0 | 2.7 | 1.2 | 4.2 | 3.2 | |
| Grandparents | |||||||
| Age in years (median (Q1, Q3)) | 50 (46, 55) | 52 (48, 58) | 51 (47, 57) | 52 (49, 57) | 54 (51, 59) | 54 (50, 59) | <0.001 |
| Education, % (n) | 0.057 | ||||||
| Illiterate | 66.7 | 69.9 | 69.1 | 57.3 | 61.0 | 60.3 | |
| Primary school | 19.8 | 17.5 | 18.1 | 26.5 | 21.6 | 22.6 | |
| Junior high school | 12.5 | 10.3 | 10.9 | 16.2 | 14.9 | 15.1 | |
| Senior high school | 0.5 | 1.5 | 1.2 | 0.0 | 1.4 | 1.1 | |
| Did not know | 0.5 | 0.8 | 0.7 | 0.0 | 1.1 | 0.9 | |
aBaseline vs follow-up for the 6–23 months age group.
Caregivers’ infant and young child knowledge and practices
As shown in Table 2, caregivers’ feeding knowledge was still poor despite having improved over the years. Less than 10% of caregivers knew that breastfeeding could be continued up to two years, less than 50% of caregivers knew the accurate duration of exclusive breastfeeding, and only around 20% of caregivers knew to start feeding children with meat from the age of 6–8 months. Similarly, infant feeding practices were suboptimal and mostly did not change, except for children who were given iron-rich or iron-fortified foods, which increased from 41.5% in 2012 to 70.9% in 2018 (P<0.001). Although more caregivers ever received breastfeeding and complementary feeding information during pregnancy or after delivery in 2018 than in 2012 ((breastfeeding information: 26.0% vs 35.2%, P<0.001; complementary feeding information: 16.2% vs 25.9%, P<0.001), the proportion was only around 30%.
Table 2. Caregivers’ infant and young child feeding knowledge and practices in both surveys.
| Indicators | Survey in 2012 | Survey in 2018 | P-values | ||||
|---|---|---|---|---|---|---|---|
| na | Nb | Percentage (%) | na | Nb | Percentage (%) | ||
| Feeding knowledge | |||||||
| Caregivers knowing the duration of exclusive breastfeeding | 336 | 1804 | 18.6 | 298 | 754 | 39.5 | <0.001 |
| Caregivers knowing continued breastfeeding until two years | 42 | 1804 | 2.3 | 47 | 754 | 6.23 | <0.001 |
| Caregivers knowing introduction of complementary foods at 6–8 months | 779 | 1804 | 43.2 | 485 | 754 | 64.3 | <0.001 |
| Caregivers knowing starting feeding children with meat at 6–8 months | 383 | 1804 | 21.2 | 148 | 754 | 19.6 | 0.362 |
| Feeding practices | |||||||
| Children breastfed until two yearsc | 39 | 502 | 7.8 | 15 | 179 | 8.4 | 0.068 |
| Children given complementary foods at 6–8 months d | 259 | 319 | 81.2 | 101 | 123 | 82.1 | 0.823 |
| Children aged 6–23 months given iron-rich or iron-fortified foods during the past 24 hours | 749 | 1804 | 41.5 | 533 | 754 | 70.7 | <0.001 |
| Children aged 6–23 months were given meat during the past 24 hours | 715 | 1804 | 39.6 | 329 | 754 | 43.6 | 0.061 |
| Minimum dietary diversity | 929 | 1804 | 51.5 | 420 | 754 | 55.7 | 0.052 |
| Minimum meal frequency | 508 | 1804 | 28.2 | 211 | 754 | 28.0 | 0.928 |
| Minimum acceptable | 188 | 1804 | 10.4 | 90 | 754 | 11.9 | 0.262 |
| Information sources | |||||||
| Caregivers ever received breastfeeding information during pregnancy or after delivery | 469 | 1804 | 26.0 | 265 | 754 | 35.2 | <0.001 |
| Caregivers ever received complementary feeding information during pregnancy or after delivery | 293 | 1804 | 16.2 | 195 | 754 | 25.9 | <0.001 |
aNumber of caregivers who responded positive on the knowledge/practices.
bTotal number of mother eligible for the question.
c Only children aged 20 to 23 months were used to calculate this indicator (From “Indicators for assessing infant and young child feeding practices”).
dOnly children aged 6 to 8 months were used to calculate this indicator (From “Indicators for assessing infant and young child feeding practices”).
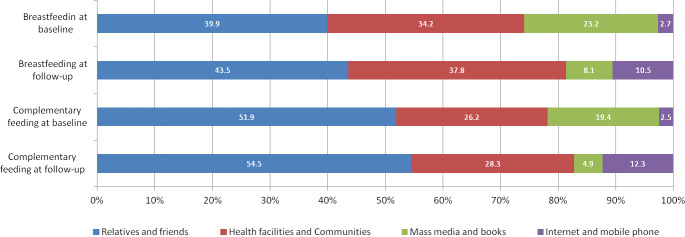
Sources of infant feeding information. Around 50% of caregivers reported having received feeding information from their relatives and friends, followed by health facilities and communities accounting for about 30% in both surveys (Fig 1). Information from mass media and books dropped from around 20% in 2012 to less than 10% in 2018, whereas Internet and mobile phones as an information source increased to more than 10% in 2018.
Fig 1. Distribution of sources for infant and young child feeding information.
Use of smartphone and WeChat
Smartphone and WeChat app usage were very popular among mothers in the survey in 2018. More than 80% of mothers were currently using both smartphone and WeChat app in their smartphones (Table 3). However, only around half of the grandparents were currently using smartphones, and less than 30% of them used WeChat app. Nearly 80% of mothers used WeChat for more than one hour every day. Around 30% of caregivers followed Infant and young child feeding official accounts, and 75.4% of them were willing to receive information from WeChat official accounts.
Table 3. Mothers’ and grandparents’ use of smartphones and WeChat in the survey in 2018 (N = 493a).
| Mothers | Grandparents | Total | ||||
|---|---|---|---|---|---|---|
| (n/N) | % | (n/N) | % | (n/N) | % | |
| Smartphone use | ||||||
| Currently using smartphones | (260/292) | 89.0 | (106/201) | 52.7 | (366/493) | 74.2 |
| Smartphone can access the internet | (236/260) | 90.8 | (56/106) | 52.8 | (292/366) | 79.8 |
| Ways to access the internet | ||||||
| WiFi at home or the workplace | (157/258) | 60.9 | (43/62) | 69.4 | (200/320) | 62.5 |
| Mobile traffic | (96/258) | 37.2 | (17/62) | 27.4 | (113/320) | 35.3 |
| Other | (5/258) | 1.9 | (2/62) | 3.2 | (7/320) | 2.2 |
| WeChat use | ||||||
| Currently using WeChat | (236 /292) | 80.8 | (58/201) | 28.9 | (294/493) | 59.6 |
| Using WeChat for more than one hour every day | (183/236) | 77.5 | (33/58) | 56.9 | (286/294) | 73.5 |
| Following infant and young child feeding official accounts | (92/236) | 39.0 | (7/58) | 12.1 | (99/294) | 33.7 |
| Willing to receive information from official accounts | (178/236) | 75.4 | (34/58) | 58.6 | (212/294) | 72.1 |
a Among 754 interviewed caregivers, there were 292 mothers and 201 grandparents.
Qualitative semi-structured interviews’ results
Participants in the qualitative interviews
A total of 17 pregnant women in their second or third trimester and 16 mothers who had a child aged 0–6 months participated in the semi-structured interviews in September 2018. The median age was 29 (ranged from 18 to 45) for pregnant women and 31 (ranged from 23 to 40) for mothers. The median gestational weeks for pregnant women were 29 weeks, ranged from 14 to 38 weeks. We interviewed seven mothers who had a children less than one week, one mother who had a child aged 2 months, and eight mothers who had children aged 4–5 months. Most of pregnant women and mothers attended junior high school or above, with four of them only attending primary school and two being illiterate. Five pregnant women and two mothers had a job, such as being a teacher, technician, or commercial service worker, and the others stayed at home for housework.
Mothers’ breastfeeding knowledge and practices in qualitative interviews
In the semi-structured interviews, pregnant women and mothers generally did not have a clear idea about exclusive breastfeeding and its recommended duration. All the interviewed pregnant women thought children should be given water during the exclusive breastfeeding period (up to six months after delivery) due to the following reasons: children may get sweaty, be thirsty, their mouths may be dry, water can replenish children’s energy and because other peoples’ advice.
Interviewed pregnant woman 1 (aged 37 years, 37 weeks of gestation, primary school education, shuangshu township) said, “Children may be thirsty (if fed only by breast milk), just like adults drink milk, milk is milk, water is water.”
Mothers’ reasons to give water to their children were: children were thirsty, refused breast milk, their stools were dry, no breast milk after delivery, hospital information. In addition, mothers fed formula or noodles to their children younger than six months, as they thought breast milk was not enough for children. The duration of exclusive breastfeeding given by pregnant women and mothers varied from 3 months to 12 months.
Interviewed mother 1 (aged 28 years, child aged 5 months, junior college education, Xishan Township) said, “Sometimes, my child’s digestion was not good, that is, his stool was dry, I would give him some water to help him digest.”
Interviewed mother 2 (aged 31 years, child aged 2 months, middle school education, Shuangshu Township) said, “The doctor told me I should give some water to my child.”
Sources of infant feeding information in qualitative interviews
In the semi-structured interviews, pregnant women and mothers said that they received feeding information from the Internet (Baidu search engine) (n = 18), hospitals (n = 17), apps on their smartphones (n = 13), the elder people (n = 7), their own experience (n = 4), maternal and child health booklets developed by local health institutions (n = 2), and books (n = 1).
Although the Internet seemed to be one of the most important sources for feeding information, pregnant women and mothers did not completely believe this information. They often referred to comments from other people, health workers, elder people at home or books before they accepted a specific piece of information.
Interviewed pregnant woman 2 (aged 24 years, 23 weeks of gestation, middle school education, Weiyuan Township) said:” I still believe doctors, and the information from the internet is only as a reference”.
Interviewed mother 3 (aged 27 years, child aged 5 days, junior college education, Weiyuan township)said: “I often searched several browsers at the same time and reviewed comments from other people, but I did not believe completely most of the time.”
Interviewed mother 4 (aged 24 years, child aged 1 days, technical secondary school education, Weiyuan Township) said: “I often read the information which had the most comments.”
WeChat usage of mothers in qualitative interviews
In the semi-structured interviews, all the pregnant women and mothers had smartphones and used WeChat, and most of them used WeChat at least more than one year. Messaging, moments, official accounts, news, and WeChat group were the most used functions. However, only one pregnant woman and two mothers followed the infant and young child feeding-related official accounts, and they explained that they had never heard of those official accounts (n = 20), or they thought it was unnecessary (n = 3). Participants who followed could read and review the contents in official accounts when they were free.
Interviewed pregnant woman 3 (aged 27 years, 14 weeks of gestation, middle school education, Shuangshu Township) said: “My (previous) children are very healthy, so I did not follow (the infant and young child feeding official accounts).”
Use experience of the WeChat feeding health education platform in qualitative interviews
Most interviewed pregnant women and mothers stated that the interface of the module was good, and they liked it. One mother said using the interface was not so smooth.
For the feeding messages module, four pregnant women and five mothers liked pictures and text for feeding knowledge as they thought it was easy to understand, they got used to reading text, or they thought videos were too fast or a bit slow. Seven pregnant women and eight mothers liked videos for feeding knowledge as they believed that videos were easy to understand, simple and convenient to watch. Other pregnant women and mothers expressed that pictures, text and videos were ‘OK’ for them. Most pregnant women and mothers said that they were interested in the feeding lecture classroom, and that the contents were easy to understand and useful.
Pregnant women wanted to know information on breastfeeding positions, how to increase breast milk supply, spitting up, child health, how to hold a baby, cough, sleep and antenatal care. Mothers wanted to know more about breastfeeding and complementary feeding, food allergies, illnesses, and growth development.
For the Baby Growth Chart module, five pregnant women and three mothers expressed that they could not understand the growth chart after they filled in the growth data.
Thirteen pregnant women and 14 mothers were willing to use this function to monitor the growth of their children. However, interviewed mother 5 (aged 33 years, child aged 2 days, Primary school education, Weiyuan Township) said: “I don’t understand the function, so I would not use it.”
Discussion
Main findings
The results of this study indicate that both pregnant women and caregivers had limited knowledge about exclusive breastfeeding and complementary feeding in our research setting in rural China. The key IYCF indicators were suboptimal and did not improve over the years. Furthermore, there was an absence of accurate information sources on infant feeding and child nutrition, and caregivers mostly received feeding information from their relatives and friends. Smartphones and WeChat app were widely used among pregnant women and mothers in this setting.
New channels are needed to deliver accurate infant feeding recommendations
Improved feeding knowledge and attitudes toward breastfeeding and complementary feeding are related to more positive child health outcomes [39, 40]. Our study indicated that the traditional infant feeding counseling provided by rural health facilities were of low quality and most of the feeding practices did not significantly improve over time, and around two-thirds of caregivers received no advice on infant feeding from health facilities. Relatives and friends were the main source of caregivers’ feeding knowledge, however, they are unlikely to have access to better information and may have misinformed mothers [17–19]. Therefore, new channels are needed in rural China to deliver accurate infant feeding information and to improve child health.
WeChat could be a potential way to deliver infant feeding recommendations
In our study, nearly 80% of mothers in the study areas used WeChat, and around 70% used WeChat more than one hour every day. Women could easily access to the internet on their smartphones, as WiFi was available at home or at the workplace. Although only 39% of mothers in the study areas followed child feeding official accounts, more than three-fourths were willing to receive feeding information in the format of text, pictures or videos through WeChat. The WeChat feeding health education platform developed by our study team was generally accepted by women, as the information was easy to understand and useful. Our platform was based on the WeChat official account of the local Maternal and Child Health Family Planning Service Centre which was trusted by women. Studies have shown that WeChat official accounts have potentials to positively impact health behavior [19–22]. Future studies are needed to test the effectiveness of a WeChat-based health education platform on key infant feeding practices in rural China.
Our study has some limitations. This study took place in one Chinese rural county and caution is needed when generalizing the findings from this study to other settings. In addition, we did not conduct qualitative interview among mothers who had children aged 6–23 months, which may not get their depth opinions on WeChat as intervention to deliver infant and young child feeding information. However, data from the survey in 2018 indicated that 75.4% of mothers aged 6–23 months were willing to received feeding information from WeChat official accounts.
Conclusions
Our study indicates that caregivers’ feeding knowledge and practices were poor in Huzhu County, and there was an absence of accurate information sources on infant feeding and child nutrition. The WeChat-based feeding health education platform was generally accepted by mothers and could also be explored in future studies to be a new channel for delivery of IYCF recommendations.
Supporting information
(XLSX)
(XLSX)
(DOCX)
Acknowledgments
The authors would like to thank all colleagues from the Huzhu Maternal and Child Health Hospital in Qinghai for providing information and helping with the study design. Also, we would like to thank the information technology company (ZYZY (Beijing) Pioneer of Cultural Essence Co. Ltd.) for providing their expertise with developing the enhanced WeChat platform.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The study is funded by the United Nations Children's Fund (UNICEF). The funder was involved in study design, preparation of the manuscript, and decision to publish.
References
- 1.Twomey A, Kiberd B, Matthews T, O’Regan M. Feeding infants—an investment in the future. Ir Med J. 2000. November;93(8):248–50. [PubMed] [Google Scholar]
- 2.Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, Ezzati M, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008. January 19;371(9608):243–60. 10.1016/S0140-6736(07)61690-0 [DOI] [PubMed] [Google Scholar]
- 3.Victora CG, Adair L, Fall C, Hallal PC, Martorell R, Richter L, et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet. 2008. January 26;371(9609):340–57. 10.1016/S0140-6736(07)61692-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013. August 3;382(9890):427–51. 10.1016/S0140-6736(13)60937-X [DOI] [PubMed] [Google Scholar]
- 5.UNICEF. Programming Guide for Infant and Young Child Feeding, Nutrition Section Programmes. New York2011.
- 6.WHO. Global Strategy for Women’s and Children’s health 2010. [Google Scholar]
- 7.Zhang Y, Dai Y, Zhang S. Impact of implementation of Integrated Management of Childhood Illness on improvement of health system in China. Journal of Paediatrics and Child Health. 2007;43(10):681–5. 10.1111/j.1440-1754.2007.01187.x [DOI] [PubMed] [Google Scholar]
- 8.Dai Y. Global strategy for Infant and Young Child Feeding. Chinese Journal of Child Health Care. 2007. December;15(6):2. [Google Scholar]
- 9.Ministry of Health China. Guidelines for Management and Supervision on Baby-friendly Hospitals. Beijing: Ministry of Health; 2002. [Google Scholar]
- 10.Donohue L. Baby Friendly Hospitals in China. Aust J Adv Nurs. 1994. December-1995 February;12(2):7. [PubMed] [Google Scholar]
- 11.Ministry of Health China. The Ministry of Health’s office of 2008 "World Breastfeeding Week " activitie notification. 2008. [Google Scholar]
- 12.Ministry of Health China. Implementation Guidelines on national basic public health service program (2009): Ministry of Health; 2009. October 16. [Google Scholar]
- 13.Duan Y, Yang Z, Lai J, Yu D, Chang S, Pang X, et al. Exclusive Breastfeeding Rate and Complementary Feeding Indicators in China: A National Representative Survey in 2013. Nutrients. 2018. February 22;10(2). 10.3390/nu10020249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vitta BS, Benjamin M, Pries AM, Champeny M, Zehner E, Huffman SL. Infant and young child feeding practices among children under 2 years of age and maternal exposure to infant and young child feeding messages and promotions in Dar es Salaam, Tanzania. Matern Child Nutr. 2016. April;12 Suppl 2:77–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vaga BB, Moland KM, Evjen-Olsen B, Blystad A. Reflections on informed choice in resource-poor settings: the case of infant feeding counselling in PMTCT programmes in Tanzania. Soc Sci Med. 2014. March;105:22–9. 10.1016/j.socscimed.2014.01.005 [DOI] [PubMed] [Google Scholar]
- 16.Piwoz EG, Huffman SL. The Impact of Marketing of Breast-Milk Substitutes on WHO-Recommended Breastfeeding Practices. Food Nutr Bull. 2015. December;36(4):373–86. 10.1177/0379572115602174 [DOI] [PubMed] [Google Scholar]
- 17.Wu Q, Scherpbier RW, van Velthoven MH, Chen L, Wang W, Li Y, et al. Poor infant and young child feeding practices and sources of caregivers’ feeding knowledge in rural Hebei Province, China: findings from a cross-sectional survey. BMJ open. 2014. July 29;4(7):e005108. 10.1136/bmjopen-2014-005108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yue A, Marsh L, Zhou H, Medina A, Luo R, Shi Y, et al. Nutritional Deficiencies, the Absence of Information and Caregiver Shortcomings: A Qualitative Analysis of Infant Feeding Practices in Rural China. PLoS One. 2016;11(4):e0153385. 10.1371/journal.pone.0153385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yue A, Zhang N, Liu X, Tang L, Luo R, Yang M, et al. Do Infant Feeding Practices Differ Between Grandmothers and Mothers in Rural China? Evidence From Rural Shaanxi Province. Fam Community Health. 2018. Oct-Dec;41(4):233–43. 10.1097/FCH.0000000000000198 [DOI] [PubMed] [Google Scholar]
- 20.Fralick M, Haj R, Hirpara D, Wong K, Muller M, Matukas L, et al. Can a smartphone app improve medical trainees’ knowledge of antibiotics? Int J Med Educ. 2017. November 30;8:416–20. 10.5116/ijme.5a11.8422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Plotnikoff RC, Wilczynska M, Cohen KE, Smith JJ, Lubans DR. Integrating smartphone technology, social support and the outdoor physical environment to improve fitness among adults at risk of, or diagnosed with, Type 2 Diabetes: Findings from the ’eCoFit’ randomized controlled trial. Prev Med. 2017. December;105:404–11. 10.1016/j.ypmed.2017.08.027 [DOI] [PubMed] [Google Scholar]
- 22.Gajecki M, Andersson C, Rosendahl I, Sinadinovic K, Fredriksson M, Berman AH. Skills Training via Smartphone App for University Students with Excessive Alcohol Consumption: a Randomized Controlled Trial. Int J Behav Med. 2017. October;24(5):778–88. 10.1007/s12529-016-9629-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Haskins BL, Lesperance D, Gibbons P, Boudreaux ED. A systematic review of smartphone applications for smoking cessation. Transl Behav Med. 2017. June;7(2):292–9. 10.1007/s13142-017-0492-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schoeppe S, Alley S, Van Lippevelde W, Bray NA, Williams SL, Duncan MJ, et al. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: a systematic review. Int J Behav Nutr Phys Act. 2016. December 7;13(1):127. 10.1186/s12966-016-0454-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liao S. How WeChat came to rule China-The multipurpose messaging app is becoming the nation’s ID systerm 2018. [Google Scholar]
- 26.WeChat. Official Account Introduction—WeChat. Available from: http://act.wechat.com/showcase/resource/OA_introduction.pdf.
- 27.Zhang X, Xiao H, Chen Y. Evaluation of a WeChat-based life review programme for cancer patients: A quasi-experimental study. J Adv Nurs. 2019. April 5. 10.1111/jan.14018 [DOI] [PubMed] [Google Scholar]
- 28.Li W, Han LQ, Guo YJ, Sun J. Using WeChat official accounts to improve malaria health literacy among Chinese expatriates in Niger: an intervention study. Malar J. 2016. November 24;15(1):567. 10.1186/s12936-016-1621-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cao Y, Lin SH, Zhu D, Xu F, Chen ZH, Shen HH, et al. WeChat Public Account Use Improves Clinical Control of Cough-Variant Asthma: A Randomized Controlled Trial. Med Sci Monit. 2018. March 14;24:1524–32. 10.12659/msm.907284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Feng S, Liang Z, Zhang R, Liao W, Chen Y, Fan Y, et al. Effects of mobile phone WeChat services improve adherence to corticosteroid nasal spray treatment for chronic rhinosinusitis after functional endoscopic sinus surgery: a 3-month follow-up study. Eur Arch Otorhinolaryngol. 2017. March;274(3):1477–85. 10.1007/s00405-016-4371-0 [DOI] [PubMed] [Google Scholar]
- 31.Dong Y, Wang P, Dai Z, Liu K, Jin Y, Li A, et al. Increased self-care activities and glycemic control rate in relation to health education via Wechat among diabetes patients: A randomized clinical trial. Medicine (Baltimore). 2018. December;97(50):e13632. 10.1097/MD.0000000000013632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.He C, Wu S, Zhao Y, Li Z, Zhang Y, Le J, et al. Social Media-Promoted Weight Loss Among an Occupational Population: Cohort Study Using a WeChat Mobile Phone App-Based Campaign. J Med Internet Res. 2017. October 23;19(10):e357. 10.2196/jmir.7861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang YF WQ, Wang W, van Velthoven MH, Chang SY, Han HJ, Xing M, et al. Effectiveness of complementary food supplement and dietary counseling on anemia and stunting in children aged 6–23 months in poor areas in Qinghai Province, China: a controlled interventional study. BMJ open. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huzhu County People’s Government. 2017 government report of Huzhu County. 2018, http://www.huzhu.gov.cn/contents/211/10406.html (In Chinese).
- 35.Zhang S, Wu Q, van Velthoven MH, Chen L, Car J, Rudan I, et al. Smartphone Versus Pen-and-Paper Data Collection of Infant Feeding Practices in Rural China. J Med Internet Res. 2012;14(5):e119. 10.2196/jmir.2183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.WHO U, USAID, AED, UCDAVIS, IFPRI. Indicators for assessing infant and young child feeding practices-part 1 Introduction. WHO 2010. [Google Scholar]
- 37.Wu Q, Huang Y, van Velthoven MH, Wang W, Chang S, Zhang Y. The effectiveness of using a WeChat account to improve exclusive breastfeeding in Huzhu County Qinghai Province, China: protocol for a randomized control trial. BMC Public Health. 2019. December 2;19(1):1603. 10.1186/s12889-019-7676-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wu Q, Huang Y, Liao Z, van Velthoven MH, Wang W, Zhang Y. Effectiveness of WeChat for Improving Exclusive Breastfeeding in Huzhu County China: Randomized Controlled Trial. J Med Internet Res. 2020. December 3;22(12):e23273. 10.2196/23273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Spiby H, McCormick F, Wallace L, Renfrew M, Dsouza L, Dyson L. A systematic review of education and evidence-based practice interventions with health professionals and breast feeding counsellors on duration of breast feeding. Midwifery. 2009;25(1):50–61. 10.1016/j.midw.2007.01.006 [DOI] [PubMed] [Google Scholar]
- 40.Dewey KG, Adu-Afarwuah S. Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. Matern Child Nutr. 2008. April;4 Suppl 1:24–85. 10.1111/j.1740-8709.2007.00124.x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
(XLSX)
(DOCX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.