Abstract
In the last 11 months, the SARS-CoV-2 pandemic has overwhelmed and disrupted the whole world in health, social and economic terms. We are progressively learning more and more about the epidemiological and clinical features that distinguish CoViD-19 from any previous experience in the emergency and critical care setting. Experiences are multiplying with regard to the use of non-invasive respiratory support techniques in the context of acute hypoxemic respiratory failure secondary to CoViD-19-related pneumonia. Doubts still far outweigh certainties, but a growing series of mostly monocentric and retrospective studies are becoming available as concrete decision-making and operational support for healthcare workers. In this review the available studies and experiences about non-invasive respiratory support in the treatment of Covid-19 related respiratory failure, mainly coming from outside the ICU setting, will be discussed.
Keywords: Covid-19 pneumonia, Acute hypoxemic respiratory failure, Non-invasive respiratory support, High-flow nasal cannulae, non-invasive ventilation
1. Introduction
While many of the epidemiological aspects and clinical characteristics of CoViD-19 disease have been understood [1], [2], [3], little has been clarified regarding the best ventilatory support to offer to affected patients. Most of the available studies are the result of monocentric experiences and are retrospective. As a consequence, many indications derive from theoretical assumptions and there is a substantial uncertainty regarding the timing, the definite indications, the duration, the success/ failure criteria of the methods.
In order to contribute to answer these questions, we consulted Pubmed with the following search terms: Covid-19 pneumonia and acute hypoxemic respiratory failure and Non-invasive respiratory support or Non-invasive ventilation, or CPAP, or Non-invasive pressure support ventilation, or non-invasive positive pressure ventilation, or high flow nasal cannulae, or high flow nasal oxygen for the years 2019 and 2020. The articles thus retrieved were selected on the basis of the following data: clear indication of the population studied, the patient inclusion criteria, clinical outcomes and success / failure predictors with particular attention to non-intensive care unit (ICU) settings.
2. A disease of a different kind
Approaching the use of non-invasive respiratory support techniques in hypoxemic respiratory failure due to CoViD-19 pneumonia, we must consider that we are facing with a peculiar pathophysiology. Unlike other pathologies in which non-invasive ventilation (NIV) has been recommended, CoViD-19 pneumonia is characterized by the development of lung injury which starts with a phase of prevalent interstitial and microvascular involvement and subsequently results in a more classic picture of diffuse alveolar damage with hyaline membranes formation, edema and fibrotic deposition [4]. It is possible to hypotesize that in the first phase lung compliance will not be significantly compromised and hypoxemia will mainly depend on the loss of the physiological mechanism of hypoxic vasoconstriction due to the inflammatory storm and the appearance of microthrombi [5,6] .
It follows that, for a good part of its course, the most suitable strategy to treat this condition is the progressive escalation of oxygen therapy, rather than the alveolar recruitment by positive pressure, the latter to be reserved for a later phase of full-blown acute respiratory distress syndrome (ARDS) [7] .
In this scenario, the role of non-invasive respiratory support (NRS) techniques, and of NIV in particular, is, at best, controversial. On the one hand, NIV carries the risk of generating excessive negative intrathoracic pressure fluctuations, increasing the risk of self-induced lung injury, and there is concern that it can cause a delay in intubation and the need for emergency airway management [8]. On the other hand, however, it should be considered that, among the non-invasive methods, continuous positive airway pressure (CPAP) consists in the application of a single level of pressure during the entire respiratory cycle, significantly reducing the risk of excessive transpulmonary pressures. Furthermore CPAP can increase the resistance in the small vessels of the non-dependent regions of the lung, favoring the redistribution of perfusion to newly recruited dependent areas in patients who have lost the mechanism of hypoxic vasoconstriction [9].
3. The outbreak of the pandemic
Some experiences conducted in the first phase of the epidemic in Europe in the operational context of the Emergency Department (ED) have described a situation characterized by an exponential growth of admitted patients and the urgent need to make more beds available in the ICU, coupled with their rapid occupation [10], [11], [12]. Criteria for initiating CPAP or non-invasive positive pressure ventilation (NPPV) in the various studies were a PaO2 of less than 60 mmHg or an oxygen saturation lower than 90-94% and or a respiratory rate greater than 25 per minute and signs of respiratory distress after application of non-rebreathing mask. In a similar way, these experiences showed a success rate (defined as avoidance of intubation and in-hospital death) of no more than one third of patients. Success predictors appeared to be a better PaO2 / FiO2 ratio or SpO2 at entry, a younger age, fewer comorbidities, earlier use of CPAP or a limited extension of lung lesions on Computed Tomography. Consistently, the authors of the various works concluded that, although the success rate of NIV techniques is not high, it is possible to identify about one third of patients who require respiratory support and who benefit from non-invasive techniques in a severe ICU bed crisis situation. In the phase immediately following the outbreak of the pandemic in Europe, new high dependency respiratory units (HDRUs) with an adequate personnel/patient ratio were specifically dedicated to treating patients with respiratory insufficiency due to CoViD-19 pneumonia with NRS techniques, in order to save the use of ICU beds. In this operational context, some studies describe a failure rate (considered both as the need for intubation and as in-hospital mortality) of around 30%, lower than that of the aforementioned studies and probably related to a better organizational setting [13], [14], [15]. Still the main predictors of death remain a lower PaO2 / FiO2 ratio at admission, older age and the presence of comorbidities, while younger and less comorbid patients were the most frequently intubated. Note the different frequency of contagion between operators equal to 11.4% in the study by Franco eta al. [13] and absent in the study of Nightingale et al., conducted in negative pressure chambers [14]. The experience of Burns et al. conducted on DNI patients (frailty score 5, average age 81.5) is also of some interest, which had a success rate of 50%, comparable to that of patients intubated in ICU, usually younger and with less co-morbidities, confirming the potential role of NRS techniques as part of a respiratory support protocol for Covid-19 related respiratory failure [15] .
Finally, Bellani and co-workers reported of 909 patients treated with NIV (85% CPAP, mainly by helmet) outside the ICU in a prospective single day observational study. Failure rate was 37,6% and was associated with lower PaO2/FiO2 ratio, higher C-reactive Protein (CRP), and platelet count [16].
It is therefore conceivable that the organization of dedicated units with appropriate staff and monitoring, along with the warranty of cooperation between different specialties and together with the correct selection of patients, could be the right way to safely apply CPAP outside the ICU, particularly in situations characterized by limited resources and reduced availability of mechanical ventilation.
Table 1 summarizes the main results of the above mentioned studies.
Table 1.
Studies on the use of CPAP/non-invasive ventilation in Covid-19-related pneumonia. Legenda: n. of pts: number of patients; DNI: Do Not Intubate; hCPAP. Helmet CPAP; NPPV: non-invasive postitive pressure ventilation; HFNC: high flow nasal cannulae; NRB: non rebreathing mask; RR: respiratory rate; SpO2: Oxygen pulse saturation; PaO2: arterial Oxygen partial pressure; AHRF: acute hypoxemic respiratory failure; PaO2/FiO2: the ratio between arterial oxygen partial pressure and fractional concentration of inspired oxygen; CXR: Chest radiography; CRP: C-reactive Protein. NR: not reported.
| Study | Design | n. of pts | Technique | Failure% | Starting crit. | Failure pred. |
| Duca et al. | Retrospective | 85 | hCPAP (71); NPPV (7); IMV (7) | 88,5% Deaths: 76.5% |
PaO2< 60, RR>30 in NRB mask |
age > 60 |
| Alviset et al. | Retrospective | 49 | Mask CPAP | 53% Deaths: 36% |
SpO < 90% in NRB mask |
Low basal PaO2 |
| Di Domenico et. Al. | Retrospective | 90 (27 DNI) |
CPAP/NPPV | 57% Deaths: 47% 89% in DNI |
SpO2 < 90% or < 94% on O2 12- 15 l/min |
Low basal PaO2/FiO2 ratio |
| Franco et al. | Prospective | 670 | 163 HFNC, 330 hCPAP, 177 NPPV | 30% Deaths: 30% |
SpO2 < 94% RR > 20 poor response to O2 15 L/min | Age, n. of comorbidities, Low PaO2/FiO2 |
| Nightingale et al. | Retrospective | 24 | Mask CPAP | 38% | Type 1 AHRF | Age, n. of comorbidities |
| Burns et al. | Retrospective | 28 (DNI) | Mask CPAP (23) NPPV (5) |
Deaths: 50% | SpO2 < 94% In O2 40% |
«Typical» aspect on CXR |
| Bellani et al | Prospective | 909 | CPAP 85% (mainly via helmet), NPPV 10%; HFNC 5% | 37,6% | n.r. | Lower PaO2/FiO2 ratio; higher CRP; platelet count |
4. Do NRS techniques impact outcome?
Due to the lack of a control population, the aforementioned studies do not allow us to express an opinion on the effectiveness of NRS techniques. In a differently conceived retrospective study, Oranger and coworkers compared a series of patients requiring oxygen to maintain a saturation greater than 90%, prior to the introduction of a protocol that involved the application of CPAP, with a similar population after the introduction of the above mentioned strategy [17]. The protocol that provided for the use of CPAP sorted a significantly lower number of intubations with a number of patients free from intubation at 7 and 14 days significantly higher than in the period prior to the introduction of the protocol. In addition, the Authors clear that, with regards to safety, none of the patients treated with CPAP had required emergency intubation or showed cardiac arrest, somehow alleviating concerns about the potential delay in intubation.
Similarly, in a small study Mukhtar reports of a population of patients treated with different techniques in the ICU in Cairo (Egypt) [18]. In the results patients treated with NIV had characteristics of severity and respiratory status comparable to those treated with invasive ventilation; however, the latter showed a significantly higher mortality. These data could suggest a protective role of NIV in this type of patients, but more carefully designed prospective studies are needed to answer this question.
5. The role of High Flow Nasal Cannulae
As to the role of HFNC, it has to be considered that following its early implementation in the pandemic [19] the available guidelines recommend its use even before resorting to NIV [20, 21]. In a retrospective study conducted in a HDRU in the Veneto region of Italy, 28 patients with CoViD-19 related pneumonia, a PaO2/FiO2 ratio less than 300 and the inability to maintain O2 saturation above 92% with a non-rebreathing mask were treated with HFNC in the context of a protocol that involved escalating therapy from conventional oxygen therapy [22] to HFNC and up to NIV and endotracheal intubation in unresponsive patients. Nineteen (67.8%) of the patients avoided intubation and were discharged from HDRU, while 9 (32.2%) required NIV, and among these 5 (17.8%) were finally intubated. Patients who failed treatment had a significantly lower PaO2 / FiO2 ratio at entry and a higher serum CRP level than responders. In multivariate analysis, PaO2 / FiO2 value below 100 was significantly associated with the failure of HFNC.
Patel et Al. applied HFNC to 104 consecutive patients with moderate to severe Covid-19 related hypoxemia at Temple University Hospital in Philadelphia (United States) [23]. As an institutional policy in this center, treatment with HFNC is preferred over NIV and is maintained as long as oxygenation and work of breathing allow. Of the treated patients, 67 avoided intubation (64.42%). Overall, 45 patients escalated the ventilatory therapy, 37 (35.58%) of these requiring intubation and 8 (7.69%) NIV. Fifteen patients died (14.44%), of which 13 (34.4%) in the group that required intubation and 2 (2.9%) in the group that did not. In multivariate analysis SpO2 / FiO2 ratio of less than 100, chronic renal failure and fibrinogen value less than 450 mg / dl were independently associated with the need for intubation.
Interestingly, in these studies inflammation indices are associated in a variable and often contradictory way with the outcomes, as it will also be evident for some other studies on prone positioning highlighting the need for more studies in this area. Table 2 Summarizes the main results of these studies.
Table 2.
Studies on the use of HFNC in Covid-19-related pneumonia. Legenda: n. of pts: number of patients; HFNC: high flow nasal cannulae; NPPV: non invasive positive pressure ventilation; n.r.: not reported; PaO2/FiO2: the ratio between arterial oxygen partial pressure and fractional concentration of inspired oxygen; RR: respiratory rate; NRB: non rebreathing mask; SO2/FiO2: the ratio between oxygen saturation and fractional concentration of inspired oxygen.
| Study | Design | n. of pts | Technique | Failure % | Starting criteria |
Failure predictors |
| Wang et al. | Retrospective | 17 | HFNC | 41% (7 needed NIV, 2 of which Escalated to ETI) |
NR | PaO2/FiO2 < 200 And not improving in 1-2 h; high RR and not improving in 1-2 h |
| Vianello et al. | Retrospective | 28 | HFNC | 32% (needed NPPV) 17,8% (intubation) |
PaO2/FiO2 < 300 and Inability to maintain SpO2 > 92% with a NRB mask |
PaO2/FiO2 < 100 Higher CRP |
| Patel et al. | Retrospective | 104 | HFNC | 35.58% (intubation) 14.44% (deaths) 7.69% (needed NPPV) |
Need for O2 > 15 L/min | SO2/FiO2 < 100 Renal failure Fibrinogen < 450 mg/dl |
An extensive systematic review by Agarwal et al. concluded that the use of HFNC may reduce the need for invasive ventilation compared with conventional oxygen therapy (COT) and it may also reduce the need for escalation of therapy (i.e. the need for another non-invasive technique or invasive ventilation) [24]. Results provided no support for differences in mortality, hospital or ICU length of stay, patient reported dyspnea or comfort, complications when compared to COT, nor provided any definite information on the risk of droplets dispersion associated with HFNC.
Also considering the paucity of contagion events among operators reported in the aforementioned studies, our opinion is that HFNC may prove to be a valid tool in correcting hypoxemia in up to two thirds of patients with CoViD-19 related pneumonia who are unable to achieve oxygen saturation greater than 92% with conventional oxygen therapy.
6. The role of awake prone-positioning
Following preliminary reports highlighting the effectiveness of the method on a short-term physiological basis in patients treated with conventional oxygen therapy in the ED [25], some centers experimented with the possibility of increasing the efficacy of NRS by applying awake prone positioning. Through pronation it should be possible to redistribute perfusion and pulmonary ventilation, albeit temporarily, in order to improve their matching in the lung [9].
A retrospective study reports 48 patients treated with CPAP or HFNC [26]. A pronation protocol was attempted (at least two pronation periods of two hours a day for two consecutive days) in 30%. In multivariate analysis, mortality rate was directly associated with age and inversely with the achievement of full proning.
Over a two-week period, Foti and coworkers prospectively enrolled with awake pronation 47 CoViD-19 patients treated with helmet CPAP or conventional oxygen therapy for acute hypoxemic respiratory failure (AHRF) [27]. The main outcome was the change in oxygenation from baseline, following the return to the supine position after a three-hour pronation period. Oxygenation significantly improved by more than 50% in the supine to prone transition, but this was not significantly maintained upon resuming the supine position. Twenty-three patients who showed significant improvement in oxygenation at this stage were referred to as responders: prone positioning was initiated significantly earlier from hospital admission in responders, and they had significantly lower platelets and higher CRP and LDH than non-responders. Lower PaO2/FiO2 at baseline was associated with a significant increase after resuming the supine position.
Some Authors in Italy proposed the combination of helmet-CPAP and pronation as an operative standard when treating AHRF due to CoViD-19 [9] as a safe, comfortable and relatively easy-to-use method in a scenario of maximum discrepancy between facilities and number of casualties.
It follows that awake prone positioning may represent a further contribution to redistribute ventilation / perfusion ratio in the early highly inflammatory phase of CoViD-19 to improve oxygenation and lung compliance, and to reduce the oxygen requirement in a strategy of "time saving”.
7. Suggestions for a protocolized approach
Some Authors concerned to provide operational indications, in the lack of conclusive evidences on the effectiveness of any NRS method and to provide useful practical information to avoid waste of ICU resources.
Bellone and collaborators propose helmet CPAP for non-responders to conventional oxygen (5 liters per minute for 10 - 15 minutes) [28], clinically monitoring every 30 minutes for the first two hours, gradually increasing PEEP from 7.5 cmH2O to 12.5 if the goal is not reached (SpO2 > 94%, RR < 25 bpm). In case of improvement CPAP is continued, possibly alternating intervals with HFNC; with no improvement the patient is selected for tracheal intubation or palliative treatment. In hypercapnic or COPD patients, a similar pathway with bilevel ventilation is offered, but for a shorter trial period of 60 minutes.
Pelosi et al. suggest helmet CPAP for those who cannot maintain SpO2 > 95% with PaO2/FiO2 > 200 with oxygen via non-rebreathing mask (15 liters per minute for 15 minutes) [8]. If no improvement is achieved after three to six hours, intubation should be considered.
Radovanovic and coworkers propose helmet CPAP in case of PaO2 / FiO2 ratio < 250, regardless of RR, or with sudden respiratory distress (RR > 30 bpm) [29]; the target is SpO2 > 97% and must be achieved by CPAP titration (starting from 5 cm H2O up to maximum 10-12). Reevaluation should be assessed after first 20 and 120 minutes of treatment. In the absence of response, the haemodynamic state, the activation of the accessory muscles of respiration, the impairment of the central drive and clinical complications should be checked. In case of unsatisfactory response, despite treatment optimization, the patient should be considered for a transfer to ICU. If, on the contrary, an adequate response is obtained, a program of support de-exacalation is initiated from the seventy-second hour of treatment.
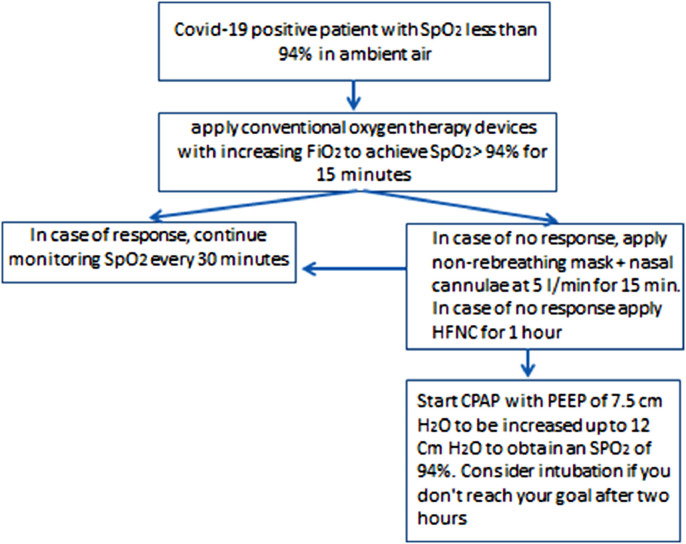
Figure 1 represents an example of an algorithm for a protocolized approach to patients suffering Covid-19 related AHRF.
Figure 1.
Suggestion for an algorithm to be adopted in a protocolized approach to the patient with Covid-19 related respiratory failure. In the absence of solid evidence on the management of these patients, this was the alogorhythm adopted in the center of one of the authors of this article (PG). Legenda: SpO2: Saturation of arterial blood with oxygen as measured by pulse-oxymetry; FiO2: Fractional concentration of inspired oxygen; Conventional oxygen therapy devices: nasal cannuae, venture mask, non-rebreathing mask; HFNC: high flow nasal cannulae; CPAP: continuous positive airway pressure; PEEP: positive end expiratory pressure.
Due to the peculiar pathophysiology of this disease, it is important to maintain a gradual administration of respiratory support (oxygen escalation) [30]. However, a retrospective study comparing 373 CoViD-19 patients with a similar group admitted to the same hospitals for viral pneumonia between 2013 and 2017, showed that rapid growth in oxygen requirements itself is highly predictive of the need for positive pressures [31].
8. Concerns about the risks of contagion among health care workers
Dealing with a communicable disease, through the dispersion of droplets, it is essential to consider the possibility that NRS devices may represent a risk of contagion for healthcare personnel. In this field, available studies are very inhomogeneous with each other in terms of methods and results [23, 32]. From what is available it can be stated that the least droplet-dispersive devices are represented by the helmet, the non-rebreathing mask and HFNC. Other devices have a different dispersion potential depending not only on their structural properties, but also on the pressures used. It is therefore strongly recommended for healthcare personnel to work in negative pressure rooms or in isolated and well ventilated rooms, avoiding the use of excessive positive pressures, taking care to cover the devices with surgical masks, when possible, using adequate personal protection equipment, avoiding aerosol generating procedures and emergency intubations.
9. Conclusions
Non-invasive respiratory support techniques are feasible outside the ICU in patients with AHRF secondary to CoViD-19 pneumonia. Evidence is lacking about their efficacy / safety profile. Notwithstanding this, they respond to a strategy to “buy time” in the scenario of shortage of ICU resources. A large part of the existing experience in this field resides on this strategy. Much more prospective studies are needed in order to define the timing for initiation, duration, suspension, failure and success of these methods
Declaration of competing interest
Both Authors declare no conflicts of interest.
References
- 1.Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human reapiratory disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- 3.Verity R, Okell LC, Dorigatti I, Winskill P, Whittaker C, Imai N, et al. Estimates of the severity of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020;20(6):669–677. doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gattinoni L, Coppola S, Cressoni M, Chiumello D. Am J Respir Crit Care Med. 2020 May 15;201(10):1299–1300. doi: 10.1164/rccm.202003-0817LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Potus F, Mai V, Lebret M, et al. Novel insights on the pulmonary vascular consequences of Covid-19. Am J Physiol Lung Cell Mol Physiol. 2020;319:L277–L288. doi: 10.1152/ajplung.00195.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dohnt S, Derom E, Van Braekel E, et al. The pathophysiology of “happy” hypoxemia in Covid-19. Respiratory Research. 2020;21:198. doi: 10.1186/s12931-020-01462-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gattinoni L, Chiumello D, Caironi P, et al. Covid -19 pneumonia: different respiratory tratments for different phenotypes? Intensive Care Med. 2020;14:1–4. doi: 10.1007/s00134-020-06033-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robba c, Battaglini D, Ball L, et al. Distinct phenotypes require distinct respiratory management strategies in severe Covid-19. Resp Physiol Neurobiol. 2020;279 doi: 10.1016/j.resp.2020.103455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Longhini F, Bruni A, Garofalo E, et al. Helmet continuous postive airway pressure and prone positioning: a proposal for an early management of Covid-19 patients. Pulmonol. 2020;26(4):186–191. doi: 10.1016/j.pulmoe.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duca A, Memaj I, Zanardi F, et al. Severity of respiratory failure and outcome of patients needing a ventilatory support in the Emergency Depatment during Italian novel coronavirus SARS-CoV2 outbrak: preliminary data on the role of helmet CPAP and non-invasive positive pressure ventilation. EClinicalMedicine. 2020;24 doi: 10.1016/j.eclinm.2020.100419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alviset S, Riller Q, Aboab J, et al. Continuous positive airway pressure (CPAP) face-mask ventilation is an easy and cheap option to manage a massive influx of patients presenting acute respiratory failure during the SARS-CoV-2 outbreak: a retrospective cohort study. PLoS ONE. 2020;15(10) doi: 10.1371/journal.pone.0240645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Di Domenico SL, Coen D, Bergamaschi M et al. Clinical characteristics and respiratory support of 310 Covid-19 patients, diagnosed at the emergency room: a single-center retrospective study. 2020 Nov 11;1-10. [DOI] [PMC free article] [PubMed]
- 13.Franco C, Facciolongo N, Tonelli R, et al. Feasibility and clinical impacto of out-of-ICU non-invasive respiratory support in patients with COVID-19 related pneumonia. Eur Respir J. 2020 Nov 5;56(5) doi: 10.1183/13993003.02130-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nightingale R, Nwosu N, Kutubudin F, et al. Is continuous positive airway pressure (CPAP) a new standard of care for type 1 respiratory failure in Covid-19 patients? A retrospective observational study of a dedicated Covid-19 CPAP service. BMJ Open Respir Res. 2020;7(1) doi: 10.1136/bmjresp-2020-000639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burns GP, Lane ND, Tedd HM, et al. Improved survival following ward-based non-invasive pressure support for severe hypoxia in a cohort of frail patients with Covid-19: retrospective analysis from a UK teaching hospital. BMJ Open Respir Res. 2020;7(1) doi: 10.1136/bmjresp-2020-000621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bellani G, Grasselli G, Cecconi M, et al. Noninvasive ventilator support of Covid-19 patients outside the intensive care units (WARd-COVID). ANNALSATS Articles in Press. Published January 04, 2021 as 10.1513/AnnalsATS.202008-1080OC.
- 17.Oranger M, Gonzalez-Bermejo J, Dacosta-Noble F, et al. Continuous positive airway pressure to avoid intubation in SARS-CoV-2 pneumonia: a two-period retrospective case-control study. Eur Respir J. 2020;56 doi: 10.1183/13993003.01692-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mukhtar A, Lofty A, Hasanin A, et al. Outcome of non-invasive ventilation in Covid-19 critically ill patients: a retrospective observational study. Anaesth Crit Care Pain Med. 2020;39:579–580. doi: 10.1016/j.accpm.2020.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang K, Wei Z, Ji L, et al. The experience of high-flow nsala cannula in hospitalized patients with 209 novel coronavirus-infected pneumonia in two hospitals of Chongqing, China. Ann Intensive Care. 2020;10:37. doi: 10.1186/s13613-020-00653-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alhazzani W, Hylander Moeller M, Arabi YM, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (Covid-19) Intensive Care Med. 2020;46(5):854–887. doi: 10.1007/s00134-020-06022-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Institute of Health (NIH). Coronavirus disease 2019 (Covid-19). Treatment Guidelines. 2020 https://www.covid19treatmentguidelines.nih.gov/. [PubMed]
- 22.Vianello A, Arcaro G, Molena B, et al. High flow nasal cannula oxygen therapy to treat patients with hypoxemic acute respiratory failure consequent to SARS-CoV-2 infection. Thorax. 2020;75(11):998–1000. doi: 10.1136/thoraxjnl-2020-214993. [DOI] [PubMed] [Google Scholar]
- 23.Patel M, Gangemi A, Marron R, et al. Retrospective analysis of high flow nasal therapy in Covid-19-related moderate-to-severe hypoxaemic failure. BMJ Open Respir Res. 2020;7(1) doi: 10.1136/bmjresp-2020-000650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Agarwal A, Basmaji J, Muttalib F, et al. High-flow nasal cannula for acute hypoxemic respiratory failure in patients with COVID-19: systematic reviews of effectiveness and its risks of aerosolization, dispersion, and infection transmission. Can J Anesth. 2020;67(9):1217–1248. doi: 10.1007/s12630-020-01740-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Caputo ND, Strayer RJ, Levitan R. Early self-proning in awake, non-intubated patients in the Emegency Department: a single ED's experience during the COVID-19 Pandemic. Acad Emerg Med. 2020;27(5):375–378. doi: 10.1111/acem.13994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hallifax RJ, Porter BML, Elder PJD, et al. Succesful awake proning is associated with improved clinical outcomes in patients with COVID-19: single-centre high-dependency unit experience. BMJ Open Respir Res. 2020;7(1) doi: 10.1136/bmjresp-2020-000678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Coppo A, Bellani G, Winterton D, et al. Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study. Lancet Respir Med. 2020;8(8):765–774. doi: 10.1016/S2213-2600(20)30268-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Privitera D, Angaroni L, Capsoni N, et al. Flowchart for non-invasive ventilation support in COVID-19 patients from anorthern Italy Emergency Department. Intern Emerg med. 2020;15(5):767–771. doi: 10.1007/s11739-020-02370-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Radovanovic D, Rizzi m, Pini S, et al. Helmet CPAP to treat acute hypoxemic respiratory failure in patients with Covid-19: a mangement strategy proposal. J Clin Med. 2020;9:1191. doi: 10.3390/jcm9041191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Long B, Lyang SY, Hicks C, Gottlieb M. Just the facts: what are the roles of oxygen escalation and noninvasive ventilation in Covid-19? CJEM. 2020:1–4. doi: 10.1017/cem.2020.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pimentel MAF, Redfern OC, Hatch R, et al. Trajectories of vital signs in patients with Covid-19. Resuscitation. 2020;156:99–106. doi: 10.1016/j.resuscitation.2020.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Crimi C, Noto A, Cortegiani A, et al. Noninvasive respiratory support in acute hypoxemic respiratory failure associated with COVID-19 and other viral infections. Minerva Anestesiol. 2020 doi: 10.23736/S0375-9393.20.14785-0. [DOI] [PubMed] [Google Scholar]