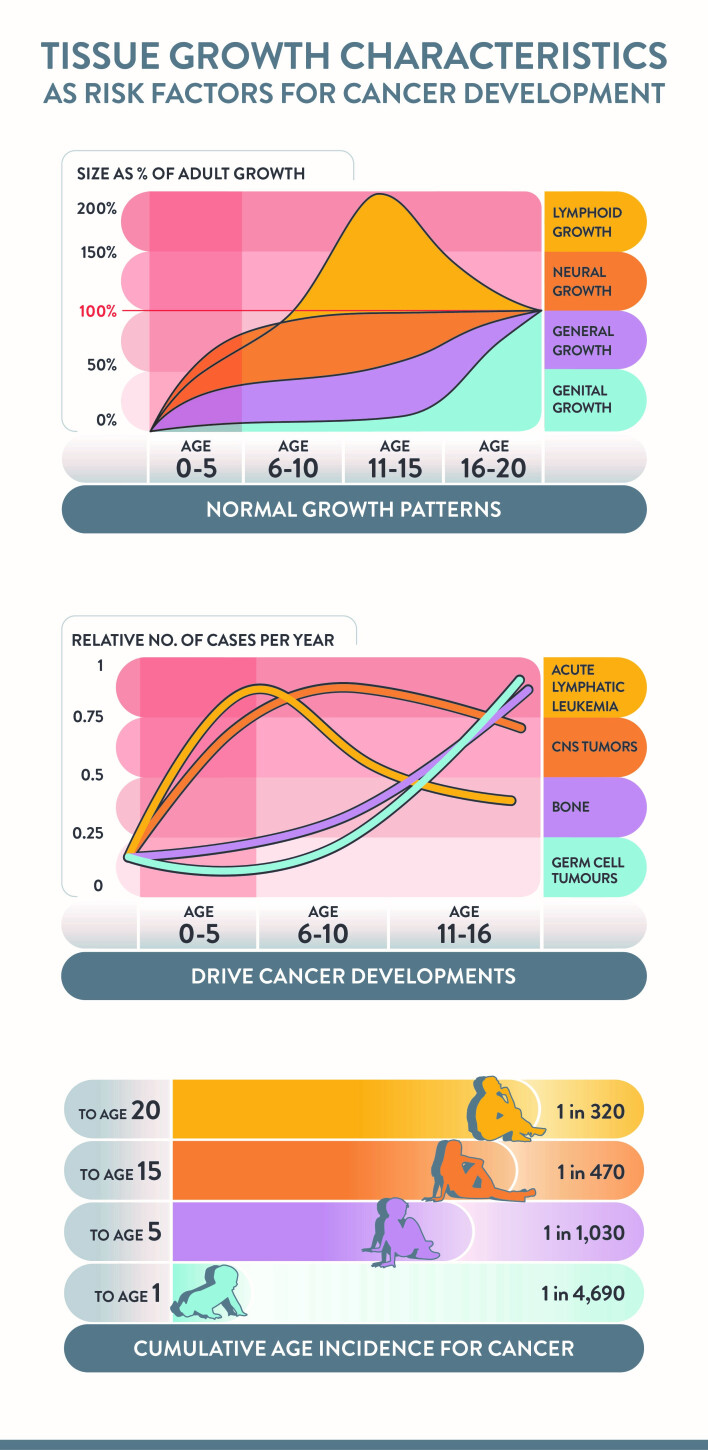
It is a misconception that cancer is rare in children and young people (CYP, aged <21 years), which contributes to GPs and paediatricians feeling inhibited from initiating cancer investigations until they are clearly progressive. This contributes to risk of delays in diagnosis and consequent adverse outcomes. As CYP constitute only 20%–25% of the population, it is estimated that a general practice will see a CYP with cancer every 1.8 years, an individual GP therefore may see only 1 per 5/10-year period.1 A recent review rephrased the risk of childhood cancer from a population perspective, to the risk for each child (Figure 1). This calculation shows that a child’s cancer risk rises from being very low (1 in 4700) in the first year of life, rising rapidly until 5 years of age (1 in 1000), achieving a moderate risk by 15 years (1 in 450) and a substantial risk by 20 years (1 in 320). These risks are comparable to risk of other common childhood conditions such as diabetes, epilepsy, and bacterial meningitis. Inherited factors play a part for a minority, associations with genetic conditions such as neurofibromatosis types 1 and 2, family cancer syndromes, and tissue overgrowth syndromes are established; rarer genetic mutations are being increasingly recognised.2
Figure 1.
Tissue growth characteristics as risk factors for cancer development.5,12,13
There is a demonstrable relationship between the age-incidence of different cancer types and the rate of physiological growth of the host tissues.3 The risk is highest in the first 5 years of life, when solid tumours and brain tumours together are more common than leukaemia. The combination of normal tissue growth and cancer development combines to make the cancers grow rapidly and present acutely. Delays can have profound clinical impact. These facts about risk mean that, while the risk of the individual GP making a diagnosis of cancer is very low, the risk for each child is significant. It is clearly not in the children’s interests for it to be disregarded. The GP needs diagnostic support with enhanced awareness, training, and guidelines relevant to current day practice.
DELAYS MATTER
UK population child cancer survival outcomes compare unfavourably to those in Northern Europe. Disease staging data of abdominal tumours shows that UK children present with larger and more advanced staged tumours,4 resulting in more intensive and prolonged therapies, risking worse survival rates, increased toxicities, and higher costs to the NHS and families. The reasons for this adverse comparison include problems with accessing GP appointments and the need for a GP referral to paediatrics, with attendant delays, for any childhood diagnostic test. When cancers present with life-threatening or disabling presentations, such as severe bone marrow failure, tumour lysis syndrome, superior vena cava syndrome, raised intracranial pressure, or spinal cord compression;5 intervals measured in hours can make the difference between life and death, and degrees of lifelong disability. With the less acute clinical presentations that occur, the total diagnostic interval (TDI) from symptom onset to diagnosis is a sum of accumulated intervals. The National Institute for Health and Care Excellence (NICE) suspected cancer guideline was launched in 2005 to accelerate cancer diagnosis6 and remains an NHS health priority, although the referral pathways are seldom used for children’s cancer.7
The HeadSmart campaign was launched in 2011 to disseminate the Royal College of Paediatrics and Child Health (RCPCH) guideline for childhood brain tumour diagnosis.8 This project was launched in response to public concerns about delays in diagnosis. Population data demonstrated that the TDI for childhood brain tumours fell from a median of 14.5 weeks to a median of 6.4 weeks between 2009 and 2013. The NICE cancer referral guidelines were revised in 2015, excluding children’s specialists; guidance for children’s cancers and leukaemias were integrated with adult cancers, using positive predictive values for ‘red flag symptoms’.9 Sadly, this approach was not sufficiently informative for children.10 The guidance did not identify the HeadSmart campaign despite its NHS evidence status, methodologies, or impact. The current NICE guidance is limited to a subset of childhood cancers and is incompatible with current GP practice, access to expert advice, or investigations within intervals. Supplementary guidelines based on a multiple stakeholder Delphi consensus process are in preparation by NICE.11
AWARENESS WORKS
The HeadSmart campaign, using precise evidence-based and age-stratified symptom advice, was disseminated widely to the public and profession supported by a mixed methods awareness campaign, public and professional champions, and a decision support website, and was monitored in its impact by a national quality improvement project. The guidance and campaign were revised in 2015 and relaunched by the President of the Royal College of General Practitioners, targeting the teenage population.8 Using this evidence, there is confidence that a carefully designed awareness campaign communicating evidence-based guidelines can change practice in CYP age groups.
A new project raising awareness of all child cancers is in progress. It is called Child Cancer Smart. A recent Ipsos MORI public survey of child cancer knowledge, showed that the majority of responders underestimated the risk of cancer in children, selected symptoms predictive of adult rather than childhood cancers, and did not recognise that disturbed growth or pubertal development were indicators of childhood ill health. Their estimate of safe intervals for health advice-seeking were measured in weeks and months for most symptoms. Such low awareness and imprecise knowledge highlights the communication challenge being faced.
PRECISE GUIDANCE
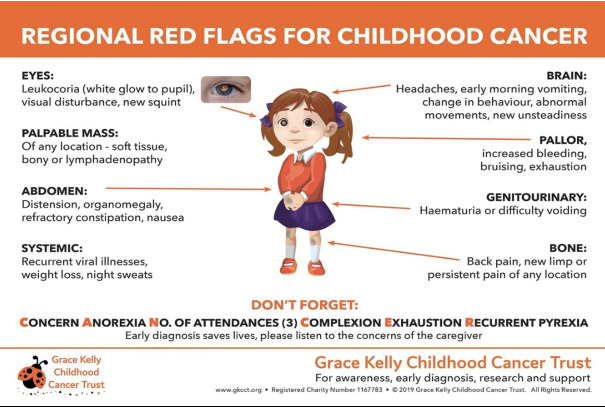
Given that childhood cancers have specific symptom presentations across the age span from 12 major categories, condensing the range of presentations to a digestible format for communication is a critical step in awareness messaging. The Grace Kelly Childhood Cancer Trust awareness tool1 will be used as a template for further refinement with the new evidence, as it emerges (Figure 2). The effectiveness of the campaign will be measured by monitoring referral pathways, 1 year survival rates, and shifts in staging of newly diagnosed patients. The aim is to reduce the risk of early, life threatening or disabling presentations and shift the staging distribution to lower categories and thereby reduce the need for more complex treatments with their side effects, and build greater confidence in the NHS for children and their families.
Figure 2.
Grace Kelly Child Cancer Trust Diagnostic support tool.1
TAKE HOME MESSAGE
For the GP today, acknowledgement that the child’s risk of cancer is almost greater than the individual GP’s risk of seeing it in their clinic, is the first step. A similar challenge is faced by paediatricians and specialist doctors seeing children. The Child Cancer Smart campaign will be raising public awareness of child cancer risk, the typical symptoms, and recommended actions. For the practitioner, identifying evidence-based decision support online and participating in training would be compatible with duties as a GP for training in resuscitation, which is a similarly rare event. There is a significant additional challenge for the current use of online consultations in children’s practice, a useful toolkit supporting this change has been produced. One research conclusion was three visits with the same symptoms within 3 months in a CYP raised risk for cancer diagnosis by ten-fold, ‘three strikes and you are in’ may serve as a useful mantra.10 Parents and practitioners have ‘gut feelings’, which for the sake of a test or a scan should not be disregarded.14 ‘Lifting the phone to ask for specialist help’ is a tried and tested strategy, when worried. No-one wants to miss such serious illness in CYP, where their interests are paramount, the consequences of delay can be so dramatic and the family’s concerns so profound.
Acknowledgments
The HeadSmart project was funded by The Health Foundation Closing the Gaps Award, The Samantha Dickson Brain Tumour Trust/The Brain Tumour Charity, and The National Community Lottery Fund, The Children’s Brain Tumour Research Centre at the University of Nottingham. Child Cancer Smart is a collaboration between Children’s Cancer and Leukaemia Group (CCLG) and the University of Nottingham, in partnership with CLIC Sargent and the Grace Kelly Childhood Cancer Trust.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
REFERENCES
- 1.Children’s Cancer & Leukaemia Group (CCLG), Grace Kelly Ladybird Trust . Childhood cancer: care and treatment. Information for general practitioners (GPs) Leicester: CCLG; 2018. [Google Scholar]
- 2.Ripperger T, Bielack SS, Borkhardt A, et al. Childhood cancer predisposition syndromes — a concise review and recommendations by the Cancer Predisposition Working Group of the Society for Pediatric Oncology and Hematology. Am J Med Genet A. 2017;173(4):1017–1037. doi: 10.1002/ajmg.a.38142. [DOI] [PubMed] [Google Scholar]
- 3.Scotting PJ, Walker DA, Perilongo G. Childhood solid tumours: a developmental disorder. Nat Rev Cancer. 2005;5(6):481–488. doi: 10.1038/nrc1633. [DOI] [PubMed] [Google Scholar]
- 4.Coleman MP, Forman D, Bryant H, et al. Cancer survival in Australia, Canada, Denmark, Norway, Sweden, and the UK, 1995–2007 (the International Cancer Benchmarking Partnership): an analysis of population-based cancer registry data. Lancet. 2011;377(9760):127–138. doi: 10.1016/S0140-6736(10)62231-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Theis J. Oncologic emergencies in pediatric patients: what oncology nurses need to know. Oncology Times. 2014;36(7):2–4. [Google Scholar]
- 6.National Institute for Health and Care Excellence (NICE) Referral guidelines for suspected cancer. CG27. London: NICE; 2005. [Google Scholar]
- 7.NHS England . Delivering cancer waiting times: a good practice guide. London: NHS England; 2014. [Google Scholar]
- 8.Shanmugavadivel D, Liu J-F, Murphy L, et al. Accelerating diagnosis for childhood brain tumours: an analysis of the HeadSmart UK population data. Arch Dis Child. 2020;105(4):355–362. doi: 10.1136/archdischild-2018-315962. [DOI] [PubMed] [Google Scholar]
- 9.NICE . Childhood cancers — recognition and referral: symptoms suggestive of childhood cancers. London: NICE; 2020. [Google Scholar]
- 10.Dommett RM, Redaniel T, Stevens MCG, et al. Risk of childhood cancer with symptoms in primary care: a population-based case-control study. Br J Gen Pract. 2013 doi: 10.3399/bjgp13X660742. [DOI] [PMC free article] [PubMed]
- 11.Murray MJ, Ruffle A, Lowis S, et al. Delphi method to identify expert opinion to support children’s cancer referral guidelines. Arch Dis Child. 2020;105(3):241–246. doi: 10.1136/archdischild-2019-317235. [DOI] [PubMed] [Google Scholar]
- 12.Harris JA, Jackson CM, Paterson DG, Scammon RE. The measurement of man. Minneapolis, MN: University Minnesota Press; 1930. [Google Scholar]
- 13.Office for National Statistics (ONS) Cancer registration statistics, England: 2017. London: ONS; 2019. [Google Scholar]
- 14.Smith CF, Drew S, Ziebland S, Nicholson BD. Understanding the role of GPs’ gut feelings in diagnosing cancer in primary care: a systematic review and meta-analysis of existing evidence. Br J Gen Pract. 2020 doi: 10.3399/bjgp20X712301. [DOI] [PMC free article] [PubMed]