Abstract
Background:
Mindfulness-training may benefit stress response and stress-eating, yet few studies have experimentally tested these effects in adolescents. In this short communication, we report whether a brief mindfulness-induction affected acute stress response and stress-eating in adolescents at-risk for adult obesity. We explored disordered eating as a moderator.
Method:
Twenty-nine adolescents (age 14±2y) at-risk for adult obesity participated in a within-subjects, randomized crossover experiment. Following a 10-minute mindfulness or neutral-induction on different days in random order, the Trier Social Stress Test adapted for adolescents was administered, followed by an ad libitum lunch meal. Physiological stress response (heart rate, blood pressure) and subjective stress response (anxiety, mindlessness) were determined with area under the curve with respect to increase. Stress-eating was measured as test meal energy consumed. Global disordered-eating and binge-eating were assessed with the Eating Disorders Examination-Questionnaire.
Results:
Relative to a neutral-induction, a mindfulness-induction reduced state anxiety response (p=.04). There were significant interactions of induction-type by global disordered-eating (p=.02) and binge-eating (p=.03), such that the mindfulness-induction most reduced anxiety response in adolescents with relatively lower global disordered-eating and those with no binge-eating. Induction-type also interacted with binge-eating in predicting diastolic blood pressure (p=.03). A mindfulness-induction, versus neutral-induction, most reduced diastolic blood pressure response in adolescents with binge-eating.
Conclusions:
Brief mindfulness-training may alter some aspects of acute stress response, with variations by disordered-eating. Future research should test alternative mindfulness induction-types (e.g., acceptance/self-compassion) to improve our understanding of how mindfulness-training may benefit adolescents at-risk for adult obesity.
Keywords: adolescent, mindfulness, stress, disordered-eating, binge-eating
1. Introduction
Dispositional mindfulness—a continuum of the propensity for non-judgmental present-moment attention (Kabat-Zinn, 1994)—can be taught and may address disordered-eating (Godfrey, Gallo, & Afari, 2015), maladaptive eating that includes binge-eating or consumption of a large amount accompanied by a sense of loss-of-control (American Psychiatric Association, 2013). Most studies on mindfulness/disordered-eating have been in adults (Katterman, Kleinman, Hood, Nackers, & Corsica, 2014). Yet, binge-eating typically emerges in adolescence (Swanson, Crow, Le Grange, Swendsen, & Merikangas, 2011) and predicts excess weight gain and worsening metabolic problems (Tanofsky-Kraff et al., 2012). Adolescence is characterized by increases in perceived stress, disordered-eating, and heightened subjective (e.g. anxiety) and physiological (e.g., heart rate, blood pressure) stress sensitivity (Loth, van den Berg, Eisenberg, & Neumark-Sztainer, 2008; Romeo & McEwen, 2006). Stress may also increase reliance on eating to cope with difficulties (i.e., stress-eating), which likely affects obesity and cardiometabolic disease risk (Johnson, Cohen, Kasen, & Brook, 2002). Although mindfulness offers a promising approach for reducing stress and associated eating among adults, scant experimental studies have tested whether inducing mindfulness affects these facets in adolescents.
From an affective theoretical framework, mindfulness may alleviate anxiety that precipitates the onset and exacerbation of binge-eating (Rosenbaum & White, 2013). State anxiety predicts greater intake among adolescents with binge-eating and precedes naturalistic binge-eating (Ranzenhofer et al., 2014; Shank et al., 2017). From a neurobiological framework, the hedonic value of food is enhanced during anxiety-provoking situations (Adam & Epel, 2007). In line with these frameworks, mindfulness-training to alleviate anxiety/stress could be anticipated to reduce disordered-eating.
In associational adult studies, higher dispositional mindfulness has been associated with lower perceived stress (Brown & Ryan, 2003), more adaptive stress-responding (e.g., lower heart rate; Bullis, Bøe, Asnaani, & Hofmann, 2014), and healthier eating (Ouwens, Schiffer, Visser, Raeijmaekers, & Nyklíček, 2015). In college students, higher mindfulness has been related to altered cortisol/anxiety response to a laboratory stressor (Brown, Weinstein, & Creswell, 2012; Lucas-Thompson, Miller, Seiter, & Prince, 2019), healthier eating (Jordan, Wang, Donatoni, & Meier, 2014), and less binge-eating (Roberts & Danoff-Burg, 2010). In adolescents with overweight/obesity, higher mindfulness also has been associated with less disordered-eating, binge-eating, and eating in the absence of hunger (Annameier et al., 2018; Pivarunas et al., 2015).
In a small body of experimental studies, brief (approximately 10–25 minute) mindfulness-inductions reduced perceived stress after a laboratory stressor in adults (Creswell, Pacilio, Lindsay, & Brown, 2014) and decreased snack food consumption among college students (Arch et al., 2016). Understanding acute effects of brief mindfulness-induction on stress response/stress-eating in adolescents is needed.
To address this gap, we evaluated effects of brief mindfulness-induction on acute subjective/physiological stress response/stress-eating in adolescents at-risk for adult obesity, based upon above-average body mass index (BMI) or obesity family history. In line with previous research (e.g., Arch et al., 2016; Creswell et al., 2014), mindfulness-induction was expected to lower state anxiety, mindlessness (inverse of mindfulness), heart rate (HR), systolic/diastolic blood pressure (SBP/DBP) stress response, and decrease stress-eating. We explored global disordered-eating (continuum of maladaptive eating attitudes/behaviors) and binge-eating (presence/absence of uncontrolled overeating) as moderators. Distinct obesity subtypes are likely undergirded by different mechanisms and require different interventions (Gillman & Hammond, 2016). Thus, exploring variability in effects of mindfulness-induction by disordered-eating offers utility for future adaptations of mindfulness-training for adolescents at-risk for adult obesity.
2. Method
2.1. Participants
Participants were N=29 boys and girls (45%) 12–17y (M±SDage 14.4±1.8y) who identified as non-Hispanic White (62%), Hispanic (35%), or Asian/Pacific Islander (3%; Supplemental Table 1). Adolescents were selected for being at-risk for adult obesity based on BMI≥70th percentile or obesity family history (parental BMI≥30 kg/m2). Most adolescents had obesity (59%; BMI≥95th percentile). Participants were recruited for a study about health behaviors through letters/flyers to area-families, physician offices, and other advertisements. Exclusion criteria were psychiatric symptoms that could impede compliance, major medical problems (e.g., diabetes), medication use affecting weight/mood, and pregnancy (females). The Institutional Review Board approved all procedures.
2.2. Procedures
A within-subjects, randomized crossover experiment occurred on two days 6±4weeks apart. Participants were instructed to fast after 10:00pm before both visits. On day one, after consent/assent, height (cm)/weight (kg; unblinded) were measured to compute BMI (kg/m2) and BMI-z/percentile (Kuczmarski et al., 2002) and the disordered-eating survey was administered. On both days, adolescents were served a standardized breakfast shake at ~9:00am. The laboratory stress-eating paradigm was administered at ~11:00am. After resting for 10-minutes, adolescents were exposed in random order to either a 10-minute audio-recorded mindfulness-induction involving focused-breathing, shown to increase breath/body awareness, or an audio-recorded neutral-induction to focus on whatever came to mind (Hafenbrack, Kinias, & Barsade, 2014). Next, the Trier Social Stress Test (TSST) adapted for adolescents (Yim, Quas, Cahill, & Hayakawa, 2010) was administered. The TSST involves preparation (3-minutes) and delivery of a 5-minute speech and a challenging 4-minute oral arithmetic task in front of a neutral evaluator, and consistently demonstrates robust subjective/objective adolescent stress-response (Seddon et al., 2020). Finally, adolescents were served a 4,500-kcal lunch and instructed, “eat as much as you normally would” (Tanofsky-Kraff et al., 2009). Foods were individually weighed before/after eating. Energy intake was determined from manufacturer data. Stress-eating measured with this paradigm relates to heightened food-reward sensitivity (Smith et al., 2020).
2.3. Measures
2.3.1. Subjective/Physiological Stress Response.
Subjective/physiological stress was assessed at rest start/end, induction end, and TSST end. State anxiety was measured on the reliable/valid 6-item State-Trait Anxiety Inventory for Children–State Version (αs=.62–.85 across intervals; Kirisci, Clark, & Moss, 1997). State mindlessness was assessed with the reliable/valid 5-item Mindfulness Attention and Awareness Scale–State Version (αs=.83–.85; Brown & Ryan, 2003). HR and SBP/DBP were recorded using a cuff-fitted monitor on the non-dominant arm. Areas-under-the-curve with respect to increase (AUCi) were computed to summarize stress responses (Pruessner, Kirschbaum, Meinlschmid, & Hellhammer, 2003).
2.3.2. Disordered-eating.
Global disordered-eating and binge-eating in the past four weeks were measured with the reliable/valid Eating Disorders Examination-Questionnaire (EDE-Q; Carter, Stewart, & Fairburn, 2001; Fairburn & Beglin, 1994). The global scale averages all items (α=.94). Adolescents were considered to have binge-eating when they endorsed, “Have there been times when you have eaten what most people would regard as an unusually large amount of food?” and “Have you experienced a sense of loss of control overeating?” Those who endorsed neither or one item only were considered to have no binge-eating or overeating without loss-of-control.
2.4. Data Analysis
Outliers were winsorized to 1.5 times the interquartile range >75th percentile or <25th percentile (6% data). Linear mixed models were performed with the dependent variables of anxiety, mindlessness, HR, SBP/DBP (AUCi) and stress-eating (kcal) using restricted maximum likelihood estimation to handle missing data. Main effects were induction-type and disordered-eating or binge-eating. Two-way interactions of induction-type by disordered-eating or binge-eating were examined separately, due to the small sample and to avoid multi-collinearity problems. Global disordered eating was analyzed as a continuous variable; we plotted significant interactions using a median split to aid interpretation. There were no induction-order effects by disordered eating, but those who received the neutral-induction first had a higher BMI-z and were younger. We controlled for induction-order (mindfulness/neutral first), age, BMI-z, sex, and initial levels of respective outcomes.
3. Results
3.1. Subjective/Physiological Stress Response
There was a main effect of induction-type on state anxiety AUCi (p=.04; Table 1). In the mindfulness-induction, adolescents had no increase in anxiety compared to an increase in the neutral-induction (mindfulness:95%CI −14.37, 11.58 vs. neutral:95%CI 3.95, 26.23). Main effect of induction-type on mindlessness AUCi was not significant (p=.26), with no change in either condition (mindfulness:95%CI −6.64, 6.09 vs. neutral:95%CI −9.53, 3.03). There were no main effects of induction-type on HR or SBP/DBP (p-values>.12).
Table 1.
Summary of Linear Mixed Models Predicting Subjective Stress Response and Physiological Stress Response
| State Anxiety | State Mindlessness | HR | SBP | DBP | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictors | B | SE | p | B | SE | p | B | SE | p | B | SE | p | B | SE | p |
|
Step 1: Audio Induction Type |
−16.43 | 7.46 | .04 | 2.98 | 2.60 | .26 | −54.66 | 41.63 | .20 | −100.08 | 96.73 | .31 | −81.51 | 52.26 | .13 |
|
Step 2a: Global Disordered Eating |
3.62 | 4.85 | .46 | 2.03 | 2.98 | .50 | −4.99 | 19.97 | .81 | −57.90 | 45.37 | .22 | 12.90 | 25.70 | .62 |
|
Step 2b: Binge-Eating |
−2.10 | 10.29 | .84 | −10.84 | 5.80 | .08 | −35.70 | 40.67 | .39 | −37.50 | 98.13 | .71 | −20.46 | 53.58 | .71 |
|
Step 3a: Audio Type × Global Disordered Eating |
16.00 | 6.66 | .02 | 2.56 | 2.56 | .33 | −31.99 | 25.48 | .22 | −42.61 | 73.25 | .57 | −50.96 | 28.46 | .09 |
|
Step 3b: Audio Type × Binge-Eating |
−32.46 | 14.28 | .03 | −1.88 | 5.37 | .73 | 64.10 | 54.51 | .25 | 54.54 | 155.32 | .73 | 135.33 | 60.17 | .03 |
Note. B = Unstandardized estimate; SE = Standard error; HR = Heart rate; SBP = Systolic blood pressure; DBP = Diastolic blood pressure; Audio Induction Type was dummy-coded: 1 = mindfulness audio-recording and 2 = neutral audio-recording. All outcomes were measured as area under the curve with respect to increase (AUCi). Covariates within each model included: sex, age, BMI-z score, audio type order (mindfulness or neutral first), and initial level (start of rest period) of the respective outcome variable. Estimates are displayed from each step upon entry into the model.
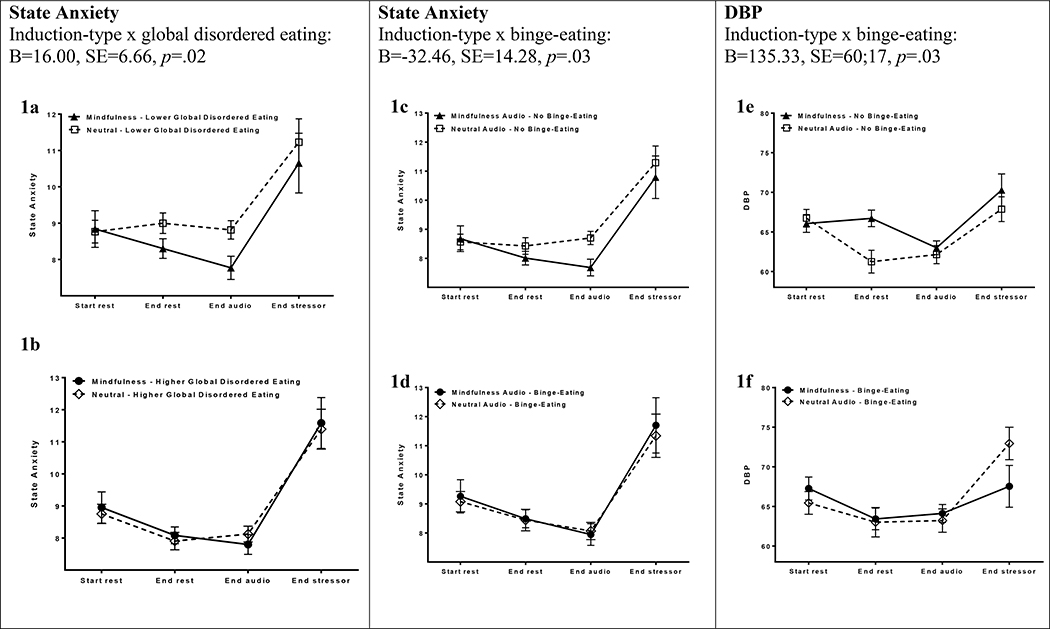
Main effects of global disordered-eating and binge-eating on state anxiety, mindlessness, and physiological responses were non-significant (p-values>.08). There were interactions of induction-type by disordered-eating (p=.02) and binge-eating (p=.03) in predicting anxiety AUCi. Reduction in anxiety from the mindfulness-induction was more pronounced among adolescents with relatively lower (Figure 1a) versus higher (Figure 1b) disordered-eating. Similarly, reduction in anxiety in the mindfulness-induction was only observed among adolescents without binge-eating (Figure 1c/d). There were no interactive effects on mindlessness (p-values>.47).
Figure 1.
During a mindfulness-induction versus neutral-induction, area under the curve with respect to increase (AUCi) for state anxiety among adolescents with relatively lower global disordered eating (1a) versus relatively higher global disordered-eating (1b), depicted as a median-split (Eating Disorder Examination-Questionnaire global score <.1.726 vs. ≥ 1.727); and adolescents with absence of binge-eating versus presence of binge-eating for AUCi for state anxiety (1c/d) and diastolic blood pressure (DBP; 1e/f).
Additionally, there was an induction-type by binge-eating interaction predicting DBP AUCi (p=.03). There was greater reduction in DBP response following the mindfulness versus neutral-induction among adolescents with binge-eating, whereas the difference in DBP response among adolescents without binge-eating was less pronounced after mindfulness versus neutral-inductions (Figure 1e/f). No other interactions were significant (p-values>.09).
3.2. Stress-Eating
There was no main effect of induction-type on stress-eating (mindfulness:814±62kcal vs. neutral:755±59kcal, p=.21). Likewise, there were no main or interactive effects of disordered-eating/binge-eating on stress-eating (p-values>.52).
4. Discussion
A brief 10-minute mindfulness-induction produced less state anxiety compared to a neutral-induction. Following a mindfulness-induction, adolescents reported no change in state anxiety, whereas they experienced an anxiety increase in the neutral-induction. These findings fit with past adult studies finding an inverse relationship between mindfulness and distress tolerance/maladaptive stress responses (e.g., Brown et al., 2012). Repeated inductions of mindfulness in prolonged mindfulness-training may be explanatory in lowering anxiety symptomatology and improving coping (Sibinga et al., 2013). This finding has potentially relevant clinical implications. Cultivating mindfulness in the face of stress may help adolescents at-risk for adult obesity to alleviate anxiety.
Mindfulness-induction effects on state anxiety were moderated by disordered-eating and binge-eating. Adolescents with lower disordered-eating/no binge-eating exhibited lower anxiety response after a mindfulness-induction, whereas those with more disordered-eating/binge-eating did not benefit. One possibility is that higher trait anxiety, frequently accompanying disordered-eating, renders state anxiety less malleable during a brief mindfulness-induction (Goldschmidt, Aspen, Sinton, Tanofsky- Kraff, & Wilfley, 2008). Prolonged training could be anticipated to overcome initial barriers, as mindfulness-based intervention programs have led to improved anxiety and eating in adults (O’Reilly, Cook, Spruijt- Metz, & Black, 2014). Furthermore, the mindfulness-induction in this study was breath-awareness only, which may be less effective than attention plus acceptance/compassion-training (Lindsay, Young, Brown, Smyth, & Creswell, 2019). Future research should disentangle effects of attention and acceptance/compassion for adolescents with disordered-eating/binge-eating.
Unexpectedly, mindfulness-induction did not have main or interactive effects on state mindlessness, physiological stress, or stress-eating. Brevity of the mindfulness-induction and/or omission of acceptance/self-compassion-training may have reduced potency. It is also possible that state anxiety is a more tangible and/or malleable construct than mindfulness/mindlessness. Mindfulness/mindlessness may be difficult to describe for adolescents, particularly under stressful circumstances (Creswell et al., 2014). Additionally, some research suggests individuals with obesity or disordered-eating have blunted cardiovascular reactions to stress (Phillips, 2011), potentially making mindfulness-induction effects on stress responding difficult to detect in this population. It will be important to test these potential explanations.
There was a moderating effect of mindfulness-induction by binge-eating on DBP. Adolescents with binge-eating experienced lower DBP response after a mindfulness versus neutral-induction, which was not apparent in those without binge-eating. This finding points to an interesting distinction between subjective and physiological stress-responding among adolescents with and without binge-eating. Adolescents with binge-eating may experience subjective and physiological stress differently, consistent with previous studies showing these two dimensions of stress response are often misaligned (Lucas- Thompson, 2012). Individuals with binge-eating tend toward more negative subjective stress appraisals (Hansel & Wittrock, 1997) and lower distress tolerance (Anestis, Selby, Fink, & Joiner, 2007). Physiological measurements may shed light on objective internal/physical stress experiences. Further investigation of the distinction between subjective-physiological stress responses among adolescents with binge-eating is warranted.
The current study used a small sample with limited representation of racial/ethnic minorities, a wide age range, and previous mindfulness practice was not measured, limiting inferences. Mechanisms by which a mindfulness-induction changed anxiety/DBP remain unclear. Mindfulness-induction did not affect state mindlessness, which may have been due to mindfulness-induction brevity, attention-training versus acceptance/self-compassion, and/or difficulty explicitly reporting mindlessness. Small samples are prone to greater standard error/less robust estimates of effect and interaction results were exploratory/hypothesis-generating. Interpretability depends upon future replication.
In conclusion, a brief mindfulness-induction potentially may reduce state anxiety among adolescents at-risk for adult obesity. Adolescents without disordered-eating benefited more from a mindfulness-induction to reduce anxiety response to stress than those with disordered-eating. In contrast, only adolescents with binge-eating had lower DBP stress response following a mindfulness-induction. Future research with a larger sample size, lengthier mindfulness-training, and/or acceptance/self-compassion induction may increase our understanding of mechanisms underlying potential benefits of mindfulness-training in adolescents at-risk for adult obesity.
Supplementary Material
Highlights.
Few experimental studies have tested acute effects of mindfulness in adolescents
A brief, 10-minute mindfulness-induction reduced state anxiety response to stress
Mindfulness-induction reduced anxiety in teens with less disordered/binge-eating
Mindfulness lowered diastolic blood pressure only in adolescents with binge-eating
Mindfulness-induction did not affect heart rate response to stress or stress-eating
Footnotes
Declarations of interest: None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adam TC, & Epel ES (2007). Stress, eating and the reward system. Physiology & Behavior, 91(4), 449–458. [DOI] [PubMed] [Google Scholar]
- Anestis MD, Selby EA, Fink EL, & Joiner TE (2007). The multifaceted role of distress tolerance in dysregulated eating behaviors. International Journal of Eating Disorders, 40(8), 718–726. [DOI] [PubMed] [Google Scholar]
- Annameier SK, Kelly NR, Courville AB, Tanofsky-Kraff M, Yanovski JA, & Shomaker LB (2018). Mindfulness and laboratory eating behavior in adolescent girls at risk for type 2 diabetes. Appetite, 125, 48–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arch JJ, Brown KW, Goodman RJ, Della Porta MD, Kiken LG, & Tillman S (2016). Enjoying food without caloric cost: The impact of brief mindfulness on laboratory eating outcomes. Behaviour Research and Therapy, 79, 23–34. [DOI] [PubMed] [Google Scholar]
- Association, A. P. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub. [DOI] [PubMed] [Google Scholar]
- Brown KW, & Ryan RM (2003). The Benefits of Being Present: Mindfulness and Its Role in Psychological Well-Being. Journal of Personality and Social Psychology, 84(4), 822–848. 10.1037/0022-3514.84.4.822 [DOI] [PubMed] [Google Scholar]
- Brown KW, Weinstein N, & Creswell JD (2012). Trait mindfulness modulates neuroendocrine and affective responses to social evaluative threat. Psychoneuroendocrinology, 37(12), 2037–2041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bullis JR, Bøe HJ, Asnaani A, & Hofmann SG (2014). The benefits of being mindful: Trait mindfulness predicts less stress reactivity to suppression. Journal of Behavior Therapy and Experimental Psychiatry, 45(1), 57–66. [DOI] [PubMed] [Google Scholar]
- Carter JC, Stewart DA, & Fairburn CG (2001). Eating disorder examination questionnaire: norms for young adolescent girls. Behaviour Research and Therapy, 39(5), 625–632. [DOI] [PubMed] [Google Scholar]
- Creswell JD, Pacilio LE, Lindsay EK, & Brown KW (2014). Brief mindfulness meditation training alters psychological and neuroendocrine responses to social evaluative stress. Psychoneuroendocrinology, 44, 1–12. [DOI] [PubMed] [Google Scholar]
- Dallman MF (2010). Stress-induced obesity and the emotional nervous system. Trends in Endocrinology & Metabolism, 21(3), 159–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon HC, & Overall NC (2016). Dispositional mindfulness attenuates the link between daily stress and depressed mood. Journal of Social and Clinical Psychology, 35(3), 255–268. [Google Scholar]
- Fairburn CG, & Beglin SJ (1994). Assessment of eating disorders: Interview or self report questionnaire? International Journal of Eating Disorders, 16(4), 363–370. [PubMed] [Google Scholar]
- Gillman MW, & Hammond RA (2016). Precision treatment and precision prevention: integrating “below and above the skin.” JAMA Pediatrics, 170(1), 9–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginty AT, Phillips AC, Higgs S, Heaney JLJ, & Carroll D (2012). Disordered eating behaviour is associated with blunted cortisol and cardiovascular reactions to acute psychological stress. Psychoneuroendocrinology, 37(5), 715–724. [DOI] [PubMed] [Google Scholar]
- Godfrey KM, Gallo LC, & Afari N (2015). Mindfulness-based interventions for binge eating: a systematic review and meta-analysis. Journal of Behavioral Medicine, 38(2), 348–362. [DOI] [PubMed] [Google Scholar]
- Goldschmidt AB, Aspen VP, Sinton MM, Tanofsky, Kraff M, & Wilfley DE (2008). Disordered eating attitudes and behaviors in overweight youth. Obesity, 16(2), 257–264. [DOI] [PubMed] [Google Scholar]
- Hafenbrack AC, Kinias Z, & Barsade SG (2014). Debiasing the mind through meditation: Mindfulness and the sunk-cost bias. Psychological Science, 25(2), 369–376. [DOI] [PubMed] [Google Scholar]
- Hansel SL, & Wittrock DA (1997). Appraisal and coping strategies in stressful situations: A comparison of individuals who binge eat and controls. International Journal of Eating Disorders, 21(1), 89–93. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, & Brook JS (2002). Eating disorders during adolescence and the risk for physical and mental disorders during early adulthood. Archives of General Psychiatry, 59(6), 545–552. [DOI] [PubMed] [Google Scholar]
- Jordan CH, Wang W, Donatoni L, & Meier BP (2014). Mindful eating: Trait and state mindfulness predict healthier eating behavior. Personality and Individual Differences, 68, 107–111. [Google Scholar]
- Kabat-Zinn J (1994). Wherever you go, there you are: Mindfulness meditation in everyday life New York, USA: Hyperion. [Google Scholar]
- Katterman SN, Kleinman BM, Hood MM, Nackers LM, & Corsica JA (2014). Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: a systematic review. Eating Behaviors, 15(2), 197–204. [DOI] [PubMed] [Google Scholar]
- Kelly AS, Marcus MD, Yanovski JA, Yanovski SZ, & Osganian SK (2018). Working toward precision medicine approaches to treat severe obesity in adolescents: report of an NIH workshop. International Journal of Obesity, 42(11), 1834–1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirisci L, Clark DB, & Moss HB (1997). Reliability and validity of the State-Trait Anxiety Inventory for Children in adolescent substance abusers: Confirmatory factor analysis and item response theory. Journal of Child & Adolescent Substance Abuse, 5(3), 57–70. [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, … Johnson CL (2002). 2000 CDC growth charts for the United States; methods and development. [PubMed]
- Lindsay EK, Young S, Brown KW, Smyth JM, & Creswell JD (2019). Mindfulness training reduces loneliness and increases social contact in a randomized controlled trial. Proceedings of the National Academy of Sciences, 116(9), 3488–3493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loth K, van den Berg P, Eisenberg ME, & Neumark-Sztainer D (2008). Stressful life events and disordered eating behaviors: Findings from Project EAT. Journal of Adolescent Health, 43(5), 514–516. [DOI] [PubMed] [Google Scholar]
- Lucas-Thompson RG, Miller RL, Seiter NS, & Prince MA (2019). Dispositional Mindfulness Predicts Cortisol, Cardiovascular, and Psychological Stress Responses in Adolescence. Psychoneuroendocrinology, 104405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas Thompson, R. G. (2012). Associations of marital conflict with emotional and physiological stress: Evidence for different patterns of dysregulation. Journal of Research on Adolescence, 22(4), 704–721. [Google Scholar]
- O’Reilly GA, Cook L, Spruijt Metz, D., & Black DS (2014). Mindfulness based interventions for obesity related eating behaviours: a literature review. Obesity Reviews, 15(6), 453–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouwens MA, Schiffer AA, Visser LI, Raeijmaekers NJC, & Nyklíček I (2015). Mindfulness and eating behaviour styles in morbidly obese males and females. Appetite, 87, 62–67. [DOI] [PubMed] [Google Scholar]
- Phillips AC (2011). Blunted cardiovascular reactivity relates to depression, obesity, and self-reported health. Biological Psychology, 86(2), 106–113. [DOI] [PubMed] [Google Scholar]
- Pivarunas B, Kelly NR, Pickworth CK, Cassidy O, Radin RM, Shank LM, … Tanofsky Kraff, M. (2015). Mindfulness and eating behavior in adolescent girls at risk for type 2 diabetes. International Journal of Eating Disorders, 48(6), 563–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruessner JC, Kirschbaum C, Meinlschmid G, & Hellhammer DH (2003). Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology, 28(7), 916–931. [DOI] [PubMed] [Google Scholar]
- Ranzenhofer LM, Engel SG, Crosby RD, Anderson M, Vannucci A, Cohen LA, … Tanofsky Kraff, M. (2014). Using ecological momentary assessment to examine interpersonal and affective predictors of loss of control eating in adolescent girls. International Journal of Eating Disorders, 47(7), 748–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts KC, & Danoff-Burg S (2010). Mindfulness and health behaviors: is paying attention good for you? Journal of American College Health, 59(3), 165–173. [DOI] [PubMed] [Google Scholar]
- Romeo RD, & McEwen BS (2006). Stress and the adolescent brain. Annals of the New York Academy of Sciences, 1094(1), 202–214. [DOI] [PubMed] [Google Scholar]
- Rosenbaum DL, & White KS (2013). The role of anxiety in binge eating behavior: A critical examination of theory and empirical literature. Health Psychology Research, 1(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seddon JA, Rodriguez VJ, Provencher Y, Raftery-Helmer J, Hersh J, Labelle PR, & Thomassin K (2020). Meta-analysis of the effectiveness of the Trier Social Stress Test in eliciting physiological stress responses in children and adolescents. Psychoneuroendocrinology, 116, 104582. [DOI] [PubMed] [Google Scholar]
- Shank LM, Crosby RD, Grammer AC, Shomaker LB, Vannucci A, Burke NL, … Reynolds JC (2017). Examination of the interpersonal model of loss of control eating in the laboratory. Comprehensive Psychiatry, 76, 36–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibinga EMS, Perry-Parrish C, Chung S, Johnson SB, Smith M, & Ellen JM (2013). School-based mindfulness instruction for urban male youth: a small randomized controlled trial. Preventive Medicine, 57(6), 799–801. [DOI] [PubMed] [Google Scholar]
- Smith AD, Sanchez N, Reynolds C, Casamassima M, Verros M, Annameier SK, … Shomaker LB (2020). Associations of parental feeding practices and food reward responsiveness with adolescent stress-eating. Appetite, 104715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson SA, Crow SJ, Le Grange D, Swendsen J, & Merikangas KR (2011). Prevalence and correlates of eating disorders in adolescents: Results from the national comorbidity survey replication adolescent supplement. Archives of General Psychiatry, 68(7), 714–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, McDuffie JR, Yanovski SZ, Kozlosky M, Schvey NA, Shomaker LB, … Yanovski JA (2009). Laboratory assessment of the food intake of children and adolescents with loss of control eating. The American Journal of Clinical Nutrition, 89(3), 738–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Shomaker LB, Stern EA, Miller R, Sebring N, DellaValle D, … Yanovski JA (2012). Children’s binge eating and development of metabolic syndrome. International Journal of Obesity, 36(7), 956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vannucci A, Nelson EE, Bongiorno DM, Pine DS, Yanovski JA, & Tanofsky-Kraff M (2015). Behavioral and neurodevelopmental precursors to binge-type eating disorders: support for the role of negative valence systems. Psychological Medicine, 45(14), 2921–2936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yim IS, Quas JA, Cahill L, & Hayakawa CM (2010). Children’s and adults’ salivary cortisol responses to an identical psychosocial laboratory stressor. Psychoneuroendocrinology, 35(2), 241–248. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.