Abstract
This study examines health and well-being priorities among BMSM in Baltimore, MD and their association with condom use. Among 148 sexually active BMSM, 43% were HIV positive. The majority ranked financial stability (68%), physical health (53%), and stable housing (59%) as top priorities. Fewer participants identified top priorities as mental health (37%), HIV prevention (35%), relationships with family (25%), and romantic partners (23%). Identifying HIV prevention (aOR:2.25; 95%CI:1.07-4.72) and relationship with family (aOR:2.19; 95%CI:0.99-4.89) as top priorities were associated with increased odds of always using condoms. Reporting stable housing as a top priority (aOR:0.47; 95%CI:0.22-1.00) reduced the odds of always using a condom. To increase relevance, HIV/AIDS prevention programs should address BMSM’s financial, housing and physical health needs.
Keywords: HIV/AIDS, BMSM, Competing Priorities, Intervention
Introduction
Black men who have sex with men (BMSM) have the highest rate of HIV infection in the United States and accounted for 10,070 (26%) new infections in 2017 (Centers for Disease Control and Prevention, 2017). In Baltimore, Maryland an estimated 48 percent of BMSM are living with HIV (German et al., 2017). Given this high rate of HIV, we were interested in how HIV prevention and care may fit into BMSM’s overall life priorities.
Previous research has identified competing priorities as a barrier to engaging in health promoting behaviors (Baggett et al., 2018; Gelberg, Gallagher, Andersen, & Koegel, 1997; Kahle, Sharma, Sullivan, & Stephenson, 2018; Palar, Wong, & Cunningham, 2018; Rezansoff et al., 2017). A recent study found that competing subsistence needs reduced retention in HIV care and increased incidence of detectable viral load among people living with HIV (Palar et al., 2018). BMSM are affected by multiple co-occurring conditions such as depression and substance use (Buttram & Kurtz, 2016; Cochran & Mays, 2013; Stall et al., 2003; Wong, Weiss, Ayala, & Kipke, 2010). BMSM in the US also experience high levels of unemployment, and urban Black men face high rates of homelessness that can be deleterious to their mental health and well-being (German et al., 2017; Maulsby et al., 2019). However, few studies have explored the multiple psychological, financial, health, and social priorities in the lives of BMSM and how these priorities may be linked to risk behaviors (Coleman, 2017; Sun, Nall, & Rhodes, 2018). Addressing competing priorities can enable greater engagement in health promoting behaviors (Rezansoff et al., 2017). In order to develop HIV prevention and care interventions that are perceived as relevant to their lives, information is needed on BMSM current life priorities. Moreover, since in this population PrEP use is highly infrequent and the proportion of HIV positive men who are virally suppressed in relatively low (Eaton, Driffin, Bauermeister, Smith, & Conway-Washington, 2015; Millett et al., 2012), a better understanding of how priorities influence condom use can help identify social/structural targets for future HIV prevention interventions among BMSM.
The goal of the current study is to assess the health and well-being priorities of sexually active BMSM and identify how competing needs are associated with consistent condom use. To address this gap in the literature, we examine the relative priority of HIV prevention in the context of seven other potentially competing health and well-being priorities. Specifically, we examined: 1) consistency of priority ranking across participants, 2) mean rank score of each priority domain, 3) the relationship between socio-demographic characteristics and priority ranking, and 4) the association between priority ranking and consistent condom use.
Methods
Participants, design, and setting
Data for this study came from a survey conducted at the six-month follow-up of a randomized controlled trial (RCT) testing the efficacy of a sexual health intervention for BMSM and their social and sexual networks, called the Social Networks and Prevention study. Individuals were recruited through venue-based outreach (bars and clubs, community-based organizations, health clinics), street outreach, virtual advertisements, passive virtual postings on social media organizations that cater to BMSM, as well as word of mouth referral. Inclusion criteria for the baseline survey consisted of: (a) age 18 years and older; (b) self-reported sex with at least one male partner within the prior 6 months; (c) self-reported male sex at birth; (d) identify as male; (e) self-reported Black or African American race/ethnicity; (f) unprotected anal or vaginal sex within the 6 months. Baseline recruitment and enrollment occurred from October 2012 to November 2015. A follow-up survey was conducted six-months after baseline for all participants who completed the baseline survey. To promote retention, participants were contacted via phone calls, e-mails, and letters. The majority of participants (85%) completed the six-month follow-up survey. Participants were paid $35 for completing the survey. Study protocols were approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board (IRB #3617).
Measurements
Common health and well-being domains relevant to BMSM were identified through a literature review and formative pilot work conducted to develop the intervention, this resulted in seven domains that were used in a priority ranking exercise (Buttram & Kurtz, 2016; Cochran & Mays, 2013; Stall et al., 2003; Wong, Weiss, Ayala, & Kipke, 2010; German et al., 2017; Maulsby et al., 2019). The priority ranking exercise consisted of ranking seven health and well-being domains, including housing stability, financial stability, HIV prevention and/or risk prevention, mental health, physical health, relationship with family, and relationship with romantic partners. Participants were asked to rank (order) the seven domains from greatest concern (1) to least concern (7). A string variable was created to assess patterns of priority ranking. Sequential response patterns (1234567 and 7654321; n=14) were not included in the analysis as they indicated that participants might not have understood the exercise. For inferential data analysis, each priority domain was categorized as a top priority, ranked as #1-3 on the priority ranking exercise, versus not at top priority domain, ranked as #4-7 in the exercise.
Chi-square tests were used to assess the relationship between each binary priority domain and HIV, social-economic status, demographic variables. HIV status was assessed through self-report of status based on the most recent HIV test. Six participants were missing HIV test results in this sample, and their HIV status was coded as negative. Age was dichotomized at 30 years of age to assess the difference between younger and older BMSM (Centers for Disease Control and Prevention, 2003). Education was classified as having completed high school or above compared to grade 11 or less. Participants with full or part-time employment were compared to those who were unemployed.
Multiple multivariate logistic regressions were used to assess the relationship between priority ranking and condom use. The outcome of interest for the multivariate analysis was reporting always using a condom during anal or vaginal sex. Condom use was assessed as a summative variable from the questions, “How often were condoms used when having anal sex [with main and non-main partner(s)]” and “How often were condoms used when having vaginal sex [with main and non-main partner(s)].” Condom use was dichotomized to compare “always” versus “more than half the time,” “half the time,” “less than half the time,” or “never.” All models were adjusted for HIV status, age, education, and employment. Data were analyzed with STATA (version 14) with a p-value < 0.05 considered statistically significant (StataCorp, 2014).
Results
About half of the study population (43%) reported being HIV positive (HIV+) at their last test. The mean age of all study participants was 38 years (SD: 11, Range: 20-68) and most of the sample (70%) was aged 30 or older (Mean age HIV+:39, SD:12, Range:20-68; Mean age HIV−:37 years, SD:11, Range:20-61). The total sample population consisted of primarily high school graduates, with 83% completing 12th grade/GED or higher (Completed high school or above HIV+:92%; HIV−:76%). Over one-third (39%) reported full or part-time employment (Full or part-time employment HIV+:34%; HIV−:42%)
Study participants showed a wide variation in ranking the seven priority domains with 124 unique patterns of ranking. Participants ranking of priority domains are displayed in Table 1. Overall financial stability, physical health, and housing stability received the highest ranking with 68% of the sample ranking financial stability as a top priority; 53% identifying physical health as a top priority; and, 59% indicating stable housing in the top three. Concerns about mental health were often in the middle of the list, usually ranked as the fourth in the priority list, with 37% of the sample identifying mental health as a top priority. On average, HIV prevention was ranked as a fourth or fifth priority, out of the seven domains. About a third of the sample (35%) identified HIV prevention as a top priority. Relationship with family and romantic partners received the lowest ranking with only 25% and 23% identifying the domains as a top priority, respectively.
Table 1:
Participant’s ranking of priority domains: Mean rank and top priority percentage
| Priority domains | All (N=148) | HIV Positive (n=64) | HIV Negative (n=84) | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Mean Rank & SD | Top priority (%) | Mean Rank & SD | Top priority (%) | Mean Rank & SD | Top priority (%) | |
| Having financial stability | 2.9 ± 1.8 | 68 | 3.0 ± 1.7 | 67 | 2.9 ± 1.9 | 68 |
| My physical health | 3.4 ± 1.5 | 53 | 3.1 ± 1.5 | 59 | 3.5 ± 1.5 | 49 |
| Having stable housing | 3.4 ± 2.3 | 59 | 3.7 ± 2.3 | 48 | 3.2 ± 2.2 | 67 |
| My mental health | 4.1 ± 1.7 | 37 | 3.9 ± 1.8 | 39 | 4.2 ± 1.6 | 36 |
| HIV prevention and/or risk | 4.4 ± 1.9 | 35 | 4.3 ± 1.9 | 36 | 4.4 ± 2.0 | 35 |
| My relationships with family | 4.7 ± 1.7 | 25 | 4.8 ± 1.7 | 25 | 4.6 ± 1.8 | 25 |
| My relationships with romantic partners | 5.2 ± 2.0 | 23 | 5.2 ± 2.1 | 25 | 5.2 ± 2.0 | 21 |
Socio-demographic characteristics were associated with few of the rankings. Financial stability, mental health, HIV prevention and/or risk, as well as relationships with family and romantic partners, were not significantly associated with socio-demographic characteristics in this study. Ranking physical health as a top priority was significantly associated with employment status, with 60% of unemployed and 42% of employed identifying physical health as a top priority (p=0.030). Ranking stable housing as a top priority was significantly associated with HIV status and marginally associated with employment. BMSM not living with HIV were more likely to rank stable housing as a top priority, with 67% of BMSM not living with HIV and 48% of BMSM living with HIV ranking stable housing as a top priority (p=0.026). Additionally, BMSM who were employed were more likely to rank stable housing as a top priority, with 68% of employed and 53% of unemployed identifying housing as a top concern (p=0.059).
Multivariate regressions assessed the relationship between participants’ ranking a domain as the top priority and condom use (Figure 1). Identifying HIV prevention as a top priority was significantly associated with higher odds of always using condoms, compared to not identifying HIV prevention as a top priority (Adjusted Odds Ratio [aOR]: 2.25; 95% CI: 1.07-4.72). Additionally, higher odds of consistent condom use were associated with ranking relationship with family as a top priority (aOR: 2.19; 95% CI: 0.99-4.89) and identifying stable housing as a top priority was associated with lower odds of always wearing a condom (aOR: 0.47; 95% CI: 0.22-1.00). Financial stability, physical health, mental health, and relationships with friends were not significantly associated consistent condom use. Hosmer-Lemeshow goodness-of-fit test assessed model fit and all models had a p-value of greater than 0.05, suggesting good model fit.
Figure 1: Adjusted odds ratios of ranking a domain as a top priority and consistent condom use (N=148)**.
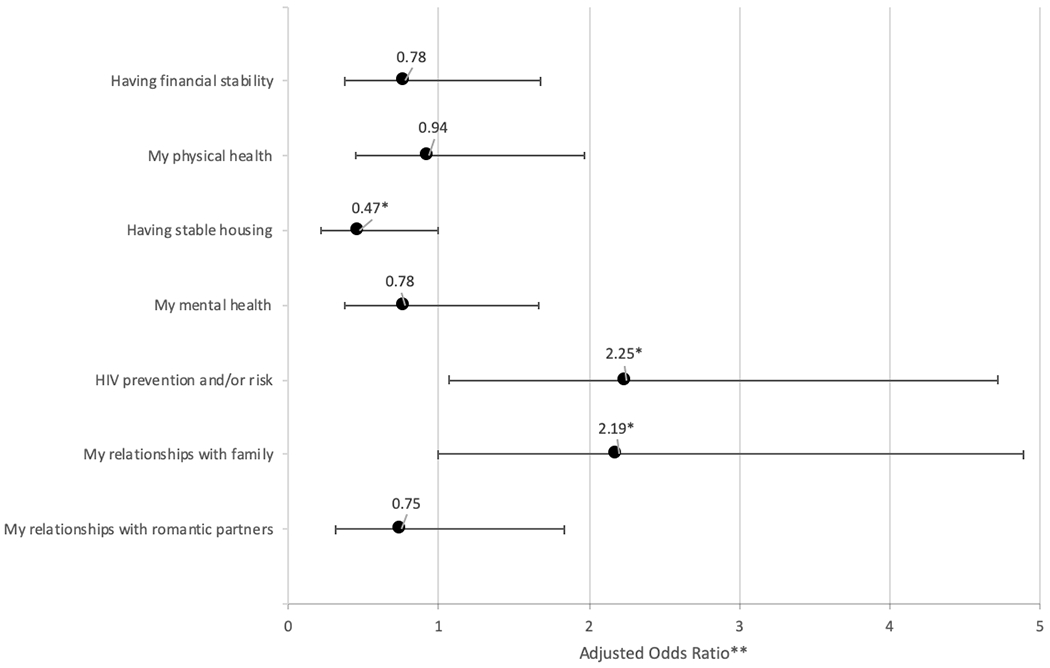
*≤0.05
** all models adjusted for age, education, employment, and HIV status
Discussion
This study identified the range of competing priorities experienced by BMSM in Baltimore, MD, and provided support to the hypothesis that competing priorities are a potential barrier to consistent condom use among sexually active BMSM. The majority of participants identified financial stability, physical health, and stable housing as top priorities. Consistent with a study by Kahle and colleagues among primarily white MSM, HIV prevention/ risk was not identified as a top priority (Kahle et al., 2018). In this study, HIV prevention/risk was often listed as the fourth or fifth highest priority. Interestingly, there were no difference in priority ranking for HIV prevention and/or risk between participants who were HIV positive and negative. The only statistical difference between BMSM living with HIV and men who were not was that participants not living with HIV were more likely to rate stable housing as one of their top three priorities. This difference may have been due to the availability of housing vouchers and supportive housing for individuals living with HIV through the federal Housing Opportunity for Persons with AIDS (HOWPA) program (US Department of Housing and Urban Development, 2020). Participants who were HIV positive and negative were highly similar in their rating of financial stability as a top priority, with approximately two-thirds rating it as one of their top three priorities. This is significant as only about one-third of the sample was employed; there was no difference by employment status in rating financial stability as a top priority. In addition to the high rates of unemployment, those who were employed may have been underemployed and had low incomes.
Relationships with family, followed by relationships with romantic partners consistently ranked at the end of the priority ranking exercise. Relationships with family may be viewed as a higher priority compared to relationships with romantic partners, as a high proportion of BMSM have found to report family as key members of their social networks (Latkin et al., 2011). Surprisingly, individuals who rated relationships with family as a top priority were also more likely to report condom use. These results coupled with Latkin and colleagues’ findings that sexual partners were not often reported as members of BMSM social support network suggest that kin may serve as critical sources of emotional and material support to BMSM and should be incorporated in HIV/AIDS prevention strategies (Latkin et al., 2011).
This study provided support to the hypothesis that competing priorities are a potential barrier to consistent condom use among sexually active BMSM. Although HIV prevention and risk was only ranked as the fifth priority, it was found that those who rated it as a top priority were significantly more likely to report always using condoms. This finding builds on prior research among MSM which did not find an association between ranking HIV prevention as a high priority and engagement in higher sexual risk behavior among a sample of primarily white men (Kahle et al., 2018). The difference between the two study findings may be reflective of the level of competing priorities faced by BMSM in the current study. Additionally, the current study found that ranking stable housing as a top priority was associated with lower odds of consistent condom use. These findings suggest that priorities of BMSM in the US may impede HIV prevention efforts and when competing priorities are addressed BMSM may more effectively engage in HIV prevention activities.
As many communities, including Baltimore, are rolling out PrEP programs, which require a more complex set of activities to initiate use than condom use, it is even more imperative that HIV prevention programs address competing needs. These programs can also be integrated with HIV care in the form of community-based interventions. Some HIV clinics do have case management to address some competing needs, such as housing, but such programs are often unavailable to HIV negative individuals. These results also suggest that programs to address employment among BMSM are likely to be viewed favorably. For HIV prevention to become more relevant, it may be helpful to integrate job training and placement with HIV prevention and care programs. These findings are consistent with O’Toole and colleagues who found that addressing the competing social and well-being needs of high-risk homeless veterans resulted in improved health outcome (O’Toole, Johnson, Aiello, Kane, & Pape, 2016).
One of the study’s limitations was that only seven priorities were listed. Issues such as violence, religion and spirituality, relationships with friends, and leisure and social activities were not assessed. The priorities were also global, such as physical health, rather than asking about specific behaviors or activities such as exercise or healthy eating habits. Moreover, these priorities may not translate into behaviors. We also do not know if the perceptions of priorities were from a deficit perspective, such as not having but wanting stable housing, or from a concern of losing the priority domain, such as losing stable housing—or both. Future research should utilize advances in decision making and ratings, such as conjoint analyses (Fletcher et al., 1983; Fried et al., 2011).
Conclusion
BMSM have numerous priorities in addition to HIV prevention. The current findings strongly suggest that HIV prevention is not one of the top three priorities in this sample of BMSM, even among those who are HIV negative, and hence prevention strategies aught not assume that the high HIV rates have naturally caused HIV to become a top priority that overrides other needs. Linking HIV prevention to higher priorities may be a viable intervention strategy. Addressing housing, employment, and other physical health needs should be considered when planning public health programs and policy.
Acknowledgements:
This work was supported by study participants and the National Institute of Health under grants R01 DA031030 & R01 DA032217. We thank Roeina Love, Tonya Johnson, Denise Mitchell, Charles Moore, Marlesha Bates, and Joanne Jenkins for their assistance and support in data collection.
Footnotes
Declaration of Interest Statement: None of the authors have financial conflicts of interests.
References:
- Baggett TP, Yaqubi A, Berkowitz SA, Kalkhoran SM, McGlave C, Chang Y, … Rigotti NA (2018). Subsistence difficulties are associated with more barriers to quitting and worse abstinence outcomes among homeless smokers: Evidence from two studies in Boston, Massachusetts. BMC Public Health, 18(1), 1–12. 10.1186/s12889-018-5375-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buttram M, & Kurtz S (2016). A mixed methods study of health and social disparities among substance-using African American/Black men who have sex with men, 35(14), 1252–1260. 10.1177/0333102415576222.Is [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2003). HIV/STD Risks in Young Men Who Have Sex with Men Who Do Not Disclose Their Sexual Orientation — Six U.S. Cities, 1994–2000. Morbidity and Mortality Weekly Report, 52(5), 1994–2000. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2017). HIV Surveillance Report 2017. Vol 29, 29, Published November 2018. 10.1017/CBO9781107415324.004 [DOI] [Google Scholar]
- Cochran S, & Mays V (2013). Depressive Distress Among Homosexually Active African American Men and Women. Am J Psychiatry, 17(5), 1–19. 10.1111/j.1532-7078.2011.00099.x.Infant [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman CL (2017). Qualitative Perspectives about Living with HIV from Seropositive African American MSM Aged 50 years and Older. Issues in Mental Health Nursing, 38(6), 486–492. 10.1080/01612840.2017.1284969 [DOI] [PubMed] [Google Scholar]
- Eaton LA, Driffin DD, Bauermeister J, Smith H, & Conway-Washington C (2015). Minimal awareness and stalled uptake of Pre-Exposure Prophylaxis (PrEP) among at risk, HIV-negative, black men who have sex with men. AIDS Patient Care and STDs, 29(8), 423–430. 10.1089/apc.2014.0303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher RH, Malley MSO, Earp JA, Littleton TA, Fletcher SW, Greganti MA, … Malley MSO (1983). Patients ‘ Priorities for Medical Care, 21(2), 234–242. [DOI] [PubMed] [Google Scholar]
- Fried T, Tinetti M, Agostini J, Iannone L, Towle V, Phil M, & Haven W (2011). Health Outcome Priortization to Elicit Preferences of Older Persons with Multiple Health Conditions. Patient Educ Couns, 83(2), 278–282. 10.1016/j.pec.2010.04.032.Health [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelberg L, Gallagher TC, Andersen RM, & Koegel P (1997). Competing priorities as a barrier to medical care among homeless adults in Los Angeles. American Journal of Public Health, 87(2), 217–220. 10.2105/AJPH.87.2.217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- German D, Brady K, Opoku J, Smith CR, Flynn C, Kuo I, … Davis WW (2017). Characteristics of Black Men Who Have Sex With Men in Baltimore, Philadelphia, and Washington, D.C. Journal of Acquired Immune Deficiency Syndromes, 75, S296–S308. 10.1097/qai.0000000000001425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahle EM, Sharma A, Sullivan SP, & Stephenson R (2018). HIV Prioritization and Risk Perception Among an Online Sample of Men Who Have Sex With Men in the United States. American Journal of Men’s Health, 12(4), 676–687. 10.1177/1557988318776581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin C, Yang C, Tobin K, Penniman T, Patterson J, & Spikes P (2011). Differences in the Social Networks of African American Men Who Have Sex With Men Only and Those Who Have Sex With Men and Women. American Journal of Public Health, 101(10), e18–e23. 10.2105/ajph.2011.300281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maulsby C, Parker LJ, White JJ, Latkin CA, Mugavero MJ, Flynn CP, & German D (2019). HIV and employment among Black men who have sex with men in Baltimore. AIDS Care, 0(0), 1–9. 10.1080/09540121.2019.1640847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WL IV, Wilson PA, … Remis RS (2012). Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: A meta-analysis. The Lancet, 380(9839), 341–348. 10.1016/S0140-6736(12)60899-X [DOI] [PubMed] [Google Scholar]
- O’Toole TP, Johnson EE, Aiello R, Kane V, & Pape L (2016). Tailoring Care to vulnerable populations by incorporating social determinants of health: The veterans health administration’s “homeless patient aligned care team” program. Preventing Chronic Disease, 13(3), 1–12. 10.5888/pcd13.150567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palar K, Wong M, & Cunningham W (2018). Competing subsistence needs are associated with retention in care and detectable viral load among people living with HIV. Journal of HIV/AIDS & Social Services, 17(3), 163–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rezansoff SN, Moniruzzaman A, Fazel S, McCandless L, Procyshyn R, & Somers JM (2017). Housing First Improves Adherence to Antipsychotic Medication among Formerly Homeless Adults with Schizophrenia: Results of a Randomized Controlled Trial. Schizophrenia Bulletin, 43(4), 852–861. 10.1093/schbul/sbw136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, … Catania JA (2003). Association of Co-Occurring Psychosocial Health Problems and Increased Vulnerability to HIV/AIDS among Urban Men Who Have Sex with Men. American Journal of Public Health, 93(6), 939–942. 10.2105/AJPH.93.6.939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. (2014). Stata Statistical Software: Release 14. College Station, TX: StataCorp LP. [Google Scholar]
- Sun C, Nall J, & Rhodes S (2018). Perceptions of Needs, Assets, and Priorities Among Black Men Who Have Sex With Men With HIV: Community-Driven Actions and Impacts of a Participatory Photovoice Process. American Journal of Men’s Health, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Housing and Urban Development. (2020). HIV/AIDS Housing. Retrieved July 6, 2020, from https://www.hud.gov/program_offices/comm_planning/aidshousing
- Wong C, Weiss G, Ayala G, & Kipke M (2010). Harassment, discrimination, violence, and illicit drug use among young men who have sex with men. AIDS Education and Prevention, 22(4), 286–298. 10.1521/aeap.2010.22.4.286 [DOI] [PMC free article] [PubMed] [Google Scholar]


