Abstract
Hypothesis/Background:
Shoulder pain and dysfunction are common indications for shoulder arthroplasty, yet the factors that are associated with these symptoms are not fully understood. This study aimed to investigate the associations of patient and disease-specific factors with preoperative patient-reported outcome measures (PROMs) in patients undergoing primary shoulder arthroplasty. We hypothesized that worse mental health status assessed by VR-12 MCS, glenoid bone loss, and increasing rotator cuff tear severity would be associated with lower preoperative total PENN Shoulder Score (PSS) and its pain, function, and satisfaction subscores.
Methods:
Twelve patient factors and four disease-specific factors were prospectively identified as possible statistical predictors for preoperative PROMs in patients undergoing primary shoulder arthroplasty at a single institution over a 3-year period. Multivariable statistical modeling and Akaike’s Information Criterion (AIC) comparisons were used to investigate the unique associations with, and relative importance of, these factors in accounting for variation in preoperative PSS and its subscores.
Results:
788 cases performed by 12 surgeons met inclusion criteria, with a preoperative median total PSS of 31 (pain 10, function 18, satisfaction 1). As hypothesized, lower VR-12 MCS was associated with lower preoperative PSS pain, function and total scores, but patients with intact or small/medium rotator cuff tears had modestly lower PSS pain scores (i.e., more pain) than patients with a large/massive superior-posterior rotator cuff tear. Glenoid bone loss was not associated with preoperative PSS. Female sex, fewer years of education (for all four outcomes), lower VR-12 MCS and preoperative opioid use (for all outcomes but satisfaction), and rotator cuff tear severity (for pain only) were the factors most prominently associated with preoperative PROMs.
Conclusion:
In addition to mental health status and rotator cuff tear status, patient sex, years of education, and preoperative opioid use were most prominently associated with preoperative PROMs in patients undergoing shoulder arthroplasty. Further studies are needed to investigate if these factors will also predict postoperative PROMs.
Keywords: Shoulder arthroplasty, pain, function, satisfaction, PROMs, PENN shoulder score, preoperative factors, multivariable model
The number of shoulder arthroplasty procedures performed in the United States continues to rise, with current estimates ranging from 55,000–80,000 per year, and increases of 300% or more expected in the coming years. 11; 25; 35 Baseline preoperative symptoms related to pain and function are often used as indications for performing primary shoulder arthroplasty 13; 26; 31; 53, yet the relationships of general patient factors and pathologic characteristics with preoperative pain and function in patients undergoing primary shoulder arthroplasty have not been studied.
To address the need for high-quality, prospective, standardized data surrounding orthopedic procedures, the Cleveland Clinic has developed the Outcomes Management and Evaluation system (OME) 7; 12; 39. Currently, OME prospectively collects sociodemographic factors, joint-specific disease severity and treatment variables, and joint-specific validated patient-reported outcome measures (PROMs), preoperatively and at one year post-treatment, for over thirty elective orthopedic procedures. Data are electronically stored in a secure Research Electronic Data Capture (REDCap) 17 database. As of November 2019, OME has been used by 72 orthopedists at 16 sites within the Cleveland Clinic Health System to document episode of care details and preoperative PROMs on 97% of over 44,000 elective knee, hip, and shoulder surgeries, including over 2,500 cases of shoulder arthroplasty. The OME cohort has been successfully used to evaluate the relationships of general patient factors and pathologic characteristics with preoperative pain and function in patients undergoing other elective orthopedic procedures, including lower extremity arthroplasty 52 and rotator cuff repair surgery 40.
We hypothesized that worse mental health status, glenoid bone loss, and increasing rotator cuff tear severity would be associated with lower/worse preoperative total PENN Shoulder Score (PSS) and its pain, function, and satisfaction subscores in patients undergoing primary shoulder arthroplasty. We tested these hypotheses and examined additional relationships in the prospectively collected, comprehensive, and standardized OME cohort data using multivariable modeling with control for confounding by general patient and disease-specific factors.
Materials and Methods
Primary Shoulder Arthroplasty Surgical Cohort
Patients undergoing primary shoulder arthroplasty (anatomic, reverse or hemiarthroplasty) at the Cleveland Clinic Health System between February 2015 and February 2018 and having a diagnosis of glenohumeral osteoarthritis (OA) or rotator cuff tear arthropathy (CTA) were eligible for the study. Patients having a history of joint infection in the operative shoulder, undergoing primary shoulder arthroplasty for a diagnosis other than OA or CTA, or having incomplete preoperative PROMs data were sequentially excluded.
Variable Selection
PSS was selected as the PROM for use. PSS is a valid and reliable outcome tool scored 0 to 100. Its sub-domains include pain (3 items, each on a 10-point scale; 0–30 points), function (20 items, each on a 4-point scale; normalized to 0–60 points), and satisfaction (1 item; 0–10 points), with higher scores representing less pain, better function, and higher satisfaction 27.
No outcome-driven variable selection was performed. A total of 16 preoperative patient and disease-specific variables were prospectively identified as possible predictors for preoperative pain, function, and satisfaction, and possible confounders of the relationships of mental health, glenoid bone loss, or tear severity with these outcomes. These preselected baseline variables included 12 general patient factors (age, sex, race, body mass index (BMI), smoking status (non-smoker, former, current), preoperative opioid use, years of education, employment status (not employed, employed, retired), worker’s compensation status, mental health status as assessed by VR-12 mental component score (VR-12 MCS), comorbidities (Charlson comorbidity index [CCI]), and chronic pain), and 4 disease-specific factors (prior shoulder surgery, glenoid bone loss, superior-posterior rotator cuff tendon status and subscapularis tendon status).
Data Source
Data on 11 of the 16 preoperative patient and disease-specific factors were obtained from the Cleveland Clinic’s OME database 7, which is approved by Cleveland Clinic’s Institutional Review Board (IRB #06–196) and has been shown to be a valid and efficient tool for collecting comprehensive and standardized data on multiple orthopedic surgeries 3; 7; 14; 32; 39; 44. The 4 disease-specific factors were entered prospectively into the OME database within 48 hours of surgery by the operating surgeon using a smartphone, laptop, or desktop computer to access an email link sent by the system immediately after procedure completion. Data on 5 preoperative factors (race, comorbidities, preoperative opioid use, chronic pain, and worker’s compensation status) were obtained from the Cleveland Clinic’s electronic medical record (EMR, Epic Systems, Verona WI), Perioperative Health Documentation System database (PHDS), and Epic Cost of Goods Sold (COGS) system. CCI was calculated from the comorbidity data 37. Preoperative opioid use was counted “yes” if an opioid was prescribed in the patient’s EMR and/or ordered from COGS between 3 months and 24 hours before surgery. Chronic pain was counted “yes” if the patient’s EMR contained an ICD-9 diagnosis code of 338.2 (chronic pain) and/or 304.0x (opioid dependence). Occasional data inconsistencies missed by routine database consistency checking were corrected when possible prior to analysis.
Statistical Analysis
Distributions of continuous variables were summarized as median (interquartile range), and of categorical variables by frequency count (%) for each category. The frequency counts for categorical predictors were assessed a priori for appropriate opportunities to group clinically similar categories, or to identify categories likely too small to allow identification of distinguishable effects. Glenoid bone loss, categorized in OME by region of the glenoid (central, anterior, posterior, superior) based on surgeon assessment of preoperative imaging and intraoperative findings, was condensed into a “yes/no” categorization for analysis. Rotator cuff pathology was assessed intraoperatively by the operating surgeon and classified, separately for each of the superior-posterior rotator cuff and the subscapularis, as intact or full-thickness tear (small: 0–1cm, medium: 1–3cm, large: 3–5cm, or massive: >5cm). For our analyses, each was initially reduced to a trichotomy of intact, small/medium, and large/massive tears due to small counts in some categories. Then, because certain tear combinations were strongly associated (Table 1), the categories were further reduced into a single composite ‘RC status’ variable with Subgroups 1: intact or small/medium tears in both the superior-posterior rotator cuff and subscapularis; 2 through 4: large/massive tears in the superior-posterior rotator cuff with subscapularis status classified respectively as intact, small/medium, or large/massive tear; and 5: large/massive subscapularis tear with intact or small/medium tear in the superior-posterior rotator cuff. Due to its small size (n=5), Subgroup 5 was dropped from further analysis (Figure 1). The distinction between RC Status Subgroup 1 and Subgroups 2–4 was found to almost perfectly capture preoperative diagnosis, with 99.6% (550/552) of Subgroup 1 patients having the diagnosis of glenohumeral OA and 94.1% (222/236) of patients in Subgroups 2 through 4 having the diagnosis of CTA. This almost complete collinearity allowed inclusion of either RC Status or diagnosis but not both in multivariable models. Therefore, for statistical analysis RC status was retained as providing more information while essentially conveying the diagnostic distinction, when dichotomized by thresholding between Subgroups 1 vs. Subgroups 2–4.
Table 1.
Coupled frequencies of superior-posterior rotator cuff and subscapularis status across the patient cohort were used to reduce patients into one of five ‘Rotator Cuff (RC) status’ Subgroups as indicated by superscripts 1–5.
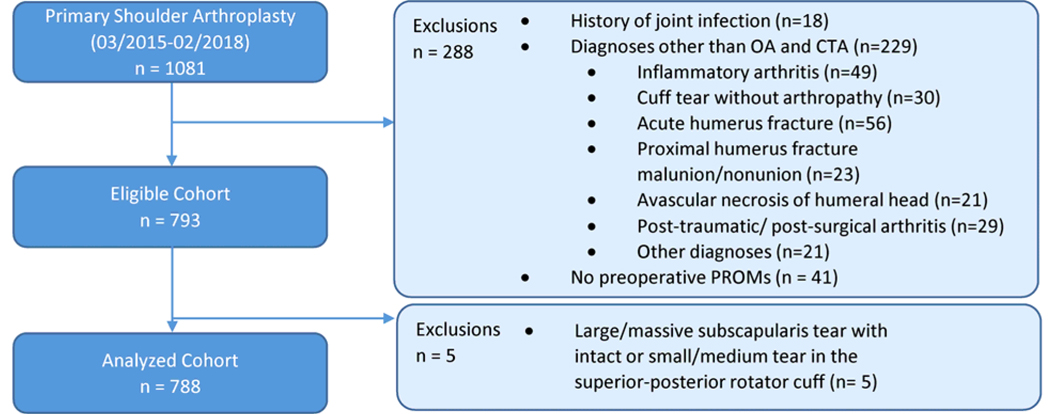
Figure 1.
Flow diagram describing sequential patient exclusions to arrive at the primary shoulder arthroplasty surgical cohort.
Of the remaining sample (n=788), 81 (10.2%) had missing data on race, 10 (1.3%) on employment status, two (0.2%) on education, one (0.1%) on smoking status, and one (0.1%) on VR-12 MCS; data on all other predictors and PSS scores were complete. The missing data were multiply imputed using multivariate imputation by chained equations (MICE), an iterative fully conditional multiple imputation approach (mice R package 45). The 16 predictors and four outcome variables were all included in the imputation model. Subsequent statistical analyses were performed identically and in parallel on all imputations, with results from the separate imputation sets combined using Rubin’s standard formula 38.
Multivariable modeling was performed to investigate the unique associations of the three hypothesized correlates (VR-12 MCS, glenoid bone loss, and RC status) with preoperative PSS (total score, pain, function, and satisfaction subscores) while adjusting to control for potential confounding by each other, the eleven other general patient factors and the single other disease-specific factor, prior shoulder surgery. PSS total score, pain, and function subscores were modeled using linear regression and PSS satisfaction scores were modeled using proportional (cumulative) odds logistic regression due to violations of linear regression assumptions. Age, BMI, years of education, VR-12 MCS, and CCI were treated as continuous variables, and their effects modeled by linear trends in their respective measurement units on the appropriate scale of the response. Trichotomous nominal predictors (race, smoking status, employment status) were modeled categorically. For the effect of RC status on preoperative PSS, we focused attention on the effect of large/massive superior-posterior tendon tears (RC status Subgroup 1 vs. Subgroups 2–4) and the “pseudo-linear” effects of increasing subscapularis tear severity in the presence of a large/massive superior-posterior tendon tear (RC status Subgroup 2 through 4 trend). We also conducted exploratory analysis of nonlinear differences among those three categories.
The effects of each predictor on the PSS total, pain, and function scores, and the cumulative odds-ratios of each variable on PSS satisfaction score were estimated, and their 95% confidence intervals and p-values and adjusted-R2 values for each model (Nagelkerke’s R2 for satisfaction) were also reported. The relative importances of each variable in explaining variation in preoperative PROMs were assessed by calculating and ranking the increases in Akaike’s Information Criterion (AIC) 21 upon removal of that variable from the full model.
Separately testing relationships of each variable of interest with the PSS total score and each of three subscores, and separately comparing multiple pairs of levels of factors with more than two levels, are conducive to false positive findings. We therefore limited false positive errors by using the Bonferroni-Holm multiple comparison adjustment, with a familywise Type I error rate of 0.05, to conduct simultaneous tests of each variable in relation to the four PSS measures, and by employing multiple degree of freedom omnibus tests rather than paired comparisons to assess differences among levels of categorical variables with > 2 levels.
We used sensitivity analyses to examine the effect of diagnosis on our results. Given the very few discrepancies between RC Status Subgroup 1 and glenohumeral OA, for consistency with all other analyses we used the RC Status dichotomization introduced above (Subgroup 1 vs. Subgroups 2–4) for this purpose rather than the diagnosis of record. We checked for whether associations of preoperative variables with preoperative PROMs varied with the two diagnostic categories by fitting models in which relationships between the preoperative variables and PROMs were allowed to vary between RC status Subgroup 1 (99.6% glenohumeral OA patients) and the combined RC status Subgroups 2–4 (94.1% CTA patients). This was done by expanding the primary multivariable model to include a separate effect of each predictor in RC status Subgroup 1, both in nested models where this was done for each predictor individually and in a single mutually adjusted nested model with separate effects of all predictors in Subgroup 1 distinct from their effects in Subgroups 2–4.
Also, possible interactions of any statistically significant focal variable (VR-12 MCS, glenoid bone loss, and RC status) with other statistically significant predictors were examined by augmenting the models for each outcome simultaneously by this subset of first-order interactions. Because correlated predictors may conceal each other’s effects, we not only examined models containing all of these interactions simultaneously, but also used forward and backward selection to check that prominent interactions were not hidden by mutual adjustments. Second, we removed plausible causal mediators, specifically, six patient factors (mental health status, chronic pain, preoperative opioid use, smoking status, employment status, and worker’s compensation status) from our prespecified primary models because such mutual-adjustment models may overmatch, obscuring stronger relationships by analytically mistaking causal mediators for confounders. We heuristically evaluated the potential masking of covariate effect by fitting six additional separate partial models, each including one of these six variables in turn and examining, in each model, the decrease in the retained variable’s effect-magnitude in the full model compared to the partial model. All statistical analyses were performed using R software (R version 3.5.0 (2018–4-23), Vienna, Austria). Consistent with recent appeals by many leaders of the statistical profession for a de-emphasis of dichotomous, null hypothesis significance testing in scientific practice 49; 50, we use statistical tests of hypotheses to inform but not dictate our assessments of scientific findings, and subordinate use of the technical term “statistical significance” to more holistic descriptions.
Results
A total of 1,081 cases undergoing primary shoulder arthroplasty at Cleveland Clinic facilities between February 2015 and February 2018 were captured in the OME database (Figure 1). 288 of these cases were sequentially excluded based on study-specific exclusion criteria: (1) a history of joint infection (n=18), (2) a diagnosis other than glenohumeral OA or CTA (n=229), and (3) incomplete preoperative PROM data (n=41). Ultimately 793 primary shoulder arthroplasty cases performed by 12 surgeons were retained, with 5 in the rare RC status subgroup 5 further excluded, leaving a cohort of 788 patients for analysis. Table 2 shows the distributions of cases by diagnosis and arthroplasty type.
Table 2.
Cross-classification of type of primary shoulder arthroplasty by primary diagnosis: n (%)
| Arthroplasty Type | Diagnosis | Total | |
|---|---|---|---|
| Glenohumeral osteoarthritis | Rotator cuff tear arthropathy | ||
| Anatomic | 354 (100%) | 0 (0%) | 354 (45%) |
| Reverse | 182 (47%) | 209 (53%) | 391 (50%) |
| Hemi | 28 (65%) | 15 (35%) | 43 (5%) |
| Total | 564 (72%) | 224 (28%) | 788 |
General patient and disease-specific characteristics
Table 3 presents the general patient and disease-specific characteristics of this sample. Patients had a median age of 68 years, BMI of 30.1, 14 years of education, VR-12 MCS of 52.1, and CCI of 2. The great majority (92%) were white, 55% were males, 50% were current or former smokers, 43% had chronic pain, and 36% had used opioids preoperatively between 3 months and 24 hours before surgery. 52% had glenoid bone loss and 18% had histories of prior shoulder surgery. Regarding rotator cuff status, 66% had an intact superior-posterior rotator cuff and 89% had an intact subscapularis tendon. Diagnosis was glenohumeral OA in 72% and CTA in 28% of cases.
Table 3.
Preoperative patient demographic and disease-specific characteristics of 788 patients undergoing primary shoulder arthroplasty. Results are presented as median (interquartile range, IQR) for numeric variables*, and counts (%) for categorical variables.
| Variable | Category | Value |
|---|---|---|
| Demographic characteristics | ||
| *Age (years) | 68 (61–74) | |
| *BMI | 30.1 (26.7–34.3) | |
| *CCI | 2 (0–4) | |
| *Education (years) | 14 (12–16) | |
| *VR-12 MCS | 52 (41.8–60.8) | |
| Sex | Female | 356 (45%) |
| Male | 432 (55%) | |
| Race | White | 650 (92%) |
| Black | 49 (7%) | |
| Other | 8 (1%) | |
| #Not available | 81 | |
| Smoking status | Current | 76 (10%) |
| Quit | 312 (40%) | |
| Never | 399 (51%) | |
| #Not available | 1 | |
| Preoperative opioid use | Yes | 285 (36%) |
| No | 503 (64%) | |
| Chronic pain | Yes | 338 (43%) |
| No | 450 (57%) | |
| Employment status | Employed | 194 (25%) |
| Retired | 253 (32%) | |
| Not employed | 331 (42%) | |
| #Not available | 10 | |
| Worker’s compensation | Yes | 16 (2%) |
| No | 772 (98%) | |
| Disease-specific characteristics | ||
| Prior shoulder surgery | Yes | 142 (18%) |
| No | 646 (82%) | |
| Glenoid bone loss | Yes | 411 (52%) |
| No | 377 (48%) | |
| Superior-posterior RC status | Large/massive tear | 236 (30%) |
| Small/medium tear | 31 (4%) | |
| Intact | 521 (66%) | |
| Subscapularis status | Large/massive tear | 38 (5%) |
| Small/medium tear | 47 (6%) | |
| Intact | 703 (89%) | |
| Rotator cuff status‡ | 1 | 552 (70%) |
| 2 | 153 (19%) | |
| 3 | 45 (6%) | |
| 4 | 38 (5%) | |
| Diagnosis | Glenohumeral osteoarthritis | 564 (72%) |
| Rotator cuff tear arthropathy | 224 (28%) | |
“Not Available” figures were not included in % calculations
Rotator cuff status subgroup 1: intact or small/medium tears in both the superior-posterior rotator cuff and subscapularis; subgroups 2 through 4: large/massive tears in the superior-posterior rotator cuff with subscapularis status classified respectively as (2) intact, (3) small/medium, or (4) large/massive tear
Preoperative PSS
Table 4 presents the preoperative PSS (total, and pain, function, satisfaction subscores) in the 788 patients. Patients had median total PSS of 31, pain score of 10, function score of 18, and satisfaction score of 1.
Table 4.
Preoperative PENN Shoulder Score (PSS) (total, and pain, function, satisfaction subscores) in the 788 patients undergoing primary shoulder arthroplasty.
| Preoperative PSS | Value [Median (IQR)] | Possible Range (min – max) |
|---|---|---|
| Total | 31 (20 – 42) | 0– 100 |
| Pain | 10 (6 – 15) | 0– 30 |
| Function | 18 (11 – 27) | 0– 60 |
| Satisfaction | 1 (0 – 3) | 0– 10 |
Multivariable modeling
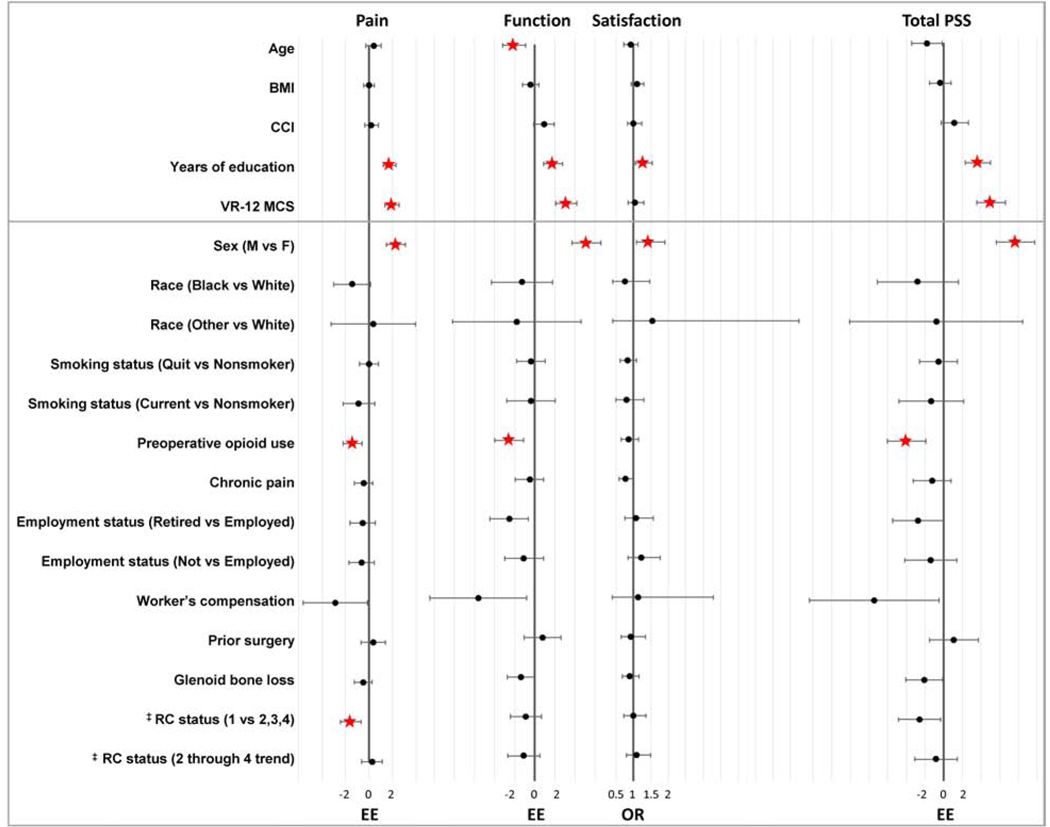
By adjusted R2, the 15 general patient and disease-specific factors in the full models accounted for 21–23% of the variability in the three continuous outcome variables (total PSS, pain and function subscores). Table 5 reports, and Figure 2 graphically portrays, the estimated effects, confidence intervals, and multiple-comparison adjusted test results for the 12 general patient and 3 disease-specific factors (including the combined superior-posterior rotator cuff and subscapularis tendon statuses) for preoperative PSS and each subscore. Of the three hypothesized predictors, lower VR-12 MCS was associated with lower (worse) PSS pain, function and total scores, with a total score difference of 5.1 points between patients at the upper and lower VR-12 MCS quartiles. Consistent with our hypothesis, patients with glenoid bone loss exhibited lower total PSS and subscores than those without, but estimated effect sizes were modest (−2.1 on total score) and all differences were within the multiple comparison adjusted range of chance variation. Patients with intact or small/medium rotator cuff tears (RC status Subgroup 1) had modestly lower (−1.6 points) PSS pain scores on average than patients with a large/massive superior-posterior rotator cuff tear (Subgroups 2, 3, 4 combined). Among the patients with large/massive superior-posterior rotator cuff tears (Subgroups 2–4), there was no substantial evidence to suggest an effect of increasing subscapularis tear size on PSS scores (Table 5).
Table 5.
Estimated effects and odds ratios of general patient factors, and disease-specific factors for preoperative PENN Shoulder Score (PSS), and 95% confidence intervals for each predictor in the full models in patients undergoing primary shoulder arthroplasty. The effects for numeric variables (Age, BMI, Education, VR-12 MCS, and CCI) are comparing the 25th vs. 75th percentiles shown in Table 1.
| PSS-Pain | PSS-Function | PSS-Satisfaction | Total PSS | ||
|---|---|---|---|---|---|
| Variable | Level | Estimated effect | Estimated effect | Odds Ratio | Estimated effect |
| Demographic characteristics | |||||
| Age | 0.4 (−0.3, 1.0) | −2.1 (−3.2, −0.9)* | 0.91 (0.72, 1.13) | −1.8 (−3.4, −0.1) | |
| BMI | −0.01 (−0.4, 0.4) | −0.4 (−1.2, 0.4) | 1.1 (0.93, 1.29) | −0.4 (−1.5, 0.8) | |
| CCI | 0.2 (−0.4, 0.8) | 0.9 (−0.1, 1.9) | 1 (0.82, 1.23) | 1.2 (−0.3, 2.6) | |
| Education | 1.7 (1.2, 2.3)* | 1.8 (0.9, 2.7)* | 1.28 (1.06, 1.54)* | 3.7 (2.3, 5.0)* | |
| VR-12 MCS | 1.9 (1.3, 2.5)* | 3.1 (2.1, 4.2)* | 1.04 (0.84, 1.29) | 5.1 (3.5, 6.6)* | |
| Sex | Female | - | - | - | - |
| Male | 2.3 (1.5, 3.1)* | 5.2 (3.7, 6.6)* | 1.43 (1.08, 1.89)* | 7.7 (5.6, 9.7)* | |
| Race | White | - | - | - | - |
| Black | −1.4 (−3.0, 0.1) | −1.3 (−4.3, 1.8) | 0.76 (0.4, 1.46) | −2.8 (−7.1, 1.6) | |
| Other/ missing | 0.3 (−3.3, 3.9) | −1.8 (−8.2, 4.6) | 1.53 (0.41, 5.75) | −0.8 (−10.1, 8.5) | |
| Smoking status | Never | - | - | - | - |
| Quit | 0 (−0.8,0.8) | −0.4 (−1.8,1.0) | 0.82 (0.62,1.08) | −0.54 (−2.6,1.5) | |
| Current | −0.9 (−2.2,0.5) | −0.4 (−2.8,2.0) | 0.79 (0.49,1.29) | −1.3 (−4.8,2.1) | |
| Preoperative opioid use | No | - | - | - | - |
| Yes | −1.4 (−2.2, −0.6)* | −2.5 (−4.0, −1.1)* | 0.86 (0.65,1.15) | −4.0 (−6.0, −1.9)* | |
| Chronic pain | No | - | - | - | - |
| Yes | −0.5 (−1.3,0.3) | −0.5 (−1.9,0.9) | 0.77 (0.58,1.01) | −1.3 (−3.3,0.8) | |
| Employment status | Employed | - | - | - | - |
| Retired | −0.6 (−1.7,0.4) | −1.1 (−3.0,0.9) | 1.22 (0.84,1.76) | −1.4 (−4.2,1.4) | |
| Not-employed | −0.6 (−1.6,0.5) | −2.5 (−4.4, −0.6) | 1.08 (0.75,1.57) | −2.7 (−5.5, −0.01) | |
| Worker’s compensation | No | - | - | - | - |
| Yes | −2.9 (−5.6, −0.2) | −5.6 (−10.4, −0.8) | 1.13 (0.39,3.28) | −7.4 (−14.4, −0.5) | |
| Surgical characteristics | |||||
| Prior surgery | No | - | - | - | - |
| Yes | 0.4 (−0.7,1.4) | 0.8 (−1.0,2.6) | 0.93 (0.64,1.34) | 1.1 (−1.5,3.7) | |
| Glenoid bone loss | No | - | - | - | - |
| Yes | −0.5 (−1.3,0.2) | −1.4 (−2.8, −0.02) | 0.89 (0.68,1.16) | −2.1 (−4.0, −0.1) | |
| RC status‡ | 1 | - | - | - | - |
| 2 | 1.7 (0.7,2.7) | 1.4 (−0.4,3.2) | 0.94 (0.65,1.35) | 3.1 (0.5,5.8) | |
| 3 | 0.05 (−1.6,1.7) | 0.6 (−2.3,3.6) | 1.41 (0.76,2.62) | 1.5 (−2.7,5.8) | |
| 4 | 2.8 (1.0,4.6) | −0.9 (−4.0,2.2) | 0.95 (0.51,1.75) | 1.7 (−2.8,6.2) | |
| 1 vs (2,3,4) | −1.6 (−2.4, −0.7)* | −0.9 (−2.4, 0.7) | 0.99 (0.72, 1.36) | −2.6 (−4.8, −0.3) | |
| 2 through 4 trend | 0.2 (−0.6, 1.1) | −1.1 (−2.7, 0.5) | 1.09 (0.80, 1.49) | −0.8 (−3.1, 1.4) | |
indicates statistically significant associations (in Bonferroni-Holm adjusted pairwise comparisons for 4 outcomes and omnibus tests for trichotomous variables).
Rotator cuff status subgroup 1: intact or small/medium tears in both the superior-posterior rotator cuff and subscapularis; subgroups 2 through 4: large/massive tears in the superior-posterior rotator cuff with subscapularis status classified respectively as (2) intact, (3) small/medium, or (4) large/massive tear
Figure 2.
Forest plot showing the estimated regression coefficients (EE) for pain and function subscores and total PENN Shoulder Score (PSS), odds ratios (OR) for satisfaction sub score, each with 95% confidence intervals, for predictors in the full models of patients undergoing primary shoulder arthroplasty. The effects for numeric variables (age, BMI, education, VR-12 MCS, and CCI) are comparing the 75th vs. 25th percentiles shown in Table 1. Predictors having statistically significant associations, both in omnibus tests and Bonferroni-Holm adjusted pairwise comparisons for trichotomous variables, with preoperative PSS are marked in red. ‡RC status Subgroup 1: intact or small/medium tears in both the superior-posterior rotator cuff and subscapularis; subgroups 2 through 4: large/massive tears in the superior-posterior rotator cuff with subscapularis status classified respectively as (2) intact, (3) small/medium, or (4) large/massive tear
In looking at the other general patient factors within the same comprehensive multivariable models, notable associations were of female sex and less education with lower total PSS (−7.7 points, and −3.7 points per 4 years, respectively) and all 3 subscores; preoperative opioid use with lower (−4.0 points) total PSS, and pain and function subscores; and older age with lower (−2.1 points per 13 years) PSS function score (Table 5).
Relative prominence of predictor associations with preoperative PSS
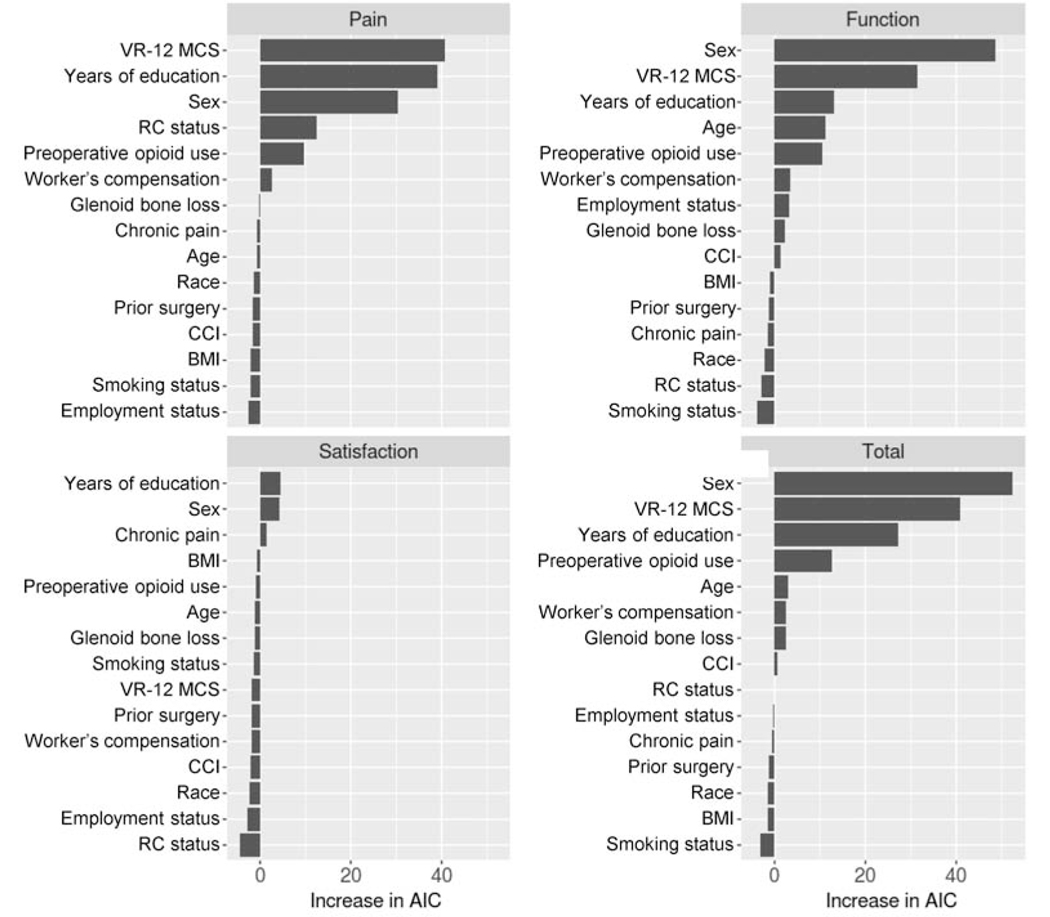
Figure 3 compares the AIC increases from removal of each variable from the full model, as a gauge of relative importance of their contributions. The top five variables accounted for 95–98% of the total variances explained by the 15 predictors in the full models for total PSS and the pain and function subscores, and 78% of the relative likelihood improvement (Nagelkerke R2) in the model for the satisfaction subscore. Sex and education were among the most important variables for all four outcomes, and VR-12 MCS and preoperative opioid use for all but the PSS satisfaction score. Rotator cuff status, reflecting tear severity, was an important contributor only to the PSS pain score.
Figure 3.
Relative variable importance of patient demographic and disease-specific characteristics on preoperative PENN Shoulder Score (PSS), based on the increase in AIC upon removal from the full model. The most influential variables are listed on the top of the respective charts.
Effect of preoperative diagnosis on preoperative PSS
Results of the mutually adjusted models with separate effects for predictors in RC status Subgroup 1 (glenohumeral OA patients) did not differ notably from results of models where this was done for each predictor individually; hence, we report only the former. Retirement was associated with a three-point lower preoperative PSS total score than current employment among glenohumeral OA patients (RC status Subgroup 1) but a five-point higher score among CTA patients (RC status Subgroups 2–4). This result was primarily driven by the function subscore but with contributions from the satisfaction and pain subscore. PSS total score was slightly (1.3 points) lower among patients at the 75th than among those at the 25th percentile of BMI in the glenohumeral OA group but slightly (1.8 points) higher among the CTA group, a result driven by the function subscore with contribution from the pain but not the satisfaction subscore. Patients with prior surgery scored 0.2 points lower than those without in the glenohumeral OA subgroup but 2.8 points higher among the CTA group, driven by both function and pain but not satisfaction. The intergroup differences in effects of retirement and BMI on total score and the function subscore and of prior surgery on pain exceeded chance variation. Other differences in associations between glenohumeral OA and CTA patients were neither clinically or statistically notable, and only the two associations with the function subscore withstood Bonferroni-Holm multiple comparison correction for parallel analyses of the PSS total and three subscores. Overall, there was minimal evidence for substantively meaningful differences between the effects of predictors studied in glenohumeral OA and CTA patients, and none of the variables for which evidence was found showed notable overall associations in our primary analyses. Supplement Table S1 summarizes the fitted mutually adjusted models.
Remaining interaction analysis
In analyses of interactions among other variables, no additional pairwise interactions among those screened exceeded chance variation after multiple comparison adjustment. Removal of possible causal mediators from the full model left the effects of VR-12 MCS for all four PSS scores relatively unchanged. The most dramatic increases in effect-sizes from the full to partial models were in the associations of chronic pain, employment status, and smoking status with the pain and function subscores and total PSS, although their associations with the satisfaction subscore were insensitive to the level of adjustment (Table S2). Among the increased associations, those of employment status with PSS function and total scores satisfied the Bonferroni-Holm criterion for familywise false positive error control.
Discussion
The purpose of this study was to investigate the extent to which general patient factors and disease-specific factors are associated with preoperative PROMs in patients undergoing primary shoulder arthroplasty. We hypothesized that worse mental health status, glenoid bone loss, and increasing rotator cuff tear severity would be associated with worse preoperative total PSS and its pain, function, and satisfaction subscores. Using prospectively collected data on 16 potential general patient and disease-specific correlates of preoperative symptoms, we performed multivariable analyses of 788 patients undergoing primary shoulder arthroplasty for a diagnosis of glenohumeral OA or CTA. After simultaneous adjustment for the other variables, lower mental health status was, as hypothesized, associated with worse preoperative PSS (total score and pain and function subscores). The associations of glenoid bone loss with PSS did not exceed chance variability and, contrary to our hypothesis, large/massive superior-posterior rotator cuff tears were associated with higher preoperative PSS pain subscores (i.e., less pain) than intact or small/medium tears.
The associations between disease-related factors (e.g., rotator cuff status, glenoid bone loss, and prior shoulder surgery) and preoperative shoulder pain and function in patients undergoing primary shoulder arthroplasty have not been previously reported. In the current investigation, lower PSS pain subscores (i.e., more pain) in patients with an intact rotator cuff or smaller tears of the superior-posterior rotator cuff may be explained by a compressive effect of an intact or nearly intact rotator cuff in an arthritic joint, although the difference (1.6 points on PSS pain) may not be clinically significant. This finding may also suggest that the primary driver of pain complaints in this patient population is the advanced arthritic changes rather than rotator cuff status. Glenoid bone loss, which is common in advanced glenohumeral OA and advanced CTA, leads to more complex glenoid deformities that can be harder to correct at the time of surgery and have been associated with worse postoperative outcomes 19; 20; 48. Our data demonstrate lower preoperative total PSS and PSS function scores in patients with glenoid bone loss; however, the estimated differences (2.1 points in PSS total and 1.4 points in PSS function) were neither clinically significant, nor statistically significant after Bonferroni-Holm adjustment. Prior shoulder surgery was not notably associated with lower preoperative PROMs, although prior surgery is associated with poorer outcomes such as worse pain, lower range of motion and inferior PROMs, as well as increased infection risk, in patients following shoulder arthroplasty 29; 30; 42; 51. Finally, although glenohumeral OA and CTA are separate disease processes, the diagnoses were found to be highly correlated with RC status in our cohort. Nested models with separate effects of factors in the RC status subgroups, that were nearly identical to the glenohumeral OA (Subgroup 1) and CTA (Subgroups 2–4) groups, were run to determine if the predictors of preoperative PROMs differed with these two diagnoses. Although some small differences were seen based on diagnosis, overall there was minimal evidence for substantively meaningful differences between the associations of preoperative PROMs with the predictors we studied in glenohumeral OA and CTA patients.
The associations between general patient factors and preoperative shoulder PROMs in patients undergoing primary shoulder arthroplasty have also received very limited investigation to date 22; 33; 34; 55. Previous studies have shown patient factors such as female sex, less education, lower mental health status, preoperative opioid use, higher age, higher BMI, smoking, more comorbidities, and receipt of worker’s compensation to be significantly and negatively associated with PROMs following shoulder arthroplasty 10; 15; 18; 43; 46; 47; 54–56. Our results showed that female sex and less education were associated with lower total preoperative PSS and all 3 subscores, and lower VR-12 MCS and preoperative opioid use were associated with lower total preoperative PSS, pain and function subscores. Two much smaller previous studies 22; 55 did not find evident of sex associated differences in preoperative shoulder PROMs in patients undergoing shoulder arthroplasty. In addition to the lower statistical power of smaller studies, these differences may also be due to prior studies’ narrower patient selection criteria (e.g., inclusion of only anatomic or reverse TSA) and much more limited control for confounding. Further, it is not clear why some general patient factors impact only postoperative PROMs but not preoperative PROMs in past literature. We plan to investigate the associations of these general patient factors with postoperative PROMs in the OME cohort in future work.
The association between lower mental health status and worse preoperative shoulder PROMs has been previously demonstrated in patients undergoing RCR 1; 5; 6; 8; 36; 40; 56; 57, but such an association has not been shown prior to shoulder arthroplasty 54. Lower preoperative pain and function scores in patients with lower preoperative VR-12 MCS could be due to preexisting mental health issues in such patients that may alter how patients perceive their shoulder pain and function. Alternatively, physical and functional limitations resulting from the underlying pathology necessitating shoulder arthroplasty may adversely affect work performance, social activities, and mood reported in the VR-12 instrument 23; 41, lowering VR-12 MCS.
In principle mental health status, as reflected in VR-12 MCS, could also exert effects on PSS scores indirectly through effects on employment status and workers compensation, perception of chronic pain, and use of drugs including opioids and nicotine. Although our fully-adjusted models would have concealed such indirect effects, no changes in VR-12 MCS associations suggestive of indirect mental health status effects emerged in sensitivity analysis using partially-adjusted models where such mediated effects could appear. However, the effects of smoking status, chronic pain, and employment status noticeably increased in partially-adjusted as compared to fully-adjusted models. Such increases may reflect either understatement of plausibly causal effects in the fully-adjusted models due to inadvertent adjustment for causal mediators, or inadequate adjustment for confounding in the partially-adjusted models, explanations that cannot be differentiated statistically by analyses of such cross-sectional preoperative data.
Similar to our results, preoperative opioid use has been previously shown to be associated with worse preoperative shoulder PROMs in patients undergoing shoulder arthroplasty 33; 34, as well as with higher rates of certain comorbidities (including depression and chronic pain conditions), inferior postoperative outcomes, and continued postoperative opioid consumption following shoulder arthroplasty 2; 4; 9; 16; 24; 28; 33; 34. Taken together, these findings suggest that a patient’s preoperative opioid use may need to be considered when setting expectations with regard to arthroplasty outcomes.
The present study has several strengths. Though cross-sectional in nature, our data derive from a large prospectively ascertained cohort that captures a wide range of patient and surgical factors relevant to shoulder arthroplasty. Factors either cited or judged to influence preoperative symptoms were prospectively chosen and used in multivariable models to identify statistically meaningful associations. This is the first study to our knowledge that identifies factors associated with preoperative symptoms in a shoulder arthroplasty patient population while extensively controlling for general patient and disease-specific factors. Furthermore, we used the PSS, which is unique among the various shoulder-specific PROMs as it measures patient satisfaction related to the shoulder on a 10-point scale, in addition to measuring shoulder pain and function.
This study also has limitations. First, it was performed in a single tertiary hospital network using data from patients who have undergone surgery. Hence, our findings may not be generalizable to the broader group of patients with glenohumeral OA or CTA who are treated nonoperatively, or other patient populations or surgical practice settings. Second, our database does not include all possible factors that might influence preoperative symptoms, and some potentially important factors may not have been investigated. The database was prospectively designed by specialty-specific orthopedic surgeons at our institution to collect sociodemographic factors, joint-specific variables of disease severity and treatment, and joint-specific validated PROMs at baseline and one-year post-treatment, for over thirty elective orthopedic procedures. The number of questions asked and the number of factors collected were thus carefully selected so as not to overburden the patient or the surgeon. Third, while we identified clinically relevant factors that were associated with preoperative symptoms to a degree not plausibly explainable by chance variation, our cross-sectional analyses cannot adequately evaluate the causal component, if any, or clinical significance of associations. In particular, we acknowledge that our models explained less than 25% of the variation in all PSS scores, and most statistical effects of individual variables on PSS were generally small.
Conclusion
In addition to mental health status and rotator cuff tear status, patient sex, years of education, and preoperative opioid use were most prominently associated with preoperative PROMs in patients undergoing shoulder arthroplasty. Our future work will use multivariable prediction modeling of this large prospective cohort to investigate the extent to which risk factors associated with poor preoperative pain, function and satisfaction in the/ current study, together with disease-related and surgical factors, can predict postoperative PROMs one or more years after primary shoulder arthroplasty. If associations of risk factors with postoperative PROMs are notably stronger than with preoperative PROMs, such multivariable models could be clinically useful for identifying patients with poorer prognoses and, conceivably, for better understanding any associations of outcomes with preoperative pathology and surgical approaches.
Supplementary Material
Table S1. Model-fitted differences of means of PENN Shoulder Score (PSS) total, function and pain subscores, and differences of log odds ratios for satisfaction subscore, from nested models including all variables simultaneously. These models estimate separate effects for each variable for Subgroup 1 and pooled Subgroups 2–4 patients, comparisons of which examine disparities in associations between patients with glenohumeral osteoarthritis (Subgroup 1, 99.6%) and with rotator cuff tear arthropathy (Subgroups 2–4, 94.1%). Interaction p-values compare the two estimated parameters and test hypotheses that the effect of each variable is independent of disease subgroup.
Table S2. Estimated effects and odds ratios of six factors considered to be possible causal mediators for preoperative PENN Shoulder Score (PSS) in partial and full models.
Examples of interpretation of total PSS and pain and function subscores (standard linear regression model):
Males have total PSS and pain and function subscores that are 7.7, 2.3, and 5.2 points higher on average respectively than females, after controlling for all other variables.
A patient with VR-12 MCS of 60.8 (75th percentile) has total PSS and pain and function subscores that are 5.1, 1.9, and 3.1 points higher on average than a patient with VR-12 MCS of 41.8 (25th percentile), after controlling for all other variables.
Examples of interpretation of PSS-satisfaction subscore (proportional-odds regression model):
The odds that males have a PSS-satisfaction score of at least X (say 5, for example) are (1.43– 1)*100 = 43% higher than the odds that females have a PSS-Satisfaction score of at least 5, after adjusting for all other variables (Note: This interpretation holds regardless of the value of X; hence proportional-odds).
The odds that a patient with education of 16 years (75th percentile) has a PSS-satisfaction score of at least X are (1.28 – 1.00)*100 = 28% higher than the odds of a patient with education of 12 years (25th percentile), after controlling for all other variables.
Acknowledgments:
The authors acknowledge the following 12 Cleveland Clinic surgeons who contributed cases to the OME database for investigation in this study: Peter Evans, MD, Gregory Gilot, MD, Kirk Haidet MD, Robert Hampton MD, Joseph Iannotti, MD, PhD, Anthony Miniaci, MD, Eric Ricchetti, MD, Vani Sabesan, MD, Mark Schickendantz, MD, William Seitz, MD, Alfred Serna, MD, and Kim Stearns, MD.
We also acknowledge the Orthopaedic and Rheumatologic Institute at Cleveland Clinic for support of the OME database and related infrastructure.
Footnotes
Level of Evidence: Level III; Retrospective Case-Control Design; Prognosis Study
Disclosures: KPS and GS are inventors with rights to royalties from nPhase/REDCap Cloud for technology related to the subject of this article. The other authors have no conflicts.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Barlow JD, Bishop JY, Dunn WR, Kuhn JE, Group MS. What factors are predictors of emotional health in patients with full-thickness rotator cuff tears? J Shoulder Elbow Surg 2016; 25:1769–73. doi: 10.1016/j.jse.2016.04.007 [DOI] [PubMed] [Google Scholar]
- 2.Berglund DD, Rosas S, Kurowicki J, Horn B, Mijic D, Levy JC. Preoperative Opioid Use Among Patients Undergoing Shoulder Arthroplasty Predicts Prolonged Postoperative Opioid Use. J Am Acad Orthop Surg 2018; 27:e691–e95. doi: 10.5435/JAAOS-D-18-00008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown MC, Westermann RW, Hagen MS, Strnad GJ, Rosneck JT, Spindler KP et al. Validation of a Novel Surgical Data Capturing System After Hip Arthroscopy. J Am Acad Orthop Surg 2019; 27:e1009–e15. doi: 10.5435/JAAOS-D-18-00550 [DOI] [PubMed] [Google Scholar]
- 4.Cheah JW, Sing DC, McLaughlin D, Feeley BT, Ma CB, Zhang AL. The perioperative effects of chronic preoperative opioid use on shoulder arthroplasty outcomes. J Shoulder Elbow Surg 2017; 26:1908–14. doi: 10.1016/j.jse.2017.05.016 [DOI] [PubMed] [Google Scholar]
- 5.Cho CH, Jung SW, Park JY, Song KS, Yu KI. Is shoulder pain for three months or longer correlated with depression, anxiety, and sleep disturbance? J Shoulder Elbow Surg 2013; 22:222–8. doi: 10.1016/j.jse.2012.04.001 [DOI] [PubMed] [Google Scholar]
- 6.Cho CH, Seo HJ, Bae KC, Lee KJ, Hwang I, Warner JJ. The impact of depression and anxiety on self-assessed pain, disability, and quality of life in patients scheduled for rotator cuff repair. J Shoulder Elbow Surg 2013; 22:1160–6. doi: 10.1016/j.jse.2013.02.006 [DOI] [PubMed] [Google Scholar]
- 7.Piuzzi NS, Strnad G, Brooks P, Hettrich CM, Higuera-Rueda C et al. Implementing a Scientifically Valid, Cost-Effective, and Scalable Data Collection System at Point of Care: The Cleveland Clinic OME Cohort. J Bone Joint Surg Am 2019; 101:458–64. doi: 10.2106/JBJS.18.00767 [DOI] [PubMed] [Google Scholar]
- 8.Curry EJ, Matzkin EE, Dong Y, Higgins LD, Katz JN, Jain NB. Structural Characteristics Are Not Associated With Pain and Function in Rotator Cuff Tears: The ROW Cohort Study. Orthop J Sports Med 2015; 3:2325967115584596. doi: 10.1177/2325967115584596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Curtis W, Rounds AD, Stone M, Vangsness CT Jr., Weber AE, Hatch GFR, 3rd et al. Effect of Preoperative Opioid Usage on Pain After Total Shoulder Arthroplasty. J Am Acad Orthop Surg 2019; 27:e734–e42. doi: 10.5435/JAAOS-D-18-00112 [DOI] [PubMed] [Google Scholar]
- 10.Cvetanovich GL, Savin DD, Frank RM, Gowd AK, Sumner SA, Romeo AA et al. Inferior outcomes and higher complication rates after shoulder arthroplasty in workers’ compensation patients. J Shoulder Elbow Surg 2019; 28:875–81. doi: 10.1016/j.jse.2018.10.007 [DOI] [PubMed] [Google Scholar]
- 11.Day JS, Lau E, Ong KL, Williams GR, Ramsey ML, Kurtz SM. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Shoulder Elbow Surg 2010; 19:1115–20. doi: 10.1016/j.jse.2010.02.009 [DOI] [PubMed] [Google Scholar]
- 12.Derwin KA, Sahoo S, Zajichek A, Strnad G, Spindler KP, Iannotti JP et al. Tear characteristics and surgeon influence repair technique and suture anchor use in repair of superior-posterior rotator cuff tendon tears. J Shoulder Elbow Surg 2018. doi: 10.1016/j.jse.2018.07.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Erickson BJ, Bohl DD, Cole BJ, Verma NN, Nicholson G, Romeo AA et al. Reverse Total Shoulder Arthroplasty: Indications and Techniques Across the World. Am J Orthop (Belle Mead NJ) 2018; 47. doi: 10.12788/ajo.2018.0079 [DOI] [PubMed] [Google Scholar]
- 14.Featherall J, Oak SR, Strnad GJ, Farrow LD, Jones MH, Miniaci AA et al. Smartphone Data Capture Efficiently Augments Dictation for Knee Arthroscopic Surgery. J Am Acad Orthop Surg 2019. doi: 10.5435/JAAOS-D-19-00074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Friedman RJ, Cheung EV, Flurin PH, Wright T, Simovitch RW, Bolch C et al. Are Age and Patient Gender Associated With Different Rates and Magnitudes of Clinical Improvement After Reverse Shoulder Arthroplasty? Clin Orthop Relat Res 2018; 476:1264–73. doi: 10.1007/s11999.0000000000000270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grace TR, Khanna K, Choo KJ, Croci R, Feeley BT, Ma CB et al. The influence of preoperative opioid use on inpatient opioid requirements and discharge prescriptions after primary shoulder arthroplasty. J Shoulder Elbow Surg 2018; 27:1572–79. doi: 10.1016/j.jse.2018.02.067 [DOI] [PubMed] [Google Scholar]
- 17.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42:377–81. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hatta T, Werthel JD, Wagner ER, Itoi E, Steinmann SP, Cofield RH et al. Effect of smoking on complications following primary shoulder arthroplasty. J Shoulder Elbow Surg 2017; 26:1–6. doi: 10.1016/j.jse.2016.09.011 [DOI] [PubMed] [Google Scholar]
- 19.Ho JC, Amini MH, Entezari V, Jun BJ, Alolabi B, Ricchetti ET et al. Clinical and Radiographic Outcomes of a Posteriorly Augmented Glenoid Component in Anatomic Total Shoulder Arthroplasty for Primary Osteoarthritis with Posterior Glenoid Bone Loss. J Bone Joint Surg Am 2018; 100:1934–48. doi: 10.2106/JBJS.17.01282 [DOI] [PubMed] [Google Scholar]
- 20.Ho JC, Sabesan VJ, Iannotti JP. Glenoid component retroversion is associated with osteolysis. J Bone Joint Surg Am 2013; 95:e82. doi: 10.2106/JBJS.L.00336 [DOI] [PubMed] [Google Scholar]
- 21.James G, Witten D, Hastie T, Tibshirani RJ. Linear Model Selection and Regularization. In. An Introduction to Statistical Learning: Springer; 2013, p. 203–64. (ISBN No. ISBN 978-1-4614-7138-7) [Google Scholar]
- 22.Jawa A, Dasti U, Brown A, Grannatt K, Miller S. Gender differences in expectations and outcomes for total shoulder arthroplasty: a prospective cohort study. J Shoulder Elbow Surg 2016; 25:1323–7. doi: 10.1016/j.jse.2016.03.003 [DOI] [PubMed] [Google Scholar]
- 23.Kazis LE, Selim A, Rogers W, Ren XS, Lee A, Miller DR. Dissemination of methods and results from the veterans health study: final comments and implications for future monitoring strategies within and outside the veterans healthcare system. J Ambul Care Manage 2006; 29:310–9. doi: 10.1097/00004479-200610000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Khazi ZM, Lu Y, Patel BH, Cancienne JM, Werner B, Forsythe B. Risk factors for opioid use after total shoulder arthroplasty. J Shoulder Elbow Surg 2019. doi: 10.1016/j.jse.2019.06.020 [DOI] [PubMed] [Google Scholar]
- 25.Kim SH, Wise BL, Zhang Y, Szabo RM. Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg Am 2011; 93:2249–54. doi: 10.2106/JBJS.J.01994 [DOI] [PubMed] [Google Scholar]
- 26.Kircher J, Morhard M, Magosch P, Ebinger N, Lichtenberg S, Habermeyer P. How much are radiological parameters related to clinical symptoms and function in osteoarthritis of the shoulder? Int Orthop 2010; 34:677–81. doi: 10.1007/s00264-009-0846-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leggin BG, Michener LA, Shaffer MA, Brenneman SK, Iannotti JP, Williams GR Jr. The Penn shoulder score: reliability and validity. The Journal of orthopaedic and sports physical therapy 2006; 36:138–51. doi: 10.2519/jospt.2006.36.3.138 [DOI] [PubMed] [Google Scholar]
- 28.Leroux TS, Saltzman BM, Sumner SA, Maldonado-Rodriguez N, Agarwalla A, Ravi B et al. Elective Shoulder Surgery in the Opioid Naive: Rates of and Risk Factors for Long-term Postoperative Opioid Use. Am J Sports Med 2019; 47:1051–56. doi: 10.1177/0363546519837516 [DOI] [PubMed] [Google Scholar]
- 29.Mahony GT, Werner BC, Chang B, Grawe BM, Taylor SA, Craig EV et al. Risk factors for failing to achieve improvement after anatomic total shoulder arthroplasty for glenohumeral osteoarthritis. J Shoulder Elbow Surg 2018; 27:968–75. doi: 10.1016/j.jse.2017.12.018 [DOI] [PubMed] [Google Scholar]
- 30.Matsen FA, 3rd, Russ SM, Vu PT, Hsu JE, Lucas RM, Comstock BA. What Factors are Predictive of Patient-reported Outcomes? A Prospective Study of 337 Shoulder Arthroplasties. Clin Orthop Relat Res 2016; 474:2496–510. doi: 10.1007/s11999-016-4990-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mattei L, Mortera S, Arrigoni C, Castoldi F. Anatomic shoulder arthroplasty: an update on indications, technique, results and complication rates. Joints 2015; 3:72–7. doi: 10.11138/jts/2015.3.2.072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mohr J, Strnad GJ, Farrow L, Heinlein K, Hettrich CM, Jones MH et al. A smart decision: smartphone use for operative data collection in arthroscopic shoulder instability surgery. J Am Med Inform Assoc 2019; 26:1030–36. doi: 10.1093/jamia/ocz074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Morris BJ, Laughlin MS, Elkousy HA, Gartsman GM, Edwards TB. Preoperative opioid use and outcomes after reverse shoulder arthroplasty. J Shoulder Elbow Surg 2015; 24:11–6. doi: 10.1016/j.jse.2014.05.002 [DOI] [PubMed] [Google Scholar]
- 34.Morris BJ, Sciascia AD, Jacobs CA, Edwards TB. Preoperative opioid use associated with worse outcomes after anatomic shoulder arthroplasty. J Shoulder Elbow Surg 2016; 25:619–23. doi: 10.1016/j.jse.2015.09.017 [DOI] [PubMed] [Google Scholar]
- 35.Palsis JA, Simpson KN, Matthews JH, Traven S, Eichinger JK, Friedman RJ. Current Trends in the Use of Shoulder Arthroplasty in the United States. Orthopedics 2018; 41:e416–e23. doi: 10.3928/01477447-20180409-05 [DOI] [PubMed] [Google Scholar]
- 36.Potter MQ, Wylie JD, Greis PE, Burks RT, Tashjian RZ. Psychological distress negatively affects self-assessment of shoulder function in patients with rotator cuff tears. Clin Orthop Relat Res 2014; 472:3926–32. doi: 10.1007/s11999-014-3833-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005; 43:1130–9. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 38.Rubin DB. Multiple imputation after 18+ years. Journal of the American statistical Association 1996; 91:473–89. [Google Scholar]
- 39.Sahoo S, Mohr J, Strnad GJ, Vega J, Jones M, Schickendantz MS et al. Validity and efficiency of a smartphone-based electronic data collection tool for operative data in rotator cuff repair. J Shoulder Elbow Surg 2019; 28:1249–56. doi: 10.1016/j.jse.2018.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sahoo S, Ricchetti ET, Zajichek A, Group” CCS, Entezari V, Imrey PB et al. Associations of preoperative patient mental health, sociodemographic and clinical characteristics with baseline pain, function and satisfaction in patients undergoing rotator cuff repairs. Am J Sports Med 2019. doi: 10.1177/0363546519892570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schalet BD, Rothrock NE, Hays RD, Kazis LE, Cook KF, Rutsohn JP et al. Linking Physical and Mental Health Summary Scores from the Veterans RAND 12-Item Health Survey (VR-12) to the PROMIS((R)) Global Health Scale. J Gen Intern Med 2015; 30:1524–30. doi: 10.1007/s11606-015-3453-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shields EJW, Koueiter DM, Maerz T, Schwark A, Wiater JM. Previous Rotator Cuff Repair Is Associated With Inferior Clinical Outcomes After Reverse Total Shoulder Arthroplasty. Orthop J Sports Med 2017; 5:2325967117730311. doi: 10.1177/2325967117730311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Solberg MJ, Alqueza AB, Hunt TJ, Higgins LD. Predicting 1-Year Postoperative Visual Analog Scale Pain Scores and American Shoulder and Elbow Surgeons Function Scores in Total and Reverse Total Shoulder Arthroplasty. Am J Orthop (Belle Mead NJ) 2017; 46:E358–E65. No doi [PubMed] [Google Scholar]
- 44.Tariq MB, Jones MH, Strnad G, Sosic E, Cleveland Clinic OMESH, Spindler KP. A Last-Ditch Effort and Personalized Surgeon Letter Improves PROMs Follow-Up Rate in Sports Medicine Patients: A Crossover Randomized Controlled Trial. The journal of knee surgery 2019. doi: 10.1055/s-0039-1694057 [DOI] [PubMed] [Google Scholar]
- 45.van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. J Stat Soft 2011; 45:1–67. doi: 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- 46.Wagner ER, Houdek MT, Schleck C, Harmsen WS, Sanchez-Sotelo J, Cofield R et al. Increasing Body Mass Index Is Associated with Worse Outcomes After Shoulder Arthroplasty. J Bone Joint Surg Am 2017; 99:929–37. doi: 10.2106/JBJS.15.00255 [DOI] [PubMed] [Google Scholar]
- 47.Wagner ER, Houdek MT, Schleck CD, Harmsen WS, Sanchez-Sotelo J, Cofield R et al. The role age plays in the outcomes and complications of shoulder arthroplasty. J Shoulder Elbow Surg 2017; 26:1573–80. doi: 10.1016/j.jse.2017.01.020 [DOI] [PubMed] [Google Scholar]
- 48.Walch G, Moraga C, Young A, Castellanos-Rosas J. Results of anatomic nonconstrained prosthesis in primary osteoarthritis with biconcave glenoid. J Shoulder Elbow Surg 2012; 21:1526–33. doi: 10.1016/j.jse.2011.11.030 [DOI] [PubMed] [Google Scholar]
- 49.Wasserstein RL, Lazar NA. The ASA Statement on p-Values: Context, Process, and Purpose. The American Statistician 2016; 70:129–33. doi: 10.1080/00031305.2016.1154108 [DOI] [Google Scholar]
- 50.Wasserstein RL, Schirm AL, Lazar NA. Moving to a World Beyond “p < 0.05”. The American Statistician 2019; 73:1–19. doi: 10.1080/00031305.2019.1583913 [DOI] [Google Scholar]
- 51.Werthel JD, Hatta T, Schoch B, Cofield R, Sperling JW, Elhassan BT. Is previous nonarthroplasty surgery a risk factor for periprosthetic infection in primary shoulder arthroplasty? J Shoulder Elbow Surg 2017; 26:635–40. doi: 10.1016/j.jse.2016.10.020 [DOI] [PubMed] [Google Scholar]
- 52.Westermann RW, Lynch TS, Jones MH, Spindler KP, Messner W, Strnad G et al. Predictors of Hip Pain and Function in Femoroacetabular Impingement: A Prospective Cohort Analysis. Orthop J Sports Med 2017; 5:2325967117726521. doi: 10.1177/2325967117726521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Westermann RW, Pugely AJ, Martin CT, Gao Y, Wolf BR, Hettrich CM. Reverse Shoulder Arthroplasty in the United States: A Comparison of National Volume, Patient Demographics, Complications, and Surgical Indications. The Iowa orthopaedic journal 2015; 35:1–7. No doi [PMC free article] [PubMed] [Google Scholar]
- 54.Wong SE, Colley AK, Pitcher AA, Zhang AL, Ma CB, Feeley BT. Mental health, preoperative disability, and postoperative outcomes in patients undergoing shoulder arthroplasty. J Shoulder Elbow Surg 2018; 27:1580–87. doi: 10.1016/j.jse.2018.02.066 [DOI] [PubMed] [Google Scholar]
- 55.Wong SE, Pitcher AA, Ding DY, Cashman N, Zhang AL, Ma CB et al. The effect of patient gender on outcomes after reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2017; 26:1889–96. doi: 10.1016/j.jse.2017.07.013 [DOI] [PubMed] [Google Scholar]
- 56.Wylie JD, Bershadsky B, Iannotti JP. The effect of medical comorbidity on self-reported shoulder-specific health related quality of life in patients with shoulder disease. J Shoulder Elbow Surg 2010; 19:823–8. doi: 10.1016/j.jse.2009.11.052 [DOI] [PubMed] [Google Scholar]
- 57.Wylie JD, Suter T, Potter MQ, Granger EK, Tashjian RZ. Mental Health Has a Stronger Association with Patient-Reported Shoulder Pain and Function Than Tear Size in Patients with Full-Thickness Rotator Cuff Tears. J Bone Joint Surg Am 2016; 98:251–6. doi: 10.2106/JBJS.O.00444 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Model-fitted differences of means of PENN Shoulder Score (PSS) total, function and pain subscores, and differences of log odds ratios for satisfaction subscore, from nested models including all variables simultaneously. These models estimate separate effects for each variable for Subgroup 1 and pooled Subgroups 2–4 patients, comparisons of which examine disparities in associations between patients with glenohumeral osteoarthritis (Subgroup 1, 99.6%) and with rotator cuff tear arthropathy (Subgroups 2–4, 94.1%). Interaction p-values compare the two estimated parameters and test hypotheses that the effect of each variable is independent of disease subgroup.
Table S2. Estimated effects and odds ratios of six factors considered to be possible causal mediators for preoperative PENN Shoulder Score (PSS) in partial and full models.