Abstract
Anterior shoulder dislocation is the most common joint dislocation, unreducible dislocations however are a rare occurrence. The causes of the irreducibility vary, with interposition of soft tissues or bony fragments within the glenohumeral joint being the usual culprits. We present the case of an irreducible anterior shoulder dislocation with concomitant greater and lesser tuberosity fractures, with interposition of the subscapularis and lesser tuberosity thereby preventing reduction.
We present the case of a 54-year-old female presenting with a left shoulder fracture dislocation after a fall from a 1.8-meter ladder. Patient was taken to the operating room after undergoing a CT scan. Attempts of closed reduction after administration of general anesthesia were unsuccessful. Open reduction and internal fixation with plate and screws was done through a deltopectoral approach. Intra-operatively, the lesser tuberosity and the subscapularis were found to be the cause of the irreducibility of the dislocation. At the latest follow up at 6 months post-op, the patient had regained a normal ROM with a good function.
The vast majority of shoulder fracture dislocations are easily reducible, with only a limited number of case reports discussing irreducible fracture-dislocations. The causes of the irreducibility comprise interposition of soft tissue or bony fragments within the glenohumeral joint such as avulsed labrum or tendons, glenoid or humeral bony fragments interposition, and tensioning of nerves or tendons such as the biceps or subscapularis around the humeral head. CT scans are in our opinion very important for proper surgical planning when needed and for possible identification of an irreducible dislocation.
Orthopedic surgeons should be aware that difficult closed reductions of the glenohumeral joint, whenever encountered, should raise the possibility of interposition of bony fragments or soft tissues where surgical treatment might be mandatory.
Keywords: Shoulder dislocation, Fracture, Subscapularis, Interposition
Introduction
Glenohumeral dislocation accounts for most of joint dislocations (45%) and is a surgical emergency [1]. As most orthopedic injuries, it has a bimodal distribution. High energy trauma accounts for the mechanism of injury in young patients compared to low energy mechanisms in older individuals [2].
An interplay of many factors confer stability to the glenohumeral joint. The glenoid fossa is supported by the glenoid labrum which provides anatomical restraint to the humeral head by deepening the glenoid fossa. Other factors of stability include the rotator cuff, glenohumeral ligaments and other static and dynamic stabilizers [3].
Anterior glenohumeral dislocation can be associated with many concomitant injuries which are important to identify in order to optimize management.
According to Robinson et al., complications of anterior glenohumeral dislocation include neurovascular deficits, rotator cuff injury and fractures of the greater tuberosity. Other associated injuries like Hill-Sachs and Bankart lesions can lead to increased instability [4].
Irreducible shoulder dislocations, even though rare, are reported in the literature. In the described cases, causes of irreducibility include impaction of the humeral head on the glenoid rim, bony interposition in cases of greater tuberosity fractures and Bankart lesions, with the most common causes being due to the soft tissue interposition of interposed labrum, posteriorly dislocated long head of the biceps tendon, or rotator cuff, such as the subscapularis tendon being interposed within the glenohumeral joint [5,6]. There has also been a reported case of an interposed musculocutaneous nerve as the cause of irreducibility [7].
This article reports the case of an irreducible anterior shoulder dislocation with concomitant greater and lesser tuberosity fractures, with interposition of the subscapularis and lesser tuberosity thereby preventing reduction. To our knowledge, no previous mention of this mechanism preventing the reduction of a shoulder joint dislocation has been previously mentioned.
Case presentation
This is the case of a 54-year-old female presenting for trauma to left arm post fall. The patient presented to our emergency department after falling on her left arm from a 1.8-meter ladder. She reported tenderness upon light palpation of affected shoulder with loss of the normal rounded appearance of the shoulder. She presented with a clinically dislocated shoulder, with an abducted and externally rotated left upper extremity. Physical examination revealed an intact neurovascular status with a limited range of motion of the left shoulder.
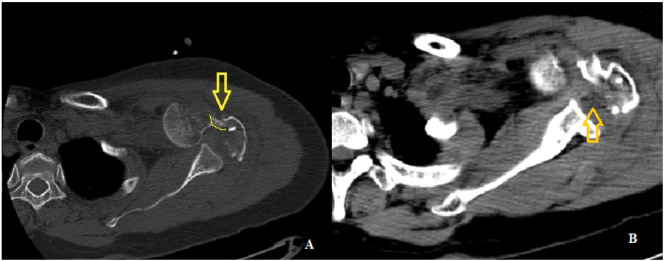
Radiological examination of her left shoulder was done in the emergency department, and showed a left shoulder anterior dislocation with a displaced fracture of the greater and lesser tuberosities [Fig. 1].
Fig. 1.
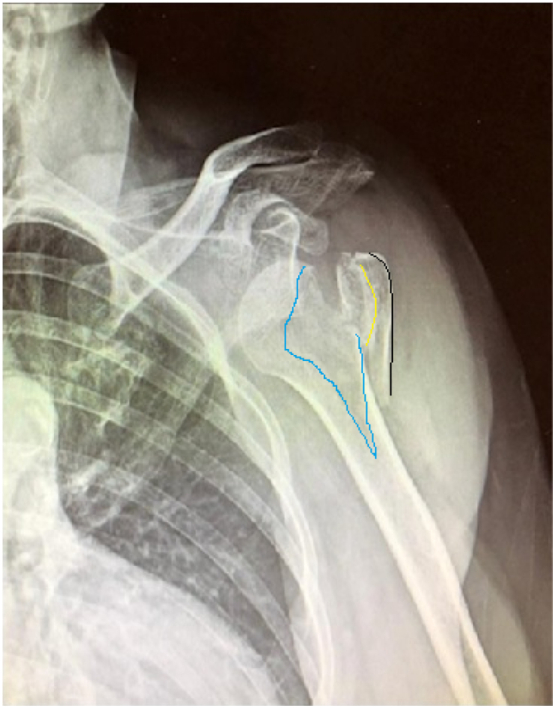
Anteroposterior view of the left shoulder radiograph showing a left shoulder anterior dislocation with a displaced fracture of the greater (black line) and lesser (yellow line) tuberosities with the fracture line on the humeral head delineated in blue. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
A CT scan was ordered for assessment and surgical planning. It confirmed the anterior glenohumeral dislocation, it also showed a humeral neck fracture with a displaced fracture of the greater humeral tuberosity and a comminuted fracture of the lesser tuberosity which was between the glenoid and dislocated humeral head [Fig. 2A]. The interposition of the comminuted lesser tuberosity fracture and of the tensioned subscapularis muscle were the physical impediments to trials of closed reduction. Retrospective post-operative analysis of the CT scan was done by a radiologist using the soft tissue filter image showed interposition of the subscapularis between the lesser tuberosity and the remainder of the humeral head [Fig. 2B].
Fig. 2.
(A) Axial CT scan, bone filter image, showing a displaced fracture of the greater humeral tuberosity, displaced fracture of the lesser humeral tuberosity (yellow line and arrow) impacted and interposed between the humeral head and the fractured fragment. (B) Axial soft tissue CT image of the left shoulder showing the anterior dislocation with acute comminuted displaced fracture of the humeral surgical neck, displaced fracture of the greater tuberosity, acute impacted displaced fracture of the lesser tuberosity and impacted bony fragment of the fractured lesser humeral tuberosity within the glenohumeral joint space with interposition of the torn subscapularis tendon within the glenohumeral joint space (arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Patient was transferred to the operation room for surgical treatment of her condition. Under general anesthesia, trials of closed reduction using the Milch and Cortes techniques were unsuccessful.
The patient was positioned in the beach chair position. After sterile preparation of the surgical field, the shoulder joint was explored using the deltopectoral approach. The humeral head was identified, it was anteriorly dislocated. The displaced greater and lesser tuberosities were also identified, with confirmation of the comminuted lesser tuberosity fracture with the attached subscapularis muscle which were interposed between the humeral head and the greater tuberosity. The subscapularis was seen to be under tension and interposed between the glenoid (fossa) and the dislocated humeral head. The interposed lesser tuberosity and the taught subscapularis were the anatomical restraints to the closed reduction of the shoulder dislocation. After proper manipulation of these structures by manual reduction of the lesser tuberosity and the freeing of the subscapularis, disimpaction of the lesser tuberosity fragment was done followed by successful reduction [Fig. 3].
Fig. 3.
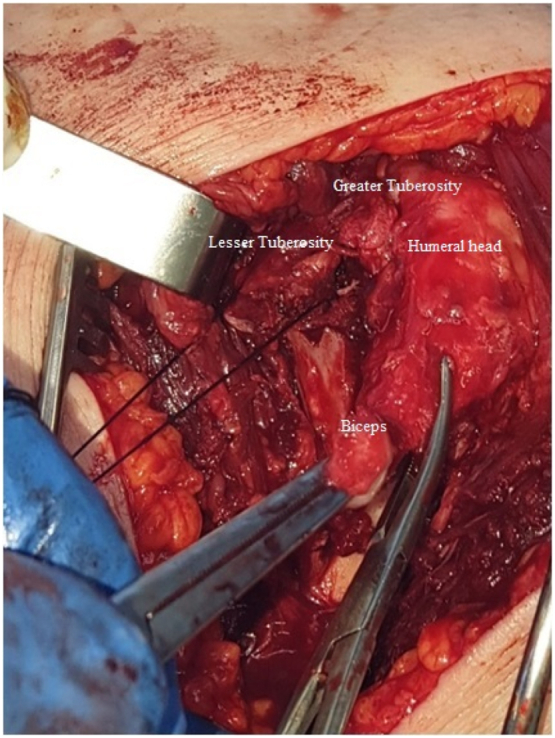
Intra-operative image showing the lesser tuberosity; which is tagged by a suture; as well as the long head of the biceps tendon and the greater tuberosity.
The long head of the biceps tendon (LHBT) was lacerated and a tenotomy was done from the supraglenoid tubercle. A proximal humeral plate was used for fixation of the fractures, the lesser tuberosity was fixated by a cannulated screw, and the LHBT was tenodesed to the plate [Fig. 4].
Fig. 4.

Postoperative radiograph showing the reduced fracture-dislocation which was fixed by a proximal humerus plate, and a cannulated screw holding the lesser tuberosity is also seen.
The shoulder was immobilized for three weeks in a shoulder immobilizer followed by initiation of physiotherapy. Follow-up at one year showed good function and range-of-motion of the shoulder joint with no episodes of subluxation or recurrent dislocation. The ROWE score functional outcome, usually used for shoulder stability assessment after bankart repair, was adopted in this case for pain and motion limitation assessment. At three months post operatively, the score ranged from 55/100 up to 90/100 at one year follow up. Post operative imaging at one year were unavailable due to patient preference during the COVID-19 pandemic to minimize exposure.
Discussion
Shoulder dislocation is a commonly seen presentation, with an incidence of 8 per 100,000 people/year [8]. The vast majority of anterior shoulder fracture dislocations are easily reducible, therefore irreducible shoulder dislocation case reports are not numerous [5,6]. Usually a rotator cuff tear results in patients older than 40, and in younger patients damage to the glenohumeral ligaments, labrum or glenoid occur with subsequent shoulder instability [8].
Failure of closed reduction is a rare event that has been described in the literature. The current literature states the identified causes of the failed closed reduction and these include impaction of the Hill-Sachs lesion into the glenoid, interposition of soft tissues such as a torn subscapularis, labrum (soft tissue Bankart), LHBT, musculocutaneous nerve [[5], [6], [7]]. Bowstringing of the subscapularis, the LHBT, or interposition of bony structures such as the greater tuberosity or a bony Bankart lesion have been described as reasons to impede closed reduction [1,5,6,9]. In rare cases, posterior shoulder fracture dislocations with both greater and lesser tuberosities fractures may lead to infraspinatous interposition impeding closed reduction trials [10].
To our knowledge, there hasn't been any previous report of a concomitant greater and comminuted lesser tuberosities fracture with interposition of the lesser tuberosity and of an intact taught subscapularis between the fracture displaced fragments and the humeral head thereby preventing reduction of the dislocation.
After the presentation of the above case, it is suggested that patients with shoulder fracture dislocations should undergo a CT scan for a better understanding of the fracture pattern and possible prediction of failure of closed reduction if the previously identified causes of irreducibility are identified.
Conclusion
Difficult closed reductions of glenohumeral joint dislocations, whenever encountered, should raise the possibility of interposition of bony fragments or soft tissues where surgical treatment may be mandatory. Orthopedic surgeons should always be attentive of this possibility.
Funding
No funds were received in support of this study.
Declaration of competing interest
All the authors declare no conflict of interest regarding the publication of this article.
Contributor Information
Dany Aouad, Email: Dany_aouad@hotmail.com.
Vladimir Kanj, Email: vmkanj@stgeorgehospital.org.
References
- 1.Khiami F., Gérometta A., Loriaut P. Management of recent first-time anterior shoulder dislocations. Orthop. Traumatol. Surg. Res. 2015;101:51–57. doi: 10.1016/j.otsr.2014.06.027. [DOI] [PubMed] [Google Scholar]
- 2.Cutts S., Prempeh M., Drew S. Anterior shoulder dislocation. Ann. R. Coll. Surg. Engl. 2009;91(1):2–7. doi: 10.1308/003588409x359123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vezeridis P.S., Ishmael C.R., Jones K.J., Petrigliano F.A. Glenohumeral dislocation arthropathy. J. Am. Acad. Orthop. Surg. 2019;27(7):227–235. doi: 10.5435/JAAOS-D-17-00056. [DOI] [PubMed] [Google Scholar]
- 4.Robinson C.M., Shur N., Sharpe T., Ray A., Murray I.R. Injuries associated with traumatic anterior glenohumeral dislocations. J. Bone Joint Surg. 2012;94(1):18–26. doi: 10.2106/JBJS.J.01795. [DOI] [PubMed] [Google Scholar]
- 5.Pantazis K., Panagopoulos A., Tatani I., Daskalopoulos B., Iliopoulos I., Tyllianakis M. Irreducible anterior shoulder dislocation with interposition of the long head of the biceps and greater tuberosity fracture: a case report and review of the literature. Open Orthop. J. 2017;11:327–334. doi: 10.2174/1874325001711010327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Connolly S., Ritchie D., Sinopidis C., Brownson P., Aniq H. Irreducible anterior dislocation of the shoulder due to soft tissue interposition of subscapularis tendon. Skelet. Radiol. 2008;37(1):63–65. doi: 10.1007/s00256-007-0370-y. [DOI] [PubMed] [Google Scholar]
- 7.Gudena R., Iyengar K., Nadkarni J., Loh W. Irreducible shoulder dislocation – a word of caution. Orthop. Traumatol. Surg. Res. 2011;97(4):451–453. doi: 10.1016/j.otsr.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 8.Bayoumy M.A., Said H.G., Abdelkawi A.F., Fetih T.N. Treatment of irreducible traumatic anterior shoulder dislocation caused by subscapularis tendon interposition. Arthrosc. Tech. Jun 2017;6(3) doi: 10.1016/j.eats.2017.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Amroodi Morteza. Irreducible anterior shoulder dislocation associated with displaced fracture of the greater tuberosity: an analysis of seven cases. Shafa Orthop. J. 2015;2 doi: 10.17795/soj-4023. [DOI] [Google Scholar]
- 10.Ogawa K., Ogawa Y., Yoshida A. Posterior fracture-dislocation of the shoulder with infraspinatus interposition: the buttonhole phenomenon. J. Trauma. 1997;43(4):688–691. doi: 10.1097/00005373-199710000-00021. [DOI] [PubMed] [Google Scholar]