Abstract
Objective
Hickman catheter placement rarely causes cardiac tamponade due to cardiac perforation in children. Cardiac perforation can be managed with timely perceive and appropriate approach. We present a case of the cardiac perforation related to Hickman catheter insertion in a 7-year-old girl and a review of the supporting literature.
Case report
The patient had previous history of Thalassemia and admitted to hospital for Hickman catheter placement for bone marrow transplantation. The catheter was placed in the right internal jugular vein by ultrasonography. During the postoperative period she had hypoxia, hypotension and tachycardia. The patient underwent an emergency surgery and there was a small perforation between vena cava superior and right atrium. That wound was managed by mediastinotomy. The patient was discharge on the 8th postoperative day.
Conclusion
Cardiac perforation is one of the rare and unexpected complications of Hickman catheter placement. Unfortunately, the complication may cause significant mortality. The prompt diagnosis and early intervention provides satisfactory results.
Keywords: Cardiac perforation, Hickman catheter, Insertion, Complication, Cardiac tamponed
Introduction
The Hickman catheter (HC) affords many advantages, including application of intense therapy via lumina of different diameters if medications are incompatible and infusion of large fluid volumes. HCs are often inserted via the jugular or subclavian veins of pediatric patients [[1], [2], [3]]. However, HCs may be associated with various complications, one of which is cardiac tamponade (CT)-related cardiac perforation (CP) [4]. Complications associated with HC insertion are similar to those associated with other central catheters and include arterial puncture, CP, hemo-/pneumothorax, thrombosis, and infections [5]. The mechanical complication such as; vascular issues and CP are the most serious life-threatening complications after central venous catheter insertion [6].
Findings indicative of problems with HC insertion include pulsus paradoxus, hypotension, tachycardia, and/or severe dyspnea. The goals of treatment are to restore the hemodynamic balance, drain any pericardial effusion, prevent complications, and improve the hemodynamics. The treatment options are limited and frequently unsuccessful. In the absence of prompt treatment, CP may cause cardiogenic shock, cardiac arrest, or death.
Here, we describe a case of HC insertion that triggered acute-onset CT caused by CP.
Case report
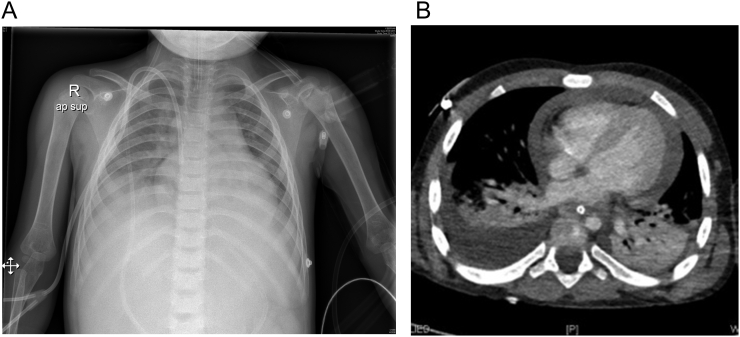
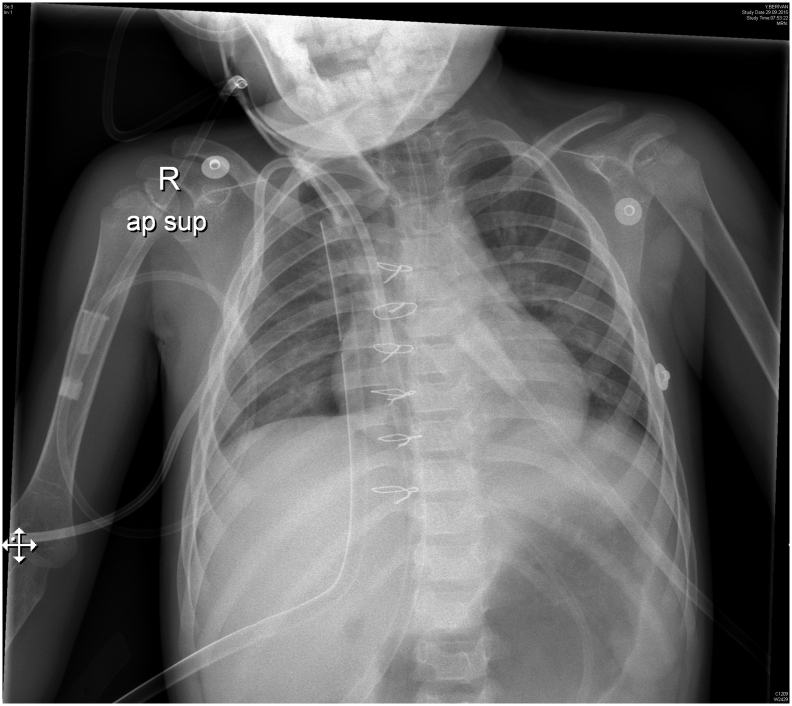
A 7-year-old girl required percutaneous HC insertion after bone marrow transplantation. She had a medical history of thalassemia. The procedure was performed under general anesthesia employing guided ultrasonography (USG). After puncture of the right vena jugularis interna, a J guidewire was placed feasibly, followed by a pleural sheet and 9-Fr catheter. After recovering from surgery, she was hemodynamically stable and was transferred to the clinic for postoperative follow-up. Soon thereafter, the patient then became hypotensive and developed dyspnea and tachycardia 4 h after HC insertion. There was no bleeding. Blood analysis showed a no decrease in the Hb level (to 8 g/dL) and increasing leukocytosis (leukocyte count, 27,000/mL). Blood gas analysis revealed low oxygen saturation, increased CO2 pressure, and acidosis. The symptoms progressed. On a chest X-ray, the catheter tip was observed within the heart, and the cardiac silhouette was enlarged and exhibited massive bilateral pleural effusion (Fig. 1a). Thorax and abdominal USG revealed massive pulmonary effusion and free fluid in the abdomen. Echocardiography revealed a large amount of pericardial effusion. Computed tomography revealed massive bilateral pleural effusion and massive amounts of free fluid in the abdomen (Fig. 1b). We considered the possibility that a cardiac or large-vessel perforation had caused CT. Red blood cells and fluid were infused. The patient was rushed to the theater, and sternotomy was performed via a midline incision approximately 8 h after HC insertion. Approximately 600 mL hemorrhagic fluid were distributed diffusely around the heart and inside the pericardial recesses; a 0.5-cm-diameter perforation lying between the right atrium and vena cava superior was closed, a drain placed in the pericardial area, and the HC removed percutaneously. On postoperative day 2, the pericardial drain was removed (Fig. 2). On postoperative day 8, she was discharged without any complications.
Fig. 1.
a Chest X-rays. A. The course of the central venous catheter commencing at the right jugular insertion site. The widening silhouette in the cardiac area. b Representative computed tomography images showing CT after HC insertion.
Fig. 2.
A chest X-ray taken after repair of the atrial wall.
Discussion
We searched the literature using the PubMed MEDLINE database. We searched titles and abstracts using a combination of the terms “cardiac perforation”, “central venous catheter”, and “children”. No data limit was imposed. We evaluated papers on 20 cases, including our case, published in the English language. Most of these reports referred to neonates (most of whom were of low birth weight, female, and premature) [7] and infants treated in pediatric intensive care units [8]. Patients with chronic diseases, and newborns, are more likely to have weak myocardial muscles and are therefore at a higher risk of perforation [5]. Our patient had thalassemia, and had received many blood transfusions. Most cases were diagnosed postmortem, and all had catheter tips within the cardiac silhouettes. CT had developed late after catheter insertion; some patients survived after pericardiocentesis or mediastinotomy. When we included guidewires in our search, all three reports referred to adults [5,14]. We excluded adult cardiac perforations caused by catheters (Table 1) [3,7,10,13,[18], [19], [20], [21], [22]]. This is the first reported case of CP caused by the J-tipped guidewire of an HC in a patient with thalassemia. In a previous study, HC insertion caused rapid CT in an adult who died [9]. We followed our patient closely, and early diagnosis allowed rescue.
Table 1.
Clinical characteristics of the present case and literature cases featuring cardiac perforations in children.
| How many case Reference | Site of perforation | Initial route | Liquid (cc) | Clinical signs | Time since catheterization | Course | Treatment | Age | Gender | Cause |
|---|---|---|---|---|---|---|---|---|---|---|
| 3 cases [11] | - RA RA |
RSV RFV LSV |
30 - 95 |
Non Dyspnea Sweating |
8 h 24 h 7 day |
Died Died Died |
Unknown | 14-day old Premature 3-year old |
Girl Girl Girl |
Tip Tip Tip |
| 2Cases [22] | RA | RSV | Unknown | Sudden | 2, 4 day | Death | Pericadrdiocentesis | Neonate | Girl | Tip |
| 1 case [21] | RA | Survived | 2-day-old | Tip | ||||||
| 5 cases [7] | PICC | Sudden | 1,2,6,7 day | Survived | Percutaneous Aspiration | 24,24,30,33 | Girl | Tip | ||
| 2 cases [20] | Unknown Unknown |
FV Unknown |
Unknown Unknown |
Shock Sudden |
12 h 3 day |
Survived Death |
Aspiration Mediastnomy |
4-year-old 12-day-old |
Unknown | Tip |
| 2 cases [3] | VCI RA |
RIJV RSV |
Large TPN |
Sudden | 5 day 5 day |
Death Death |
- - |
25-day-old 4-year-old |
Boy Boy |
Tip |
| 1 case [10] | RV | RIJV | large | Apnea | 12 h | Death | Mediastnomy and aspiration | 12-year-old | Girl | Tip |
| 1 case [13] | Unknown | R SaV | 23 ml | Tachypnea | 12 day | Survived | Perikardiosentesis | Premature | Girl | Tip |
| 3 cases [15] | RV | PICC | 8 ml 20 ml |
Apnea - |
15 day 5 day |
Death Survived | -CVC removed - |
Premature | Boy boy |
Tip |
| 11cases18 | Unknown | Death | – | Infant | Unknown | Tip | ||||
| Our case | RA | RIJV | 600 ml | Dyspnea | 4 h | Survived | Mediastinomy cardioraphy | 7 year-old | Girl | Guide-wire |
RA: Right atrium, RV; Right Ventricule, VCI: Vena Cava Inferior, RSV; Right Subclvian Ven, RFV; Right Femoreal Ven, LSV; Left Subclavian Ven, RIJV; Right Interneal Jugular Ven, RSaV; Right sapheneous Ven, PICC; Peripherally inserted central catheter.
Complications associated with the use of HCs are early or late is a serious but rare complication [8,10]. Complications can be divided into those that develop early (<24 h after HC insertion; hemothorax, pneumothorax, catheter malpositioning, and CP) and those that develop late (>24 h after insertion; sepsis and thrombosis) [10,11]. Early complications are usually mechanical in nature and more serious than late complications [10,11]. The complication rate associated with central catheter insertion in children is 2.4–4.6% [1]. The CT incidence is quite variable, ranging from 0.0001 to 1.4% [2,[10], [11], [12]]. CT constitutes approximately 5% of all mechanical complications [4,17]. Mortality caused by CT also varies (30–100%) [3,10,11,13]. Diagnosis is usually not determined until postmortem [13]. We inserted more than 500 HCs over a 5-year period and encountered only this single CT incident. The time from central catheter insertion to CT ranges from hours to days [8]. In our present case, signs of iatrogenic CT developed 4 h after HC insertion. Rapid diagnosis and treatment are essential. Other patients developed symptoms between 8 h and 15 days after HC insertion [ 3,7,10,13,[18], [19], [20], [21], [22]].
Catheter insertion aided by fluoroscopy and USG has improved child safety; these guidance modalities are now the recognized standard of care. We insert HCs employing USG guidance in patients under general anesthesia.
CP caused by CT may be affected by the time of catheter insertion, movement of the catheter tip, angle of insertion, movement of the cardiac chambers, and direct trauma [5]. CP associated with central catheter placement features puncture of the cardiac wall, superior vena cava, or inferior vena cava by the guidewire, dilator, or catheter per se [ 2,6,11,14,20]. In our present case, the wound was located in the right atrium, as in many other cases. All venous insertions feature a risk of CP. J-tipped guidewires are safe and rarely cause complications such as CP [5]. The J-tip is blunt; no sharp guidewire tip can contact or perforate any structure during travel [5]. Usually, CT is associated with the placement procedure per se11 and may develop immediately after catheter insertion or after several days depending on the rate of fluid accumulation [3]. In our present case, the diameter of the right atrial perforation was approximately 5 mm. We did not force the dilator; we therefore suspect that the guidewire caused the perforation. Late CT complications associated with accumulation of hyperosmolar fluid include osmotic injury, shallow breathing, catheter displacement to the myocardial wall, erosion, thrombosis causing transmural necrosis, and local inflammation [3,7,8,13,20]. Polyethylene catheters are more rigid than silicone catheters and thus more likely to cause CP. Serious/fatal complications may occur despite careful placement and follow-up [15].
A small amount of fluid is present in the pericardial sac (between the smooth-surfaced viscera and parietal pericardial layer) to facilitate heart lubrication [16]. If that fluid accumulates (either slowly or rapidly), CT may follow. Any pressure increase in the pericardium and/or thoracic cavity may affect the cardiac chambers [16]. As the pressure within the pericardium increases, the central vascular pressure increases because of the resistance imparted by the pressure associated with right atrial filling. Thus, blood returning from the veins fills the right heart chambers with difficulty, triggering cardiogenic shock and death [12,16].
CP symptoms and signs are nonspecific and various. CP onset may be sudden or progressive, and CT may develop at various times after catheter insertion [17]. The symptoms include nausea, dyspnea, chest pain, tachypnea, hemodynamic instability, and confusion [16,20]. The objective findings include hypotension, tachycardia, soft heart sounds that vary in intensity with respiration, venous engorgement, pulsus paradoxus, and shock [20]. The presentation of Beck and classic triad-related acute CT features hypotension, increased vascular pressure, and muffled heart sounds [12,16]. The present and other patients lacking symptoms or dyspnea suddenly entered crises.
CP is survivable if detected early and treated promptly [4]. Electrocardiography (both direct and Doppler) facilitates rapid CP diagnosis, assessment of the presence, volume, and distribution of pericardial fluid, and evaluation of intrapericardial tissue [12,16]. However, diagnosis is not always obtained by electrocardiography. Chest X-ray has been used to locate the catheter and pleural effusion, but it may not reveal any abnormality until considerable fluid has accumulated in the pericardial sac [12]. Computed tomography and magnetic resonance imaging can detect the presence of pericardial fluid and may afford some insight into the causative pathology.
Treatment is influenced by multiple factors such as the lesion size, hemodynamic effect, and etiology [16]. A small traumatic ventricular septum may close spontaneously, but an atrial defect may not [6]. Because our patient had an atrial defect, we scheduled surgery. CP should be surgically treated immediately after diagnosis, as cardiac lesions are fatal [18].
CT temporarily protects against massive volume loss, affording a window for diagnosis and surgical intervention [18]. Once a diagnosis has been made, prompt treatment is required. The catheter should be removed. Pericardiocentesis and drain placement may be performed in an emergency [4,12]. After catheter withdrawal, failure to improve necessitates pericardiocentesis followed by mediastinotomy or thoracotomy, pericardiotomy, and a cardiac procedure [8,19]. In our case, we did not know the side of perforation, and the condition of our patient worsened after accumulation of intra-abdominal, intrathoracic, and intrapericardial fluid. She therefore underwent mediastinotomy to identify the site of trauma.
In conclusion, CP associated with HC placement is rare, serious, and associated with high mortality, and it can occur any time after insertion. Strategies should be formulated to avoid the risk of CP. If CP is suspected, close follow-up and early treatment are essential. The guidewire should not be forced, and fluoroscopic guidance should be employed in cases of doubt.
References
- 1.Christensen L.D., Holst M., Bech L.F. Comparison of complications associated with peripherally inserted central catheters and HickmanTM catheters in patients with intestinal failure receiving home parenteral nutrition. Six-year follow up study. Clin. Nutr. 2016;35(4):912–917. doi: 10.1016/j.clnu.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 2.Butt M.U., Gurley J.C., Bailey A.L., Elayi C.S. Pericardial tamponade caused by perforation of Marshall vein during left jugular central venous catheterization. Am J Case Rep. 2018;19:932–934. doi: 10.12659/AJCR.909005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.dos Santos Modelli M.E., Cavalcanti F.B. Fatal cardiac tamponade associated with central venous catheter: a report of 2 cases diagnosed in autopsy. Am J Forensic Med Pathol. 2014;35(1):26–28. doi: 10.1097/PAF.0000000000000084. [DOI] [PubMed] [Google Scholar]
- 4.Kayashima K. Factors affecting survival in pediatric cardiac tamponade caused by central venous catheters. J. Anesth. 2015;29(6):944–952. doi: 10.1007/s00540-015-2045-5. [DOI] [PubMed] [Google Scholar]
- 5.Dwivedi S., Siddiqui F., Patel M., Cardozo S. Guide wire induced cardiac tamponade: the soft J tip is not so benign. Case Rep Crit Care. 2016;2016:1436924. doi: 10.1155/2016/1436924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Premuzic V., Katalinic L., Pasalic M., Jurin H. Nonfatal cardiac perforation after central venous catheter insertion. Saudi J Anaesth. 2018;12(1):118–120. doi: 10.4103/sja.SJA_365_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sertic A.J., Connolly B.L., Temple M.J., Parra D.A., Amaral J.G., Lee K.S. Perforations associated with peripherally inserted central catheters in a neonatal population. Pediatr Radiol. 2018;48(1):109–119. doi: 10.1007/s00247-017-3983-x. [DOI] [PubMed] [Google Scholar]
- 8.Barreiros L.L., Andrade F.M., Torres R.A. Cardiac tamponade by peripherally inserted central catheter in preterm infants: role of bedside ultrasonography and therapeutic approach. Rev Col Bras Cir. 2018;45(3) doi: 10.1590/0100-6991e-20181818. [DOI] [PubMed] [Google Scholar]
- 9.Murray B.H., Cohle S.D., Davison P. Pericardial tamponade and death from Hickman catheter perforation. Am. Surg. 1996;62(12):994–997. [PubMed] [Google Scholar]
- 10.Towbin R. The bowed catheter sign: a risk for pericardial tamponade. Pediatr. Radiol. 2008;38(3):331–335. doi: 10.1007/s00247-007-0674-z. [DOI] [PubMed] [Google Scholar]
- 11.Shamir M.Y., Bruce L.J. Central venous catheter-induced cardiac tamponade: a preventable complication. Anesth. Analg. 2011;112(6):1280–1282. doi: 10.1213/ANE.0b013e318214b544. [DOI] [PubMed] [Google Scholar]
- 12.Forauer A.R. Pericardial tamponade in patients with central venous catheters. J. Infus. Nurs. 2007;30(3):161–167. doi: 10.1097/01.NAN.0000270675.21063.f3. [DOI] [PubMed] [Google Scholar]
- 13.Cade A., Puntis J.W. Pericardial parenteral nutrition infusion following acute angulation of a neonatal polyurethane central venous catheter tip. Clin. Nutr. 1997;16(5):263–264. doi: 10.1016/s0261-5614(97)80039-8. [DOI] [PubMed] [Google Scholar]
- 14.Hiroshima Y., Tajima K., Shiono Y., Suzuki I., Kohno K., Kato Y., Shunji K., Kato T. Soft J-tipped guide wire-induced cardiac perforation in a patient with right ventricular lipomatosis and wall thinning. Intern. Med. 2012;51(18):2609–2612. doi: 10.2169/internalmedicine.51.7794. [DOI] [PubMed] [Google Scholar]
- 15.Leipälä J.A., Petäjä J., Fellman V. Perforation complications of percutaneous central venous catheters in very low birth weight infants. J. Paediatr. Child Health. 2001;37(2):168–171. doi: 10.1046/j.1440-1754.2001.00625.x. [DOI] [PubMed] [Google Scholar]
- 16.Appleton C., Gillam L., Koulogiannis K. Cardiac tamponade. Cardiol. Clin. 2017;35(4):525–537. doi: 10.1016/j.ccl.2017.07.006. [DOI] [PubMed] [Google Scholar]
- 17.Chabanier A., Dany F., Brutus P., Vergnoux H. Iatrogenic cardiac tamponade after central venous catheter. Clin. Cardiol. 1988;11(2):91–99. doi: 10.1002/clc.4960110207. [DOI] [PubMed] [Google Scholar]
- 18.Collier P.E., Goodman G.B. Cardiac tamponade caused by central venous catheter perforation of the heart: a preventable complication. J. Am. Coll. Surg. 1995;181(5):459–463. [PubMed] [Google Scholar]
- 19.Darling J.C., Newell S.J., Mohamdee O., Uzun O., Cullinane C.J., Dear P.R. Central venous catheter tip in the right atrium: a risk factor for neonatal cardiac tamponade. J. Perinatol. 2001;21(7):461–464. doi: 10.1038/sj.jp.7210541. [DOI] [PubMed] [Google Scholar]
- 20.Yoder D. Cardiac perforation and tamponade: the deadly duo of central venous catheters. Int J Trauma Nurs. 2001;7(3):108–112. doi: 10.1067/mtn.2001.117434. [DOI] [PubMed] [Google Scholar]
- 21.Agarwal K.C., Khan M.A., Falla A., Amato J.J. Cardiac perforation from central venous catheters: survival after cardiac tamponade in an infant. Pediatrics. 1984;73(3):333–338. [PubMed] [Google Scholar]
- 22.Bar-Joseph G., Galvis A.G. Perforation of the heart by central venous catheters in infants: guidelines to diagnosis and management. J. Pediatr. Surg. 1983;18(3):284–287. doi: 10.1016/s0022-3468(83)80103-1. [DOI] [PubMed] [Google Scholar]