Abstract
Background
Understanding adverse events among children treated in the emergency department (ED) offers an opportunity to improve patient safety by providing evidence of where to focus efforts in a resource-restricted environment.
Objective
To estimate the risk of adverse events, their type, preventability and severity, for children seen in a paediatric ED.
Methods
This prospective cohort study examined outcomes of patients presenting to a paediatric ED over a 1-year period. The primary outcome was the proportion of patients with an adverse event (harm to patient related to healthcare received) related to ED care within 3 weeks of their visit. We conducted structured telephone interviews with all patients and families over a 3-week period following their visit to identify flagged outcomes (such as repeat ED visits, worsening symptoms) and screened admitted patients’ health records with a validated trigger tool. For patients with flagged outcomes or triggers, three ED physicians independently determined whether an adverse event occurred.
Results
Of 1567 eligible patients, 1367 (87.2%) were enrolled and 1319 (96.5%) reached in follow-up. Median patient age was 4.34 years (IQR 1.5 to 10.57 years) and most (n=1281; 93.7%) were discharged. Among those with follow-up, 33 (2.5%, 95% CI 1.8% to 3.5%) suffered an adverse event related to ED care. None experienced more than one event. Twenty-nine adverse events (87.9%, 95% CI 72.7% to 95.2%) were deemed preventable. The most common types of adverse events (not mutually exclusive) were management issues (51.5%), diagnostic issues (45.5%) and suboptimal follow-up (15.2%).
Conclusion
One in 40 children suffered adverse events related to ED care. A high proportion of events were preventable. Management and diagnostic issues warrant further study.
Keywords: adverse events, epidemiology and detection; emergency department; paediatrics
Introduction
The emergency department (ED) is inherently a high-risk environment—large volumes of patients arrive outside of daytime hours, many with undifferentiated or high acuity conditions, to a work environment characterised by frequent interruptions.1–5 Providing medical care to children also has unique challenges. Children require weight-based medication dosing; they may be unable to adequately communicate complaints; and their physical and developmental characteristics affect diagnosis, treatment strategies, procedures and medication regimens.6 7 Given the challenges in providing clinical care in the ED setting and the inherent vulnerability of children, children treated in the ED are potentially a high-risk population from a patient safety perspective.
The majority of patient safety research has focused on hospitalised adult patients. We know that hospitalised children are at high risk for suffering adverse events.8 9 Adverse events are broadly defined as unintended harm to the patient that is related to healthcare provided to the patient rather than the patient’s underlying medical condition.10 Canadian children, however, are more likely to visit an ED, than be admitted to hospital.11 Yet we do not know how commonly children treated in the ED suffer adverse events related to the care provided to them in the ED.
The aim of our study was to generate an estimate of the risk and type of adverse events, as well as their preventability and severity, for all children seen in a paediatric ED and to explore patient characteristics and system factors associated with adverse events. Understanding adverse events among children treated in the ED offers an opportunity to improve patient safety by providing evidence of where to focus efforts in a resource-restricted environment.
Methods
Study design, setting and participants
This prospective cohort study enrolled patients who presented to the CHEO ED over a 1-year period from October 2012 to September 2013. CHEO is a free-standing, tertiary care, paediatric hospital located in Ottawa, Canada, with an annual ED census of 70 000 visits. The CHEO Research Ethics Board approved this study.
Patients less than 18 years of age presenting for care during 1 of 28 study shifts were eligible. Patients were excluded if a significant language barrier prevented informed consent or they were unavailable for telephone follow-up in the 3 weeks following their ED visit.
Sampling strategy
Patient presentations to the ED may vary by time of day, day of week and time of the year. Studies have suggested patients may have worse outcomes when presenting ‘outside of regular hours’.12–14 We used a stratified cluster random sampling scheme to ensure shift distribution in proportion to our institution’s historical distribution of ED visits. We chose independent random samples from three time strata (08:00–15:59 hours, 16:00–23:59 hours and 00:00–07:59 hours), used a ratio of 4:4:1 for day : evening : night shifts and sampled across all days of the week.
Overview of data collection procedures in the ED
Research assistants (RAs) approached patients, assessed eligibility, obtained written informed consent and collected study data. RAs interviewed families and patients to obtain demographics, previous medical history and current medication usage. Data regarding presenting complaint, the Pediatric Canadian Triage Acuity Score (a triage acuity scale where 1=resuscitation, 2=emergent, 3=urgent, 4=semiurgent and 5=non-urgent),15 vital signs, disposition, and discharge diagnosis were collected through ED record review. RAs prospectively recorded the ED census as well as numbers of patients waiting to be seen and awaiting inpatient beds every hour. We selected these as our measures of ED crowding16–18 as there is no validated dichotomous measure of crowding for the paediatric ED. Other systems factors (online supplementary material 1) were collected through ED record review.
bmjqs-2019-010055supp001.pdf (447.7KB, pdf)
Outcomes
The primary outcome was the proportion of enrolled patients who experienced an adverse event related to ED care provided at the enrolment ED visit within 3 weeks of their ED visit. We defined an adverse event as any event that resulted in unintended harm to the patient and was related to the healthcare provided to the patient rather than to the patient’s underlying medical condition.10 We included harm related to acts of omission (eg, failure to diagnose or treat) and commission (eg, incorrect treatment) and considered the actions of individual hospital staff as well as the broader systems and care processes.8 19–21 We chose to take a broad patient-centred approach to the definition of harm as advocated by the Institute for Healthcare Improvement22 and did not require an intervention as part of the definition of an adverse event. ED care was defined as any care provided in the ED by its staff (such as ED physicians, nurses or allied health providers) or consulting specialty services (eg, surgical consultants or subspecialty medical consultants).3 4 Adults treated in the ED suffer the majority of ED care-related adverse events within 72 hours of their ED visit, 85% by 2 weeks and the remainder by 3 weeks;4 thus, we selected 3 weeks as the time frame for our primary outcome.
Secondary outcomes included the proportion of patients experiencing a preventable adverse event (defined as an avoidable adverse event based on currently available knowledge and accepted practices), the proportion of patients for whom an adverse event was related to ED provider care versus specialty service care provided in the ED, the types (online supplementary material 2) and clinical severity of adverse events and the system response required. For clinical severity, we used a previously published schema for outpatient adverse event studies and categorised as (1) abnormality on laboratory testing, (2) ≤1 day of symptoms, (3) >1 day of symptoms, (4) non-permanent disability, (5) permanent disability and (6) death.3 4 20 Non-permanent disability was defined as temporary impairment of function likely to last <3 months. Permanent disability was defined as a permanent impairment of function. For the system response required, we used previously published broad categories to address the effect of the adverse event at both the patient and healthcare system levels (online supplementary material 2).3 4 23 Box 1 provides examples of adverse events, their preventability, severity and system response required.
Box 1. Examples of adverse events (AEs) and a flagged outcome deemed not to be an AE.
Medication adverse effect (not preventable): A 4-year-old girl presents with dysuria and frequency of 2 days. Urinalysis is positive for nitrites, leucocytes and red blood cells. Diagnosed with a urinary tract infection and started on oral cephalexin. Develops an itchy, urticarial rash after 2 days for which she visits her primary care provider. Rash resolves in a further 2 days with discontinuation of the antibiotics.
AE severity:>1 day of symptoms.
System response: Physician visit.
Responsible service: Emergency department (ED) services.
Diagnostic and management adverse event (preventable): A 12-year-old boy falls on outstretched arm. He is tender over the scaphoid on examination. Radiograph is read by the treating ED physician as normal. Child is discharged home with only pain medications. Radiograph is read by radiologist as showing a scaphoid fracture the next day. Child returns to the ED less than 24 hours after initial visit and has a thumb spica cast placed.
AE severity: ≤1 day of symptoms.
System response: Repeat ED visit.
Responsible service: ED services (diagnostic AE due to missing fracture on radiograph and management AE as physical examination would suggest need for thumb spica cast/splint not withstanding presumed negative radiograph).
Unsafe disposition decision and management adverse event (preventable): A 7-year-old child with history of asthma presents with moderate respiratory distress, inspiratory and expiratory wheezing, and oxygen saturation of 90% on room air, and paediatric respiratory asthma measure score of eight. Treated by metered dose inhaler with salbutamol and ipratropium bromide (three treatments in 1 hour) and oral dexamethasone. Discharged home 60 min after completing beta‐agonist treatment. No reassessment examination documented. Child returns to the ED 2 hours after discharge in marked respiratory distress requiring resuscitation room care. Admitted to hospital.
AE severity: ≤1 day of symptoms.
System response: Repeat ED visit and admission to hospital.
Responsible service: ED services (unsafe disposition decision given no reassessment examination documented, management AE based on discharge 1 hour after arrival in moderate respiratory distress).
Procedural complication (not preventable): A 1-year-old child presents with worsening cellulitis of left leg despite 4 days of adequate dose outpatient antibiotics. An intravenous is placed for intravenous antibiotics in left hand and admission to hospital planned. Good blood flow from intravenous after placement, intravenous is well secured and child’s arm is placed on an arm board. One hour after intravenous placement, intravenous pump rings as occluded and left hand is noted to be puffy and slightly tender on palpation, and intravenous is found to be interstitial. Intravenous is removed. Puffy hand/tenderness resolve within 2 hours.
AE severity:≤1 day of symptoms.
System response: Symptoms only.
Responsible service: ED services.
Suboptimal follow-up (preventable): A 15-year-old boy presents with 2-week history of diarrhoea, now bloody for last 3 days. History of 1 kg weight loss. Family history of Crohn’s disease, no travel history. Examination including vitals is normal. Complete blood count shows haemoglobin of 95 g/L with normocytic pattern and erythrocyte sedation rate is reported as 50. Child is discharged with follow‐up to gastroenterology service in 48 hours. Child returns to the ED 7 days later with increasing bloody diarrhoea, tachycardia, dizziness and a further 2 kg of weight loss and has not been seen by gastroenterology service. Admitted to the hospital for management of presumed inflammatory bowel disease presentation.
Example of flagged outcome deemed to not be AEs
Progression of disease: A 1-year-old child presents to the ED with 2-day history of fever and no other symptoms. Child looks well on examination, has no abnormal findings on examination and a urinalysis is normal. Parents are counselled to have child re‐examined if still febrile in 48 to 72 hours and advised on antipyretic medication dosing. Child returns 3 days later to the ED with ongoing fever and new onset of diffuse rash, red sclera, swollen hands and feet, and red lips. Child is diagnosed with Kawasaki’s syndrome and admitted to hospital for immunoglobulin treatment.
Outcome assessment
We followed an established two-step outcome assessment modelled on the seminal Harvard Practice Study and other studies that sought to measure adverse events.3 4 8 19–21
Step 1: Identifying patients at risk of adverse events
In the first step, we identified patients with flagged outcomes or triggers (which are events that may be associated with adverse events). For all patients, a research nurse administered a structured telephone interview (online supplementary material 3) modified from that used in other ED-based adverse event studies3 4 on day 7, 14 and 21 following enrolment to identify flagged outcomes. Children with any of the following were deemed to have flagged outcomes: new or worsening symptoms, exacerbation of a chronic underlying illness, an unscheduled visit to ED or health professional or an unscheduled admission to hospital or death. For children with mental health presentations, flagged outcomes also included subsequent harm to self or others, involvement of police for mental health concerns or calls to mental health crisis lines. As patients and families may identify patient safety concerns not identified in the hospital record,23 24 we also explicitly asked for concerns regarding medication problems, complications of care, miscommunications between staff or between staff and patient/family, equipment problems or other issues of perceived harm during their ED enrolment visit. If described, we considered these flagged outcomes.
To ensure that hospitalisation and deaths were not missed among patients who did not complete all three telephone follow-up calls, we undertook the following process. For patients who were reached by phone at day 7 and/or day 14 but who did not complete the 21-day telephone follow-up, an RA reviewed their hospital record for ED visits or admissions between the date of last telephone contact and 21 days after enrolment. For patients lost to all telephone follow-up, the hospital record was reviewed 6 months after enrolment for any subsequent hospital visits and admissions; if no hospital visit or admission was identified within the 6-month time frame, the provincial coroner’s database was reviewed to ensure the patient had not died. Any patient found to have an ED visit, hospital admission or death within the 3 weeks of the study period was considered to have a flagged outcome.
To identify triggers among patients admitted to hospital at their enrolment visit, a review of the hospital admission was completed by a research nurse using the validated 35-item Canadian Paediatric Trigger Tool (CPTT).25 Triggers include, but are not limited to, blood transfusions, transfer to a higher care level, unplanned surgery or death. The research nurse received detailed training on chart abstraction and the CPTT, with dual, independent review of 30 charts by the research nurse and principal investigator (ACP), followed by discussion and exploration of discrepancies.
Any patient with a flagged outcome or trigger had a narrative case summary created by a trained research nurse. As part of narrative summary creation, the research nurse undertook a structured review of the patient’s entire hospital record during the 3 weeks of the study period, including a review of the enrolment ED visit, any subsequent ED visits or visits to other hospital-based subspecialists, and any hospital admissions. The research nurse then used data collected both on telephone follow-up and on hospital record review to create the summary. These summaries, created to reduce the risk of handwriting recognition by physician reviewers in step 2, summarised patient demographics, the ED enrolment visit, details about the flagged outcomes/triggers (such as description of symptoms, timing of and description of subsequent visits to healthcare provider and the ED) and any hospital admissions. The summary did not include information that identified patients or treating physicians. Training of the research nurse include a detailed review of the protocol, definitions and relevant examples, followed by review and feedback for a 10% sample of all cases by the principal investigator (ACP). The oversight process ensured important clinical details were not missed.
Step 2: Determining occurrence of adverse events
Three ED physicians received comprehensive training in adverse event determination. This training was facilitated by the senior author (LAC), an experienced patient safety researcher. Training included a didactic lecture including review of the definition of adverse events, followed by interactive discussion of sample summaries, as well as independent review of sample summaries followed by interactive group discussions. After completion of training, the three ED physicians independently reviewed each case summary. Previous research demonstrates using multiple reviews reduces uncertainty in adverse event determination.26 27 Using a structured outcome assessment form, the reviewers rated their level of certainty that the outcome was associated with healthcare management on a six-point Likert scale (online supplementary material 4) used in previous studies.4 19 20 If two reviewers had a level of certainty of four (management causation greater than 50:50 chance, but close call) or greater, the outcome was classified as an adverse event. If reviewers needed further information to make an outcome determination, this was made available. For example, the reviewer could examine the ED record or discharge summary (with patient and treating physician identifying details removed). To not under-report adverse events, if one reviewer scored the outcome as at least a five (strong evidence for management causation) and the other reviewers scored as three (management causation less than 50:50 but close call) or less, the reviewers discussed the case and then independently rescored the outcome. For all identified adverse events, one reviewer determined whether they were preventable using a four-point Likert scale (online supplementary material 4) as well the adverse event type(s), the severity and system response. A score of three (probably preventable) or higher was considered a preventable adverse event.
Sample size
An adult ED study using similar methodology documented ED care-related adverse events among 5% of high acuity patients.4 Hospitalised paediatric patients have reported an adverse event occurrence of up to 9.6%.8 We aimed to detect a proportion of patients with adverse event of 7%. To achieve a 2% margin of error surrounding our estimate and assuming a 25% loss to follow-up rate, a minimum sample size of 835 patients was needed. Given our ED census and sampling strategy, we determined 28 8-hour study shifts were needed to meet our recruitment target.
Data analysis
We used descriptive statistics to summarise the baseline demographic and clinical characteristics of all patients enrolled in the study. Enrolled patients for whom follow-up data were available were included in the analysis of the primary and secondary outcomes. The primary analysis estimated the proportion of children with adverse events related to ED care together with 95% CIs. As we oversampled night shifts in an effort to capture more night shift patients who may be under-represented by virtue of the natural pattern of ED traffic, we used a logistic regression model to adjust all analyses by study shift (day, evening, night). The proportion of children with preventable adverse events was similarly determined. We explored the association of patient characteristics and systems factors (online supplementary material 1) with adverse events using univariate logistic regression. Associations involving continuous variables were examined for evidence of non-linearity using the Loess smoother and, if necessary, quadratic terms were included. We ran shift-adjusted univariate logistic regression analyses using Firth’s penalised likelihood for outcomes with low prevalence.28 Factors associated with adverse events (p<0.10) in univariate analysis were included in multiple logistic regression analyses using Firth’s penalised likelihood, adjusting for study shift. We did not impute missing data and undertook complete case analysis. All analyses were conducted using IBM SPSS Statistics 25 and R V.3.0.2.
Results
Patient recruitment
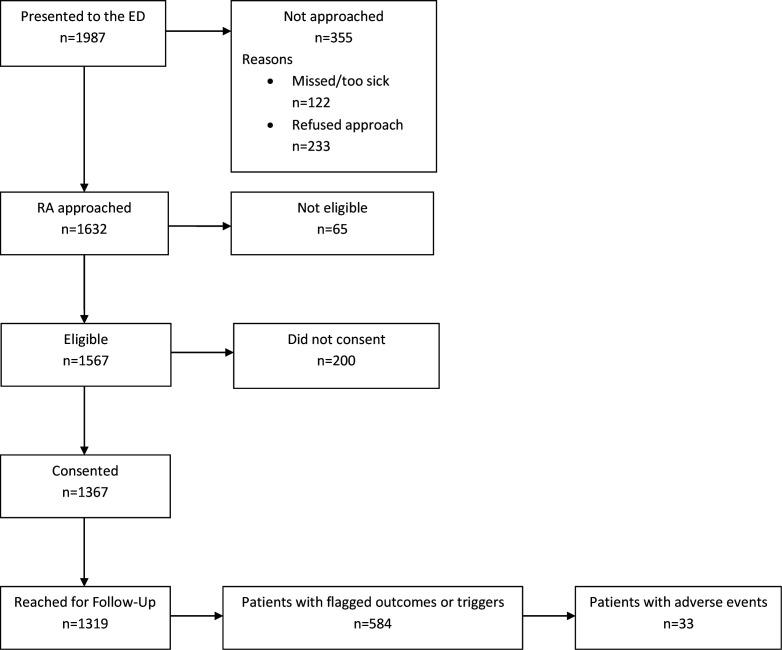
Over the 28 study shifts, 1987 patients presented to the ED. Of these 1987 patients, 1632 were approached by our RAs for participation, 1567 were eligible, and 1367 (87.2%) consented to participation (figure 1).
Figure 1.
Flow diagram of patient enrolment and follow-up. ED, emergency department; RA, research assistant.
Follow-up success
Of the 1367 enrolled patients, 1319 (96.5%) were reached at least once by telephone during the follow-up period and 1276 (93.3%) were reached at the 3-week follow-up. None of the 91 patients reached by telephone at week 1 or 2 but not reached at week 3 were found to have ED visits or hospital admissions between the last completed telephone follow-up and the 3-week follow-up mark. Of the 48 patients lost to all telephone follow-up, none had a hospital visit or admission within the 3-week study period. Among those with no hospital visits or admissions within 6 months of enrolment (n=18), a review of the provincial coroner’s database identified no deaths.
Eligible, non-enrolled patients
We collected baseline demographics and dispositions for 369 eligible, non-enrolled patients (online supplementary material 5). These patients represent those screened retrospectively (ie, missed during a study shift and deemed eligible on retrospective review) (n=239) or those screened in person and who declined study participation but agreed to a limited chart review (n=130). Non-enrolled eligible patients were slightly older (median age 6.21 years vs 4.34 years), were more likely to be admitted (9.5% vs 5.0%) and be in the higher acuity triage categories.
Patient characteristics and systems factors
Table 1 describes the demographic and clinical characteristics of all enrolled children and the ED systems factors at the time of their enrolment visit. Enrolled children were of equal sex distribution, had a median age of 4.34 years (IQR 1.5 to 10.57 years) and most commonly presented with complaints of fever, cough/congestion and difficulty breathing/shortness of breath (15.1 %, 9.9% and 7.9% of patients, respectively). Only a small proportion of patients (4.2%) presented by ambulance. The majority (75.3%) of patients were assessed in the minor/ambulatory section of the ED and had only one ED staff physician involved in their care (93.8%) (ie, no handover occurred).
Table 1.
Baseline characteristics of enrolled patients and system factors related to their ED visit
| Patient characteristic | N | n (%)* |
| Age (years), median (IQR) | 1367 | 4.34 (1.50–10.57) |
| Female sex | 1367 | 676 (49.5) |
| First language of both parents is neither French nor English† | 1367 | 60 (4.4) |
| Both parents immigrated in the previous 5 years† | 1358 | 72 (5.3) |
| Use of prescription medication prior to ED visit | 1367 | 309 (22.6) |
| Chronic medical condition | 1365 | 285 (20.9) |
| Indwelling line, or indwelling urinary catheter, or dialysis catheter or respiratory support needed | 1367 | 26 (1.9) |
| Pediatric Canadian Triage Acuity Score | 1367 | |
| 1 – Resuscitation | 4 (0.3) | |
| 2 – Emergent | 84 (6.1) | |
| 3 – Urgent | 691 (50.5) | |
| 4 – Semiurgent | 495 (36.2) | |
| 5 – Non-urgent | 93 (6.8) | |
| Presenting complaint (top 5) | 1367 | |
| Fever | 207 (15.1) | |
| Cough/congestion | 135 (9.9) | |
| Difficulty breathing/SOB | 108 (7.9) | |
| Upper extremity injury | 92 (6.7) | |
| Abdominal pain | 72 (5.3) | |
| Mental health presentation | 1367 | 29 (2.2) |
| Arrival by ambulance | 1367 | 57 (4.2) |
| Disposition | 1367 | |
| Discharged | 1281 (93.7) | |
| Admitted | 68 (5.0) | |
| Left without being seen | 15 (1.1) | |
| Left against medical advice | 3 (0.2) | |
| System factors | N | n (%)* |
| Location in the ED | 1367 | |
| Acute care area | 337 (24.7) | |
| Ambulatory/minor treatment area | 1030 (75.3) | |
| Time of presentation | 1367 | |
| Day (08:00 to 15:59) | 681 (49.8) | |
| Evening (16:00 to 23:59) | 628 (45.9) | |
| Night (12:00 to 07:59) | 58 (4.2) | |
| Weekday presentation (Monday to Friday) | 1367 | 948 (69.3) |
| Wait time to MD assessment (hours), median IQR | 1344 | 1.5 (0.9–2.1) |
| Length of stay in the ED (time of triage to time of discharge OR time of admission to floor, hours), median (IQR) | 1364 | 2.6 (1.9–3.8) |
| Number of patients waiting to be seen when triaged, median (IQR)‡ | 1367 | 13 (9–19) |
| Number of patients awaiting inpatient beds at time of registration‡ | 1367 | |
| 0 | 157 (11.5) | |
| 1 | 389 (28.5) | |
| 2 | 374 (27.4) | |
| 3 or more | 447 (32.7) | |
| ED census at time of registration, median (IQR)‡ | 1367 | 31 (22–38) |
| Involvement of subspecialty consulting services§ | 1367 | 66 (4.8) |
| First ED-specific services assessment by staff ED physician¶ | 1341 | 542 (40.4) |
| Number of ED staff physicians involved in patient care¶ | 1341 | |
| 0** | 9 (0.7) | |
| 1 | 1258 (93.8) | |
| 2 | 71 (5.3) | |
| 3 or more | 3 (0.2) |
*Unless otherwise indicated.
†Or of sole parent as appropriate to child’s circumstances.
‡For pragmatic reasons, we measured these variables at the midpoint of the hour for each shift (eg, 08:30, 09:30, 10:30) and used for each patient the midpoint of the hour that they were triaged (eg, for a patient triaged at 09:20, we used data collected at 9:30). Triage occurred before registration.
§N includes patients for whom the ED-specific staff requested a subspecialty service consultation (n=55) and those who were seen directly by subspecialty service at the time of their presentation to the ED (n=11).
¶N reflects the 1341 patients who were seen first by ED-specific services (rather than directly by a subspecialty service).
**Represents mental health crisis workers (under the auspices of ED-specific services) directly caring for patients.
ED, emergency department; SOB, shortness of breath.
Flagged outcomes/triggers
Of the 1319 patients with follow-up information available, 584 patients (44.4%) had at least one trigger or flagged outcome (online supplementary material 6). Among these 584 patients, the median number of triggers or flags was 2 (IQR 1–3). The multiple flags per patient were typically related. For example, 339 children reported unresolved symptoms on at least one follow-up call and of these, 120 (35.4%) saw a healthcare provider or visited an ED for these symptoms. Likewise, 124 children reported new symptoms on at least one follow-up call, and 56 (45.2%) visited a healthcare provider or ED for these symptoms.
Adverse events
Thirty-three patients (2.5%, 95% CI 1.8% to 3.5%) suffered an adverse event related to care at the enrolment ED visit within the 3-week study time frame. No patient suffered more than one adverse event related to care at the enrolment ED visit. Twenty-nine adverse events (87.9%, 95% CI 72.7% to 95.2%) were deemed preventable.
Type of adverse event, clinical severity and system response
The most common types of adverse events were management issues (51.5%), diagnostic issues (45.5%) and suboptimal follow-up (15.2%) (see table 2). The adverse events identified only through family/parent report included one management adverse event and two medication adverse events. Sixteen of the adverse events (48.5%) occurred within 72 hours of the ED visit. Overall adverse events were most likely to occur in the first week after the ED visit (n=28, 84.8% of adverse events) with 15.2% (n=5) occurring in the second week and none occurring in the third week.
Table 2.
Type, severity and system response for 33 AEs detected
| N (%)* | |
| Adverse event related to care provided by: | |
| ED-specific services | 26 (78.8) |
| Subspecialist services | 2 (6.1) |
| Both ED-specific services and subspecialist services | 5 (15.2) |
| Type of adverse event† | |
| Diagnostic issue | 15 (45.5) |
| Management issue | 17 (51.5) |
| Unsafe disposition decision | 3 (9.1) |
| Suboptimal follow-up | 5 (15.2) |
| Procedural complication | 2 (6.1) |
| Medication adverse effect | 4 (12.1) |
| Severity of AE | |
| An abnormality on laboratory testing | 0 (0.0) |
| ≤1 day of symptoms | 7 (21.2) |
| >1 day of symptoms | 24 (72.7) |
| Non-permanent disability | 2 (6.1) |
| Permanent disability | 0 (0.0) |
| Death | 0 (0.0) |
| System response required for AE‡ | |
| No treatment (symptoms only) | 3 (9.1) |
| Visit to ED | 15 (45.5) |
| Required medical intervention | 15 (45.5) |
| Required surgical intervention | 4 (12.1) |
| Transfer to critical care | 0 (0.0) |
| Visit to MD office | 12 (36.4) |
| Visit to health facility/laboratory | 6 (18.2) |
| Admission to hospital | 5 (15.2) |
| Death | 0 (0.0) |
*Unless otherwise indicated.
†AEs may be of more than one type.
‡AEs may require more than one type of system response.
AE, adverse event; ED, emergency department.
Most adverse events resulted in symptom prolongation only (table 2). There were two severe adverse events (associated with non-permanent disability), both involving delayed diagnoses that required prolonged admission and treatment. Other examples of adverse events included children with fractures missed on radiographs at the enrolment ED visit that required subsequent immobilisation and use of non-absorbable sutures to repair a laceration while informing family that sutures were absorbable that resulted in delayed and uncomfortable suture removal.
Almost half (45.5%) of all patients with adverse events required some form of medical or surgical intervention to manage their adverse event. Twelve patients required a visit to an MD’s office, 15 required an ED visit and 5 required an admission to hospital following their initial ED visit (table 2).
Patient and system characteristics associated with adverse events
In the univariate analysis (table 3), we found that presentation on a weekend, presentation with a mental health concern, arrival by ambulance and age were associated with adverse events. Age was associated with the odds of an adverse event in a non-linear manner, with older age groups and younger age groups being at greater risk (online supplementary material 7). As a result, a quadratic term for age was added in the multivariate analysis. In the multivariate analysis, age (linear term adjusted OR=0.96 (95% CI: 0.87 to 1.05) and quadratic term adjusted OR=1.02 (95% CI 1.01 to 1.04)), and presentation on a weekday were associated with adverse events (adjusted OR=2.50, 95% CI 1.01 to 7.69) (online supplementary material 8).
Table 3.
Results of single variable* logistic regression for adverse events (n=1319 patients)
| Characteristic | N | n (%) | OR | P value |
| Sex | 0.38 | |||
| Male | 668 | 19 (2.8) | Ref | |
| Female | 651 | 14 (2.2) | 0.73 (0.36–1.46) | |
| Both parents (or single parent) speak English or French | 0.44 | |||
| Yes | 1260 | 31 (2.5) | Ref | |
| No | 59 | 2 (3.4) | 1.74 (0.35–5.42) | |
| Both parents (or single parent) are immigrants† | 0.22 | |||
| No | 1244 | 33 (2.7) | Ref | |
| Yes | 71 | 0 (0.0) | 0.26 (0.00–1.84) | |
| Paediatric Canadian Triage Acuity Scale | 0.23 | |||
| 1, 2 Resus/emergent | 84 | 1 (1.2) | Ref | |
| 3 Urgent | 664 | 22 (3.3) | 1.96 (0.50–17.75) | |
| 4, 5 Semiurgent/non-urgent | 571 | 10 (1.8) | 1.07 (0.25–10.04) | |
| After hours | 0.47 | |||
| No (08:00 to 17:00) | 735 | 16 (2.2) | Ref | |
| Yes (>17:00 to <08:00) | 584 | 17 (2.9) | 0.64 (0.22–2.48) | |
| Weekend | 0.02 | |||
| No (Mon–Friday) | 915 | 29 (3.2) | Ref | |
| Yes (Saturday–Sunday) | 404 | 4 (1.0) | 0.35 (0.11–0.87) | |
| Disposition | 0.98 | |||
| Discharged | 1235 | 32 (2.6) | Ref | |
| Admitted | 66 | 1 (1.5) | 0.87 (0.10–3.39) | |
| Left without being seen or against medical advice | 18 | 0 (0.0) | 1.00 (0.01–7.65) | |
| Indwelling line or urinary catheter, or dialysis catheter or respiratory support needed | 0.74 (0.06–5.52) | 0.83 | ||
| No | 1294 | 33 (2.6) | Ref | |
| Yes | 25 | 0 (0.0) | 0.74 (0.06–5.52) | |
| Mental health visit | 0.04 | |||
| No | 1301 | 31 (2.4) | Ref | |
| Yes | 18 | 2 (11.1) | 5.68 (1.09–19.41) | |
| Patient has at least one chronic medical condition | 0.89 | |||
| No | 1043 | 26 (2.5) | Ref | |
| Yes | 276 | 7 (2.5) | 1.06 (0.43–2.29) | |
| Arrival by ambulance | ||||
| No | 1263 | 29 (2.3) | Ref | |
| Yes | 56 | 4 (7.1) | 3.39 (1.05–8.74) | |
| Initial ED location | 0.94 | |||
| Main ED | 324 | 10 (3.1) | Ref | |
| Ambulatory zone/minor treatment area | 995 | 23 (2.3) | 0.62 (0.08–79.79) | |
| Subspecialty services involved‡ | ||||
| No | 1250 | 30 (2.4) | Ref | 0.12 |
| Yes | 54 | 3 (5.6) | 2.78 (0.73–7.73) | |
| Primary assessor was ED staff§ | 0.38 | |||
| No | 769 | 22 (2.9) | Ref | |
| Yes | 524 | 11 (2.1) | 0.73 (0.34–1.47) | |
| Number of ED staff physicians involved in patient’s care§ | 0.59 | |||
| 1 | 1212 | 31 (2.6) | Ref | |
| 2 | 69 | 2 (2.9) | 1.42 (0.28–4.40) | |
| 3+ | 3 | 0 (0.0) | 5.43 (0.04–60.75) | |
| Continuous variables | ||||
| Patient level | ||||
| Age in years, median (IQR) | 11.87 (1.29–15.48) | <0.001 | ||
| Linear term | 0.96 (0.87–1.05) | |||
| Quadratic term | 1.02 (1.01–1.04) | |||
| Time to see doctor (hours), median (IQR) | 1.13 (0.78–1.95) | 0.97 (0.64–1.24) | 0.87 | |
| Number of patients waiting to be seen when registered, median (IQR) | 14 (11-20) | 0.55 | ||
| Linear term | 1.04 (0.98–1.10) | |||
| Quadratic term | 1.00 (0.99–1.00) | |||
| ED census at time of registration, median (IQR) | 31 (27–42) | 1.02 (0.99–1.06) | 0.18 | |
| Number of patients awaiting admission to the ward, median (IQR) | 2 (1–3) | 1.01 (0.81–1.23) | 0.49 | |
| LOS in the ED (hours) (time to discharge OR time to admission to floor), median (IQR) | 3.08 (1.87–4.28) | 1.10 (0.99–1.20) | 0.08 |
*All logistic regression analyses adjusted for shift (day, evening, night) to account for oversampling of night shifts.
†N is less than 1319 as this data were not collected for four enrolled patients.
‡N is less than 1319 as this does not include the 15 patients who left without being seen. Patients who were seen directly by subspecialty service (n=11) and those patients who were seen first by ED-specific services but for whom a referral to a subspecialty service was also made (n=43) were deemed as having subspecialty service involvement.
§N is less than 1319 as includes only the 1293 patients seen by ED-specific services (11 were seen by subspecialty services directly and 15 left without being seen).
¶N is less than 1319 as this includes only patients seen by an ED-specific service physician (9 of the 1293 patients seen by ED-specific services were managed by a mental health crisis worker with no ED physician involvement).
ED, emergency department; LOS, length of stay.
Discussion
This prospective study estimated the risk, type and preventability of adverse events related to care received among children in a paediatric ED. Overall, 2.5% (95% CI 1.8% to 3.5%) of children in our study suffered an adverse event related to care received in the ED, with 87.9% of these adverse events being preventable. Management and diagnostic issues were the most common types of adverse events. Most adverse events were not severe, with patients primarily having prolonged symptoms. No patient died or suffered permanent injury as result of their adverse event. While the overall number of patients with adverse events were small, almost half of patients with adverse events required a follow-up ED visit and about a third required a visit to a primary healthcare provider.
Other ED-based studies have reported adverse event rates ranging from 0.16% to 6% among patients visiting adult or mixed (adult and paediatric) EDs, with preventability ranging from 36% to 71%.2–5 29–35 Studies that used a multistep methodology similar to ours and followed patients after their ED visit identified that 3% to 6% of patients suffered adverse events related to ED care.3 4 The proportion of patients suffering an adverse event in our study was lower than these similar ED-based studies. This difference may reflect that children presenting to the ED have less comorbidities than adults and that overall the acuity of presentation (as measured by the Canadian Triage Acuity Scale and likelihood of admission) is less than adult ED patients.11 36 Among both hospitalised adults and children, comorbidities are a risk factor for adverse events.8 37 Among admitted adults, increasing age is a risk factor for adverse events.18 38–40 While we found a high proportion of adverse events were preventable, this is in keeping with other ED-based studies with similar methodology.3 4 Such high preventability may reflect the nature of the ED environment and the patient population.
Our study found that management and diagnostic issues underlay the majority of adverse events (51.5% and 45.5%, respectively). The majority of ED-based studies have reported that management adverse events are most common,2–4 but others have reported diagnostic,29 31 medication5 34 and procedural adverse events33 as the most common types. In a multicentre Canadian inpatient study that considered children admitted to both paediatric and community hospitals, surgical causes were the most common source of adverse events. When admissions to community hospitals were considered, adverse events were more likely related to diagnostic and management issues.8 Examination of incident reports of near misses and unsafe conditions among hospitals in a large paediatric emergency network demonstrated most incidents were medication related, followed by laboratory related, radiology related and finally process related.41 These differences may be due to the limitations of voluntary incident reporting systems versus the strengths of prospective observational cohort studies.42 43
A review of adult/mixed population ED studies demonstrated a lack of consistent, independent risk factors for adverse events.44 We identified age as the only independent patient level risk factor for adverse events with children at the extreme ends of age at greater risk for adverse events. We hypothesise that the increased risk in older children may represent a lack of clinical comfort by paediatric emergency physicians in treating ‘near adults’. While other studies have suggested that presentation ‘outside of regular hours’ increases the risk for adverse events,12–14 in contrast, we found that presentation on a weekend was associated with a lower risk adverse event. The reason for this reduced risk is unclear and may represent a sample size limitation. While there is evidence that crowding may affect overall measures of the quality of care provided in the ED,45 we did not find our selected crowding measures to be independently associated with adverse events.
Limitations and strengths of this study
Our study has several limitations. As a single-centre study, our results may not be applicable to other paediatric EDs or to community EDs who may not have ready access to highly specialised paediatric trained personnel. As the number of adverse events detected was low, the power to detect associations was limited. The multivariable analysis of associations should be considered exploratory. Adverse event detection can also be influenced by hindsight bias and outcome bias although we attempted to reduce these by having reviewers consider only information available to the treating physician at the time of the ED visit, using case summaries to reduce handwriting recognition, and blinding treating physician and patient identity. While adverse event determination was on the basis of reviews by three independent physicians, a single reviewer determined the preventability of each adverse event. Multiple reviewers for this step may have resulted in less risk of bias. To mitigate against selection bias, we attempted to approach all patients who presented for care during a study shift. Non-enrolled patients did, however, have higher triage acuity scores than enrolled patients. It is unclear whether adverse events among non-enrolled patients would be systematically different from those in the study population. Finally, the patients were enrolled in this study from 2012 to 2013. We cannot account for any secular trends since this time although we believe the standard of care has not substantially changed.
Our study has a number of strengths. We recruited 83% of eligible patients and reached the overwhelming majority (96.5 %) in follow-up. We took several steps to avoid under-reporting of adverse events. We followed our patients for 3 weeks and used a standardised, two-step process which better detects adverse events than other methods such as voluntary reporting systems.42 43 We used a broad, patient-oriented approach to identifying triggers and flagged outcomes requiring record review, including eliciting specific safety concerns from patients and families. Any cases in which the adverse event determination was widely discrepant were also discussed by the three reviewers and independently rescored. Finally, for all patients lost to telephone follow-up, we undertook a hospital record review and coroner’s database review as necessary to ensure no serious adverse events were missed among these patients. These steps make it unlikely that we missed any serious adverse events among the patients in our study.
Implications for clinical practice and research
Our study has important implications for clinical practice and future research. ED clinicians should be aware that several populations appear at increased risk for adverse events—children at the extremes of age, those presenting with mental health complaints and those arriving by ambulance. As well, while crowding is a concern for ED clinicians,46 47 we did not find an association between our ED crowding measures and adverse events. Patient populations at risk of adverse events and the influence of ED crowding need to be confirmed at a multicentre level. Finally, clinicians should be aware that diagnostic and management issues play significant roles in the occurrence of adverse events. While the science of reducing diagnostic error is rapidly advancing,48 children as a population can present unique diagnostic challenges to clinicians and our study would support further work in this area.
Conclusions
Although we found that children suffer adverse events related to care in the ED less commonly than adults, this study would suggest that 1:40 children suffer adverse events related to ED care. We note that the vast majority of these adverse events were preventable and were related to management or diagnostic issues, suggesting opportunities for improvement of care in these areas.
Footnotes
Contributors: ACP was responsible for study conception, overseeing research staff in administering the study, data interpretation, and drafting the manuscript. LAC assisted with study design, study implementation, data interpretation and drafting of the manuscript. ASN and AS assisted with study design and study implementation. KF, WDC, DWJ and TPK assisted with study design. MA and NB were responsible for data analysis and assisted with study design. DD assisted in study implementation and data acquisition. ST and GN assisted in data acquisition. All authors have reviewed the manuscript, provided critical input and agreed to the publication of the manuscript.
Funding: This study were supported by a grant from the Ontario Academic Health Science Centres Alternate Funding Plan (AFP) Innovation Fund. ACP is supported in part by a Tier II University of Ottawa Research Chair.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The CHEO Research Ethics Board approved this study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1. Croskerry P, Sinclair D. Emergency medicine: a practice prone to error? CJEM 2001;3:271–6. 10.1017/S1481803500005765 [DOI] [PubMed] [Google Scholar]
- 2. Fordyce J, Blank FSj, Pekow P, et al. Errors in a busy emergency department. Ann Emerg Med 2003;42:324–33. 10.1016/S0196-0644(03)00398-6 [DOI] [PubMed] [Google Scholar]
- 3. Forster AJ, Rose NGW, van Walraven C, et al. Adverse events following an emergency department visit. Qual Saf Health Care 2007;16:17–22. 10.1136/qshc.2005.017384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Calder LA, Forster A, Nelson M, et al. Adverse events among patients registered in high-acuity areas of the emergency department: a prospective cohort study. CJEM 2010;12:421–30. 10.1017/S1481803500012574 [DOI] [PubMed] [Google Scholar]
- 5. Friedman SM, Provan D, Moore S, et al. Errors, near misses and adverse events in the emergency department: what can patients tell us? CJEM 2008;10:421–7. 10.1017/S1481803500010484 [DOI] [PubMed] [Google Scholar]
- 6. Barata IA, Benjamin LS, Mace SE, et al. Pediatric patient safety in the prehospital/emergency department setting. Pediatr Emerg Care 2007;23:412–8. 10.1097/01.pec.0000278393.32752.9f [DOI] [PubMed] [Google Scholar]
- 7. Committee on Pediatric Emergency Medicine, American Academy of Pediatrics, Krug SE, Frush K. Patient safety in the pediatric emergency care setting. Pediatrics 2007;120:1367–75. 10.1542/peds.2007-2902 [DOI] [PubMed] [Google Scholar]
- 8. Matlow AG, Baker GR, Flintoft V, et al. Adverse events among children in Canadian hospitals: the Canadian paediatric adverse events study. CMAJ 2012;184:E709–18. 10.1503/cmaj.112153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Agarwal S, Classen D, Larsen G, et al. Prevalence of adverse events in pediatric intensive care units in the United States. Pediatr Crit Care Med 2010;11:568–78. 10.1097/PCC.0b013e3181d8e405 [DOI] [PubMed] [Google Scholar]
- 10. Patient Safety Net . Agency for healthcare Reseach and quality: patient safety primer. Available: https://psnet.ahrq.gov/primers/primer/34/Adverse-Events-Near-Misses-and-Errors [Accessed 30 June 2019].
- 11. Canadian Institute for Health Information . Quick STATs. Available: https://apps.cihi.ca/mstrapp/asp/Main.aspx [Accessed 17 May 2019].
- 12. Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med 2001;345:663–8. 10.1056/NEJMsa003376 [DOI] [PubMed] [Google Scholar]
- 13. Cram P, Hillis SL, Barnett M, et al. Effects of weekend admission and hospital teaching status on in-hospital mortality. Am J Med 2004;117:151–7. 10.1016/j.amjmed.2004.02.035 [DOI] [PubMed] [Google Scholar]
- 14. Arias Y, Taylor DS, Marcin JP. Association between evening admissions and higher mortality rates in the pediatric intensive care unit. Pediatrics 2004;113:e530–4. 10.1542/peds.113.6.e530 [DOI] [PubMed] [Google Scholar]
- 15. Warren DW, Jarvis A, LeBlanc L, et al. Revisions to the Canadian triage and acuity scale paediatric guidelines (PaedCTAS). CJEM 2008;10:224–32. 10.1017/S1481803500010149 [DOI] [PubMed] [Google Scholar]
- 16. Stang AS, McGillivray D, Bhatt M, et al. Markers of overcrowding in a pediatric emergency department. Acad Emerg Med 2010;17:151–6. 10.1111/j.1553-2712.2009.00631.x [DOI] [PubMed] [Google Scholar]
- 17. Weiss SJ, Ernst AA, Sills MR, et al. Development of a novel measure of overcrowding in a pediatric emergency department. Pediatr Emerg Care 2007;23:641–5. 10.1097/PEC.0b013e31814a69e2 [DOI] [PubMed] [Google Scholar]
- 18. Timm NL, Ho ML, Luria JW. Pediatric emergency department overcrowding and impact on patient flow outcomes. Acad Emerg Med 2008;15:832–7. 10.1111/j.1553-2712.2008.00224.x [DOI] [PubMed] [Google Scholar]
- 19. Baker GR, Norton PG, Flintoft V, et al. The Canadian adverse events study: the incidence of adverse events among hospital patients in Canada. CMAJ 2004;170:1678–86. 10.1503/cmaj.1040498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Forster AJ, Clark HD, Menard A, et al. Adverse events among medical patients after discharge from hospital. CMAJ 2004;170:345–9. [PMC free article] [PubMed] [Google Scholar]
- 21. Leape LL, Brennan TA, Laird N, et al. The nature of adverse events in hospitalized patients. Results of the Harvard medical practice study II. N Engl J Med 1991;324:377–84. 10.1056/NEJM199102073240605 [DOI] [PubMed] [Google Scholar]
- 22. Schall M, Sevin C, Wasson JH. Making high-quality, patient-centered care a reality. J Ambul Care Manage 2009;32:3–7. 10.1097/01.JAC.0000343118.23091.8a [DOI] [PubMed] [Google Scholar]
- 23. Weingart SN, Pagovich O, Sands DZ, et al. What can hospitalized patients tell us about adverse events? learning from patient-reported incidents. J Gen Intern Med 2005;20:830–6. 10.1111/j.1525-1497.2005.0180.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Daniels JP, Hunc K, Cochrane DD, et al. Identification by families of pediatric adverse events and near misses overlooked by health care providers. CMAJ 2012;184:29–34. 10.1503/cmaj.110393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Matlow AG, Cronin CMG, Flintoft V, et al. Description of the development and validation of the Canadian Paediatric Trigger Tool. BMJ Qual Saf 2011;20:416–23. 10.1136/bmjqs.2010.041152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hanskamp-Sebregts M, Zegers M, Vincent C, et al. Measurement of patient safety: a systematic review of the reliability and validity of adverse event detection with record review. BMJ Open 2016;6:e011078. 10.1136/bmjopen-2016-011078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Forster AJ, O'Rourke K, Shojania KG, et al. Combining ratings from multiple physician reviewers helped to overcome the uncertainty associated with adverse event classification. J Clin Epidemiol 2007;60:892–901. 10.1016/j.jclinepi.2006.11.019 [DOI] [PubMed] [Google Scholar]
- 28. Firth D. Bias reduction of maximum likelihood estimates. Biometrika 1993;80:27–38. 10.1093/biomet/80.1.27 [DOI] [Google Scholar]
- 29. Hendrie J, Sammartino L, Silvapulle MJ, et al. Experience in adverse events detection in an emergency department: nature of events. Emerg Med Australas 2007;19:9–15. 10.1111/j.1742-6723.2006.00897.x [DOI] [PubMed] [Google Scholar]
- 30. Hendrie J, Sammartino L, Silvapulle MJ, et al. Experience in adverse events detection in an emergency department: incidence and outcome of events. Emerg Med Australas 2007;19:16–24. 10.1111/j.1742-6723.2006.00896.x [DOI] [PubMed] [Google Scholar]
- 31. Wolff AM, Bourke J. Detecting and reducing adverse events in an Australian rural base hospital emergency department using medical record screening and review. Emerg Med J 2002;19:35–40. 10.1136/emj.19.1.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wolff AM, Bourke J, Campbell IA, et al. Detecting and reducing hospital adverse events: outcomes of the Wimmera clinical risk management program. Med J Aust 2001;174:621–5. 10.5694/j.1326-5377.2001.tb143469.x [DOI] [PubMed] [Google Scholar]
- 33. Hall KK, Schenkel SM, Hirshon JM, et al. Incidence and types of non-ideal care events in an emergency department. Quality and Safety in Health Care 2010;19:i20–5. 10.1136/qshc.2010.040246 [DOI] [PubMed] [Google Scholar]
- 34. Henneman PL, Blank FSJ, Smithline HA, et al. Voluntarily reported emergency department errors. J Patient Saf 2005;1:126–32. 10.1097/01.jps.0000175694.39559.12 [DOI] [Google Scholar]
- 35. Freund Y, Goulet H, Leblanc J, et al. Effect of systematic physician cross-checking on reducing adverse events in the emergency department: the CHARMED cluster randomized trial. JAMA Intern Med 2018;178:812–9. 10.1001/jamainternmed.2018.0607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. McDermott KW, Stocks C, Freeman WJ. Overview of Pediatric Emergency Department Visits, 2015. HCUP Statistical Brief #242. Agency for Healthcare Research and Quality. Available: https://hcup-us.ahrq.gov/reports/statbriefs/sb242-Pediatric-ED-Visits-2015.jsp [Accessed 3 Jun 2019]. [PubMed]
- 37. Aranaz-Andrés JM, Limón R, Mira JJ, et al. What makes hospitalized patients more vulnerable and increases their risk of experiencing an adverse event? Int J Qual Health Care 2011;23:705–12. 10.1093/intqhc/mzr059 [DOI] [PubMed] [Google Scholar]
- 38. Wilson RM, Runciman WB, Gibberd RW, et al. The quality in Australian health care study. Med J Aust 1995;163:458–71. 10.5694/j.1326-5377.1995.tb124691.x [DOI] [PubMed] [Google Scholar]
- 39. Thomas EJ, Studdert DM, Burstin HR, et al. Incidence and types of adverse events and negligent care in Utah and Colorado. Med Care 2000;38:261–71. 10.1097/00005650-200003000-00003 [DOI] [PubMed] [Google Scholar]
- 40. Davis P, Lay-Yee R, Briant R, et al. Adverse events in New Zealand public hospitals I: occurrence and impact. N Z Med J 2002;115:U271. [PubMed] [Google Scholar]
- 41. Ruddy RM, Chamberlain JM, Mahajan PV, et al. Near misses and unsafe conditions reported in a pediatric emergency research network. BMJ Open 2015;5:e007541. 10.1136/bmjopen-2014-007541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Naessens JM, Campbell CR, Huddleston JM, et al. A comparison of hospital adverse events identified by three widely used detection methods. Int J Qual Health Care 2009;21:301–7. 10.1093/intqhc/mzp027 [DOI] [PubMed] [Google Scholar]
- 43. Classen DC, Resar R, Griffin F, et al. 'Global trigger tool' shows that adverse events in hospitals may be ten times greater than previously measured. Health Aff 2011;30:581–9. 10.1377/hlthaff.2011.0190 [DOI] [PubMed] [Google Scholar]
- 44. Stang AS, Wingert AS, Hartling L, et al. Adverse events related to emergency department care: a systematic review. PLoS One 2013;8:e74214. 10.1371/journal.pone.0074214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Stang AS, Crotts J, Johnson DW, et al. Crowding measures associated with the quality of emergency department care: a systematic review. Acad Emerg Med 2015;22:643–56. 10.1111/acem.12682 [DOI] [PubMed] [Google Scholar]
- 46. American College of Emergency Physicians . Crowding. ACEP, 2006. Available: https://www.acep.org/patient-care/policy-statements/crowding/ [Accessed 3 Jun 2019].
- 47. Affleck A, Parks P, Drummond A, et al. Emergency department overcrowding and access block. CAEP 2013;15:359-370. Available: https://caep.ca/wp-content/uploads/2016/03/cjem_2013_overcrowding_and_access_block.pdf [Accessed 3 Jun 2019]. [DOI] [PubMed]
- 48. Bates DW, Singh H. Two decades since to err is human: an assessment of progress and emerging priorities in patient safety. Health Aff 2018;37:1736–43. 10.1377/hlthaff.2018.0738 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjqs-2019-010055supp001.pdf (447.7KB, pdf)