Abstract
Objectives
The current systematic review (SR) was undertaken to identify and summarise the published literature reporting on the clinical and economic value of automated in-hospital pharmacy services with a primary focus on systems supporting the dispensing of medicines.
Methods
Literature searches were conducted in MEDLINE, Embase and the Cochrane Library on 17 December 2017 to identify English-language publications investigating any automated dispensing systems (ADSs) in the inpatient setting to include central pharmacy and ward-based systems.
Results
4320 publications were screened by title and abstract and 45 of 175 full publications screened were included. Grey literature searching identified an additional three publications. Therefore, 48 publications relating to ADSs were eligible for inclusion. Although a relatively large evidence base was identified as part of the current SR, the eligible studies were inconsistent in terms of their design and the format of reporting of outcomes. The studies demonstrate that both pharmacy and ward-based ADSs offer benefits over traditional manual dispensing methods in terms of clinical and economic outcomes. The primary benefits following implementation of an ADS include reductions in medication errors, medication administration time and costs. Studies examining optimisation/inventory management strategies/refill programmes for these systems suggest that optimal implementation of the ADS is required to ensure that clinical success and economic benefits are maximised.
Conclusions
The published evidence suggests positive impacts of ADS and should encourage hospitals to invest in automation, with a global strategy to improve the reliability and the efficiency of the medication process. However, one of the key findings of the current SR is the need for further data from adequately powered studies reporting clinically relevant outcomes which would allow for robust, evidence-based recommendations on the return on investment of the technologies. These studies would probably contribute to a larger adoption of these technologies by European hospitals.
Keywords: dispensing robots, hospital pharmacy automation, dispensing forms, uni dose system, clinical pharmacy
Introduction
Medication management within a hospital environment is a complex process usually involving at least four stages from (1) prescribing, (2) transcription and verification, (3) dispensing by nurse to the patient and (4) administration by nurse to the patient.1 Medication management is associated with a risk of errors and inefficiencies across all stages of the process. There is considerable variability in the estimates of medication errors reported in the prescription (approximately 10%–39%), dispensing (approximately 11%–40%) and administration (approximately 10.5%–38%) stages of medication management across different territories with multifactorial causes.2–10 Healthcare policy is therefore focused on methods to reduce the burden of medication errors.1 In recent years, the automation of medication process services such as ordering, dispensing, delivery and administration of medications has been promoted as an important strategy for improving dispensary efficiency, maximising storage capacity and minimising dispensing errors.11 For example, The UK National Health Service has undertaken a review of operational productivity and performance in acute hospitals in England and has recommended a Hospital Pharmacy Transformation Programme (HPTP). A key part of this HPTP is to develop services by “increasing pharmacist prescribers, e-prescribing and administration, accurate cost coding of medicines and consolidating stockholding by April 2020, so that pharmacists and clinical pharmacy technicians spend more time on patient-facing medicines optimisation activities”. There are initiatives and guidelines to improve medication safety and automation is one of the proposed important strategies.12–16
There are many commercially available systems developed to automate in-hospital pharmacy services and the most advanced systems allow for integration of multiple technologies (such as barcode scanning for dispensing and electronic medical record systems) to increase patient safety and the efficiency of healthcare professionals, and to improve pharmacy inventory functions.11 In the pharmacy, these systems can improve organisation of drugs, monitoring of expiration dates and preparation of prescriptions. Automatic stock control and replacement ordering improves efficiency, requiring less technician time. This latter issue is important, as up to 55% of pharmacy staff time is reported to be spent on ‘infrastructure services’, the largest component of which is supply chain activities which includes the buying, making and supplying of medicines. Finally, there is a reduced risk of medication errors.11 These automated systems may be used both by the central hospital pharmacy (‘pharmacy based’) and during decentralised dispensing on the ward (‘ward-based’) (with increased efficiencies gained through automation in both settings). On the ward, these systems improve drug storage until needed by the patient and simplify dispensing of drugs by the nurse.11 This again results in a lower risk of medication errors, improved usage of drugs, and a reduced requirement for nurse and pharmacist time which can then be redeployed to patient care.11 Following the development of technologies to automate in-hospital pharmacy services, it is critical to evaluate their implementation in a real-world hospital setting to ensure that the proposed benefits are in fact apparent in daily use.
Objectives
The current systematic review (SR) was undertaken to identify and summarise the published literature on the clinical and economic value of the automation of in-hospital pharmacy services with a primary focus on systems supporting the dispensing of medicines. The SR was performed in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.17
Methods
Search strategy
Searches of MEDLINE In-Process, MEDLINE, Embase and the Cochrane Library were performed via Ovid on 17 December 2017. The search strategy used to interrogate the EMBASE database is provided in online supplementary table 1. Supplementary searches of conference proceedings for the Clinical Pharmacy Congress, World Congress on Clinical Pharmacy and Pharmacy Practice, Medication Safety Conference, European Association of Hospital Pharmacists, American Pharmacists Association Congress, International Society for Pharmacoeconomics and Outcomes Research, and British Oncology Pharmacy Association were carried out for 2014 to 2017. Additional searches of professional societies including the Institute for Safe Medication Practices (ISMP), Royal Pharmaceutical Society and European Association of Hospital Pharmacists were also conducted.
ejhpharm-2019-002081supp001.pdf (517KB, pdf)
Inclusion and exclusion criteria
Search results were screened for studies of any design reporting at least one outcome measure of interest (ie, clinical or economic) related to ADSs. English-language publications and publications with an abstract in English published 2009 or later were included. The 2009 restriction was chosen because the Canadian Agency for Drugs & Technologies in Health (CADTH) undertook an SR (searches conducted in January 2009) to review technologies available to reduce errors in dispensing and administration of medications in hospitals.18 Due to the overlapping objectives of the SRs, the current SR serves as an update to the previously conducted SR. Full details of the eligibility criteria are provided in table 1.
Table 1.
Eligibility criteria for study inclusion in the clinical SR
| Criteria | Inclusion | Exclusion |
| Population |
|
|
| Intervention |
|
|
| Outcomes | Clinical:
|
|
| Study design | To include:
|
|
| Date of publication/territory of interest | Restricted to publications published from 2009 No restriction on territory of interest |
Articles published prior to 2009 |
| Language of publication | English-language publications or foreign-language publications with an English abstract | – |
ADS, automated dispensing system; SR, systematic review.
Study selection and data extraction
Citations of interest were identified by a member of the team (authors SB or SM) and verified by an independent reviewer (authors SB or SM), based on title and abstract. Full publications were obtained for all citations of interest and were assessed by one reviewer and verified by a second reviewer. Any uncertainties were resolved through discussion. Data were extracted into an Excel spreadsheet by one reviewer and checked against the original publication by a second reviewer.
To ensure that comparable technologies were considered within the current SR, ADS is considered an umbrella term for technologies which automate the dispensing process and includes automated dispensing cabinets, automated dispensing devices and automated dispensing machines (ADMs).
Quality assessment
Included primary studies were assessed using the quality assessment tool for quantitative studies of the Effective Public Health Practice Project (EPHPP).19 The EPHPP tool is considered suitable for use in SR publications including studies of different designs.
Due to the inconsistent reporting of outcomes across the primary studies, a formal quantitative evidence synthesis of the results was not feasible. Rather, a qualitative summary of the results was reported.
Results
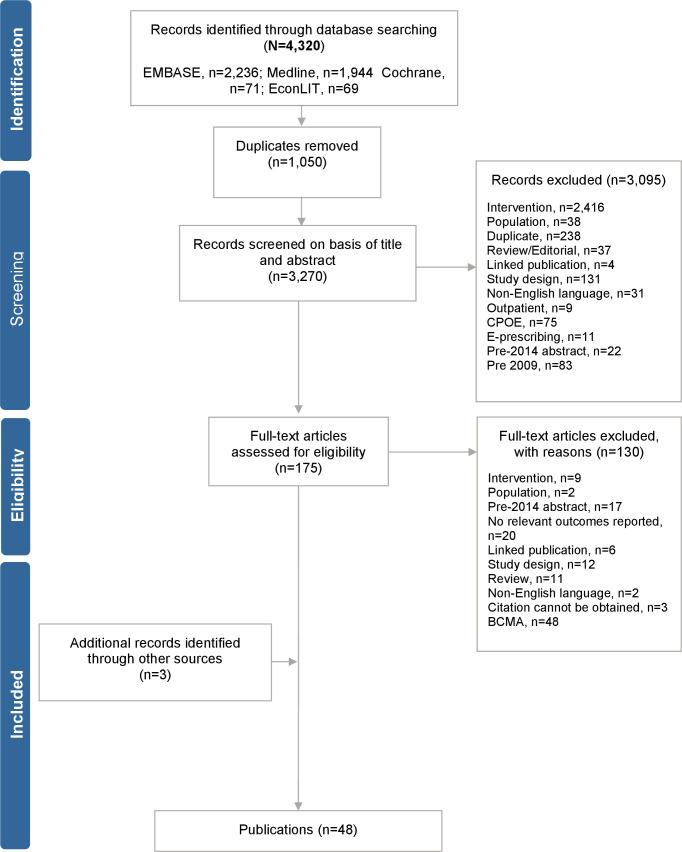
A total of 4320 unique citations of potential interest were identified in the electronic searches and after the removal of 1050 duplicates, 3270 articles were screened by title and abstract. In total, 3095 articles were excluded, and 175 articles were deemed potentially relevant. On completion of full publications review, 45 publications were eligible for inclusion.20–64 Hand searching of conference proceedings, additional sources and reference lists of included studies yielded an additional three eligible publications for inclusion.65–67 This resulted in a total of 48 publications which met the inclusion criteria for the SR.20–67 The PRISMA flow diagram is presented in figure 1. A summary of study design and results is provided in online supplementary table 2. The results of the quality assessment are provided in online supplementary table 3.
Figure 1.
PRISMA flow diagram. BCMA, bar-code medication administration; CPOE, computerised physician order entry.
ejhpharm-2019-002081supp002.xlsx (112.4KB, xlsx)
A total of 35 publications included in the SR reported on ADSs with 13 publications reporting on pharmacy-based dispensing systems24 33 37–39 42 49 51 52 55 63 65 66 and 22 publications reported on ward-based dispensing systems.22 25 27 29–32 35 36 41 43 44 53 56–62 64 67 An additional 13 publications that investigated ADSs integrated with other technologies were also included; five publications reported on dispensing systems and e-prescribing systems20 21 23 34 47 and three publications reported on dispensing and bar-code medication administration (BCMA) systems.26 45 46 The five remaining publications reported on ADS with barcode scanning for dispensing,40 a barcode packager,48 an electronic medical record system,54 dispensing robots28 or barcode scanning during the dispensing process.50
All studies were observational in design20–67 and were conducted across 10 countries with the majority of evidence reported in Europe (14 studies), USA (17 studies) and Australia (4 studies). A large proportion of the studies (n=21) did not report the brand of technology under investigation. The most reported ward-based ADS was Pyxis (6 studies) followed by Omnicell (5 studies). The most reported pharmacy-based ADS was the Rowa Vmax (5 studies) with single studies investigating Omnicell, MedCarousel and ROBOT-Rx.
Thirty-three of the studies were prospective, although it was challenging to ascertain the perspective if not explicitly stated in the publication. Forty of the studies were comparative, comparing pre-intervention periods with post-intervention periods or the automated dispensing technology in parallel with manual dispensing. All studies were conducted in the inpatient setting and 33 studies were set either in the central hospital pharmacy or in general hospital wards. Eleven studies were conducted in specific high-risk hospital departments such as the emergency department (ED)53 54 59 60 62 64 or intensive care unit.56–58 61 63 The duration of study follow-up ranged from 1 week47 to at least 8 years.20 A summary of the study designs and key results of the 48 publications reporting on ADSs is provided in online supplementary appendix table 2.
Pharmacy-based automated dispensing systems
Thirteen studies reported the implementation of ADSs across a range of commercial brands; McKesson’s MedCarousel CDT52 and ROBOT-Rx,55 Omnicell cabinets,24 Becton Dickinson systems (including the Rowa Speedcase,33 Rowa Vmax models49 65 and an unspecified model66), Aethon TUG pharmacy delivery robots,63 Tosho Main Topra and Xana models,42 and Yuyama’s YS-TR-406FDS.38 Three studies did not report the brand or manufacturer of the ADS used.37 39 51
A summary of the outcomes of the pharmacy-based technologies for the 11/13 studies reporting comparative data versus manual dispensing by type and brand is provided in online supplementary appendix table 4. Although there were limited clinical outcomes reported, data suggest that pharmacy-based ADSs are effective in reducing dispensing errors; a statistically significant reduction in dispensing incidents from 0.64% to 0.28% was reported with the ARX Rowa33; an average error rate of 0.10% (with a maximum of rate of 0.16%) was reported following implementation of an ADS in Sutra et al 51 and an increase in the accuracy of dispensing from 99.02% to 99.48% post-implementation of McKesson’s MedCarousel was reported in Temple 2010.52
The studies generally suggest improvements in economic outcomes. In a US-based study, time-savings associated with using an Omnicell ADS accounted for a total decrease of 35 labour hours per week resulting in cost savings of $64 300 for labour annually.24 An additional study conducted in Thailand reported a decrease in pharmacy technician requirements from 132.66 to 55.38 full-time equivalents (FTEs) post-implementation of a YS-TR-406FDS Yuyama ADM. However, this study also reported an increase in the requirement for pharmacists from 46.84 to 117.61 FTEs which was reported to be driven by additional pharmacy roles related to screening and verification for the ADM.38 A study investigating the performance of McKesson’s MedCarousel reported a net reduction of 2.0 pharmacy technician FTEs post-automation and reorganisation of the department.52 James et al reported a statistically significant increase in workload post-automation with ARX Rowa Speedcase ADS from 9.20 pre-automation to 13.17 items/person/hour (p=0.001).33 A single study reported an increase in the costs of inpatient prescriptions post-implementation of an ADS (unknown brand). In this study, the authors concluded that the increase in costs was due to the ADS not being continuously used throughout the day and projected a decrease in unit costs with an increase of ADS coverage from 23% to 75%.39
Ward-based automated dispensing systems
Fifteen of the ward-based studies investigated the implementation of ADSs,25 27 29 30 35 44 53 56–59 61 62 64 67 five studies investigated inventory management and optimisation techniques,22 32 36 41 43 and single studies evaluated an automated refill programme for ADSs31 and the effect of adding broad-spectrum antibiotics to an ADS.60 The studies reported data for the following brands: Medi365 vending unit (n=1),53 Omnicell (n=5),32 36 56 57 59 Pyxis ADSs (n=6)32 41 58 62 64 67 and CardinalASSIST ADS logistics system (n=1).22 The remaining nine studies did not report the brand or manufacturer of the ADS used.25 27 29 30 35 43 44 60 61 A top-line summary of findings from the 20 studies providing comparative data versus manual dispensing is provided in online supplementary appendix table 5.
Several studies reported clinical benefits of ward-based ADSs, including a tendency to a reduction of medication errors,27 59 a reduction in time for treatment dispensing,35 and a reduction in refill and medication errors following the implementation of inventory management and optimisation techniques for ADSs.22 31 A single study also reported that with regard to the manual interventions required following the implementation of an ADS, the majority were related to incorrect ADS procedures and handling (59.7%) rather than those related to structure and functioning of the ADS (29.3%) or inappropriate drugs handling and storage (11.0%).30
Where economic data were reported, data consistently suggested that the implementation of ward-based ADS were associated with a reduction in costs as a result of labour savings, reduced stock and inventory costs, and reduced waste (ie, from expired drugs).32 36 41 56 58 A single study reported a 46% saving of the original investment of the ADS through a decrease in purchased stock.25 Similarly, a study investigating the implementation of the Pyxis MedStation 3500 reported a reduction in stock quantities which could correspond to a saving over an 8-month period of approximately €22 300, while the impact of drug wastage avoidance was reported to be modest at €650.68 This study also reported that staff time savings during the 8-month study period corresponded to a saving of €4120 and €3730 for operating room staff and hospital pharmacy staff, respectively.
A reduction in administration time following the implementation of ward-based ADSs was consistently reported across studies.27 29 35 53 60 A single study reported that the implementation of ADSs in an ED was associated with a statistically significant increase in the overall mean time taken to retrieve medications (5.7 s, p<0.01), which was driven by an increase in retrieval time for less restricted or unscheduled medications.62
Automated dispensing systems integrated with other technologies
In addition to the studies in the SR investigating ADSs (pharmacy or ward-based), 13 publications examining ADSs integrated with other technologies were identified, including e-prescribing,20 21 23 34 47 BCMA systems,26 45 46 or integrated with other technologies such as barcode scanning for dispensing and electronic medical record systems.28 40 48 50 54 The data from these studies were limited but suggested that the integration of multiple technologies could have an additive effect, further improving the medication process.20 21 23 26 28 34 40 45–48 50 54 No studies which investigated ‘closed-loop’ systems automating the entire medication workflow system from prescription to administration were identified.
Discussion
The primary comparison of interest for the current SR is that of ADSs versus manual dispensing approaches. Data from the studies investigating pharmacy or ward-based ADSs consistently demonstrated benefits over traditional manual dispensing methods with regard to both clinical and economic outcomes. The principal benefits following implementation of an ADS included reductions in medication errors and administrations times, and cost savings related to decreased stock, labour savings and waste.10 12 13 15 17–21 23–27 29–32 37 39 40 45 48–54 56–58 60 61 While no formal cost-effectiveness analyses were identified, a single study suggested that implementation of a pharmacy-based ADS was cost-effective compared with manual dispensing if sufficient prescriptions were covered by the system.39 With regard to the potential clinical impact of automation, the inclusion of intravenous antibiotics in an ADS was associated with a reduced incidence of medication errors and a subsequent 4% reduction in patient mortality.23 However, data from studies assessing the impact of optimisation/inventory management strategies/refill programmes indicated that optimal implementation of an ADS was required to achieve the maximum clinical and economic benefits.10 19 29 31 37
The integration of multiple automation components across the medication workflow (ie, e-prescribing systems and BCMA) with ADSs provides additive benefits in the medication process compared with the use of ADSs in isolation.20 21 23 26 28 34 40 45–48 50 54 While no studies were included in the SR which investigated ‘closed-loop’ systems automating the entire prescription to administration medication workflow, data indicate that the integration of multiple automation components across the medication workflow (ie, e-prescribing systems and BCMA) with ADSs provides additive benefits in the medication process compared with the use of ADSs in isolation.69 70 E-prescribing and BCMA are two processes which have been shown to be important for medication prescription and administration errors. For example, an SR investigating the impact of BCMA on the frequency, type and severity of medication administration errors reported BCMA to be associated with a reduction in errors, but also highlighted that the long-term (>1.5 years) effects of BCMA on error reduction were often not assessed.69 Also, there is a paucity of data for the role of e-prescribing. An SR investigating the economic value of e-prescribing in the hospital setting identified only three, low-quality, poorly reported studies, highlighting the need for further well-designed studies to be conducted.70
The studies included in the current SR focused primarily on the impact of technology systems on medication errors. There are limited data associated with the patient consequences (or associated costs) of medication errors.27 34 35 A recent SR published in 2017 summarised the economic impact of medication errors and highlighted that considerable variability existed between the 16 studies identified in terms of financial cost, patient settings and the reported errors.71 The true economic impact of medication errors has not been accurately estimated to date and further studies are required to assess the economic impact of medication errors.
It is widely acknowledged that the ED and intensive care unit (ICU) are associated with a high risk of medication errors, and it is intuitive that pharmacy automation would be associated with a greater beneficial impact in these settings.72 73 A total of 11 studies identified in the SR were conducted exclusively in the ED (n=6)53–55 59 60 62 64 or ICU (n=5).56–58 61 63 However, due to the heterogeneity in study designs, it was not possible to ascertain if pharmacy automation technologies had a greater impact in these high-risk departments compared with general hospital wards.
The results of the current SR are largely consistent with those from the previously conducted SRs investigating pharmacy automation technologies.18 74–78 In general, the SRs reported that automated pharmacy technologies were associated with a reduction in medication errors, dispensing time and cost savings (primarily in high-expense units). However, a recent SR of automated and semi-automated drug distributions systems in hospitals reported that despite improved medication safety with automated drug distribution systems, error types such as prescription errors persisted.78
One of the key findings from the current SR is a ‘call to action’ to encourage pharmacists to perform evaluations when implementing automated pharmacy technologies in their hospital and to publish these data. Ideally, these publications should be submitted to a peer-reviewed journal (even if they take the form of a brief communication) and we would encourage the reporting of data in a consistent format using standardised definitions and allowing comparisons with outcomes prior to the implementation of the technologies. Over time, this would ideally lead to the development of a robust published evidence base for all available technologies and assist with a qualitative (or even quantitative) comparison of technologies and allow for firm evidence-based recommendations on the benefits of hospital pharmacy technologies to be reported in subsequent updates to international guidelines.
Limitations
The results of the current SR must be interpreted in light of several potential limitations. The review was restricted to English-language publications which may limit the global relevance of the findings. A post hoc date restriction (2009) was applied following the initial screening for the electronic database searches. However, previous relevant SRs were identified during the review which included primarily pre-2009 studies which corroborate the findings of the current SR. The absence of published evidence in the public domain for some commercial technologies confirms that there is a lack of peer-reviewed studies investigating these interventions. This may be due to publication bias, whereby results not deemed to be supportive of commercial claims are not published by manufacturers.75 The observational design of the included studies is associated with well-characterised bias from unknown confounders which can impact outcome measurements.76 The lack of both consistent study designs and reporting of comparable outcomes across the studies also limit our ability to make robust inferences both within and between the commercially available technologies. Due to limited evidence relating to the patient consequences of medication errors, it was not possible to infer the impact of a change in the medication error rate on patient outcome.
Footnotes
Twitter: @bonnabry
Correction notice: This paper has been amended since it was published online. The third author's name was spelt incorrectly and this has now been corrected.
Contributors: All authors made substantial contributions to the current manuscript. In particular, SB, SAM and MC designed and finalised the study protocol. SB and SAM conducted the systematic review. All authors provided input into the initial manuscript draft, critiqued and revised the subsequent drafts, and approved the final version of the manuscript. BD were unable to veto the final draft of the manuscript.
Funding: BD funded the research through Mtech Access.
Competing interests: PB and AH report personal fees from Becton Dickinson, outside the submitted work. SB and SAM of Mtech Access were paid consultants to BD.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as online supplementary information.
References
- 1. Allard J, Carthey J, Cope J, et al. Medication errors: causes, prevention and reduction. Br J Haematol 2002;116:255–65. 10.1046/j.1365-2141.2002.03272.x [DOI] [PubMed] [Google Scholar]
- 2. Aldhwaihi K, Schifano F, Pezzolesi C, et al. A systematic review of the nature of dispensing errors in hospital pharmacies. Integr Pharm Res Pract 2016;5:1–10. 10.2147/IPRP.S95733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cheung K-C, Bouvy ML, De Smet PAGM. Medication errors: the importance of safe dispensing. Br J Clin Pharmacol 2009;67:676–80. 10.1111/j.1365-2125.2009.03428.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lewis PJ, Dornan T, Taylor D, et al. Prevalence, incidence and nature of prescribing errors in hospital inpatients: a systematic review. Drug Saf 2009;32:379–89. 10.2165/00002018-200932050-00002 [DOI] [PubMed] [Google Scholar]
- 5. Berdot S, Gillaizeau F, Caruba T, et al. Drug administration errors in hospital inpatients: a systematic review. PLoS One 2013;8:e68856. 10.1371/journal.pone.0068856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tully MP, Ashcroft DM, Dornan T, et al. The causes of and factors associated with prescribing errors in hospital inpatients: a systematic review. Drug Saf 2009;32:819–36. 10.2165/11316560-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 7. Dornan T, Ashcroft DM, Heathfield H, et al. An in depth investigation into causes of prescribing errors by foundation trainees in relation to their medical education. Available: https://wwwgmc-ukorg/FINAL_Report_prevalence_and_causes_of_prescribing_errorspdf_28935150pdf.GeneralMedicalCouncil
- 8. Leape LL, Bates DW, Cullen DJ, et al. Systems analysis of adverse drug events. ADE Prevention Study Group. JAMA 1995;274:35–43. [PubMed] [Google Scholar]
- 9. Keers RN, Williams SD, Cooke J, et al. Prevalence and nature of medication administration errors in health care settings: a systematic review of direct observational evidence. Ann Pharmacother 2013;47:237–56. 10.1345/aph.1R147 [DOI] [PubMed] [Google Scholar]
- 10. McLeod MC, Barber N, Franklin BD. Methodological variations and their effects on reported medication administration error rates. BMJ Qual Saf 2013;22:278–89. 10.1136/bmjqs-2012-001330 [DOI] [PubMed] [Google Scholar]
- 11. Kuiper SA, McCreadie SR, Mitchell JF, et al. Medication errors in inpatient pharmacy operations and technologies for improvement. Am J Health Syst Pharm 2007;64:955–9. 10.2146/ajhp060267 [DOI] [PubMed] [Google Scholar]
- 12. Canadian Pharmacists Association . Pharmacy Thought Leadership Summit Research Report: toward an optimal future: priorities for action, 2016. Available: https://wwwpharmacistsca/cpha-ca/assets/File/pharmacy-in-canada/Thought%20Leadership%20Summit%20Research%20Report_01pdf
- 13. Canadian Society of Hospital Pharmacists . Pharmacy practice in hospitals and other collaborative healthcare settings: position statements, 2016. Available: https://cshpca/sites/default/files/files/publications/Official%20Publications/Position%20Statements/1_Pharmacy-Practice-in-Hospitals-and-Other-Collaborative-Healthcare-Settings-Position-Statements_V2pdf
- 14. SHPA Western Australian Branch submission to the Sustainable Health Review—a prescription for success, 2017. Available: https://wwwshpaorgau/sites/default/files/uploaded-content/website-content/Branches/shpa_wa_branch_-_sustainable_health_reviewpdf
- 15. Hawkins B. ASHP guidelines on the safe use of automated dispensing devices. Am J Health Syst Pharm 2010;67:483–90. 10.2146/sp100004 [DOI] [PubMed] [Google Scholar]
- 16. Billstein-Leber M, Carrillo CJD, Cassano AT, et al. ASHP guidelines on preventing medication errors in hospitals. Am J Health Syst Pharm 2018;75:1493–517. 10.2146/ajhp170811 [DOI] [PubMed] [Google Scholar]
- 17. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Open Med 2009;3:e123–30. [PMC free article] [PubMed] [Google Scholar]
- 18. Perras C, Jacobs P, Boucher M, et al. Technologies to reduce errors in dispensing and administration of medication in hospitals: clinical and economic analyses. CADTH Technol Overv 2010;1:e0116. [PMC free article] [PubMed] [Google Scholar]
- 19. Effective Public Health Practice Project . Quality assessment tool for quantitative studies. Hamilton, ON: Effective Public Health Practice Project, 1998. https://merst.ca/ephpp/ [Google Scholar]
- 20. Alonso AH, Gonzalez CGR, Saez MS. Information technology and automation in hospitals: strategies and experience in a tertiary hospital in Spain. EJHP Practice 2011;17:26–31. [Google Scholar]
- 21. Alvarez Díaz AM, Delgado Silveira E, Pérez Menéndez-Conde C, et al. [New technologies applied to the medication-dispensing process, error analysis and contributing factors]. Farm Hosp 2010;34:59–67. 10.1016/S2173-5085(10)70001-0 [DOI] [PubMed] [Google Scholar]
- 22. Decentralizing the pharmacy: Baystate Health improves patient safety while enhancing labor and inventory management efficiency. Healthc Exec 2014;29:30–1. [PubMed] [Google Scholar]
- 23. Beard RJ, Smith P. Integrated electronic prescribing and robotic dispensing: a case study. Springerplus 2013;2:295. 10.1186/2193-1801-2-295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Caldwell R, Jamriska B. DD-001 Effect of automated dispensing cabinets on drug distribution in 5 hospitals. Eur J Hosp Pharm 2015;22:A70.1–A70. 10.1136/ejhpharm-2015-000639.166 [DOI] [Google Scholar]
- 25. Clou E, Dompnier M, Kably B, et al. [Impact of an automated dispensing system for medical devices in cardiac surgery department]. Ann Pharm Fr 2018;76:64-70. 10.1016/j.pharma.2017.10.003 [DOI] [PubMed] [Google Scholar]
- 26. Cochran GL, Barrett RS, Horn SD. Comparison of medication safety systems in critical access hospitals: combined analysis of two studies. Am J Health Syst Pharm 2016;73:1167–73. 10.2146/ajhp150760 [DOI] [PubMed] [Google Scholar]
- 27. Cottney A. Improving the safety and efficiency of nurse medication rounds through the introduction of an automated dispensing cabinet. BMJ Qual Improv Rep 2014;3. 10.1136/bmjquality.u204237.w1843. [Epub ahead of print: 25 Apr 2014]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cousein E, Mareville J, Lerooy A, et al. Effect of automated drug distribution systems on medication error rates in a short-stay geriatric unit. J Eval Clin Pract 2014;20:678–84. 10.1111/jep.12202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Douglas C, Desai N, Aroh DAM, et al. Automated dispensing cabinets and nurse satisfaction. Nurs Manage 2017;48:21–4. 10.1097/01.NUMA.0000526064.53973.54 [DOI] [PubMed] [Google Scholar]
- 30. Gómez de Travecedo MT, Gómez F, Moreno M, et al. DD-007 Pharmaceuticals interventions in the drugs dispensation process by automated cabinets in a specialty hospital. Eur J Hosp Pharm 2015;22:A72.2–A72. 10.1136/ejhpharm-2015-000639.172 [DOI] [Google Scholar]
- 31. Helmons PJ, Dalton AJ, Daniels CE. Effects of a direct refill program for automated dispensing cabinets on medication-refill errors. Am J Health Syst Pharm 2012;69:1659–64. 10.2146/ajhp110503 [DOI] [PubMed] [Google Scholar]
- 32. Hussey AP, Cook BM, Quane AD, et al. Implementation of an automated dispensing cabinet stewardship program at a tertiary academic medical center. J Pharm Technol 2014;30:191–4. 10.1177/8755122514551560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. James KL, Barlow D, Bithell A, et al. The impact of automation on workload and dispensing errors in a hospital pharmacy. Int J Pharm Pract 2013;21:92–104. 10.1111/j.2042-7174.2012.00238.x [DOI] [PubMed] [Google Scholar]
- 34. Jiménez Muñoz AB, Muiño Miguez A, Rodriguez Pérez MP, et al. Comparison of medication error rates and clinical effects in three medication prescription-dispensation systems. Int J Health Care Qual Assur 2011;24:238–48. 10.1108/09526861111116679 [DOI] [PubMed] [Google Scholar]
- 35. Lo A, Zhu JN, Richman M, et al. Effect of adding piperacillin–tazobactam to automated dispensing cabinets on promptness of first-dose antibiotics in hospitalized patients. Am J Health Syst Pharm 2014;71:1662–7. 10.2146/ajhp130694 [DOI] [PubMed] [Google Scholar]
- 36. McCarthy BC, Ferker M. Implementation and optimization of automated dispensing cabinet technology. Am J Health Syst Pharm 2016;73:1531–6. 10.2146/ajhp150531 [DOI] [PubMed] [Google Scholar]
- 37. Noparatayaporn P, Sakulbumrungsil R, Thaweethamcharoen T, et al. Comparison of unit cost of pharmacy service using automatic and manual dispensing system. TJPS 2016;40:168–71. [Google Scholar]
- 38. Noparatayaporn P, Sakulbumrungsil R, Thaweethamcharoen T, et al. Comparison on human resource requirement between manual and automated dispensing systems. Value Health Reg Issues 2017;12:107–11. 10.1016/j.vhri.2017.03.007 [DOI] [PubMed] [Google Scholar]
- 39. Noparatayaporn P, Thaweethamcharoen T, Sakulbumrungsil R, et al. Cost comparison between the manual system and automated dispensing systems; how to use effective health technology at a large academic hospital in Thailand. Value Health 2016;19:A31. 10.1016/j.jval.2016.03.360 [DOI] [Google Scholar]
- 40. Oldland AR, Golightly LK, May SK, et al. Electronic inventory systems and barcode technology: impact on pharmacy technical accuracy and error liability. Hosp Pharm 2015;50:034–41. 10.1310/hpj5001-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. O'Neil DP, Miller A, Cronin D, et al. A comparison of automated dispensing cabinet optimization methods. Am J Health Syst Pharm 2016;73:975–80. 10.2146/ajhp150423 [DOI] [PubMed] [Google Scholar]
- 42. Palttala I, Heinämäki J, Honkanen O, et al. Towards more reliable automated multi-dose dispensing: retrospective follow-up study on medication dose errors and product defects. Drug Dev Ind Pharm 2013;39:489–98. 10.3109/03639045.2012.670860 [DOI] [PubMed] [Google Scholar]
- 43. Radparvar S, Tesch J, Gull L, et al. 1202. Crit Care Med 2016;44:376. 10.1097/01.ccm.0000509876.34535.dd [DOI] [Google Scholar]
- 44. Recuero Galve L, Marcos Perez G, Sanchez Gundin J, et al. Impact of stock discrepancies in automated dispensing cabinets. Eur J Hosp Pharm 2016;23. [Google Scholar]
- 45. Risor B, Lisby M, Sorensen J. Complex automated medication systems reduce medication administration error rates in an acute medical ward. Eur J Hosp Pharm 2017;24:A236–7. [Google Scholar]
- 46. Risør BW, Lisby M, Sørensen J. Cost-effectiveness analysis of an automated medication system implemented in a Danish hospital setting. Value Health 2017;20:886–93. 10.1016/j.jval.2017.03.001 [DOI] [PubMed] [Google Scholar]
- 47. Rodriguez-Gonzalez CG, Herranz-Alonso A, Martin-Barbero ML, et al. Prevalence of medication administration errors in two medical units with automated prescription and dispensing. J Am Med Inform Assoc 2012;19:72–8. 10.1136/amiajnl-2011-000332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Silverstein S. Pharmacy automation and workflow implications: a case study. J Pharm Technol 2010;26:60–5. 10.1177/875512251002600203 [DOI] [Google Scholar]
- 49. Skalafouris C, Pons JL, Plassart F, et al. DD-005 Developing a management strategy for medication units free of secondary packaging in a hospital pharmacy. Eur J Hosp Pharm 2015;22:A71.2–A71. 10.1136/ejhpharm-2015-000639.170 [DOI] [Google Scholar]
- 50. Smidt CF, Clemmensen MH, Christrup LL, et al. Barcode scanning in the drug dispensing process improves patient safety. Eur J Hosp Pharm 2017;24:A272. [Google Scholar]
- 51. Sutra C, Vitale G, Pages A, et al. Automated unit-dose dispensing system: data collection and analysis of nonconformities over a 13-month period in Ttoulouse Hospital. Pharmacien Hospitalier et Clinicien 2016;51:164–71. [Google Scholar]
- 52. Temple J, Ludwig B. Implementation and evaluation of carousel dispensing technology in a university medical center pharmacy. Am J Health Syst Pharm 2010;67:821–9. 10.2146/ajhp090307 [DOI] [PubMed] [Google Scholar]
- 53. Ardern-Jones J, Hughes DK, Rowe PH, et al. The impact of the introduction of a ward-based automated medicines vending unit on nursing tasks and time in the emergency department. Int J Pharm Pract 2009;17:345–9. 10.1211/ijpp.17.06.0005 [DOI] [Google Scholar]
- 54. Barra ME, Culbreth SE, Sylvester KW, et al. Utilization of an integrated electronic health record in the emergency department to increase prospective medication order review by pharmacists. J Pharm Pract 2018;31:636-641. 10.1177/0897190017735390 [DOI] [PubMed] [Google Scholar]
- 55. Bepko RJ, Moore JR, Coleman JR. Implementation of a pharmacy automation system (robotics) to ensure medication safety at Norwalk Hospital. Qual Manag Health Care 2009;18:103–14. 10.1097/QMH.0b013e3181a02771 [DOI] [PubMed] [Google Scholar]
- 56. Chapuis C, Bedouch P, Detavernier M, et al. Automated drug dispensing systems in the intensive care unit: a financial analysis. Crit Care 2015;19:318. 10.1186/s13054-015-1041-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Chapuis C, Roustit M, Bal G, et al. Automated drug dispensing system reduces medication errors in an intensive care setting. Crit Care Med 2010;38:2275–81. 10.1097/CCM.0b013e3181f8569b [DOI] [PubMed] [Google Scholar]
- 58. de-Carvalho D, Alvim-Borges JL, Toscano CM. Impact assessment of an automated drug-dispensing system in a tertiary hospital. Clinics 2017;72:629–36. 10.6061/clinics/2017(10)07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Fanning L, Jones N, Manias E. Impact of automated dispensing cabinets on medication selection and preparation error rates in an emergency department: a prospective and direct observational before-and-after study. J Eval Clin Pract 2016;22:156–63. 10.1111/jep.12445 [DOI] [PubMed] [Google Scholar]
- 60. Hitti EA, Lewin JJ, Lopez J, et al. Improving door-to-antibiotic time in severely septic emergency department patients. J Emerg Med 2012;42:462–9. 10.1016/j.jemermed.2011.05.015 [DOI] [PubMed] [Google Scholar]
- 61. Mehta S, Deshmukh M, Donnan F, et al. Automated pharmacy dispensing system in neonatal intensive care unit. J Paediatr Child Health 2017;53:67. [Google Scholar]
- 62. Roman C, Poole S, Walker C, et al. A 'time and motion' evaluation of automated dispensing machines in the emergency department. Australas Emerg Nurs J 2016;19:112–7. 10.1016/j.aenj.2016.01.004 [DOI] [PubMed] [Google Scholar]
- 63. Summerfield MR, Seagull FJ, Vaidya N, et al. Use of pharmacy delivery robots in intensive care units. Am J Health Syst Pharm 2011;68:77–83. 10.2146/ajhp100012 [DOI] [PubMed] [Google Scholar]
- 64. Ward MJ, Boyd JS, Harger NJ, et al. An automated dispensing system for improving medication timing in the emergency department. World J Emerg Med 2012;3:102–7. 10.5847/wjem.j.issn.1920-8642.2012.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Kunkel M, Kramer R. Automation and optimisation of pharmaceutical logistics with the Rowa Vmax logistics system in the pharmacy department of the University Medical Center Mainz. Krankenhauspharmazie 2016;37:1–8. [Google Scholar]
- 66. Weeks GR, Thefty S, et al. A pre–post implementation evaluation of a robotic inventory and dispensing system in a tertiary hospital.
- 67. Portelli G, Canobbio M, Bitonto R, et al. The impact of an automated dispensing system for supplying narcotics in a surgical unit: the experience of the National cancer Institute Foundation of Milan. Hosp Pharm 2018;54:1–8. [Google Scholar]
- 68. Portelli G, Canobbio M, Bitonti R, et al. The impact of an automated dispensing system for supplying narcotics in a surgical unit: the experience of the National cancer Institute Foundation of Milan. Hosp pharm 2018;54. [Google Scholar]
- 69. Hassink JJM, Jansen MMPM, Helmons PJ. Effects of bar code-assisted medication administration (BCMA) on frequency, type and severity of medication administration errors: a review of the literature. Eur J Hosp Pharm 2012;19:489–94. 10.1136/ejhpharm-2012-000058 [DOI] [Google Scholar]
- 70. Ahmed Z, Barber N, Jani Y, et al. Economic impact of electronic prescribing in the hospital setting: a systematic review. Int J Med Inform 2016;88:1–7. 10.1016/j.ijmedinf.2015.11.008 [DOI] [PubMed] [Google Scholar]
- 71. Walsh EK, Hansen CR, Sahm LJ, et al. Economic impact of medication error: a systematic review. Pharmacoepidemiol Drug Saf 2017;26:481–97. 10.1002/pds.4188 [DOI] [PubMed] [Google Scholar]
- 72. Weant KA, Bailey AM, Baker SN. Strategies for reducing medication errors in the emergency department. Open Access Emerg Med 2014;6:45–55. 10.2147/OAEM.S64174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Kruer RM, Jarrell AS, Latif A. Reducing medication errors in critical care: a multimodal approach. Clin Pharmacol 2014;6:117–26. 10.2147/CPAA.S48530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Thomsen LA, Herborg H, Rossing C. From machine to mouth: how can automated dose dispensing lead to safer and more effective patient medication? Int J Clin Pharm 2011;33:715. [Google Scholar]
- 75. Tsao NW, Lo C, Babich M, et al. Decentralized automated dispensing devices: systematic review of clinical and economic impacts in hospitals. Can J Hosp Pharm 2014;67:138–48. 10.4212/cjhp.v67i2.1343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Keers RN, Williams SD, Cooke J, et al. Impact of interventions designed to reduce medication administration errors in hospitals: a systematic review. Drug Saf 2014;37:317–32. 10.1007/s40264-014-0152-0 [DOI] [PubMed] [Google Scholar]
- 77. Sng Y, Ong CK, Lai YF. Approaches to outpatient pharmacy automation: a systematic review. Eur J Hosp Pharm 2019;26:157–62. 10.1136/ejhpharm-2017-001424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Ahtiainen HK, Kallio MM, Airaksinen M, et al. Safety, time and cost evaluation of automated and semi-automated drug distribution systems in hospitals: a systematic review. Eur J Hosp Pharm 2020;27:253–62. 10.1136/ejhpharm-2018-001791 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ejhpharm-2019-002081supp001.pdf (517KB, pdf)
ejhpharm-2019-002081supp002.xlsx (112.4KB, xlsx)