Abstract
Background
The spread of the COVID-19 pandemic in China demonstrated at an early stage the high rate of moderate to severe acute respiratory distress syndrome (ARDS) in the patient population. An intervention that has proved beneficial is the use of prone positioning (PP) for mechanically ventilated patients with ARDS. In one institution, PP was practiced in the medical ICU for this population. However, with the dramatically increasing patient load, staff anticipated that greater capacity to provide this treatment to all qualifying patients would be required.
Methods
A group of physical therapists and occupational therapists (PT/OTs) with ICU experience was redeployed from their regular roles to receive training in PP from an experienced medical ICU (MICU) RN. After intensive training, the team was ready to provide PP to patients. As the workload increased, additional PT/OTs were recruited to the team. A coordinating structure comprising attending pulmonologists screened and advised on appropriate patients. A communication and feedback structure was also implemented.
Results
Over a period of seven weeks, the team provided PP to more than 100 patients, with 577 individual interventions in a total of 14 ICUs and one emergency department. There were no major airway or central venous access complications, and only one anterior pressure injury was recorded.
Conclusion
The rapid implementation of an interdisciplinary PP team in a crisis situation is feasible. It can provide a safe and efficient alternative to adding to the workload of an overloaded nursing staff.
Keywords: Prone Positioning, Interdisciplinary team, Acute Respiratory Distress Syndrome, Acute Hypoxemic Respiratory Failure, Mechanical Ventilation, COVID-19, SAR-CoV-2
The coronavirus 2019 (COVID-19) outbreak resulted in more than 80,000 cases and 3,000 deaths in mainland China between December 2019 and March 2020.1 The most severe complication in this population was acute hypoxemic respiratory failure or acute respiratory distress syndrome (ARDS), with more than 3% of total cases requiring intubation and mechanical ventilation.1 Critically ill patients with ARDS present with acute hypoxemia, noncardiogenic pulmonary edema, reduced lung compliance, and increased work on breathing, and the need for positive-pressure ventilation can result in lung endothelial and epithelial injury.2 In March and April of 2020, New York City was at the epicenter of the COVID-19 pandemic. At the peak in April, New York City reported more than 6,000 new cases with more than 1,500 hospitalizations and 400 deaths in a single day.3 Based on case reports from China, it was anticipated that prone positioning (PP) would be widely used in the mechanically ventilated COVID-19 population.1 , 4 PP has been shown to significantly decrease mortality in patients with moderate to severe ARDS.5 This intervention consists of delivering mechanical ventilation to a patient turned face-down.6 PP sessions of 12 hours or more, in conjunction with low tidal volume ventilation and neuromuscular blockade agents, are associated with a survival benefit in patients with moderate to severe ARDS.4 , 6 , 7 However, there are risks when performing PP. Adverse events, such as dislodgement or disruption of peripheral or central venous catheters, complications with the airway, and pressure injuries on the anterior surfaces of the patient occur with higher frequency compared to patients who are positioned in supine.8., 9., 10.
At our institution, prior to the COVID-19 pandemic, PP was confined to two medical ICUs (MICUs) and performed exclusively by MICU staff. Manually positioning a patient to prone requires a minimum of four people for turning and line management, and one additional person for airway management.11 , 12 The large influx of patients with COVID-19 and moderate to severe ARDS in our hospital prompted a need to develop a specialized interdisciplinary Prone Team to match the increased demand for PP interventions.
The goal in establishing the Prone Team, consisting of physical and occupational therapists (PT/OTs) and registered nurses (RNs), was to safely provide PP capability to all mechanically ventilated patients for whom the intervention was clinically indicated. Currently, the COVID-19 pandemic continues to spread and affect new regions of the United States. As a result, hospital systems will need to rapidly adapt to the demand of PP. The purpose of this article is to outline the development and implementation of an efficient interdisciplinary team dedicated to the critical need of PP interventions.
Methods
Prone Team Assembly
Prior to the pandemic, our institution managed patients with moderate to severe ARDS or hypoxemic respiratory failure in two MICUs. In response to the immediate demand for additional critical care capacity, nonconventional spaces were converted to ICUs. In addition, operating rooms, cardiac catheterization labs, and step-down units were transformed into ICUs. During the COVID-19 pandemic, ICU capacity increased from approximately 100 ICU beds in 8 ICUs to 240 ICU beds in 14 ICUs.
Initially, several RNs from multiple ICUs were trained in PP. However, rapidly increasing RN workloads and the high acuity of patients made it clear that a separate dedicated team was required for PP interventions. PT/OTs in the ICU setting have the ability to mobilize critically ill patients safely and with low incidence of harmful adverse events.13 , 14 Prior to the pandemic, PT/OT responsibility in the ICU included management of central and arterial lines, transfer training, rapid interpretation of vital signs, knowledge of basic ICU pharmacology, pulmonary toileting skills, and ventilator management. For these reasons, PT/OTs were ideal candidates to support PP. In addition, due to high critical acuity of the majority of patients in the hospital, PT/OTs had fewer therapy consults, allowing PT/OTs to be available to create the Prone Team. Consequently, senior leadership made the decision to redeploy a group of PT/OTs to meet the new demand for PP under the supervision of an ICU clinical nurse specialist (CNS).
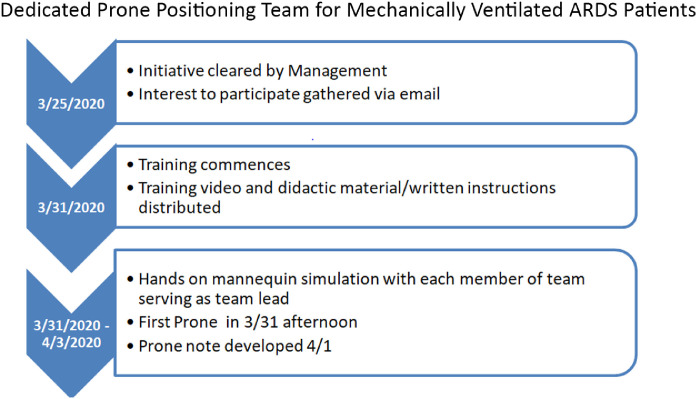
Five days elapsed from initial communication to the first live-patient intervention (Figure 1 ). As demand for PP grew, additional therapists were added to the team. Ultimately, the Prone Team totaled 29 members (12 PTs, 13 OTs, and 4 RNs). The majority of the PT/OTs on the Prone Team had experience with cardiopulmonary rehabilitation and early mobilization in the ICU.
Figure 1.
This time line illustrates the time elapsed from conception of the Prone Team initiative to training and first intervention.
Prone Team: Staffing and Training
Training of the PT/OT group was led by an experienced ICU CNS with eight years of PP experience. Prior to hands-on simulation, the PT/OT group was provided with education on ARDS and PP via a literature review, including the PROSEVA study,5 , 15 that highlighted PP indications, rationale, and contraindications. An instructional video and handout with step-by-step directions for PP, supine positioning, and repositioning were used. Next, a mannequin with simulated lines (endotracheal tube [ETT], central line, radial arterial line, chest tube, and indwelling urinary catheter) was used for in-person repetitive practice of supining, proning, and head turning in accordance with our institution's nursing protocol. Each team member rotated and practiced all bedside positions to gain proficiency and understanding of tasks associated with each role. These roles and their responsibilities included the following:
-
•
Team Lead: Communicated with airway manager to ensure airway security; ensured closed-loop communication and synchronized mobilization.
-
•
Airway Manager: Secured ETT and ventilator management, supported head.
-
•
Positioners: Performed proning or supinating maneuvers.
-
•
Recorder: Documented safety measures, ETT depth, ventilator settings, and any adverse events in the electronic medical record (EMR).
-
•
Runner: Supplied additional materials from outside of the room to minimize personal protective equipment (PPE) waste and improve efficiency.
-
•
ICU RN: Performed overall supervision, managed lines and airway, monitored vitals.
In many cases, the above roles were fluid. Team members shared the tasks of placing electrocardiogram (ECG) electrodes, managing linens and fluidized positioning pillows (FPPs), maintaining line security, and ensuring closed-loop communication. Repetitive practice continued until the CNS deemed the PT/OT group competent prior to the first live-patient PP intervention. Initial competency was achieved within a few hours. Group simulation training allowed rapid visual and tactile skill acquisition in the shortest amount of time. Simultaneously it emphasized qualities that promoted success, such as open verbal communication, central team leader ensuring individual ownership of specific tasks, and pacing and sequencing of tasks.
During PP, the airway manager was at the head of the bed, with two therapists situated on each side of the bed. The airway manager was preferably a respiratory therapist, but the role could be assumed by a physician, nurse practitioner, physician assistant, or ICU RN with airway management skills. The ICU RN was positioned with line visualization and management to assist and supervise the intervention. In addition, the primary RN was present to manage intravenous pumps stationed outside the room (one of our institution's initiatives to minimize exposure and PPE usage), while a primary provider was available in case of emergencies.
Typically, the patient was moved laterally toward the side of the arterial line via a lateral transfer device. The patient was then transitioned to side-lying with the arterial line facing superiorly. In side-lying, the patient's anterior chest ECG electrodes were removed as a new set was simultaneously placed posteriorly. The two team members closest to the foot of the bed prepared the new set of linens, gown, and FPP. While maintaining in side-lying, the patient was transitioned laterally to ensure enough bed space to accept the patient's torso. When the airway manager was ready to turn the patient's head, the patient was then transitioned to prone or supine. When the patient was proned, a large FPP was placed underneath the patient lengthwise from shoulder to hip on one side, and a smaller FPP was placed underneath the head and molded to off-load vulnerable areas. During a handful of occasions in which FPPs were unavailable in the makeshift and popup ICUs, pillows and sheet rolls were used in replacement for pressure off-loading. In an effort to prevent pressure injuries, the patients were repositioned every two hours. Lubricant and transparent dressings were used for eye protection.
Increasing daily PP intervention highlighted the need for documentation to track PP duration, and thus the Recorder position was added. Often the Recorder also served as the Runner to obtain any missing equipment needed for PP intervention. The addition of Recorder/Runner positions offered PT/OT members a short rest break between interventions amid long strenuous Prone Team shifts.
Prone Process: Indications, Materials, and Accessibility
The Prone Team covered 14 separate ICUs across two hospital buildings within this institution. Although rare, the Prone Team also answered consults in the emergency department. The team worked a 12-hour shift from 7:00 a.m. to 7:00 p.m., seven days a week. Each shift, the Prone Team consisted of five to six PT/OTs and one experienced ICU RN.
When the request for PP is established, the pulmonary/critical care attending or fellow overseeing the ICUs (also known as the oversight attending) was then consulted to confirm appropriateness of PP. The oversight attending remained available to consult if repeated PP interventions were indicated and therapeutic. The Prone Team was contacted in person or via the dedicated mobile phone line, the Prone Phone. This phone was the primary method of contact for new and repeating consults, scheduling, emergencies, and cancellations. Orders for PP were placed in the EMR. Guidelines for PP describing indication, contraindication, general approach, personnel, timing, and safety were created for our institution using the PROSEVA study as guide.5 , 15 For PP indications and contraindications see Table 1 .
Table 1.
PP Indications and Contraindications*
| 1. PP is indicated when P/F ratio is < 150 and patient is RASS -5. |
| 2. PP is indicated when P/F ratio < 150 despite ventilator support > 0.60 FiO2 or PEEP > 10 cm H2O. |
| 3. Potential contraindications must be assessed prior to intervening (for example, severe acidemia, hemodynamic instability). |
| 4. Patient must be optimized prior to intervention: a. Deep sedation and/or paralytics b. Hemodynamically optimized (pressors) c. Respiratory (pre-oxygenating, pulmonary toileting, ventilator management, ETT location, and cuff/harness security |
Guidelines for PP describing indication, contraindication, general approach, personnel, timing and safety were created for our institution using the PROSEVA study as guide5,15.
PP, prone positioning; P/F, partial pressure of oxygen / fraction of inspired oxygen; RASS, Richmond Agitation-Sedation Scale; FiO2, fraction of inspired oxygen; PEEP, positive end expiratory pressure; ETT, endotracheal tube.
References can be found at the end of this article.
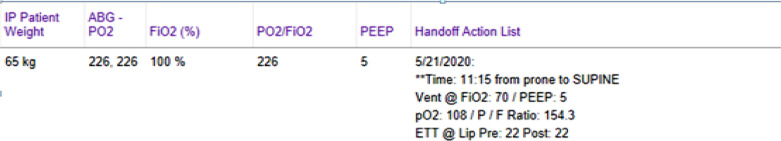
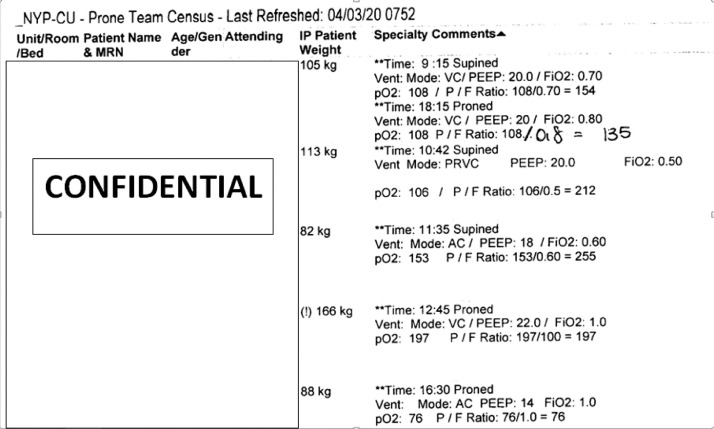
Each morning a prone census list (Figure 2 ) was printed (Figure 3 ) from the EMR, noting patient location, the time the patient was positioned on the previous day, ventilator settings, partial pressure of arterial oxygen (PaO2), PaO2/fraction of inspired oxygen (FiO2) (P/F ratio), and ETT depth. The team lead was responsible for organization of daily triage and communication with the consulting team via use of the Prone Phone. Supination generally took place in the morning and proning in mid-morning/afternoon. Patients were placed in PP for 16–20 hours per session. Effort was made to minimize time spent in transit by grouping patients on the same floors and buildings of the hospital. In addition, communication between disciplines helped to ensure that patients were optimized for intervention prior to Prone Team arrival. If PP was required outside of Prone Team hours, the calls were answered by a core group of MICU nurses.
Figure 2.
The prone census list, shown here as it appears in the electronic medical record, provides a preview of daily updated lab/vent settings and allows for communication and scheduling for the following shift.
Figure 3.
Shown here is a sample prone census list printout, which serves as a daily scheduling list organized by time of previous intervention. This allows the Prone Team leader to schedule following interventions.
Initial PP interventions highlighted medical supplies that were often used but missing or stocked obscurely in various units. To answer this need, the Runner position and Prone Bag/Bundle was conceptualized. The Prone Bag and Bundles (Table 2 ) containing ECG electrodes/leads, central line lock plugs, and syringes allowed increased efficiency, minimized waste of PPE, and helped maintain strict isolation protocols. Equipment was carried via a wheeled cart to reduce the physical burden of having to carry the supplies throughout all units of the hospital.
Table 2.
Prone Bag and Bundles
| Item | Count |
|---|---|
| Alcohol swab | 10 |
| ECG leads set and trunk cable | 5+ |
| ECG electrode set | 5+ |
| ETT cuff flush | 1-2 |
| Rigid oral suction catheter | 1-2 |
| Saline flushes 2.5/10 mL | 5+ |
| Sterile Luer lock plugs | 10 |
| SpO2 sensors | 5+ |
| Tape | 5 |
| Transparent film dressing—small | 5 |
| Transparent film dressing—large | 5 |
Prone bundles (per intervention):
| |
PPE (per staff)
| |
ECG, electrocardiogram; ETT, endotracheal tube; SpO2, oxygen saturation; PPE, personal protective equipment.
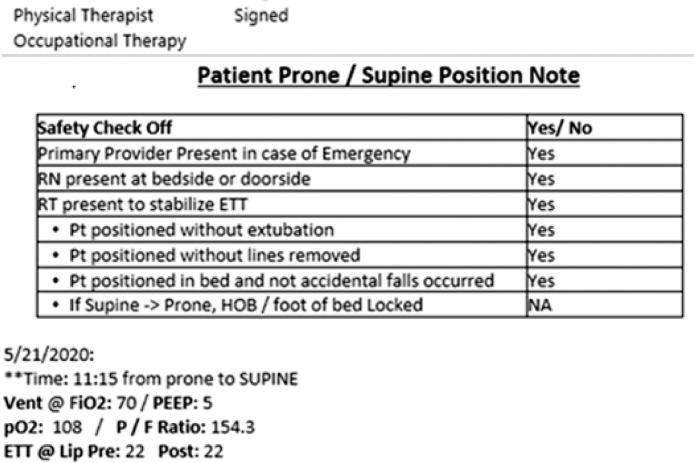
Documentation and Safety Checklist
Prior-day interventions were organized by time of intervention in the EMR. Documentation was done by the Recorder during the PP procedure. Figure 4 shows a sample of the prone document template in the EMR. Documentation included a safety checklist, time of intervention, ventilator settings, and arterial blood gas. When a note was completed, the information was copied into a handoff column within the EMR (Figure 2). This allowed the team leader of the following shift to sort the prone census list according to the time the patient was positioned (Figure 3).
Figure 4.
The note template serves as a safety checklist and documentation of prone intervention to aid scheduling and quality improvement
Results
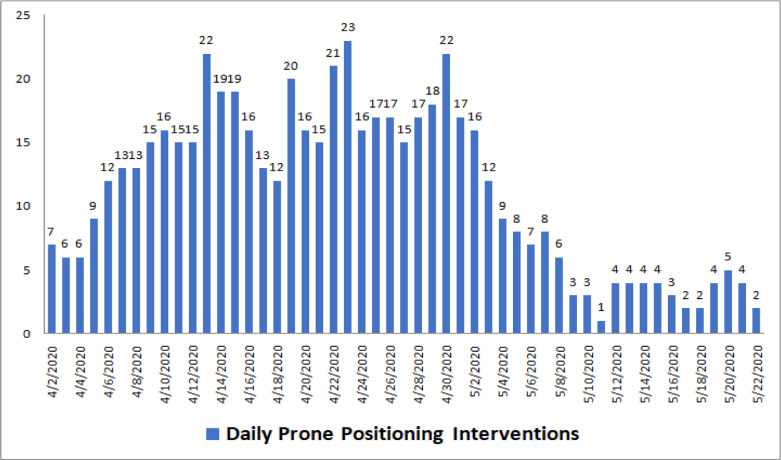
Between March 30, 2020, and May, 22, 2020, the Prone Team safely performed 577 interventions (prone to supine or supine to prone) on 101 unique patients. The majority of patients required multiple PP interventions (Figure 5 ). The patients remained prone for a median of 19 hours per session, with interquartile range (IQR) duration of 17.5 to 20.75 hours.
Figure 5.
The graph illustrates the number of daily interventions provided by the Prone Team between April 2 and May 22, 2020.
There were no incidents of central venous catheter or airway loss. Recorded adverse events included loss of two peripheral intravenous lines and one facial pressure injury. No staff members were injured (Table 3 ).
Table 3.
Recorded Adverse Events
| Adverse Events | Occurrence |
|
|---|---|---|
| During Proning | Noted Postproning | |
| Unplanned patient extubation | 0 | 0 |
| Unplanned patient central line removal | 0 | 0 |
| Unplanned patient peripheral line removal | 2 | 0 |
| Patient falling out of bed | 0 | 0 |
| Other patient injury | 0 | 1 facial DTI Unable to specify cause of injury—PP + ETT bracket vs. adhesive sensitivity |
| Staff and team member physical injury | 0 | 0 |
| PPE failure leading to COVID exposure | 0 | 0 |
DTI, deep tissue injury; PP, prone positioning; ETT, endotracheal tube; PPE, personal protective equipment.
Discussion
During the COVID-19 pandemic, the Prone Team was developed to respond to the rapidly growing number of patients with respiratory distress, and for whom PP was indicated. Overall, the interdisciplinary expertise, training, and collaboration of the Prone Team members allowed for quick deployment and helped to enhance safety and efficiency of proning interventions.
PP remains underutilized as a treatment modality for ARDS.4 Barriers to PP include inexperience in managing pressure areas, suctioning, accidental injuries, and management of emergencies.4 , 5 , 16 , 17 Infrequent use of PP has been identified as a barrier to maintaining PP competency in ICU staff.16 Nurses have noted patients were heavy to manuever manually and were stressed by the lack of clear coordination during interventions.16 Other issues include difficulty performing tracheal suctioning, obtaining intravenous access, regurgitation of enteral feed, and the lack of manpower to address emergencies during night shift.16 At this institution, fears of overburdening an already exhausted nursing staff with additional PP demand was prevalent. The Prone Team used standardized training protocol based on the PROSEVA study5 , 15 led by an experienced ICU RN to address these barriers. Enhanced individual and team competence helped the team to become an autonomous, mobile unit. This mobile format combined with a high level of self-sufficiency allowed increased capacity with minimal disruption to unit activity.
To our knowledge, there has been no peer-reviewed literature outlining the implementation of an interdisciplinary team for the purpose of safe PP. Some articles noted how the rapid deployment of specialized teams can improve safety and efficiency.18 , 19 Safe PP requires proficiency with body mechanics and transfers, a specialization of PT/OTs. This baseline skill set along with involvement in a long-standing early mobilization program at our institution allowed for a more than capable Prone Team.
Loss of venous access and displacement of ETT or thoracotomy tube are among the reported complications of PP.20 , 21 Complications were prevented through adherence to protocol, clearly defined roles, and closed-loop communication. Hemodynamic stability was closely monitored by the Prone Team and communicated to the primary providers during PP interventions. In the case of adverse responses, such as desaturation or dysrhythmia, the onus is on the medical team to provide necessary intervention via modification of ventilator settings or pharmacologic support. Requiring oversight attending approval prior to any intervention helped to ensure appropriate referrals. During adverse events, the oversight attending can be consulted to suggest if PP intervention should be reversed. The use of the Prone Phone allowed timely intervention for all referrals placed during Prone Team hours. In addition, documentation enhanced efficient scheduling. As a token of appreciation, the Prone Team was awarded the “2020 Friend of Nursing Award” by senior management.
There are distinct limitations to this study. The Prone Team was possible in this institution because of the availability of ICU–experienced PT/OTs, who could be redeployed. The staffing and procedures may not be replicable at other institutions due to limited resources. Although there was a considerably low number of adverse events, there were no comparators to assess the relative effectiveness of the team. Data collected reflect incidents recorded by the Prone Team and do not capture any intervention or adverse events provided by ICU staffing outside of Prone Team hours. Finally, the long-term effects of an interdisciplinary Prone Team were not assessed and should be considered for future research.
Conclusion
The Prone Team successfully provided skilled and safe PP to all ICUs throughout our institution. The extent of the success of the Prone Team required an interdisciplinary approach including experienced clinicians with support from hospital leadership. The rapid creation of an interdisciplinary team during a crisis is feasible, safe, and efficient.
Acknowledgments
Acknowledgments
The authors would like to thank New York-Presbyterian Hospital senior and departmental leadership for their support, direction, and confidence. Thank you to Dr. Briana Short and Dr. Daniel Brodie for the conceptualization of the Prone Team and their continued clinical support. Thank you to Dr. Eileen Carter, PhD, RN, and Dr. Mark Vorensky, MS, DPT, SCS, OCS, for their assistance in this manuscript. Finally, a very special thank you to all the members of the multidisciplinary Prone Team—a team whose expertise, commitment, and courage need to be acknowledged and commended: Abigail Zemelman, OTR/L; Allison Gardner, OTR/L; Amanda Cypher, OTR/L; Atara Sheinson, OTR/L; Amy Sommerville, OTR/L, CLTA; Carly Goldberg, OTR/L; Christopher John, PT, DPT; Daphne Polynice, MS, RN, ACCNS-AG, CCRN; Dean Morgan, PT, DPT, CSC; Ellie Jun, BSN, CCRN; Emily Fleisch, PT, DPT; Kelsey LaTourette, OTR/L; Keri Galuskin, MA, OTR/L; Kevin Lindsay, PT, DPT; Lori Buck, PT, MSPT, CCS; Madeline Arena, PT, DPT; Marcin Madej, PT, DPT; Marisa Glasser, PT, MSPT; Nicole Pieszchata, PT, DPT, CCS; Portia Adu Sarhene, DNP, AGACNP-BC, RN, CCRN; Stephen Evans, PT, DPT; Vanessa Sorrentino, PT, DPT; Victoria Parkes, OTR/L.
Conflicts of Interest
All authors report no conflicts of interest.
References
- 1.Meng L. Intubation and ventilation amid the COVID-19 outbreak: Wuhan's experience. Anesthesiology. 2020;132:1317–1332. doi: 10.1097/ALN.0000000000003296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Matthay MA. Acute respiratory distress syndrome. Nat Rev Dis Primers. 2019;5:18. doi: 10.1038/s41572-019-0069-0. Mar 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.NYC Health. COVID-19: Data. (Updated: Jul 13, 2020.) Accessed: July 13, 2020. https://www1.nyc.gov/site/doh/covid/covid-19-data.page.
- 4.Ziehr DR. Respiratory pathophysiology of mechanically ventilated patients with COVID-19: a cohort study. Am J Respir Crit Care Med. 2020;201:1560–1564. doi: 10.1164/rccm.202004-1163LE. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guérin C. A prospective international observational prevalence study on prone positioning of ARDS patients: the APRONET (ARDS Prone Position Network) study. Intensive Care Med. 2018;44:22–37. doi: 10.1007/s00134-017-4996-5. [DOI] [PubMed] [Google Scholar]
- 6.Poston JT, Patel BK, Davis AM. Management of critically ill adults with COVID-19. JAMA. 2020;323:1839–1841. doi: 10.1001/jama.2020.4914. May 12. [DOI] [PubMed] [Google Scholar]
- 7.Beitler JR. Prone positioning reduces mortality from acute respiratory distress syndrome in the low tidal volume era: a meta-analysis. Intensive Care Med. 2014;40:332–341. doi: 10.1007/s00134-013-3194-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park SY. The efficacy and safety of prone positioning in adults patients with acute respiratory distress syndrome: a meta-analysis of randomized controlled trials. J Thorac Dis. 2015;7:356–367. doi: 10.3978/j.issn.2072-1439.2014.12.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee JM. The efficacy and safety of prone positional ventilation in acute respiratory distress syndrome: updated study-level meta-analysis of 11 randomized controlled trials. Crit Care Med. 2014;42:1252–1262. doi: 10.1097/CCM.0000000000000122. [DOI] [PubMed] [Google Scholar]
- 10.Munshi L. Prone position for acute respiratory distress syndrome: a systematic review and meta-analysis. Ann Am Thorac Soc. 2017;14:S280–S288. doi: 10.1513/AnnalsATS.201704-343OT. [DOI] [PubMed] [Google Scholar]
- 11.Athota KP. A practical approach to the use of prone therapy in acute respiratory distress syndrome. Expert Rev Respir Med. 2014;8:453–463. doi: 10.1586/17476348.2014.918850. [DOI] [PubMed] [Google Scholar]
- 12.Dalmedico MM. Efficacy of prone position in acute respiratory distress syndrome: overview of systematic reviews. Rev Esc Enferm USP. 2017;51:e03251. doi: 10.1590/S1980-220X2016048803251. Oct 9. [DOI] [PubMed] [Google Scholar]
- 13.Nydahl P. Safety of patient mobilization and rehabilitation in the intensive care unit: systematic review with meta-analysis. Ann Am Thorac Soc. 2017;14:766–777. doi: 10.1513/AnnalsATS.201611-843SR. [DOI] [PubMed] [Google Scholar]
- 14.Zhang L. Early mobilization of critically ill patients in the intensive care unit: a systematic review and meta-analysis. PLoS One. 2019;14 doi: 10.1371/journal.pone.0223185. Oct 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bein T. The standard of care of patients with ARDS: ventilatory settings and rescue therapies for refractory hypoxemia. Intensive Care Med. 2016;42:699–711. doi: 10.1007/s00134-016-4325-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCormick J, Blackwood B. Nursing the ARDS patient in the prone position: the experience of qualified ICU nurses. Intensive Crit Care Nurs. 2001;17:331–340. doi: 10.1054/iccn.2001.1611. [DOI] [PubMed] [Google Scholar]
- 17.Chadwick JR. Prone positioning in trauma patients: nursing roles and responsibilities. J Trauma Nurs. 2010;17:201–207. doi: 10.1097/JTN.0b013e3181ff2813. [DOI] [PubMed] [Google Scholar]
- 18.Sheth PD. Development of a surgical workforce access team in the battle against COVID-19. J Vasc Surg. 2020;72:414–417. doi: 10.1016/j.jvs.2020.04.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coons BE, Tam SF, Okochi S. Rapid development of resident-led procedural response teams to support patient care during the coronavirus disease 2019 epidemic: a surgical workforce activation team. JAMA Surg. 2020;155:683–684. doi: 10.1001/jamasurg.2020.1782. [DOI] [PubMed] [Google Scholar]
- 20.Gattinoni L. Effect of prone positioning on the survival of patients with acute respiratory failure. N Engl J Med. 2001;345:568–573. doi: 10.1056/NEJMoa010043. Aug 23. [DOI] [PubMed] [Google Scholar]
- 21.Taccone P. Prone positioning in patients with moderate and severe acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2009;302:1977–1984. doi: 10.1001/jama.2009.1614. Nov 11. [DOI] [PubMed] [Google Scholar]