Highlights
-
•
Fertility preservation services are utilized in 9% of reproductive age males with cancer.
-
•
While use of fertility preservation services is increasing, rates of use remain modest.
-
•
Younger age men and those receiving chemotherapy and radiation are more likely to utilize fertility preservation services.
Keywords: Infertility, Fertility, Reproduction, Cryopreservation, Sperm, Cancer
Abstract
While fertility preservation is a major concern among reproductive age cancer patients, little is known about access and use of fertility preserving services. We examined use of fertility preserving services among men with common solid tumors.
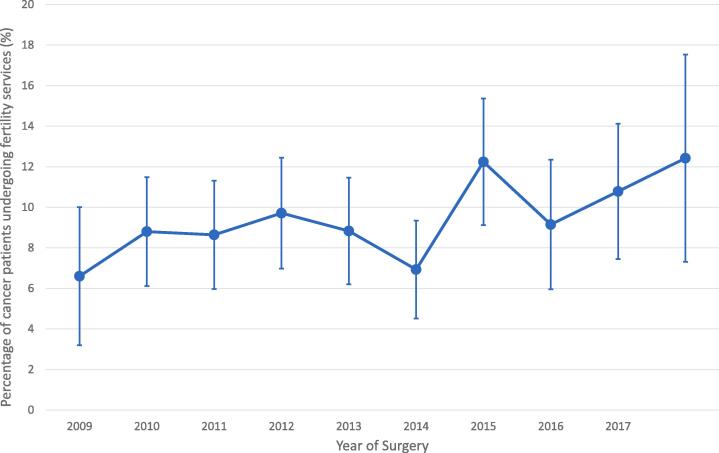
A total of 3648 men age 18–40 including 2610 (71.6%) with testicular cancer, 939 (25.7%) with colorectal and 99 (2.7%) with prostate cancer were identified. Fertility preservation services were utilized in 9.3% of men overall including 4.1% who underwent fertility evaluation only and 7.8% who had a fertility preservation procedure. The rate of fertility preservation services rose from 6.6% (95%CI, 3.2–10.0) in 2008 to 12.4% (95%CI, 7.3–17.5) in 2017 (P = 0.04).
Use of fertility preservation service was more common in patients with testicular (11.6%, aRR = 3.31; 95% CI 2.22–4.92) and prostate cancer (6.1%, aRR = 3.14; 95% CI 1.28–7.70) compared to those with colon cancer (3.4%). Younger men were more likely to utilize fertility preservation services. 11.5% of men age ≤ 35 years vs. 5.2% of men 36–40 used these services (P < 0.0001). Fertility preservation services were used in 10.8% of those who received chemotherapy (aRR = 1.81; 95% CI, 1.45–2.27) and in 8.1% of those who received radiation (aRR = 1.30 95% CI, 0.98–1.73). Medicaid patients were less likely to receive fertility preservation services than those with commercial insurance (0.7% vs. 10.1%; aRR = 11.58, 95%CI 2.10–63.69). These data indicate that while use of fertility preserving services is increasing, overall use of services is low among reproductive age males with cancer.
1. Introduction
Advances in cancer treatment for reproductive-aged males have resulted in greater life expectancies and long term survival (Barak, 2019). As survival improves for young adults, the desire for paternity has become an increasingly important issue (Green et al., 2010). The use of sperm cryopreservation prior to cancer treatment is a safe and effective method for male fertility preservation with success rates approaching 90% (Menon et al., 2009). While guidelines for oncologists recommend consideration of fertility preserving options for reproductive age male cancer patients, little is known about the utilization of these services (Oktay et al., 2018). We analyzed the use and predictors of fertility preservation services among reproductive-aged male cancer patients.
2. Methods
We used the IBM Watson MarketScan database which annually captures claims from >50 million privately insured patients nationwide and 6 million Medicaid enrollees from 12 states (MarketScan Research Database). Data were de-identified and deemed exempt by the Columbia University Institutional Review Board.
We identified men 18–40 years of age with incident testicular, prostate, or colorectal cancer who underwent cancer-directed surgery from 2008 to 2017. Use of fertility preservation services were classified using available billing codes including evaluation and counseling for fertility preservation as well as fertility preservation procedures including sperm cryopreservation/storage. Covariates in the analysis included age, type of cancer, year of surgery, insurance status, region of residence, Elixhauser co-morbidity index, metropolitan statistical area (MSA), and use of radiation or chemotherapy within 6 months of surgery. Associations between fertility preservation services and the covariates of interest were analyzed using χ2 tests and multivariable log-linear regression models.
3. Results
We identified a total of 3648 men including 2610 (71.6%) with testicular cancer, 939 (25.7%) with colorectal and 99 (2.7%) with prostate cancer (Table 1). Fertility preservation services were utilized in 9.3% of men overall including 4.1% who underwent fertility evaluation only and 7.8% who had a fertility preservation procedure. The rate of fertility preservation services rose from 6.6% (95%CI, 3.2–10.0) in 2008 to 12.4% (95%CI, 7.3–17.5) in 2017 (P = 0.04) (Fig. 1).
Table 1.
Rate of fertility services among male reproductive-aged cancer patients.
| Entire Cohort |
Fertility Service^ |
|||||
|---|---|---|---|---|---|---|
| N | % | N | % | P-value | aRR (95%CI)# | |
| All | 3648 | 100.0 | 340 | 9.3 | ||
| Age (years) | <0.0001 | |||||
| ≤35 | 2389 | 40.4 | 274 | 11.5 | 1.76 (1.33, 2.34)** | |
| 36–40 | 1259 | 21.3 | 66 | 5.2 | Referent | |
| Cancer | <0.0001 | |||||
| Testicular Cancer | 2610 | 71.6 | 302 | 11.6 | 3.31 (2.22, 4.92)** | |
| Colorectal Cancer | 939 | 25.7 | 32 | 3.4 | Referent | |
| Prostate Cancer | 99 | 2.7 | 6 | 6.1 | 3.14 (1.28, 7.70)* | |
| Health insurance | <0.0001 | |||||
| Medicaid | 285 | 7.8 | 2 | 0.7 | Referent | |
| Commercial | 3363 | 92.2 | 338 | 10.1 | 11.58 (2.10, 63.69)* | |
| Region | <0.0001 | |||||
| Northeast | 622 | 17.1 | 100 | 16.1 | 1.85 (1.41, 2.45)** | |
| North Central | 783 | 21.5 | 87 | 11.1 | 1.30 (0.98, 1.74) | |
| South | 1209 | 33.1 | 104 | 8.6 | Referent | |
| West | 694 | 19.0 | 43 | 6.2 | 0.65 (0.45, 0.92)* | |
| Unknown | 340 | 9.3 | 6 | 1.8 | 0.38 (0.08, 1.70) | |
| MSA | <0.0001 | |||||
| No | 418 | 11.5 | 31 | 7.4 | Referent | |
| Yes | 2881 | 79.0 | 300 | 10.4 | 1.36 (0.94, 1.97) | |
| Unknown | 349 | 9.6 | 9 | 2.6 | 3.08 (0.94, 10.06) | |
| Elixhauser comorbidity | 0.0133 | |||||
| 0 | 3121 | 85.6 | 309 | 9.9 | Referent | |
| 1 | 348 | 9.5 | 20 | 5.8 | 0.80 (0.51, 1.27) | |
| ≥2 | 179 | 4.9 | 11 | 6.2 | 1.10 (0.59, 2.03) | |
| Year of surgery | 0.0963 | |||||
| 2008–2009 | 644 | 17.7 | 52 | 8.1 | Referent | |
| 2010–2011 | 881 | 24.2 | 81 | 9.2 | 1.07 (0.76, 1.52) | |
| 2012–2013 | 886 | 24.3 | 70 | 7.9 | 0.96 (0.67, 1.38) | |
| 2014–2015 | 742 | 20.3 | 81 | 10.9 | 1.34 (0.94, 1.91) | |
| 2016–2017 | 495 | 13.6 | 56 | 11.3 | 1.49 (1.01, 2.20)* | |
| Radiotherapy | 0.1664 | |||||
| No | 2865 | 78.5 | 277 | 9.7 | Referent | |
| Yes | 783 | 21.5 | 63 | 8.1 | 1.30 (0.98, 1.73) | |
| Chemotherapy | 0.0022 | |||||
| No | 1866 | 51.2 | 147 | 7.9 | Referent | |
| Yes | 1782 | 48.9 | 193 | 10.8 | 1.81 (1.45, 2.27)** | |
Fertility evaluation 4.1%, fertility preservation 7.8%. Some patients (2.6%) had both fertility evaluation and preservation.
aRR: Adjusted risk ratio from multivariable log-linear model.
P-value < 0.05.
P-value < 0.0001.
Fig. 1.
Use of fertility services over time (P < 0.001).
Use of fertility preservation service was more common in patients with testicular (11.6%, aRR = 3.31; 95% CI 2.22–4.92) and prostate cancer (6.1%, aRR = 3.14; 95% CI 1.28–7.70) compared to those with colon cancer (3.4%). Younger men were more likely to utilize fertility preservation services. 11.5% of men age ≤35 years vs. 5.2% of men 36–40 used these services (P < 0.0001). Fertility preservation services were used in 10.8% of those who received chemotherapy (aRR = 1.81; 95% CI, 1.45–2.27) and in 8.1% of those who received radiation (aRR = 1.30 95% CI, 0.98–1.73). Medicaid patients were less likely to receive fertility preservation services than those with commercial insurance (0.7% vs. 10.1%; aRR = 11.58, 95% CI 2.10–63.69).
4. Discussion
Fertility preservation services were utilized in fewer than 10% of reproductive-aged men with cancer. These findings are similar to smaller scale single institution studies showing low rates of fertility counseling and referral for sperm banking in young male cancer patients despite the fact that reproductive function is a major concern among patients (Grover et al., 2016). Underuse of fertility preservation is likely driven by a multitude of factors including lack of awareness among patients and providers, cost, patient ambivalence or self-consciousness, and lack of facilities for preservation procedures (Coward et al., 2013)
We recognize several limitations. The use of administrative data may under-capture services paid for out of pocket; we lacked data on men’s reproductive history and goals, cultural beliefs, and our cohort was limited to men with incident cancer. We lack data on several important covariates including race/ethnicity, sexual orientation, and tumor characteristics. Furthermore, we were unable to include other common cancers such as leukemia and lymphoma due to challenges in capturing newly diagnosed cases. Nevertheless, these data highlight the urgent need to raise awareness of fertility preservation options for reproductive-aged male oncology patients and to address barriers to reproductive care.
Author contributions
Selter: Conception, study design, data collection, statistical analysis, manuscript drafting, final approval of manuscript.
Huang: Conception, study design, data collection, statistical analysis, manuscript drafting, final approval of manuscript.
Williams: Study design, statistical analysis, final approval of manuscript.
Brady: Study design, statistical analysis, final approval of manuscript.
Melamed: Study design, statistical analysis, final approval of manuscript.
Hershman: Study design, statistical analysis, final approval of manuscript.
Wright: Conception, study design, data collection, statistical analysis, manuscript drafting, final approval of manuscript.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Dr. Wright has served as a consultant for Clovis Oncology and received research funding from Merck.
References
- Barak S. Fertility preservation in male patients with cancer. Best Pract. Res. Clin. Obstet. Gynaecol. 2019;55:59–66. doi: 10.1016/j.bpobgyn.2018.12.004. [DOI] [PubMed] [Google Scholar]
- Coward R.M., Kovac J.R., Smith R.P., Lipshultz L.I. Fertility Preservation in Young Men Treated for Malignancies: Options for Precancer Treatment. Sex Med. Rev. 2013;1:123–134. doi: 10.1002/smrj.13. [DOI] [PubMed] [Google Scholar]
- Green D.M., Kawashima T., Stovall M. Fertility of male survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J. Clin. Oncol. 2010;28:332–339. doi: 10.1200/JCO.2009.24.9037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grover N.S., Deal A.M., Wood W.A., Mersereau J.E. Young men with cancer experience low referral rates for fertility counseling and sperm banking. J. Oncol. Pract. 2016;12:465–471. doi: 10.1200/JOP.2015.010579. [DOI] [PubMed] [Google Scholar]
- MarketScan Research Database. (accessed March 10, 2012, at http://marketscan.thomsonreuters.com/marketscanportal/).
- Menon S., Rives N., Mousset-Simeon N. Fertility preservation in adolescent males: experience over 22 years at Rouen University Hospital. Hum. Reprod. 2009;24:37–44. doi: 10.1093/humrep/den361. [DOI] [PubMed] [Google Scholar]
- Oktay K., Harvey B.E., Partridge A.H. Fertility Preservation in Patients With Cancer: ASCO Clinical Practice Guideline Update. J. Clin. Oncol. 2018;36:1994–2001. doi: 10.1200/JCO.2018.78.1914. [DOI] [PubMed] [Google Scholar]