Abstract
Purpose
Completely displaced distal radius fractures in children have been traditionally reduced and immobilized with a cast or pin fixed. Cast immobilization leaving the fracture displaced in the bayonet position has been recently suggested as a non-invasive and effective treatment alternative. This is a pilot comparative study between reduction and no reduction.
Methods
We assessed subjective, functional and radiographic outcome after a minimum 2.5-year follow-up in 12 children under ten years of age who had sustained a completely displaced metaphyseal radius fracture, which had been immobilized leaving the fracture in an overriding position (shortening 3 mm to 9 mm). A total of 12 age-matched patients, whose similar fractures were reduced and pin fixed, were chosen for controls.
Results
At follow-up none of the 24 patients had visible forearm deformity and the maximal angulation in radiographs was 5° Forearm and wrist movement was restored (< 10° of discrepancy) in all 24 patients. Grip strength ratio was normal in all but three surgically treated patients. All patients had returned to their previous activities. One operatively treated boy who was re-operated on reported of pain (visual analogue scale 2).
Conclusion
The results of this study do not demonstrate the superiority of reduction and pin fixation over cast immobilization in the bayonet position of closed overriding distal metaphyseal radius fractures in children under ten years with normal neurovascular findings.
Level of evidence
III
Keywords: children’s fracture, distal metaphyseal radius fracture, overriding fracture, bayonet position, cast immobilization, pin fixation
Introduction
Displaced paediatric distal metaphyseal radius fractures have been traditionally reduced either in local or general anaesthesia. It has been reported, however, that most of these fractures heal well despite failed or lost reductions and shortening up to 10 mm and angulations up to 35° in the sagittal plane can be expected to remodel.1,2 In fact, Crawford et al3 have recently claimed that distal metaphyseal radius fractures in children younger than 11 years of age can be immobilized without reduction in an overriding position with good outcome. On the other hand, several authors4-10 advocate reduction and percutaneous pin fixation, because the risk of re-displacement of the fracture during immobilization is high (14% to 91%).
Half of the attending paediatric orthopaedic surgeons in our department were inspired by the report of Crawford et al3 to try treatment of completely displaced distal metaphyseal radius fractures in children with cast immobilization without reduction, expecting a non-inferior outcome compared with traditional treatment of reduction and pin fixation. The aim of this study is to compare subjective, functional and radiographic outcome in children with an overriding distal metaphyseal radius fracture treated with immobilizing the radius in a bayonet position with reduction and pin fixation of the fracture.
Materials and methods
All fractures have been prospectively registered in our tertiary level teaching institution by Kids’ Fracture Tool Helsinki (electronic registration device, New Children’s Hospital, Helsinki, Finland and BCB Medical, Turku, Finland). After institutional review board approval (365/13/03/03/2015), the database was searched for paediatric forearm fractures. A total of 79 children under 10 years old that had sustained a closed distal forearm fracture with completely displaced and shortened metaphyseal fracture of the radius (AO 23-M/3.1) were treated in our hospital between 2015 and 2017. In all, 66 of those fractures were reduced (35 reduced and casted; 31 reduced, percutaneously pin fixed and casted). A total of 13 were immobilized in the bayonet position: three patients after attempted reduction by a registrar (operating theatre: one, emergency department: two) and ten random patients without an attempt of reduction in the emergency department according to a decision made by one of four of the eight attending orthopaedic surgeons in our department (Fig. 1a). Neurovascular findings were normal before, during and after casting in all 13 patients, whose fractures were immobilized in the bayonet position. These 13 patients were seen one week from casting to assess that the synthetic splints fit well. None of these 13 children required a cast change during their treatment.
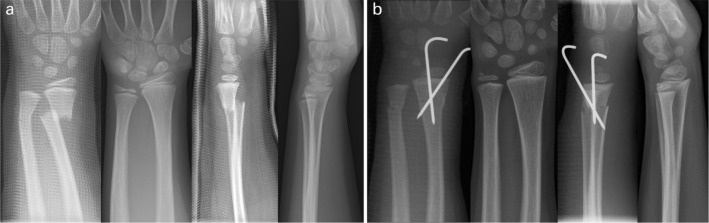
Fig 1.
a) Distal forearm fracture in a five-year-old girl (Table 1, case 3), which was immobilized with synthetic splints (above elbow dorsal and a below elbow volar) applied in finger trap traction leaving the radius in bayonet position. Immobilization was discontinued at four weeks. Complete radiographic remodelling is evident 43 months later; b) a similar distal forearm fracture in another five-year-old boy (Table 1, case 14), which was treated by reduction and pin fixation under general anaesthesia. Synthetic splints and both pins were removed four weeks after surgery. Radiographic result 43 months later.
In all, 11 of the 13 patients whose fractures were not reduced, but were immobilized in the bayonet position, came to a clinical examination and had radiographs of their injured forearms taken. One girl denied attending the clinical examination, but agreed to be interviewed by phone and have her radiographs taken (Table 1, case 5). One five-year old boy, who claimed to have no pain and normal function four years after the fracture, was excluded from the analysis because he refused to attend both the clinical and the radiographic follow-up examinations. We then chose 12 age-matched children that had their completely displaced distal metaphyseal radius fractures reduced and pin fixed, who all agreed to be called-back for research purposes (Fig. 1b). In the 24-patient study population 22 children had different types of associated ulna fractures (greenstick: nine, complete in overriding position: seven, torus: five, physeal: one) with an uneven distribution between the treatment groups (Table 1).
Table 1.
Demographics, fracture type of the associated ipsilateral ulna fracture in 24 prepubertal children with an overriding distal metaphyseal radius fracture. Range of movement and grip strength ratios at mean 3.3-year follow-up. Cases 1 to 12, immobilized in overriding position, and cases 13 to 24 reduced and pin fixed
| Case number | Age, yrs | Sex | Injured side | Ulna fracture type | Length of immobilization* | Pronation | Supination | Extension | Flexion | Grip strength ratio† |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 4.8 | Boy | Left | Greenstick | 30 | 0.98 | 1.13 | 1.03 | 0.99 | 1 |
| 2 | 5.1 | Boy | Left | Overriding | 29 | 1 | 0.91 | 0.94 | 1.02 | 0.88 |
| 3 | 5.4 | Girl** | Left | Greenstick | 31 | 1.07 | 0.83 | 1.08 | 1.1 | 0.88 |
| 4 | 5.8 | Boy | Right | Torus | 30 | 0.85 | 0.88 | 1.08 | 0.97 | 1 |
| 5 | 5.9 | Girl | Left | Torus | 24 | na | na | na | na | na |
| 6 | 6.8 | Girl | Left | Greenstick | 32 | 0.96 | 1.06 | 1.02 | 0.8 | 0.95 |
| 7 | 6.9 | Boy | Left | Greenstick | 24 | 1 | 0.96 | 0.97 | 1.07 | 1 |
| 8 | 7.3 | Boy | Right | Greenstick | 28 | 0.98 | 1.01 | 0.95 | 0.96 | 1 |
| 9 | 7.4 | Girl | Left | Peterson I | 28 | 0.84 | 1 | 0.98 | 0.89 | 1 |
| 10 | 8.6 | Boy | Left | Greenstick | 24 | 0.97 | 0.97 | 1.13 | 1.04 | 1 |
| 11 | 8.6 | Boy | Left | Overriding | 29 | 1.34 | 1.17 | 1.04 | 1.04 | 1.2‡ |
| 12 | 9.9 | Boy‡‡ | Left | Greenstick | 38 | 1 | 0.95 | 0.96 | 0.9 | 0.93 |
| Mean | 28.9 | 1 | 0.99 | 1.02 | 0.98 | |||||
| Median | 29 | 0.98 | 0.97 | 1.02 | 0.99 | |||||
| Range | 24 to 38 | 0.85 to 1.34 | 0.83 to 1.17 | 0.94 to 1.13 | 0.8 to 1.07 | |||||
| 13 | 5 | Girl | Left | Torus | 27 (27) | 1.05 | 1.08 | 1.01 | 0.87 | 0.7 |
| 14 | 5.3 | Boy†† | Left | Overriding | 21 (21) | 1.01 | 0.95 | 1.03 | 1.03 | 1 |
| 15 | 5.8 | Boy | Right | Greenstick | 25 (24) | 0.99 | 0.98 | 1 | 0.94 | 1.14 |
| 16 | 6.2 | Boy | Right | Greenstick | 32 (31) | 1.02 | 0.96 | 0.79 | 0.89 | 1.64 |
| 17 | 6.3 | Boy | Right | Torus | 32 (31) | 0.84 | 1.07 | 0.87 | 1.21 | 1.06 |
| 18 | 6.8 | Boy | Left | No | 33 (31) | 1.06 | 1.13 | 1.11 | 1.02 | 1.13 |
| 19 | 6.8 | Girl | Left | Overriding | 36 (36) | 0.91 | 1.02 | 1.06 | 0.94 | 0.89 |
| 20 | 7.3 | Girl | Left | Overriding | 30 (30) | 0.94 | 1.05 | 1 | 0.99 | 1 |
| 21 | 7.8 | Boy | Right | Overriding | 22 (21) | 0.85 | 0.98 | 1.12 | 0.95 | 1.06 |
| 22 | 8.3 | Boy | Right | Torus | 32 (32) | 1 | 1.01 | 0.95 | 0.99 | 1 |
| 23 | 8.9 | Boy*** | Left | Overriding | 34 (32) | 1.09 | 0.98 | 1 | 1.07 | 0.61 |
| 24 | 9.3 | Boy | Right | No | 45 (35) | 1.02 | 0.82 | 1.08 | 1.01 | 1.17 |
| Mean | 30.8 (39.3) | 0.98 | 1 | 1 | 0.99 | |||||
| Median | 32 (31) | 1 | 0.98 | 1 | 0.99 | |||||
| Range | 21 to 45 (21 to 36) | 0.84 to 1.09 | 0.82 to 1.13 | 0.79 to 1.12 | 0.87 to 1.21 |
Dominant side in bold.
days from injury to cast removal (days from pin fixation to cast removal)
injured/uninjured
sustained right index finger fracture three weeks before follow-up examination
na, not available
Pin fixation (two pins in ten, one pin in two patients) was performed within two days of the injury, except in one child who was operated on ten days after injury because the fracture alignment was regarded as unsatisfactory at one week from injury. Surgery was performed either by an attending surgeon alone (six cases), registrar alone (three cases) or by both attending and registrar (three cases). All 24 patients’ fractures were immobilized with above elbow dorsal- and volar forearm splint. Splints and pins were removed in the outpatient clinic at four weeks, except in one child whose cast and pin were removed at three weeks.
Fracture shortening and angulation were measured from plain radiographs (Fig. 2). The mean shortening of the radius was 5 mm (3 to 9) after cast application in fractures that were immobilized in the overriding position. A total of 11/12 of the operatively treated children’s fractures were reduced anatomically. One fracture was pin fixed in 4-mm dorsal displacement and in 2-mm shortening (Table 1, case 17 ). Mean sagittal plane dorsal angulation in the cast was 6° (2° to 17°) in the nonoperatively treated children. In all, 11 operatively treated patients had dorsal (mean 4° (0° to 11°)) and one volar (3°) angulation. Mean radial angulation in the cast was 8° (0° to 16°) in nonoperatively treated patients and 4° (0° to 6°) after reduction and pin fixation. Angulation of the associated ulna fracture was clearly more pronounced than angulation of the radius in the cast in one five-year old boy with 30° of radial angulation in his ulna and 9° in his radius (Table 1, case 2).
Fig 2.
Angulation was measured in frontal and sagittal planes by measuring the angle between the longitudinal axes (red lines that bisect the width of radius at two reference points) of the radius proximal and distal to the fracture. Shortening was measured from the best available location.
The follow-up appointments for research purposes were arranged at a mean 3.3 years (2.5 to 4.5) from the injury. A professional photographer photographed both forearms (Fig. 3). Two authors (AS and JK) not involved in treatment of the patients, assessed asymmetry and measured forearm and wrist range of movement (ROM) from the photographs, and registered possible axial deformity (Fig. 4) and ulnar variance according to the method of Hafner11 from anteroposterior and lateral radiographs taken in neutral forearm rotation. Grip strength (kg) of both hands was recorded using a hydraulic handheld dynamometer (the Jamar; Lafayette Instrument Company, Lafayette, Indiana) by two different orthopaedic registrars (AS and JK). All the patients were asked to complete the QuickDASH disability/symptom score questionnaire12 (0-100 points, 0 no disability, 100 most severe disability) and the PedsQL Pediatric Pain Questionnaire13 (0 mm to 100 mm, 0 representing no pain and 100 mm worst imaginable pain). Patients who practised sports were also asked to answer the QuickDASH hobby module. Complications from treatment were recorded.
Fig 3.
This nine-year-old girl sustained an overriding distal metaphyseal fracture of her left radius and an associated greenstick type fracture of her left ulna at five years of age (Table 1, case 3). Her fractures were treated with synthetic splints (above elbow dorsal and below elbow volar) leaving the radius fracture displaced in an overriding position: a) forearms, anterior view; b) forearms, dorsal view; c) forearms, ulnar view; d) passive wrist flexion; e) passive wrist extension; f) active pronation; g) active supination; h) active ulnar deviation; i) active radial deviation.
Fig 4.
The two patients’ (Table 1, cases 12 and 23) with the most pronounced radiographic deformity of radius in both treatment groups with 5° of apex volar angulation of the radius (a, b – cast immobilization in bayonet position, c, d – reduction and pin fixation). Both children reported normal pain free upper limb functions at follow-up (three years and 4.4 years, respectively).
Results
At follow-up none of the patients had a visible deformity (Fig. 3). Mean dorsal angulation of the radius at 2.5 to 4.5 years follow-up was 2° in both treatment groups (0° to 5°) (Fig. 4). Six nonoperatively and six operatively treated children had 0° lateral angulation in follow-up radiographs. At 3.3 years follow-up from the injury, the boy whose ulna was immobilized in 30° of radial angulation, had a straight looking radius with a radially 20° curved ulna (Table 1, case 2). Ulnar variance was neutral or negative at follow-up in all 24 cases, with no difference between the treatment groups.
Forearm and wrist ROM showed no significant differences between the method of treatment in both injured and uninjured sides (Table 1). In the affected side of all 24 children the mean recorded pronation was 81° (59° to 120°), supination 112° (79° to 123°), wrist extension 91° (75° to 107°) and wrist flexion 88° (65° to 108°). The grip strengths were equal or higher in the dominant hand in all patients and there was no difference between the treatment groups. Grip strength ratio (injured/uninjured) was ≤ 0.7 in two children that had their non-dominant radius fractures reduced and pin fixed (Table 1).
In terms of the QuickDASH disability/symptom score, 23/24 of the patients scored 0 points and reported no pain in the PedsQL Pediatric Pain Questionnaire. One 11-year-old girl that had her fracture pin fixed scored 4.5 points (scale 0 to 100) in the QuickDASH and reported mild pain (21 mm, scale 0 mm to 100 mm) in the –questionnaire (Table 1, case 19). All patients reported that they had returned to their previous daily and sport activities.
No complications were recorded in the nonoperatively treated patients, whereas 2/12 operatively treated children had complications: one six-year-old boy developed a superficial pin site infection that healed with wound therapy and per oral cephalexin (Table 1, case 17). One seven-year-old boy’s fracture alignment was lost within days after his pin was removed at three weeks from surgery (Table 1, case 21). His fracture malunited in 35° of apex volar angulation. Therefore, a corrective osteotomy was performed five weeks from the fracture.
Discussion
According to the literature, reduction of overriding distal metaphyseal radius fractures in children has been a standard of treatment.1,2 Loss of reduction has been described in 29% to 91% of these fractures during casting.4-6,8,14,15 Both-bone fracture, complete displacement of the distal radius fracture and non-anatomical reduction are risk factors for redisplacement in the cast, according to a meta-analysis by Sengab et al15 recommending reduction and pin fixation of displaced distal radius fractures in paediatric patients regardless of their age. The superiority of reduction and percutaneous pin fixation over reduction and cast-immobilization could not, be proven in a randomized controlled treatment study in ten- to 14-year-old skeletally immature patients with complete fractures of the distal radius metaphysis.6 In this study 7/18 children treated primarily without pins had loss of reduction with re-reduction under anaesthesia in four cases. On the other hand in another study, 6/16 children that had their fractures primarily pinned, developed pin-related complications, of which two were treated under anaesthesia.10 Miller et al10 did not find any significant differences in the costs or in the final outcome between patients treated with casting or with pins. The results of our study support these earlier findings, demonstrating that pin fixation is effective in preventing loss of reduction, also in children younger than ten years old. Pin-related complications (2/12) were less common in our patients than in the study of Miller et al,10. We are not aware of any previous studies comparing reduction and pin fixation to cast immobilization leaving the distal metaphyseal radius fracture in a bayonet position.
Crawford et al3 published a consecutive series of 51 children (three to ten years old) with an overriding distal radius fracture treated without formal reduction. They corrected their patient’s visible axial wrist deformity, but the fractures were left displaced and immobilized in bayonet position with a below elbow cast with good clinical and radiological results at a minimum one-year follow-up. They did not register forearm and wrist ROM or document any patient-reported outcomes, however. We measured forearm rotations and wrist movements from the photographs. The ratio of ROM between injured and uninjured forearms and wrists were similar in both groups, with mean and median values at or close to ratio 1.0 (Table 1).
Do et al1 suggested that 15° of primary angulation and 10 mm of shortening is acceptable in distal forearm fractures in boys < 14 years old and girls < 12 years old. The results of our study support these findings in the prepubertal census population, since up to 17° of dorsal angulation and 9 mm of shortening remodelled well in our patients. The only patient in our series with a clear residual deformity on radiographs at a 3.4-year follow-up was the five-year-old boy who was casted at a radial angulation of 9° in the radius and 30° in the ulna (Table 1, case 2), which is more than Do et al1 and Wilkins2 estimate to remodel. The patient had no visible deformity, however, and despite 12° of supination discrepancy he and his parents were satisfied with the cosmetic and functional result.
The present study had several limitations. The first limitation is the small number of patients in both treatment groups. Secondly, pin fixation was not performed in a uniform way and in one patient the pin was removed at three weeks, one week earlier than in all others. Thirdly, the 12 operatively treated children represent only 39% of all pin fixed patients at our institution during the study period, therefore, the results concerning the quality of pin fixation in our hands should be assessed with caution. Fourthly, the two treatment groups were not homogenous concerning the type of associated ulna fracture, which may have influenced the outcome. Fifthly, we did not arrange routine follow-up for the patients after cast and pin removal and Kirschner-wire removal and thus possible differences in early recovery between the treatment groups could not be evaluated. Furthermore, the method used in our study to measure active forearm rotation is not completely accurate, since it is difficult to control children to keep their wrists in a neutral position during the assessment. The bimanually self-tested passive wrist extension and flexion in our study is also susceptible to error and potentially a too low maximum value for the wrist with better ROM was recorded. The absolute values of forearm and wrist ROM were, however, good; it is doubtful that a more accurate measuring method would have given clinically more valuable data. This assumption is supported by the fact that all but one surgically-treated child reported no functional restrictions at follow-up in the QuickDASH nor pain in the PedsQL. The strength of this study is the very high follow-up rate, with 23/24 (patients seen in the outpatient clinic at 2.5 to 4.5 years after treatment). One patient was interviewed by phone and agreed to attend the radiographic follow-up, but declined the clinical examination because according to his parents’ assessment he had made a full functional recovery of his injury (Table 1, case 5). This is to our knowledge the first study comparing subjective, functional and radiographic results of cast immobilization without formal reduction and pin fixation in distal metaphyseal radius fractures in children.
Conclusions
The results of this study do not demonstrate the superiority of reduction and pin fixation over cast immobilization in the bayonet position of closed overriding distal metaphyseal radius fractures in children under ten years with normal neurovascular findings. Pin fixation requires anaesthesia, involves a risk of infection and necessitates pin removal. A randomized controlled trial is warranted to verify the results of this study.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional committee and with the 1964 Helsinki declaration and its later amendments of comparable ethical standards. This study received no financial support.
Informed consent: Informed consent was obtained from all individual participants included in the study.
ICMJE Conflict of interest statement
None declared.
Author Contributions
TL: Study design, Data acquisition, Manuscript preparation.
JP: Study design, Manuscript preparation.
AS: Study design, Data acquisition, Manuscript preparation.
JK: Study design, Data acquisition, Manuscript preparation.
MA: Manuscript preparation.
YN: Study design, Manuscript preparation.
References
- 1. Do TT, Strub WM, Foad SL, Mehlman CT, Crawford AH. Reduction versus remodeling in pediatric distal forearm fractures: a preliminary cost analysis. J Pediatr Orthop B 2003;12:109-115. [DOI] [PubMed] [Google Scholar]
- 2. Wilkins KE. Principles of fracture remodeling in children. Injury 2005;36(suppl 1):A3-A11. [DOI] [PubMed] [Google Scholar]
- 3. Crawford SN, Lee LS, Izuka BH. Closed treatment of overriding distal radial fractures without reduction in children. J Bone Joint Surg [Am] 2012;94-A:246-252. [DOI] [PubMed] [Google Scholar]
- 4. CLMH Gibbons, Woods DA, Pailthorpe C, Carr AJ, Worlock P. The management of isolated distal radius fractures in children. J Pediatr Orthop 1994;14:207-210. [DOI] [PubMed] [Google Scholar]
- 5. Choi KY, Chan WS, Lam TP, Cheng JC. Percutaneous Kirschner-wire pinning for severely displaced distal radial fractures in children. A report of 157 cases. J Bone Joint Surg [Br] 1995;77-B:797-801. [PubMed] [Google Scholar]
- 6. McLauchlan GJ, Cowan B, Annan IH, Robb JE. Management of completely displaced metaphyseal fractures of the distal radius in children. A prospective, randomised controlled trial. J Bone Joint Surg [Br] 2002;84-B:413-417. [DOI] [PubMed] [Google Scholar]
- 7. Miller BS, Taylor B, Widmann RF, et al. Cast immobilization versus percutaneous pin fixation of displaced distal radius fractures in children: a prospective, randomized study. J Pediatr Orthop 2005;25:490-494. [DOI] [PubMed] [Google Scholar]
- 8. Zamzam MM, Khoshhal KI. Displaced fracture of the distal radius in children: factors responsible for redisplacement after closed reduction. J Bone Joint Surg [Br] 2005;87-B:841-843. [DOI] [PubMed] [Google Scholar]
- 9. Hang JR, Hutchinson AF, Hau RC. Risk factors associated with loss of position after closed reduction of distal radial fractures in children. J Pediatr Orthop 2011;31:501-506. [DOI] [PubMed] [Google Scholar]
- 10. Miller BS, Taylor B, Widmann RF, et al. Cast immobilization versus percutaneous pin fixation of displaced distal radius fractures in children: a prospective, randomized study. J Pediatr Orthop 2005;25:490-494. [DOI] [PubMed] [Google Scholar]
- 11. Kox LS, Jens S, Lauf K, et al. Well-founded practice or personal preference: a comparison of established techniques for measuring ulnar variance in healthy children and adolescents. Eur Radiol 2020;30:151-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Beaton DEWright JG, Katz JN, Upper Extremity Collaborative Group , . Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg [Am] 2005;87-A:1038-1046. [DOI] [PubMed] [Google Scholar]
- 13. Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care 1999;37:126-139. [DOI] [PubMed] [Google Scholar]
- 14. Colaris JW, Allema JH, Biter LU, et al. Re-displacement of stable distal both-bone forearm fractures in children: a randomised controlled multicentre trial. Injury 2013;44:498-503. [DOI] [PubMed] [Google Scholar]
- 15. Sengab A, Krijnen P, Schipper IB. Risk factors for fracture redisplacement after reduction and cast immobilization of displaced distal radius fractures in children: a meta-analysis. Eur J Trauma Emerg Surg 2020;46:789-800. [DOI] [PMC free article] [PubMed] [Google Scholar]