Abstract
Purpose
In myelomeningocele, several classifications have been used. The present manuscript proposes a new functional classification to better assess the prognosis and management of these patients.
Methods
The manual muscle test is what defines the actual group in which the patient should be included. Furthermore, this new classification brings information about the bracing and external supports recommended to each functional level. We also recommend that the patient’s Functional Mobility Scale should always be mentioned together with their functional level.
Results
The four levels in this classification are MMFC1, MMFC2, MMFC3 and MMFC4. The MMFC1 group includes patients with significant muscle weakness. They need to use high braces crossing the hip joint with a walker to achieve some ambulation. The MMFC2 group includes patients who have functional hip flexors, knee extensors and knee flexors. However, the hip abductors are quite weak. These patients usually need to use a walker - or crutches - and Ankle-Foot Orthosis (AFOs). The MMFC3 group includes patients with functional hip flexors, knee extensors, knee flexors and hip abductors. However, the ankle plantar flexion function is absent. Most of them are able to walk independently, only using AFOs without any external support. The MMFC4 group includes patients who have preserved function in the entire lower limb musculature. These patients don’t need any assistive devices to achieve an adequate ambulation pattern.
Conclusions
We hope that this new classification is a system that is simple to understand, serves as a gait prognosis guide and facilitates communication among healthcare professionals.
Level of evidence
V
Keywords: myelomeningocele, spina bifida, classification, ambulatory function, functional mobility scale
Introduction
In orthopaedic surgery, several classifications have been created to facilitate the understanding of diseases and the communication among surgeons and healthcare professionals. An effective classification system must be easy to understand, have a good inter- and intraobserver reliability, predict prognosis and be able to guide treatments.1-6
In paediatric orthopaedics, several classification systems have been used successfully. For example, for Legg-Calvé-Perthes, the lateral pillar classification by Herring et al7,8 has four easy-to-reproduce groups that efficiently assist communication between surgeons and predict prognosis. For proximal femoral focal deficiency, Aitken9 proposed a classification into four groups, which is easy to interpret and also helps the surgeon in terms of prognosis and choice of treatment.
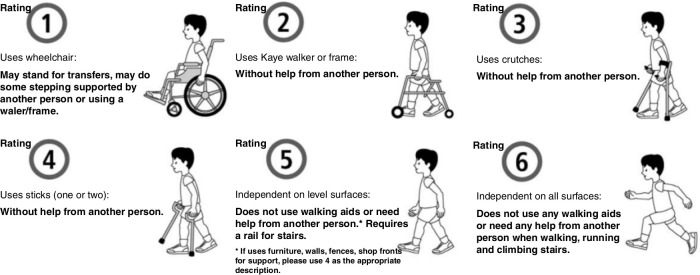
Within the neuromuscular population, two important functional classification scales have been introduced: the Gross Motor Function Classification System10 and the Functional Mobility Scale (FMS)11 (Fig. 1). These classifications are simple to interpret, have great prognostic value and are helpful in the formulation of the treatment plan.
Fig 1.
Functional Mobility Scale (FMS) classification patients rated at 5 m (e.g. home), 50 m (e.g. school) and 500 m (e.g. shopping mall). A rating of 1, 2, 3, 4, 5 or 6 is given for each distance (reproduced with permission from Kerr Graham)21
For the diagnosis of myelomeningocele (spina bifida), several classification systems have been created in an attempt to classify the different clinical and anatomical aspects of the disease.12-18 Sharrard,12 Lindseth,17 Ferrari et al18 and Broughton et al14 have all developed classification systems dividing patients into seven to nine subgroups, using the anatomical terms thoracic, lumbar and sacral. Hoffer et al13 proposed a division of patients with myelomeningocele into four functional categories: community ambulator, household ambulator, nonfuctional ambulator and nonambulator. McDonald et al15 proposed a classification system to predict patients’ ability to walk from the assessment of muscle strength. Bartonek et al19 published a review of these classification systems and concluded that there was incompatibility between the anatomically based and the functional ambulation-based classifications. In other words, the same lesion levels described in the different classifications do not correlate to the actual ambulatory function of the patients. It is important to mention that Bartonek et al19 did not include the classifications proposed by Schafer and Dias20 in 1983 and Swank and Dias16 in 1994 in the analysis.
In 2009, our group proposed the use of a functional classification combined with the FMS (Table 1).11,21 This system is inclusive of the muscles that are strong, the types of external support and braces that are indicated for each functional level, as well as the distance that the patient might be able to walk. The inclusion of the FMS scale within a myelomeningocele classification system allows for the quantification of the patient’s functionality, which helps the healthcare team communication and understanding of the disease evolution in every single patient.
Table 1.
Swaroop and Dias Spina Bifida classification (2009)22 (adapted with permission from L. S. Dias)
| Group | Level of lesion | Functional hallmark | Ambulatory capacity | FMS classification |
|---|---|---|---|---|
| 1 | Thoracic, high-lumbar | Lack quadriceps function | As children, require hip-spanning orthosis for ambulation (RGO, HKAFO) In adulthood, majority require wheelchair for mobility |
FMS 1,1,1 |
| 2 | Low-lumbar | Lack gluteus medius and maximus function Retain quadriceps and medial hamstring function |
Require crutches and AFOs for ambulation Most retain community ambulation as adults |
FMS 3,3,1 |
| 3 | Sacral | Retain quadriceps and gluteus medius function | FMS 6,6,6 | |
| High-sacral | Lack gastrocnemius-soleus function | Ambulate with AFOs and no support | ||
| Low-sacral | Retain gastrocnemius-soleus function | Ambulate without braces or support |
FMS, Functional Mobility Scale; RGO, Reciprocating Gait Orthosis; HKAFO, Hip-Knee-Ankle-Foot Orthosis; AFO, Ankle-Foot Orthosis
While there are many published classifications for myelomeningocele, there is not one unifying or universal system that integrates qualitative and quantitative information about the functionality level of each patient. Based on an adaptation of our last classification system,22 which Rethlefsen et al23 has shown to have excellent correlation with the patient’s ambulatory function, we propose a new classification that can provide the gait prognosis, facilitates patient care decision-making process and enhances communication among healthcare professionals.
Materials and methods
Our clinical experience of over 45 years suggests that an ideal classification system for myelomeningocele should:
reflect the functional capacity of the patient;
have few classification levels;
avoid anatomical nomenclature.
We propose the inclusion of the assessment of muscle strength based on the manual muscle test24 (MMT), ideally done by a physiotherapist. This evaluation is what defines the actual level in which the patient should be included. Based in our experience in gait analysis in the last 30 years, the muscle evaluated is considered functional if its strength is greater than or equal to 3, except for the medial hamstrings and the gluteus medius, which are considered functional if muscle strength is greater than or equal to 2. Thus, the muscle is considered functional if it is able to assist in some way in the patient’s gait. Furthermore, this new classification brings information about the bracing and external supports recommended to each functional level.
To facilitate communication, we suggest some changes in how to express the patient’s functional level. Instead of using the anatomical level of the spinal cord lesion, as has been done before by several authors,12,15,16,22 we propose the use of a numerical graduation from 1 to 4. Because healthcare professionals tend to abbreviate the term myelomeningocele using the acronym ‘MM’, the four levels in this classification are MMFC1, MMFC2, MMFC3 and MMFC4 (i.e. Myelomeningocele Functional Classification). We also recommend that the patient’s FMS11 should always be mentioned together with their functional level.
It is relevant to mention that this classification system is dynamic. It may change due to tethered cord complications, shunt malfunction followed by infection and severe orthopaedic deformities that prevent the use of braces.21,23,25,26
Therefore, the classification should be as follows (Table 2).
Table 2.
The Myelomeningocele Functional Classification (MMFC)
| Group | Functional hallmark | FMS classification | Assistive devices |
|---|---|---|---|
| MMFC1 | Might retain iliopsoas function or not Lack quadriceps function |
Maximum 2,2,1 | - Walker - Hip Spanning Orthoses (RGO or HKAFO) - Wheelchair for long distances |
| MMFC2 | Retain quadriceps and medial hamstrings function Lack gluteus medius function |
Maximum 3, 3, 3 | - Walker or Crutches - HKAFOs or AFOs |
| MMFC3 | Retain quadriceps and gluteus medius function Lack gastrocnemius-soleus function |
Maximum 5, 5, 5 | - No external support - AFOs only |
| MMFC4 | Retain quadriceps and gluteus medius function Retain gastrocnemius-soleus function |
Maximum 6, 6, 6 | - No external support - SMOs, insoles or nothing |
FMS, Functional Mobility Scale; RGO, Reciprocating Gait Orthosis; HKAFO, Hip-Knee-Ankle-Foot Orthosis; AFO, Ankle-Foot Orthosis; SMO, Supramalleolar Orthosis
Results
MMFC1
This group includes patients with significant muscle weakness. The hip flexor strength, represented by the iliopsoas muscle, may be present, but these patients do not have significant quadriceps strength. They need to use a Reciprocating Gait Orthosis or a Hip-Knee-Ankle-Foot Orthosis to achieve some ambulation. Most of them will need a walker as an external support, and some might be able to use even crutches depending on their level of coordination and balance.27 However, some may be unable to walk due to a poor sitting balance.20
Regarding the FMS, most of them will be 2/2/1 when young, i.e. under the age of 11 years old. As they gain weight and get older, which results in high energy cost for ambulation, they might become 2/1/1 and, invariably, by the age of 11 to 13 years old, they will become 1/1/1. Few exceptions are seen. For example, the senior author (LD) knows at least three MMFC1 patients that are FMS 3/3/1.
Our clinical experience suggests that patients can be classified within this level as early as birth when the newborn child shows no active movement of the entire lower limbs.
MMFC2
This group includes patients who have preserved hip flexor and knee extensor strength. The medial hamstrings present, at least, a muscle strength grade 2, which prevents excessive anterior pelvic tilt.27 However, the function of the hip abductors, represented by the gluteal muscles, is not significant, i.e. less than grade 2 on MMT. These patients need to use a walker and Ankle-Foot Orthosis (AFOs) usually before the age of four, and crutches and AFOs thereafter. As the hip abductors strength is not present, it is very unusual for these patients to achieve a good ambulation pattern without using an external support.27 For these children, the effectiveness of the ambulation pattern could be best determined by an instrumented gait analysis evaluation.
Regarding the FMS, most of them will be 3/3/3, 3/3/2 or 3/3/1 when young, usually before the age of 13. As they get older and gain some weight, they might become 3/2/1, 2/2/1 or 2/1/1.
Based on our experience, we cannot predict with certainty this functional level until the patient is at least four years old.
MMFC3
This group includes patients with preserved hip flexor strength, knee extensor and flexor strength and hip abductors strength, represented mainly by the gluteus medius function. However, the ankle plantar flexion function, represented by the gastrocnemius and soleus muscles, is absent. Most of them are able to walk independently, only using AFOs without any external support. However, depending on the degree of their gluteus lurch, a few might benefit from the use of crutches for long distances.27
Regarding the FMS, most of them are 5/5/5, 5/5/3 or 5/3/3. As adults, they might become 5/5/1 or 5/3/1.
Similar to the MMFC2, this level cannot be predicted until the age of four. An instrumented gait analysis should be recommended to evaluate their ambulatory status.
MMFC4
This group includes patients who have preserved function in the entire lower limb musculature, including the ankle plantar flexors. These patients don’t need any assistive devices to achieve an adequate ambulation pattern. However, some might benefit from the use of a Supramalleolar Orthosis or insoles to maintain a good foot alignment.
Regarding the FMS, they are 6/6/6.
Similar to the MMFC1, this level can be predicted in the newborn period.
Discussion
Several classifications for myelomeningocele have been developed in the past but there is no clear agreement among the anatomical levels proposed by these different classification systems.19 It should also be noted that many of these classifications do not take into account the patient’s functional capacity as the main factor.4,19,23,28,29 When referring to a patient with lumbar myelomeningocele, for example, the reader may not understand exactly which of the numerous lumbar levels already proposed the author refers to.12,15,16 Also, the patients’ grouping by anatomical level can generate misunderstandings, since, for example, several lumbar level patients may have different functional levels. Thus, within the same anatomical group, we can include patients who have no gait prognosis and patients who can walk without assistive devices.
As previously mentioned, Rethlefsen et al23 demonstrated that the anatomical classifications, like the International Myelodysplasia Study Group’s functional neurological level and lesion level on radiograph findings, were less descriptive of ambulatory mobility than our functional classification,22 which is based on muscle function, braces and assistive devices used.
Furthermore, in 2015, Bisaro et al30 showed that there are at least 19 measures that have been used to examine walking in children with myelomeningocele, and that there is still no system that is universally used to categorize the ability to walk in these patients. This hinders communication among healthcare professionals, prevents the formulation of standard treatment guidelines and undermines the performance of systematic reviews to assess the results of treatments performed in this population.
We believe that the functional classification, using a numerical scale in conjunction with the FMS, is efficient in predicting gait prognosis, assisting in management decisions and facilitating communication among healthcare professionals. For example, when referring to a six-year-old boy that has a grade 3 gluteus medius strength but does not have strength in the plantar flexors, and can walk independently at home and school using only AFOs, but needs crutches for long distances, we would classify him as an MMFC3 - FMS 5/5/3.
In addition, information about the maximum level expected in the FMS and the recommendations about the assistive devices provide practical guidelines for less experienced professionals. This can improve the understanding of the gait prognosis of each functional level and the counselling of family members regarding the ability to walk expected for each child.
Our clinical experience suggests that this scaling approach is dynamic in nature. The functional level can change with time, as mentioned before, due to several factors like tethered cord syndrome, shunt malfunction and severe orthopaedic deformities.21,25,26 One should always be aware that classification level changes may be a sign of a complication, which should require additional investigation.
In conclusion, as demonstrated earlier,16,19,22,23,30 the best classification systems rely on a functional grouping. This is even more essential in myelomeningocele, since what guides the patient’s treatment is their functional capacity and not the anatomical level of their spinal cord lesion. We hope that this new functional classification brings a system that is simple to understand, easy to apply in clinical practice, serve as a gait prognosis guide and facilitates communication among healthcare professionals, generating a positive impact in patients’ care.
OA licence text
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: This work did not involve human participants and/or animals.
Informed consent: No informed consent was required.
ICMJE Conflict of interest statement
None declared.
Author Contributions
LSD: Study design, Manuscript preparation, Manuscript review.
VTS: Study design, Manuscript preparation, Manuscript review.
LRAdA: Manuscript preparation, Manuscript review.
JEL: Manuscript preparation.
A-MR: Manuscript preparation.
TK: Manuscript preparation, Manuscript review.
References
- 1. Kural C, Sungur I, Kaya I, et al. Evaluation of the reliability of classification systems used for distal radius fractures. Orthopedics 2010;27:801. [DOI] [PubMed] [Google Scholar]
- 2. Ilyas AM, Jupiter JB. Distal radius fractures—classification of treatment and indications for surgery. Orthop Clin North Am 2007;27:167-173. [DOI] [PubMed] [Google Scholar]
- 3. Cheng J, Liu P, Sun D, et al. Reliability and reproducibility analysis of the AOSpine thoracolumbar spine injury classification system by Chinese spinal surgeons. Eur Spine J 2017;27:1477-1482. [DOI] [PubMed] [Google Scholar]
- 4. Rethlefsen SA, Ryan DD, Kay RM. Classification systems in cerebral palsy. Orthop Clin North Am 2010;27:457-467. [DOI] [PubMed] [Google Scholar]
- 5. Lenarz CJ, Place HM, Lenke LG, Alander DH, Oliver D. Comparative reliability of 3 thoracolumbar fracture classification systems. J Spinal Disord Tech 2009;27:422-427. [DOI] [PubMed] [Google Scholar]
- 6. Penteado FT, Dos Santos JB, Caporrino FA, et al. Scaphoid nonunion advanced collapse classifications: a reliability study. J Hand Microsurg 2012;27:12-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Herring JA, Neustadt JB, Williams JJ, Early JS, Browne RH. The lateral pillar classification of Legg-Calvé-Perthes disease. J Pediatr Orthop 1992;27:143-150. [DOI] [PubMed] [Google Scholar]
- 8. Herring JA, Hui TK, Browne R. Legg-Calvé-Perthes disease. Part II: Prospective multicenter study of the effect of treatment on outcome. J Bone Joint Surg [Am] 2004;86-A:2121-2134. [PubMed] [Google Scholar]
- 9. Aitken G. Proximal femoral focal deficiency: a congenital anomaly. : Aitken G, . A symposium on proximal femoral focal deficiency: a congenital anomaly. Washington, DC: National Academy of Sciences, 1969. [Google Scholar]
- 10. Palisano R, Rosenbaum P, Walter S, et al. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 1997;27:214-223. [DOI] [PubMed] [Google Scholar]
- 11. Graham HK, Harvey A, Rodda J, Nattrass GR, Pirpiris M. The Functional Mobility Scale (FMS). J Pediatr Orthop 2004;27:514-520. [DOI] [PubMed] [Google Scholar]
- 12. Sharrard WJ. The segmental innervation of the lower limb muscles in man. Ann R Coll Surg Engl 1964;27:106-122. [PMC free article] [PubMed] [Google Scholar]
- 13. Hoffer MM, Feiwell E, Perry R, Perry J, Bonnett C. Functional ambulation in patients with myelomeningocele. J Bone Joint Surg [Am] 1973;55-A:137-148. [PubMed] [Google Scholar]
- 14. Broughton NS, Menelaus MB, Cole WG, et al. The natural history of hip deformity in myelomeningocele. J Bone Joint Surg [Br] 1993;75-B:760-763. [DOI] [PubMed] [Google Scholar]
- 15. McDonald CM, Jaffe KM, Mosca VS, Shurtleff DB. Ambulatory outcome of children with myelomeningocele: effect of lower-extremity muscle strength. Dev Med Child Neurol 1991;27:482-490. [DOI] [PubMed] [Google Scholar]
- 16. Swank M, Dias LS. Walking ability in spina bifida patients: a model for predicting future ambulatory status based on sitting balance and motor level. J Pediatr Orthop 1994;27:715-718. [PubMed] [Google Scholar]
- 17. Lindseth RE. Treatment of the lower extremity in children paralyzed by myelomeningocele (birth to 18 months). Am Acad Orthop Surg Instr Course Lect 1976;27:76-82. [Google Scholar]
- 18. Ferrari A, Boccardi S, Licari V. La stazione eretta ed il cammino nella spina bifida. In: Proceedings from the 14 meetings of the Italian Society of Physical Medicine and Rehabilitation. Ferrara. Liviana Editrice, Padova. 1985:167-204. [Google Scholar]
- 19. Bartonek A, Saraste H, Knutson LM. Comparison of different systems to classify the neurological level of lesion in patients with myelomeningocele. Dev Med Child Neurol 1999;27:796-805. [DOI] [PubMed] [Google Scholar]
- 20. Schafer M, Dias L. Myelomeningocele, orthopaedic treatment. Baltimore, MD: Lippincott Williams & Wilkins, 1983. [Google Scholar]
- 21. Battibugli S, Gryfakis N, Dias L, et al. Functional gait comparison between children with myelomeningocele: shunt versus no shunt. Dev Med Child Neurol 2007;27:764-769. [DOI] [PubMed] [Google Scholar]
- 22. Swaroop VT, Dias L. Orthopedic management of spina bifida. Part I: hip, knee, and rotational deformities. J Child Orthop 2009;27:441-449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rethlefsen S, Mueske N, Wren T. Classifications of motor level in myelomeningocele: are they indicative of ambulatory function? In: Special Issue: Abstracts for the 73rd American Academy for Cerebral Palsy and Developmental Medicine, 18-21 September 2019 . Dev Med Child Neurol 2019;61-S3:8-9. [Google Scholar]
- 24. Hislop JH, Avers D, Brown M, et al. Daniels and Worthingham’s muscle testing: techniques of manual examination and performance testing. 9th ed. St. Louis, MO: Elsevier/Saunders, 2014. [Google Scholar]
- 25. Swaroop VT, Dias L. Orthopaedic management of spina bifida-part II: foot and ankle deformities. J Child Orthop 2011;27:403-414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Shields LBE, Mutchnick IS, Peppas DS, et al. Importance of physical examination and imaging in the detection of tethered cord syndrome. Glob Pediatr Heal 2019;27:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Vankoski S, Moore C, Statler KD, Sarwark JF, Dias L. The influence of forearm crutches on pelvic and hip kinematics in children with myelomeningocele: don’t throw away the crutches. Dev Med Child Neurol 1997;27:614-619. [DOI] [PubMed] [Google Scholar]
- 28. Farmer DL, Thom EA, Brock JW III, et al. The Management of Myelomeningocele Study: full cohort 30-month pediatric outcomes. Am J Obstet Gynecol 2018;27:256.e1-256.e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Adzick NS, Thom EA, Spong CY, et al. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med 2011;27:993-1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bisaro DL, Bidonde J, Kane KJ, Bergsma S, Musselman KE. Past and current use of walking measures for children with spina bifida: a systematic review. Arch Phys Med Rehabil 2015;27:1533-1543.e31. [DOI] [PubMed] [Google Scholar]