Abstract
Purpose
To assess the reliability and efficacy of the modified oblique high tibial osteotomy for correction of complex deformity in adolescent tibia vara.
Methods
A total of 19 patients (25 legs) with adolescent tibia vara were enrolled in this study. There were 16 male (84.2%) and three female (15.8%) patients who had modified Rab oblique osteotomy with minimal fixation performed. The age of the patients at time of surgery ranged from 12 years to 30 years (mean 17.23 (sd 5.27)). The body mass index ranged from 22 kg/m2 to 42 kg/m2 (mean 32.05 (sd 6.13)). All patients were followed up for over two years (mean 3.4; 2 to 5).
Results
The femoro-tibial angle was improved from -34° to -12° (mean -20.04° (sd 5.24°) preoperatively and from -12° to 7°, postoperatively (mean 2.04° (sd 4.07)). Medial deviation of the mechanical axis corrected from 38 mm to 125 mm (mean 76.13 (sd 23.29)) preoperatively to 0 mm to 36 mm (mean 5.74 (sd 7.3)) postoperatively. The time needed to achieve union ranged from eight weeks to 16 weeks (mean 10.2 (sd 2.42)). According to the Lysholm functional knee score scale, there were 15 excellent (78.9%), two good (10.5%), one fair (5.2%) and one poor (5.2%) after correction of the deformity.
Conclusion
Modified Rab osteotomy with minimal fixation by two or three screws shows promising results with good correction of varus deformity (coronal plane), internal torsion (axial plane) and procurvatum (sagittal plane), in management of adolescent tibia vara with minimal morbidity and complications.
Level of evidence
IV
Keywords: tibia vara, Blount, Rab osteotomy, oblique osteotomy, angular deformity
Introduction
Genu varum is an angular deformity of the lower limb characterized by medial deviation of the mechanical axis in the coronal plane, that potentiates the development of degenerative arthritis of the knee.1
Genu varum may be an isolated deformity or part of a complex deformity in different planes. Tibia vara (Blount’s disease) is a complex deformity of the proximal tibia composed of varus deformity in the coronal plane, internal tibial torsion in the transverse plane and procurvatum in the sagittal plane.2
In 1988 George Rab3 described the oblique proximal tibial osteotomy as a surgical option for the correction of deformity associated with the infantile tibia vara (Blount’s disease), especially when a significant internal tibial torsion is present. In 2010,4 a theoretical modification of oblique high tibial osteotomy was published by Rab in correction of infantile tibia vara. In 2012, Elzohairy5 applied the modified Rab osteotomy for correction of infantile tibia vara as a case series.
The aim of this study is to evaluate the efficiency, advantages, disadvantages and possible complications that may occur with acute correction of adolescent tibia vara using a modified Rab osteotomy (a single oblique high tibial osteotomy) as a case series study, not a theoretical study.
The tibial osteotomy is directed from the anteromedial cortex distally to the posterolateral cortex proximally, and a minimal fixation is done using two or three screws.
Patients and Methods
This study is a prospective case series study, conducted on 19 patients (25 legs) with adolescent tibia vara. A total of 16 male (84.2%) and three female (15.8%) patients were enrolled in this study. The mean age at time of surgery was 17.23 years (sd 5.27; 12 to 30). The affected limb was the right in six cases (24%), the left in seven cases (28%) and bilateral in six cases (48%). The body mass index (BMI) ranged from 22 kg/m2 to 42 kg/m2 (mean 32.05 (sd 6.13)). All patients were followed up for over two years, for a mean of 3.4 years (2 to 5).
The common complaint of our patients is limping, knee pain during walking and activities, sense of instability (lateral thrust) especially with severe deformities and difficulty in using stairs.
All of our patients were evaluated preoperatively by clinical examination and radiologically using standard weight-bearing (anteroposterior and lateral long radiographs of both lower extremities) from hip to ankle with patella facing forward. Mechanical axis deviation, the femoro-tibial angle, the medial proximal tibial angle (MPTA), the posterior proximal tibial angle (PPTA) and the angle of medial tibial plateau depression were measured (Table 1).6 Assessment of internal tibial torsion was done by measuring the foot thigh angle in the prone position, as described by Staheli’s profile,7 both preoperatively and at latest follow-up.
Table 1.
Preoperative and postoperative tibia vara data of the studied cases (n = 25)
| Preoperative mean (sd; range) | Postoperative mean (sd; range) | |
|---|---|---|
| Femero-tibial angle, ° | -20.04 (5.24; -34 to -15) | 2.04 (4.07; -12 to 7) |
| MAD, mm | 76.13 (23.29; 38 to 125) | 5.74 (7.3; 0 to 36) |
| MPTA, ° | 75.57 (3.29; 67 to 81) | 87.96 (3.05; 78 to 90) |
| LDTA, ° | 87.52 (3.23; 79 to 93) | 87.04 (1.77; 83 to 90) |
| PPTA, ° | 77.48 (8.5; 60 to 87) | 82.65 (2.66; 79 to 87) |
| Rotation, ° | -20.22 (7.71; -30 to -5) | 5.65 (3.42; -5 to 12) |
| LDFA, ° | 87.09 (1.62; 85 to 90) | 86.83 (1.34; 85 to 90) |
MAD, mechanical axis deviation; MPTA, medial proximal tibial angle; LDTA, lateral distal tibial angle; PPTA, posterior proximal tibial angle; LDFA, lateral distal femoral angle
All of our patients were assessed functionally according to the Lysholm knee scoring scale.7 The scale consists of a questionnaire that includes eight items: 1) limp; 2) support; 3) locking; 4) instability; 5) pain; 6) swelling; 7) stair climbing; and 8) squatting.
All of our patients filled out the questionnaire both preoperatively and six months postoperatively. There was a significant improvement in the functional scale after correction of the deformity (Table 2).
Table 2.
Significant improvement in the functional scale of the patients after correction of the deformity.
| Outcomes | All patients (n = 19) | Bilateral (n = 6) | Unilateral (n = 13) |
|---|---|---|---|
| Preoperative, n (%) | |||
| Excellent | 2 (10.53) | 0 (0) | 2 (15.38) |
| Good | 3 (15.79) | 2 (33.33) | 1 (7.69) |
| Fair | 9 (47.37) | 2 (33.33) | 7 (53.85) |
| Poor | 5 (26.32) | 2 (33.33) | 3 (23.08) |
| Postoperative, n (%) | |||
| Excellent | 15 (78.95) | 5 (83.33) | 10 (76.92) |
| Good | 2 (10.53) | 1 (16.67) | 1 (7.69) |
| Fair | 1 (5.26) | 0 (0) | 1 (7.69) |
| Poor | 1 (5.26) | 0 (0) | 1 (7.69) |
| p-value | < 0.001 | 0.025 | 0.013 |
Patients who had a medial tibial plateau depression, were aged < 11 years old, had congenital or metabolic anomalies that affected the growth of the diseased extremity, had previous surgery of the affected limb and any other aetiology for varus deformity were excluded from this study.
Surgical technique
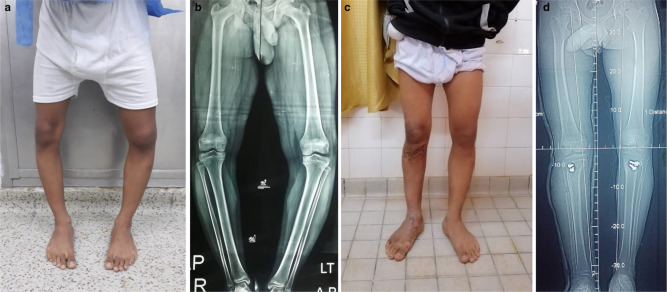
As described by Rab,4 an oblique incision was made beginning from the medial joint line in the mid-medial line and directed 45° laterally and inferiorly to end in the mid-lateral line (Fig. 1). Fibular osteotomy was done from the same incision (at the distal-most portion of the oblique incision) with excision of 1 cm to 2 cm, which allows safer and easier correction especially for a larger degree.
Fig. 1.
a) The incision for oblique proximal tibial osteotomy allows access to the medial tibial physis and lateral exposure for fibular osteotomy;4 b) intraoperative photography of the incision.
Internal rotation of the leg was done until the patella was facing up, then a small Steinmann pin was placed at the same angle of osteotomy that was estimated simply from the preoperative radiograph. Fortunately, all of our patients had equal degree of varus and internal tibial torsion, so the Steinmann pin was placed at 45°, which was appropriate for complete clinical correction. The pin was directed from the anteromedial cortex distally to the posterolateral cortex proximally, starting 1 cm below the tibial tubercle.
The nomogram provides a quick estimation of the osteotomy angle (° angle), if a different degree between external rotation and valgus correction are required. The θ angle ranged from 30° to 60° (mean 45.4° (sd 8.25°)).
The osteotomy cut was made immediately beneath the pin using the oscillating saw. The blade of the saw should be collinear to the ankle and not the knee; this will improve the PPTA and decrease the procurvatum.
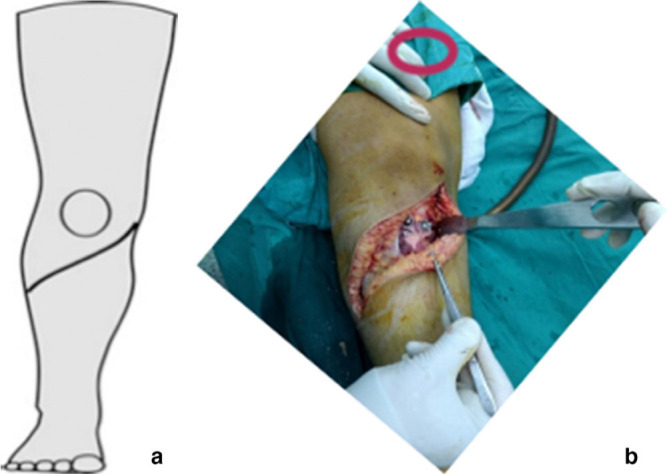
After the osteotomy was completed, sliding of the two faces of the osteotomy will correct the internal torsion (axial plane), varus deformity (coronal plane) and procurvatum (sagittal plane). Final fixation by two or three cortical solid 4.5-mm screws was done from anterior to posterior (Fig. 2).
Fig. 2.

Radiograph anteroposterior and lateral views of adolescent tibia vara, corrected by modified high tibial osteotomy and fixed by two screws directed from anterior to posterior.
Closure in layers without a drain was performed, and then long above knee cast had been used for all of our cases.
Postoperatively, all of our patients were followed up clinically and radiologically at two, four, six and eight weeks, then at every three months. The cast was applied for eight weeks or until union was evident radiographically. The time to union ranged from eight weeks to 16 weeks (mean 10.2 (sd 2.42)).
Results
The femoro-tibial angle was improved from a mean of -20.04° (sd 5.24°; -34° to -12°) preoperatively, to 2.04° (sd 4.07°; -12° to 7°) postoperatively. Medial deviation of the mechanical axis corrected from a mean of 76.13 mm (sd 23.29; 38 to 125) preoperatively, to 5.74 mm (sd 7.3; 0 to 36) postoperatively. The mean preoperative MPTA was measured as 75.57° (sd 3.29°; 67° to 81°) compared with a mean postoperative MPTA that was improved to 87.96° (sd 3.05°; 78° to 90°).
The internal tibial torsion was improved from a mean -20.22° (sd 7.71°; -30° to -5°) preoperatively, to 5.65° (sd 3.42°; -5° to 12°) postoperatively. Mean PPTA was 77.48° (sd 8.5°; 60° to 87°) preoperatively, and tibial slope was improved to a mean of 82.65° (sd 2.66°; 79° to 87°) postoperatively (Table 1).
We correlated the time of union to rotational degree, angular degree and BMI. There was insignificant correlation between the time to achieve union and rotational difference (r = -0.108; p = 0.312). There was no significant correlation with angular difference (r = 0.141; p = 0.26), while there was a significant correlation between time to union and BMI (r = 0.4; p = 0.029).
By a simple linear regression analysis, time to union = 0.1595 × BMI + 5.1668 which means that every increase of 1 kg/m2 in BMI was suspected to lead to an increase in the time of healing by 0.1595 weeks (Fig. 3).
Fig. 3.
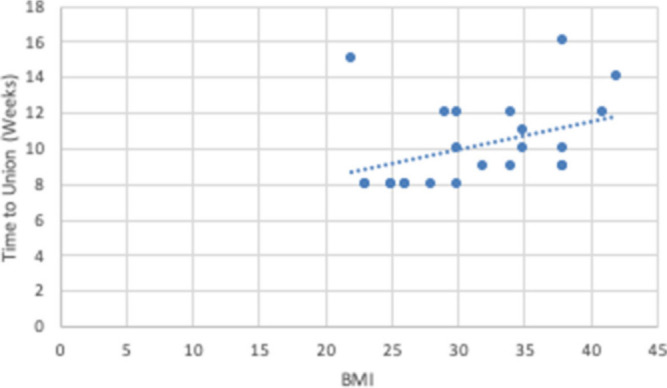
Correlation between body mass index (BMI) and time of union.
According to Lysholm score,8 there was a significant improvement six months after removal of the cast and with full weight-bearing postoperatively; 15 excellent (78.9%), two good (10.5%), one fair (5.2%) and one poor (5.2%), compared with two excellent (10.5%), three good (15.7%), nine fair (47.3%) and five poor (26.3%) preoperatively (Fig. 4).
Fig. 4.
Preoperative photograph (a) and long film (b) of 17-year-old male, with bilateral Blount’s disease. Photograph (c) and long film (d) six months after correction.
Limping, knee pain and sense of instability (lateral thrust) were improved in all of our patients. There were five patients (five legs) with complications (20%); under-correction was observed in two cases (two legs) (8%) (one underwent revision by osteotomy and fixation by a plate, and the second was satisfied by the result), superficial wound infection in two cases (two legs) (8%) (resolved by dressing and antibiotic without the need for debridement) and tingling in the lateral aspect of the leg in one case (one leg) (4%). There were no complications specific to the procedure.
Discussion
Patients with adolescent Blount’s disease usually present with marked genu varum. Although the procedure of choice for correction of this deformity is not fully agreed upon, the goal is to shift the mechanical axis of the lower limb from medial to lateral. Oblique high tibial osteotomy obtains correction with a simple procedure carried out as high as possible in the tibia to provide rapid union, quick remodelling and minimal proximal shaft deformity. It showed a good result for correction of complex deformity in infantile tibia vara whatever the degree of the deformity was. It is not the preferable method if there is a medial condyle depression or leg-length discrepancy.3
Nine tibiae with Blount’s disease were treated in this Rab series, with a single-plane oblique proximal tibial osteotomy allowing simultaneous correction of varus and internal rotation.3 All nine osteotomies achieved the desired correction of deformity. The same results in 14 tibiae treated with a similar technique were described by Kruse et al.9 The concept of the osteotomy was that the correction of a pure rotational deformity requires an osteotomy in the transverse plane. If pure varus-valgus correction is desired, the osteotomy must be in the frontal (coronal) plane. Flexion-extension correction requires a sagittal plane osteotomy. Because in most clinical deformities of Blount’s disease varus and internal rotation must be corrected, the osteotomy should have transverse and frontal plane components. An oblique osteotomy directed from antero-distal to postero-proximal corrects the deformity in both transverse and frontal planes.3
Rab4 in his last review of his technique, found that it is theoretically possible to modify the extent of angular correction in each plane by varying the angle of cut in the sagittal plane. He noticed that most cases of Blount’s disease have equal degrees of tibia vara and tibial internal rotation. For this reason, variations from a 45° upward cut have not proven to be necessary. As regarding orienting the plane of cut, informal reports from surgeons following the initial publication mentioned that excessive procurvatum of the tibia (beyond that which is typical of Blount’s disease) was seen with larger angular corrections. The procurvatum can be improved by basing the approach for the plane of cut collinear to the ankle and not the knee. In other words, the 45° upward cuts should be made proximally, based on the coordinate system of the distal tibia, not the proximal.
Elzohairy5 conducted the modification of the Rab osteotomy for correction of 17 patients with infantile tibia vara. The mean age at time of surgery was three years and six months. Correction of the deformity was achieved in all patients.
In this study, we conducted the modification of the Rab osteotomy, for the first time, in a case series study (not a theoretical study) for correction of adolescent tibia vara (not infantile tibia vara). We used a 45° upward cut collinear to the ankle not the knee, and fixation by two or three screws. An above knee cast was applied after that. The mean age at time of surgery was 17.23 years (sd 5.27; 12 to 30). Correction of the deformity was achieved in all of our patients except two patients who were under corrected. Union with no excessive procurvatum occurred in each patient. There were no deep infections and no instances of compartment syndrome. All patients regained their preoperative knee and ankle range of movement.
Several methods were described for management of tibia vara. Lateral hemiepiphesiodesis is used for children younger than ten years old with less preoperative varus angulation (average 15°).10-12 Opening and closing wedge proximal tibial osteotomies are generally used, together with dome and cheveron-type osteotomies.5 All authors performing metaphyseal osteotomy for Blount`s correction concluded that the metaphyseal osteotomy used to correct a physeal deformity results in the need for lateral translation at the osteotomy site, thus particularly in larger deformities it will be difficult to hold the correction with a plate.13-15
Asymmetrical physeal distraction with a monolateral fixator is also used for treatment of adolescent tibia vara. In all cases, the distraction had resulted in proximal tibial growth plate closure and carried risk of septic knee.16 Elevation of the medial tibial plateau is recommended for children older than six years of age, who have severe early-onset Blount’s disease and substantial posterior depression of the medial tibial plateau.17-19 Gradual correction with distraction osteogenesis appears to be a safe and reliable means of treating multiplanar deformities, including limb-length discrepancy, especially in obese patients.19-23
The Taylor Spatial Frame (TSF) and the multiaxial correction external fixation system are modern options that are more expensive than the procedure reported in this study. The advantages of these newer systems are that they allow correction of multiplanar deformities, lower rate of over or under correction due to the ability of adjustment of the struts in the clinic to have no residual deformity and simultaneous leg lengthening while allowing weight-bearing throughout the entire period of treatment. However, they are complicated and time-consuming treatment strategies that depend on the cooperation of the patient and their parents. The complication rate in TSF is 18%. Pin tract infection is the most common complication with external fixators which sometimes need debridement under anaesthesia. Close attention is required to avoid premature consolidation of the proximal osteotomy.24 Modified oblique high tibial osteotomy is considered successful and results in an acceptable correction of adolescent tibia vara in a relatively shorter time with lower rate of complication in comparison with TSF.
Modified oblique high tibial osteotomy with limited internal fixation is an effective method for treatment of adolescent tibia vara. It allows a proximal cut without damage to the apophysis of the upper tibial tubercle. It corrects both varus and internal rotation deformities in patients with Blount’s disease. The broad metaphyseal flat surface at the osteotomy sites allows rapid healing.
The drawback of this study is the limited number of patients we had. We need a greater number of patients with longer follow-up periods to be included in further studies.
Conclusion
Modified Rab osteotomy with minimal fixation by two or three screws shows promising results with good correction of varus deformity (coronal plane), internal torsion (axial plane) and procurvatum (sagittal plane), in management of adolescent tibia vara with minimal morbidity and complications.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all parents of the children included in the study.
ICMJE Conflict of interest statement
None declared.
Author Contributions
ASA: Conceived and designed the study, Managed cases, Collected data.
ARAA: Literature search, Managed cases.
HAF: Drafted the mansuscript, Shared in writing.
TAF: Acquisition, analysis and interpretation of data.
References
- 1. Janoyer M. Blount disease. Orthop Traumatol Surg Res 2019;105:S111-S121. [DOI] [PubMed] [Google Scholar]
- 2. Erlacher P. Deforming processes of the epiphyseal area in children. Arch Orthop Trauma Surg 1922;20:81-96. [Google Scholar]
- 3. Rab GT. Oblique tibial osteotomy for Blount’s disease (tibia vara). J Pediatr Orthop 1988;8:715-720. [DOI] [PubMed] [Google Scholar]
- 4. Rab GT. Oblique tibial osteotomy revisited. J Child Orthop 2010;4:169-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Elzohairy MM. Modified oblique proximal tibial osteotomy for deformity correction of tibia vara (Blount disease). Orthop Muscular Syst 2012;1:1-4. [Google Scholar]
- 6. Gordon JE, Heidenreich FP, Carpenter CJ, Kelly-Hahn J, Schoenecker PL. Comprehensive treatment of late-onset tibia vara. J Bone Joint Surg [Am] 2005;87-A:1561-1570. [DOI] [PubMed] [Google Scholar]
- 7. Seber S, Hazer B, Köse N, Göktürk E, Günal I, Turgut A. Rotational profile of the lower extremity and foot progression angle: computerized tomographic examination of 50 male adults. Arch Orthop Trauma Surg 2000;120:255-258. [DOI] [PubMed] [Google Scholar]
- 8. Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: international knee documentation committee (IKDC) subjective knee evaluation form, knee injury and osteoarthritis outcome score (KOOS), knee injury and osteoarthritis outcome score physical function short form (KOOS‐PS), knee outcome survey activities of daily living scale (KOS‐ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken) 2011;63(suppl 11):S208-S228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kruse RW, Bowen JR, Heithoff S. Oblique tibial osteotomy in the correction of tibial deformity in children. J Pediatr Orthop 1989;9:476-482. [PubMed] [Google Scholar]
- 10. Park SS, Gordon JE, Luhmann SJ, Dobbs MB, Schoenecker PL. Outcome of hemiepiphyseal stapling for late-onset tibia vara. J Bone Joint Surg [Am] 2005;87-A:2259-2266. [DOI] [PubMed] [Google Scholar]
- 11. Westberry DE, Davids JR, Pugh LI, Blackhurst D. Tibia vara: results of hemiepiphyseodesis. J Pediatr Orthop B 2004;13:374-378. [DOI] [PubMed] [Google Scholar]
- 12. Stevens PM. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop 2007;27:253-259. [DOI] [PubMed] [Google Scholar]
- 13. Martin SD, Moran MC, Martin TL, Burke SW. Proximal tibial osteotomy with compression plate fixation for tibia vara. J Pediatr Orthop 1994;14:619-622. [DOI] [PubMed] [Google Scholar]
- 14. Griswold B, Gilbert S, Khoury J. Opening wedge osteotomy for the correction of adolescent tibia vara. Iowa Orthop J 2018;38:141-146. [PMC free article] [PubMed] [Google Scholar]
- 15. Khalifa AA, Fadle AA, Alzohiry MA, Elsherif ME, Refai O. Medial wedge opening high tibial osteotomy (MWOHTO) with an extra screw fixation: a technical note. Int J Surg 2019;6:45-48. [Google Scholar]
- 16. de Pablos J, Franzreb M. Treatment of adolescent tibia vara by asymmetrical physeal distraction. J Bone Joint Surg [Br] 1993;75-B:592-596. [DOI] [PubMed] [Google Scholar]
- 17. Abraham E, Toby D, Welborn MC, Helder CW, Murphy A. New single-stage double osteotomy for late-presenting infantile tibia vara: a comprehensive approach. J Pediatr Orthop 2019;39:247-256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schoenecker PL, Johnston R, Rich MM, Capelli AM. Elevation of the medical plateau of the tibia in the treatment of Blount disease. J Bone Joint Surg [Am] 1992;74-A:351-358. [PubMed] [Google Scholar]
- 19. Hefny H, Shalaby H. A safer technique for the double elevation osteotomy in severe infantile tibia vara. Strategies Trauma Limb Reconstr 2010;5:79-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Alekberov C, Shevtsov VI, Karatosun V, Günal I, Alici E. Treatment of tibia vara by the Ilizarov method. Clin Orthop Relat Res 2003;409:199-208. [DOI] [PubMed] [Google Scholar]
- 21. Stanitski DF, Dahl M, Louie K, Grayhack J. Management of late-onset tibia vara in the obese patient by using circular external fixation. J Pediatr Orthop 1997;17:691-694. [DOI] [PubMed] [Google Scholar]
- 22. de Pablos J, Azcárate J, Barrios C. Progressive opening-wedge osteotomy for angular long-bone deformities in adolescents. J Bone Joint Surg [Br] 1995;77-B:387-391. [PubMed] [Google Scholar]
- 23. Stanitski DF, Dahl M, Louie K, Grayhack J. Management of late-onset tibia vara in the obese patient by using circular external fixation. J Pediatr Orthop 1997;17:691-694. [DOI] [PubMed] [Google Scholar]
- 24. Feldman DS, Madan SS, Koval KJ, et al. . Correction of tibia vara with six-axis deformity analysis and the Taylor Spatial Frame. J Pediatr Orthop 2003;23:387-391. [PubMed] [Google Scholar]